Pediatric Direct Admission Forms
Pediatric Direct Admission Forms
Pediatric Direct Admission Forms
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
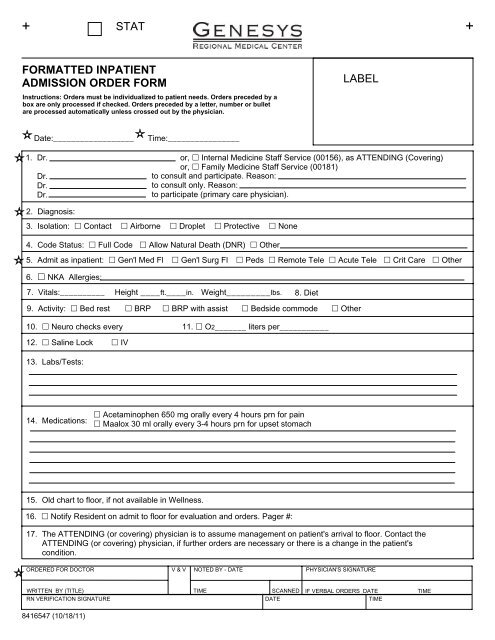
+ STAT +FORMATTED INPATIENTADMISSION ORDER FORMInstructions: Orders must be individualized to patient needs. Orders preceded by abox are only processed if checked. Orders preceded by a letter, number or bulletare processed automatically unless crossed out by the physician.LABELDate:__________________1. Dr.Dr.Dr.Dr.or, Internal Medicine Staff Service (00156), as ATTENDING (Covering)or, Family Medicine Staff Service (00181)to consult and participate. Reason:to consult only. Reason:to participate (primary care physician).2. Diagnosis:4. Code Status: Full Code Allow Natural Death (DNR) Other5. Admit as inpatient: Gen'l Med Fl Gen'l Surg Fl Peds Remote Tele Acute Tele Crit Care Other6. NKA Allergies:8. Diet9. Activity: Bed rest BRP BRP with assist Bedside commode Other10. Neuro checks every 11. O2_______ liters per___________12. Saline Lock IV13. Labs/Tests:Time:________________3. Isolation: Contact Airborne Droplet Protective None7. Vitals:__________ Height ____ft.____in. Weight_________lbs.14. Medications: Acetaminophen 650 mg orally every 4 hours prn for pain Maalox 30 ml orally every 3-4 hours prn for upset stomach15. Old chart to floor, if not available in Wellness.16. Notify Resident on admit to floor for evaluation and orders. Pager #:17. The ATTENDING (or covering) physician is to assume management on patient's arrival to floor. Contact theATTENDING (or covering) physician, if further orders are necessary or there is a change in the patient'scondition.ORDERED FOR DOCTOR V & V NOTED BY - DATE PHYSICIAN'S SIGNATUREWRITTEN BY (TITLE) TIME SCANNED IF VERBAL ORDERS DATE TIMERN VERIFICATION SIGNATURE DATE TIME8416547 (10/18/11)
PEDS GENERAL ADMISSION ORDERSInstructions: Orders must be individualized to patient needs. Orders preceded by a boxare only processed if checked. Orders preceded by a letter, number or bullet areprocessed automatically unless crossed out by the physician.Date: ________________________Time: _____________________Labs:Hematology£ Complete blood cell count with automated white blood cell differential£ C-reactive protein (CRP)£ Erythrocyte sedimentation rate (ESR)£ Reticulocyte countPanels£ Basic metabolic panel (BUN, Creatinine, Sodium, Potassium, CO2, Chloride, Glucose, Calcium)£ Comprehensive Metabolic Panel (Albumin, Alkaline Phosphatase, Bilirubin, BUN, Calcium, CO2, Chloride, Creatinine,Glucose, Potassium, Protein, Sodium, SGOT, SGPT)Microbiology£ Culture, blood£ Culture, urine clean catch£ Culture, urine (via straight catheterization)Urinalysis£ Urinalysis (UA) with microscopyRadiology:£ Chest, 2 viewsConsults:£ Consult to case management£ Consult to social servicesK1028167 11-16-11 Page 3 of 3
PEDS ASTHMA ADMISSION ORDERSInstructions: Orders must be individualized to patient needs. Orders preceded by a boxare only processed if checked. Orders preceded by a letter, number or bullet areprocessed automatically unless crossed out by the physician.KDate: ________________________K1028169 11-23-11 Page 1 of 3Time: _____________________Diagnosis: Acute Status Asthmaticus Condition £ Stable / GoodKKAllergies: £ NKAK£ FairThe content below was developed to facilitate computerized provider order entry (CPOE) and the application ofevidence-based medicine. This content is not a substitute for clinical judgment and individual patient treatment mayrequire adaptation as determined by the treating physician(s).Admit as Inpatient to: £ <strong>Pediatric</strong>s general floor £ Place in <strong>Pediatric</strong> Observation Unit£ Admitting Physician _________________________ Pager # __________________Phone # _________________£ Other: ____________________________________________________________________Vital Signs: (Temperature, HR, RR, BP, SpO2) £ every 2 hours £ every 4 hours £ routine every 6 hoursDiet:£ Diet, regular per home routine £ NPO except medications £ Clear liquids and advance to regular diet as toleratedActivity:£ As tolerated £ Bed rest with bathroom privileges £ Respiratory isolation (Droplet) £ Contact precautionsNursing Orders:Assessments• Measure height at admission• Measure weight at admission£ Measure head circumference once at admission (indicated for children less than 2 years)Pulse oximetry£ continuous£ check with vitals£ check with breathing treatment£ Cardiac pulmonary monitorContingency• Notify provider if oxygen initiated and document room air SpO2.• Notify provider if evidence of Albuterol toxicity, including heart rate greater than 40 beats above baseline• Notify provider if no clinical response to Albuterol• Supplemental oxygen titration to keep SpO2 greater than or equal 92%. Nurse or RT may select device best tolerated.• Wean O2 for SpO2 over 95% in acute stage, once the patient starts to clinically improve wean if SpO2 92%.