TLC City West 0692 nursing home inspection report - hiqa.ie
TLC City West 0692 nursing home inspection report - hiqa.ie
TLC City West 0692 nursing home inspection report - hiqa.ie
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
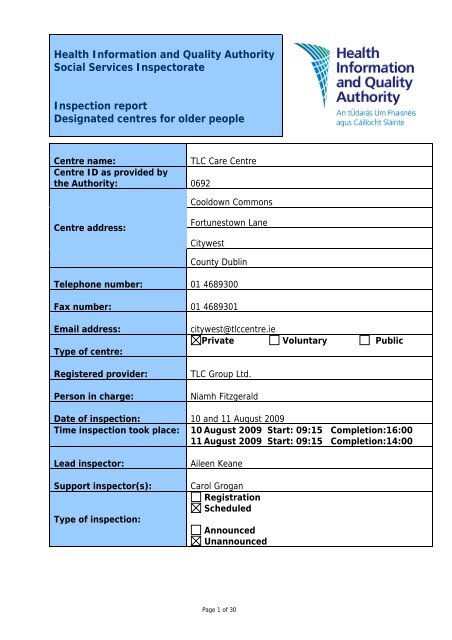
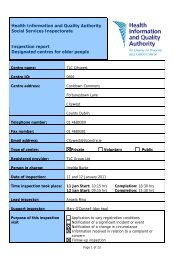
Health Information and Quality AuthoritySocial Services InspectorateInspection <strong>report</strong>Designated centres for older peopleCentre name:<strong>TLC</strong> Care CentreCentre ID as provided bythe Authority: <strong>0692</strong>Cooldown CommonsCentre address:Fortunestown Lane<strong>City</strong>westCounty DublinTelephone number: 01 4689300Fax number: 01 4689301Email address:Type of centre:Registered provider:Person in charge:citywest@tlccentre.<strong>ie</strong>Private Voluntary Public<strong>TLC</strong> Group Ltd.Niamh FitzgeraldDate of <strong>inspection</strong>: 10 and 11 August 2009Time <strong>inspection</strong> took place: 10 August 2009 Start: 09:15 Completion:16:0011 August 2009 Start: 09:15 Completion:14:00Lead inspector:Support inspector(s):Type of <strong>inspection</strong>:Aileen KeaneCarol GroganRegistrationScheduledAnnouncedUnannouncedPage 1 of 30
About <strong>inspection</strong>The purpose of <strong>inspection</strong> is to gather evidence on which to make judgments aboutthe fitness of the registered provider and to <strong>report</strong> on the quality of the service. Thisis to ensure that providers are complying with the requirements and conditions oftheir registration and meet the standards; that they have systems in place to bothsafeguard the welfare of service users and to provide information and evidence ofgood and poor practice.In assessing the overall quality of the service provided, inspectors examine how wellthe provider has met the requirements of the Health Act 2007, the Health Act 2007(Care and Welfare of Residents in Designated Centres for Older People) Regulations2009 and the National Quality Standards for Residential Care Settings for OlderPeople in Ireland under the following topics:1. Governance and leadership: how well the centre is organised.2. The quality of the service.3. How well the healthcare needs of residents are met.4. Premises and equipment: appropriateness and adequacy.5. Communication: information provided to residents, relatives and staff.6. Staffing: the recruitment, supervision and competence of staff.This <strong>report</strong> summarises the findings of the <strong>inspection</strong> under some or all of thesetopics, highlighting areas of good practice as well as areas where improvementswere required as follows:Evidence of good practice - this means that an acceptable standard was reachedand the provider demonstrated a culture of rev<strong>ie</strong>w and improvement and aimed todrive forward best practice.Some improvements required – this means that practice was generallysatisfactory but there were areas that need attention.Significant improvements required – this means that unacceptable practice wasfound.The <strong>report</strong> also identif<strong>ie</strong>s minor issues, where applicable, to which the providershould give consideration to enhance the quality of the service.The <strong>report</strong> is available to residents, relatives, providers of services and members ofthe public, and is published on our website www.<strong>hiqa</strong>.<strong>ie</strong>.AcknowledgementsThe inspectors wish to acknowledge the co-operation and assistance of the residents,relatives, provider and staff during the <strong>inspection</strong>.Page 2 of 30
About the centreDescription of services and premises<strong>TLC</strong> <strong>City</strong>west is a three story, purpose-built centre with 82 places. The residents usethe ground and first floors, as the second floor was not registered for use by theHealth Service Executive (HSE) under previous legislation. The accommodation on theground and first floors consists of 46 single rooms with en suite bathrooms and 18twin rooms with en suite bathrooms. There are three sitting rooms on the ground floorand seating is available at the reception area and also near the nurses’ station. Thereare two sitting rooms on the first floor and seating is available near the nurses’ station.The hairdressing salon, activit<strong>ie</strong>s room and oratory are located near the receptionarea. The dining room is on the ground floor and is open all day with tea/coffeemaking facilit<strong>ie</strong>s available for residents and visitors.There is an enclosed secure garden with a sheltered smoking area for residents, withseating and tables for their use in the garden area.Each floor has two bathrooms in addition to the en suite facilit<strong>ie</strong>s. These bathroomshave hydrotherapy baths with whirlpool features.There is car parking available to the front of the <strong>home</strong> for relatives and other visitors.Location<strong>TLC</strong> <strong>City</strong>west is located off Fortunestown Lane within ten minutes walk of <strong>City</strong>westshopping centre. The centre is within ten minutes drive of Saggart village.Date centre was first established: December 2008Number of residents on the date of<strong>inspection</strong> 39Dependency level of Max High Medium Lowcurrent residentsNumber of residents 10 10 7 12Management structureThe providers for this centre are Dr Liam Lacey and Michael Featherston. The Personin Charge, Niamh Fitzgerald, <strong>report</strong>s to them. The Clinical Nurse Manager 1 (CNM1),the <strong>nursing</strong> staff and the care staff <strong>report</strong> to the Person in Charge. Household andcatering staff <strong>report</strong> to a household and catering manager who <strong>report</strong>s to the Personin Charge.Page 3 of 30
StaffdesignationNumber ofstaff on dutyon day of<strong>inspection</strong>PersoninChargeNursesCarestaffCateringstaffCleaningandlaundrystaffAdminstaff1 3 6 3 3 2 0OtherstaffPage 4 of 30
