EUCAST posters at ECCMID 2012
EUCAST posters at ECCMID 2012
EUCAST posters at ECCMID 2012
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
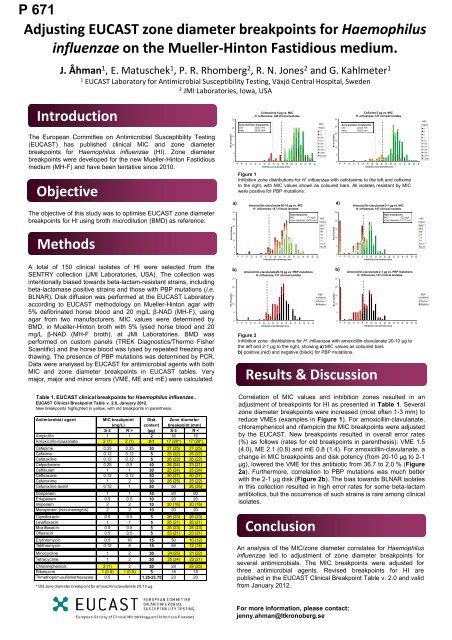
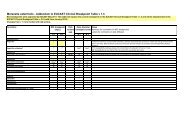
66668888066668888P682<strong>EUCAST</strong> standardised disk diffusion methodologyfor Campylobacter jejuni and C. coliE. M<strong>at</strong>uschek 1 , K. Veldman 2 , A. Hakanen 3 , S. Bengtsson 1 , M. Lehtopolku 3 , D. Mevius 2 and G. Kahlmeter 11<strong>EUCAST</strong> Labor<strong>at</strong>ory for AST, Växjö, Sweden, 2 Central Veterinary Institute (CVI), Lelystad, the Netherlands3N<strong>at</strong>ional Institute for Health and Welfare (THL), Turku, FinlandIntroductionAntimicrobial susceptibility testing of Campylobacter spp. inclinical labor<strong>at</strong>ories is often performed using gradient MIC testsor disk diffusion, but standardised methodology and interpretivecriteria are often lacking. The European Committee onAntimicrobial Susceptibility Testing (<strong>EUCAST</strong>) is in the processof establishing clinical MIC breakpoints for C. jejuni and C. coli.ObjectiveThe objective of this study was to investig<strong>at</strong>e if the standard<strong>EUCAST</strong> MH-F medium and disk diffusion criteria can be usedfor reproducible antimicrobial susceptibility testing of C. jejuniand C. coli.MethodsPreliminary testing was performed on 15 C. jejuni and 15 C. colifrom the Netherlands with known MIC values (brothmicrodilution) including isol<strong>at</strong>es with and without resistancemechanisms. Additional testing was performed on 17 C. jejuniand 12 C. coli from Finland. All isol<strong>at</strong>es were tested in triplic<strong>at</strong>efor ciprofloxacin 5 µg, erythromycin 15 µg and tetracycline 30 µg.Investig<strong>at</strong>ed variables are shown in Table 1.Table 1Investig<strong>at</strong>ed variablesMediumIncub<strong>at</strong>ionReading of zonesResultsUnsupplemented Mueller-Hinton agar (MH) and Mueller-Hinton agarwith 5% defibrin<strong>at</strong>ed horse blood and 20 mg/L β-NAD (MH-F)35, 37, 39 and 41°C24 and 44 hSmallest and largest appearing zone when tilting the pl<strong>at</strong>eAll tests were performed with a 0.5 McFarland inoculum and microaerobicincub<strong>at</strong>ion in plastic jars.The proposed <strong>EUCAST</strong> disk diffusion methodology for C. jejuniand C. coli is presented in Table 2. BothC. jejuni and C. coligrew best on MH-F pl<strong>at</strong>es <strong>at</strong> 41°C. All C. jejuni grew well after 24h of incub<strong>at</strong>ion, whereas some C. coli required 44 h beforeinhibition zones could be read. Swarming was avoided by dryingpl<strong>at</strong>es before inocul<strong>at</strong>ion.All isol<strong>at</strong>es with MICs above the epidemiological cut off (ECOFF)were identified as non-wild type also with the disk diffusion test(Figure 1), irrespective of whether the smallest or largest zonewas used. The results were reproducible within and between thesites. The standard devi<strong>at</strong>ion for triplic<strong>at</strong>e tests ranged from 0.4-1.7 mm, with the largest vari<strong>at</strong>ion for inhibition zones read after44 h of incub<strong>at</strong>ion. Examples of combined inhibition zonedistributions from several sites are shown in Figure 2.No of isol<strong>at</strong>esNo of isol<strong>at</strong>esNo of isol<strong>at</strong>esNo of isol<strong>at</strong>esReproducible disk diffusion testing of C. jejuni and C. coli can beperformed using the <strong>EUCAST</strong> MH-F media. Swarming waseffectively avoided by pre-drying of pl<strong>at</strong>es. Disk diffusioncorrel<strong>at</strong>ed well to MIC determin<strong>at</strong>ion and reliably distinguishedbetween wild-type and non-wild type isol<strong>at</strong>es. Further evalu<strong>at</strong>ionof the methodology is currently performed <strong>at</strong> several labor<strong>at</strong>oriesin Europe.40353025201510180160140120100807060504030201050121086420806040200ConclusionsTable 2<strong>EUCAST</strong> proposed disk diffusion methodology for Campylobacter jejuni andCampylobacter coli .Mueller-Hinton agar with 5% defibrin<strong>at</strong>ed horse blood and 20 mg/L β-NAD (MH-F)Medium(Pl<strong>at</strong>es should be dried before incub<strong>at</strong>ion to avoid swarming, either <strong>at</strong>room temper<strong>at</strong>ure (20-22°C) over night or <strong>at</strong> 35°C for 1-2 hours.)Inoculum McFarland 0.5Incub<strong>at</strong>ionReading of zonesCiprofloxacin 5 µg vs. MIC, Campylobacter jejuni and coli57 clinical isol<strong>at</strong>es tested in duplic<strong>at</strong>e1010ECOFF: WT ≤ 1 mg/L1012Campylobacter jejuni with ciprofloxacin 5 µg414 clinical isol<strong>at</strong>es121412141614161816182022182024202226Erythromycin 15 µg vs. MIC, Campylobacter jejuni30 clinical isol<strong>at</strong>es tested in duplic<strong>at</strong>eECOFF: WT ≤ 4 mg/L2422282628303234Inhibition zone diameter (mm)Campylobacter coli with ciprofloxacin 5 µg170 clinical isol<strong>at</strong>es3024322634Inhibition zone diameter (mm)28Inhibition zone diameter (mm)Microaerobic environment41°C24 hours ± 30 minutes(C. coli with non-sufficient growth after 24 h incub<strong>at</strong>ion are reincub<strong>at</strong>edimmedi<strong>at</strong>ly and read after totally 40-48 h incub<strong>at</strong>ion.)<strong>EUCAST</strong> standard reading instructions:Read MH-F pl<strong>at</strong>es from the front with the lid removed illumin<strong>at</strong>ed withreflected light. Zone edges should be read <strong>at</strong> the point of completeinhbition as judged by the unaided eye.3630383640323842344044364642483844504046MIC(mg/L)≥32481684210.50.25≤0.12MIC(mg/L)≥12864321684210.550No of isol<strong>at</strong>esNo of isol<strong>at</strong>esNo of isol<strong>at</strong>esNo of isol<strong>at</strong>es1098765432103530252015105050454035302520151050605040302010Tetracycline 30 µg vs. MIC, Campylobacter jejuni and coli29 clinical isol<strong>at</strong>es tested in duplic<strong>at</strong>e1010ECOFF: WT ≤ 2 mg/LErythromycin 15 µg vs. MIC, Campylobacter coli27 clinical isol<strong>at</strong>es tested in duplic<strong>at</strong>e1012Campylobacter jejuni with tetracycline 30 µg409 clinical isol<strong>at</strong>es12141214161416101214161820222426283032343638404244184616481850202218202420222624222826Campylobacter coli with tetracycline 30 µg168 clinical isol<strong>at</strong>es24302832263034Inhibition zone diameter (mm)ECOFF: WT ≤ 16 mg/L28Inhibition zone diameter (mm)Figure 1. Inhibition zone distributions for C.jejuni and C. coli with MIC values as colouredbars. Inhibition zones were read according to <strong>EUCAST</strong> standard reading instructions <strong>at</strong> onesite on MH from two manufacturers. D<strong>at</strong>a for erythromycin are presented separ<strong>at</strong>ely, due todifferent ECOFFs.3236303438Inhibition zone diameter (mm)364038404244464850010121416182022242628303234363840424446485032423444364638485040MIC(mg/L)≥12864321684210.50.250.12MIC(mg/L)≥12832168421Inhibition zone diameter (mm)Inhibition zone diameter (mm)For more inform<strong>at</strong>ion, please contact:erika.m<strong>at</strong>uschek@ltkronoberg.seFigure 2. Combined inhibition zone distributions for ciprofloxacin and tetracycline from 4-6 sites for C. jejuni and C. coli, respectively.
