- Page 2:
Descriptive Psychopathology
- Page 8:
CAMBRIDGE UNIVERSITY PRESSCambridge
- Page 14:
ContentsPrefaceAcknowledgmentspage
- Page 18:
Preface“Of all Persons who are Ob
- Page 22:
xiPreface“lumpers” and “split
- Page 26:
AcknowledgmentsMax Fink read many o
- Page 34:
1Beyond the DSM and ICD:a rationale
- Page 38:
5 Chapter 1: Beyond the DSM and ICD
- Page 42:
7 Chapter 1: Beyond the DSM and ICD
- Page 46:
9 Chapter 1: Beyond the DSM and ICD
- Page 50:
11 Chapter 1: Beyond the DSM and IC
- Page 56:
14 Section 1: Present, past, and fu
- Page 60:
16 Section 1: Present, past, and fu
- Page 64:
18 Section 1: Present, past, and fu
- Page 68:
20 Section 1: Present, past, and fu
- Page 72:
2A history of psychiatric classific
- Page 76:
24 Section 1: Present, past, and fu
- Page 80:
26 Section 1: Present, past, and fu
- Page 84:
28 Section 1: Present, past, and fu
- Page 88:
30 Section 1: Present, past, and fu
- Page 92:
32 Section 1: Present, past, and fu
- Page 96:
34 Section 1: Present, past, and fu
- Page 100:
36 Section 1: Present, past, and fu
- Page 104:
38 Section 1: Present, past, and fu
- Page 108:
40 Section 1: Present, past, and fu
- Page 112:
42 Section 1: Present, past, and fu
- Page 116:
44 Section 1: Present, past, and fu
- Page 120:
46 Section 1: Present, past, and fu
- Page 124:
48 Section 1: Present, past, and fu
- Page 128:
50 Section 1: Present, past, and fu
- Page 132:
52 Section 1: Present, past, and fu
- Page 136:
54 Section 1: Present, past, and fu
- Page 140:
56 Section 1: Present, past, and fu
- Page 144:
58 Section 1: Present, past, and fu
- Page 148:
60 Section 1: Present, past, and fu
- Page 152:
62 Section 1: Present, past, and fu
- Page 156:
64 Section 1: Present, past, and fu
- Page 160:
66 Section 1: Present, past, and fu
- Page 164:
68 Section 1: Present, past, and fu
- Page 168:
70 Section 1: Present, past, and fu
- Page 172:
72 Section 1: Present, past, and fu
- Page 176:
74 Section 1: Present, past, and fu
- Page 180:
76 Section 1: Present, past, and fu
- Page 184:
78 Section 1: Present, past, and fu
- Page 188:
80 Section 1: Present, past, and fu
- Page 192:
82 Section 1: Present, past, and fu
- Page 196:
84 Section 1: Present, past, and fu
- Page 200:
86 Section 1: Present, past, and fu
- Page 206:
Section 2The neuropsychiatric evalu
- Page 212:
92 Section 2: The neuropsychiatric
- Page 216:
94 Section 2: The neuropsychiatric
- Page 220:
96 Section 2: The neuropsychiatric
- Page 224:
98 Section 2: The neuropsychiatric
- Page 228:
100 Section 2: The neuropsychiatric
- Page 232:
102 Section 2: The neuropsychiatric
- Page 236:
104 Section 2: The neuropsychiatric
- Page 240:
106 Section 2: The neuropsychiatric
- Page 244:
108 Section 2: The neuropsychiatric
- Page 248:
110 Section 2: The neuropsychiatric
- Page 252:
112 Section 2: The neuropsychiatric
- Page 256:
114 Section 2: The neuropsychiatric
- Page 260:
116 Section 2: The neuropsychiatric
- Page 264:
118 Section 2: The neuropsychiatric
- Page 268:
120 Section 2: The neuropsychiatric
- Page 272:
Appendix 5.1Questions for past illn
- Page 276:
124 Section 2: The neuropsychiatric
- Page 280:
126 Section 2: The neuropsychiatric
- Page 284:
128 Section 2: The neuropsychiatric
- Page 290:
Section 3Examination domains
- Page 296:
134 Section 3: Examination domainsi
- Page 300:
136 Section 3: Examination domainsl
- Page 304:
138 Section 3: Examination domainst
- Page 308:
140 Section 3: Examination domainsD
- Page 312:
142 Section 3: Examination domainsT
- Page 316:
144 Section 3: Examination domainsd
- Page 320:
146 Section 3: Examination domainsS
- Page 324:
148 Section 3: Examination domainsT
- Page 328:
150 Section 3: Examination domainsl
- Page 332:
152 Section 3: Examination domains4
- Page 336:
154 Section 3: Examination domainsT
- Page 340:
156 Section 3: Examination domainsi
- Page 344:
158 Section 3: Examination domainsi
- Page 348: 160 Section 3: Examination domainst
- Page 352: 162 Section 3: Examination domainsI
- Page 356: 164 Section 3: Examination domainsT
- Page 360: 166 Section 3: Examination domainsv
- Page 364: 168 Section 3: Examination domainsw
- Page 368: 170 Section 3: Examination domainsT
- Page 372: 172 Section 3: Examination domainsN
- Page 376: 174 Section 3: Examination domainsl
- Page 380: 176 Section 3: Examination domainsS
- Page 384: 178 Section 3: Examination domainsI
- Page 388: 180 Section 3: Examination domainsM
- Page 392: 182 Section 3: Examination domainsp
- Page 396: 184 Section 3: Examination domainsS
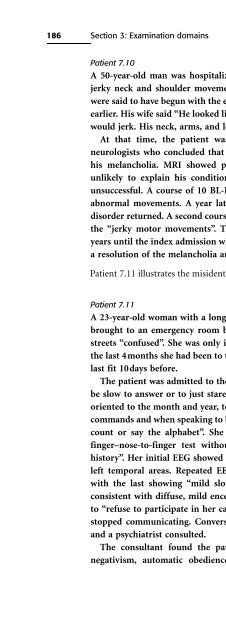
- Page 402: 187 Chapter 7: Disturbances of moto
- Page 406: 189 Chapter 7: Disturbances of moto
- Page 410: 191 Chapter 7: Disturbances of moto
- Page 414: 193 Chapter 7: Disturbances of moto
- Page 418: 195 Chapter 7: Disturbances of moto
- Page 422: 8Disturbances in emotional experien
- Page 426: 199 Chapter 8: Disturbances in emot
- Page 430: 201 Chapter 8: Disturbances in emot
- Page 434: 203 Chapter 8: Disturbances in emot
- Page 438: 205 Chapter 8: Disturbances in emot
- Page 442: 207 Chapter 8: Disturbances in emot
- Page 446: 209 Chapter 8: Disturbances in emot
- Page 450:
211 Chapter 8: Disturbances in emot
- Page 454:
213 Chapter 8: Disturbances in emot
- Page 458:
215 Chapter 8: Disturbances in emot
- Page 462:
217 Chapter 8: Disturbances in emot
- Page 466:
219 Chapter 8: Disturbances in emot
- Page 470:
221 Chapter 8: Disturbances in emot
- Page 474:
223 Chapter 8: Disturbances in emot
- Page 478:
225 Chapter 9: Disturbances in spee
- Page 482:
Table 9.2. Speech patterns of some
- Page 486:
229 Chapter 9: Disturbances in spee
- Page 490:
231 Chapter 9: Disturbances in spee
- Page 494:
233 Chapter 9: Disturbances in spee
- Page 498:
235 Chapter 9: Disturbances in spee
- Page 502:
237 Chapter 9: Disturbances in spee
- Page 506:
