Palliative Care - Mount Sinai Hospital
Palliative Care - Mount Sinai Hospital
Palliative Care - Mount Sinai Hospital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Fall 2008<br />
<strong>Palliative</strong> <strong>Care</strong><br />
Lilian and Benjamin Hertzberg<br />
<strong>Palliative</strong> <strong>Care</strong> Institute<br />
Giving | PAGE 8 How Can We Improve <strong>Care</strong> | PAGE 1<br />
Massage Therapy | PAGE 6<br />
Brookdale Department of Geriatrics and Adult Development<br />
The <strong>Mount</strong> <strong>Sinai</strong> School of Medicine<br />
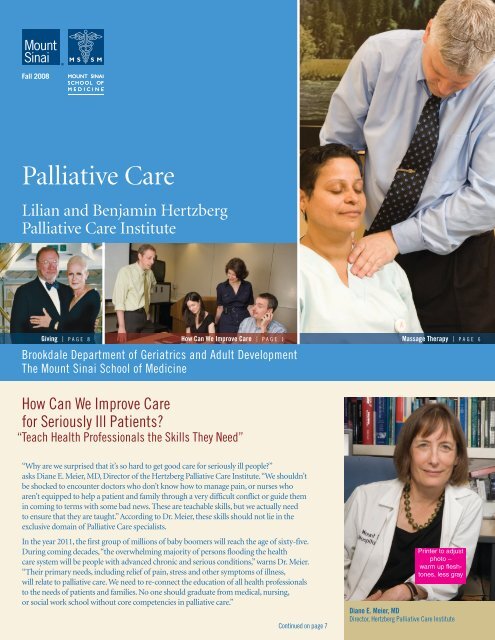
How Can We Improve <strong>Care</strong><br />
for Seriously Ill Patients?<br />
“ Teach Health Professionals the Skills They Need”<br />
“Why are we surprised that it’s so hard to get good care for seriously ill people?”<br />
asks Diane E. Meier, MD, Director of the Hertzberg <strong>Palliative</strong> <strong>Care</strong> Institute. “We shouldn’t<br />
be shocked to encounter doctors who don’t know how to manage pain, or nurses who<br />
aren’t equipped to help a patient and family through a very difficult conflict or guide them<br />
in coming to terms with some bad news. These are teachable skills, but we actually need<br />
to ensure that they are taught.” According to Dr. Meier, these skills should not lie in the<br />
exclusive domain of <strong>Palliative</strong> <strong>Care</strong> specialists.<br />
In the year 2011, the first group of millions of baby boomers will reach the age of sixty-five.<br />
During coming decades, “the overwhelming majority of persons flooding the health<br />
care system will be people with advanced chronic and serious conditions,” warns Dr. Meier.<br />
“Their primary needs, including relief of pain, stress and other symptoms of illness,<br />
will relate to palliative care. We need to re-connect the education of all health professionals<br />
to the needs of patients and families. No one should graduate from medical, nursing,<br />
or social work school without core competencies in palliative care.”<br />
Continued on page 7<br />
Printer to adjust<br />
photo –<br />
warm up fleshtones,<br />
less gray<br />
Diane E. Meier, MD<br />
Director, Hertzberg <strong>Palliative</strong> <strong>Care</strong> Institute
2<br />
Lilian and Benjamin Hertzberg<br />
<strong>Palliative</strong> <strong>Care</strong> Institute<br />
Brookdale Department of Geriatrics<br />
and Adult Development<br />
<strong>Mount</strong> <strong>Sinai</strong> School of Medicine<br />
One Gustave L. Levy Place, Box 1070, NY, NY 10029<br />
Tel. 212-241-1446<br />
www.mssm.edu/palliative<br />
Diane E. Meier, MD<br />
Director, Hertzberg <strong>Palliative</strong> <strong>Care</strong> Institute<br />
Director, Center to Advance <strong>Palliative</strong> <strong>Care</strong><br />
Catherine Gaisman Professor of Medical Ethics<br />
Professor, Departments of Geriatrics and Medicine<br />
Albert L. Siu, MD, MSPH<br />
Ellen and Howard C. Katz Chairman’s Chair<br />
Brookdale Department of Geriatrics<br />
and Adult Development<br />
<strong>Mount</strong> <strong>Sinai</strong> School of Medicine<br />
Director of the GRECC at the James J. Peters<br />
VA Medical Center<br />
R. Sean Morrison, MD<br />
Vice-Chair for Research<br />
Director, National <strong>Palliative</strong> <strong>Care</strong> Research Center<br />
Director of Research, Hertzberg <strong>Palliative</strong> <strong>Care</strong> Institute<br />
Hermann Merkin Professor of <strong>Palliative</strong> <strong>Care</strong><br />
Emily J. Chai, MD<br />
Medical Director<br />
Hertzberg <strong>Palliative</strong> <strong>Care</strong> Institute<br />
Assistant Professor, Brookdale Department<br />
of Geriatrics and Adult Development<br />
Gabrielle Goldberg, MD<br />
Education Director<br />
Hertzberg <strong>Palliative</strong> <strong>Care</strong> Institute<br />
Assistant Professor, Brookdale Department<br />
of Geriatrics and Adult Development<br />