06688668866886688P676Antimicrobial susceptibility testing of Listeria monocytogeneswith <strong>EUCAST</strong> breakpoints: A multi‐labor<strong>at</strong>ory study.Karen Bowker 1 , Jenny Åhman 2 , Olav N<strong>at</strong>ås 3 , Israel Nissan 4 , Pia Littauer 5 and Erika M<strong>at</strong>uschek 21Dept of Microbiology, Southmead Hospital, Bristol, United Kingdom, 2 <strong>EUCAST</strong> Labor<strong>at</strong>ory for AST, Växjö, Sweden3Dept of Medical Microbiology, Stavanger University Hospital, Norway4Government Central Labor<strong>at</strong>ories, Jerusalem, Israel, 5 Dept of Clinical Microbiology, Hvidovre Hospital, DenmarkIntroductionThe European Committee on Antimicrobial Susceptibility Testing(<strong>EUCAST</strong>) has recently proposed clinical MIC breakpoints basedon epidemiological cut-off (ECOFF) values for Listeriamonocytogenes.ObjectiveThe objective of this study was to establish corresponding zonediameter breakpoints based on the <strong>EUCAST</strong> Mueller-HintonFastidious medium (MH-F) in a multi-labor<strong>at</strong>ory study and tovalid<strong>at</strong>e the use of a gradient test for MIC determin<strong>at</strong>ion usingbroth microdilution (BMD) as reference.MethodsA total of 129 clinical isol<strong>at</strong>es of L. monocytogenes werecollected from five sites in Denmark, Israel, Norway, Swedenand the United Kingdom. Antimicrobial susceptibility testing wasperformed against ampicillin, benzylpenicillin, erythromycin,meropenem and trimethoprim-sulfamethoxazole. Disk diffusionwas performed for all isol<strong>at</strong>es <strong>at</strong> all sites on Mueller-Hinton agarwith 5% defibrin<strong>at</strong>ed horse blood and 20 mg/L β-NAD (MH-F)according to <strong>EUCAST</strong> methodology. Media (commercial and inhouseprepared pl<strong>at</strong>es) and disks from different manufacturerswere used <strong>at</strong> the various sites. MIC determin<strong>at</strong>ion wasperformed with BMD (TREK Diagnostics/Thermo FisherScientific) and Etest (bioMérieux) <strong>at</strong> Southmead Hospital, UK.BMD was performed on custom panels containing MH broth with5% lysed horse blood (by repe<strong>at</strong>ed freezing and thawing) and 20mg/L β-NAD (MH-F broth) and Etest was performed on MH-Fmedia. All d<strong>at</strong>a were analysed by <strong>EUCAST</strong>.ResultsAll L. monocytogenes isol<strong>at</strong>es grew well within 16-20 hours ofincub<strong>at</strong>ion on the MH-F medium. The correl<strong>at</strong>ion between BMDand Etest MICs was excellent, with 99.4% of Etest values within± 1 dilution of the BMD values. Zone diameter breakpoints wereestablished (Table 1) in such a way th<strong>at</strong> the MIC ECOFFcorresponded to the zone diameter distribution ECOFF for eachantibiotic agent (examples in Figure 1a). Reproducibilitybetween the sites was good (Figure 1b) and small vari<strong>at</strong>ions ininhibition zones were mainly due to vari<strong>at</strong>ions in media and disksfrom different manufacturers.Table 1<strong>EUCAST</strong> clinical MIC breakpoints for Listeria monocytogenesand corresponding zone diameter breakpoints.<strong>EUCAST</strong> Clinical Breakpoint Table v 2.0MIC breakpoint Disk Zone diameterAntibiotic agent(mg/L) content breakpoint (mm)S ≤ R > (µg) S ≥ R
6688Susceptibility testing of ten antibiotics against Corynebacterium spp. determined bybroth microdilution, Etest and <strong>EUCAST</strong> disk diffusion methodsC. Salas *1, C. Karlsson 2 , A. Åkerlund3 , C. RodríguezMirones 1 , E. M<strong>at</strong>uschek 2 ,L. Martíneznez-Martínez1,4 , G. Kahlmeter 21Servicio de Microbiología, Hosp. Univ. Marqués de Valdecilla, Santander, Spain. 2 <strong>EUCAST</strong> Labor<strong>at</strong>ory for Antimicrobial Susceptibility Testing, Växjö,Sweden. 3 Department of Clinical and Experimental Medicine, Linköping University, Sweden. 4 Fac. de Medicina, Universidad de Cantabria, Spain.[Revised] AbstractM<strong>at</strong>erial and MethodsObjective: <strong>EUCAST</strong> has not yet defined breakpoints forclinical c<strong>at</strong>egories of clinically relevant antibiotics forCorynebacterium. In this study, the performance of threemethods for susceptibility testing of five Corynebacteriumspecies has been evalu<strong>at</strong>ed.Methods: The activity of penicillin G (PNG), ciprofloxacin(CIP), moxifloxacin (MOX), gentamicin (GEN),vancomycin (VAN), clindamycin (CLI), tetracycline (TET),linezolid (LNZ), rifampin (RIF) and cotrimoxazole (SXT)against 60 Corynebacterium spp. (12 isol<strong>at</strong>es each of thefollowing species: C. stri<strong>at</strong>um, C. amycol<strong>at</strong>um, C. jeikeium,C. urealyticum and C. pseudodiphtheriticum) weredetermined using BMD (broth microdilution with c<strong>at</strong>ionadjustedMueller-Hinton broth with 3% laked horseblood), or on solid medium MH-F (Mueller-Hinton agarwith 5% defibrin<strong>at</strong>ed horse blood and 20 mg β-NAD/L) byEtest and disk diffusion (disk contents as defined by<strong>EUCAST</strong>). BMD was performed in one lab in Spain, Etestin one lab in Sweden and disk diffusion in three labs (onein Spain and two in Sweden). Pl<strong>at</strong>es were incub<strong>at</strong>ed <strong>at</strong> 35ºCin air (microdilution) or 5% CO 2 (agar media) and readafter 16-20 h or, in case of insufficient growth, afteranother 24 h.Results: Microdilution results could be read after 16-20 hincub<strong>at</strong>ion for all species but C. pseudodiphtheriticum. EtestMICs and inhibition zones could be determined <strong>at</strong> 16-20 hfor all 12 C. stri<strong>at</strong>um, but incub<strong>at</strong>ion for 40-44 h wasneeded to a varying degree for other species. Essentialagreement (EA, th<strong>at</strong> in ±1 dilution) between microdilutionand Etest was: PNG (81,7%), CIP (77,9%), MOX (49,1%),GEN (83,0%), VAN (96,6%), CLI (61,0%), TET (59,3%),LNZ (71,1%), RIF (88,3%) and SXT (42,4%). For species,EA were: C. jeikeium (84,2%), C. stri<strong>at</strong>um (77,5%), C.amycol<strong>at</strong>um (73,3%), C. ure<strong>at</strong>lyticum (60,8%) and C.pseudodiphtheriticum (58,5%). Correl<strong>at</strong>ion between BMDMICs and inhibition zones was good, i.e. isol<strong>at</strong>es with highMICs had small inhibition zones and viceversa. Correl<strong>at</strong>ionbetween inhibition zones from three labs was overall good,even when zones had to be read after another 24 h.Conclusions: Growth of Corynebacterium spp. on MH-Fdiffers between species and it is sometimes necessary toincub<strong>at</strong>e pl<strong>at</strong>es for longer than the standard 16-20 h. Thereis a good correl<strong>at</strong>ion between BMD and Etest forvancomycin. More studies on MIC/zone