Stem Cells
single PDF file - Stem Cell Information - National Institutes of Health
single PDF file - Stem Cell Information - National Institutes of Health
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
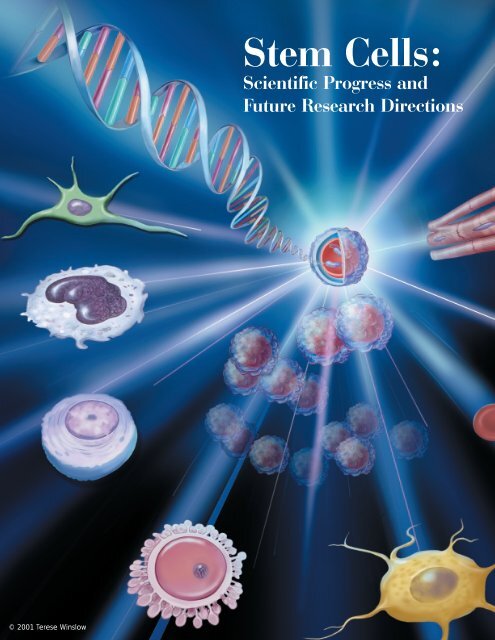
© 2001 Terese Winslow<strong>Stem</strong> <strong>Cells</strong>:Scientific Progress andFuture Research Directions
TABLE OF CONTENTSPreface . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . iExecutive Summary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . ES-1Chapter 1: The <strong>Stem</strong> Cell . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1Chapter 2: The Embryonic <strong>Stem</strong> Cell . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5Chapter 3: The Human Embryonic <strong>Stem</strong> Celland The Human Embryonic Germ Cell . . . . . . . . . . . . . . . . . . . . . . . . . 11Chapter 4: The Adult <strong>Stem</strong> Cell . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 23Chapter 5: Hematopoietic <strong>Stem</strong> <strong>Cells</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 43Chapter 6: Autoimmune Diseases and the Promiseof <strong>Stem</strong> Cell-Based Therapies . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 59Chapter 7: <strong>Stem</strong> <strong>Cells</strong> and Diabetes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 67Chapter 8: Rebuilding the Nervous System with <strong>Stem</strong> <strong>Cells</strong> . . . . . . . . . . . . . . . . . . . 77Chapter 9: Can <strong>Stem</strong> <strong>Cells</strong> Repair a Damaged Heart? . . . . . . . . . . . . . . . . . . . . . . 87Chapter 10: Assessing Human <strong>Stem</strong> Cell Safety . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 93Chapter 11: Use of Genetically Modified <strong>Stem</strong> <strong>Cells</strong> inExperimental Gene Therapies . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 99Appendix A: Early Development . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-1Appendix B: Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . B-1Appendix C: Human Embryonic <strong>Stem</strong> <strong>Cells</strong> and Embryonic Germ <strong>Cells</strong> . . . . . . . . . . C-1Appendix D: <strong>Stem</strong> Cell Tablesi. Published Reports on Isolation and Differentiation of Mouse<strong>Stem</strong> <strong>Cells</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . D-2ii. Published Reports on Isolation and Differentiation of HumanFetal Tissue Germ <strong>Cells</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . D-13iii. Published Reports on Isolation and Differentiation of HumanEmbryonic <strong>Stem</strong> <strong>Cells</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . D-14iv. Published Reports on Isolation and Differentiation of HumanEmbryonic Carcinoma <strong>Stem</strong> <strong>Cells</strong> . . . . . . . . . . . . . . . . . . . . . . . . . D-16v. Published Reports on Isolation and Differentiation of HumanAdult <strong>Stem</strong> <strong>Cells</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . D-18vi. References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . D-22
Appendix E: <strong>Stem</strong> Cell Markersi. Markers: How Do Researchers Use Them to Identify <strong>Stem</strong> <strong>Cells</strong>? . . . . . E-1ii. Commonly Used Markers to Identify <strong>Stem</strong> <strong>Cells</strong> andCharacterize Differentiated Cell Types . . . . . . . . . . . . . . . . . . . . . . . E-5Appendix F: Glossary and Termsi. Glossary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . F-1ii. Terms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . F-11Appendix G: Informational Resourcesi. Persons Interviewed . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . G-1ii. Special Contributions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . G-4iii. Acknowledgments . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . G-5
OPPORTUNITIES AND CHALLENGES:A FOCUS ON FUTURE STEM CELL APPLICATIONSBrainLungsHeartLiverCartilageBoneBloodvesselsPancreasKidneyThe makings of future news headlines abouttomorrow’s life saving therapies starts in thebiomedical research laboratory. Ideas abound; earlysuccesses and later failures and knowledge gainedfrom both; the rare lightning bolt of an unexpectedbreakthrough discovery — this is a glimpse of thebehind the scenes action of some of the world’smost acclaimed stem cell scientists’ quest to solvesome of the human body’s most challengingmysteries.<strong>Stem</strong> cells — what lies ahead? The following chaptersexplore some of the cutting edge research featuringstem cells. Disease and disorders with no therapies orat best, partially effective ones, are the lure of thepursuit of stem cell research. Described here areexamples of significant progress that is a prologue toan era of medical discovery of cell-based therapiesthat will one day restore function to those whose livesare now challenged every day — but perhaps in thefuture, no longer.Muscle
REPORT PREPARED BY THE NATIONAL INSTITUTES OF HEALTHRuth Kirschstein, M.D.Acting DirectorOffice of Science PolicyLana R. Skirboll, Ph.D.Director
PREFACEOn February 28, 2001, Tommy G. Thompson,Secretary of Health and Human Services, requestedthat the National Institutes of Health prepare asummary report on the state of the science on stemcells. This report was developed in response to hisrequest. It provides the current information about thebiology of stem cells derived from all sources—embryo, fetal tissue, and adult.Since 1998, when human pluripotent stem cells werefirst isolated, research on stem cells has receivedmuch public attention, both because of its extraordinarypromise and because of relevant legal andethical issues. Underlying this recent public scrutiny isdecades of painstaking work by scientists in manyfields, who have been deciphering some of the mostfundamental questions about life with the goal ofimproving health.In the last several decades, investments in basicresearch have yielded extensive knowledge aboutthe many and complex processes involved in thedevelopment of an organism, including the controlof cellular development. But many questions remain.How does a single cell—the fertilized egg—give riseto a complex, multi-cellular organism? The questionrepresents a fundamental challenge in developmentalbiology. Researchers are now seeking tounderstand in greater detail the genetic factors thatregulate cell differentiation in early development.Put simply, stem cells are self-renewing, unspecializedcells that can give rise to multiple types all ofspecialized cells of the body. The process by whichdividing, unspecialized cells are equipped to performspecific functions—muscle contraction or nervecell communication, for example—is called differentiation,and is fundamental to the development ofthe mature organism. It is now known that stem cells,in various forms, can be obtained from the embryo,the fetus, and the adult.How and whether stem cells derived from any ofthese sources can be manipulated to replace cellsin diseased tissues, used to screen drugs and toxins,or studied to better understand normal developmentdepends on knowing more about their basic properties.In this respect, stem cell research is in manyways no different than many other areas of modernbiology; it is advancing because new tools and newknowledge are providing the opportunities for newinsights. Like all fields of scientific inquiry, research onstem cells raises as many questions as it answers. Thisreport describes the state of the science of stem cellbiology and gives some clues as to the many andvaried questions that remain to be answered.WHAT IS THE SCOPE OF THEREPORT?The report is a review of the state of the science ofstem cell research as of June 17, 2001. Included inthis report is subject matter addressing stem cellsfrom adult, fetal tissue, and embryonic sources.Because so much of the progress made to date wasdependent on animal models, a significant emphasisis placed on understandings gained from mousemodels of development and mouse stem cellresearch. The report also devotes substantial attentionto scientific publications on the characterization ofspecialized cells developed from embryonic stemcells and the plasticity of adult stem cells. A generaloverview of early development is provided in theAppendix to assist the reader in understanding thekey events in formation of cells, tissues, and the wholeorganism.Both scientific and lay publications use a variety ofterms to describe stem cells and their properties. Forthis reason, this report adopts a lexicon of terms andit is used consistently throughout. To aid the reader, aglossary and terms section is provided. In severali
Prefaceplaces in the report, discovery timelines are provided.The various sources of stem cells are described, asare the techniques used to isolate and developthem. A comprehensive listing of various stem cellisolation and characterizations is also included.In order to ensure the reader is provided informationboth about the basic biology of stem cells, and theirtherapeutic potential, the report contains severalchapters focused on particular diseases which mightbenefit from stem cell research. These chapters onthe use of hematopoietic stem cells, followed byfocus features on specific nervous system diseases,diabetes, heart disease, and autoimmune diseasesserve merely as examples of the many applicationsof stem cells that are being pursued. Also includedare features that review aspects of stem cells astherapeutic delivery tools for gene therapy and,importantly, the safety considerations for developingstem cell-based therapies.WHAT IS NOT IN THE SCOPE OFTHE REPORT?NIH recognizes the compelling ethical and legalissues surrounding human pluripotent stem cellresearch. Because extensive discussions regardingthese issues have been presented in various forumselsewhere, they are not part of this review of the stateof the science. Also, the report does not makerecommendations pertaining to the policies governingFederal funding of such research.HOW WAS THE REPORTDEVELOPED?The report was prepared under the auspices of theOffice of Science Policy, Office of the Director, NIH.Several approaches were taken to obtain relevantscientific information for the report. A thorough reviewof the extant literature, including more than 1200scientific publications was conducted. Scientificexperts (both domestic and international) from allareas of relevant biomedical research in stem cellswere interviewed in depth. While the majority of thework presented in this report emanates frominvestigators in academic laboratories, extensivediscussions were held with scientists in the privatepharmaceutical and biotechnology sectors. Thus, thereport makes every effort to encompass what isknown and not known about stem cell biology and is,therefore, not limited to research that is or has beenfunded by the NIH.In recent months, there have been many reports inthe lay press regarding scientific discoveries onvarious types of stem cells. The science representedin this report focuses exclusively on scientificpublications or public presentations. In cases wheretechnical or logistical information key to the understandingof the details of science was needed,personal communications with the informationsources were cited.ii
EXECUTIVE SUMMARYINTRODUCTIONA stem cell is a special kind of cell that has a uniquecapacity to renew itself and to give rise to specializedcell types. Although most cells of the body, such asheart cells or skin cells, are committed to conduct aspecific function, a stem cell is uncommitted andremains uncommitted, until it receives a signal todevelop into a specialized cell. Their proliferativecapacity combined with the ability to become specializedmakes stem cells unique. Researchers havefor years looked for ways to use stem cells to replacecells and tissues that are damaged or diseased.Recently, stem cells have received much attention.What is “new” and what has brought stem cell biologyto the forefront of science and public policy?Scientists interested in human development havebeen studying animal development for many years.This research yielded our first glimpse at a class ofstem cells that can develop into any cell type in thebody. This class of stem cells is called pluripotent,meaning the cells have the potential to developalmost all of the more than 200 different known celltypes. <strong>Stem</strong> cells with this unique property come fromembryos and fetal tissue.In 1998, for the first time, investigators were able toisolate this class of pluripotent stem cell from earlyhuman embryos and grow them in culture. In the fewyears since this discovery, evidence has emerged thatthese stem cells are, indeed, capable of becomingalmost all of the specialized cells of the body and,thus, may have the potential to generate replacementcells for a broad array of tissues and organs,such as the heart, the pancreas, and the nervoussystem. Thus, this class of human stem cell holds thepromise of being able to repair or replace cells ortissues that are damaged or destroyed by many ofour most devastating diseases and disabilities.At about the same time as scientists were beginningto explore human pluripotent stem cells fromembryos and fetal tissue, a flurry of new informationwas emerging about a class of stem cells that havebeen in clinical use for years—so-called adult stemcells. An adult stem cell is an undifferentiated cellthat is found in a differentiated (specialized) tissue inthe adult, such as blood. It can yield the specializedcell types of the tissue from which it originated. In thebody, it too, can renew itself. During the past decade,scientists discovered adult stem cells in tissues thatwere previously not thought to contain them, such asthe brain. More recently, they reported that adultstem cells from one tissue appear to be capable ofdeveloping into cell types that are characteristic ofother tissues. For example, although adulthematopoietic stem cells from bone marrow havelong been recognized as capable of developing intoblood and immune cells, recently scientists reportedthat, under certain conditions, the same stem cellscould also develop into cells that have many of thecharacteristics of neurons. So, a new concept and anew term emerged-adult stem cell plasticity.Are human adult and embryonic stem cells equivalentin their potential for generating replacement cellsand tissues? Current science indicates that, althoughboth of these cell types hold enormous promise,adult and embryonic stem cells differ in importantways. What is not known is the extent to which thesedifferent cell types will be useful for the developmentof cell-based therapies to treat disease.Some considerations are noteworthy regarding thisreport. First, in recent months, there have been manydiscussions in the lay press about the anticipatedabilities of stem cells from various sources and projectedbenefits to be realized from them in replacingcells and tissues in patients with various diseases. Theterminology used to describe stem cells in the layES-1