Bette Kerr<br />
Writer and Editor<br />
Co-Editor: Susie West<br />
Photographers: Bruce Kushnick and Ana Blohm, MD<br />
Art Director: E.Fitz Art, Inc.<br />
The Hertzberg Philanthropic<br />
Leadership Council<br />
Peggy Danziger<br />
Joseph Hertzberg<br />
Walter W. Hess, Jr.<br />
Ellen Katz<br />
Ruth Madoff<br />
Diane E. Meier, MD<br />
Susan L. West<br />
Zena Wiener<br />
The Chaplaincy<br />
Another Way to Provide Comfort and Healing<br />
“In a hospital, people can easily lose their sense of identity,”<br />
observes Rabbi Edith Meyerson, Chaplain for the Hertzberg<br />
<strong>Palliative</strong> <strong>Care</strong> Institute. “Clad in hospital gowns, with only<br />
wrist name bands to identify them, patients can feel like<br />
prisoners in their beds. I’m here to remind them of who they are,<br />
to invite them to share their stories, their thinking, their lives.”<br />
Religion can play a major part in the healing process. “In pastoral<br />
care it’s important to meet people wherever they are,” explains<br />
Rabbi Meyerson. “Rather than asking someone to come into my<br />
boat, I board patients’ boats. They hold the oars and take me where<br />
Rabbi Edith Meyerson<br />
they want to go. My role as chaplain is to row with them as they<br />
share experiences of life, illness, faith, God, relationship – whatever they have on their<br />
minds and in their hearts. The simple yet deeply profound goal is to let them share<br />
their stories and feel heard.”<br />
When people are strongly connected to their faith, Rabbi Meyerson asks if they would<br />
like to talk with her about their beliefs. If they are affiliated with a particular house of<br />
worship, she offers to contact their clergy person. When there is a specific religious need<br />
that she can not fulfill, Rabbi Meyerson finds someone who can meet that need.<br />
A generous gift from<br />
Idee Schoenheimer and her<br />
husband Pierre, together<br />
“The simple yet deeply profound<br />
with a contribution from the<br />
Hebrew Union College, funded<br />
goal is to let patients share their<br />
the chaplaincy internship that<br />
stories and feel heard.”<br />
first brought Rabbi Meyerson<br />
to <strong>Palliative</strong> <strong>Care</strong>. “Healing<br />
– RABBI EDITH MEYERSON<br />
takes many forms,” reflects<br />
Mrs. Schoenheimer, adding,<br />
“There is a spiritual aspect<br />
to it. It doesn’t necessarily have<br />
to be God. During the crisis of serious illness we are vulnerable, we need someone to<br />
offer some grounding. The <strong>Palliative</strong> <strong>Care</strong> physicians do this so well. Why not offer<br />
them the assistance of a chaplain to augment their services?”<br />
Comfortable in a hospital setting, Rabbi Meyerson has found her niche in her new<br />
position. She reveals, “I was exposed early to the beautiful way my Dad, a cardiologist,<br />
practiced medicine, the way he related to his patients. I saw evidence of the spiritual<br />
gifts his patients gave to him, too.” In the <strong>Sinai</strong> <strong>Palliative</strong> <strong>Care</strong> team, Rabbi Meyerson<br />
sees a similar respect for patients’ humanity. In addition to patients and families,<br />
she provides support to clinicians and staff, allowing them to talk about personal issues<br />
and feelings that may emerge while they care for seriously ill people.<br />
To spend time with a family during a patient’s final hours is “a very holy experience,”<br />
says Rabbi Meyerson. “The family welcomes me on to sacred ground.” Officiating<br />
at a recent <strong>Palliative</strong> <strong>Care</strong> Memorial Service, she helped provide “an opportunity to<br />
think about ways to honor our loved ones, to remember the lives that touched us<br />
and to reflect on our own lives.”<br />
“Every day has been well spent if I know I’ve touched someone, if I’ve provided some<br />
sort of comfort or healing,” concludes Rabbi Meyerson.