Summary of findings from this <strong>inspection</strong>This was an unannounced <strong>inspection</strong>, carr<strong>ie</strong>d out over two days. The Authority’sCh<strong>ie</strong>f Inspector of Social Services received a copy of a complaint from a relativemade to the person in charge. The <strong>inspection</strong> was informed by this complaint andthe issues in it were considered by the inspectors during the <strong>inspection</strong>. On the dayof <strong>inspection</strong>, this complaint was discussed with the person in charge, who showedthe inspectors the complaint investigation <strong>report</strong> she had completed. The person incharge told the inspectors that she was awaiting the return of the provider fromannual leave in order to arrange a meeting with the complainant, to discuss thefindings of her investigation.The <strong>inspection</strong> was facilitated in a helpful and welcoming way by the person incharge and staff working at the centre. The inspectors spoke with the residents andrelatives, observed what happened in the centre and v<strong>ie</strong>wed records.Staff provided care to residents in a competent and respectful manner. However,there were significant improvements required in assessment and care planning forresidents, to ensure that all their needs were identif<strong>ie</strong>d and the appropriate careplans implemented for each resident. The medication management policy requiressignificant improvement to support the delivery of care and ensure all medicationsare available for residents when required.Residents could choose from a var<strong>ie</strong>ty of things to do in the centre and many of theresidents spoke positively about these activit<strong>ie</strong>s. There were some improvementsrequired in this area to ensure the participation and fulfilment of more highlydependant residents.The occupancy of the centre was at 50% of its registered capacity. This <strong>report</strong>identif<strong>ie</strong>s a number of areas of significant improvements required before fulloccupancy is reached, in order to ensure that residents receive a quality service andare safe.The person in charge was required to submit an Action Plan to the Authority withinten days, to ensure the accurate and timely assessment of residents and theimplementation of care plans, with particular attention to be given to the continuityof care from hospital to the <strong>nursing</strong> <strong>home</strong>.Residents’ and relatives’ commentsResidents told inspectors that they felt well cared for and that all of their needs weremet. Residents and relatives complimented the staff and said they were fr<strong>ie</strong>ndly. Oneresident said the staff were “hand picked”. A relative said “every member of staff isgreat from the cleaner to the matron. You can talk to them at any time”. Residentsalso said that they feel very safe because the staff are always available to them andthe staff answer the call bells promptly.Page 5 of 30
A number of the residents spoke very positively about the daily exercise class whichwas well attended; one resident said she “loves the exercise class”. They said theyhad made fr<strong>ie</strong>nds with other residents and that they enjoyed chatting.Relatives said they could visit the centre any time of the day. They told theinspectors that they had an opportunity to visit the centre prior to their familymember coming to live there. One relative described how her mother had “improvedso much since coming here. She is eating and drinking, interacting and is moresettled.”Residents and relatives spoke highly of the environment describing it as being “like ahotel”. One resident said she liked having her own room and bathroom with a bigshower.The relative who had made a written complaint expressed her concern about thequality of <strong>nursing</strong> care, quality of personal care and residents’ access to medicalservices. These issues were considered as part of the <strong>inspection</strong>.Page 6 of 30
Overall findings1. Governance: how well the centre is organisedOutcome: The centre is well organised and managed and compl<strong>ie</strong>s with therequirements of the Health Act 2007, the regulations and standards.Good governance involves the effective and effic<strong>ie</strong>nt deployment ofresources in accordance with the stated purpose and function of thecentre. Governance includes setting clear direction for the service, acommitment to continual improvement and having a system in place toeffectively assess and manage risk.Evidence of good practiceThe person in charge works full time at the centre and meets with one of theproviders on a weekly basis to discuss resident and management issues. Theprovider and person in charge said they discussed the staffing levels required tomeet residents’ needs, as the centre had not reached full capacity. The inspectorssaw an action plan which had been drawn up after one such meeting.Staff said they had received training on the National Quality Standards for ResidentialCare Settings for Older People in Ireland. Staff showed inspectors a photocopy of theNational Quality Standards for Residential Care Settings for Older People in Ireland,which was available on each floor.Following an audit of incidents and accidents, the person in charge introduced a fallsteam. The inspectors noted that this was a multidisciplinary team consisting of theperson in charge, a physiotherapist, a clinical nurse manager 1 (CNM1) and a careattendant. All falls were rev<strong>ie</strong>wed and risks for residents were identif<strong>ie</strong>d. Individualactions for residents were identif<strong>ie</strong>d and implemented to reduce their risk of falls.The inspectors saw monitoring information on falls, which suggested the incidents offalls had reduced since the introduction of the “Falls Team”.The inspectors v<strong>ie</strong>wed the health and safety statement, which was centre-specificand up-to-date.The provider had carr<strong>ie</strong>d out an investigation into the written complaint and hadproduced a <strong>report</strong> which was given to the inspectors. She had taken action toaddress issues and improve quality of life for residents.Page 7 of 30
Some improvements requiredThe polic<strong>ie</strong>s and procedures documents v<strong>ie</strong>wed by the inspectors were not specific tothe centre. One example was the missing person policy which stated “after 20minutes contact Northwood Park Security”. This was not the procedure for thiscentre.The person in charge showed the inspectors a computerised spreadsheet identifyingall staff training. This was not comprehensively completed. For example, it was notpossible to determine if all staff had received mandatory training in manual handling.The person in charge told the inspectors that this information was available andwould be put onto the system.There was no record of each resident’s personal property taken on admission to thecentre. The person in charge informed the inspectors on the second day of the<strong>inspection</strong> that a book had been ordered and a record of residents’ property wouldbe made.The person in charge had begun gathering information for monitoring areas such