• Pulse oximetry may be discontinued if SpO2 greater than or equal to 90% on room air for 4 hours.£ Oxygen cylinder for ambulation: dispense and instruct patient/caregiver on use£ Measure intake and output£ strict£ routine every shift£ Notify provider if new temperature greater than 38.3 C or 101F.• Notify provider if O2 required is FIO2 over 50% via mask and/or more than 2L via nasal cannula (in age less than 2 yrs).• Notify provider if post treatment peak flow is in the red zone (50% or less than predicted)Education• Discuss symptom recognition and management with the patient and/or family members• Discuss trigger avoidance with the patient and/or family members• Smoking cessation counseling should be provided to smokers including caretakers and parents• JC Disease Specific Core Performance Measure• Patient Education regarding <strong>Pediatric</strong> Asthma• Environmental tobacco-smoke exposure - nurse to provide printed information to caregiver/patient
PEDS ASTHMA ADMISSION ORDERSInstructions: Orders must be individualized to patient needs. Orders preceded by a boxare only processed if checked. Orders preceded by a letter, number or bullet areprocessed automatically unless crossed out by the physician.Date: ________________________Time: _____________________Respiratory:• Measure peak expiratory flow before and after treatments while awake for ages greater than 5 years. Please documentpredicted green zone parameters.• SVN request, follow <strong>Pediatric</strong> Bronchodilator ProtocolE V I D E N C E B A S E D G U I D E L I N EPlace patient on the <strong>Pediatric</strong> Bronchodilator ProtocolQualifying patients meet all these criteria: Admit to <strong>Pediatric</strong>s Observation Unit, Over 12 months oldDiagnosis: Acute Status AsthmaticusPatient has been evaluated and does not require continuous Albuterol of the time of initiation of Protocol.Exclusion criteria include any of the following: history of intubation for status asthmaticus, active heart disease, homeoxygen therapy, tracheostomy, chronic lung disease other than asthma, or significant neuromuscular disorder.RT to assess the patient and document Asthma Score at the start of the protocol and with every subsequent assessmentuntil patient is tolerating Albuterol 2.5 mg via small volume nebulizer or 2 puffs via MDI every 4 hours times 2 treatments£ Small Volume Nebulizer only option - remember to contact case management for home nebulizer machine if patient doesnot currently have one in good working order£ Small Volume Nebulizer to MDI option - when Albuterol is weaned to 2.5 mg every 4 hours, please change patient toAlbuterol MDI with spacer at dose of 2 puffs every 4 hours and label.£ MDI only optionIV Fluids:17 years and youngerWeight______________kgIV FLUIDS£ IV FLUID BOLUS DEHYDRATION_______ml of 0.9% Sodium Chloride IV(20 ml/kg/dose)£ IV MAINTENANCE(for patient with normal serum Sodium and Potassium)Gray3 kg4 kg5 kg60 ml (3 kg)80 ml (4 kg)100 ml (5 kg)13 ml (3 kg)______ml/hr of D5/0.2% Sodium Chloride with 20 mEq KCl/1,000 ml 17 ml (4 kg)21 ml (5 kg)______ml/hr of D5/0.2% Sodium Chloride with 20 mEq KCI/1,000 ml______ml/hr of D5/0.3% Sodium Chloride with 30 mEq KCI/1,000 ml______ml/hr of D5/0.45% Sodium Chloride with 40 mEq KCI/1,000 mlPink6-7kg130 ml27 mlRed8-9kg160 ml35 mlPurple10-11kg200 ml42 mlYellow12-14kg240 ml47 mlWhite15-18kg300 ml52 mlBlue19-23kg400 ml63 mlOrange24-29kg500 ml69 mlGreen30-36kg650 ml88 mlTan37-45kg900 ml 1000 ml96+ mlTealAdultover 45kgMedications:Albuterol weight-based dosing£ weight under 5 kg administer 1.25 mg (0.25 ml) SVN£ weight 5-10 kg administer 2.5 mg (0.5 ml) SVN£ weight under 5 kg administer 5 mg per hour continuously SVN£ weight 5-10 kg administer 10 mg per hour continuously SVNMedications continued on page 31028169 11-23-11 Page 2 of 3
PEDS ASTHMA ADMISSION ORDERSInstructions: Orders must be individualized to patient needs. Orders preceded by a boxare only processed if checked. Orders preceded by a letter, number or bullet areprocessed automatically unless crossed out by the physician.Date: ________________________Time: _____________________Medications:17 years and youngerPAIN AND FEVER MEDICATIONS£ Acetaminophen FEVER/PAIN_______mg rectally every 4-6 hrs PRN fever/pain(10-15 mg/kg/dose) Max dose=2600 mg/24 hrs£ Acetaminophen_______mg orally every 4-6 hrs PRN fever/pain(10-15 mg/kg/dose) Max dose=90 mg/kg/24 hrs£ Acetaminophen with Codeine *Age over 3 years PAIN_______mg Codeine orally every 4-6 hrs PRN pain(0.5-1 mg codeine/kg/dose) Max dose=360 mg/24 hrs£ Ibuprofen *Age 6 months FEVER/PAIN_______mg orally every 6-8 hrs PRN fever/pain(5-10 mg/kg/dose)Gray3 kg4 kg5 kg40 mg (3 kg)40 mg (4 kg)60 mg (5 kg)*Leukotriene Receptor AntagonistsMontelukast£ 4 mg granules orally once a day, in the evening age 2-5 years (Age, not weight-based dosing)£ 5 mg chew tablet orally once a day, in the evening age 6-14 years (Age, not weight-based dosing)£ 10 mg tablet