A Growing Demand for <strong>Palliative</strong> <strong>Care</strong><br />
“Our Program began as a small consultative service,” says Dr. Emily<br />
Chai, Medical Director of Clinical Services in <strong>Palliative</strong> <strong>Care</strong>.<br />
“In 1998 we had one attending physician and one nurse. <strong>Hospital</strong><br />
physicians called on us mainly when their patients were near<br />
the end of life. We helped them alleviate symptoms and make<br />
patients comfortable. Today we are consulting and caring for<br />
seriously ill patients throughout the hospital, regardless of whether<br />
they will live for a week or for years. We help many people lead<br />
long, high-quality lives. Our staff has grown exponentially.”<br />
Now in its tenth anniversary year, the Hertzberg <strong>Palliative</strong> <strong>Care</strong><br />
Institute has two full-time clinical teams, both with physicians,<br />
nurse practitioners, and social workers. A massage therapist works<br />
with both teams. “We will soon be heading toward a third team,”<br />
adds Dr. Chai. “Meanwhile, we have to be creative to meet a<br />
steadily increasing need. We designated one team to see older<br />
adults and one for younger patients. Since we’re part of the<br />
Geriatrics Department, we can augment our coverage when<br />
Geriatrics physicians see <strong>Palliative</strong> <strong>Care</strong> patients. Most important,<br />
we can be even more patient-centered, determining which<br />
physicians are best equipped to serve patients’ specific needs.”<br />
Another move towards efficiency and better care involves<br />
the Fellows, young physicians pursuing specialized training<br />
in <strong>Palliative</strong> <strong>Care</strong>. On weekends, patients are given the Fellows’<br />
pager numbers and can obtain access to a physician around<br />
the clock. According to Dr. Chai, “This is tremendously<br />
reassuring for patients, and it’s a learning opportunity for<br />
Fellows, who can always call upon an attending physician<br />
if consultation is needed.”<br />
In only five years, the number of inpatients seen annually by<br />
the <strong>Palliative</strong> <strong>Care</strong> service has doubled from 619 in 2003 to 1138<br />
in 2007. “That’s without counting outpatients,” adds Dr. Chai.<br />
What is <strong>Palliative</strong> <strong>Care</strong> Anyway?<br />
“<strong>Palliative</strong> care (pronounced pal-lee-uh-tiv) specializes<br />
in the relief of the pain, symptoms, and stress of serious<br />
illness. <strong>Palliative</strong> care is appropriate at any point in an<br />
illness, and it can be provided at the same time as treatment<br />
that is meant to cure you.”<br />
Information on free resources for<br />
help in situations that may require<br />
palliative care can be found at:<br />
www.getpalliativecare.org<br />
Lilian and Benjamin Hertzberg <strong>Palliative</strong> <strong>Care</strong> Institute<br />
<strong>Palliative</strong> <strong>Care</strong> Clinical Team Meeting<br />
Carol Stangby, LCSW; Emily Chai, MD and Sue McHugh-Salera, NP<br />
“More and more, physicians throughout the <strong>Hospital</strong> realize<br />
they’re not equipped to treat all the symptoms of critically ill<br />
patients, and to hold the time-consuming, intense, in-depth<br />
conversations that we have with both patients and family.<br />
Education is a big part of our mission. We’re teaching both doctors<br />
and the general public to understand and value <strong>Palliative</strong> <strong>Care</strong>.”<br />
“We are consulting and caring for seriously<br />
ill patients throughout the hospital, regardless<br />
of whether they will live for a week or for years.”<br />
– EMILY CHAI, MD<br />
Under Dr. Chai’s leadership, a recent all-day retreat allowed faculty<br />
and staff to dedicate themselves to strategic planning, and, for<br />
the first time in a retreat, self-care. “We were able to focus a little<br />
more on ourselves than we do in regular clinical sessions where<br />
we talk about emotions that come up with specific patients.<br />
Increased awareness of our own feelings enables us to take better<br />
care of our patients,” reveals Dr. Chai, adding, “I so enjoy the<br />
interaction with my staff. Every single one is a highly skilled<br />
clinician and a team player. My patients – and the staff – draw me<br />
back and motivate me to do more each day.”<br />
According to Dr. Chai, the next big step forward is to create a<br />
<strong>Palliative</strong> <strong>Care</strong> Inpatient Unit. The <strong>Hospital</strong> has agreed to provide<br />
the raw space, but the Program has to raise money for everything<br />
else. “We want all nurses and floor staff to be trained in <strong>Palliative</strong><br />
<strong>Care</strong>,” says Dr. Chai. “ If we don’t have to teach them what to do,<br />
and we have a smaller patient to nursing ratio, we can spend<br />
more time taking better care of very sick patients in a state of the<br />