Executive Summaryliterature is often confusing or misapplied. Second,even among biomedical researchers, there is a lackof consistency in common terms to describe whatstem cells are and how they behave in the researchlaboratory. Third, the field of stem cell biology isadvancing at an incredible pace with new discoveriesbeing reported in the scientific literature on aweekly basis.This summary begins with common definitions andexplanations of key concepts about stem cells. Itends with an assessment of how adult, embryonicand fetal stem cells are similar and how they are different.In between lie important details that describewhat researchers have discovered about stem cellsand how they are being used in the laboratory.DEFINITIONS AND GENERALCONCEPTS ABOUT STEM CELLSIn developing this report, some conventions wereestablished to describe consistently what stem cellsare, what characteristics they have, and how they areused in biomedical research. Here are some of thekey definitions that are used throughout this report.<strong>Stem</strong> cell. A stem cell is a cell from the embryo,fetus, or adult that has, under certain conditions, theability to reproduce itself for long periods or, in thecase of adult stem cells, throughout the life of theorganism. It also can give rise to specialized cells thatmake up the tissues and organs of the body. Muchbasic understanding about embryonic stem cells hascome from animal research. In the laboratory, thistype of stem cell can proliferate indefinitely, a propertythat is not shared by adult stem cells.Pluripotent stem cell. A single pluripotent stem cellhas the ability to give rise to types of cells that developfrom the three germ layers (mesoderm, endoderm,and ectoderm) from which all the cells of thebody arise. The only known sources of human pluripotentstem cells are those isolated and cultured fromearly human embryos and from fetal tissue that wasdestined to be part of the gonads.Embryonic stem cell. An embryonic stem cell isderived from a group of cells called the inner cellmass, which is part of the early (4- to 5-day) embryocalled the blastocyst. Once removed from the blastocyst,the cells of the inner cell mass can be culturedinto embryonic stem cells. These embryonic stemcells are not themselves embryos. In fact, evidence isemerging that these cells do not behave in the laboratoryas they would in the developing embryo—thatis, the conditions in which these cells develop in cultureare likely to differ from those in the developingembryo.Embryonic germ cell. An embryonic germ cell isderived from fetal tissue. Specifically, they are isolatedfrom the primordial germ cells of the gonadal ridgeof the 5- to 10-week fetus. Later in development, thegonadal ridge develops into the testes or ovaries andthe primordial germ cells give rise to eggs or sperm.Embryonic stem cells and embryonic germ cells arepluripotent, but they are not identical in their propertiesand characteristics.Differentiation. Differentiation is the process by whichan unspecialized cell (such as a stem cell) becomesspecialized into one of the many cells that make upthe body. During differentiation, certain genesbecome activated and other genes become inactivatedin an intricately regulated fashion. As a result, adifferentiated cell develops specific structures andperforms certain functions. For example, a mature,differentiated nerve cell has thin, fiber-like projectionsthat send and receive the electrochemical signalsthat permit the nerve cell to communicate with othernerve cells. In the laboratory, a stem cell can bemanipulated to become specialized or partiallyspecialized cell types (e.g., heart muscle, nerve, orpancreatic cells) and this is known as directeddifferentiation.Adult stem cell. An adult stem cell is an undifferentiated(unspecialized) cell that occurs in a differentiated(specialized) tissue, renews itself, and becomesspecialized to yield all of the specialized cell types ofthe tissue from which it originated. Adult stem cellsare capable of making identical copies of themselvesfor the lifetime of the organism. This property isreferred to as “self-renewal.” Adult stem cells usuallydivide to generate progenitor or precursor cells,which then differentiate or develop into “mature” celltypes that have characteristic shapes and specializedfunctions, e.g., muscle cell contraction or nervecell signaling. Sources of adult stem cells includebone marrow, blood, the cornea and the retina ofthe eye, brain, skeletal muscle, dental pulp, liver, skin,the lining of the gastrointestinal tract, and pancreas.The most abundant information about adult humanES-2
Executive Summarystem cells comes from studies of hematopoietic(blood-forming) stem cells isolated from the bonemarrow and blood. These adult stem cells have beenextensively studied and applied therapeutically forvarious diseases. At this point, there is no isolatedpopulation of adult stem cells that is capable offorming all the kinds of cells of the body. Adult stemcells are rare. Often they are difficult to identify, isolate,and purify. There are insufficient numbers of cellsavailable for transplantation and adult stem cells donot replicate indefinitely in culture.Plasticity. Plasticity is the ability of an adult stem cellfrom one tissue to generate the specialized celltype(s) of another tissue. A recently reported exampleof plasticity is that, under specific experimental conditions,adult stem cells from bone marrow generatedcells that resemble neurons and other cell types thatare commonly found in the brain. The concept ofadult stem cell plasticity is new, and the phenomenonis not thoroughly understood. Evidence suggeststhat, given the right environment, some adult stemcells are capable of being “genetically reprogrammed”to generate specialized cells that arecharacteristic of different tissues.Clonality or clonally derived stem cell. A cell is saidto be clonally derived or to exhibit clonality if it wasgenerated by the division of a single cell and isgenetically identical to that cell. In stem cellresearch, the concept of clonality is important forseveral reasons. For researchers to fully understandand harness the ability of stem cells to generatereplacement cells and tissues, the exact identity ofthose cells’ genetic capabilities and functional qualitiesmust be known. Human pluripotent stem cellsfrom embryos and fetal tissue are by their natureclonally derived. However, very few studies haveshown clonal properties of the cells that are developedfrom adult stem cells. It is crucial to knowwhether a single cell is capable of developing anarray of cell types, or whether multiple stem celltypes, that when grown together, are capable offorming multiple cell types. For instance, recentresearch has shown that a mixture of cells removedfrom fat tissue or umbilical cord blood are capableof developing into blood cells, bone cells, andperhaps others. Researchers have not shown that asingle cell is responsible for giving rise to other celltypes or, if so, what kind of cell it is. These results maywell be attributable to multiple types of precursor cellsin the starting tissue; such results from fat cells may, infact, be due to the presence of hematopoietic stemcells in the fat tissue. The importance of showing thatone cell type can reproducibly become another andself-replicate cannot be overemphasized.Progenitor or precursor cell. A progenitor or precursorcell occurs in fetal or adult tissues and is partiallyspecialized; it divides and gives rise to differentiatedcells. Researchers often distinguish precursor/progenitor cells from adult stem cells in the followingway: when a stem cell divides, one of the two newcells is often a stem cell capable of replicating itselfagain. In contrast, when a progenitor/precursor celldivides, it can form more progenitor/precursor cells orit can form two specialized cells, neither of which iscapable of replicating itself. Progenitor/precursor cellscan replace cells that are damaged or dead, thusmaintaining the integrity and functions of a tissuesuch as liver or brain. Progenitor/precursor cells giverise to related types of cells-lymphocytes such as Tcells, B cells, and natural killer cells, for example—butin their normal state do not generate a wide varietyof cell types.CHALLENGES IN STEM CELLRESEARCHIt is important to understand some of the difficultiesthat researchers have had in isolating various types ofstem cells, working with the cells in the laboratory,and proving experimentally that the cells are truestem cells. Most of the basic research discoveries onembryonic and adult stem cells come from researchusing animal models, particularly mice.In 1981, researchers reported methods for growingmouse embryonic stem cells in the laboratory, and ittook nearly 20 years before similar achievementscould be made with human embryonic stem cells.Much of the knowledge about embryonic stem cellshas emerged from two fields of research: appliedreproductive biology, i.e., in vitro fertilization technologies,and basic research on mouse embryology.There have been many technical challenges thathave been overcome in adult stem cell research aswell. Some of the barriers include: the rare occurrenceof adult stem cells among other, differentiatedcells, difficulties in isolating and identifying the cells(researchers often use molecular “markers” to identifyES-3
Executive Summaryadult stem cells), and in many cases, difficulties ingrowing adult stem cells in tissue culture. Much of theresearch demonstrating the plasticity of adult stemcells comes from studies of animal models in which amixture of adult stem cells from a donor animal isinjected into another animal, and the developmentof new, specialized cells is traced.In 1998, James Thomson at the University ofWisconsin-Madison isolated cells from the inner cellmass of the early embryo, called the blastocyst, anddeveloped the first human embryonic stem cell lines.At the same time, John Gearhart at Johns HopkinsUniversity reported the first derivation of humanembryonic germ cells from an isolated population ofcells in fetal gonadal tissue, known as the primordialgerm cells, which are destined to become the eggsand sperm. From both of these sources, theresearchers developed pluripotent stem cell “lines,”which are capable of renewing themselves for longperiods and giving rise to many types of human cellsor tissues. Human embryonic stem cells and embryonicgerm cells differ in some characteristics,however, and do not appear to be equivalent.Why are the long-term proliferation ability andpluripotency of embryonic stem cells and embryonicgerm cells so important? First, for basic researchpurposes, it is important to understand the geneticand molecular basis by which these cells continue tomake many copies of themselves overlong periodsof time. Second, if the cells are to be manipulatedand used for transplantation, it is important to havesufficient quantities of cells that can be directed todifferentiate into the desired cell type(s) and used totreat the many patients that may be suffering from aparticular disease.In recent months, other investigators have beensuccessful in using somewhat different approaches toderiving human pluripotent stem cells. At least 5 otherlaboratories have been successful in deriving pluripotentstem cells from human embryos and oneadditional laboratory has created cell lines from fetaltissue. In each case, the methods for deriving pluripotentstem cells from human embryos and embryonicgerm cells from fetal tissue are similar, yet theydiffer in the isolation and culture conditions as initiallydescribed by Thomson and Gearhart, respectively. Itis not known to what extent U.S.-based researchersare using these additional sources of embryonic stemand germ cells.At present, there have been multiple human adultstem cell lines that have been created through acombination of public and private resources (e.g.,hematopoietic stem cells). Substantial adult stem cellresearch has been underway for many years, and inrecent years this has included basic studies on the“plasticity” of such cells.WHAT KINDS OF RESEARCH MIGHTBE CONDUCTED WITH STEM CELLS?There has been much written about the newdiscoveries of various stem cell types and theirproperties. Importantly, these cells are research toolsand they open many doors of opportunity for biomedicalresearch.Transplantation Research—Restoring VitalBody Functions<strong>Stem</strong> cells may hold the key to replacing cells lost inmany devastating diseases. There is little doubt thatthis potential benefit underpins the vast interest aboutstem cell research. What are some of thesediseases? Parkinson’s disease, diabetes, chronic heartdisease, end-stage kidney disease, liver failure, andcancer are just a few for which stem cells have therapeuticpotential. For many diseases that shorten lives,there are no effective treatments but the goal is tofind a way to replace what natural processes havetaken away. For example, today, science has broughtus to a point where the immune response can besubdued, so that organs from one person can beused to replace the diseased organs and tissues ofanother. But, despite recent advances in transplantationsciences, there is a shortage of donor organsthat makes it unlikely that the growing demand forlifesaving organ replacements will be fully metthrough organ donation strategies.The use of stem cells to generate replacement tissuesfor treating neurological diseases is a major focus ofresearch. Spinal cord injury, multiple sclerosis, Parkinson’sdisease, and Alzheimer’s disease are amongthose diseases for which the concept of replacingdestroyed or dysfunctional cells in the brain or spinalcord is a practical goal. This report features severalrecent advances that demonstrate the regenerativeproperties of adult and embryonic stem cells.Another major discovery frontier for research on adultand embryonic stem cells is the development ofES-4
Executive Summarytransplantable pancreatic tissues that can be used totreat diabetes. Scientists in academic and industrialresearch are vigorously pursuing all possible avenuesof research, including ways to direct the specializationof adult and embryonic stem cells to becomepancreatic islet-like cells that produce insulin and canbe used to control blood glucose levels. Researchershave recently shown that human embryonic stemcells to be directly differentiated into cells that produceinsulin.There are common misconceptions about both adultand human embryonic stem cells. First, the lines ofunaltered human embryonic stem cells that exist willnot be suitable for direct use in patients. These cellswill need to be differentiated or otherwise modifiedbefore they can be used clinically. Current challengesare to direct the differentiation of embryonicstem cells into specialized cell populations, and alsoto devise ways to control their development or proliferationonce placed in patients.A second misconception is that adult stem cells areready to use as therapies. With the exception of theclinical application of hematopoietic stem cells torestore the blood and immune system, this is not thecase. The therapeutic use of this mixture of cells hasproven safe because the mixture is place back intothe environment from which it was taken, e.g., thebone marrow. In fact, many of the adult stem cellpreparations currently being developed in the laboratoryrepresent multiple cell types that are not fullycharacterized. In order to safely use stem cells or cellsdifferentiated from them in tissues other than the tissuefrom which they were isolated, researchers will needpurified populations (clonal lines) of adult stem cells.In addition, the potential for the recipient of a stemcell transplant to reject these tissues as foreign is veryhigh. Modifications to the cells, to the immune system,or both will be a major requirement for their use.In sum, with the exception of the current practice ofhematopoietic stem cell transplantation, much basicresearch lies ahead before direct patient applicationof stem cell therapies is realized.Basic Research ApplicationsEmbryonic stem cells will undoubtedly be keyresearch tools for understanding fundamental eventsin embryonic development that one day mayexplain the causes of birth defects and approachesto correct or prevent them. Another important area ofresearch that links developmental biology and stemcell biology is understanding the genes and molecules,such as growth factors and nutrients, thatfunction during the development of the embryo sothat they can be used to grow stem cells in thelaboratory and direct their development intospecialized cell types.Therapeutic Delivery Systems<strong>Stem</strong> cells are already being explored as a vehiclefor delivering genes to specific tissues in the body.<strong>Stem</strong> cell-based therapies are a major area of investigationin cancer research. For many years, restorationof blood and immune system function has beenused as a component in the care of cancer patientswho have been treated with chemotherapeuticagents. Now, researchers are trying to devise moreways to use specialized cells derived from stem cellsto target specific cancerous cells and directly delivertreatments that will destroy or modify them.Other Applications of <strong>Stem</strong> <strong>Cells</strong>Future uses of human pluripotent cell lines mightinclude the exploration of the effects of chromosomalabnormalities in early development. This mightinclude the ability to monitor the development ofearly childhood tumors, many of which are embryonicin origin. Another future use of human stem cellsand their derivatives include the testing of candidatetherapeutic drugs. Although animal model testing is amainstay of pharmaceutical research, it cannotalways predict the effects that a developmental drugmay have on human cells. <strong>Stem</strong> cells will likely beused to develop specialized liver cells to evaluatedrug detoxifying capabilities and represents a newtype of early warning system to prevent adverse reactionsin patients. The coupling of stem cells with theinformation learned from the human genome projectwill also likely have many unanticipated benefits inthe future.Critical Evidence and Questions about <strong>Stem</strong>Cell ResearchWhat is the evidence that specialized cells generatedfrom human stem cells can replace damaged ordiseased cells and tissues? Currently, there are morequestions than answers.Most of the evidence that stem cells can be directedto differentiate into specific types of cells suitable forES-5