correl<strong>at</strong>ion onspecies-identified Corynebacterium must be performedbefore breakpoints (or ECOFFs) can be established.Background<strong>EUCAST</strong> has not yet established specific criteria forclinical interpret<strong>at</strong>ion of susceptibility testing results forCorynebacterium spp.In this study, we have compared three different methods(broth microdilution, disk-diffusion and gradient-diffusion)to study the in vitro activity of ten antimicrobial agentsagainst five of the more clinically relevant species ofcorynebacteria.We aimed to obtain inform<strong>at</strong>ion aboutperformance of the assays and on the agreement of resultsobtained with every methodology.Bacterial isol<strong>at</strong>es: 60 clinical isol<strong>at</strong>es (12 isol<strong>at</strong>es perspecies), including C. stri<strong>at</strong>um, C. amycol<strong>at</strong>um, C.jeikeium, C. urealyticum and C. pseudodiphtheriticum.Susceptibility testing:Broth-microdilution:In-house prepared microdilution pl<strong>at</strong>es using c<strong>at</strong>ionadjustedMueller-Hinton broth with 3% laked horseblood. The following 10 antibiotics were tested:penicillin G (PNG), ciprofloxacin (CIP), moxifloxacin(MOX), gentamicin (GEN), vancomycin (VAN),clindamycin (CLI), tetracycline (TET), linezolid(LIN), rifampin (RIF) and cotrimoxazole (SXT).Pl<strong>at</strong>es were incub<strong>at</strong>ed <strong>at</strong> 35±2ºC and read after anincub<strong>at</strong>ion in air for 16-20 h.Disk diffusion:<strong>EUCAST</strong> method, using Mueller-Hinton agar with5% of defibrin<strong>at</strong>ed horse blood and 20 mg β-NAD/L(Mueller-Hinton F).ResultsPercentages of strains growing in Mueller-Hinton broth (microdilution) and on Mueller-Hinton F(gradient diffusion) <strong>at</strong> 20/44 h.Essential agreement (%) (in ±1 dilution) between MICs of 10 agents against Corynebacterium spp.determined by gradient diffusion (Etest) with broth microdilution as referencePNG CIP MOX GEN VAN CLIN TET LIN RIF SXT% agreementper speciesC. stri<strong>at</strong>um 83.3 83.3 50.0 91.7 91.7 91.7 66.7 75.0 75.0 66.7 77.5C. amycol<strong>at</strong>um 83.3 100 16.7 100 100 83.3 66.7 83.3 91.7 8.3 73.3C. jeikeium 91.7 100 83.3 91.7 100 83.3 66.7 75.0 100 66.7 84.2C. urealyticum 75.0 75.0 58.3 83.3 100 25.0 25.0 66.7 75.0 25.0 60.8C. pseudodiph. 75.0 27.3 36.4 45.4 90.9 18.2 90.9 54.5 100 45.4 58.5% agreementper antibiotic 81.7 77.9 49.1 83.0 96.6 61.0 59.3 71.1 88.3 42.4The following disks were evalu<strong>at</strong>ed: PNG 1 unit, CIP 5μg, MOX 5 μg, GEN 10 μg, VAN 5 μg, CLI 2 μg, TET30 μg, LIN 10 μg, RIF 5 μg and SXT 1.25-23.75 μg.Gradient diffusion:The <strong>EUCAST</strong> method for disk diffusion was also used,with Etest strips of the same agents considered in thetwo other assays.Agar pl<strong>at</strong>es (both disk diffusion and gradient diffusionmethods) were incub<strong>at</strong>ed in 5% CO 2 for 16-20 h.When growth was insufficient <strong>at</strong> th<strong>at</strong> time, incub<strong>at</strong>ionwas extended for 24 h (total incub<strong>at</strong>ion in these cases:40-44 h.).S. pneumoniae ATCC 49619 and S. aureus ATCC29213 were used as quality control strains.C. stri<strong>at</strong>um ATCC 6940 and C. urealyticum ATCC43042 were also included in the study.ConclusionsNo of readingsNo of readings807060504030201001614121086420Moxifloxacin 5 µg vs. MIC (BMD)Corynebacterium spp, 60 isol<strong>at</strong>es tested <strong>at</strong> three sites10Tetracycline 30 µg vs. MIC (BMD)Corynebacterium spp, 60 isol<strong>at</strong>es tested <strong>at</strong> three sites10121214141616181820202222242426262828Inhibition zone diameter (mm)3032Inhibition zone diameter (mm) Growth on MH-F differs between Corynebacterium species. For some organisms, it is necessary toincub<strong>at</strong>e pl<strong>at</strong>es for longer than the standard 16-20 h, up to 40-44h.There is a good correl<strong>at</strong>ion between BMD/Etest for vancomycin, and to a lesser extent (>80%) forpenicillin, gentamicin and rifampin.Correl<strong>at</strong>ion between MIC/disk difussion was good with small inhibiton zones corresponding tohigh MICs. More studies must be performed before breakpoints (or ECOFFs) can be established.A good correl<strong>at</strong>ion among inhibition zones determined by disk diffussion in the three particip<strong>at</strong>inglabor<strong>at</strong>ories was noted.303432363438364038424044MIC(mg/L)>161684210.50.250.120.060.031684210.50.250.12Examples of combined inhibition zone distributions for Corynebacterium spp.from the three sites with corresponding MIC values as coloured bars.Carlos Salas VeneroE-mail: csalas@humv.es
The Brucella blood agar for disc diffusionantimicrobial susceptibility testing– reproducibility results for Clostridium difficile ATCC 700057U. S. Justesen 1 , L. T. Erikstrup 2 , T. K. Danielsen 1 , E. M<strong>at</strong>uschek 3 and G. Kahlmeter 31) Department of Clinical Microbiology, Odense University Hospital, Odense,2) Department of Clinical Microbiology, Aarhus University Hospital, Aarhus, Denmark and3) <strong>EUCAST</strong> Labor<strong>at</strong>ory for Antimicrobial Susceptibility Testing, Växjö, Sweden.Introduction and PurposeResultsThe <strong>EUCAST</strong> disk diffusion antimicrobial susceptibilitytesting method for fastidious organisms is based onthe Mueller-Hinton fastidious agar (MH-F). In a pilotstudy, most anaerobic bacteria did not grow wellenough on MH-F to permit antimicrobialsusceptibility testing (Justesen et al.). We decided toinvestig<strong>at</strong>e whether or not the Brucella Blood Agarsupplemented with hemin and vitamin K (BBA),recommended for antimicrobial susceptibility testingof anaerobic bacteria with gradient strips, might alsobe suited for disk diffusion testing of C. difficile.Table 1. Zone diameter mean values and ranges are shown in the table.Antimicrobial agent Inhibition zone diameters (mm) for Clostridium difficile ATCC 700057Piperacillin/tazobactam(30/6 μg)Meropenem(10 μg)Metronidazole(5 μg)Clindamycin(2 μg)Day 1 and 2 <strong>at</strong> 37°C(10% CO 2, 10% H 2and 80% N 2)(n=12)27.5 (25.7-28.3)26.7 (25.6-28.2)29.7 (28.7-30.1)29.7 (28.9-30.2)38.7 (37.6-40.9)35.5 (35.3-36.4)10.3 (10.1-10.5)10.3 (9.6-10.9)5% CO 2(10% H 2, 85% N 2and 37°C)(n=12)35°C(10% CO 2, 10% H 2and 80% N 2)(n=12)26.0 (25.2-26.3) 26.5 (25.7-27.3)31.4 (30.5-32.1) 31.5 (30.9-31.8)38.6 (37.6-39.7) 38.9 (38.2-40.6)10.8 (10.4-11.1) 11.8 (10.8-12.3)MethodsPenicillin G(1 U)Vancomycin(5 μg)6.0 (6.0) NO ZONE6.0 (6.0) NO ZONE23.1 (22.5-24.0)25.5 (24.5-26.3)8.3 (6.0-9.0) 6.4 (6.0-8.2)23.0 (22.6-23.7) 23.5 (23.1-24.3)C. difficile ATCC 700057 was tested with Etest(bioMérieux, Craponne, France) gradient