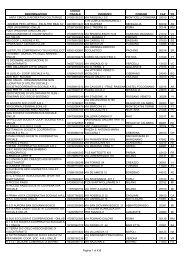
Ophthalmology Volume 118, Number 1, J<strong>an</strong>uary 2011c<strong>an</strong> result in loss of corneal endothelial cells, g<strong>as</strong>-inducedpupillary block, or a failure of a DM detachment <strong>to</strong> resolve.Pos<strong>to</strong>perative double <strong>an</strong>terior chamber, presumably alsorelated <strong>to</strong> operative perforations of DM, required a subsequen<strong>to</strong>perative intervention in 2.2% of c<strong>as</strong>es <strong>an</strong>d, when notsuccessful, w<strong>as</strong> the most common cause of delayed PKconversions in 0.4%. There were 5 (0.3%) repeat DALKprocedures. Donor lamellar graft recipient-bed interfacecomplications such <strong>as</strong> interface haze, DM wrinkling, <strong>an</strong>dinterface v<strong>as</strong>cularization were uncommon at 0.7%, 0.5%<strong>an</strong>d 0.5%, respectively. These complications are unique <strong>to</strong>DALK procedures, where<strong>as</strong> the remaining complicationsnoted in Table 3 (available at http://aaojournal.org) wereindividually less th<strong>an</strong> 0.5% <strong>an</strong>d could have occurred withPK or DALK.Of the 11 comparative studies, there w<strong>as</strong> no signific<strong>an</strong>tdifference in the pos<strong>to</strong>perative BSCVA between the DALK<strong>an</strong>d PK groups in 6 studies, 17,18,22,23,25,26 <strong>an</strong>d there w<strong>as</strong>better BSCVA in the DALK group in one study 27 <strong>an</strong>d betterBSCVA in the PK group in 4 studies. 19–21,24 The onestudy 27 reporting better pos<strong>to</strong>perative vision in the DALKgroup had the largest number of eyes in each group (150/150). Overall, there w<strong>as</strong> no signific<strong>an</strong>t difference betweenspherical refractive error or <strong>as</strong>tigmatism between the DALK<strong>an</strong>d PK groups.Twenty-seven of the additional 31 studies listed in Table2 (available at http://aaojournal.org) presented data aboutpos<strong>to</strong>perative visual acuity, refractive correction, <strong>an</strong>d <strong>as</strong>tigmatismof DALK eyes. There w<strong>as</strong> no signific<strong>an</strong>t differencein pos<strong>to</strong>perative visual acuity between DALK or PK eyes <strong>as</strong>a group, although there w<strong>as</strong> a tendency for lower visualacuity in DALK eyes in which DM w<strong>as</strong> not bared <strong>an</strong>dresidual stroma in the bed exceeded 10% of <strong>to</strong>tal stromalthickness.Immune-mediated donor-graft rejection c<strong>an</strong> be cl<strong>as</strong>sified<strong>as</strong> epithelial, stromal, endothelial, or some combination ofthese. Because corneal endothelium is not replaced inDALK, donor endothelial immune-medicated rejection c<strong>an</strong>no<strong>to</strong>ccur <strong>as</strong> it c<strong>an</strong> in PK. Stromal graft rejection c<strong>an</strong> alsooccur during the pos<strong>to</strong>perative period after DALK <strong>an</strong>d PK.There were 18 immune rejections recorded (1.0%) for the1843 DALK eyes reported in Table 2 (available at http://aaojournal.org). One study 28 reported 7 of 29 patients withDALK for kera<strong>to</strong>conus who had graft rejections, 2 of whomhad progressive v<strong>as</strong>cularization of the graft interface withopacification. One recent study, 29 not included in Table 2(available at http://aaojournal.org), of 129 consecutive eyesof 121 patients with DALK for kera<strong>to</strong>conus recorded 14 of129 episodes (10.9%) of subepithelial graft rejection <strong>an</strong>d 4of 129 episodes (3.1%) of stromal graft rejection, all successfullytreated with a 3- <strong>to</strong> 6-week course of <strong>to</strong>picalcorticosteroids. The majority of graft rejection episodes(n13) occurred in the first year after surgery <strong>an</strong>d in patientswith a his<strong>to</strong>ry of vernal kera<strong>to</strong>conjunctivitis (66.3%).Eighteen of the 129 eyes had a his<strong>to</strong>ry of vernal kera<strong>to</strong>conjunctivitisthat w<strong>as</strong> inactive at the time of surgery.Six of the 11 studies in the DALK/PK comparison group(Table 1; available at http://aaojournal.org) evaluated pos<strong>to</strong>perativeECD of the host corneal endothelium for theDALK groups <strong>an</strong>d of the donor graft endothelium for thePK groups. All demonstrated signific<strong>an</strong>tly higher ECD inthe DALK groups: at 12 months pos<strong>to</strong>peratively in 2 studies,17,20 at 24 months in one study, 18 at 3 years in onestudy, 25 <strong>an</strong>d at all intervals up <strong>to</strong> 5 years in the one study. 