art facility.” Rooms will be private – with kitchenettes – and family<br />
members can stay overnight. “We envision an attractive, inviting,<br />
less institutional space. Finding funding and moving ahead with<br />
this is a huge challenge,” concludes Dr. Chai.<br />
3
4<br />
Medical Students’ Education:<br />
“ My Week in <strong>Palliative</strong> <strong>Care</strong> Reminded Me of Why I Entered Medical School.”<br />
“Only during my week on the <strong>Palliative</strong> <strong>Care</strong> service was I able to<br />
focus on patients in a way that I envisioned doing before coming<br />
to medical school,” reflects a third-year medical student.<br />
“Since 2006 we require all medical students to have a rather<br />
unique one-week rotation in <strong>Palliative</strong> <strong>Care</strong> as part of their<br />
12-week combined clerkship in Internal Medicine and Geriatrics,”<br />
explains Dr. Gabrielle Goldberg, Director of the <strong>Palliative</strong> <strong>Care</strong><br />
Education Center. “Our intention is not to make all students<br />
<strong>Palliative</strong> <strong>Care</strong> physicians, but to educate them to be better<br />
doctors – more compassionate, more aware of the wishes of<br />
patients and families.”<br />
The palliative care requirement for medical students involves<br />
collaboration among many individuals and groups. Dr. Reena<br />
Karani of Geriatrics and Dr. Peter Gliatto of Internal Medicine<br />
co-direct the 12-week clerkship. Professional and support<br />
staff are augmented via a gift from the <strong>Mount</strong> <strong>Sinai</strong> Auxiliary<br />
Board to fund the <strong>Palliative</strong> <strong>Care</strong> Education Center. According to<br />
Dr. David Muller, Dean of Medical Education, “We are one of only<br />
a handful of schools in the country to require this type of rotation<br />
and it is in keeping with the mission and tradition of <strong>Mount</strong> <strong>Sinai</strong>.<br />
Our educational program is focused on service, altruism, and<br />
the pivotal role of the physician in society. <strong>Palliative</strong> <strong>Care</strong> is one of<br />
the best expressions of those goals in the practice of medicine.”<br />
“It’s all about putting patients and their families<br />
first, focusing on their goals of care even<br />
when they aren’t necessarily ‘medical.’”<br />
– DAVID MULLER, MD<br />
During their rotation, students participate in interactive<br />
sessions on pain management and communication skills<br />
and review their learning goals with faculty members.<br />
Making rounds with the <strong>Palliative</strong> <strong>Care</strong> teams, students observe<br />
patient care as well as meetings with families. “They may<br />
take part of the patient history, talk to patients, do examinations,<br />
or collect laboratory data from the computer,” reveals Dr. Karani.<br />
In addition, she notes that “this is the only time in their medical<br />
school training that students are exposed to one of the most<br />
highly functioning teams in medical care. Students are always<br />
seeing patients throughout the hospital, but until this week<br />
they don’t get a sense of how people from different disciplines –<br />
medicine, social work, nursing, physical therapy – can really<br />
work together with complex patients.”<br />
Gabrielle Goldberg, MD, instructing Medical Student Deena Adimoolam<br />
Comments from different sectors about the<br />
<strong>Palliative</strong> <strong>Care</strong> rotation for medical students bear<br />
strikingly similar themes:<br />
Dr. Karani:<br />
“Since we have one of the best, most renowned programs<br />
in <strong>Palliative</strong> <strong>Care</strong> with an amazing team of providers,<br />
not exposing students to this until recently seemed like<br />
a glaring absence.”<br />
Dr. Goldberg:<br />
“It’s rejuvenating for all of us to work with the medical students<br />
and see them immediately appreciate the amount of time<br />
we spend with patients and families and our intense and<br />
compassionate focus.”<br />
Dean Muller:<br />
“It’s all about putting patients and their families first, focusing<br />
on their goals of care even when they aren’t necessarily ‘medical,’<br />
and the privilege of doing things beyond the call of duty for<br />
people at their most vulnerable. These are the most important<br />
messages we can send to our students.”<br />
Medical student:<br />
“My week helped me learn that palliative care is not a service<br />
to sign out to once I have exhausted medical interventions<br />
with a patient. Rather, it is one to partner with as I care for<br />
individuals with either chronic or terminal illnesses and<br />
try to help their families too. I am grateful to the palliative<br />
care team for not only teaching me these valuable lessons<br />
but also supporting me as I struggled with the difficult issues<br />
they confront daily.”