asmedication management, falls and <strong>nursing</strong> documentation. Data was not collected onresidents who had pressure sores, in-dwelling catheters and those takingpsychotropic drugs (including sleeping tablets) and those who exper<strong>ie</strong>nced significantweight loss.Significant improvements requiredThe register of residents rev<strong>ie</strong>wed by the inspectors was not in compliance with theHealth Act 2007 (Care and Welfare of Residents in Designated Centres for OlderPeople) Regulations 2009. The register v<strong>ie</strong>wed did not accurately reflect the currentnumber of residents in the centre on the day of the <strong>inspection</strong>.There was no written statement of purpose.The complaints policy was not in line with the Health Act 2007 (Care and Welfare ofResidents in Designated Centres for Older People) Regulations 2009. Residents andrelatives told inspectors that they would <strong>report</strong> any issues to a member of staff onduty or at the reception. Residents were not aware that there was a complaintspolicy. The complaints policy was on display on the wall near the visitors’ sign inbook, but was placed high on the wall and was not accessible to residents or visitorswho were unable to stand. A register of complaints was not maintained in the<strong>nursing</strong> <strong>home</strong> and there was no evidence of learning and improving practice as aresult of monitoring complaints.Page 8 of 30
2. Quality of the serviceOutcome: Residents receive a good standard of service, appropriatetreatment and are treated with courtesy and respect.A quality service is one where residents are protected from harm or abuse,where practice is person-centred, where rights are protected, whereresidents are enabled to play an active part in the centre and wheremanagement, staff and residents work together towards continuousimprovement.Evidence of good practiceThe inspectors saw that the privacy and dignity of residents was respected andpromoted by staff. Staff members knocked and waited before entering residents’bedrooms and ensured doors were closed and curtains drawn while deliveringpersonal care. The inspectors observed that the manner in which residents wereaddressed by staff was pleasant and respectful. Residents spoke highly of the staffwithin the <strong>home</strong>.There were eight communal areas of varying sizes throughout the centre. Theinspectors saw residents using these areas throughout the day. Many residents mettogether at the open seating area near the nurses’ desk at 11am for tea, coffee andsnacks. The snacks included a var<strong>ie</strong>ty of chopped fresh fruit, scones and biscuits.Residents sat and chatted with each other. They introduced other residents to theinspectors as fr<strong>ie</strong>nds. Tea, coffee and snacks were also taken by staff to other areas.The choice, quality and presentation of meals were of a high standard. Inspectorsobserved residents having their meals in a bright, relaxed environment. There was amix of rectangular and round tables and the seating arrangements were conducive tocommunication among residents. The tables were set with wine glasses, napkins,table mats and cutlery and residents were able to help themselves to condiments. Aselection of drinks such as cranberry juice, orange juice, milk and water were servedto residents by catering staff. The chef served the food from an open serving stationand portion sizes were adjusted in accordance with residents stated preference.A different member of staff was required to taste the food each day, prior to lunchbeing served, to ensure that it was of a high standard. Staff told the inspectors thatif there was a problem with the food, for example the gravy was too salty, it wouldbe returned to the kitchen and made again. All food was presented in an attractivemanner, including modif<strong>ie</strong>d consistency d<strong>ie</strong>ts. The inspectors joined the residents forlunch and found it appetising. Some relatives sat with residents at dinner time andsome assisted their family member to eat. Residents said meal times were enjoyable,social and relaxing occasions.Page 9 of 30
A resident told inspectors that she liked to dust and tidy her own room and wasgiven assistance by the care assistants and cleaning staff for more strenuous tasks,such as vacuuming and making the bed. Each resident has access to a telephone intheir bedroom, for use in private. Each bedroom has a television. There are radiosand televisions available in many of the communal rooms around the centre. Theinspectors noted that newspapers were available to residents.Some residents told inspectors about a recent trip to Newbridge and how theyenjoyed it. Residents also spoke of a recent party held in the centre for them andtheir famil<strong>ie</strong>s and said they all had a “great day”.Inspectors saw residents and relatives using the enclosed garden. Tables and chairswere provided in the garden and residents told inspectors that on a nice day they sitout and staff will bring them soft drinks.Some improvements requiredThe residents’ assessments and care plans did not fully utilise the sections for qualityof life and social interactions, or clearly outline the preferred routines andexpectations of the resident. There was no assessment of residents’ preferredrecreational activit<strong>ie</strong>s. The inspectors noted a “daily activit<strong>ie</strong>s/leisure activit<strong>ie</strong>s” careplan on each resident’s file. There was no record of residents’ likes or dislikes beingconsidered in the development of the general activity schedule and residents did notparticipate in its development. One resident told inspectors that day trips wereorganised and said that “they decide on a good place and they’ll see who wants togo”. During the morning, inspectors found that there were no activit<strong>ie</strong>s for residentsupstairs when the activit<strong>ie</strong>s coordinator was organising a game downstairs. Theactivit<strong>ie</strong>s coordinator organised and carr<strong>ie</strong>d out all activit<strong>ie</strong>s; if she was absent, therewas nothing for the residents to do. The focus was on activit<strong>ie</strong>s, rather thanfulfilment for residents.Up-to-date information on activit<strong>ie</strong>s was not available to residents on the day of<strong>inspection</strong>. Staff informed the inspectors that it is normally displayed, but was not yetcompleted for that week.Significant improvements requiredThere was no evidence that staff had received training on the prevention anddetection of elder abuse. There was no plan in place to provide this training.Minor issues to be addressedThere was no daily menu displayed for residents.Two residents told inspectors that sometimes they found the meat difficult to chewbut had not told anyone at the <strong>home</strong> about this.Page 10 of 30