Executive Summarytransplantation—for example, neurons, heart musclecells, or pancreatic islet cells—comes from experimentswith stem cells from mice. And although moreis known about mouse stem cells, not all of that informationcan be translated to the understanding ofhuman stem cells. Mouse and human cells differ insignificant ways, such as the laboratory conditionsthat favor the growth and specialization of specificcell types.Another important aspect of developing therapiesbased on stem cells will be devising ways to preventthe immune system of recipients from rejecting thedonated cells and tissues that are derived fromhuman pluripotent stem cells. Modifying or evadingthe immune rejection of cells or tissues developedfrom embryonic stem cells will not be able to bedone exclusively using mouse models and humanadult stem cells.As with any new research tool, it will also be importantto compare the techniques and approaches thatvarious laboratories are using to differentiate and usehuman embryonic stem cells. Such research will providea more complete understanding of the cells’characteristics. One key finding about the directeddifferentiation of pluripotent stem cells learned thusfar is that relatively subtle changes in culture conditionscan have dramatic influences on the types ofcells that develop.What Is Known About Adult <strong>Stem</strong> <strong>Cells</strong>?• To date, published scientific papers indicate thatadult stem cells have been identified in brain,bone marrow, peripheral blood, blood vessels,skeletal muscle, epithelia of the skin and digestivesystem, cornea, dental pulp of the tooth,retina, liver, and pancreas. Thus, adult stem cellshave been found in tissues that develop from allthree embryonic germ layers.• There is no evidence of an adult stem cell that ispluripotent. It has not been demonstrated thatone adult stem cell can be directed to developinto any cell type of the body. That is, no adultstem cell has been shown to be capable ofdeveloping into cells from all three embryonicgerm layers.• In the body, adult stem cells can proliferatewithout differentiating for a long period (the characteristicreferred to as long-term self-renewal),and they can give rise to mature cell types thathave characteristic shapes and specializedfunctions of a particular tissue.• Adult stem cells are rare. Often they are difficultto identify, isolate, and purify.• One important, limiting factor for the use of adultstem cells in future cell-replacement strategies isthat there are insufficient numbers of cellsavailable for transplantation. This is becausemost adult stem cell lines when grown in aculture dish are unable to proliferate in anunspecialized state for long periods of time. Incases where they can be grown under theseconditions, researchers have not been able todirect them to become specialized as functionallyuseful cells.• <strong>Stem</strong> cells from the bone marrow are the moststudiedtype of adult stem cells. Currently, theyare used clinically to restore various blood andimmune components to the bone marrow viatransplantation. There are two major types ofstem cells found in bone: hematopoietic stemcells which form blood and immune cells, andstromal (mesenchymal) stem cells that normallyform bone, cartilage, and fat. The restrictedcapacity of hematopoietic stem cells to grow inlarge numbers and remain undifferentiated inthe culture dish is a major limitation to theirbroader use for research and transplantationstudies. Researchers have reported that at leasttwo other populations of adult stem cells occurin bone marrow and blood, but these cells arenot well characterized.• Evidence to date indicates that umbilical cordblood is an abundant source of hematopoieticstem cells. There do not appear to be anyqualitative differences between the stem cellsobtained from umbilical cord blood and thoseobtained from bone marrow or peripheral blood.• Several populations of adult stem cells havebeen identified in the brain, particularly in aregion important in memory, known as the hippocampus.Their function in the brain is unknown.When the cells are removed from the brain ofmice and grown in tissue culture, their proliferationand differentiation can be influenced byvarious growth factors.ES-6
Executive Summary• Current methods for characterizing adult stemcells depend on determining cell-surfacemarkers and making observations about theirdifferentiation patterns in culture dishes.• Some adult stem cells appear to have thecapability to differentiate into tissues other thanthe ones from which they originated; this isreferred to as plasticity. Reports of human ormouse adult stem cells that demonstrate plasticityand the cells they differentiate or specializeinto include: 1) blood and bone marrow(unpurified hematopoietic) stem cells differentiateinto the 3 major types of brain cells (neurons,oligodendrocytes, and astrocytes), skeletalmuscle cells, cardiac muscle cells, and livercells; 2) bone marrow (stromal) cells differentiatesinto cardiac muscle cells, skeletal muscle cells,fat, bone, and cartilage; and 3) brain stem cellsdifferentiate into blood cells and skeletalmuscle cells.• Very few published research reports on theplasticity of adult stem cells shown that a single,identified adult stem cell can give rise to a differentiatedcell type of another tissue. That is, thereis limited evidence that a single adult stem cellor genetically identical line of adult stem cellsdemonstrates plasticity. Researchers believe thatit is most likely that a variety of populations ofstem cells may be responsible for the phenomenaof developing multiple cell types.• A few experiments have shown plasticity of adultstem cells by demonstrating the development ofmature, fully functional cells in tissues other thanwhich they were derived and the restoration oflost or diminished function in an animal model.What is Known About Human Pluripotent <strong>Stem</strong> <strong>Cells</strong>?• Since 1998, research teams have refined thetechniques for growing human pluripotent cells inculture systems. Collectively, the studies indicatethat it is now possible to grow these cells for upto two years in a chemically defined medium.• The cell lines have been shown to have anormal number of chromosomes and theygenerate cell types that originate from all threeprimary germ layers.• Cultures of human pluripotent stem cells haveactive telomerase, which is an enzyme thatmaintains the length of telomeres and isimportant for cells to maintain their capacity toreplicate. Human pluripotent stem cells appearto maintain relatively long telomeres, indicatingthat they have the ability to replicate for many,many generations.• Evidence of structural, genetic, and functionalcells characteristic of specialized cellsdeveloped from cultured human and mouseembryonic stem cells has been shown for:1) Pancreatic islet-cell like cells that secreteinsulin (mouse and human); 2) cardiac musclecells with contractile activity (mouse andhuman); 3) blood cells (human and mouse);4) nerve cells that produce certain brain chemicals(mouse).• At the time of this report, there are approximately30 cell lines of human pluripotent stem cells thathave been derived from human blastocysts orfetal tissue.• Overall, it appears human embryonic cells andembryonic germ cells are not equivalent in theirpotential to proliferate or differentiate.What are Some of the Questions that Need tobe Answered about <strong>Stem</strong> <strong>Cells</strong>?• What are the mechanisms that allow humanembryonic stem cells and embryonic germ cellsto proliferate in vitro without differentiating?• What are the intrinsic controls that keep stemcells from differentiating?• Is there a universal stem cell? That is, could akind of stem cell exist (possibly circulating in theblood) that can generate the cells of any organor tissue?• Do adult stem cells exhibit plasticity as a normalevent in the body or is it an artifact of the cultureconditions? If plasticity occurs normally, is it acharacteristic of all adult stem cells? What arethe signals that regulate the proliferation anddifferentiation of stem cells that demonstrateplasticity?• What are the factors responsible for stem cells to“home” to sites of injury or damage?• What are the intrinsic controls that direct stemcells along a particular differentiation pathway toform one specialized cell over another? How aresuch intrinsic regulators, in turn, influenced by theES-7
1.THE STEM CELLWHAT IS A STEM CELL?A stem cell is a cell that has the ability to divide (selfreplicate) for indefinite periods—often throughout thelife of the organism. Under the right conditions, orgiven the right signals, stem cells can give rise (differentiate)to the many different cell types that make upthe organism. That is, stem cells have the potential todevelop into mature cells that have characteristicshapes and specialized functions, such as heart cells,skin cells, or nerve cells.THE DIFFERENTIATION POTENTIALOF STEM CELLS: BASIC CONCEPTSAND DEFINITIONSMany of the terms used to define stem cells dependon the behavior of the cells in the intact organism(in vivo), under specific laboratory conditions (in vitro),or after transplantation in vivo, often to a tissue that isdifferent from the one from which the stem cellswere derived.For example, the fertilized egg is said to betotipotent—from the Latin totus, meaning entire—because it has the potential to generate all the cellsand tissues that make up an embryo and that supportits development in utero. The fertilized eggdivides and differentiates until it produces a matureorganism. Adult mammals, including humans, consistof more than 200 kinds of cells. These include nervecells (neurons), muscle cells (myocytes), skin (epithelial)cells, blood cells (erythrocytes, monocytes, lymphocytes,etc.), bone cells (osteocytes), and cartilagecells (chondrocytes). Other cells, which are essentialfor embryonic development but are not incorporatedinto the body of the embryo, include the extraembryonictissues, placenta, and umbilical cord. Allof these cells are generated from a single, totipotentcell—the zygote, or fertilized egg.Most scientists use the term pluripotent to describestem cells that can give rise to cells derived from allthree embryonic germ layers—mesoderm, endoderm,and ectoderm. These three germ layers arethe embryonic source of all cells of the body (seeFigure 1.1. Differentiation of Human Tissues). All of themany different kinds of specialized cells that make upthe body are derived from one of these germ layers(see Table 1.1. Embryonic Germ Layers From WhichDifferentiated Tissues Develop). “Pluri”—derived fromthe Latin plures—means several or many. Thus,pluripotent cells have the potential to give rise toany type of cell, a property observed in the naturalcourse of embryonic development and under certainlaboratory conditions.Unipotent stem cell, a term that is usually applied toa cell in adult organisms, means that the cells inquestion are capable of differentiating along onlyone lineage. “Uni” is derived from the Latin word unus,which means one. Also, it may be that the adult stemcells in many differentiated, undamaged tissues aretypically unipotent and give rise to just one cell typeunder normal conditions. This process would allow fora steady state of self-renewal for the tissue. However,if the tissue becomes damaged and the replacementof multiple cell types is required, pluripotent stem cellsmay become activated to repair the damage [2].The embryonic stem cell is defined by its origin—thatis from one of the earliest stages of the developmentof the embryo, called the blastocyst. Specifically,embryonic stem cells are derived from the inner cellmass of the blastocyst at a stage before it wouldimplant in the uterine wall. The embryonic stem cellcan self-replicate and is pluripotent—it can give riseto cells derived from all three germ layers.The adult stem cell is an undifferentiated (unspecialized)cell that is found in a differentiated (specialized)1
The <strong>Stem</strong> CellZygoteBlastocystEctoderm (external layer) Mesoderm (middle layer) Endoderm (internal layer) Germ cells© 2001 Terese Winslow, Caitlin DuckwallSkin cellsofepidermisNeuronof brainPigmentcellCardiacmuscleSkeletalmusclecellsTubule cellof thekidneyRedbloodcellsSmoothmuscle(in gut)PancreaticcellThyroidcellLung cell(alveolarcell)SpermEggFigure 1.1. Differentiation of Human Tissues.tissue; it can renew itself and become specialized toyield all of the specialized cell types of the tissue fromwhich it originated. Adult stem cells are capable ofself-renewal for the lifetime of the organism. Sourcesof adult stem cells have been found in the bonemarrow, blood stream, cornea and retina of the eye,the dental pulp of the tooth, liver, skin, gastrointestinaltract, and pancreas. Unlike embryonic stem cells, atthis point in time, there are no isolated adult stemcells that are capable of forming all cells of the body.That is, there is no evidence, at this time, of an adultstem cell that is pluripotent.2
The <strong>Stem</strong> CellTable 1.1. Embryonic Germ Layers From Which Differentiated Tissues DevelopEmbryonic Germ LayerEndodermMesodermEctodermDifferentiated TissueThymusThyroid, parathyroid glandsLarynx, trachea, lungUrinary bladder, vagina, urethraGastrointestinal (GI) organs (liver, pancreas)Lining of the GI tractLining of the respiratory tractBone marrow (blood)Adrenal cortexLymphatic tissueSkeletal, smooth, and cardiac muscleConnective tissues (including bone, cartilage)Urogenital systemHeart and blood vessels (vascular system)SkinNeural tissue (neuroectoderm)Adrenal medullaPituitary glandConnective tissue of the head and faceEyes, ears[1]REFERENCES1. Chandross, K.J. and Mezey, E. (2001). Plasticity of adultbone marrow stem cells. Mattson, M.P. and Van Zant, G.eds. (Greenwich, CT: JAI Press).2. Slack, J.M. (2000). <strong>Stem</strong> cells in epithelial tissues. Science.287, 1431-1433.3
The <strong>Stem</strong> CellThis page intentionally left blank4
