Subacromial Decompression Protocol - South Shore Hospital
Subacromial Decompression Protocol - South Shore Hospital
Subacromial Decompression Protocol - South Shore Hospital
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
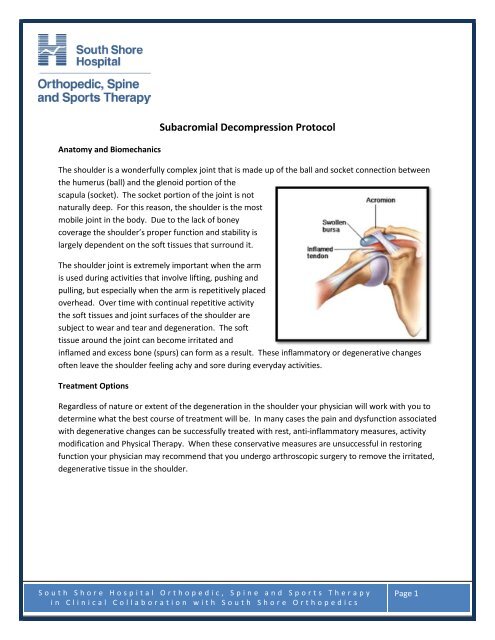
Anatomy and Biomechanics<strong>Subacromial</strong> <strong>Decompression</strong> <strong>Protocol</strong>The shoulder is a wonderfully complex joint that is made up of the ball and socket connection betweenthe humerus (ball) and the glenoid portion of thescapula (socket). The socket portion of the joint is notnaturally deep. For this reason, the shoulder is the mostmobile joint in the body. Due to the lack of boneycoverage the shoulder’s proper function and stability islargely dependent on the soft tissues that surround it.The shoulder joint is extremely important when the armis used during activities that involve lifting, pushing andpulling, but especially when the arm is repetitively placedoverhead. Over time with continual repetitive activitythe soft tissues and joint surfaces of the shoulder aresubject to wear and tear and degeneration. The softtissue around the joint can become irritated andinflamed and excess bone (spurs) can form as a result. These inflammatory or degenerative changesoften leave the shoulder feeling achy and sore during everyday activities.Treatment OptionsRegardless of nature or extent of the degeneration in the shoulder your physician will work with you todetermine what the best course of treatment will be. In many cases the pain and dysfunction associatedwith degenerative changes can be successfully treated with rest, anti-inflammatory measures, activitymodification and Physical Therapy. When these conservative measures are unsuccessful in restoringfunction your physician may recommend that you undergo arthroscopic surgery to remove the irritated,degenerative tissue in the shoulder.<strong>South</strong> <strong>Shore</strong> <strong>Hospital</strong> Orthopedic, Spine and Sports Therapyin Clinical Collaboration with <strong>South</strong> <strong>Shore</strong> OrthopedicsPage 1
SurgeryThe subacromial decompression procedure involves removing tissuefrom the front part of the shoulder. This part of the shoulder isreferred to as the subacromial space, as it is located below theoutcropping of bone on the scapula (shoulder blade) know as theacromian process. During the procedure the end of the acromianprocess and any inflamed tissue including the subacromial bursa isdebrided. This creates more room in the front of the shoulder sothat the tendons of the rotator cuff can move freely without gettingirritated or pinched. The procedure is performed arthroscopicallyand is, in most cases an outpatient day surgery. This means that itis very rare to have to spend the night in the hospital.Recovery/Time off WorkBefore undergoing subacromial decompression surgery your doctor will discuss the recovery processwith you. It is very important that the patient knows that the recovery process is fairly difficult and timeconsuming. He or she must be an active participant during this process, performing daily exercises toensure there is proper return of the shoulder’s range of motion and strength. There is a large amount ofvariability in the time it takes to fully recover from this procedure and is typically dependant on theextent of the damage that needs to be fixed. It is usually estimated that it will take at least 3-4 monthsto feel as though you have completely regained the use of your arm. Some cases may take as long as 6-9 months to make a full recovery. People with desk jobs should plan to take at least 1 week off fromwork. Those with jobs that require physical activity and lifting will likely be out of work for at least 3months. Recovery is different in each case. Your individual time table for return to activities and workwill be discussed by your surgeon during post operative office visits.Post Operative VisitsYour first post-op visit to the doctor’s office will be approximately 7-10 days after the operation. At thisvisit any stitches you have will be removed and you will review the surgery with the doctor or hisassistant. At this time you will most likely be cleared to make an appointment to begin Physical Therapy.You should also plan to check in with your surgeon at 6 and 12 weeks after the operation. The surgeonmay create a different timetable for postoperative office visits if your case warrants it.At HomeYou may remove your post-op dressing 2 days after the operation and replace it as needed. Do notremove the tape (steri-strips) that is across your incisions. Allow them to fall off on their own. You mayshower after 2 days, but use a water-tight dressing until your sutures are removed. Bathing withoutgetting the shoulder wet or sponge baths are a good alternative. You may wash under the affected armby leaning forward and letting the arm dangle. You may move your arm in front of your body, but not<strong>South</strong> <strong>Shore</strong> <strong>Hospital</strong> Orthopedic, Spine and Sports Therapyin Clinical Collaboration with <strong>South</strong> <strong>Shore</strong> OrthopedicsPage 2