Meals were not served in the dining room until all residents had arrived. This meantthat some residents were in the dining room for a long period before receiving theirlunch.3. Healthcare needsOutcome: Residents’ healthcare needs are met.Healthcare is integral to meeting individual’s needs. It requires thatresidents’ health, personal and social care needs are assessed andrev<strong>ie</strong>wed on an on-going basis, within a care planning process that isperson centred. Emphasis is firmly placed on health promotion,independence and meaningful activity.Evidence of good practiceInspectors saw that a general practitioner (GP) from a local practice attended thecentre each day, from Monday to Friday, to rev<strong>ie</strong>w residents as required. If residentsneeded medical attention outside of these times, the D-Doc service was contacted.Medical rev<strong>ie</strong>ws were recorded in the medical notes.The inspectors noted that residents looked well cared for. Residents told inspectorsthat their daily personal care needs were met. The inspectors found that residents’appearance, clothing, footwear, haircare and skincare needs were met.The activit<strong>ie</strong>s coordinator provided a daily exercise class in one of the large sittingrooms. Many of the residents chose to attend this and said they enjoyed it. Twovisitors stayed during the class. One resident told the inspector she felt her arm wasgetting better because of the exercise.The nurses carr<strong>ie</strong>d out phlebotomy as the doctor required. Six-monthly bloodsamples were taken for those who required regular monitoring. There was routinemonitoring of residents’ weights and blood pressure.A physiotherapist attended the centre once a week. All residents were assessed onadmission to determine if they need specialist physiotherapy. The person in chargeand provider aim to develop this service as occupancy increases.Staff were seen to adhere to best practice guidelines in the prevention of the spreadof infection.Some improvements requiredWhile drinks were frequently served to residents and fresh drinking water dispenserswere readily available throughout the building, these were not easily accessible to allresidents.Page 11 of 30
Significant improvements requiredCare plans were not begun in a timely manner for new residents (or those returningto the centre), to ensure continuity of care from the hospital to the centre. Careplans were not updated to reflect residents’ changing needs. Care plans were notbased on the individual person and were not suffic<strong>ie</strong>ntly detailed to understand theresidents’ current health or social care needs. One resident was not having her bloodsugar levels monitored in accordance with instructions received from the hospital.An inspector examined one resident’s records and found the information contained inthe assessment and care plan was conflicting. The assessment identif<strong>ie</strong>d that theresident was “immobile and wheelchair bound” yet the care plan recorded that thisresident required “supervision and assistance while walking”. The assessments andcare plans did not demonstrate that residents and/or relatives participated in andcontributed to the assessment and care plan development.The inconsistent and inaccurate recording of residents’ healthcare needs posed asignificant risk to residents’ safety as they might not receive necessary care andinterventions.The practice described by staff in relation to the ordering, administration anddisposal of medication was not in line with the centre’s medication policy. The centrehad introduced a computerised medication management system, which was linked tothe pharmacy suppl<strong>ie</strong>r. This process was not included in the medication managementpolicy.The inspectors identif<strong>ie</strong>d one instance where prescribed medication, “occasionallyrequired”, was not available when needed for a resident.Page 12 of 30
4. Premises and equipment: appropriateness and adequacyOutcome: The residential care setting provides premises and equipmentthat are safe, secure and suitable.A good physical environment is one that enhances the quality of life forresidents and is a pleasant place to live. It meets residents’ individual andcollective needs in a comfortable and <strong>home</strong>ly way, and is accessible, safe,clean and well-maintained. Equipment is provided in response to theassessed needs of each of the residents and maintained appropriately.Evidence of good practiceInspectors looked at some of the residents’ bedrooms, the communal bathrooms,sitting rooms, the laundry, the kitchen, dining room, garden and other communalareas.The inspectors saw that the centre met the needs of the residents as it was <strong>home</strong>ly,bright and clean throughout and was pleasantly furnished and decorated. Theentrance foyer provided a reception area with seating available for visitors andresidents. This was in use throughout the day. The hairdressing salon was located inthis area and a resident was having her hair done on the day of <strong>inspection</strong>. Thedining room was located near the entrance. This remained open throughout the day,with facilit<strong>ie</strong>s for residents and their visitors to meet and make tea or coffee.Corridors were wide and spacious, allowing residents to move around easily and forwheelchair users to pass safely.Inspectors noted that residents’ bedrooms were spacious and comfortable. Allbedrooms had en suite bathrooms with shower facilit<strong>ie</strong>s. There were baths availablein the assisted bathrooms. Staff told inspectors they would like to see residents usethe bath facilit<strong>ie</strong>s more frequently, but the current residents prefer to use the ensuite showers. Inspectors noted that some of the bedrooms had been personalisedby residents with their own belongings. Some of the arts and crafts produced by theresidents were on display in the activit<strong>ie</strong>s room.The inspectors found the kitchen was clean and well organised. There were adequateamounts of fresh and frozen foods available. Food stored in the fridges was labelledand dated. The inspector saw fresh soup being prepared. The inspectors saw thetraining records and noted that the chef had received Hazard Analysis and CriticalControl Points (HACCP) training.The laundry staff member was knowledgeable about her role and responsibilit<strong>ie</strong>s.She told inspectors how contaminated laundry was managed and this was in linewith best practice. There was a supply of labels for residents’ clothes available andresidents’ clothing was labelled in a discrete manner.Page 13 of 30