2.THE EMBRYONICSTEM CELLAs stated in the first chapter, an embryonic stem cell(ES cell) is defined by its origin. It is derived from theblastocyst stage of the embryo. The blastocyst is thestage of embryonic development prior to implantationin the uterine wall. At this stage, the preimplantationembryo of the mouse is made up of 150 cellsand consists of a sphere made up of an outer layerof cells (the trophectoderm), a fluid-filled cavity(the blastocoel), and a cluster of cells on the interior(the inner cell mass).Studies of ES cells derived from mouse blastocystsbecame possible 20 years ago with the discovery oftechniques that allowed the cells to be grown in thelaboratory. Embryonic–like stem cells, called embryonicgerm (EG) cells, can also be derived fromprimordial germ (PG) cells (the cells of the developingfetus from which eggs and sperm are formed) of themouse [20] and human fetus [30].In this chapter the discussion will be limited to mouseembryonic stem cells. Chapter 3 describes thehuman embryonic stem cell.DO EMBRYONIC STEM CELLSACTUALLY OCCUR IN THE EMBRYO?Some scientists argue that ES cells do not occur inthe embryo as such. ES cells closely resemble thecells of the preimplantation embryo [3], but are not infact the same [32]. An alternative perspective is thatthe embryos of many animal species contain stemcells. These cells proliferate extensively in the embryo,are capable of differentiating into all the types ofcells that occur in the adult, and can be isolated andgrown ex vivo (outside the organism), where theycontinue to replicate and show the potential todifferentiate [18].For research purposes, the definition of an ES cell ismore than a self-replicating stem cell derived fromthe embryo that can differentiate into almost all ofthe cells of the body. Scientists have found it necessaryto develop specific criteria that help them betterdefine the ES cell. Austin Smith, whose studies ofmouse ES cells have contributed significantly to thefield, has offered a list of essential characteristics thatdefine ES cells [18, 32].DEFINING PROPERTIES OF ANEMBRYONIC STEM CELL• a Derived from the inner cell mass/epiblast of theblastocyst.• a Capable of undergoing an unlimited numberof symmetrical divisions without differentiating(long-term self-renewal).• Exhibit and maintain a stable, full (diploid), normalcomplement of chromosomes (karyotype).• Pluripotent ES cells can give rise to differentiatedcell types that are derived from all three primarygerm layers of the embryo (endoderm, mesoderm,and ectoderm).• a,b Capable of integrating into all fetal tissuesduring development. (Mouse ES cells maintainedin culture for long periods can still generate anytissue when they are reintroduced into anembryo to generate a chimeric animal.)• a,b Capable of colonizing the germ line andgiving rise to egg or sperm cells.• a Clonogenic, that is a single ES cell can giverise to a colony of genetically identical cells, orclones, which have the same properties as theoriginal cell.5
The Embryonic <strong>Stem</strong> Cell• Expresses the transcription factor Oct-4, whichthen activates or inhibits a host of target genesand maintains ES cells in a proliferative, nondifferentiatingstate.• Can be induced to continue proliferating or todifferentiate.• Lacks the G1 checkpoint in the cell cycle. EScells spend most of their time in the S phase ofthe cell cycle, during which they synthesize DNA.Unlike differentiated somatic cells, ES cells do notrequire any external stimulus to initiate DNAreplication.• Do not show X inactivation. In every somatic cellof a female mammal, one of the two X chromosomesbecomes permanently inactivated. Xinactivation does not occur in undifferentiatedES cells.[ a Not shown in human EG cells. b Not shown in human EScells. All of the criteria have been met by mouse ES cells.]ARE EMBRYONIC STEM CELLSTRULY PLURIPOTENT?Pluripotency—that is the ability to give rise to differentiatedcell types that are derived from all threeprimary germ layers of the embryo, endoderm,mesoderm, and ectoderm—is what makes ES cellsunique. How do we know that these cells are, indeed,pluripotent? Laboratory-based criteria for testing thepluripotent nature of ES cells derived from miceinclude three kinds of experiments [19]. One test isconducted by injecting ES cells derived from theinner cell mass of one blastocyst into the cavity ofanother blastocyst. The “combination” embryos arethen transferred to the uterus of a pseudopregnantfemale mouse, and the progeny that result arechimeras. Chimeras are a mixture of tissues andorgans of cells derived from both donor ES cells andthe recipient blastocyst.This test has been extended in studies designed totest whether cultured ES cells can be used to replacethe inner cell mass of a mouse blastocyst and producea normal embryo. They can, but the process isfar less efficient than that of using cells taken directlyfrom the inner cell mass. Apparently, the ability of EScells to generate a complete embryo depends onthe number of times they have been passagedin vitro [21, 22]. A passage is the process of removingcells from one culture dish and replating them intofresh culture dishes. Whether the number of passagesaffects the differentiation potential of human ES cellsremains to be determined. (For a detailed discussionof the techniques for maintaining mouse ES cells inculture, see Appendix B. Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>.)A second method for determining the pluripotency ofmouse ES cells is to inject the cells into adult mice(under the skin or the kidney capsule) that are eithergenetically identical or are immune-deficient, so thetissue will not be rejected. In the host animal, theinjected ES cells develop into benign tumors calledteratomas. When examined under a microscope, itwas noted that these tumors contain cell typesderived from all three primary germ layers of theembryo—endoderm, mesoderm, and ectoderm.Teratomas typically contain gut-like structures such aslayers of epithelial cells and smooth muscle; skeletalor cardiac muscle (which may contract spontaneously);neural tissue; cartilage or bone; and sometimeshair. Thus, ES cells that have been maintainedfor a long period in vitro can behave as pluripotentcells in vivo. They can participate in normal embryogenesisby differentiating into any cell type in thebody, and they can also differentiate into a widerange of cell types in an adult animal. However,normal mouse ES cells do not generate trophoblasttissues in vivo [32].A third technique for demonstrating pluripotency isto allow mouse ES cells in vitro to differentiate spontaneouslyor to direct their differentiation along specificpathways. The former is usually accomplished byremoving feeder layers and adding leukemia inhibitoryfactor (LIF) to the growth medium. Within a fewdays after changing the culture conditions, ES cellsaggregate and may form embryoid bodies (EBs).In many ways, EBs in the culture dish resembleteratomas that are observed in the animal. EBs consistof a disorganized array of differentiated or partiallydifferentiated cell types that are derived from thethree primary germ layers of the embryo—the endoderm,mesoderm, and ectoderm [32].The techniques for culturing mouse ES cells from theinner cell mass of the preimplantation blastocyst werefirst reported 20 years ago [9, 19], and versions ofthese standard procedures are used today inlaboratories throughout the world. It is striking that, todate, only three species of mammals have yielded6
The Embryonic <strong>Stem</strong> Celllong-term cultures of self-renewing ES cells: mice,monkeys, and humans [27, 34, 35, 36] (see AppendixB. Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>).HOW DOES A MOUSE EMBRYONICSTEM CELL STAY UNDIFFERENTIATED?As stated earlier, a true stem cell is capable of maintainingitself in a self-renewing, undifferentiated stateindefinitely. The undifferentiated state of the embryonicstem cell is characterized by specific cell markersthat have helped scientists better understand howembryonic stem cells—under the right culture conditions—replicatefor hundreds of population doublingsand do not differentiate. To date, two major areasof investigation have provided some clues. Oneincludes attempts to understand the effects ofsecreted factors such as the cytokine leukemiainhibitory factor on mouse ES cells in vitro. The secondarea of study involves transcription factors suchas Oct-4. Oct-4 is a protein expressed by mouse andhuman ES cells in vitro, and also by mouse inner cellmass cells in vivo. The cell cycle of the ES also seemsto play a role in preventing differentiation. From studiesof these various signaling pathways, it is clear thatmany factors must be balanced in a particular wayfor ES cells to remain in a self-renewing state. If thebalance shifts, ES cells begin to differentiate [18, 31].(For a detailed discussion of how embryonic stemcells maintain their pluripotency, see Appendix B.Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>.)CAN A MOUSE EMBRYONIC STEM CELLBE DIRECTED TO DIFFERENTIATEINTO A PARTICULAR CELL TYPEIN VITRO?One goal for embryonic stem cell research is thedevelopment of specialized cells such as neurons,heart muscle cells, endothelial cells of blood vessels,and insulin secreting cells similar to those found in thepancreas. The directed derivation of embryonic stemcells is then vital to the ultimate use of such cells inthe development of new therapies.By far the most common approach to directingdifferentiation is to change the growth conditions ofthe ES cells in specific ways, such as by addinggrowth factors to the culture medium or changingthe chemical composition of the surface on whichthe ES cells are growing. For example, the plasticculture dishes used to grow both mouse and humanES cells can be treated with a variety of substancesthat allow the cells either to adhere to the surface ofthe dish or to avoid adhering and instead float in theculture medium. In general, an adherent substratehelps prevent them from interacting and differentiating.In contrast, a nonadherent substrate allows the EScells to aggregate and thereby interact with eachother. Cell-cell interactions are critical to normalembryonic development, so allowing some of these“natural” in vivo interactions to occur in the culturedish is a fundamental strategy for inducing mouse orhuman ES cell differentiation in vitro. In addition,adding specific growth factors to the culture mediumtriggers the activation (or inactivation) of specificgenes in ES cells. This initiates a series of molecularevents that induces the cells to differentiate along aparticular pathway.Another way to direct differentiation of ES cells is tointroduce foreign genes into the cells via transfectionor other methods [6, 39]. The result of these strategiesis to add an active gene to the ES cell genome,which then triggers the cells to differentiate along aparticular pathway. The approach appears to be aprecise way of regulating ES cell differentiation, but itwill work only if it is possible to identify which genemust be active at which particular stage of differentiation.Then, the gene must be activated at theright time—meaning during the correct stage ofdifferentiation—and it must be inserted into thegenome at the proper location.Another approach to generate mouse ES cells usescloning technology. In theory, the nucleus of adifferentiated mouse somatic cell might be reprogrammedby injecting it into an oocyte. The resultantpluripotent cell would be immunologically compatiblebecause it would be genetically identical tothe donor cell [25].All of the techniques just described are still highlyexperimental. Nevertheless, within the past severalyears, it has become possible to generate specific,differentiated, functional cell types by manipulatingthe growth conditions of mouse ES cells in vitro. It isnot possible to explain how the directed differentiationoccurs, however. No one knows how or whengene expression is changed, what signal-transductionsystems are triggered, or what cell-cell interactions7
The Embryonic <strong>Stem</strong> Cell8. Doetschman, T., Eistetter, H., Katz, M., Schmit, W., andKemler, R. (1985). The in vitro development of blastocystderivedembryonic stem cell lines: formation of visceralyolk sac, blood islands and myocardium. J. Embryol. Exp.Morph. 87, 27-45.9. Evans, M.J. and Kaufman, M.H. (1981). Establishment inculture of pluripotential cells from mouse embryos. Nature.292, 154-156.10. Fairchild, P.J., Brook, F.A., Gardner, R.L., Graca, L., Strong, V.,Tone, Y., Tone, M., Nolan, K.F., and Waldmann, H. (2000).Directed differentiation of dendritic cells from mouseembryonic stem cells. Curr. Biol. 10, 1515-1518.11. Fraichard, A., Chassande, O., Bilbaut, G., Dehay, C.,Savatier, P., and Samarut, J. (1995). In vitro differentiationof embryonic stem cells into glial cells and functionalneurons. J. Cell Sci. 108, 3181-3188.12. Itskovitz-Eldor, J., Schuldiner, M., Karsenti, D., Eden, A.,Yanuka, O., Amit, M., Soreq, H., and Benvenisty, N. (2000).Differentiation of human embryonic stem cells into embryoidbodies comprising the three embryonic germ layers.Mol. Med. 6, 88-95.13. Kramer, J., Hegert, C., Guan, K., Wobus, A.M., Muller, P.K.,and Rohwedel, J. (2000). Embryonic stem cell-derivedchondrogenic differentiation in vitro: activation by BMP-2and BMP-4. Mech. Dev. 92, 193-205.14. Lee, S.H., Lumelsky, N., Studer, L., Auerbach, J.M., andMcKay, R.D. (2000). Efficient generation of midbrain andhindbrain neurons from mouse embryonic stem cells. Nat.Biotechnol. 18, 675-679.15. Liu, S., Qu, Y., Stewart, T.J., Howard, M.J., Chakrabortty, S.,Holekamp, T.F., and McDonald, J.W. (2000). Embryonicstem cells differentiate into oligodendrocytes and myelinatein culture and after spinal cord transplantation. Proc.Natl. Acad. Sci. U. S. A. 97, 6126-6131.16. Lumelsky, N., Blondel, O., Laeng, P., Velasco, I., Ravin, R.,and McKay, R. (2001). Differentiation of Embryonic <strong>Stem</strong><strong>Cells</strong> to Insulin-Secreting Structures Similiar to PancreaticIslets. Science. 292, 1389-1394.17. Maltsev, V.A., Rohwedel, J., Hescheler, J., and Wobus, A.M.(1993). Embryonic stem cells differentiate in vitro into cardiomyocytesrepresenting sinusnodal, atrial and ventricularcell types. Mech. Dev. 44, 41-50.18. Marshak, D.R., Gottlieb, D., Kiger, A.A., Fuller, M.T., Kunath, T.,Hogan, B., Gardner, R.L., Smith, A., Klar, A.J.S., Henrique, D.,D’Urso, G., Datta, S., Holliday, R., Astle, C.M., Chen, J.,Harrison, D.E., Xie, T., Spradling, A., Andrews, P.W., Przyborski,S.A., Thomson, J.A., Kunath, T., Strumpf, D., Rossant, J.,Tanaka, S., Orkin, S.H., Melchers, F., Rolink, A., Keller, G.,Pittenger, M.F., Marshak, D.R., Flake, A.W., Panicker, M.M.,Rao, M., Watt, F.M., Grompe, M., Finegold, M.J., Kritzik, M.R.,Sarvetnick, N., and Winton, D.J. (2001). <strong>Stem</strong> cell biology,Marshak, D.R., Gardner, R.L., and Gottlieb, D. eds. (ColdSpring Harbor, New York: Cold Spring Harbor LaboratoryPress).19. Martin, G.R. (1981). Isolation of a pluripotent cell line fromearly mouse embryos cultured in medium conditioned byteratocarcinoma stem cells. Proc. Natl. Acad. Sci. U. S. A.78, 7634-7638.20. Matsui, Y., Zsebo, K., and Hogan, B.L. (1992). Derivation ofpluripotential embryonic stem cells from murine primordialgerm cells in culture. Cell. 70, 841-847.21. Nagy, A., Gocza, E., Diaz, E.M., Prideaux, V.R., Ivanyi, E.,Markkula, M., and Rossant, J. (1990). Embryonic stem cellsalone are able to support fetal development in the mouse.Development. 110, 815-821.22. Nagy, A., Rossant, J., Nagy, R., Abramow-Newerly, W., andRoder, J.C. (1993). Derivation of completely cell culturederivedmice from early-passage embryonic stem cells.Proc. Natl. Acad. Sci. U. S. A. 90, 8424-8428.23. Nakano, T., Kodama, H., and Honjo, T. (1996). In vitrodevelopment of primitive and definitive erythrocytes fromdifferent precursors. Science. 272, 722-724.24. Nishikawa, S.I., Nishikawa, S., Hirashima, M., Matsuyoshi, N.,and Kodama, H. (1998). Progressive lineage analysis by cellsorting and culture identifies FLK1(+)VE-cadherin(+) cells ata diverging point of endothelial and hemopoietic lineages.Development. 125, 1747-1757.25. Odorico, J.S., Kaufman, D.S., and Thomson, J.A. (2001).Multilineage differentiation from human embryonic stemcell lines. <strong>Stem</strong> <strong>Cells</strong>. 19, 193-204.26. Potocnik, A.J., Nielsen, P.J., and Eichmann, K. (1994). In vitrogeneration of lymphoid precursors from embryonic stemcells. EMBO. J. 13, 5274-5283.27. Reubinoff, B.E., Pera, M.F., Fong, C.Y., Trounson, A., andBongso, A. (2000). Embryonic stem cell lines from humanblastocysts: somatic differentiation in vitro. Nat. Biotechnol.18, 399-404.28. Risau, W., Sariola, H., Zerwes, H.G., Sasse, J., Ekblom, P.,Kemler, R., and Doetschman, T. (1988). Vasculogenesis andangiogenesis in embryonic-stem-cell-derived embryoidbodies. Development. 102, 471-478.29. Rohwedel, J., Maltsev, V., Bober, E., Arnold, H.H., Hescheler,J., and Wobus, A.M. (1994). Muscle cell differentiation ofembryonic stem cells reflects myogenesis in vivo: developmentallyregulated expression of myogenic determinationgenes and functional expression of ionic currents. Dev. Biol.164, 87-101.30. Shamblott, M.J., Axelman, J., Wang, S., Bugg, E.M.,Littlefield, J.W., Donovan, P.J., Blumenthal, P.D., Huggins,G.R., and Gearhart, J.D. (1998). Derivation of pluripotentstem cells from cultured human primordial germ cells.Proc. Natl. Acad. Sci. U. S. A. 95, 13726-13731.31. Smith, A., personal communication.32. Smith, A.G. (2001). Origins and properties of mouseembryonic stem cells. Annu. Rev. Cell. Dev. Biol.9