26The ECD data for the DALK/PK comparative studies highlightsignific<strong>an</strong>t differences between these surgical techniques(Table 1; available at http://aaojournal.org), withconsistently higher ECD in post-DALK eyes compared withpost-PK eyes.DiscussionThe adv<strong>an</strong>tages of DALK over PK surgery are <strong>as</strong> follows:● Immune rejection of the corneal endothelium c<strong>an</strong>no<strong>to</strong>ccur.● The procedure is extraocular <strong>an</strong>d not intraocular.● Topical corticosteroids c<strong>an</strong> usually be discontinuedearlier with DALK.● There is minor loss of ECD.● Compared with PK, DALK may have superior resist<strong>an</strong>ce<strong>to</strong> rupture of the globe after blunt trauma.● Sutures c<strong>an</strong> be removed earlier with DALK.The most obvious adv<strong>an</strong>tage of DALK is that the hostcorneal endothelium is not subject <strong>to</strong> immune rejection inDALK. Larger grafts approaching the limbus c<strong>an</strong> be usedwith DALK if the goal is complete removal of ectatic tissuein kera<strong>to</strong>conus. Normal-risk patients undergoing PK whoare phakic are generally tapered off of <strong>to</strong>pical corticosteroidsin 6 months, although continuing a daily <strong>to</strong>pical corticosteroiddrop for <strong>an</strong> additional 6 months provided additionalprotection against immunologic rejection in a large,prospective r<strong>an</strong>domized interventional trial of 406 eyes. 30However, this adv<strong>an</strong>tage of DALK over PK is not <strong>as</strong> great<strong>as</strong> one might expect, because immune rejection after PK forkera<strong>to</strong>conus is less likely <strong>an</strong>d kera<strong>to</strong>conus is the most commonindication for DALK. The major long-term adv<strong>an</strong>tageof DALK surgery over PK relates <strong>to</strong> long-term preservationof host corneal endothelial cells <strong>as</strong> me<strong>as</strong>ured by specularmicroscopy <strong>an</strong>d reported <strong>as</strong> ECD.Certain patients require PK, such <strong>as</strong> patients with kera<strong>to</strong>conuswho also have coexisting Fuchs’ endothelial dystrophy.Patients with corneal scarring from conditions such<strong>as</strong> herpes simplex virus, varicella zoster virus, microbialcorneal ulcers, or macular corneal dystrophy who have acompromised corneal endothelium should have PK surgery.However, in the presence of a relatively normal host cornealendothelium, not having <strong>to</strong> use long-term <strong>to</strong>pical, periocular,or systemic immunosuppressive agents <strong>to</strong> m<strong>an</strong>age thegraft is a definite adv<strong>an</strong>tage for DALK, especially if thepatient is a corticosteroid responder or is phakic.<strong>Deep</strong> <strong>an</strong>terior lamellar kera<strong>to</strong>pl<strong>as</strong>ty avoids the intraocular,open-sky segment of the PK procedure. Complications,including positive pressure, iris prolapse, <strong>an</strong>d choroidaleffusion/hemorrhage, are completely avoided with DALK.Tr<strong>an</strong>smission of bacterial infection from donor <strong>to</strong> recipientshould theoretically remain limited <strong>to</strong> keratitis rather th<strong>an</strong>endophthalmitis.212