The inspectors saw a maintenance person attending to minor repairs. Staff membersrecorded any item for the attention of the maintenance staff.5. Communication: information provided to residents, relativesand staffOutcome: Information is relevant, clear and up to date for residents.Information is accessible, accurate, and appropriate to residents’ and staffneeds. Feedback is actively sought from residents and relatives and thisinforms future planning and service provision. Information is recorded andmaintained in accordance with legal requirements and best practice and iscommunicated to staff on a need to know basis to ensure residents’privacy is respected.Evidence of good practiceResidents and relatives told inspectors that they got on well with staff. Residents andrelatives said they received information about their care from the staff members asrequired. The inspectors observed staff talking to residents in a caring and respectfulmanner.Residents and famil<strong>ie</strong>s told inspectors they had an opportunity to visit the centreprior to the resident coming to live there.Regular staff meetings were held and a copy of the minutes of the meetings wasissued to all staff with their salary slip.Inspectors read the accidents/falls forms which recorded that relatives were informedwhen a resident had a fall.At the end of each shift, the staff nurse on duty completed a day/night duty <strong>report</strong>detailing changes to residents’ condition which was sent to the person in charge.Inspectors saw that there were agreements of care on file signed by residents and/orrelatives.Some improvements requiredThe <strong>nursing</strong> staff informed the chef of any resident’s d<strong>ie</strong>tary needs on admission andthese were recorded in a communication book. However, there was no formalcommunication between the kitchen and <strong>nursing</strong> staff for regular monitoring andupdating specific d<strong>ie</strong>tary requirements of residents.Page 14 of 30
Significant improvements requiredThere was no evidence that feedback was actively sought from residents on anongoing basis to inform future planning. While the person in charge said there areplans to develop a residents’ committee, this has not been implemented.There was no residents’ guide available.Page 15 of 30
6. Staff: the recruitment, supervision and competence of staffOutcome: Staff are competent and recruited in suffic<strong>ie</strong>nt numbers to meetresidents’ needsStaff numbers and skill-mix are determined by the size and complexity ofthe service and there should be suffic<strong>ie</strong>nt competent staff on duty, bothday and night, to meet the needs of residents. Robust recruitment andselection procedures ensure the appointment of suitably qualif<strong>ie</strong>d andexper<strong>ie</strong>nced staff. Staff are supported in their work by ongoing trainingand supervision.Evidence of good practiceThe inspectors observed that the number and the skill mix of the staff on duty on theday of the <strong>inspection</strong> was appropriate to the needs of the residents. There were tencare staff members on duty on the day: one person in charge, CNM1, two nurses,and six carers. Residents told inspectors that there were suffic<strong>ie</strong>nt care staff andnurses on duty for their needs and that staff were always available when needed.One relative said that her mother got up early in the morning and that staff wouldbring her a cup of tea and sit with her. Inspectors noted that call bells wereanswered promptly. The person in charge told inspectors that staffing levels werecontinually adjusted according to the dependency and number of residents.In discussions with inspectors, staff demonstrated a clear understanding of theirroles and responsibilit<strong>ie</strong>s. Nursing staff supervised the overall care residents received.Each day, a staff nurse was allocated to each floor and was responsible forsupervising and monitoring the care of residents on that floor. There were seniorcare attendant staff who supervised newly recruited or junior care staff.Some staff training had been provided in the areas of moving and handling residents,infection control, care planning, modif<strong>ie</strong>d consistency d<strong>ie</strong>ts and incontinencemanagement. One staff member told inspectors that as part of the training onmodif<strong>ie</strong>d consistency d<strong>ie</strong>ts, they exper<strong>ie</strong>nced being fed by another staff member (thistraining was provided by a speech and language therapist). The staff explained thiswas done so staff would know what it felt like for a resident who required assistancewith feeding.Some improvements requiredThe staffing rota did not clearly identify all staff on duty each day at the centre. TheCNM1 was not recorded on the rota for each day and staff might not know when asenior member of staff was expected on duty should a resident or relative request tomeet them. The person in charge and the CNM1 told the inspectors that they werecurrently rev<strong>ie</strong>wing the rota and exploring the introduction of team <strong>nursing</strong> for eachfloor.Page 16 of 30
Significant improvements requiredSeven staff files were rev<strong>ie</strong>wed by the inspectors. The information anddocumentation required by Schedule 2 of the Health Act 2007 (Care and Welfare ofResidents in Designated Centres for Older People) Regulations 2009 were not evidenton each file. Three staff members had no evidence of Garda Síochána vetting. Fourstaff had no evidence of references on their file. There was no evidence of a formalinduction programme for all staff.Report compiled byAileen KeaneInspector of Social ServicesSocial Services InspectorateHealth Information and Quality Authority13 October 2009Page 17 of 30