strips(piperacillin/tazobactam, meropenem,metronidazole, clindamycin, penicillin G,vancomycin, moxifloxacin and tigecycline) on BBA(Becton Dickinson, Heidelberg, Germany) accordingto the manufacturer’s instructions. Thecorresponding disk (<strong>EUCAST</strong> disk strength) wasincluded on each pl<strong>at</strong>e (Oxoid, Basingstoke, UK). Alltests were repe<strong>at</strong>ed twelve times. I.e. twelve pl<strong>at</strong>eswere incub<strong>at</strong>ed day 1 <strong>at</strong> 37°C in an anaerobeenvironment (10% CO 2 , 10% H 2 and 80% N 2 ) for 24hours with each antimicrobial agent to assess intradayvariability. This was repe<strong>at</strong>ed day 2 to assessinter-day variability. Etest results were comparedwith the acceptable ranges for ATCC 700057(reference agar dilution testing, CLSI guideline M11-A7). Twelve pl<strong>at</strong>es with disks only were alsoincub<strong>at</strong>ed <strong>at</strong> 5% CO 2 (10% H 2 and 85% N 2 ) <strong>at</strong> 37°Cand another twelve pl<strong>at</strong>es <strong>at</strong> 35°C with 10% CO 2 ,10% H 2 and 80% N 2 . Also; the effect of thioglycoll<strong>at</strong>eversus saline 0.85% for inoculum prepar<strong>at</strong>ion andprereduction of the BBA pl<strong>at</strong>es were investig<strong>at</strong>ed forvancomycin, metronidazole, moxifloxacin andclindamycin (Figure 1).Moxifloxacin(5 μg)Tigecycline(15 μg)23.0 (22.4-23.6)22.7 (21.8-23.7)34.5 (34.0-34.9)33.1 (32.2-34.6)Figure 1.Clostridium difficile ATCC 700057, McFarland 1.0on BBA with clindamycin 2 μg (DA 2),metronidazole 5 μg (MTZ 5), vancomycin 5 μg (VA5) and moxifloxacin 5 μg (MXF 5) disks. Growth isconfluent on the BBA.All Etest results were within acceptable rangesand the intra- and inter-day variability was
Disk diffusion an,microbial suscep,bility tes,ng of Clostridium difficile L. T. Erikstrup 1,2 , T. K. Danielsen 3 , V. Hall 4 , K. Fuursted 1 , G. Kahlmeter 5 , and U. S. Justesen 3 1) Department of Clinical Microbiology, Aarhus University Hospital, Aarhus, Denmark 2) InsCtute of Clinical Medicine, Aarhus University, Aarhus, Denmark 3) Department of Clinical Microbiology, Odense University Hospital, Odense, Denmark, 4) Anaerobe Reference Unit, University Hospital of Wales, Cardiff, Wales, 5) <strong>EUCAST</strong> Labor<strong>at</strong>ory for AnCmicrobial SuscepCbility TesCng, Växjö, Sweden. Introduc,on and Purpose Results The clinical significance of Clostridium difficile and the emergence of decreased suscep,bility towards metronidazole and vancomycin have highlighted the importance of an,microbial suscep,bility tes,ng of C. difficile and the importance of having a simple tes,ng method for the rou,ne labor<strong>at</strong>ory. The aim of our study was to evalu<strong>at</strong>e disk diffusion for suscep,bility tes,ng of C. difficile by comparing disk diffusion zone diameters with MICs from gradient tests. MIC (mg/L)MIC (mg/L)MIC (mg/L)MIC (mg/L)MIC (mg/L) Methods Consecu,ve clinical and toxigenic isol<strong>at</strong>es of C. difficile (n=211) were collected from pa,ents with diarrhoea hospitalised <strong>at</strong> Aarhus University Hospital (n=110) in 2008 and from Odense University Hospital (n=101) in 2010. Furthermore, ten clinical isol<strong>at</strong>es of C. difficile from the University Hospital of Wales with Figure 1. Distribu,on of inhibi,on zone diameters (disk diffusion method) and MICs (gradient test) for 221 isol<strong>at</strong>es of C. difficile tested against metronidazole (5 μg disk), vancomycin (5 μg disk), moxifloxacin (5 μg disk), and clindamycin (2 μg disk). Each isol<strong>at</strong>e is represented in the zone diameter histogram in a colour represen,ng its MIC value. known reduced suscep,bility to either metronidazole (n=4, MIC 1.5, 2, 2, 3 mg/L, ECOFF ≤ 2 mg/L) or vancomycin (n=6, MIC 1.5, 2, 2, 2, 3, 3 mg/L, ECOFF ≤ 2 mg/L) were included. MIC determina,on was performed by gradient test. Etest strips (bioMérieux, Craponne, France) with metronidazole, vancomycin, moxifloxacin, and clindamycin were placed on Brucella Blood Agar supplemented with hemin and vitamin K (Becton Dickinson, Heidelberg, Germany) A total of 221 clinical isol<strong>at</strong>es of C. difficile from Denmark and Wales were tested. The distribu,on of inhibi,on zone diameters and MICs for C. difficile isol<strong>at</strong>es towards metronidazole, vancomycin, moxifloxacin, and clindamycin are illustr<strong>at</strong>ed in the histograms (Figure 1). The four isol<strong>at</strong>es with known reduced suscep,bility to metronidazole were clearly separ<strong>at</strong>ed from the wild type by 9 mm. The six isol<strong>at</strong>es with known reduced suscep,bility to vancomycin had zone diameters between 15 to 19 mm as compared to the consecu,ve clinical isol<strong>at</strong>es from Denmark which all had zone diameters above 18 mm. Bivariable regression analysis showed an acceptable to excellent correla,on between the log-transformed MIC versus the untransformed zone diameter, thus the R 2 was 0.75 for metronidazole, 0.55 for vancomycin, 0.97 for moxifloxacin and 0.63 for clindamycin. according to the manufacturer’s instruc,ons. Disk diffusion was performed with Oxoid disks (Oxoid, Basingstoke, UK) with vancomycin (5 Conclusion μg), metronidazole (5 μg), moxifloxacin (5 μg) and clindamycin (2 μg) on Brucella Blood Agar. Pl<strong>at</strong>es were incub<strong>at</strong>ed <strong>at</strong> 37°C in an anaerobic <strong>at</strong>mosphere (10% CO 2 , 10% H 2 and 80% N 2 ) for 24 hours. The zone diameter was read <strong>at</strong> 100% inhibi,on. For most reference strains, almost regardless of species and an,microbial agent, the aggreg<strong>at</strong>ed inhibi,on zone values, of repe<strong>at</strong>ed tes,ng, form a distribu,on most o`en covering 6-‐8 mm [1]. For the 221 clinical isol<strong>at</strong>es of C. difficile tested towards metronidazole, vancomycin, moxifloxacin, and clindamycin we found th<strong>at</strong> for each MIC value, the inhibi,on zones varied from 0 to 8 mm with the majority exhibi,ng 5 to 6 mm varia,on. Therefore, we conclude th<strong>at</strong> there is an excellent agreement between disk diffusion zone diameter and the MIC as measured by Etest and consequently we recommend the disk diffusion method as a reliable op,on for an,microbial suscep,bility tes,ng of C. difficile. Zone diameter breakpoints can now be established by <strong>EUCAST</strong> Correspondence References Corresponding author: Lise Tornvig Erikstrup E-‐mail: liseerik@rm.dk Poster 681, <strong>ECCMID</strong>, London <strong>2012</strong> 1. Kronvall G, Giske CG, Kahlmeter G. Seqng interpre,ve breakpoints for an,microbial suscep,bility tes,ng using disk diffusion. Int. J. An,microb. Agents. 2011 Oct;38(4):281–90.