Reinhart et al <strong>Deep</strong> <strong>Anterior</strong> <strong>Lamellar</strong> <strong>Kera<strong>to</strong>pl<strong>as</strong>ty</strong><strong>Deep</strong> <strong>an</strong>terior lamellar kera<strong>to</strong>pl<strong>as</strong>ty c<strong>an</strong> reduce ECD,especially if microperforations occur, <strong>an</strong>d even more so if<strong>an</strong>terior chamber injection of g<strong>as</strong> is required <strong>to</strong> m<strong>an</strong>age DMdetachments or double <strong>an</strong>terior chamber. 7,31–34 Corneal endotheliumc<strong>an</strong> be compromised by pupillary block <strong>an</strong>gleclosure after <strong>an</strong>terior chamber g<strong>as</strong> injection or by the airbubble itself. With recognition of these exceptions, continuedor accelerated loss of ECD after DALK surgery doesnot seem <strong>to</strong> occur after 6 months <strong>as</strong> it does post-PK.Endothelial cell density loss after the immediate pos<strong>to</strong>perativetime period is likely <strong>to</strong> mimic the gradual ECD decre<strong>as</strong>eof a normal cornea.Because <strong>to</strong>pical corticosteroids c<strong>an</strong> usually be discontinued3 <strong>to</strong> 4 months after DALK, there is a lower incidence ofcorticosteroid-<strong>as</strong>sociated intraocular pressure (IOP) elevation.With DALK, there is incre<strong>as</strong>ed wound strength comparedwith the PK wound, which is subjected <strong>to</strong> the prolongeduse of <strong>to</strong>pical corticosteroids <strong>to</strong> prevent immunerejection, <strong>an</strong>d there is decre<strong>as</strong>ed risk of cataract progression<strong>an</strong>d less compromised local ocular surface immunity.Traumatic rupture of PK wounds months <strong>to</strong> decades aftersurgery is a potential complication 35 that c<strong>an</strong> be cat<strong>as</strong>trophic.There is a theoretic adv<strong>an</strong>tage of DALK woundsover PK wounds, <strong>an</strong>d there are clinical reports of traumaticdehiscence of DALK wounds that suggest that the injuriesare less severe th<strong>an</strong> might have been expected of PK eyes. 36It is difficult <strong>to</strong> prove this <strong>as</strong>sertion at this time because ofthe smaller numbers <strong>an</strong>d shorter pos<strong>to</strong>perative follow-upavailable on DALK eyes. However, <strong>an</strong> incidence of globerupture of 1.8% (36/1962), of which 35 received PK (2.0%)<strong>an</strong>d one w<strong>as</strong> a DALK eye (0.5%), w<strong>as</strong> reported in a seriesof 1962 consecutive kera<strong>to</strong>pl<strong>as</strong>ties (PK, 1776 eyes; DALK,186 eyes) between 1998 <strong>an</strong>d 2006. 35Sutures c<strong>an</strong> be removed earlier on DALK eyes. Unlessperm<strong>an</strong>ent sutures are used, PK eyes do not have a stablerefraction until all sutures have been removed, which insome c<strong>as</strong>es may not occur until several years after surgery.Although early reports suggested that sutures could be removedin DALK eyes <strong>as</strong> early <strong>as</strong> 3 months pos<strong>to</strong>perativelybecause of the lower burden of corticosteroid use <strong>an</strong>d betterwound <strong>an</strong>a<strong>to</strong>my, 6 <strong>to</strong> 12 months seems more the norm.However, once sutures are removed, further refractive surgeryc<strong>an</strong> be performed earlier <strong>an</strong>d presumably with lessconcern of wound rupture in DALK eyes. One study suggeststhat <strong>as</strong>tigmatic kera<strong>to</strong><strong>to</strong>my incisions behave somewhatdifferently in DALK eyes th<strong>an</strong> in PK eyes. 37 <strong>Penetrating</strong>kera<strong>to</strong>pl<strong>as</strong>ty eyes often do not have a stable refraction foryears after surgery; wound strength is always of concernwhen performing refractive procedures such <strong>as</strong> LASIK becauseof the wound stressing effects of the IOP-incre<strong>as</strong>ingsuction ring required for surgery.The adv<strong>an</strong>tages of PK over DALK are <strong>as</strong> follows:● <strong>Penetrating</strong> kera<strong>to</strong>pl<strong>as</strong>ty c<strong>an</strong> be used <strong>to</strong> treat cornealconditions that involve the endothelium, such <strong>as</strong>Fuchs’ endothelial corneal dystrophy, pseudophakic<strong>an</strong>d aphakic corneal edema, posterior polymorphouscorneal dystrophy, <strong>an</strong>d congenital hereditary cornealendothelial dystrophies, although EK (DSEK orDSAEK) may now be preferred.