orally once a day, in the evening age 15 years or older (Age, not weight-based dosing)Systemic CorticosteroidsE V I D E N C E B A S E D G U I D E L I N EA systemic corticosteroid should be administeredMethylprednisolone£______mg (1 mg/kg per dose) IV every 12 hours (maximum 30 mg per dose)£______mg (2 mg/kg per dose) IV once a day, in the AM (maximum 60 mg per dose)Prednisone tablet£______mg (1 mg/kg per dose) orally every 12 hours (maximum 30 mg per dose)£______mg (2 mg/kg per dose) orally once daily (maximum 60 mg per dose)Prednisolone liquid£______mg (1mg/kg per dose) orally or by feeding tube every 12 hours (maximum 30 mg per dose)£______mg (2 mg/kg per dose) orally or by feeding tube once daily (maximum 60 mg per dose)Vaccines• Influenza vaccine prior to discharge. Complete influenza vaccine order form.Consults: £ Consult to case management £ Consult to social services £ Consult <strong>Pediatric</strong> IntensivistRefer to the back of this page for Discharge Criteria and Discharge InstructionsKWeight______________kgORDERED FOR DOCTOR V & V NOTED BY - DATE PHYSICIAN'S SIGNATURE**Pink6-7kg*50 mgRed8-9kg*80 mgPurple10-11kg*100 mgYellow12-14kg80 mg 120 mg 120 mg 160 mg12 mg100 mgWhite15-18kg200 mg12 mg150 mgBlue19-23kg240 mg18 mg180 mgOrange24-29kg320 mg24 mg200 mgGreen30-36kg400 mg30 mg300 mgTan37-45kg480/500 mg36 mg300 mgTealAdultover 45kg325to650 mg15 to60 mg200 to600 mgWRITTEN BY (TITLE) TIME SCANNED1028169 11-23-11 Page 3 of 3 FRONTIF VERBAL ORDERS DATETIME
DISCHARGE CRITERIA• Patient is not in any distress• Able to maintain oral intake• Albuterol need is less than 6 times/24 hours• Oxygen saturation over 92% on room air• Asthma family education have completed• Reliable caregiverDISCHARGE INSTRUCTIONS• Diet: Normal for age• Activity: as tolerated• Medications:• Follow-up with primary care physician in______days• Asthma clinic in ______week(s).1028169 Page 3 BACK
PEDS BRONCHIOLITIS ADMISSION ORDERSInstructions: Orders must be individualized to patient needs. Orders preceded by a boxare only processed if checked. Orders preceded by a letter, number or bullet areprocessed automatically unless crossed out by the physician.KDate: ________________________KTime: _____________________Diagnosis: Viral Bronchiolitis Condition £ Stable / Good£ FairKKThe content below was developed to facilitate computerized provider order entry (CPOE) and the application ofevidence-based medicine. This content is not a substitute for clinical judgment and individual patient treatment mayrequire adaptation as determined by the treating physician(s).Admit as Inpatient to: £ <strong>Pediatric</strong>s general floor £ Place in <strong>Pediatric</strong> Observation Unit£ Admitting Physician ___________________________ Pager # ___________________Phone # ___________________Allergies: £ NKA£ Other: _________________________________________________________________________Vital Signs: (Temperature, HR, RR, BP, SpO2) £ every 2 hours £ every 4 hours £ routine every 6 hoursDiet:£ Diet, regular for age £ Clear liquids and advance as tolerated £ NPO except medications £ Tube feedingActivity:£ Age appropriate activity as tolerated £ Contact precautions £ Respiratory isolation (Droplet)PNursing Orders:Assessments• Measure height – once at admission£ Measure weight – once at admission once a day in morning£ Measure head circumference once at admission (indicated for children less than 2 years)Pulse oximetry£ continuous£ with each set of vitals£ Cardiac apnea monitor• Measure intake and output£ routine£ strict£ Bronchiolitis Score on admission and every shift (See back for Bronchiolitis Assessment Score)Contingency• Smoking cessation counseling should be provided to smokers including caretakers and parents• Notify provider if oxygen initiated and document room air SpO2.• Notify provider if FIO2 over 50% via mask and/or more than 2L nasal cannula O2 required (age less than 2 years)• Pulse oximetry may be discontinued if SpO2 greater than or equal to 90% on room air for 4 hours. Then spot check withvitals.• Education, disease process or condition regarding <strong>Pediatric</strong> Bronchiolitis.• Education, smoking cessation – nurse to provide information to caregiver / patient.E V I D E N C E B A S E D G U I D E L I N ERoutine chest x-ray not generally indicatedRoutine inhaled bronchodilators provide no clinical benefit-Continue only if documented benefitInhaled corticosteroids provide no clinical benefitViral studies are not routinely indicated1028166 12-6-11 Page 1 FRONT of 3Nursing Orders: continued on page 2