A Family Commitment to Philanthropy<br />
and a Fellowship in <strong>Palliative</strong> <strong>Care</strong><br />
Concern for the future of health care and a strong philanthropic<br />
spirit are hardly novel in the Leader family, where feelings are<br />
translated into actions by each generation. The Sidney D. and<br />
Ruby F. Leader Fellowship in <strong>Palliative</strong> Medicine, endowed this<br />
year, “is something my parents would have wanted us to do,”<br />
says Steven D. Leader. “It’s also a natural outgrowth of where<br />
Steve and I are right now,” adds his wife Barbara. “We’re teaching<br />
and mentoring, working on the new generation in so many<br />
aspects of our lives. Enabling advanced training for young<br />
palliative care physicians is a perfect fit.”<br />
“A <strong>Mount</strong> <strong>Sinai</strong> pediatrician, my dad was always focused on<br />
the humanity of medicine,” says Steven Leader. “He felt that<br />
some of that focus was lost in later years and he wanted to bring<br />
it back. Mom was trained as a speech teacher. Like her brothers,<br />
James and Irving Felt, she was committed to volunteerism,<br />
social issues, and giving back. James Felt was President of the<br />
Nursing College at <strong>Sinai</strong>, and he assembled much of the<br />
land on which <strong>Sinai</strong> built. I followed his career path as a real<br />
estate consultant.”<br />
When Ruby Felt Leader approached ninety with increasing<br />
visual limitations, she remained adamant about continuing<br />
her daily walks of a mile or two. “No taxis or buses for her,”<br />
says Steve. “But after a lifetime of independence and<br />
taking care of others, she became distressed at having to<br />
depend more on help for the tasks of daily life. Fortunately<br />
for all of us, Dr. Diane Meier was able to accept her as a<br />
geriatrics patient.”<br />
“We learned about palliative care through my mother-in-law’s<br />
relationship with Dr. Meier,” reflects Barbara Leader, a<br />
speech-language pathologist now on the faculty at New York<br />
Medical College and in private practice in Manhattan.<br />
The Leader Family:<br />
Two Generations of Philanthropy<br />
Ruby F. and Sidney D. Leader, left.<br />
Barbara and Steven Leader, right.<br />
Lilian and Benjamin Hertzberg <strong>Palliative</strong> <strong>Care</strong> Institute 5<br />
“Steve’s mother remained at home until the end of her life.<br />
She was fortunate to have a doctor who treated not only her<br />
physical symptoms but relieved some of the depression that<br />
came on with increased disability. Dr Meier talked to her,<br />
spent time with her, listened, placed value on what she said,<br />
never minimized her as an old lady talking. She cherished her<br />
and gave her the respect she was due for her 92 years.” Adds Steve,<br />
“When it became clear that Mom was near the end of her life,<br />
I was at peace with that because she was comfortable and taken<br />
care of so well. When Mom died in 2006, our family decided<br />
to make this gift in honor of both my parents.”<br />
“A <strong>Mount</strong> <strong>Sinai</strong> pediatrician, my dad was<br />
always focused on the humanity of medicine.”<br />
– STEVEN LEADER<br />
Experiencing what the palliative care approach encompasses,<br />
Barbara and Steven Leader found it “unbelievable” that<br />
“no component is overlooked. There’s even an element<br />
of spirituality.” According to Barbara, “Sure, there are<br />
practical things to provide – tests, medications, and more.<br />
But providing emotional support for the patient, while<br />
meeting the family’s needs too, distinguishes this program<br />
from other fields of medicine.”<br />
The Leaders want others to experience the type of care that<br />
Dr. Sidney Leader hoped would return to medical practice.<br />
By endowing the fellowship, “the fact that we might be able<br />
to influence the growth and expansion of palliative care<br />
is very satisfying,” states Barbara. During Ruby’s final weeks,<br />
she enjoyed sharing cross-generational perspectives with<br />
the fellows and medical students assigned to visit her at home.<br />
“What a great plan – to enable young medical students to<br />
learn from and become comfortable working with the elderly,’’<br />
adds Barbara.<br />
“We came away so impressed,” says Steve, after he, Barbara<br />
and their daughters Jaclyn and Allison recently met the<br />
current fellows. “This program is attracting young physicians<br />
of extraordinary talent.” Adds Barbara, “It makes us optimistic<br />
about the future. How far the field of medicine strayed from<br />
the days Steve’s dad made house calls and took payment in<br />
produce or chickens! Hopefully the circle is closing in the other<br />
direction. It’s a pleasure to affirm our confidence in the<br />
Hertzberg Institute’s success.”
6<br />
Massage Therapy: A Gentle Touch<br />
From left: JD Elder, LMT and Coordinator; Jean Blackman, LMT; Sandra Cherry, LMT; Molly Brooks, LMT; Fran Whelan, LMT; Sharon Houlihan,<br />
LMT; and Deborah Matza, RN and Yoga Coordinator. Volunteers not pictured: Jason Alcantara; Leela Southworth; Andrea Sandahl-Hart<br />
Brought to the Hertzberg Institute by a fortunate confluence of<br />
events, the Massage Therapy Program provides comfort and relief<br />
from stress not only to countless patients, but also to caregivers<br />
and hospital staff. “I had a long career in fitness and sports-related<br />