P1092<strong>ECCMID</strong> <strong>2012</strong>JMI Labor<strong>at</strong>oriesNorth Liberty, IA, USAwww.jmilabs.com319.665.3370, fax 319.665.3371helio-sader@jmilabs.comAntimicrobial Susceptibility and Species Identific<strong>at</strong>ion ofCorynebacterium spp. Strains Collected in Europe andUSA Medical Centers (2006-2010)HS SADER, PR RHOMBERG, RN JONES, J ÅHMAN, E MATUSCHEK, G KAHLMETERJMI Labor<strong>at</strong>ories, North Liberty, Iowa, USA; <strong>EUCAST</strong> Labor<strong>at</strong>ory for Antimicrobial Susceptibility TestingAbstractObjectives: To evalu<strong>at</strong>e the antimicrobial susceptibility ofCorynebacterium spp. clinical strains collected fromEuropean and USA medical centers. The accuracy ofspecies identific<strong>at</strong>ions performed <strong>at</strong> local labs was alsoassessed.Methods: 121 Corynebacterium strains were collectedfrom serious infections between 2006 and 2010 as part ofthe SENTRY Antimicrobial Surveillance Program from 15and 18 medical centers in 9 European countries and USA,respectively. The strains were susceptibility (S) tested bythe CLSI broth microdilution method in c<strong>at</strong>ion-adjustedMueller-Hinton broth against numerous antimicrobialagents. MIC results were interpreted according to CLSIM45 breakpoint criteria. There are yet no criteria from<strong>EUCAST</strong>. Species identific<strong>at</strong>ions were performed byMALDI-TOF methodology using the Bruker Biotypersystem.Results: Isol<strong>at</strong>es were from bacteremia (53.6%), skin andskin structure (17.3%), pneumonia (12.7%), among otherinfection sites. Vancomycin (100.0% S) and daptomycin(99.1% S) showed potent activity against Corynebacteriumwith MIC 50/90 of 0.25/0.5 and ≤0.06/0.25 mg/L, respectively.C. jeikeium and C. urealyticum species groupsdemonstr<strong>at</strong>ed lower S r<strong>at</strong>es, 0.0% for penicillin and 36.8-40.0% for gentamicin, compared to other Corynebacteriumspecies groups (see Table). 61 of 121 strains (50.4%)were identified to species level by the clinical labor<strong>at</strong>oriesand species identific<strong>at</strong>ion was confirmed by the MALDI-TOF analysis on 47 (77.0%) of those strains. Theremaining 14 strains had incorrect species (12) or genus(2 strains, Brevibacterium and Microbacterium). Among the60 strains submitted as unspeci<strong>at</strong>ed Corynebacterium, 51(85.0%) strains were confirmed as Corynebacterium andidentified to species level, while the remaining 9 strainswere identified to a different genus (Brevibacterium [3],Microbacterium [2], Dermabacter [1], Rhodococcus [1],Staphylococcus [1], Turicella [1]) by the MALDI-TOFanalysis.Conclusions: Antimicrobial resistance differences amongCorynebacterium species were noted with higher r<strong>at</strong>esamong the C. jeikeium and C. urealyticum species groups.Identific<strong>at</strong>ion to the species level in clinical labor<strong>at</strong>ories forCorynebacterium remains a challenge; however, theMALDI-TOF method appears to gener<strong>at</strong>e more completeand accur<strong>at</strong>e identific<strong>at</strong>ions to be compared toantimicrobial-S profiles.Organism/speciesMIC 50 (mg/L) / % susceptible(no. tested)DAP ERY GENT PEN VANCAll Corynebacterium spp.(110)≤0.06/99.1 >2/24.6 ≤2/80.9 1/51.8 0.25/100.0C. amycol<strong>at</strong>um (33) ≤0.06/100.0 >2/27.3 ≤2/84.9 1/63.3 0.5/100.0C. jeikeium (19) 0.12/100.0 2/10.5 >8/36.8 >4/0.0 0.5/100.0C. stri<strong>at</strong>um (37) ≤0.06/99.3 >2/24.3 ≤2/97.3 1/56.8 0.25/100.0C. urealyticum (5) ≤0.06/100.0 >2/40.0 >8/40.0 >4/0.0 0.5/100.0Other Corynebacterium≤0.06/100.0 2/31.3 ≤2/100.0 0.25/93.8 0.25/100.0spp. (16)DAP = daptomycin, ERY = erythromycin, GENT = gentamicin, PEN = penicillin, VAN = vancomycin.IntroductionThe genus Corynebacterium is composed of <strong>at</strong> least 67species of which many are medically important. WhenGram's stained, corynebacteria are slightly curved Grampositiverods with one end slightly wider giving theappearance of a club shape and clusters on the slide give aChinese letter type appearance. Corynebacteria areaerobic, non-spore forming, c<strong>at</strong>alase positive and usuallynon-motile.Many species of corynebacteria are part of the normal floraof the skin which makes the correl<strong>at</strong>ion with clinicalsignificance (cause of infection) difficult when they areisol<strong>at</strong>ed from specimens. Corynebacteria should beidentified to species level only if isol<strong>at</strong>ed from normallysterile body sites or when they are alone or the predominantp<strong>at</strong>hogen from an adequ<strong>at</strong>ely collected clinical sample,especially when m<strong>at</strong>ched with a Gram's stain report. Manyautom<strong>at</strong>ed systems and biochemical reaction methods havebeen developed and optimized for the identific<strong>at</strong>ion ofclinically relevant Corynebacterium species.One new method for the identific<strong>at</strong>ion of bacterial speciesunder development is the use of M<strong>at</strong>rix Assisted LaserDesorption Ioniz<strong>at</strong>ion-Time of Flight (MALDI-TOF) massspectrometry to measure the unique molecular fingerprint ofa tested organism and compare to the extensive storedd<strong>at</strong>abase to determine the identity to the species level.M<strong>at</strong>erials and MethodsBacterial isol<strong>at</strong>es: 121 Corynebacterium strains werecollected between 2006 and 2010 from serious infectionsand submitted to the SENTRY Antimicrobial SurveillanceProgram. Fifteen participant medical centers were loc<strong>at</strong>edin Europe (Belgium, France, Germany, Ireland, Italy, Spain,Sweden, Switzerland and United Kingdom) and 18 wereloc<strong>at</strong>ed in the United St<strong>at</strong>es (USA). The isol<strong>at</strong>es werecollected primarily from bloodstream (53.6%) followed bylower numbers from skin and skin structure infections(17.3%), pneumonia (12.7%), and other infection sites.Identific<strong>at</strong>ion: Local microbiology labor<strong>at</strong>ories in eachmedical center performed species identific<strong>at</strong>ions oncoryneform p<strong>at</strong>hogens as per local SOP criteria andmethods. Upon receipt <strong>at</strong> JMI Labor<strong>at</strong>ories (North Liberty,Iowa, USA) each strain was reviewed for colony morphologyand tested by Gram’s stain and Vitek or Vitek 2 using ANIcards for identific<strong>at</strong>ion, as necessary. Definitiveidentific<strong>at</strong>ion was assigned from testing on the BrukerBiotyper system using the MALDI-TOF methodology.Susceptibility