_____________________________________________________________________________________________BRONCHIOLITIS ASSESSMENT TOOL_____________________________________________________________________________________________Respiratory Assessment Mild Moderate SeverePulse ox in room air 95% or over 91-94% 90% or underRespiratory rate Under 60 60-70 over 70Mental status Normal Irritable but active LethargicFeeding Normal Less but adequate PoorIncreased WOBRetractions Minimal/None Intercostal SubsternalAccessory musclesNeck or abdominal musclesWheeze Minimal/None Moderate expiratory Severe inspiratory/expiratory_____________________________________________________________________________________________Air exchange Good, equal BS Localized decreased BS Multiple areas decreased_____________________________________________________________________________________________Classification of severity by using assessment toolSingle SeverityMild5 or over factors in the Mild categoryModerate5 or over factors in the Moderate categorySevere5 or over factors in the Severe categoryMixed SeverityMild/Moderate Majority of factors are in Mild and Moderate categories_____________________________________________________________________________________________Moderate/Severe Majority of factors are in Moderate and Severe categories_____________________________________________________________________________________________Measuring response to Albuterol/Racemic epi using the assessment tool_____________________________________________________________________________________________Improvement noted in at least 3 of 7 categoriesBronchiolitis High Risk Group• Prematurity• Chronic Lung Disease• Congenital Heart Disease• Congenital Airway Anamolies• Immune Deficiency• Cystic Fibrosis• Neuromuscular Disease1028166 12-6-11 Page 1 BACK
PEDS BRONCHIOLITIS ADMISSION ORDERSInstructions: Orders must be individualized to patient needs. Orders preceded by a boxare only processed if checked. Orders preceded by a letter, number or bullet areprocessed automatically unless crossed out by the physician.Date: ________________________Time: _____________________Nursing Orders: continuedInterventions• Supplemental oxygen titration to keep SpO2 greater than 94%. Nurse or RT may select device best tolerated.• Once the patient improves clinically, wean oxygen for SpO2 greater than 92%.• Saline nasal drops and suctioning every 2 hours as needed for congestion. Nurse to instruct caregiver on proper technique.£ Nasogastric/orogastric tube insertion/management£ Once patient improves, continuous pulse oximetry is not indicatedIV Fluids: Bolus (Consider NG feeding rather than IV fluids)17 years and youngerWeight______________kgIV FLUIDSGray3 kg4 kg5 kgPink6-7kgRed8-9kgPurple10-11kgYellow12-14kgWhite15-18kgBlue19-23kgOrange24-29kgGreen30-36kgTan37-45kgTealAdultover 45kg£ IV FLUID BOLUS DEHYDRATION_______ml of 0.9% Sodium Chloride IV(20 ml/kg/dose)£ IV MAINTENANCE(for patient with normal serum Sodium and Potassium)60 ml (3 kg)80 ml (4 kg)100 ml (5 kg)130 ml160 ml200 ml240 ml300 ml400 ml500 ml650 ml900 ml 1000 ml______ml/hr of D5/0.2% Sodium Chloride with 20 mEq KCl/1,000 ml13 ml (3 kg)17 ml (4 kg)21 ml (5 kg)27 ml35 ml______ml/hr of D5/0.2% Sodium Chloride with 20 mEq KCI/1,000 ml______ml/hr of D5/0.3% Sodium Chloride with 30 mEq KCI/1,000 ml______ml/hr of D5/0.45% Sodium Chloride with 40 mEq KCI/1,000 ml42 ml47 ml52 ml63 ml69 ml88 ml96+ mlRespiratory:Respiratory SVN request, institute <strong>Pediatric</strong> Bronchodilator Protocol£ Albuterol trial x one or two treatments, continue if documented improvementAlbuterol weight-based dosing£ weight under 5 kg administer 1.25 mg (0.25 ml) SVN£ weight 5-10 kg administer 2.5 mg (0.5 ml) SVN£ weight under 5 kg administer 5 mg per hour continuously SVN£ weight 5-10 kg administer 10 mg per hour continuously SVNRacemic Epinephrine (Racepinephrine) 2.25%-0.5 ml for inhalation£ Weight under 5 kg place 0.25 ml in Sodium Chloride 0.9% to a total volume of 2.5 ml via SVN, PRN Croup Score£ Weight 5-10 kg place 0.5 ml in Sodium Chloride 0.9% to a total volume of 2.5 ml via SVN, PRN Croup Score£ Dilute Racemic Epinephrine dose with 3% Sodium Chloride to total volume of 2.5 ml via SVN, PRN Croup Score£ Nebulized 3% Saline:£ 3 ml every 2 hours x 3£ 3 ml every 4 hours x 4£ 3 ml every 6 hours x 6 till discharge.1028166 12-6-11 Page 2 of 3
PEDS BRONCHIOLITIS ADMISSION ORDERSInstructions: Orders must be individualized to patient needs. Orders preceded by a boxare only processed if checked. Orders preceded by a letter, number or bullet areprocessed automatically unless crossed out by the physician.Date: ________________________Time: _____________________Medications:• Sodium Chloride 0.65% (soln) Nasal Drops every 2 hours PRN nasal congestion followed by bulb suction17 years and youngerWeight______________kgPAIN AND FEVER MEDICATIONS£ Acetaminophen FEVER/PAIN_______mg rectally every 4-6 hrs PRN fever/pain(10-15 mg/kg/dose) Max dose=2600 mg/24 hrs£ Acetaminophen_______mg orally every 4-6 hrs PRN fever/pain(10-15 mg/kg/dose) Max dose=90 mg/kg/24 hrs£ Acetaminophen with Codeine *Age over 3 years PAIN_______mg Codeine orally every 4-6 hrs PRN pain(0.5-1 mg codeine/kg/dose) Max dose=360 mg/24 hrs£ Ibuprofen *Age 6 months FEVER/PAIN_______mg orally every 6-8 hrs PRN fever/pain(5-10 