massage, but I always volunteered in other settings,” says JD Elder,<br />
a Licensed Massage Therapist who now heads the program.<br />
Eight years ago, officers of the Balm Foundation saw the Bill Moyers<br />
PBS television special “On Our Own Terms: A Different Kind<br />
of <strong>Care</strong>,” featuring the Hertzberg <strong>Palliative</strong> <strong>Care</strong> Institute. Aware<br />
of massage’s power as a therapeutic intervention for seriously ill<br />
patients, Balm Foundation officers contacted Hertzberg, offering<br />
funds to establish a massage therapy component, reveals Mr. Elder.<br />
“I was asked to become its Coordinator. The Balm Foundation continues<br />
to support us, allowing us to offer our services free of charge.”<br />
“We fully subscribe to the concept of treating<br />
the whole person, not just the illness.”<br />
– JD ELDER, LMT<br />
Augmented by a cadre of seven volunteers, the program has<br />
provided more than 5,500 massages since its inception. According to<br />
Mr. Elder, “For patients, our focus is comfort. Working with people<br />
who suffer from pain, shortness of breath, depression, agitation, or<br />
loneliness, we try to reduce physical and psychological stress. A calm<br />
environment is important. We make certain that the room is quiet.<br />
If patients wish, we play soft music or televised nature scenes.”<br />
Elaborating on why massage therapy and meditation techniques<br />
mesh perfectly with palliative medicine, Mr. Elder adds, “We fully<br />
subscribe to the concept of treating the whole person, not just the<br />
illness. We’re not only treating a heart surgery patient – but a person<br />
who might have a spouse, children, grandchildren, interests.<br />
JD Elder works with our patient, Mr. André<br />
Chervin at the Martha Stewart Center For Living<br />
We have a special fund set up by a donor to purchase magazines<br />
or provide hair styling and manicures. Amenities like these can<br />
improve a patient’s sense of well-being.”<br />
Extolling his volunteers, all Licensed Massage Therapists, JD Elder<br />
describes them as “keenly intelligent and sensitive, caring, loyal,<br />
and with varying specialties.” He coordinates their schedules and<br />
supervises them. “We train them in how to use massage therapy<br />
as a palliative measure, always employing a gentle touch. At the<br />
end of a session, they need to be sure that the call button, TV remote,<br />
tray and telephone are within the patient’s reach.”<br />
Several volunteers who provide massage therapy comment on<br />
their work:<br />
“I continue to learn so much from JD and the staff, as the training is<br />
ongoing. I know I make a difference – with patients, family members,<br />
and caregivers. I always leave with a smile on my face and memories<br />
in my heart.” Sandra Cherry<br />
“People have a view of massage as vigorous, but it can be adapted to<br />
meet all needs. The impact of the tender, compassionate touch we give<br />
to patients is amazing. Touch is an important part of life, especially<br />
for people who are at a crossroads. <strong>Care</strong>givers need to be touched, too.”<br />
Sharon Houlihan<br />
“In my early training, I was wrongly taught that massage therapists<br />
could work only on healthy people. Volunteering in palliative care is<br />
the best thing I have done for my professional and personal life. I’ve<br />
learned how profound the experience of a modified massage technique<br />
can be when it is provided with care and compassion.” Molly Brooks<br />
Gratified to head a program that has now been adapted by other<br />
hospitals and by the Visiting Nurse Service, JD Elder comments<br />
on his annual interdisciplinary workshop, where attendance<br />
has grown from 25 to 45 in only three years. “Funding from the<br />
Altman Foundation enabled us to develop this seminar, which is<br />
now supported by the Balm Foundation. We train Licensed Massage<br />
Therapists from all over so that they may branch out to work in<br />
hospital settings with seriously ill patients. They leave our workshop<br />
thinking very differently about massage therapy.”
Research Holds the Power to Improve <strong>Palliative</strong> <strong>Care</strong><br />
“To improve care for people with serious illness, we must do<br />
a far better job of equipping health care professionals with the<br />
knowledge base they need,” insists R. Sean Morrison, MD, Director<br />
of the National <strong>Palliative</strong> <strong>Care</strong> Research Center (NPCRC) which<br />
is housed at <strong>Mount</strong> <strong>Sinai</strong> School of Medicine. Focusing on pain<br />
and symptom management and better communication between<br />
clinicians and patients, NPCRC fosters research into new<br />
models and better delivery of palliative care.<br />
“To treat high blood pressure, I have eighty medications. For pain,<br />
a far more prevalent problem, I have only ten, all with side effects,”<br />
says Dr. Morrison, Hermann Merkin Professor of <strong>Palliative</strong> <strong>Care</strong><br />
and Professor of Geriatrics and Medicine. “We have a paucity<br />
of research that can guide doctors on treating shortness of breath<br />
or even fatigue, the most common and distressing symptom in<br />
people with advanced illness.”<br />
Continued funding from the Kornfeld and Olive Branch<br />
Foundations and major new investments from the Brookdale<br />
Foundation and Y.C. Ho /Helen and Michael Chiang Foundation<br />
have allowed the NPCRC to move forward in some major<br />