testing: Antimicrobial susceptibility testing wasperformed by Clinical and Labor<strong>at</strong>ory Standards Institute(CLSI) broth microdilution methods in valid<strong>at</strong>ed, panelsmanufactured by Thermo Fisher Scientific (formerly TREKDiagnostics Systems; Cleveland, Ohio, USA). The testmedium was c<strong>at</strong>ion-adjusted Mueller-Hinton brothsupplemented with 2.5-5.0% lysed horse blood withincub<strong>at</strong>ion <strong>at</strong> 37 ºC for 24 hours. CLSI interpretive criteriawere used to c<strong>at</strong>egorize the isol<strong>at</strong>es as susceptible,intermedi<strong>at</strong>e and resistant as described in the M45document; European Committee on AntimicrobialSusceptibility Testing (<strong>EUCAST</strong>) has not yet definedinterpretive criteria. The quality control organismStreptococcus pneumoniae ATCC 49619 was concurrentlytested; all QC results were within published limits.Results• Among the collection of Corynebacterium strainsassembled, only 61 of the 121 strains (50.4%) wereidentified to the species level by the clinicalmicrobiology labor<strong>at</strong>ories due to local standardoper<strong>at</strong>ing procedures or by limited abilities of theautom<strong>at</strong>ed/biochemical identific<strong>at</strong>ion systems utilizedin the monitored European or USA medical centers.• Accuracy to species level among these identifiedisol<strong>at</strong>es as confirmed by the MALDI-TOF method was73.8% (45/61) agreement, 23.0% (14/61) had incorrectCorynebacterium species assigned and 3.3% (2/61)had an incorrect genus (Table 1).• Most common incorrect species identific<strong>at</strong>ionsobserved were C. jeikeium → C. amycol<strong>at</strong>um (5), C.xerosis → C. stri<strong>at</strong>um (3) and C. stri<strong>at</strong>um → C.amycol<strong>at</strong>um (2). Incorrect genus identific<strong>at</strong>ion wasobserved only twice; once each as C. afermentans →Brevibacterium casei and C. jeikeium →Staphylococcus warneri (Table 1).• Among the 60 unspeci<strong>at</strong>ed Corynebacterium strainsstudied, 51 (85.0%) demonstr<strong>at</strong>ed a good identific<strong>at</strong>ionto species level using the MALDI-TOF method, while 9strains (15.0%) were confirmed as other Gram-positivebacilli including; Brevibacterium (3), Microbacterium(3), Dermabacter, Rhodococcus and Turicella (oneeach, Table 1).• Gre<strong>at</strong>est in vitro potency against the collection (110Corynebacterium spp; Table 2) was observed withtigecycline (MIC 50/90 , ≤0.03/0.06 mg/L), daptomycin(MIC 50/90 , ≤0.06/0.25 mg/L), linezolid (MIC 50/90 ,0.25/0.25 mg/L) and vancomycin (MIC 50/90 , 0.25/0.5mg/L).• Based on CLSI M45 breakpoint criteria forCorynebacterium, highest resistance r<strong>at</strong>es wereobserved for ciprofloxacin (73.7%), followed bytrimethoprim/sulfamethoxazole (71.6%), erythromycin(65.5%) and ceftriaxone (63.6%; Table 2).• Analysis by sub-groups showed C. jeikeium and C.urealyticum species groups had reduced susceptibilityr<strong>at</strong>es for penicillin (0.0%) and gentamicin (36.8-40.0%)compared to other Corynebacterium spp. groups.Table 1. Summary of identific<strong>at</strong>ion (ID) discords between MALDI-TOF and other methods for Corynebacterium species isol<strong>at</strong>es from European andUSA medical centers between 2006-2010.Corynebacterium misidentific<strong>at</strong>ionsGenus misidentific<strong>at</strong>ionsSite ID MALDI-TOF ID (no.) Site ID MALDI-TOF ID (no.)C. jeikeium → C. afermentans C. afermentans → Brevibacterium caseiC. jeikeium → C. amycol<strong>at</strong>um (5) C. jeikeium → Staphylococcus warneriC. minutissimum → C. aurimucosum Unspeci<strong>at</strong>ed Corynebacterium → Brevibacterium casei (2)C. pseudodiptheriticum → C. propinquum Unspeci<strong>at</strong>ed Corynebacterium → Brevibacterium iodinumC. stri<strong>at</strong>um → C. amycol<strong>at</strong>um (2) Unspeci<strong>at</strong>ed Corynebacterium → Dermobacter hominisC. stri<strong>at</strong>um → C. aurimucosum Unspeci<strong>at</strong>ed Corynebacterium → Microbacterium maritypicumC. xerosis → C. stri<strong>at</strong>um (3) Unspeci<strong>at</strong>ed Corynebacterium → Microbacterium oxydansUnspeci<strong>at</strong>ed Corynebacterium → Microbacterium spp.Unspeci<strong>at</strong>ed Corynebacterium → Rhodococcus erythropolisUnspeci<strong>at</strong>ed Corynebacterium → Turicella otitidisTable 2. Activity of 13 antimicrobial agents when tested againstCorynebacterium species isol<strong>at</strong>es from European and USA medicalcenters between 2006-2010.Organism (no. tested)/MIC (mg/L)% susceptible /% resistantAntimicrobial agentMIC 50 MIC 90 CLSI aAll Corynebacterium spp. (110)Ceftriaxone 4 >8 26.4 / 63.6Ciprofloxacin >4 >4 20.9 / 73.7Clindamycin >2 >2 - b / -Daptomycin ≤0.06 0.25 99.1 / -Erythromycin >2 >2 24.6 / 65.5Gentamicin ≤2 >8 80.9 / 14.6Linezolid 0.25 0.25 100.0 / -Penicillin 1 >4 51.8 / 41.8Piperacillin/tazobactam 16 >64 - / -Tetracycline ≤2 >8 75.5 / 23.6Tigecycline ≤0.03 0.06 - / -Trimethoprim/sulfamethoxazole >2 >2 28.4 / 71.6Vancomycin 0.25 0.5 100.0 / -Corynebacterium amycol<strong>at</strong>um (33)Ceftriaxone 1 >8 57.6 / 30.3Ciprofloxacin >4 >4 15.2 / 75.8Clindamycin >2 >2 - / -Daptomycin ≤0.06 0.12 100.0 / -Erythromycin >2 >2 27.3 / 66.7Gentamicin ≤2 8 84.9 / 3.0Linezolid 0.12 0.25 100.0 / -Penicillin 1 >8 63.6 / 33.3Piperacillin/tazobactam ≤0.5 >64 - / -Tetracycline ≤2 ≤2 93.9 / 6.1Tigecycline ≤0.03 0.12 - / -Trimethoprim/sulfamethoxazole >2 >2 36.4 / 63.6Vancomycin 0.5 0.5 100.0 / -Corynebacterium jeikeium (19)Ceftriaxone >8 >8 0.0 / 100.0Ciprofloxacin >4 >4 10.5 / 89.5Clindamycin >2 >2 - / -Daptomycin 0.12 0.25 100.0 / -Erythromycin 2 >2 10.5 / 63.2Gentamicin >8 >8 36.8 / 63.2Linezolid 0.25 0.5 100.0 / -Penicillin >4 >4 0.0 / 94.8Piperacillin/tazobactam >64 >64 - / -Tetracycline ≤2 >8 84.2 / 15.8Tigecycline ≤0.03 0.06 - / -Trimethoprim/sulfamethoxazole >2 >2 0.0 / 100.0Vancomycin 0.5 0.5 100.0 / -Corynebacterium stri<strong>at</strong>um (37)Ceftriaxone 8 >8 0.0 / 94.6Ciprofloxacin >4 >4 8.1 / 83.8Clindamycin >2 >2 - / -Daptomycin ≤0.06 0.12 97.3 / -Erythromycin >2 >2 24.3 / 70.3Gentamicin ≤2 4 97.3 / 0.0Linezolid 0.25 0.25 100.0 / -Penicillin 1 >4 56.8 / 29.7Piperacillin/tazobactam 16 >64 - / -Tetracycline >8 >8 46.0 / 51.4Tigecycline ≤0.03 0.06 - / -Trimethoprim/sulfamethoxazole >2 >2 13.5 / 86.5Vancomycin 0.25 0.25 100.0 / -Corynebacterium urealyticum (5)Ceftriaxone 4 - 40.0 / 60.0Ciprofloxacin >4 - 0.0 / 100.0Clindamycin >2 - - / -Daptomycin ≤0.06 - 100.0 / -Erythromycin >2 - 40.0 / 60.0Gentamicin >8 - 40.0 / 