mg/kg/dose)Gray3 kg4 kg5 kg40 mg (3 kg)40 mg (4 kg)60 mg (5 kg)***Pink6-7kg80 mg*50 mgRed8-9kg120 mg 120 mg*80 mgPurple10-11kg*100 mgYellow12-14kg160 mg12 mg100 mgWhite15-18kg200 mg12 mg150 mgBlue19-23kg240 mg18 mg180 mgOrange24-29kg320 mg24 mg200 mgGreen30-36kg400 mg30 mg300 mgTan37-45kg480/500 mg36 mg300 mgTealAdultover 45kg325to650 mg15 to60 mg200 to600 mgLab:Microbiology£ Viral antigens, nasopharyngeal respiratory syncytial virus (RSV)£ Viral antigens, nasopharyngeal viral respiratory panel (VRP)£ Rapid Test for Influenza A and B antigen detection (nasopharyngeal swab)Radiology:£ Chest, 1 view portable £ Chest, 2 viewsConsults:£ Consult to case management£ Consult to social servicesRefer to the back of this page for Discharge Criteria and Discharge Instructions.K1028166 12-6-11 Page 3 of 3 FRONT
DISCHARGE CRITERIA• Respiratory rate under 70 per minute• Oxygen saturation over 92% on room air• Able to drink/eat without difficulty• Reliable caregiverDISCHARGE INSTRUCTIONS• Diet: Normal for age• Activity: as tolerated• Medications:• Follow-up with primary care physician in______days1028166 Page 3 BACK
PEDS CROUP ADMISSION ORDERSInstructions: Orders must be individualized to patient needs. Orders preceded by a boxare only processed if checked. Orders preceded by a letter, number or bullet areprocessed automatically unless crossed out by the physician.KDate: ________________________KTime: _____________________Diagnosis: Croup Condition £ Stable / Good£ FairKKThe content below was developed to facilitate computerized provider order entry (CPOE) and the application ofevidence-based medicine. This content is not a substitute for clinical judgment and individual patient treatment mayrequire adaptation as determined by the treating physician(s).Admit as Inpatient to: £ <strong>Pediatric</strong>s general floor £ Place in <strong>Pediatric</strong> Observation Unit£ Admitting Physician _________________________ Pager # __________________Phone # ______________Allergies: £ NKA£ Other: _________________________________________________________________________Vital Signs: (Temperature, HR, RR, BP, SpO2) £ every 2 hours £ every 4 hours £ routine every 6 hoursDiet:£ Diet, regular for age £ NPO except medications £ Tube feedingActivity:£ As tolerated £ Bed rest £ Respiratory isolation (Droplet) £ Contact isolationNursing Orders:Assessments• Measure height on admissionMeasure weight£ once at admission£ once a day£ Measure head circumference once at admission (indicated for children less than 2 years)Pulse oximetry£ continuous£ routine with vitals£ Cardiac apnea monitorMeasure intake and output£ every shift£ every 6 hours strict£ Croup Score on admission and every shift (See back for Croup Score)Contingency• Notify provider if oxygen initiated and document room air SpO2.• Supplemental oxygen titration to keep SpO2 greater than 94%. Nurse or RT may select device best tolerated.• Wean O2 for SpO2 over 95% if patient acutely ill keep SpO2 greater than 95%, however once improved keep over 92%.• Pulse oximetry may be discontinued if SpO2 greater than or equal to 90% on room air for 4 hours.• Education, disease process or condition regarding <strong>Pediatric</strong> croup.£ Notify provider if new temperature greater than 38.3 C or 101F.• Education, smoking cessation – nurse to provide information to caregiver / patient.E V I D E N C E B A S E D G U I D E L I N ERoutine use of humidified air is not recommended1028173 11-23-11 Page 1 of 3
PEDS CROUP ADMISSION ORDERSInstructions: Orders must be individualized to patient needs. Orders preceded by a boxare only processed if checked. Orders preceded by a letter, number or bullet areprocessed automatically unless crossed out by the physician.Date: ________________________Time: _____________________IV Fluids:17 years and youngerWeight______________kgIV FLUIDS£ IV FLUID BOLUS DEHYDRATION_______ml of 0.9% Sodium Chloride IV(20 ml/kg/dose)£ IV MAINTENANCE(for patient with normal serum Sodium and Potassium)Gray3 kg4 kg5 kg60 ml (3 kg)80 ml (4 kg)100 ml (5 kg)13 ml (3 kg)______ml/hr of D5/0.2% Sodium Chloride with 20 mEq KCl/1,000 ml 17 ml (4 kg)21 ml (5 kg)______ml/hr of D5/0.2% Sodium Chloride with 20 mEq KCI/1,000 ml______ml/hr of D5/0.3% Sodium Chloride with 30 mEq KCI/1,000 ml______ml/hr of D5/0.45% Sodium Chloride with 40 mEq KCI/1,000 mlPink6-7kg130 ml27 mlRed8-9kg160 ml35 mlPurple10-11kg200 ml42 mlYellow12-14kg240 ml47 mlWhite15-18kg300 ml52 mlBlue19-23kg400 ml63 mlOrange24-29kg500 ml69 mlGreen30-36kg650 ml88 mlTan37-45kg900 ml 1000 ml96+ mlTealAdultover 45kgMedications:Racemic Epinephrine (Racepinephrine) 2.25%-0.5 ml for inhalation£ Weight under 5 kg place 0.25 ml in Sodium Chloride 0.9% to a total volume of 2.5 ml via SVN, PRN Croup Score£ Weight 5-10 kg place 0.5 ml in Sodium Chloride 0.9% to a total volume of 2.5 ml via SVN, PRN Croup Score£ Dilute Racemic Epinephrine dose with 3% Sodium Chloride to total volume of 2.5 ml via SVN, PRN Croup Score(See back of page 2 PEDS Croup Score)£ Dexamethasone 0.6 mg/kg x 1 dose, IV Push (max 16 mg) administer_________________________mg£ Dexamethasone 0.6 mg/kg x 1 dose, IM administer ______________________mgPrednisone tablet£______mg (1 mg/kg per dose) orally every 12 hours (maximum 30 mg per dose)£______mg (2 mg/kg per dose) orally once daily (maximum 60 mg per dose)Prednisolone liquid£______mg (1mg/kg per dose) orally or by feeding tube every 12 hours (maximum 30 mg per dose)£______mg (2 mg/kg per dose) orally or by feeding tube once daily (maximum 60 mg per dose)Medications continued on page 21028173 11-23-11 Page 2 of 3
