Dressings and Topical Agents for Chronic Wounds - NIHR Health ...
Dressings and Topical Agents for Chronic Wounds - NIHR Health ...
Dressings and Topical Agents for Chronic Wounds - NIHR Health ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
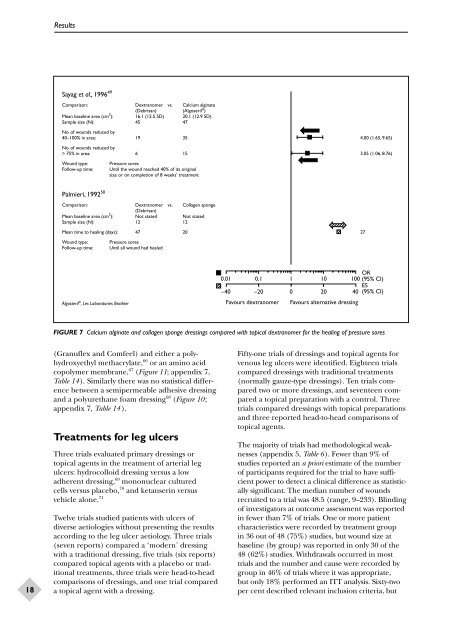
ResultsSayag et al., 1996 49Comparison: Dextranomer vs. Calcium alginate(Debrisan) (Algoseril ® )Mean baseline area (cm 2 ): 16.1 (12.5 SD) 20.1 (12.9 SD)Sample size (N): 45 47No. of wounds reduced by40–100% in area: 19 35 4.00 (1.65, 9.65)No. of wounds reduced by> 75% in area: 6 15 3.05 (1.06, 8.76)Wound type:Follow-up time:Pressure soresUntil the wound reached 40% of its originalsize or on completion of 8 weeks’ treatmentPalmieri, 1992 50Comparison: Dextranomer vs. Collagen sponge(Debrisan)Mean baseline area (cm 2 ): Not stated Not statedSample size (N): 12 12Mean time to healing (days): 47 20 27Wound type: Pressure soresFollow-up time: Until all wound had healedAlgosteril ® , Les Laboratories Brothier0.01 0.1 1 10 100 OR(95% CI)ES–40 –20 0 20 40 (95% CI)Favours dextranomer Favours alternative dressingFIGURE 7 Calcium alginate <strong>and</strong> collagen sponge dressings compared with topical dextranomer <strong>for</strong> the healing of pressure sores18(Granuflex <strong>and</strong> Comfeel) <strong>and</strong> either a polyhydroxyethylmethacrylate, 66 or an amino acidcopolymer membrane, 67 (Figure 11; appendix 7,Table 14). Similarly there was no statistical differencebetween a semipermeable adhesive dressing<strong>and</strong> a polyurethane foam dressing 68 (Figure 10;appendix 7, Table 14 ).Treatments <strong>for</strong> leg ulcersThree trials evaluated primary dressings ortopical agents in the treatment of arterial legulcers: hydrocolloid dressing versus a lowadherent dressing, 69 mononuclear culturedcells versus placebo, 70 <strong>and</strong> ketanserin versusvehicle alone. 71Twelve trials studied patients with ulcers ofdiverse aetiologies without presenting the resultsaccording to the leg ulcer aetiology. Three trials(seven reports) compared a ‘modern’ dressingwith a traditional dressing, five trials (six reports)compared topical agents with a placebo or traditionaltreatments, three trials were head-to-headcomparisons of dressings, <strong>and</strong> one trial compareda topical agent with a dressing.Fifty-one trials of dressings <strong>and</strong> topical agents <strong>for</strong>venous leg ulcers were identified. Eighteen trialscompared dressings with traditional treatments(normally gauze-type dressings). Ten trials comparedtwo or more dressings, <strong>and</strong> seventeen compareda topical preparation with a control. Threetrials compared dressings with topical preparations<strong>and</strong> three reported head-to-head comparisons oftopical agents.The majority of trials had methodological weaknesses(appendix 5, Table 6). Fewer than 9% ofstudies reported an a priori estimate of the numberof participants required <strong>for</strong> the trial to have sufficientpower to detect a clinical difference as statisticallysignificant. The median number of woundsrecruited to a trial was 48.5 (range, 9–233). Blindingof investigators at outcome assessment was reportedin fewer than 7% of trials. One or more patientcharacteristics were recorded by treatment groupin 36 out of 48 (75%) studies, but wound size atbaseline (by group) was reported in only 30 of the48 (62%) studies. Withdrawals occurred in mosttrials <strong>and</strong> the number <strong>and</strong> cause were recorded bygroup in 46% of trials where it was appropriate,but only 18% per<strong>for</strong>med an ITT analysis. Sixty-twoper cent described relevant inclusion criteria, but