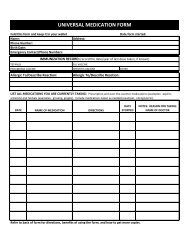
out to the side until your doctor allows you. You may remove your sling several times a day and gentlymove your hand, wrist and elbow and perform shoulder pendulum exercises.MedicationYour surgeon will prescribe pain medicine for you after the operation. Please call the doctor’s office ifyou have any questions regarding medication.IceYou must use ice on your shoulder after the operation for management of pain and swelling. Ice shouldbe applied 3-5 times a day for 10-20 minutes at a time until the postoperative inflammation hasresolved. Always maintain one layer between ice and the skin. Putting a pillow case over your ice packworks well for this.SlingYou will be provided with a sling to wear after the operation. Remove it when bathing/showering, or todo your exercises. You should remove the sling several times a day to perform pendulum exercises asinstructed. Wear the sling most of the time (especially when out in public) until you see your doctor foryour first post op visit. Most patients use their sling for about 2 weeks. If your case is atypical yourdoctor may have custom guidelines for you regarding use of the sling.SleepingYou may sleep with a pillow propped under your arm to keep it slightly away from the body if you needto. For many patients lying flat is uncomfortable at first. It is generally easier to sleep propped up for ashort period of time after the operation. Do not attempt to sleep on your operated shoulder for at least6 weeks.<strong>South</strong> <strong>Shore</strong> <strong>Hospital</strong> Orthopedic, Spine and Sports Therapyin Clinical Collaboration with <strong>South</strong> <strong>Shore</strong> OrthopedicsPage 3
Rehabilitation**The following is an outlined progression for rehab. Time tables are approximate. Advancementfrom phase to phase, as well as specific exercises performed, should be based on each individualpatient’s case and sound clinical judgment on the part of the rehab professional. **Phase 1 (0-2 Weeks) ROM PhaseGoalsControl Pain and SwellingProtect Healing TissueBegin to Restore Range of MotionPrecautionsDo not actively use your arm for reaching, especially overhead.Do not lift anything with your arm.Recommended ExercisesPendulumsStanding Scapular Mobility (no resistance)Supine or Standing Passive External RotationSupine, Seated or Standing Passive Shoulder Flexion (elevation)Passive Internal RotationPassive Horizontal AdductionGuidelinesPerform these exercises 3-5 times a day. Do 1-2 sets of 10-20 repetitions of each exercise.Phase 2 (2-6 Weeks) Active ROM PhaseGoalsContinued protection of healing tissueContinue to improve ROMInitiate gentle peri-scapular and rotator cuff strengtheningBegin using your arm for daily activities in front of bodyPrecautionsDiscontinue use of sling if you have not alreadyBe careful with raising your arm, especially overhead, and away from your bodyContinue to avoid lifting or carrying anything<strong>South</strong> <strong>Shore</strong> <strong>Hospital</strong> Orthopedic, Spine and Sports Therapyin Clinical Collaboration with <strong>South</strong> <strong>Shore</strong> OrthopedicsPage 4
Recommended ExercisesROMContinue passive ROM with physical therapistPendulumsSupine Stick FlexionTable Slides with progression to Wall SlidesSupine or Standing Passive External Rotation with gentle progression of abduction anglePassive Internal RotationGentle supine or standing cross body stretchAROM Against GravityProne RowProne ExtensionProne Horizontal AbductionSidelying External RotationGuidelinesPerform all exercises once a day. Do 2-3 sets of 15-20 repetitions.Phase 3 (6-12 Weeks) Strengthening PhaseGoalsContinue to acquire normal ROM (both passive and active)Progressive strengthening of rotator cuff and shoulder blade muscle groupsBegin limited use arm for daily activities in all planesPrecautionsNo lifting away from your body or overhead greater than 1 or 2 poundsCaution with repetitive use of arm especially overheadStop activity if it causes pain in shoulderRecommended ExercisesRange of MotionContinue passive ROM with physical therapist as neededContinue ROM exercises from phase 2 until ROM is normalizedStrengthening (Resistance Band or Dumbell)RowProne ExtensionProne Horizontal AbductionStanding/Prone ScaptionInternal RotationExternal RotationDynamic StrengtheningManual Resistance Rythmic StabilizationProprioceptive Drills (90⁰ of Elevation or Below)<strong>South</strong> <strong>Shore</strong> <strong>Hospital</strong> Orthopedic, Spine and Sports Therapyin Clinical Collaboration with <strong>South</strong> <strong>Shore</strong> OrthopedicsPage 5