PEDS CROUP ADMISSION ORDERSInstructions: Orders must be individualized to patient needs. Orders preceded by a boxare only processed if checked. Orders preceded by a letter, number or bullet areprocessed automatically unless crossed out by the physician.Date: ________________________Time: _____________________Medications:17 years and youngerWeight______________kgPAIN AND FEVER MEDICATIONS£ Acetaminophen FEVER/PAIN_______mg rectally every 4-6 hrs PRN fever/pain(10-15 mg/kg/dose) Max dose=2600 mg/24 hrs£ Acetaminophen_______mg orally every 4-6 hrs PRN fever/pain(10-15 mg/kg/dose) Max dose=90 mg/kg/24 hrs£ Acetaminophen with Codeine *Age over 3 years PAIN_______mg Codeine orally every 4-6 hrs PRN pain(0.5-1 mg codeine/kg/dose) Max dose=360 mg/24 hrs£ Ibuprofen *Age 6 months FEVER/PAIN_______mg orally every 6-8 hrs PRN fever/pain(5-10 mg/kg/dose)Gray3 kg4 kg5 kg40 mg (3 kg)40 mg (4 kg)60 mg (5 kg)***Pink6-7kg80 mg*50 mgRed8-9kg120 mg 120 mg*80 mgPurple10-11kg*100 mgYellow12-14kg160 mg12 mg100 mgWhite15-18kg200 mg12 mg150 mgBlue19-23kg240 mg18 mg180 mgOrange24-29kg320 mg24 mg200 mgGreen30-36kg400 mg30 mg300 mgTan37-45kg480/500 mg36 mg300 mgTealAdultover 45kg325to650 mg15 to60 mg200 to600 mgLab:£ CBC £ Electrolytes £ Other________________________________________________________________________E V I D E N C E B A S E D G U I D E L I N EViral Antigen Testing are not indicated• CBC if high fever over 38.3 c or toxic child• Consider work up for serious bacterial illness in infants under 2 months presenting with fever over 38.2o c or whoappear ill or toxic• Electrolytes in patients with significant dehydrationRadiology:£ AP lateral neck x-ray£ Chest x-rayRefer to criteria for admission, PEDS Croup Score, and History of recurrent Croup on back of this pageK1028173 11-23-11 Page 3 of 3 FRONT
PEDIATRIC CROUP SCORE0 1 2 3Inspiratory Stridor None When Agitated On/Off at Rest ContinuousRetractions None Mild Moderate SevereAir Entry Normal Decreased Moderately Decreased Severely DecreasedCyanosis None When Crying At RestAlertness Alert Restless/Anxious DepressedLess than 2 very Mild 2-7 Mild-Moderate over 9 SevereCRITERIA FOR ADMISSION• Toxic appearance, poor feeding, lethargy, and dehydration• Moderate to severe respiratory distress• Apnea• Hypoxemia• The parent is unable to care for the child at home• History of airway abnormalitiesHistory of recurrent CroupConsider:• Asthma• Ig A deficiency• Anamalies of the airway such as:– Subglottic Stenosis– Laryngo Trachomeomalacia– Hemangioma or webDISCHARGE CRITERIA• Patient is not in any distress• Oxygen saturation over 92% on room air• Able to drink/eat per age• Last Racemic Epinephrine was over 6 hours• Reliable caregiverDISCHARGE INSTRUCTIONS• Diet: Normal for age• Activity: as tolerated• Follow-up with primary care physician in______days1028173 Page 3 BACK
PEDIATRIC ACUTE GASTROENTERITISADMISSION ORDERSInstructions: Orders must be individualized to patient needs. Orders preceded by a boxare only processed if checked. Orders preceded by a letter, number or bullet areprocessed automatically unless crossed out by the physician.KKDate: ________________________Time: _____________________Diagnosis: Gastroenteritis Condition £ Stable / GoodKKK£ FairThe content below was developed to facilitate computerized provider order entry (CPOE) and the application ofevidence-based medicine. This content is not a substitute for clinical judgment and individual patient treatment mayrequire adaptation as determined by the treating physician(s).Admit as Inpatient to: £ <strong>Pediatric</strong>s general floor £ Place in <strong>Pediatric</strong> Observation Unit£ Admitting Physician ___________________________ Pager # ___________________Phone # ___________________Allergies: £ NKA£ Other: _________________________________________________________________________Vital Signs: (Temperature, HR, RR, BP, SpO2) £ every 2 hours £ every 4 hours £ routine every 6 hoursDiet:£ Advance diet as tolerated starting with oral rehydration solution£ Resume breastfeeding as soon as possible£ NPO£ except medication£ except sips of clear liquids, for 4 hours post last emesis£ strictActivity:£ Progress as tolerated £ Bed restNursing Orders:Assessments• Measure height – once• Measure weight at admission and once a day£ Cardiac monitor• Measure head circumference (indicated for children less than 2 years) – onceMeasure intake and output strict£ every 8 hours£ every 4 hoursContingency• Notify provider for bilious emesis• Notify provider for uncontrolled painInterventions• Education, diet regarding the appropriate utilization of an oral electrolyte solution and initiation of an age appropriate dietfollowing rehydration1028165 11-15-11 Page 1 of 3