Health Information and Quality AuthoritySocial Services InspectorateAction PlanProvider’s response to <strong>inspection</strong> <strong>report</strong>Centre:<strong>TLC</strong> Care CentreCentre ID as provided bythe Authority: <strong>0692</strong>Date of <strong>inspection</strong>:DAY/MONTH/YEAR 10 and 11 August 2009Date of response:DAY/MONTH/YEAR 25 August 2009RequirementsThese requirements set out what the registered provider must do to meet the HealthAct 2007, the Health Act 2007 (Care and Welfare of Residents in Designated Centresfor Older People) Regulations 2009 and the National Quality Standards forResidential Care settings for Older People in Ireland.1. The provider is failing to comply with a regulatory requirement in thefollowing respect:Each resident’s needs were not set out in an individual care plan developed and agreedwith each resident.Action required:Ensure the assessment and care plans for residents are accurately and comprehensivelyrecorded and that the care plan developed from the assessment is agreed and formallyrev<strong>ie</strong>wed with each resident.Reference:Act: Health Act 2007Regulation 8: Assessment and Care PlanRegulation 9: Health CareStandard 10: Assessment and StandardStandard 11: The Resident’s Care PlanStandard 13: Health CarePage 18 of 30
Please state the actions you have taken or are planning totake with timescales:Timescale:Provider’s response:A meeting was held of all staff following the HIQA <strong>inspection</strong>(minutes of same forwarded)Adjustments have been made to our care plans to bring them intoline with the new regulations.This would include three monthly audits.The admission form has been changed to include initial assessmentof ADL’s. This aids in further development of care plans.Cl<strong>ie</strong>nt/family involvement will be clearly documented.A standard letter for family members, where indicated, will be a partof update and participation/development of the rev<strong>ie</strong>w of care planson an ongoing basis.2 The provider is failing to comply with a regulatory requirement in thefollowing respect:There was no appropriate policy or practice for ordering of medications.Action required:Maintain residents’ welfare and well-being by ensuring that there are appropriate andsuitable practices and written operational polic<strong>ie</strong>s relating to the ordering, storing andadministration of medication to residents.Reference:Act: Health Act 2007Regulation 33 (1): Ordering, Prescribing, Storing and Administering ofMedicinesStandard 14: Medication ManagementPlease state the actions you have taken or are planning totake with timescales:Timescale:Provider’s response:Medication policy has been expanded and developed relating tostoring and administration of medications.Our pharmacy provider has been contacted to assist in documentinginstructions and policy re: ordering medication and a rev<strong>ie</strong>wmeeting has been arranged with them to rev<strong>ie</strong>w all polic<strong>ie</strong>s andprocedures relating to medications in order to meet HIQAstandards.Page 19 of 30
3. The provider has failed to comply with a regulatory requirement in thefollowing respect:There were no arrangements (training or other measures), aimed at informing staff onthe prevention and detection of abuse.Action required:Deliver training to staff during their induction and provide ongoing training inprevention, detection and <strong>report</strong>ing of abuse.Reference:Act: Health Act 2007Regulation 6: General Welfare and ProtectionStandard 8: ProtectionPlease state the actions you have taken or are planning totake following the <strong>inspection</strong> with timescales:Timescale:Providers Response:The HSE DVD has been obtained re: elder abuse.Training sessions have been set up on initial weekly basis.The plan is for this module to be included on induction and incontinuing education re: elder abuse policy. All staff currentlyemployed at <strong>TLC</strong> <strong>City</strong>west will have participated in HSE module,Recognising and Responding to Elder Abuse in Residential CareSettings.Our policy and procedures document on elder abuse has beenupdated.End October 20094. The provider has failed to comply with a regulatory requirement in thefollowing respect:There were no arrangements to facilitate consultation and participation with residents inthe organisation of the designated centre.Action required:Ensure residents are consulted and participate in the organisation of the centre. Ensurefeedback is actively sought from residents on an ongoing basis to inform futureplanning.Reference:Act: Health Act 2007Regulation 10: Residents’ Rights, Dignity and ConsultationStandard 2: Consultation and ParticipationPage 20 of 30
Please state the actions you have taken or are planning totake with timescales:Timescale:Provider’s response:Our interpretation of the feedback from the inspectors on this actionrequired (No. 4), that <strong>TLC</strong> had failed to produce a feedback form forresidents and their famil<strong>ie</strong>s.Feedback forms developed.We are in the process of developing a residents council, we haveinvited both family members and next of kin to participate in thiscommittee if they so wish. This will be resourced by a <strong>TLC</strong> staffmember. It is also our intention as this council develops to seek theinvolvement of an external independent advocate.This concept is in keeping with <strong>TLC</strong> group policy.5. The provider is failing to comply with a regulatory requirement in thefollowing respect:There was no residents’ guide available.Action required:Produce a written residents’ guide, which contains the information as outlined in theHealth Act 2007 (Care and Welfare of Residents in Designated Centres For Older People)Regulations 2009.Reference:Act: Health Act 2007Regulation 21: Provision of Information to ResidentStandard 1: Information.Please state the actions you have taken or are planning totake with timescales:Timescale:Providers Response:Same being developedEnd October6. The provider is failing to comply with a regulatory requirement in thefollowing respect:The information and documentation required by Schedule 2 of the Health Act 2007 (Careand Welfare of Residents in Designated Centres for Older People) Regulations 2009were not evident on each staff file. Three staff members had no evidence of GardaSíochána vetting. Four staff had no evidence of references on their file. No staff hadevidence of their induction on file.Page 21 of 30