60.0Linezolid 0.25 - 100.0 / -Penicillin >32 - 0.0 / 100.0Piperacillin/tazobactam >64 - - / -Tetracycline ≤2 - 100.0 / 0.0Tigecycline ≤0.03 - - / -Trimethoprim/sulfamethoxazole >2 - 0.0 / 100.0Vancomycin 0.5 - 100.0 / -Other Corynebacterium spp. (16) cCeftriaxone 1 4 50.0 / 18.8Ciprofloxacin ≤0.5 >4 81.3 / 27.8Clindamycin >2 >2 - / -Daptomycin ≤0.06 0.12 100.0 / -Erythromycin 2 >2 31.3 / 56.3Gentamicin ≤2 ≤2 100.0 / 0.0Linezolid 0.25 0.5 100.0 / -Penicillin 0.25 1 93.8 / 6.2Piperacillin/tazobactam 1 16 - / -Tetracycline ≤2 >8 87.5 / 12.5Tigecycline ≤0.03 0.06 - / -Trimethoprim/sulfamethoxazole 1 >2 87.5 / 12.5Vancomycin 0.25 0.25 100.0 / -a. Criteria as published by the FDA or CLSI [<strong>2012</strong>].b. "-" = No criteria defined.c. Includes Corynebacterium afermentans (3), C. aurimucosum (2), C. glucuronolyticum (1), C. initans (1), C.minutissimum (2), C. propinquum (3), C. pseudodiptheriticum (3), and C. singulare (1).Conclusions• Identific<strong>at</strong>ion of Corynebacterium to the species levelremains a challenge for clinical microbiologylabor<strong>at</strong>ories, due to the compromised accuracy of theautom<strong>at</strong>ed/biochemical systems in use. The MALDI-TOF method appears to gener<strong>at</strong>e more complete andaccur<strong>at</strong>e identific<strong>at</strong>ions to the species level.• This contemporary, well characterized collection ofCorynebacterium strains can be used to predicteffective empiric therapeutic choices and shows thehigher r<strong>at</strong>es of antimicrobial resistance for selectedagents among the C. jeikeium and C. urealyticumspecies groups.References1. Clinical and Labor<strong>at</strong>ory Standards Institute (<strong>2012</strong>). M07-A9.Methods for dilution antimicrobial susceptibility tests forbacteria th<strong>at</strong> grow aerobically; approved standard: ninthedition. Wayne, PA: CLSI.2. Clinical and Labor<strong>at</strong>ory Standards Institute (2010). M45-A2.Methods for antimicrobial dilution and disk susceptibilitytesting of infrequently isol<strong>at</strong>ed or fastidious bacteria:second edition. Wayne, PA: CLSI.3. Clinical and Labor<strong>at</strong>ory Standards Institute (<strong>2012</strong>). M100-S22. Performance standards for antimicrobial susceptibilitytesting: 22nd inform<strong>at</strong>ional supplement. Wayne, PA: CLSI.4. Funke G, Bernard KA (2011). Coryneform Gram-PositiveRods. In Manual of Clinical Microbiology. Washington, D.C.:ASM Press.5. Wolk DM, Dunne WM, Jr. (2011). New technologies inclinical microbiology. J Clin Microbiol 49: S62-S67.
European Committee on Antimicrobial Susceptibility Testing2011-<strong>2012</strong><strong>EUCAST</strong> General CommitteeAustralia - J TurnidgeAustria -P ApfalterBelgium - J VerhaegenBosnia - S Uzunovic-KamberovicBulgaria - K MetodievCro<strong>at</strong>ia - A Tambic-AndrasevicCzech Republic - H ZemlickovaDenmark -R SkovEstonia - M IvanovaFinland - A HakanenFrance - L DubreuilGermany - B WiedemannGreece - A V<strong>at</strong>opoulosHungary -ATóthIceland - K Gustaf KristinssonIreland - M MulhernIsrael - Y KenessItaly -P VaraldoL<strong>at</strong>via -A BalodeLithuania - J MiciulevicieneNetherlands –G KampingaNorway - M SteinbakkPoland -W HryniewiczPortugal - J Melo CristinoRomania -I coditaRussia - M SukhorukovaSerbia - L RaninSlovak Rep -M NiksSlovenia -J KolmanSpain - L Martinez MartinezSweden - B Olsson-LiljequistSwitzerland - J BilleTurkey - D GürUK - A MacGowanISC - P TulkensFESCI - D LivermorePharmaceutical Industry andSusceptibility Testing DeviceManufacturersThese groups are informed of <strong>EUCAST</strong>activity and consulted via an e-mailnetwork open to all companies with aninterest in antimicrobial susceptibilitytesting.The <strong>EUCAST</strong> steering committeeChairman Gunnar Kahlmeter (2014)Scientific secretary, Derek Brown(2014)Clinical D<strong>at</strong>a Coordin<strong>at</strong>or RafaelCanton (2014)BSAC (The UK), Alasdair MacGowan(2014)CA-SFM (France), Claude-JamesSoussy / Luc Dubreuil (2014)CRG (The Netherlands) Johan Mouton(2014)NWGA (Norway), Arnfinn Sundsfjord /Martin Steinbakk (2014)SRGA (Sweden), Christian Giske (2014)<strong>EUCAST</strong> rep 1, Petra Apfalter (Austria),(2013)<strong>EUCAST</strong> rep 2, Marina Ivanova(Estonia), (<strong>2012</strong>)Luis Martinez Martinez (Spain), (fromApril <strong>2012</strong>-2014)<strong>EUCAST</strong> rep 3, Robert Skov (Denmark),(From April <strong>2012</strong>-2014)Questions on <strong>EUCAST</strong>Website:www.eucast.orge-mail:gunnar.kahlmeter@escmid.orgderek.brown222@escmid.orgrcanton.hcr@escmid.orgAppointments by ESCMID- Chairholder, Scientific Secretary and Clinical D<strong>at</strong>aCoordin<strong>at</strong>or (3 years)- N<strong>at</strong>ional breakpoint committee se<strong>at</strong>s on the SteeringCommittee (3 years)- Three represent<strong>at</strong>ives from the <strong>EUCAST</strong> generalcommittee from countries not otherwise represented on thesteering committee (2 years).Appointments by European countries- Each country with an active n<strong>at</strong>ional breakpoint committeeappoints one represent<strong>at</strong>ive to serve for 3 years on theSteering Committee (active n<strong>at</strong>ional committees only, i.e.committees with >2 meetings per year, are eligible)- Countries without represent<strong>at</strong>ives on the SteeringCommittee may apply to the ESCMID board for a positionon the Steering Committee to serve for 2 years-- Each country appoints one represent<strong>at</strong>ive to serve on theGeneral Committee (no set term of office).<strong>EUCAST</strong> objectives<strong>EUCAST</strong> was set up to standardize susceptibility testing inEurope so th<strong>at</strong> comparable results and interpret<strong>at</strong>ions areproduced.<strong>EUCAST</strong> websitesThe <strong>EUCAST</strong> websites continue to be developed andupd<strong>at</strong>ed, and all <strong>EUCAST</strong> breakpoints and documents arefreely available from the website. Under “SusceptibilityTesting” a new section has been added on “Calibr<strong>at</strong>ionand Valid<strong>at</strong>ion” of the <strong>EUCAST</strong> disk diffusion method. Inaddition, there is a new section on “Projects and D<strong>at</strong>aSubmission” where labor<strong>at</strong>ories are invited to particip<strong>at</strong>e inspecific projects to develop methods.The <strong>EUCAST</strong> methodology and breakpoints for a diskdiffusion method are available on the <strong>EUCAST</strong> website andtechnical documents rel<strong>at</strong>ing to the method have recentlybeen upd<strong>at</strong>ed. The section on “Frequently askedquestions” about <strong>EUCAST</strong> breakpoints and methodscontinues to be expanded as questions are received.The “News” section on the website has been extended andusers can now subscribe to the <strong>EUCAST</strong> website RSSfeed. This means th<strong>at</strong> <strong>EUCAST</strong> news items can beautom<strong>at</strong>ically presented on other websites or in thebrowsers of individual computers.