new initiatives including funding two additional junior faculty<br />
career development awards and a research consultancy program.<br />
Additionally, a recent multi-million dollar grant from the<br />
How Can We Improve <strong>Care</strong> for Seriously Ill Patients?<br />
Continued from page 1<br />
Dr. Diane Meier holds a family meeting with patient Mr. André Chervin<br />
and his partner Ms. Carola Vecchio<br />
Decrying medical education’s emphasis on machinery and technology,<br />
Dr. Meier is passionate about the need to focus on fundamental<br />
public health issues, preventive medicine, communication skills,<br />
and coordination of care across all settings. Medical and nursing<br />
students “need to spend less time memorizing and more time<br />
learning how to care for and communicate with patients,” she says.<br />
There is substantial progress. <strong>Palliative</strong> medicine has expanded<br />
greatly during the past 10 years, with 80% of teaching hospitals in<br />
the United States now reporting palliative care programs. Dr. Meier<br />
cautions: “That doesn’t necessarily mean that all the learners are<br />
getting exposure. It wasn’t until last year that our own <strong>Mount</strong> <strong>Sinai</strong><br />
medical students began a mandatory rotation in <strong>Palliative</strong> <strong>Care</strong>,<br />
despite our <strong>Palliative</strong> <strong>Care</strong> services having existed for 10 years.”<br />
Lilian and Benjamin Hertzberg <strong>Palliative</strong> <strong>Care</strong> Institute 7<br />
National Institute on Aging is enabling Dr.<br />
Morrison, in collaboration with Dr. Knox Todd<br />
of Beth Israel Medical Center, to seek ways to<br />
improve pain management in older adults.<br />
In April the NPCRC awarded its second series<br />
of annual grants. “We were overwhelmed and<br />
excited by the number of qualified applicants<br />
from across the country and thrilled to<br />
fund four junior and two senior investigators,”<br />
reports Dr. Morrison. Projects focus on<br />
R. Sean Morrison, MD<br />
research to improve communication about<br />
symptoms and goals of care among patients, their families, and<br />
doctors. Several center on outpatient palliative care models for<br />
people living in the community with cognitive impairment and pain.<br />
Asked about his drive to conduct and foster research and the<br />
extraordinary number of major grants he continues to receive,<br />
Dr. Morrison replies, “I want to reach the greatest number of<br />
people, to improve care at the highest level. The fact that <strong>Palliative</strong><br />
<strong>Care</strong> clinicians accomplish as much as they do is a testament to<br />
the innovative, committed people who enter this field. Think about<br />
the power they will have when we can supply the evidence base<br />
they need to treat symptoms far more effectively.”<br />
In April 2008 a New York State Council funded by the Legislature<br />
was created to advise the Health Commissioner on ways to improve<br />
training in pain management and palliative care. In a press release<br />
citing the need for the Council, on which Dr. Meier serves, Assembly<br />
Health Committee Chair Richard N. Gottfried stated that “many<br />
physicians do not have adequate or up-to-date education and<br />
training in palliative care and the diagnosis and treatment of pain.”<br />
Ten years ago the Textbook Project assembled teams of health<br />
professionals to scrutinize medical and nursing texts, exposing an<br />
appalling lack of palliative care content. Now, new editions of<br />
major texts in medicine, pediatrics, surgery, and nursing contain<br />
a significant amount of material related to palliative care.<br />
Another giant step forward took place in 2006, when palliative<br />
medicine was recognized as an official medical subspecialty –<br />
just like cardiology or pulmonary medicine. “That greatly legitimizes<br />
its role and presence in medical schools, both from the educational<br />
and research standpoint,” explains Dr. Meier.<br />
“When patients’ needs are not met,” concludes Dr. Meier, “it’s not<br />
usually because physicians or nurses are uncaring or indifferent.<br />
More often, they simply don’t know how to provide what’s needed.<br />
At <strong>Mount</strong> <strong>Sinai</strong> we are working to solve this problem by changing the<br />
way we educate our future doctors. As other institutions follow our<br />
lead and infuse palliative care content into the training of every health<br />
professional, we will see a difference in the way medicine is practiced.”
8<br />
Making Life Better by Giving<br />
Having experienced how much palliative care meant to her family,<br />
Zena Wiener, now an active Hertzberg Advisory Board member,<br />
approached Dr. Diane Meier and said: “I’d like to be in your<br />
army and follow you into battle.” “I saluted,” adds Mrs. Wiener,<br />
“and we started to laugh.” Thus began a collaborative relationship<br />
and a continuous outpouring of generosity. The most recent<br />
gift from the Wiener family – one million dollars over the<br />
next five years – will be used toward creating a palliative care<br />
inpatient unit in the <strong>Mount</strong> <strong>Sinai</strong> Medical Center.<br />
During both her father’s decline from Alzheimer’s disease and<br />
her sister-in-law’s serious illness, Mrs. Wiener learned that palliative<br />
medicine “is an inclusive discipline that connects family and<br />