PEDIATRIC ACUTE GASTROENTERITISADMISSION ORDERSInstructions: Orders must be individualized to patient needs. Orders preceded by a boxare only processed if checked. Orders preceded by a letter, number or bullet areprocessed automatically unless crossed out by the physician.Date: ________________________Time: _____________________IV Fluids:17 years and youngerWeight______________kgIV FLUIDS£ IV FLUID BOLUS DEHYDRATION_______ml of 0.9% Sodium Chloride IV(20 ml/kg/dose)£ IV MAINTENANCE(for patient with normal serum Sodium and Potassium)Gray3 kg4 kg5 kg60 ml (3 kg)80 ml (4 kg)100 ml (5 kg)13 ml (3 kg)______ml/hr of D5/0.2% Sodium Chloride with 20 mEq KCl/1,000 ml 17 ml (4 kg)21 ml (5 kg)______ml/hr of D5/0.2% Sodium Chloride with 20 mEq KCI/1,000 ml______ml/hr of D5/0.3% Sodium Chloride with 30 mEq KCI/1,000 ml______ml/hr of D5/0.45% Sodium Chloride with 40 mEq KCI/1,000 mlPink6-7kg130 ml27 mlRed8-9kg160 ml35 mlPurple10-11kg200 ml42 mlYellow12-14kg240 ml47 mlWhite15-18kg300 ml52 mlBlue19-23kg400 ml63 mlOrange24-29kg500 ml69 mlGreen30-36kg650 ml88 mlTan37-45kg900 ml 1000 ml96+ mlTealAdultover 45kgMedications:17 years and youngerWeight______________kgPAIN AND FEVER MEDICATIONS£ Acetaminophen FEVER/PAIN_______mg rectally every 4-6 hrs PRN fever/pain(10-15 mg/kg/dose) Max dose=2600 mg/24 hrs£ Acetaminophen_______mg orally every 4-6 hrs PRN fever/pain(10-15 mg/kg/dose) Max dose=90 mg/kg/24 hrs£ Acetaminophen with Codeine *Age over 3 years PAIN_______mg Codeine orally every 4-6 hrs PRN pain(0.5-1 mg codeine/kg/dose) Max dose=360 mg/24 hrs£ Ibuprofen *Age 6 months FEVER/PAIN_______mg orally every 6-8 hrs PRN fever/pain(5-10 mg/kg/dose)Gray3 kg4 kg5 kg40 mg (3 kg)40 mg (4 kg)60 mg (5 kg)***Pink6-7kg80 mg*50 mgRed8-9kg120 mg 120 mg*80 mgPurple10-11kg*100 mgYellow12-14kg160 mg12 mg100 mgWhite15-18kg200 mg12 mg150 mgBlue19-23kg240 mg18 mg180 mgOrange24-29kg320 mg24 mg200 mgGreen30-36kg400 mg30 mg300 mgTan37-45kg480/500 mg36 mg300 mgTealAdultover 45kg325to650 mg15 to60 mg200 to600 mgOther: _______________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________1028165 11-15-11 Page 2 of 3
PEDIATRIC ACUTE GASTROENTERITISADMISSION ORDERSInstructions: Orders must be individualized to patient needs. Orders preceded by a boxare only processed if checked. Orders preceded by a letter, number or bullet areprocessed automatically unless crossed out by the physician.Date: ________________________Time: _____________________Labs:Panels:£ Basic Metabolic Panel (BUN, Creatinine, Sodium, Potassium, CO2, Chloride, Glucose)Microbiology£ Culture, blood £ Culture, rotavirus, stool, direct detection £ Culture, stool£ Culture, urine £ Culture, urine (via straight catheterization)Urinalysis£ Urinalysis (UA) with microscopy£ Stool Occult Blood£ Stool C. DifficileRadiology:£ Ultrasound, abdomen £ Abdomen, AP £ Chest, 2 views£ Upper gastrointestinal series £ Upper gastrointestinal series with small bowel follow-throughConsults:£ Gastroenterology, <strong>Pediatric</strong>:__________________________________________________________________________£ Surgery consult: ___________________________________________________________________________________£ Discharge planning or Case Management: ______________________________________________________________£ Placement _____________________________________________________________________________________£ Home Care ____________________________________________________________________________________£ Durable Medical Equipment _______________________________________________________________________£ Dietician, pediatric:_________________________________________________________________________________E V I D E N C E B A S E D G U I D E L I N EAdvance to a regular diet as tolerated 4 hours after the last episode of vomitingAvoid the routine use of antidiarrheal agentsConsider the use of an antiemetic in vomiting patientsEvidence for the use of glutamine supplementation is inconclusiveEvidence regarding the routine use of an antimicrobial agent in immunocompetent patients is not recommendedRefer to back of this page for Discharge Criteria and Discharge Instructions.K1028165 11-15-11 Page 3 of 3 FRONT
DISCHARGE CRITERIA• Child has no signs of distress or dehydration• Able to drink/eat per age• Reliable caregiverDISCHARGE INSTRUCTIONS• Diet: Normal for age• Activity: as tolerated• Medications:• Follow-up with primary care physician in 2-3 days1028165 Page 3 BACK