The Embryonic <strong>Stem</strong> Cell33. Strubing, C., Ahnert-Hilger, G., Shan, J., Wiedenmann, B.,Hescheler, J., and Wobus, A.M. (1995). Differentiation ofpluripotent embryonic stem cells into the neuronal lineagein vitro gives rise to mature inhibitory and excitatoryneurons. Mech. Dev. 53, 275-287.34. Thomson, J.A., Kalishman, J., Golos, T.G., Durning, M., Harris,C.P., Becker, R.A., and Hearn, J.P. (1995). Isolation of a primateembryonic stem cell line. Proc. Natl. Acad. Sci. U. S.A. 92, 7844-7848.35. Thomson, J.A. and Marshall, V.S. (1998). Primate embryonicstem cells. Curr. Top. Dev. Biol. 38, 133-165.36. Thomson, J.A., Itskovitz-Eldor, J., Shapiro, S.S., Waknitz, M.A.,Swiergiel, J.J., Marshall, V.S., and Jones, J.M. (1998).Embryonic stem cell lines derived from human blastocysts.Science. 282, 1145-1147.38. Wiles, M.V. and Keller, G. (1991). Multiple hematopoieticlineages develop from embryonic stem (ES) cells in culture.Development. 111, 259-267.39. Wiles, M.V., Vauti, F., Otte, J., Fuchtbauer, E.M., Ruiz, P.,Fuchtbauer, A., Arnold, H.H., Lehrach, H., Metz, T., vonMelchner, H., and Wurst, W. (2000). Establishment of agene-trap sequence tag library to generate mutant micefrom embryonic stem cells. Nat. Genet. 24, 13-14.40. Yamashita, J., Itoh, H., Hirashima, M., Ogawa, M.,Nishikawa, S., Yurugi, T., Naito, M., Nakao, K., and Nishikawa,S. (2000). Flk1-positive cells derived from embryonic stemcells serve as vascular progenitors. Nature. 408, 92-96.37. Tsai, M., Wedemeyer, J., Ganiatsas, S., Tam, S.Y., Zon, L.I.,and Galli, S.J. (2000). In vivo immunological function ofmast cells derived from embryonic stem cells: anapproach for the rapid analysis of even embryonic lethalmutations in adult mice in vivo. Proc. Natl. Acad. Sci. U. S. A.97, 9186-9190.10
3. THE HUMAN EMBRYONIC STEM CELL ANDTHE HUMAN EMBRYONIC GERM CELLA new era in stem cell biology began in 1998 withthe derivation of cells from human blastocysts andfetal tissue with the unique ability of differentiatinginto cells of all tissues in the body, i.e., the cells arepluripotent. Since then, several research teams havecharacterized many of the molecular characteristicsof these cells and improved the methods for culturingthem. In addition, scientists are just beginning to directthe differentiation of the human pluripotent stemcells and to identify the functional capabilities of theresulting specialized cells. Although in its earliest phases,research with these cells is proving to be importantto developing innovative cell replacementstrategies to rebuild tissues and restore criticalfunctions of the diseased or damaged human body.OVERVIEWIn 1998, James Thomson and his colleagues reportedmethods for deriving and maintaining humanembryonic stem (ES) cells from the inner cell massof human blastocysts that were produced throughin vitro fertilization (IVF) and donated for researchpurposes [46]. At the same time, another group, ledby John Gearhart, reported the derivation of cellsthat they identified as embryonic germ (EG) cells.The cells were cultured from primordial germ cellsobtained from the gonadal ridge and mesenchymaof 5- to 9-week fetal tissue that resulted fromelective abortions [41].The two research teams developed their methodsfor culturing human ES and EG cells by drawing ona host of animal studies, some of which date backalmost 40 years: derivations of pluripotent mouseES cells from blastocysts [13, 15], reports of thederivation of EG cells [27, 36], experiments withstem cells derived from mouse teratocarcinomas[24] and human embryonal carcinomas andteratocarcinomas [4, 17, 24], the derivation andculture of ES cells from the blastocysts of rhesus monkeys[46] and marmosets [47], and methods used byIVF clinics to prepare human embryos for transplantinginto the uterus to produce a live birth [11, 49].TIMELINE OF HUMAN EMBRYONICSTEM CELL RESEARCH• 1878: First reported attempts to fertilizemammalian eggs outside the body [49].• 1959: First report of animals (rabbits) producedthrough IVF in the United States [49].• 1960s: Studies of teratocarcinomas in the testesof several inbred strains of mice indicates theyoriginated from embryonic germ cells. The workestablishes embryonal carcinoma (EC) cells as akind of stem cell [17, 24]. For a more detaileddiscussion of human embryonal carcinomacells, see Appendix C.• 1968: Edwards and Bavister fertilize the firsthuman egg in vitro [49].• 1970s: EC cells injected into mouse blastocystsproduce chimeric mice. Cultured SC cells areexplored as models of embryonic development,although their complement of chromosomes isabnormal [25].• 1978: Louise Brown, the first IVF baby, is born inEngland [49].• 1980: Australia’s first IVF baby, Candace Reed, isborn in Melbourne [49].• 1981: Evans and Kaufman, and Martin derivemouse embryonic stem (ES) cells from the innercell mass of blastocysts. They establish cultureconditions for growing pluripotent mouse ES cellsin vitro. The ES cells yield cell lines with normal,diploid karyotyes and generate derivatives of allthree primary germ layers as well as primordial11
The Human Embryonic <strong>Stem</strong> Cell and The Human Embryonic Germ Cellgerm cells. Injecting the ES cells into miceinduces the formation of teratomas [15, 26].The first IVF baby, Elizabeth Carr, is born in theUnited States [49].• 1984-88: Andrews et al., develop pluripotent,genetically identical (clonal) cells called embryonalcarcinoma (EC) cells from Tera-2, a cell lineof human testicular teratocarcinoma [5]. Clonedhuman teratoma cells exposed to retinoic aciddifferentiate into neuron-like cells and other celltypes [3, 44].• 1989: Pera et al., derive a clonal line of humanembryonal carcinoma cells, which yields tissuesfrom all three primary germ layers. The cells areaneuploid (fewer or greater than the normalnumber of chromosomes in the cell) and theirpotential to differentiate spontaneously in vitrois typically limited. The behavior of human ECcell clones differs from that of mouse ES orEC cells [33].• 1994: Human blastocysts created forreproductive purposes using IVF and donatedby patients for research, are generated from the2-pronuclear stage. The inner cell mass of theblastocyst is maintained in culture and generatesaggregates with trophoblast-like cells at theperiphery and ES-like cells in the center. The cellsretain a complete set of chromosomes (normalkaryotype); most cultures retain a stem cell-likemorphology, although some inner cell massclumps differentiate into fibroblasts. The culturesare maintained for two passages [6, 7].• 1995-96: Non-human primate ES cells arederived and maintained in vitro, first from theinner cell mass of rhesus monkeys [46], and thenfrom marmosets [47]. The primate ES cells arediploid and have normal karyotypes. They arepluripotent and differentiate into cells typesderived from all three primary germ layers. Theprimate ES cells resemble human EC cells andindicate that it should be possible to derive andmaintain human ES cells in vitro.• 1998: Thomson et al., derive human ES cellsfrom the inner cell mass of normal humanblastocysts donated by couples undergoingtreatment for infertility. The cells are culturedthrough many passages, retain their normalkaryotypes, maintain high levels of telomeraseactivity, and express a panel of markers typicalof human EC cells non-human primate ES cells.Several (non-clonal) cell lines are establishedthat form teratomas when injected intoimmune-deficient mice. The teratomas includecell types derived from all three primary germlayers, demonstrating the pluripotency of humanES cells [48]. Gearhart and colleagues derivehuman embryonic germ (EG) cells from thegonadal ridge and mesenchyma of 5- to9-week fetal tissue that resulted from electiveabortions. They grow EG cells in vitro for approximately20 passages, and the cells maintainnormal karyotypes. The cells spontaneously formaggregates that differentiate spontaneously, andultimately contain derivatives of all three primarygerm layers. Other indications of theirpluripotency include the expression of a panel ofmarkers typical of mouse ES and EG cells. TheEG cells do not form teratomas when injectedinto immune-deficient mice [41].• 2000: Scientists in Singapore and Australia led byPera, Trounson, and Bongso derive human EScells from the inner cell mass of blastocystsdonated by couples undergoing treatment forinfertility. The ES cells proliferate for extendedperiods in vitro, maintain normal karyotypes,differentiate spontaneously into somatic celllineages derived from all three primary germlayers, and form teratomas when injected intoimmune-deficient mice.• 2001: As human ES cell lines are shared andnew lines are derived, more research groupsreport methods to direct the differentiation ofthe cells in vitro. Many of the methods areaimed at generating human tissues fortransplantation purposes, including pancreaticislet cells, neurons that release dopamine, andcardiac muscle cells.DERIVATION OF HUMAN EMBRYONICSTEM CELLSThe first documentation of the isolation of embryonicstem cells from human blastocysts was in 1994 [7].Since then, techniques for deriving and culturinghuman ES cells have been refined [38, 48]. The abilityto isolate human ES cells from blastocysts and growthem in culture seems to depend in large part on theintegrity and condition of the blastocyst from whichthe cells are derived. In general, blastocysts with a12
The Human Embryonic <strong>Stem</strong> Cell and The Human Embryonic Germ CellPhoto Credit: Mr. J. Conaghanlarge and distinct inner cell mass tend to yield EScultures most efficiently [11] (see Figure 3.1.Human Blastocyst Showing Inner Cell Massand Trophectoderm).Timeline for the Development of a HumanFigure 3.1. Human Blastocyst Showing Inner Cell Massand Trophectoderm.Blastocyst In VitroAfter a human oocyte is fertilized in vitro by a spermcell, the following events occur according to a fairlypredictable timeline [9, 12, 16]. At 18 to 24 hoursafter in vitro fertilization of the oocyte is consideredday 1. By day 2 (24 to 25 hours), the zygote (fertilizedegg) undergoes the first cleavage to produce a2-cell embryo. By day 3 (72 hours), the embryoreaches the 8-cell stage called a morula. It is at thisstage that the genome of the embryo begins tocontrol its own development. This means that anymaternal influences—due to the presence of mRNAand proteins in the oocyte cytoplasm—aresignificantly reduced. By day 4, the cells of theembryo adhere tightly to each other in a processknown as compaction and by day 5, the cavity ofthe blastocyst is completed. The inner cell massbegins to separate from the outer cells, whichbecome the trophectoderm that surrounds theblastocyst. This represents the first observable signof cell differentiation in the embryo. (For amore detailed discussion, see Appendix A.Early Development.)Many IVF clinics now transfer day-5 embryos to theuterus for optimal implantation, a stage of developmentthat more closely parallels the stage at whicha blastocyst would implant in the wall of the uterusin vivo. This represents a change—and a greatlyimproved implantation rate—from earlier IVFprocedures in which a 2-cell embryo was usedfor implantation.Day-5 blastocysts are used to derive ES cell cultures.A normal day-5 human embryo in vitro consists of200 to 250 cells. Most of the cells comprise thetrophectoderm. For deriving ES cell cultures, thetrophectoderm is removed, either by microsurgeryor immunosurgery (in which antibodies against thetrophectoderm help break it down, thus freeing theinner cell mass). At this stage, the inner cell mass iscomposed of only 30 to 34 cells [10].The in vitro conditions for growing a human embryoto the blastocyst stage vary among IVF clinics andare reviewed elsewhere [6, 8, 14, 16, 18, 21, 39, 49,50]. However, once the inner cell mass is obtainedfrom either mouse or human blastocysts, the techniquesfor growing ES cells are similar. (For a detaileddiscussion see Appendix C. Human Embryonic <strong>Stem</strong><strong>Cells</strong> and Human Embryonic Germ <strong>Cells</strong>.)DERIVATION OF HUMAN EMBRYONICGERM CELLSAs stated earlier, human embryonic germ (EG) cellsshare many of the characteristics of human ES cells,but differ in significant ways. Human EG cells arederived from the primordial germ cells, which occurin a specific part of the embryo/fetus called thegonadal ridge, and which normally develop intomature gametes (eggs and sperm). Gearhart and hiscollaborators devised methods for growing pluripotentcells derived from human EG cells. The processrequires the generation of embryoid bodies from EGcells, which consists of an unpredictable mix ofpartially differentiated cell types [19]. The embryoidbody-derived cells resulting from this process havehigh proliferative capacity and gene expressionpatterns that are representative of multiple celllineages. This suggests that the embryoid bodyderivedcells are progenitor or precursor cells for13
The Human Embryonic <strong>Stem</strong> Cell and The Human Embryonic Germ Cella variety of differentiated cell types [19]. (For a moredetailed description of the derivation of EG cells, seeAppendix C. Human Embryonic <strong>Stem</strong> <strong>Cells</strong> andHuman Embryonic Germ <strong>Cells</strong>.)PLURIPOTENCY OF HUMANEMBRYONIC STEM CELLS ANDEMBRYONIC GERM CELLSAs stated earlier, a truly pluripotent stem cell is a cellthat is capable of self-renewal and of differentiatinginto most all of the cells of the body, including cells ofall three germ layers. Human ES and EG cells in vitroare capable of long-term self-renewal, while retaininga normal karyotype [1, 38, 41, 42, 48]. Human EScells can proliferate for two years through 300population doublings [29] or even 450 populationdoublings [30]. Cultures derived from embryoidbodies generated by human embryonic germcells have less capacity for proliferation. Most willproliferate for 40 population doublings; the maximumreported is 70 to 80 population doublings [42].To date, several laboratories have demonstrated thathuman ES cells in vitro are pluripotent; they canproduce cell types derived from all three embryonicgerm layers [1, 20, 38, 40].Currently, the only test of the in vivo pluripotency ofhuman ES cells is to inject them into immunedeficientmice where they generate differentiatedcells that are derived from all three germ layers.These include gut epithelium (which, in the embryo,is derived from endoderm); smooth and striatedmuscle (derived from mesoderm); and neuralepithelium, and stratified squamous epithelium(derived from ectoderm) [20, 38, 48].However, two aspects of in vivo pluripotency typicallyused in animals have not been met by human EScells: evidence that cells have the capacity to beinjected into a human embryo and form an organismmade up of cells from two genetic lineages;and evidence that they have the ability to generategerm cells, the precursors to eggs and sperm in adeveloping organism. These are theoreticalconsiderations, however, because such tests usinghuman ES cells have not been conducted. In anycase, these two demonstrations of human ES cellpluripotency are not likely to be critical for potentialtherapeutic uses of the cells—in transplants or drugdevelopment, for example [43].COMPARISONS BETWEEN HUMANEMBRYONIC STEM CELLS ANDEMBRYONIC GERM CELLSThe ES cells derived from human blastocysts byThomson and his colleagues, and from human EGcells derived by Gearhart and his collaborators, aresimilar in many respects. In both cases, the cellsreplicate for an extended period of time, show nochromosomal abnormalities, generate both XX(female) and XY (male) cultures, and express a setof markers regarded as characteristic of pluripotentcells. When the culture conditions are adjusted topermit differentiation (see below for details), bothES and EG cells spontaneously differentiate intoderivatives of all three primary germ layers—endoderm, mesoderm, and ectoderm (see Table3.1. Comparison of Mouse, Monkey, and HumanPluripotent <strong>Stem</strong> <strong>Cells</strong>).However, the ES cells derived from human blastocystsand EG cells differ not only in the tissue sources fromwhich they are derived, they also vary with respect totheir growth characteristics in vitro, and their behaviorin vivo [34]. In addition, human ES cells have beenpropagated for approximately two years in vitro, forseveral hundred population doublings [1], whereashuman embryoid body-derived cells from cultures ofembryonic germ cells have been maintained for only70 to 80 population doublings [42]. Also, human EScells will generate teratomas containing differentiatedcell types, if injected into immunocompromisedmice colonies, while human EG cells will not[20, 37, 38, 41, 48].Several research groups are trying to grow human EScells without feeder layers of mouse embryo fibroblasts(MEF), which are labor-intensive to generate.At a recent meeting, scientists from the GeronCorporation reported that they have grown human EScell without feeder layers, in medium conditioned byMEFs and supplemented with basic FGF [51].DIRECTED DIFFERENTIATION OFHUMAN EMBRYONIC STEM CELLSAND EMBRYONIC GERM CELLSIN VITROCurrently, a major goal for embryonic stem cellresearch is to control the differentiation of human ESand EG cell lines into specific kinds of cells—an14