patient. It provides incredible care and pain relief; it encompasses<br />
the needs of all members of the family.” She knows that for seriously<br />
ill hospital patients, a palliative care inpatient unit, with private<br />
rooms and an attractive physical environment, can offer optimal<br />
care and comfort.<br />
A dynamic and vibrant force, Mrs. Wiener seeks ways “to take away<br />
the strain of fundraising, to enable <strong>Palliative</strong> <strong>Care</strong> at <strong>Sinai</strong> to help as<br />
many people as possible.” Zena (“Zee”), a classically trained musician<br />
and former teacher, together with her husband Michael A.<br />
Wiener, a retired broadcasting entrepreneur and executive,<br />
have not only provided generous funding for Hertzberg year after<br />
year, but have also organized and sponsored fundraising events.<br />
Hertzberg Highlights<br />
Diane Meier, MD; Jane Brody and Susie West at<br />
the Douglas West Annual Endowed Lecture in<br />
<strong>Palliative</strong> <strong>Care</strong><br />
PHOTO CREDIT: ERIN GLEESON<br />
Kathy A. McMahon, President and CEO, HPCANYS,<br />
presents Susie West with the Ambassador of<br />
Hospice and <strong>Palliative</strong> <strong>Care</strong> Award<br />
Recognizing exceptional achievement in clinical research<br />
addressing health care problems of older adults, the<br />
American Geriatrics Association presented its Outstanding<br />
Scientific Achievement for Clinical Investigation Award to<br />
R. Sean Morrison, MD. This Award to an investigator involved<br />
in direct patient care was made May 2, 2008, at the Association’s<br />
Annual Meeting in Washington, D.C. Dr. Morrison addressed the<br />
group on the intersection of palliative care and geriatric medicine.<br />
These include a dinner to acquaint others<br />
with the efficacy of palliative care and its<br />
need for support.<br />
The Wieners rank among the strongest<br />
advocates for <strong>Mount</strong> <strong>Sinai</strong>, where Michael<br />
Wiener serves as a Trustee. Among their<br />
major gifts are an endowed chair in cancer,<br />
and funding to establish the Zena and<br />
Michael Wiener Cardiovascular Institute,<br />
Zena Wiener<br />
headed by Dr. Valentin Fuster. “We had the<br />
most devastating experience in 1996, suddenly and tragically losing<br />
our son Gabe,” reveals Mrs. Wiener. “I realized how random life can<br />
be. Living well while I’m here means doing what I can for others.”<br />
The Wieners and their daughter are committed to supporting many<br />
areas, with medicine and education as priorities. In honor of their<br />
son, a classical music producer, they endowed a music library at<br />
Columbia University and provided an organ to Central Synagogue.<br />
“If you can change only one thing, or one person, that person is a<br />
domino and changes another,’’ according to Mrs. Wiener, who<br />
has surely created a large corps of change agents. “If you have any<br />
money to give, give it well – to a place where it will do some good.”<br />
In “helping Dr. Meier and her palliative care program develop<br />
an army of recruits and enhanced facilities,” Zee Wiener knows<br />
she has found the right place.<br />
Speaking at <strong>Mount</strong> <strong>Sinai</strong> on May 6, 2008,<br />
New York Times personal health columnist<br />
Jane Brody delivered the Hertzberg Institute’s<br />
12th Annual Douglas West Lecture in<br />
Geriatrics and <strong>Palliative</strong> <strong>Care</strong>. Ms. Brody<br />
asked medical professionals to speak frankly<br />
with seriously ill patients and their families<br />
about quality of life and palliative and<br />
advance care planning. The lecture series was<br />
endowed by Susie West in memory of her husband<br />
Douglas.<br />
At its Annual Award Luncheon May 16, 2008,<br />
in Saratoga Springs, the Hospice and <strong>Palliative</strong><br />
<strong>Care</strong> Association of New York State honored<br />
Susie West with its Ambassador of Hospice and <strong>Palliative</strong> <strong>Care</strong><br />
Award. A letter informing Mrs. West of the Award stated: “The<br />
breadth and longevity of your experience as a volunteer is exceptional<br />
and your commitment to supporting the advancement of<br />
palliative care is truly admirable and deeply appreciated.” Mrs. West<br />
has been a full-time volunteer and generous supporter of the<br />
Hertzberg Institute for over ten years.


![December 2, 2012 [PDF] - Mount Sinai Hospital](https://img.yumpu.com/51092274/1/190x245/december-2-2012-pdf-mount-sinai-hospital.jpg?quality=85)
![January 21, 2013 [PDF] - Mount Sinai Hospital](https://img.yumpu.com/50916550/1/190x245/january-21-2013-pdf-mount-sinai-hospital.jpg?quality=85)
![February 3, 2013 [PDF] - Mount Sinai Hospital](https://img.yumpu.com/50584982/1/190x245/february-3-2013-pdf-mount-sinai-hospital.jpg?quality=85)
![March 18, 2012 [PDF] - Mount Sinai Hospital](https://img.yumpu.com/50462098/1/190x245/march-18-2012-pdf-mount-sinai-hospital.jpg?quality=85)


![Partners Program Guide [PDF] - Mount Sinai Hospital](https://img.yumpu.com/49411954/1/190x245/partners-program-guide-pdf-mount-sinai-hospital.jpg?quality=85)

![March 19 - April 1, 2012 [PDF] - Mount Sinai Hospital](https://img.yumpu.com/48990923/1/190x245/march-19-april-1-2012-pdf-mount-sinai-hospital.jpg?quality=85)
![PGY-1 Residency Application [PDF] - Mount Sinai Hospital](https://img.yumpu.com/48577701/1/190x245/pgy-1-residency-application-pdf-mount-sinai-hospital.jpg?quality=85)