GuidelinesPerform ROM and stretching exercises once a day until normal ROM is achieved. Do 2 sets of 15-20Reps. Once normal ROM is achieved continue exercises to maintain ROM 3-5 times a week.Perform strengthening exercises 3-5 times a week. Do 2-3 sets of 15-20 Reps. Strict attention must bepaid to scapulohumeral rhythm with completion of all strengthening exercises.Phase 4 (12 Weeks +) Sport Specific and Return to Activity PhaseGoalsAchieve normal ROM and strengthContinue to encourage progressive use of arm for functional daily activityPrecautionsEncourage return to full use of arm for daily activitiesPay particular attention to scapulohumeral rhythm especially with abduction and overhead activityDiscuss return to sport and activity plan with physicianRecommended ExercisesROM and StretchingContinue ROM and stretching exercises from phase 2-3 as neededStrengtheningContinue strengthening exercises from phase 3IR/ER strengthening at 90 deg of abductionMay begin supervised weight training pending surgeons clearanceDynamic StrengtheningProgress manual resistance patternsProgress proprioceptive drills to include rhythmic stabilizationSlowly progress to overhead proprioceptive and plyometric drillsPush up progressionGuidelinesPerform ROM and stretching program 1-3 times a week to maintain normal ROM. Do 1-2 sets of 15-20Reps. Perform ROM and stretching more frequently in any planes of motion that are still deficientPerform strengthening 3 times a week. Do 2-3 sets of 15-20 Reps.<strong>South</strong> <strong>Shore</strong> <strong>Hospital</strong> Orthopedic, Spine and Sports Therapyin Clinical Collaboration with <strong>South</strong> <strong>Shore</strong> OrthopedicsPage 6
Time Focus Range of MotionPhase 10-2 WeeksPhase 22-6 WeeksPhase 36-12Weeks*Tissue Healing*Decrease PainandInflammation*Start EarlyPassive ROMwith Attention toRestrictions*Continue toDecrease PainandInflammation*Improve Passiveand Active ROM*ProgressiveStrengthening*ContinuedAttention toROM if StillDeficient*Establish ProperScapulohumeralRhythm*EnhanceProprioception*PROM with PT astolerated in allplanes*Avoid AROM inCoronal Plane*Continue PassiveROM as tolerated.*Slowly EncouragePain Free ActiveROM*Passive andActive ROM astolerated in allplanesRecommendedExercisesPassive/Active ROMPendulumsScapular MobilityPassive External RotationPassive FlexionPassive Internal RotationPassive Horizontal AdductionPassive ROMContinue PROM ExercisesActive Assisted ROMSupine to Standing FlexionCross-body AdductionProgress Abd angle with ERActive ROM Against GravitySidelying ERProne RowProne ExtensionProne Horizontal AbductionPassive ROMContinue as NeededActive Assisted/Active ROMand StretchingContinue Phase 2 ExercisesStrengthening (Dumbbell/Tband)RowProne ExtensionProne Horizontal AbductionStanding/Prone ScaptionInternal RotationExternal Rotation“W” (Row/ER)Bicep CurlDynamic ProgressionsRhythmic StabilizationProprioceptive DrillsPrecautions*Sling 0-2Weeks or perMD Instruction*Limit ActiveROM*Limit Use ofArm, EspeciallyOverhead andin Abduction*No ResistedActivity/Lifting*AvoidRepetitiveMotionEspeciallyOverhead*Must havegood ScapularControl withActive ROMAgainst Gravity*No Heavy orRepetitiveOverheadLifting/Reaching*DynamicProgressions ifPain Free/FullROM with allROM andStrengtheningExercises<strong>South</strong> <strong>Shore</strong> <strong>Hospital</strong> Orthopedic, Spine and Sports Therapyin Clinical Collaboration with <strong>South</strong> <strong>Shore</strong> OrthopedicsPage 7
Phase 412 Weeks +*Progressstrengthening*Regain use ofarm for all dailyactivities.*Prepare forReturn to Sportand PhysicalActivity*ContinueStretchingProgram asneeded.ROM/StretchContinue Phase 3 As NeededStrengtheningContinue T-band andDumbbell Progressions fromPhase 3Progress to Diagonal PatternsIR/ER at 90⁰ AbdMay Begin Limited WeightTrainingDynamic ProgressionsPushup ProgressionContinue Proprioceptive DrillsPlyometrics/RebounderProgress to OverheadRhythmic StabilizationManual Resistance Patterns* Return toGym Lifting perMD Approval*AvoidActivities thatCause ShoulderPain*BeginProgressiveReturn toSports andPhysical ActivityProgram AfterMD Evaluation*Reviewed by Michael Geary, MD<strong>South</strong> <strong>Shore</strong> <strong>Hospital</strong> Orthopedic, Spine and Sports Therapyin Clinical Collaboration with <strong>South</strong> <strong>Shore</strong> OrthopedicsPage 8