Action required:Obtain the information and documentation specif<strong>ie</strong>d in Schedule 2 of the Health Act2007 (Care and Welfare of Residents in Designated Centres for Older People)Regulations 2009 for each staff member.Reference:Act: Health Act 2007Regulation 18: RecruitmentStandard 22: RecruitmentPlease state the actions you have taken or are planning totake with timescales:Timescale:Providers Response:In keeping with the new regulations we are currently rev<strong>ie</strong>wing allstaff files and standardising information that is required on each <strong>TLC</strong>employee.End OctoberOur staff manual, including induction pack is currently under rev<strong>ie</strong>wand will be implemented immediately on completion.7. The provider is failing to comply with a regulatory requirement in thefollowing respect:The register of residents v<strong>ie</strong>wed did not accurately reflect the current number ofresidents in the centre on the day of the <strong>inspection</strong>.Action required:Establish and maintain a directory of residents.Reference:Act: Health Act 2007Regulation 23: Directory of ResidentsStandard 32: Register and Residents’ RecordsPlease state the actions you have taken or are planning totake with timescales:Timescale:Providers Response:We would like it reflected that this omission only referred to oneresident and this was immediately corrected.Same will be updated within 24 hours of cl<strong>ie</strong>nt’s admission.A policy is being put in place regarding same.Page 22 of 30
8. The provider is failing to comply with a regulatory requirement in thefollowing respect:The complaints policy was not in line with the Health Act 2007 (Care and Welfare ofResidents in Designated Centres for Older People) Regulations 2009. Residents were notaware that there was a complaints policy. A register of complaints was not maintained inthe <strong>nursing</strong> <strong>home</strong> and there was no evidence of learning and improving practice as aresult of monitoring complaints.Action required:Revise the complaints policy so that it is in line with the Health Act 2007 (Care andWelfare of Residents in Designated Centres for Older People) Regulations 2009 and isavailable to residents in an accessible format.Reference:Act: Health Act 2007Regulation Article 39: Complaints ProceduresStandard: 6: ComplaintsPlease state the actions you have taken or are planning totake with timescales:Timescale:Providers Response:On rev<strong>ie</strong>wing our complaints policy and taking cognisance of thenew regulations it has become clear to us that we need to compile anew policy and procedures document to take into account the needsof each resident and famil<strong>ie</strong>s.The complaints register that we had was in paper file. This wasshown to the designated inspectors. This has now been transferredto a computerised record system.We would like to bring to your notice that complaints/issue formswere always available at all nurses stations and at reception.We have taken great care to ensure that full information regardingcomplaints/issues will be included in the new residents informationpack.Page 23 of 30
9. The provider is failing to comply with a regulatory requirement in thefollowing respect:There was no written statement of purpose.Action required:Compile a statement of purpose which contains the matters as outlined in Schedule 1 ofthe Health Act 2007 (Care and Welfare of Residents in Designated Centres For OlderPeople) Regulations 2009.Reference:Act: Health Act 2007Regulation 5: Statement of PurposeStandard 28: Purpose and FunctionPlease state the actions you have taken or are planning totake with timescales:Timescale:Provider’s response:We have taken your observation on board and are in the process ofputting the finishing touches to this document.10. The provider has failed or is failing to comply with a regulatoryrequirement in the following respect:Some of the polic<strong>ie</strong>s and procedure documents rev<strong>ie</strong>wed were not specific to the centreand did not guide practice for staff, for example the missing person policy.Action required:Draw up polic<strong>ie</strong>s and procedures that are specific to this particular centre.Reference:Act: Health Act 2007Regulation 27: Operating Polic<strong>ie</strong>s and ProceduresStandard 29: Management SystemsPlease state the actions you have taken or are planning totake with timescalesProviders Response:A policy committee has been formed. This consists of Dr LiamLacey, CEO of <strong>TLC</strong> group, Ms Niamh Fitzgerald, DON <strong>TLC</strong> <strong>City</strong>west,Ms Niamh Carmody, CNM <strong>TLC</strong> <strong>City</strong>west.This committee is further resourced by Ms Ciara Hopper, DON <strong>TLC</strong>TimescaleTo be completedby 31 st January2010Page 24 of 30
Santry and Mrs Tanya Spellman, DON <strong>TLC</strong> Maynooth.The objectives of the committee is to systematically rev<strong>ie</strong>w andupdate all polic<strong>ie</strong>s relevant to <strong>TLC</strong> <strong>City</strong>west.11. The provider has failed or is failing to comply with a regulatoryrequirement in the following respect:It was not possible to determine if all staff had received mandatory training in movingand handling.Action required:Implement a system for monitoring of mandatory staff training which ensures training ismaintained and is up-to–date.Reference:Act: Health Act 2007Regulation 31: Risk Management ProceduresStandard 24: Training and SupervisionPlease state the actions you have taken or are planning totake with timescalesTimescaleProviders Response:We would like to assure HIQA that the mandatory training wascarr<strong>ie</strong>d out by all staff members. In keeping with your observationof not being able to determine this fact we have now updated ourTraining tracker.3 weeks12. The provider has failed or is failing to comply with a regulatoryrequirement in the following respect:There was no record of residents’ personal property.Action required:Create a record of residents’ personal property signed by the resident and this record iskept up to date.Reference:Act: Health Act 2007Regulation 7 (2): Residents’ Personal Property and PossessionsStandard 9: The Residents’ FinancesPage 25 of 30
Please state the actions you have taken or are planning totake with timescalesTimescaleProviders Response:This has now been rectif<strong>ie</strong>d in line with the new HIQA regulations.13. The provider has failed or is failing to comply with a regulatoryrequirement in the following respect:The preferred routines and expectations, likes and dislikes of residents were notrecorded.Action required:Develop systems for seeking and recording residents’ preferences in regard to theirroutines and expectations.Reference:Act: Health Act 2007Regulation 8: Assessment and Care PlanningStandard 18: Routines and ExpectationsStandard 2: Consultation and ParticipationPlease state the actions you have taken or are planning totake with timescalesTimescaleProviders Response:The record of preferred routine and expectations, likes and dislikesof residents which were held by activity co-ordinators have nowbeen added to the <strong>nursing</strong> notes as requested by the HIQAinspectors.This information is also being recorded in the quality of life andsocial interactions section of the care plans as per Action 1.Page 26 of 30