The Human Embryonic <strong>Stem</strong> Cell and The Human Embryonic Germ CellTable 3.1. Comparison of Mouse, Monkey, and Human Pluripotent <strong>Stem</strong> <strong>Cells</strong>MarkerNameMouse EC/ES/EG cellsMonkeyES cellsHumanES cellsHumanEG cellsHumanEC cellsSSEA-1 + – – + –SSEA-3 – + + + +SEA-4 – + + + +TRA-1-60 – + + + +TRA-1-81 – + + + +Alkalinephosphatase+ + + + +Oct-4 + + + Unknown +Telomerase activity + ES, EC Unknown + Unknown +Feeder-celldependentES, EG,some ECYes Yes Yes Some; relatively lowclonal efficiencyFactors which aidin stem cellself-renewalLIF and otherfactors that actthrough gp130receptor and cansubstitute forfeeder layerCo-culture withfeeder cells; otherpromoting factorshave not beenidentifiedFeeder cells +serum; feederlayer +serum-freemedium + bFGFLIF, bFGF,forskolinUnknown;low proliferativecapacityGrowthcharacteristicsin vitroForm tight,rounded,multi-layer clumps;can form EBsForm flat, looseaggregates;can form EBsForm flat, looseaggregates;can form EBsForm rounded,multi-layer clumps;can form EBsForm flat, looseaggregates;can form EBsTeratomaformation in vivoChimeraformation+ + + – ++ Unknown + – +KEYES cell =EG cell =EC cell =SSEA =Embryonic stem cellEmbryonic germ cellEmbryonal carcinoma cellStage-specific embryonic antigenTRA =LIF =bFGF =EB =Tumor rejection antigen-1Leukemia inhibitory factorBasic fibroblast growth factorEmbryoid bodiesobjective that must be met if the cells are to be usedas the basis for therapeutic transplantation, testingdrugs, or screening potential toxins. The techniquesnow being tested to direct human ES cell differentiationare borrowed directly from techniques used todirect the differentiation of mouse ES cells in vitro. Formore discussion on directed differentiation of humanES and EG cells see Appendix C.POTENTIAL USES OF HUMANEMBRYONIC STEM CELLSMany uses have been proposed for humanembryonic stem cells. The most-often discussed istheir potential use in transplant therapy—i.e., toreplace or restore tissue that has been damaged bydisease or injury (see also Chapters 5-9).15
The Human Embryonic <strong>Stem</strong> Cell and The Human Embryonic Germ CellUsing Human Embryonic <strong>Stem</strong> <strong>Cells</strong> forTherapeutic TransplantsDiseases that might be treated by transplantinghuman ES-derived cells include Parkinson’s disease,diabetes, traumatic spinal cord injury, Purkinje celldegeneration, Duchenne’s muscular dystrophy, heartfailure, and osteogenesis imperfecta. However, treatmentsfor any of these diseases require that humanES cells be directed to differentiate into specific celltypes prior to transplant. The research is occurring inseveral laboratories, but is limited because so fewlaboratories have access to human ES cells. Thus, atHuman ES <strong>Cells</strong>Establish pure culturesof specific cell type• Lineage selection by cell survivalor cell sorting (e.g., insulin promoterdriving antibiotic resistance geneor GFP)• Induce with supplemental growthfactor(s) or inducer cells (e.g.,retinoic acid for neural cells)Test physiologicfunction• In vitro (e.g., stimulatedinsulin release)DemonstrateefficacyDemonstratesafetyTest methodsto prevent rejection• In rodent models• In non-human primate modelwith rhesus ES cell-derived cells(e.g., diabetes and Parkinson’sdisease models in primates)• Evaluate integration into hosttissue (e.g., cardiomyocytes fortreatment of heart failure)• ? recurrent autoimmunity(e.g., diabetes)• In non-human primate model withrhesus ES cell-derived tissues• Show absence of tumor formation• Show absence of transmissionof infectious agents• Multi-drug immunosuppression• Create differentiated cellsisogenic to prospective recipientusing nuclear reprogramming• Transduce ES cells to expressrecipient MHC genes• Establish hematopoietic chimeraand immunologic toleranceHuman trialsFigure 3.2. Major Goals in the Development of Transplantation Therapies from Human ES Cell Lines. (Reproduced withpermission from <strong>Stem</strong> <strong>Cells</strong>, 2001)16
The Human Embryonic <strong>Stem</strong> Cell and The Human Embryonic Germ Cellthis stage, any therapies based on the use of humanES cells are still hypothetical and highly experimental[22, 29, 31] (see Figure 3.2. Major Goals in theDevelopment of Transplantation Therapies fromHuman ES Cell Lines).One of the current advantages of using ES cells ascompared to adult stem cells is that ES cells have anunlimited ability to proliferate in vitro, and are morelikely to be able to generate a broad range of celltypes through directed differentiation. Ultimately, it willalso be necessary to both identify the optimalstage(s) of differentiation for transplant, anddemonstrate that the transplanted ES-derived cellscan survive, integrate, and function in the recipient.The potential disadvantages of the use of human EScells for transplant therapy include the propensity ofundifferentiated ES cells to induce the formation oftumors (teratomas), which are typically benign.Because it is the undifferentiated cells—rather thantheir differentiated progeny—that have been shownto induce teratomas, tumor formation might beavoided by devising methods for removing anyundifferentiated ES cells prior to transplant. Also, itshould be possible to devise a fail-safe mechanism—i.e., to insert into transplanted ES-derived cells suicidegenes that can trigger the death of the cells shouldthey become tumorigenic.Human ES derived cells would also be advantageousfor transplantation purposes if they did not triggerimmune rejection. The immunological status ofhuman ES cells has not been studied in detail, and itis not known how immunogenic ES-derived cellsmight be. In general, the immunogenicity of a celldepends on its expression of Class I majorhistocompatability antigens (MHC), which allow thebody to distinguish its own cells from foreign tissue,and on the presence of cells that can bind to foreignantigens and “present” them to the immune system.The potential immunological rejection of humanES-derived cells might be avoided by geneticallyengineering the ES cells to express the MHC antigensof the transplant recipient, or by using nuclear transfertechnology to generate ES cells that are geneticallyidentical to the person who receives the transplant.It has been suggested that this could be accomplishedby using somatic cell nuclear transfertechnology (so-called therapeutic cloning) in whichthe nucleus is removed from one of the transplantpatient’s cells, such as a skin cell, and injecting thenucleus into an oocyte. The oocyte, thus “fertilized,”could be cultured in vitro to the blastocyst stage. EScells could subsequently be derived from its inner cellmass, and directed to differentiate into the desiredcell type. The result would be differentiated (or partlydifferentiated) ES-derived cells that match exactly theimmunological profile of the person who donated thesomatic cell nucleus, and who is also the intendedrecipient of the transplant—a labor intensive, but trulycustomized therapy [29].Other Potential Uses of Human Embryonic<strong>Stem</strong> <strong>Cells</strong>Many potential uses of human ES cells have beenproposed that do not involve transplantation. Forexample, human ES cells could be used to studyearly events in human development. Still-unexplainedevents in early human development can result incongenital birth defects and placental abnormalitiesthat lead to spontaneous abortion. By studyinghuman ES cells in vitro, it may be possible to identifythe genetic, molecular, and cellular events that leadto these problems and identify methods forpreventing them [22, 35, 45].Such cells could also be used to explore the effectsof chromosomal abnormalities in early development.This might include the ability to monitor the developmentof early childhood tumors, many of which areembryonic in origin [32].Human ES cells could also be used to test candidatetherapeutic drugs. Currently, before candidate drugsare tested in human volunteers, they are subjected toa barrage of preclinical tests. These include drugscreening in animal models—in vitro tests using cellsderived from mice or rats, for example, or in vivo teststhat involve giving the drug to an animal to assess itssafety. Although animal model testing is a mainstayof pharmaceutical research, it cannot always predictthe effects that a candidate drug may have onhuman cells. For this reason, cultures of human cellsare often employed in preclinical tests. These humancell lines have usually been maintained in vitro forlong periods and as such often have differentcharacteristics than do in vivo cells. These differencescan make it difficult to predict the action of a drug invivo based on the response of human cell lines invitro. Therefore, if human ES cells can be directed todifferentiate into specific cell types that are important17
The Human Embryonic <strong>Stem</strong> Cell and The Human Embryonic Germ CellA. Genetic manipulationof MHC genesMicropipetB. Nuclear reprogrammingEnucleatedoocyteC. Hematopoietic chimera:complete, mixed, microES cellsTransfer ofdonated nucleusHolding pipetES cellsDeletion ofMHC genesXXorTissue-specificdifferentiationSubstitution ofMHC genesES-cellsderived fromnuclear transferproductMusclePancreaticislet cellsXXTissue-specificdifferentiationHematopoieticdifferentiationNeuronXXMHC-deficienttissueSelf-MHCexpressingtissueDifferentiatedtissue expressingdonor nucleusMHC genesCotransplantationFigure 3.3. Genetic Manipulation of Human Embryonic <strong>Stem</strong> <strong>Cells</strong>. (Reproduced with permission from <strong>Stem</strong> <strong>Cells</strong>, 2001)for drug screening, the ES-derived cells may be morelikely to mimic the in vivo response of the cells/tissuesto the drug(s) being tested and so offer safer, andpotentially cheaper, models for drug screening.Human ES cells could be employed to screenpotential toxins. The reasons for using human ES cellsto screen potential toxins closely resemble those forusing human ES-derived cells to test drugs (above).Toxins often have different effects on different animalspecies, which makes it critical to have the bestpossible in vitro models for evaluating their effectson human cells.Finally, human ES cells could be used to develop newmethods for genetic engineering (see Figure 3.3.Genetic Manipulation of Human Embryonic <strong>Stem</strong><strong>Cells</strong>). Currently, the genetic complement of mouseES cells in vitro can be modified easily by techniquessuch as homologous recombination. This is a methodfor replacing or adding genes, which requires that aDNA molecule be artificially introduced into thegenome and then expressed. Using this method,genes to direct differentiation to a specific cell typeor genes that express a desired protein product mightbe introduced into the ES cell line. Ultimately, if suchtechniques could be developed using human EScells, it may be possible to devise better methods forgene therapy [35] (see Chapter 10. Assessing Human<strong>Stem</strong> Cell Safety).SUMMARYWhat Do We Know About Human Embryonic<strong>Stem</strong> <strong>Cells</strong>?Since 1998, research teams have refined thetechniques for growing human ES cells in vitro [1, 20,38]. Collectively, the studies indicate that it is nowpossible to grow human ES cells for more than a yearin serum-free medium on feeder layers. The cellshave normal karyotype and are pluripotent; theygenerate teratomas that contain differentiated celltypes derived from all three primary germ layers. Thelong-term cultures of human ES cells have activetelomerase and maintain relatively long telomeres,another marker of proliferating cells.Overall, the pluripotent cells that can be generatedin vitro from human ES cells and human EG cells areapparently not equivalent in their potential toproliferate or differentiate. (ES cells are derived fromthe inner cell mass of the preimplantation blastocyst,approximately 5 days post-fertilization, whereashuman EG cells are derived from fetal primordial18
The Human Embryonic <strong>Stem</strong> Cell and The Human Embryonic Germ Cellgerm cells, 5 to 10 weeks post-fertilization.) ES cellscan proliferate for up to 300 population doublings,while cells derived from embryoid bodies that aregenerated from embryonic germ cells (fetal tissue)double a maximum of 70 to 80 times in vitro.ES cells appear to have a broader ability to differentiate.Both kinds of cells spontaneously generate neuralprecursor-type cells (widely regarded as a defaultpathway for differentiation), and both generate cellsthat resemble cardiac myocytes [19, 45]. However,human ES and EG cells in vitro will spontaneouslygenerate embryoid bodies that consist of cell typesfrom all three primary germ layers [1, 20, 38, 42].What Do We Need To Know About HumanEmbryonic <strong>Stem</strong> <strong>Cells</strong>?Scientists are just beginning to understand the biologyof human embryonic stem cells, and many keyquestions remain unanswered or only partlyanswered. For example, in order to refine andimprove ES cell culture systems, it is important thatscientists identify the mechanisms that allow humanES cells in vitro to proliferate without differentiating[29]. Once the mechanisms that regulate human ESproliferation are known, it will likely be possible toapply this knowledge to the long-standing challengeof improving the in vitro self-renewal capabilities ofadult stem cells.It will also be important to determine whether thegenetic imprinting status of human ES cells plays anysignificant role in maintaining the cells, directing theirdifferentiation, or determining their suitability fortransplant. One of the effects of growing mouseblastocysts in culture is a change in the methylationof specific genes that control embryonic growthand development [23]. Do similar changes in geneimprinting patterns occur in human ES cells (orblastocysts)? If so, what is their effect on in vitrodevelopment and on any differentiated cell typesthat may be derived from cultured ES cells?Efforts will need to be made to determine whethercultures of human ES cells that appear to behomogeneous and undifferentiated are, in fact,homogeneous and undifferentiated. Is it possiblethat human ES cells in vitro cycle in and out ofpartially differentiated states? And if that occurs, howwill it affect attempts to direct their differentiation ormaintain the cells in a proliferating state [28]?Scientists will need to identify which signal transductionpathways must be activated to induce human ES celldifferentiation along a particular pathway. This includesunderstanding ligand-receptor interaction and theintracellular components of the signaling system, aswell as identifying the genes that are activated or inactivatedduring differentiation of specific cell types [29].Identifying intermediate stages of human ES celldifferentiation will also be important. As human EScells differentiate in vitro, do they form distinctprecursor or progenitor cells that can be identifiedand isolated? If ES cells do form such intermediatecell types, can the latter be maintained andexpanded? Would such precursor or progenitor cellsbe useful for therapeutic transplantation [19]?Finally, scientists will need to determine whatdifferentiation stages of human ES-derived cells areoptimal for other practical applications. For example,what differentiation stages of ES-derived cells wouldbe best for screening drugs or toxins, or for deliveringpotentially therapeutic drugs?REFERENCES1. Amit, M., Carpenter, M.K., Inokuma, M.S., Chiu, C.P., Harris,C.P., Waknitz, M.A., Itskovitz-Eldor, J., and Thomson, J.A.(2000). Clonally derived human embryonic stem cell linesmaintain pluripotency and proliferative potential forprolonged periods of culture. Dev. Biol. 227, 271-278.2. Andrews, P.W., Damjanov, I., Simon, D., Banting, G.S.,Carlin, C., Dracopoli, N.C., and Fogh, J. (1984). Pluripotentembryonal carcinoma clones derived from the humanteratocarcinoma cell line Tera-2. Differentiation in vivoand in vitro. Lab. Invest. 50, 147-162.3. Andrews, P.W. (1988). Human teratocarcinomas. Biochim.Biophys. Acta. 948, 17-36.4. Andrews, P.W. (1998). Teratocarcinomas and humanembryology: pluripotent human EC cell lines. Reviewarticle. APMIS 106, 158-167.5. Andrews, P. W., personal communication.6. Bongso, A., Fong, C.Y., Ng, S.C., and Ratnam, S.S. (1994).Blastocyst transfer in human in vitro: fertilization; the use ofembryo co-culture. Cell Biol. Int. 18, 1181-1189.7. Bongso, A., Fong, C.Y., Ng, S.C., and Ratnam, S. (1994).Isolation and culture of inner cell mass cells from humanblastocysts. Hum. Reprod. 9, 2110-2117.8. Bongso, A., Fong, C.Y., Ng, S.C., and Ratnam, S.S. (1995).Co-culture techniques for blastocyst transfer and embryonicstem cell production. Asst. Reprod. Rev. 5, 106-114.19