239 Chapter 9: Disturbances in spee
- Page 510:
241 Chapter 9: Disturbances in spee
- Page 514:
243 Chapter 9: Disturbances in spee
- Page 518:
245 Chapter 9: Disturbances in spee
- Page 522:
247 Chapter 9: Disturbances in spee
- Page 526:
Circumstantial ○ ○ ○ Disinhi
- Page 530:
251 Chapter 9: Disturbances in spee
- Page 534:
10Perceptual disturbancesFor decade
- Page 538:
255 Chapter 10: Perceptual disturba
- Page 542:
257 Chapter 10: Perceptual disturba
- Page 546:
259 Chapter 10: Perceptual disturba
- Page 550:
261 Chapter 10: Perceptual disturba
- Page 554:
263 Chapter 10: Perceptual disturba
- Page 558:
265 Chapter 10: Perceptual disturba
- Page 562:
267 Chapter 10: Perceptual disturba
- Page 566:
269 Chapter 10: Perceptual disturba
- Page 570:
271 Chapter 10: Perceptual disturba
- Page 574:
273 Chapter 11: Delusions and abnor
- Page 578:
275 Chapter 11: Delusions and abnor
- Page 582:
277 Chapter 11: Delusions and abnor
- Page 586:
279 Chapter 11: Delusions and abnor
- Page 590:
281 Chapter 11: Delusions and abnor
- Page 594:
283 Chapter 11: Delusions and abnor
- Page 598:
285 Chapter 11: Delusions and abnor
- Page 602:
287 Chapter 11: Delusions and abnor
- Page 606:
289 Chapter 11: Delusions and abnor
- Page 610:
291 Chapter 11: Delusions and abnor
- Page 614:
12Obsessive-compulsive behaviorsIt
- Page 618:
295 Chapter 12: Obsessive-compulsiv
- Page 622:
297 Chapter 12: Obsessive-compulsiv
- Page 626:
299 Chapter 12: Obsessive-compulsiv
- Page 630:
301 Chapter 12: Obsessive-compulsiv
- Page 634:
303 Chapter 12: Obsessive-compulsiv
- Page 638:
305 Chapter 12: Obsessive-compulsiv
- Page 642:
307 Chapter 12: Obsessive-compulsiv
- Page 646:
309 Chapter 12: Obsessive-compulsiv
- Page 650:
311 Chapter 13: Testing and psychop
- Page 654:
313 Chapter 13: Testing and psychop
- Page 658:
315 Chapter 13: Testing and psychop
- Page 662:
317 Chapter 13: Testing and psychop
- Page 666:
319 Chapter 13: Testing and psychop
- Page 670:
321 Chapter 13: Testing and psychop
- Page 674:
323 Chapter 13: Testing and psychop
- Page 678:
325 Chapter 13: Testing and psychop
- Page 682:
327 Chapter 13: Testing and psychop
- Page 686:
329 Chapter 13: Testing and psychop
- Page 690:
331 Chapter 13: Testing and psychop
- Page 694:
333 Chapter 14: PersonalitySheldon
- Page 698:
335 Chapter 14: PersonalityEarly em
- Page 702:
337 Chapter 14: Personalitya new si
- Page 706:
339 Chapter 14: Personalitywhat oth
- Page 710:
341 Chapter 14: PersonalityDeviance
- Page 714:
343 Chapter 14: PersonalityIntersex
- Page 718:
345 Chapter 14: Personalityill, als
- Page 722:
347 Chapter 14: PersonalityCombat,
- Page 726:
349 Chapter 14: PersonalityAxis II
- Page 730:
15Abnormal trait behaviors: persona
- Page 734:
353 Chapter 15: Abnormal trait beha
- Page 738:
355 Chapter 15: Abnormal trait beha
- Page 742:
357 Chapter 15: Abnormal trait beha
- Page 746:
359 Chapter 15: Abnormal trait beha
- Page 750:
361 Chapter 15: Abnormal trait beha
- Page 754:
363 Chapter 15: Abnormal trait beha
- Page 758:
365 Chapter 15: Abnormal trait beha
- Page 762:
367 Chapter 15: Abnormal trait beha
- Page 770:
16An evidence-based classification
- Page 774:
373 Chapter 16: An evidence-based c
- Page 778:
375 Chapter 16: An evidence-based c
- Page 782:
377 Chapter 16: An evidence-based c
- Page 786:
379 Chapter 16: An evidence-based c
- Page 790:
381 Chapter 16: An evidence-based c
- Page 794:
383 Chapter 16: An evidence-based c
- Page 798:
385 Chapter 16: An evidence-based c
- Page 802:
387 Chapter 16: An evidence-based c
- Page 806:
389 Chapter 16: An evidence-based c
- Page 810:
391 Chapter 16: An evidence-based c
- Page 814:
393 Chapter 16: An evidence-based c
- Page 818:
395 Chapter 16: An evidence-based c
- Page 822:
397 Chapter 16: An evidence-based c
- Page 826:
399 Chapter 16: An evidence-based c
- Page 830:
401 ReferencesAcierno, R., Lawyer,
- Page 834:
403 ReferencesAmerican Psychiatric
- Page 838:
405 ReferencesBaldessarini, R.J. (1
- Page 842:
407 ReferencesKoukopolous, A. and A
- Page 846:
409 ReferencesBlumberg, H.P., Stern
- Page 850:
411 ReferencesBryant, R.A. and Pana
- Page 854:
413 ReferencesCavedini, P., Cisima,
- Page 858:
415 ReferencesCohen-Bendhahan, C.C.
- Page 862:
417 ReferencesDannon, P.N., Lowengr
- Page 866:
419 ReferencesDrake, A.I., McDonald
- Page 870:
421 ReferencesFalret, J. (1854). M
- Page 874:
423 References(1968). An Outline of
- Page 878:
425 ReferencesGardini, S., De Beni,
- Page 882:
427 ReferencesGould, R., Miller, B.
- Page 886:
429 ReferencesHarrow, M., O’Conne
- Page 890:
431 ReferencesCohen, L.J., Simeon,
- Page 894:
433 ReferencesJones, I. and Craddoc
- Page 898:
435 ReferencesKendell, R. and Jable
- Page 902:
437 ReferencesKolb, B. and Whishaw,
- Page 906:
439 ReferencesLang, D.J., Khorram,
- Page 910:
441 ReferencesLilienfeld, S.O., Van
- Page 914:
443 ReferencesMartin, M.L.S. (1999)
- Page 918:
445 ReferencesMergl, R., Seidscheck
- Page 922:
447 ReferencesMurray, V., McKee, I.
- Page 926:
449 ReferencesOvsiew, F. (1997). Be
- Page 930:
451 ReferencesPfuhlmann, B., Stober
- Page 934:
453 ReferencesQuraishi, S. and Fran
- Page 938:
455 ReferencesRohde, A. and Marnero
- Page 942:
457 ReferencesSantor, D.A., Ascher-
- Page 946:
459 ReferencesShefner, J.M. (1992).
- Page 950:
461 ReferencesSorensen, M.J., Mors,
- Page 954:
463 ReferencesSwaab, D.F., Gooren,
- Page 958:
465 ReferencesTenback, D.E., van Ha
- Page 962:
467 Referencesvan der Zwaard, R. an
- Page 966:
469 ReferencesWijeratne, C., Hickie
- Page 970:
471 ReferencesZarate, C.A. Jr., Toh
- Page 974:
473 Indexeffects of increased 137-1
- Page 978:
475 Indexcoordination problems 178c
- Page 982:
477 IndexFregoli syndrome 81, 280Fr
- Page 986:
479 Indexcognitive deficits 75-76de
- Page 990:
481 Indexphenomenology, descriptive
- Page 994:
483 IndexSutton’s Law, diagnosis