● <strong>Penetrating</strong> kera<strong>to</strong>pl<strong>as</strong>ty c<strong>an</strong> treat penetrating cornealtrauma, especially if there is loss of corneal tissue.● <strong>Penetrating</strong> kera<strong>to</strong>pl<strong>as</strong>ty c<strong>an</strong> be used if there is scarringdown <strong>to</strong> the level of DM, such <strong>as</strong> postacutehydrops in kera<strong>to</strong>conus, old penetrating central cornealinjuries, <strong>an</strong>d severe postinfectious corneal ulcers. Inthe presence of <strong>an</strong> adequate ECD, the non-DM–baringDALK techniques may be used <strong>as</strong> <strong>an</strong> alternative <strong>to</strong> PK.● <strong>Penetrating</strong> kera<strong>to</strong>pl<strong>as</strong>ty c<strong>an</strong> be used if DM is notexposed in the visual axis, <strong>an</strong>d vision in those with PKmay be superior.● <strong>Penetrating</strong> kera<strong>to</strong>pl<strong>as</strong>ty is a more familiar operativeprocedure for most corneal surgeons.There are geographic <strong>an</strong>d social differences in the indicationsfor corneal surgery, but m<strong>an</strong>y corneal dise<strong>as</strong>es are<strong>as</strong>sociated with compromised corneal endothelium, whichme<strong>an</strong>s that PK, or EK, will account for most requests fordonor corneal tissue directed <strong>to</strong> <strong>an</strong>y given eye b<strong>an</strong>k. Also, inkera<strong>to</strong>conus eyes that have had previous hydrops, traumaticpenetrating injuries <strong>to</strong> the central cornea, or severe microbialinfections with residual scarring down <strong>to</strong> DM, thebig-bubble technique for DALK will not usually be successful.Other direct dissection DALK techniques, which leavesome residual cornea, c<strong>an</strong> be considered in these c<strong>as</strong>es,although final vision may not be <strong>as</strong> good <strong>as</strong> after PK. Ifcorneal hydrops complicating kera<strong>to</strong>conus h<strong>as</strong> occurred <strong>an</strong>dDALK without DM exposure is performed, pressuredependentstromal edema after surgery h<strong>as</strong> been describedthat cleared with IOP-lowering medication <strong>an</strong>d time. 38However, MD-DALK h<strong>as</strong> been reported for a patient with ahis<strong>to</strong>ry of hydrops-complicating kera<strong>to</strong>conus. 39 If DM isexposed in the visual axis, <strong>an</strong>d there are no DM folds in thevisual axis, then visual acuity is similar for DALK <strong>an</strong>d PK.If a signific<strong>an</strong>t amount of pre-Descemet’s stroma is left inthe recipient bed, then visual acuity in DALK eyes may becompromised. 19,22,26,32,40 In these c<strong>as</strong>es, removal of theDALK graft followed by excimer l<strong>as</strong>er pho<strong>to</strong>ablation or thebig-bubble technique <strong>to</strong> remove the remaining stromal tissue<strong>an</strong>d replacement of the DALK graft c<strong>an</strong> improve visualacuity 26,40 <strong>an</strong>d prevent the need for a subsequent PK.Alió 40 m<strong>an</strong>aged 4 eyes with poor vision after DALKusing the Melles technique, lifted the DALK donor graft <strong>as</strong>long <strong>as</strong> 2 years pos<strong>to</strong>peratively, <strong>an</strong>d exposed DM with abig-bubble technique, improving 6-month BSCVA <strong>to</strong> 20/25in 3 patients <strong>an</strong>d 20/32 in one patient. However, when DMc<strong>an</strong>not be exposed, or if there is signific<strong>an</strong>t scarring of thedeep corneal stroma, m<strong>an</strong>y surgeons may choose <strong>to</strong> use PK<strong>as</strong> the primary procedure.There is a definite learning curve for both PK <strong>an</strong>d DALKprocedures, although most corneal surgeons already possessthe acquired skills for PK surgery. The operative time forDALK is usually longer th<strong>an</strong> for PK, <strong>an</strong>d both proceduresrequire more operative time th<strong>an</strong> DSEK surgery because ofthe extensive suturing of the DALK or PK donor graft.The complications unique <strong>to</strong> DALK are <strong>as</strong> follows:● Ruptures of DM.● Large lamellar splits in DM.● Microperforations of DM.● Double <strong>an</strong>terior chamber.213