<strong>EUCAST</strong> public<strong>at</strong>ionsSee www.eucast.org.<strong>EUCAST</strong> expert rulesThe Expert Rules subcommittee (chairman RolandLeclercq) has upd<strong>at</strong>ed the <strong>EUCAST</strong> expert rules and thenew version 2.0 has been published in Clinical Microbiologyand Infection (Epub ahead of print, October 2011) and isavailable from the <strong>EUCAST</strong> website. Major modific<strong>at</strong>ionsinclude, among others, deletion of previous expert rules onextended spectrum β-lactamases and carbapenemasesand rewording of expert rules on quinolones with Salmonellaspp. and β-lactams with Haemophilus influenzae. Thebasisof all these modific<strong>at</strong>ions is explained in the public<strong>at</strong>ion. Thesubcommittee has achieved its objectives and has nowbeen disbanded.Antimicrobial resistance mechanismsA new subcommittee on antimicrobial resistancemechanisms of clinical and/or epidemiological importancehas recently been set up (chairman Christian Giske). Theremit is to develop practical guidelines for detection ofresistance mechanisms.<strong>EUCAST</strong> disk diffusion methodThe <strong>EUCAST</strong> disk diffusion method calibr<strong>at</strong>ed to <strong>EUCAST</strong> clinicalMIC breakpoints is now well established with methodology andbreakpoints (v 2.0) available on the <strong>EUCAST</strong> website. Breakpointsand the disk diffusion technique are being developed for severaladditional organisms such as Listeria monocytoenes, Pasteurellamultocida, Campylobacter spp. and Corynebacterium spp.The <strong>EUCAST</strong> MIC and zone diameter website presents MIC andzone diameter distributions of bacteria and fungi based on acontinually increasing number of distributions. Graphs showingMIC-zone diameter correl<strong>at</strong>ions also continue to be expanded. Thedistributions highlight wild type popul<strong>at</strong>ions and giveepidemiological cut-off values (ECOFFs).Antifungal breakpointsThe Antifungal Susceptibility Testing (AFST) subcommittee is astanding <strong>EUCAST</strong> subcommittee dealing with all issues rel<strong>at</strong>ed tobreakpoints and susceptibility testing for fungi. The AFST SteeringCommittee currently consists of Maiken C. Arendrup, (chairman),William Hope (secretary), Cornelia Lass-Floerl, and ManuelCuenca-Estrella. R<strong>at</strong>ionale documents and technical notes forCandida spp. with amphotericin, posaconazole and anidulafungin,and for Aspergillus spp. with amphotericin, itraconazole andposaconazole are now available from the <strong>EUCAST</strong> website. Arevised version of the <strong>EUCAST</strong> reference method for susceptibilitytesting of ferment<strong>at</strong>ive yeasts (EDEF 7.1) was recently posted onthe <strong>EUCAST</strong> website for consult<strong>at</strong>ion.<strong>EUCAST</strong> activities 2011-<strong>2012</strong>BreakpointsBreakpoint tables v 2.0 were published on the <strong>EUCAST</strong> website inDecember 2011. Breakpoints for various fastidious organisms arebeing developed in collabor<strong>at</strong>ion with relevant ESCMID studygroups and through this process breakpoints for Clostridiumdifficile, Helicobacter pylori and Listeria monocytogenes wereadded.Breakpoints for new agentsBreakpoints for new agents are set by <strong>EUCAST</strong> as part of thelicensing process through EMA. Breakpoints were set fortelavancin and several other agents are currently <strong>at</strong> various stagesof the licencing procedure.Revision of breakpointsSeveral breakpoints, including ceftibuten for Enterobacteriaceaeand Streptococcus pneumoniae, fosfomycin for Pseudomonasspp., vancomycin for coagulase-neg<strong>at</strong>ive staphylococci,nitrofurantoin for enterococci, phenoxymethylpenicillin andtrimethoprim for group B streptococci, and amoxicillin, amoxicillinclavulan<strong>at</strong>e,chloramphenicol and rifampicin for Haemophilusinfluenzae, have been revised in the light of new inform<strong>at</strong>ion.Implement<strong>at</strong>ion of breakpointsIn Europe, the trend from using other breakpoint guidelines tousing <strong>EUCAST</strong> breakpoints and methods continues. In the EARS-Net resistance surveillance external quality assessment exercisein May 2011, <strong>EUCAST</strong> breakpoints were used by around 50% ofparticip<strong>at</strong>ing labor<strong>at</strong>ories, compared with around 30% a yearearlier. Several more countries are in the process of changing orplan to change to <strong>EUCAST</strong> in the near future. The interest in<strong>EUCAST</strong> breakpoints from outside Europe is highlighted byAustralia joining the <strong>EUCAST</strong> General Committee.Autom<strong>at</strong>ed systemsThe manufacturers of autom<strong>at</strong>ed susceptibility testing devicescontinue to implement <strong>EUCAST</strong> breakpoints in their systems.Some outstanding issues are being dealt with <strong>at</strong> a considerablyslower pace than desirable. Up-to-d<strong>at</strong>e inform<strong>at</strong>ion on the current<strong>EUCAST</strong> st<strong>at</strong>us of manufacturers is given on the <strong>EUCAST</strong>website.<strong>EUCAST</strong> structure<strong>EUCAST</strong> is a standing ESCMIDcommittee, funded by ECDC, ESCMID,and particip<strong>at</strong>ing n<strong>at</strong>ional breakpointcommittees. It was formed in 1996 andrestructured <strong>at</strong> the <strong>ECCMID</strong> in Milan2002. It consists of a GeneralCommittee, with represent<strong>at</strong>ives from allEuropean countries, and is led by anESCMID-appointed Steering Committee,which includes a Chairman, ScientificSecretary, Clinical D<strong>at</strong>a Coordin<strong>at</strong>or, fiveN<strong>at</strong>ional Breakpoint Committeerepresent<strong>at</strong>ives and three represent<strong>at</strong>ivesof the <strong>EUCAST</strong> General Committee.Decisions are made by the SteeringCommittee after consult<strong>at</strong>ion with theGeneral Committee and expert groups.<strong>EUCAST</strong> General Committee meeting <strong>at</strong> <strong>ECCMID</strong> 2011