PEDIATRIC DEPARTMENT PRE-PROCEDUREASSESSMENT AND ORDERSTo be completed on pediatric patients receiving moderate or deep sedation provided bynon-anesthesia personnel outside the operating roomKDiagnosis: ________________________________________ Procedure:____________________________________Pertinent Medical History: ________________________________________________________________________Surgical History: ________________________________________________________________________Allergies:_____________________________________________________________________________________Past Medical History: £ Asthma £ Sleep Apnea £ Snoring £ Seizures £ Heart DiseaseMedications: £ Reviewed patient’s list of medications OR £ List medications patient is currently taking___________________________________________________________________________________________KPhysician Signature ______________________________________ Date __________________Time______________Physical: - General Appearance:HEENT: WNL Other ________________________________________________________________________________________Nasal Patency: Left £ Yes £ No Right £ Yes £ NoMouth: Tonsils_______ Bite_______ Palate_______Heart £ Within normal limits £ Other__________________________________________________________Lungs: £ Within normal limits £ Other__________________________________________________________Abdomen: £ Within normal limits £ Other__________________________________________________________Neuro: £ Within normal limits £ Other__________________________________________________________MALLAMPATTI SCALE (circle below)ASA CLASSIFICATION (check box below)£ Class 1 Patient without systemic illness£ Class 2 Patient with mild to mod systemic disease£ Class 3 patient with severe systemic illness£ Class 4 Patient with severe systemic disease/disorders£ Class 5 Moribund patient with little chance of survivalProcedure done in desperation1. (Easy) visualization of the soft palate, fauces, uvula,and both anterior and posterior pillars.2. Visualization of the soft palate, fauces, and uvula.3. Visualization of the soft palate and the base of the uvula.4. (Difficult) the soft palate is not visible at all.5. N/A patient is intubated£ Previous complications with anesthesia explain____________________________________________________________________________________________________________________________________________________Pregnancy test £ Neg £ Pos £ N/A per Genesys policy (Between 10 and 55 if menstruating regularly)Last time ate solid food_________________Plan: Urgent and Emergent situation in which gastric emptying is impaired, the potential for pulmonary aspiration of gastric contentsis considered in determining the target level of sedation.Patient is a candidate for Select one: £ Moderate (Conscious) Sedation £ Deep Sedation £ Intubation prior to sedationPlan for sedation: Medications/Route ___________________________________________________________________KPhysician Signature _______________________________________ Date _________________Time ______________£ Second assessment prior to induction completed and no change in plan indicatedKPhysician Signature _______________________________________________ Date _____________________Time _________________1028280 9-20-11 Page 1 of 2
Procedure Documentation:Procedure performed ___________________________________________________________________________Description of Procedure £ Post Procedure Description entered into electronic documentation£ Post Procedure Description to be documented/dictated by physician performing the procedureFindings_____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________ Specimens to lab £ _____________________________Recommendations ___________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________Physician Orders:TimeMed/Dose/Route<strong>Pediatric</strong> Dosing Guideline<strong>Pediatric</strong> Patient Weight____________KgMidazolam (Versed) 6 months to 12 years 0.05-0.1 mg/Kg; IV(Titrate to desired effect)Fentanyl Less than 6 years 0.3-1.5 mcg/Kg/Dose IV6 years or older 1-5 mcg/Kg/Dose IVMorphine Sulfate 0.08-0.1 mg/Kg/Dose IV, IM, SubcutKetamine 1.5-2 mg/Kg IV4 mg/Kg IMPropofol (Diprivan) 0.5-1 mg/Kg IVNaloxone (Narcan) 5 years or younger 0.1 mg/Kg IV, IM, Subcutor weight less now orequal to 20 KgOlder than 5 years or 2 mg IV, IM, subcutweight greater than20 KgComplete calculation for _____________________________________, drug name____________ mcg/mg/kgx___________Kg = _______________.dose circle oneweight total doseKPhysician Signature _______________________________________________ Date _____________________Time _________________Note after recovery from DEEP SEDATIONProblems, treatments or complications during recovery ___________________________________________________£ Anesthetic Complications ______________________________________________________________________£ No apparent anesthetic complicationsKPhysician Signature _______________________________________ Date _________________Time ______________1028280 9-20-11 Page 2 of 2