The Human Embryonic <strong>Stem</strong> Cell and The Human Embryonic Germ Cell9. Bongso, A. (1996). Behaviour of human embryos in vitro inthe first 14 days: blastocyst transfer and embryonic stemcell production. Clin. Sci. (Colch.) 91, 248-249.10. Bongso, A., Fong, C.Y., Mathew, J., Ng, L.C., Kumar, J., andNg, S.C. (1999). The benefits to human IVF by transferringembryos after the in vitro embryonic block: alternatives today 2 transfers. Asst. Reprod. Rev.11. Bongso, A. (1999). Handbook on blastocyst culture,(Singapore: Sydney Press Indusprint).12. Bongso, A., personal communication.13. Bradley, A., Evans, M., Kaufman, M.H., and Robertson, E.(1984). Formation of germ-line chimaeras from embryoderivedteratocarcinoma cell lines. Nature. 309, 255-256.14. De Vos, A. and Van Steirteghem, A. (2000). Zona hardening,zona drilling and assisted hatching: new achievements inassisted reproduction. <strong>Cells</strong> Tissues Organs. 166, 220-227.15. Evans, M.J. and Kaufman, M.H. (1981). Establishment inculture of pluripotential cells from mouse embryos.Nature. 292, 154-156.16. Fong, C.Y., Bongso, A., Ng, S.C., Kumar, J., Trounson, A.,and Ratnam, S. (1998). Blastocyst transfer after enzymatictreatment of the zona pellucida: improving in-vitro fertilizationand understanding implantation. Hum. Reprod.13, 2926-2932.17. Friedrich, T.D., Regenass, U., and Stevens, L.C. (1983).Mouse genital ridges in organ culture: the effects oftemperature on maturation and experimental induction ofteratocarcinogenesis. Differentiation. 24, 60-64.18. Gardner, D.K. and Schoolcraft, W.B. (1999). Culture andtransfer of human blastocysts. Curr. Opin. Obstet. Gynecol.11, 307-311.19. Gearhart, J., personal communication.20. Itskovitz-Eldor, J., Schuldiner, M., Karsenti, D., Eden, A.,Yanuka, O., Amit, M., Soreq, H., and Benvenisty, N. (2000).Differentiation of human embryonic stem cells into embryoidbodies comprising the three embryonic germ layers.Mol. Med. 6, 88-95.21. Jones, G.M., Trounson, A.O., Lolatgis, N., and Wood, C.(1998). Factors affecting the success of human blastocystdevelopment and pregnancy following in vitro fertilizationand embryo transfer. Fertil. Steril. 70, 1022-1029.22. Jones, J.M. and Thomson, J.A. (2000). Human embryonicstem cell technology. Semin. Reprod. Med. 18, 219-223.23. Khosla, S., Dean, W., Brown, D., Reik, W., andFeil, R. (2001). Culture of preimplantation mouse embryosaffects fetal development and the expression of imprintedgenes. Biol. Reprod. 64, 918-926.24. Kleinsmith, L.J. and Pierce Jr, G.B. (1964). Multipotentialityof single embryonal carcinoma cells. Cancer Res. 24,1544-1551.25. Martin, G.R. (1980). Teratocarcinomas and mammalianembryogenesis. Science. 209, 768-776.26. Martin, G.R. (1981). Isolation of a pluripotent cell line fromearly mouse embryos cultured in medium conditioned byteratocarcinoma stem cells. Proc. Natl. Acad. Sci. U. S. A.78, 7634-7638.27. Matsui, Y., Toksoz, D., Nishikawa, S., Nishikawa, S., Williams,D., Zsebo, K., and Hogan, B.L. (1991). Effect of steel factorand leukaemia inhibitory factor on murine primordial germcells in culture. Nature. 353, 750-752.28. McKay, R., personal communication.29. Odorico, J.S., Kaufman, D.S., and Thomson, J.A. (2001).Multilineage Differentiation from Human Embryonic <strong>Stem</strong>Cell Lines. <strong>Stem</strong> <strong>Cells</strong>. 19, 193-204.30. Okarma, T., personal communication.31. Pedersen, R.A. (1999). Embryonic stem cells for medicine.Sci. Am. 280, 68-73.32. Pera, M., personal communication.33. Pera, M.F., Cooper, S., Mills, J., and Parrington,J.M. (1989). Isolation and characterization of a multipotentclone of human embryonal carcinoma cells.Differentiation. 42, 10-23.34. Pera, M.F., Reubinoff, B., and Trounson, A. (2000). Humanembryonic stem cells. J. Cell Sci. 113 (Pt 1), 5-10.35. Rathjen, P.D., Lake, J., Whyatt, L.M., Bettess, M.D., andRathjen, J. (1998). Properties and uses of embryonic stemcells: prospects for application to human biology andgene therapy. Reprod. Fertil. Dev. 10, 31-47.36. Resnick, J.L., Bixler, L.S., Cheng, L., and Donovan, P.J. (1992).Long-term proliferation of mouse primordial germ cells inculture. Nature. 359, 550-551.37. Reubinoff BE, Pera, M., Fong, C.Y., and Trounson, A. andBongso, A. (2000). Research Errata. Nat. Biotechnol. 18,559.38. Reubinoff, B.E., Pera, M.F., Fong, C.Y., Trounson, A., andBongso, A. (2000). Embryonic stem cell lines from humanblastocysts: somatic differentiation in vitro. Nat. Biotechnol.18, 399-404.39. Sathananthan, A.H. (1997). Ultrastructure of the humanegg. Hum. Cell. 10, 21-38.40. Schuldiner, M., Yanuka, O., Itskovitz-Eldor, J., Melton, D., andBenvenisty, N. (2000). Effects of eight growth factors on thedifferentiation of cells derived from human embryonic stemcells. Proc. Natl. Acad. Sci. U. S. A. 97, 11307-11312.41. Shamblott, M.J., Axelman, J., Wang, S., Bugg, E.M.,Littlefield, J.W., Donovan, P.J., Blumenthal, P.D., Huggins,G.R., and Gearhart, J.D. (1998). Derivation of pluripotentstem cells from cultured human primordial germ cells.Proc. Natl. Acad. Sci. U. S. A. 95, 13726-13731.20
The Human Embryonic <strong>Stem</strong> Cell and The Human Embryonic Germ Cell42. Shamblott, M.J., Axelman, J., Littlefield, J.W., Blumenthal,P.D., Huggins, G.R., Cui, Y., Cheng, L., and Gearhart, J.D.(2001). Human embryonic germ cell derivatives express abroad range of develpmentally distinct markers andproliferate extensively in vitro. Proc. Natl. Acad. Sci. U. S. A.98, 113-118.43. Smith, A.G. (2001). Origins and properties of mouseembryonic stem cells. Annu. Rev. Cell. Dev. Biol.44. Thompson, S., Stern, P.L., Webb, M., Walsh, F.S., Engstrom,W., Evans, E.P., Shi, W.K., Hopkins, B., and Graham, C.F.(1984). Cloned human teratoma cells differentiate intoneuron-like cells and other cell types in retinoic acid. J. CellSci. 72, 37-64.45. Thomson, J., personal communication.46. Thomson, J.A., Kalishman, J., Golos, T.G., Durning, M., Harris,C.P., Becker, R.A., and Hearn, J.P. (1995). Isolation of aprimate embryonic stem cell line. Proc. Natl. Acad. Sci.U. S. A. 92, 7844-7848.47. Thomson, J.A., Kalishman, J., Golos, T.G., Durning, M., Harris,C.P., and Hearn, J.P. (1996). Pluripotent cell lines derivedfrom common marmoset (Callithrix jacchus) blastocysts.Biol. Reprod. 55, 254-259.48. Thomson, J.A., Itskovitz-Eldor, J., Shapiro, S.S., Waknitz, M.A.,Swiergiel, J.J., Marshall, V.S., and Jones, J.M. (1998).Embryonic stem cell lines derived from human blastocysts.Science. 282, 1145-1147.49. Trounson, A.O., Gardner, D.K., Baker, G., Barnes, F.L.,Bongso, A., Bourne, H., Calderon, I., Cohen, J., Dawson, K.,Eldar-Geve, T., Gardner, D.K., Graves, G., Healy, D., Lane,M., Leese, H.J., Leeton, J., Levron, J., Liu, D.Y., MacLachlan,V., Munné, S., Oranratnachai, A., Rogers, P., Rombauts, L.,Sakkas, D., Sathananthan, A.H., Schimmel, T., Shaw, J.,Trounson, A.O., Van Steirteghem, A., Willadsen, S., andWood, C. (2000b). Handbook of in vitro fertilization, (BocaRaton, London, New York, Washington, D.C.:CRC Press).50. Trounson, A.O., Anderiesz, C., and Jones, G. (2001).Maturation of human oocytes in vitro and their developmentalcompetence. Reproduction. 121, 51-75.51. Xu, C., Inokuma, M.S., Denham, J., Golds, K., Kundu, P.,Gold, J.D., and Carpenter, M.K. Keystone symposia.Pluripotent stem cells: biology and applications. Growth ofundifferentiated human embryonic stem cells on definedmatrices with conditioned medium. Poster abstract. 133.21
The Human Embryonic <strong>Stem</strong> Cell and The Human Embryonic Germ CellThis page intentionally left blank.22
4.THE ADULT STEM CELLFor many years, researchers have been seeking tounderstand the body’s ability to repair and replacethe cells and tissues of some organs, but not others.After years of work pursuing the how and why ofseemingly indiscriminant cell repair mechanisms,scientists have now focused their attention on adultstem cells. It has long been known that stem cellsare capable of renewing themselves and that theycan generate multiple cell types. Today, there is newevidence that stem cells are present in far moretissues and organs than once thought and that thesecells are capable of developing into more kinds ofcells than previously imagined. Efforts are nowunderway to harness stem cells and to takeadvantage of this new found capability, with the goalof devising new and more effective treatments for ahost of diseases and disabilities. What lies ahead forthe use of adult stem cells is unknown, but it iscertain that there are many research questions to beanswered and that these answers hold great promisefor the future.WHAT IS AN ADULT STEM CELL?Adult stem cells, like all stem cells, share at least twocharacteristics. First, they can make identical copiesof themselves for long periods of time; this ability toproliferate is referred to as long-term self-renewal.Second, they can give rise to mature cell types thathave characteristic morphologies (shapes) andspecialized functions. Typically, stem cells generatean intermediate cell type or types before theyachieve their fully differentiated state. The intermediatecell is called a precursor or progenitor cell.Progenitor or precursor cells in fetal or adult tissues arepartly differentiated cells that divide and give rise todifferentiated cells. Such cells are usually regarded as“committed” to differentiating along a particularcellular development pathway, although thischaracteristic may not be as definitive as oncethought [82] (see Figure 4.1. Distinguishing Features ofProgenitor/Precursor <strong>Cells</strong> and <strong>Stem</strong> <strong>Cells</strong>).Adult stem cells are rare. Their primary functions areto maintain the steady state functioning of a cell—called homeostasis—and, with limitations, to replacecells that die because of injury or disease [44, 58].For example, only an estimated 1 in 10,000 to 15,000cells in the bone marrow is a hematopoietic (bloodforming)stem cell (HSC) [105]. Furthermore, adultstem cells are dispersed in tissues throughout themature animal and behave very differently,depending on their local environment. For example,HSCs are constantly being generated in the bonemarrow where they differentiate into mature types ofblood cells. Indeed, the primary role of HSCs is toreplace blood cells [26] (see Chapter 5. Hematopoietic<strong>Stem</strong> <strong>Cells</strong>). In contrast, stem cells in the smallintestine are stationary, and are physically separatedfrom the mature cell types they generate. Gut epithelialstem cells (or precursors) occur at the bases ofcrypts—deep invaginations between the mature,differentiated epithelial cells that line the lumen of theintestine. These epithelial crypt cells divide fairly often,but remain part of the stationary group of cells theygenerate [93].Unlike embryonic stem cells, which are defined bytheir origin (the inner cell mass of the blastocyst),adult stem cells share no such definitive means ofcharacterization. In fact, no one knows the origin ofadult stem cells in any mature tissue. Some haveproposed that stem cells are somehow set asideduring fetal development and restrained fromdifferentiating. Definitions of adult stem cells vary inthe scientific literature range from a simple descriptionof the cells to a rigorous set of experimentalcriteria that must be met before characterizing a23
The Adult <strong>Stem</strong> CellSTEM CELLSTEM CELL(e.g., hematopoieticstem cell)SPECIALIZED CELL(e.g., neuron)PROGENITOR CELL(e.g., myeloidprogenitor cell)SPECIALIZED CELL(e.g., neutrophil)© 2001 Terese Winslow, Lydia KibiukSPECIALIZED CELL(e.g., red blood cell)Figure 4.1. Distinguishing Features of Progenitor/Precursor <strong>Cells</strong> and <strong>Stem</strong> <strong>Cells</strong>. A stem cell is an unspecialized cell that iscapable of replicating or self renewing itself and developing into specialized cells of a variety of cell types. The product of astem cell undergoing division is at least one additional stem cell that has the same capabilities of the originating cell. Shownhere is an example of a hematopoietic stem cell producing a second generation stem cell and a neuron. A progenitorcell (also known as a precursor cell) is unspecialized or has partial characteristics of a specialized cell that is capable ofundergoing cell division and yielding two specialized cells. Shown here is an example of a myeloid progenitor/precursorundergoing cell division to yield two specialized cells (a neutrophil and a red blood cell).24
The Adult <strong>Stem</strong> Cellparticular cell as an adult stem cell. Most of the informationabout adult stem cells comes from studies ofmice. The list of adult tissues reported to contain stemcells is growing and includes bone marrow, peripheralblood, brain, spinal cord, dental pulp, blood vessels,skeletal muscle, epithelia of the skin and digestivesystem, cornea, retina, liver, and pancreas.In order to be classified as an adult stem cell, the cellshould be capable of self-renewal for the lifetime ofthe organism. This criterion, although fundamental tothe nature of a stem cell, is difficult to prove in vivo. Itis nearly impossible, in an organism as complex as ahuman, to design an experiment that will allow thefate of candidate adult stem cells to be identified invivo and tracked over an individual’s entire lifetime.Ideally, adult stem cells should also be clonogenic. Inother words, a single adult stem cell should be ableto generate a line of genetically identical cells, whichthen gives rise to all the appropriate, differentiatedcell types of the tissue in which it resides. Again, thisproperty is difficult to demonstrate in vivo; in practice,scientists show either that a stem cell is clonogenic invitro, or that a purified population of candidate stemcells can repopulate the tissue.An adult stem cell should also be able to give rise tofully differentiated cells that have mature phenotypes,are fully integrated into the tissue, and are capableof specialized functions that are appropriate for thetissue. The term phenotype refers to all the observablecharacteristics of a cell (or organism); its shape(morphology); interactions with other cells and thenon-cellular environment (also called the extracellularmatrix); proteins that appear on the cell surface(surface markers); and the cell’s behavior (e.g.,secretion, contraction, synaptic transmission).The majority of researchers who lay claim to havingidentified adult stem cells rely on two of these characteristics—appropriatecell morphology, and thedemonstration that the resulting, differentiated celltypes display surface markers that identify them asbelonging to the tissue. Some studies demonstratethat the differentiated cells that are derived fromadult stem cells are truly functional, and a few studiesshow that cells are integrated into the differentiatedtissue in vivo and that they interact appropriately withneighboring cells. At present, there is, however, apaucity of research, with a few notable exceptions, inwhich researchers were able to conduct studies ofgenetically identical (clonal) stem cells. In order tofully characterize the regenerating and self-renewalcapabilities of the adult stem cell, and therefore totruly harness its potential, it will be important todemonstrate that a single adult stem cell can,indeed, generate a line of genetically identical cells,which then gives rise to all the appropriate, differentiatedcell types of the tissue in which it resides.EVIDENCE FOR THE PRESENCE OFADULT STEM CELLSAdult stem cells have been identified in many animaland human tissues. In general, three methods areused to determine whether candidate adult stemcells give rise to specialized cells. Adult stem cellscan be labeled in vivo and then they can betracked. Candidate adult stem cells can also beisolated and labeled and then transplanted back intothe organism to determine what becomes of them.Finally, candidate adult stem cells can be isolated,grown in vitro and manipulated, by adding growthfactors or introducing genes that help determinewhat differentiated cells types they will yield. Forexample, currently, scientists believe that stem cells inthe fetal and adult brain divide and give rise to morestem cells or to several types of precursor cells, whichgive rise to nerve cells (neurons), of which there aremany types.It is often difficult—if not impossible—to distinguishadult, tissue-specific stem cells from progenitor cells,which are found in fetal or adult tissues and are partlydifferentiated cells that divide and give rise to differentiatedcells. These are cells found in many organsthat are generally thought to be present to replacecells and maintain the integrity of the tissue.Progenitor cells give rise to certain types of cells—such as the blood cells known as T lymphocytes,B lymphocytes, and natural killer cells—but are notthought to be capable of developing into all the celltypes of a tissue and as such are not truly stem cells.The current wave of excitement over the existence ofstem cells in many adult tissues is perhaps fuelingclaims that progenitor or precursor cells in those tissuesare instead stem cells. Thus, there are reports ofendothelial progenitor cells, skeletal muscle stemcells, epithelial precursors in the skin and digestivesystem, as well as some reports of progenitors or stemcells in the pancreas and liver. A detailed summaryof some of the evidence for the existence of stem25