14. The provider has failed or is failing to comply with a regulatoryrequirement in the following respect:There was no evidence that residents participated in developing a programme for theiroccupation and recreation.Action required:Develop systems which allow each resident to contribute to the development of anactivit<strong>ie</strong>s programme appropriate to his or her interests and capabilit<strong>ie</strong>s.Reference:Act: Health Act 2007Regulation 10 (a) and (g): Residents’ Rights, Dignity and ConsultationStandard 18: Routines and ExpectationsStandard 2: Consultation and ParticipationPlease state the actions you have taken or are planning totake with timescalesTimescaleProviders Response:The record that residents participated in developing a program fortheir occupation and recreation and developing a residents programappropriate to his/hers capabilit<strong>ie</strong>s were recorded by the activit<strong>ie</strong>sco-ordinator on paper file. These records have now been placed inthe <strong>nursing</strong> files.In addition to this action it is also our intention to have this topicdiscussed at the residents council meetings.15. The provider has failed or is failing to comply with a regulatoryrequirement in the following respect:Fresh drinking water was not easily accessible to a few residents in some of thecommunal areas.Action required:Provide drinking water to residents in all areas of the centre.Reference:Act: Health Act 2007Regulation 20 (1): Food and NutritionStandard 19: Meals and MealtimesPage 27 of 30
Please state the actions you have taken or are planning totake with timescalesTimescaleProviders Response:Fresh piped filtered water is available at all nurses’ stations and inall dining areas. In keeping with the inspectors’ observations, anyresident who cannot access drinking water themselves is included inour regular beverage rounds or is suppl<strong>ie</strong>d with drinks on demand.Outside of this there is a policy that all residents, who cannotrequest drinks, would be offered fluids on a regular basis by staffmembers appointed to oversee their care.Page 28 of 30
RecommendationsThese recommendations are taken from the best practice described in theNational Quality Standards for Residential Care settings for Older People inIreland and the registered provider should consider them as a way ofimproving the service.StandardStandard 30QualityAssuranceandContinuousImprovementStandard 19Meals andMealtimesBest practice recommendationsFor the purpose of quality improvement, the person in charge shoulddevelop the areas of data collection to include residents who havepressure sores, in-dwelling catheters and receive psychotropic drugs(including sleeping tablets) and those who exper<strong>ie</strong>nce weight loss.Appropriate action should be taken in response to any findings ofconcern rising from the above.Develop a formal communication process with the catering/kitchen staffwhich ensures residents’ d<strong>ie</strong>tary preferences and special therapeuticd<strong>ie</strong>tary needs are monitored and rev<strong>ie</strong>wed.The daily menu should be displayed in a suitable format and in anappropriate location so that the residents or his/her representativeknows what is available at each meal.Seek resident feedback on meals and mealtimes, taking cognisance ofthe feedback given to the inspectors on the difficulty of chewing themeat and waiting for other residents before the meal is served.Page 29 of 30
Any comments the provider may wish to make:Provider’s response:The <strong>inspection</strong> was carr<strong>ie</strong>d out on the 10 th and 11 th of August 2009, all in all wefound dealing with the two HIQA inspectors very pleasant but stressful. This hasbeen a whole new exper<strong>ie</strong>nce for our management team. Given that the <strong>inspection</strong>was conducted using the new HIQA regulations as guidelines it became obvious to usat <strong>TLC</strong> <strong>City</strong>west that this process constitutes a whole new approach. This willobviously pose challenges for both ourselves and HIQA overall. The new <strong>report</strong>ingprocess seems to represent a more fair and accurate method of assessing our abilityto provide a safe and secure environment. At <strong>TLC</strong> <strong>City</strong>west it has always been apriority to provide accommodation for our residents which is a <strong>home</strong> from <strong>home</strong>.Dignity and respect are at the top of our agenda. We feel that we already providethis service and see the new health act and HIQA regulations as a positive support tohelp us ach<strong>ie</strong>ve and maintain our standards.We would like to take this opportunity to point out that we did not receive the HIQAinformation folder, Registration and Inspection of Residential Care Settings for OlderPeople in Ireland, or the pre-<strong>inspection</strong> questionnaire until two weeks post<strong>inspection</strong>.With regards to best practice recommendations, we have taken on board yoursuggestions and although these were already recorded in our records at the time ofyour <strong>inspection</strong> we undertake to continue to do regular audits and to have thisinformation available for use at each nurse’s station. This will obviously include anupdate in our action plan to be implemented as necessary.With regards to Standard 19 we would like to highlight that we continue to retain theservices of a D<strong>ie</strong>tician and SALT. These services are available to all our residents.Your observations regarding display of menu and feedback of information from bothresidents and famil<strong>ie</strong>s has been taken on board and questionnaires have beendesigned to ach<strong>ie</strong>ve this. In keeping with your own observations during the<strong>inspection</strong> (of staff tasting the food to ensure its quality prior to serving it), weintend to combine all this information to ensure that our resident’s d<strong>ie</strong>taryrequirements are maintained at the high standard they are used to.We would like to take this opportunity to wish your inspectors and HIQA success intheir task and we look forward to working with you to ach<strong>ie</strong>ve best practice in ourresidential care setting.Signed: Dr Liam LaceyRegistered ProviderPage 30 of 30