Sphincter of Oddi Physiology
Sphincter of Oddi Physiology
Sphincter of Oddi Physiology
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
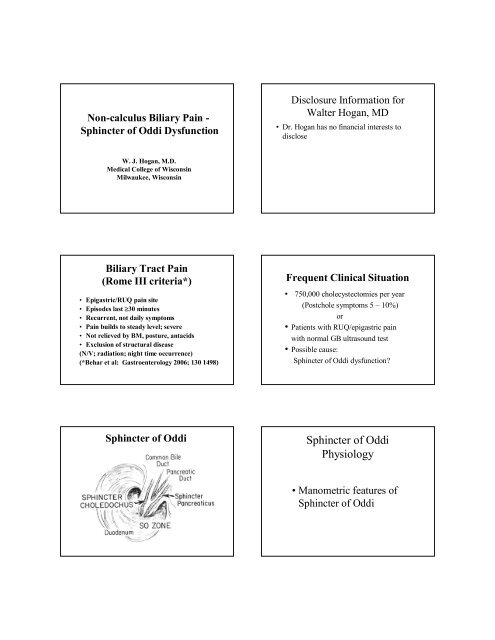
Non-calculus Biliary Pain -<strong>Sphincter</strong> <strong>of</strong> <strong>Oddi</strong> DysfunctionDisclosure Information forWalter Hogan, MD• Dr. Hogan has no financial interests todiscloseW. J. Hogan, M.D.Medical College <strong>of</strong> WisconsinMilwaukee, WisconsinBiliary Tract Pain(Rome III criteria*)• Epigastric/RUQ pain site• Episodes last 30 minutes• Recurrent, not daily symptoms• Pain builds to steady level; severe• Not relieved by BM, posture, antacids• Exclusion <strong>of</strong> structural disease(N/V; radiation; night time occurrence)(*Behar et al: Gastroenterology 2006; 130 1498)Frequent Clinical Situation• 750,000 cholecystectomies per year(Postchole symptoms 5 – 10%)or• Patients with RUQ/epigastric painwith normal GB ultrasound test• Possible cause:<strong>Sphincter</strong> <strong>of</strong> <strong>Oddi</strong> dysfunction?<strong>Sphincter</strong> <strong>of</strong> <strong>Oddi</strong><strong>Sphincter</strong> <strong>of</strong> <strong>Oddi</strong><strong>Physiology</strong>• Manometric features <strong>of</strong><strong>Sphincter</strong> <strong>of</strong> <strong>Oddi</strong>
<strong>Sphincter</strong> <strong>of</strong> <strong>Oddi</strong> Pressure Pr<strong>of</strong>ileSO Pressure Pr<strong>of</strong>ile TraceSO Phasic Waves
CCK Effect on SO Motor Activity<strong>Sphincter</strong> <strong>of</strong> <strong>Oddi</strong> Pressures*(Manometric Recording)Feature Normal Abnormal[median range]Basal pressure (mmHg) 15 3-35 >40ContractionsAmplitude (mmHg) 135 95-195 >300Frequency (n/min) 4 2-6 >7SequencesAntegrade % 80 12-100Simultaneous % 13 0-50Retrograde % 9 0-50CCK cholecystokinin inhibits contracts[Toouli: Gastro 1985;88:1243}<strong>Sphincter</strong> <strong>of</strong> <strong>Oddi</strong>Pathophysiology•Manometric features <strong>of</strong><strong>Sphincter</strong> <strong>of</strong> <strong>Oddi</strong>Paradoxical SO Response to CCK
Paradoxical Motor Response to CCK inPatients With Suspected SO Dysfunction(SO manometric recording)*SO Rapid Phasic Wave ActivityBasal SOPressure(mmHg)200180160140[ ]5 <strong>of</strong> 38 pts suspected SOD21 controls pts120100 CCK80 20 ng/kg IV60402000 30 60 90 120 150[Time in seconds]* [Hogan, et al. Gastroenterology 1980; 78:317-324]Elevated SO Basal PressureBiliary <strong>Sphincter</strong>mmHgSO Dysfunction• Structural alteration –(SO Stenosis)• Functional Abnormalities –(So Dysfunction)• Criteria: Abnormal Basal SOP± Response to smooth muscle relaxant<strong>Sphincter</strong> <strong>of</strong> <strong>Oddi</strong> Dysfunction (SOD)Modified Milwaukee ClassificationBiliaryTypeBiliaryPainLFTAbn.DilatedCBD >10 mmEtiologySten vs DyskType 1 + + + +Type II + 1 or 2 <strong>of</strong> above + +Type III + None <strong>of</strong> above +[Hogan, Geenen. Endoscopy 1998;1:179]
SO Dysfunction: Type II<strong>Sphincter</strong>otomy vs ShamProceduresSO DysfunctionBiliary Classification (85 pts.)Response to <strong>Sphincter</strong>otomy(2 year follow-up)*Bili type Abn SOP Post Endo SphPercentI 14 12 85%II 32 23 72%III 39 13 33%*[Rosenblatt ML, et al. Gastro Endosc 2001;54:697]SOD: Methods <strong>of</strong> Diagnosis• Quantitative hepatobiliary scan(QHBS)Morphine augmentation?• Fatty-meal ultrasound study• CCK stimulated MRCP• Imaging combinationsSO Dysfunction (85 pts)*Comparison: Results SO manometryversus non-invasive studies (HBS/FMS)Abnormal ResultsBil.Types SO Mano HBS/FMS % Correl.I 14 12 86%II 32 20 63%III 39 16 41%(HBS - Scintigraphy; FMS - fatty meal US)*[Rosenblatt ML, et al. Gastro Endosc 2001;54:697]ERCP (SO) Manometry- Clinical useConcerns:• Availability –few centers currently• Operator expertise/experience• Variable recording techniques• Scoring criteria not standardized• Post SOM pancreatitis:Reports vary:1 in 10/20 studies or not?Summary• Review <strong>of</strong> SO physiology and pathophysiology• Patients with suspected SO dysfunction– Pain history important– Eliminate structural causes• Type I: SOM unnecessary• Type II: SOM recommended• Type III: SOM recommend with patient caveat