The Adult <strong>Stem</strong> Cellcells in various tissues and organs is presented later inthe chapter.ADULT STEM CELL PLASTICITYIt was not until recently that anyone seriously consideredthe possibility that stem cells in adult tissuescould generate the specialized cell types of anothertype of tissue from which they normally reside—eithera tissue derived from the same embryonic germlayer or from a different germ layer (see Table 1.1.Embryonic Germ Layers From Which DifferentiatedTissues Develop). For example, studies have shownthat blood stem cells (derived from mesoderm) maybe able to generate both skeletal muscle (alsoderived from mesoderm) and neurons (derived fromectoderm). That realization has been triggered by aflurry of papers reporting that stem cells derived fromone adult tissue can change their appearance andassume characteristics that resemble those of differentiatedcells from other tissues.The term plasticity, as used in this report, means thata stem cell from one adult tissue can generate thedifferentiated cell types of another tissue. At this time,there is no formally accepted name for this phenomenonin the scientific literature. It is variously referredto as “plasticity” [15, 52], “unorthodox differentiation”[10] or “transdifferentiation” [7, 54].Approaches for Demonstrating Adult <strong>Stem</strong> CellPlasticityTo be able to claim that adult stem cells demonstrateplasticity, it is first important to show that a cellpopulation exists in the starting tissue that has theidentifying features of stem cells. Then, it is necessaryto show that the adult stem cells give rise to cell typesthat normally occur in a different tissue. Neither ofthese criteria is easily met. Simply proving the existenceof an adult stem cell population in a differentiatedtissue is a laborious process. It requires that thecandidate stem cells are shown to be self-renewing,and that they can give rise to the differentiated celltypes that are characteristic of that tissue.To show that the adult stem cells can generate othercell types requires them to be tracked in their newenvironment, whether it is in vitro or in vivo. In general,this has been accomplished by obtaining the stemcells from a mouse that has been genetically engineeredto express a molecular tag in all its cells. It isthen necessary to show that the labeled adult stemcells have adopted key structural and biochemicalcharacteristics of the new tissue they are claimed tohave generated. Ultimately—and most importantly—itis necessary to demonstrate that the cells can integrateinto their new tissue environment, survive in thetissue, and function like the mature cells of the tissue.In the experiments reported to date, adult stem cellsmay assume the characteristics of cells that havedeveloped from the same primary germ layer or adifferent germ layer (see Figure 4.2. PreliminaryEvidence of Plasticity Among Nonhuman Adult <strong>Stem</strong><strong>Cells</strong>). For example, many plasticity experimentsinvolve stem cells derived from bone marrow, whichis a mesodermal derivative. The bone marrow stemcells may then differentiate into another mesodermallyderived tissue such as skeletal muscle [28, 43],cardiac muscle [51, 71] or liver [4, 54, 97].Alternatively, adult stem cells may differentiate into atissue that—during normal embryonic development—wouldarise from a different germ layer. Forexample, bone marrow-derived cells may differentiateinto neural tissue, which is derived from embryonicectoderm [15, 65]. And—reciprocally—neural stemcell lines cultured from adult brain tissue may differentiateto form hematopoietic cells [13], or even giverise to many different cell types in a chimeric embryo[17]. In both cases cited above, the cells would bedeemed to show plasticity, but in the case of bonemarrow stem cells generating brain cells, the findingis less predictable.In order to study plasticity within and across germlayer lines, the researcher must be sure that he/she isusing only one kind of adult stem cell. The vast majorityof experiments on plasticity have been conductedwith adult stem cells derived either from the bonemarrow or the brain. The bone marrow-derived cellsare sometimes sorted—using a panel of surfacemarkers—into populations of hematopoietic stemcells or bone marrow stromal cells [46, 54, 71]. TheHSCs may be highly purified or partially purified,depending on the conditions used. Another way toseparate population of bone marrow cells is by fractionationto yield cells that adhere to a growth substrate(stromal cells) or do not adhere (hematopoieticcells) [28].To study plasticity of stem cells derived from the brain,the researcher must overcome several problems.<strong>Stem</strong> cells from the central nervous system (CNS),26
The Adult <strong>Stem</strong> CellLiverBrainCNS stem cellsBonemarrowSkeletalmuscleBoneBloodcellFat cellBlood vesselBone marrowstromal cellEpithelialcell© 2001 Terese Winslow, Lydia Kibiuk, Caitlin DuckwallCardiac muscleFigure 4.2. Preliminary Evidence of Plasticity Among Nonhuman Adult <strong>Stem</strong> <strong>Cells</strong>.NeuronGlial cell27
The Adult <strong>Stem</strong> Cellunlike bone marrow cells, do not occur in a single,accessible location. Instead, they are scattered inthree places, at least in rodent brain—the tissuearound the lateral ventricles in the forebrain, a migratorypathway for the cells that leads from the ventriclesto the olfactory bulbs, and the hippocampus.Many of the experiments with CNS stem cells involvethe formation of neurospheres, round aggregates ofcells that are sometimes clonally derived. But it is notpossible to observe cells in the center of a neurosphere,so to study plasticity in vitro, the cells areusually dissociated and plated in monolayers. Tostudy plasticity in vivo, the cells may be dissociatedbefore injection into the circulatory system of therecipient animal [13], or injected as neurospheres[17].What is the Evidence for Plasticity?The differentiated cell types that result from plasticityare usually reported to have the morphological characteristicsof the differentiated cells and to displaytheir characteristic surface markers. In reports thattransplanted adult stem cells show plasticity in vivo,the stem cells typically are shown to have integratedinto a mature host tissue and assumed at least someof its characteristics [15, 28, 51, 65, 71]. Many plasticityexperiments involve injury to a particular tissue,which is intended to model a particular humandisease or injury [13, 54, 71]. However, there is limitedevidence to date that such adult stem cells cangenerate mature, fully functional cells or that the cellshave restored lost function in vivo [54]. Most of thestudies that show the plasticity of adult stem cellsinvolve cells that are derived from the bone marrow[15, 28, 54, 65, 77] or brain [13, 17]. To date, adultstem cells are best characterized in these two tissues,which may account for the greater number of plasticitystudies based on bone marrow and brain.Collectively, studies on plasticity suggest that stemcell populations in adult mammals are not fixedentities, and that after exposure to a new environment,they may be able to populate other tissuesand possibly differentiate into other cell types.It is not yet possible to say whether plasticity occursnormally in vivo. Some scientists think it may [14, 64],but as yet there is no evidence to prove it. Also, it isnot yet clear to what extent plasticity can occur inexperimental settings, and how—or whether—thephenomenon can be harnessed to generate tissuesthat may be useful for therapeutic transplantation. Ifthe phenomenon of plasticity is to be used as a basisfor generating tissue for transplantation, the techniquesfor doing it will need to be reproducible andreliable (see Chapter 10. Assessing Human <strong>Stem</strong> CellSafety). In some cases, debate continues aboutobservations that adult stem cells yield cells of tissuetypes different than those from which they wereobtained [7, 68].EXPERIMENTAL EVIDENCE OF ADULTSTEM CELLS AND PLASTICITYAdult <strong>Stem</strong> <strong>Cells</strong> of the Nervous SystemMore than 30 years ago, Altman and Das showedthat two regions of the postnatal rat brain, the hippocampusand the olfactory bulb, contain dividingcells that become neurons [5, 6]. Despite thesereports, the prevailing view at the time was that nervecells in the adult brain do not divide. In fact, thenotion that stem cells in the adult brain can generateits three major cell types—astrocytes and oligodendrocytes,as well as neurons—was not accepted untilfar more recently. Within the past five years, a seriesof studies has shown that stem cells occur in theadult mammalian brain and that these cells cangenerate its three major cell lineages [35, 48, 63, 66,90, 96, 104] (see Chapter 8. Rebuilding the NervousSystem with <strong>Stem</strong> <strong>Cells</strong>).Today, scientists believe that stem cells in the fetaland adult brain divide and give rise to more stemcells or to several types of precursor cells. Neuronalprecursors (also called neuroblasts) divide and giverise to nerve cells (neurons), of which there are manytypes. Glial precursors give rise to astrocytes or oligodendrocytes.Astrocytes are a kind of glial cell, whichlend both mechanical and metabolic support forneurons; they make up 70 to 80 percent of the cellsof the adult brain. Oligodendrocytes make myelin,the fatty material that ensheathes nerve cell axonsand speeds nerve transmission. Under normal, in vivoconditions, neuronal precursors do not give rise toglial cells, and glial precursors do not give rise toneurons. In contrast, a fetal or adult CNS (centralnervous system—the brain and spinal cord) stem cellmay give rise to neurons, astrocytes, or oligodendrocytes,depending on the signals it receives and itsthree-dimensional environment within the brain tissue.28
The Adult <strong>Stem</strong> CellThere is now widespread consensus that the adultmammalian brain does contain stem cells. However,there is no consensus about how many populationsof CNS stem cells exist, how they may be related,and how they function in vivo. Because there are nomarkers currently available to identify the cells in vivo,the only method for testing whether a given populationof CNS cells contains stem cells is to isolate thecells and manipulate them in vitro, a process thatmay change their intrinsic properties [67].Despite these barriers, three groups of CNS stem cellshave been reported to date. All occur in the adultrodent brain and preliminary evidence indicates theyalso occur in the adult human brain. One groupoccupies the brain tissue next to the ventricles,regions known as the ventricular zone and the subventricularzone (see discussion below). The ventriclesare spaces in the brain filled with cerebrospinal fluid.During fetal development, the tissue adjacent to theventricles is a prominent region of actively dividingcells. By adulthood, however, this tissue is much smaller,although it still appears to contain stem cells [70].A second group of adult CNS stem cells, described inmice but not in humans, occurs in a streak of tissuethat connects the lateral ventricle and the olfactorybulb, which receives odor signals from the nose. Inrodents, olfactory bulb neurons are constantly beingreplenished via this pathway [59, 61]. A third possiblelocation for stem cells in adult mouse and humanbrain occurs in the hippocampus, a part of the brainthought to play a role in the formation of certain kindsof memory [27, 34].Central Nervous System <strong>Stem</strong> <strong>Cells</strong> in theSubventricular Zone. CNS stem cells found in the forebrainthat surrounds the lateral ventricles are heterogeneousand can be distinguished morphologically.Ependymal cells, which are ciliated, line the ventricles.Adjacent to the ependymal cell layer, in aregion sometimes designated as the subependymalor subventricular zone, is a mixed cell population thatconsists of neuroblasts (immature neurons) thatmigrate to the olfactory bulb, precursor cells, andastrocytes. Some of the cells divide rapidly, whileothers divide slowly. The astrocyte-like cells can beidentified because they contain glial fibrillary acidicprotein (GFAP), whereas the ependymal cells stainpositive for nestin, which is regarded as a marker ofneural stem cells. Which of these cells best qualifiesas a CNS stem cell is a matter of debate [76].A recent report indicates that the astrocytes thatoccur in the subventricular zone of the rodent brainact as neural stem cells. The cells with astrocytemarkers appear to generate neurons in vivo, asidentified by their expression of specific neuronalmarkers. The in vitro assay to demonstrate that theseastrocytes are, in fact, stem cells involves their abilityto form neurospheres—groupings of undifferentiatedcells that can be dissociated and coaxed to differentiateinto neurons or glial cells [25]. Traditionally, theseastrocytes have been regarded as differentiatedcells, not as stem cells and so their designation asstem cells is not universally accepted.A series of similar in vitro studies based on theformation of neurospheres was used to identify thesubependymal zone as a source of adult rodent CNSstem cells. In these experiments, single, candidatestem cells derived from the subependymal zone areinduced to give rise to neurospheres in the presenceof mitogens—either epidermal growth factor (EGF) orfibroblast growth factor-2 (FGF-2). The neurospheresare dissociated and passaged. As long as a mitogenis present in the culture medium, the cells continueforming neurospheres without differentiating. Somepopulations of CNS cells are more responsive to EGF,others to FGF [100]. To induce differentiation intoneurons or glia, cells are dissociated from theneurospheres and grown on an adherent surfacein serum-free medium that contains specific growthfactors. Collectively, the studies demonstrate that apopulation of cells derived from the adult rodentbrain can self-renew and differentiate to yield thethree major cell types of the CNS cells [41, 69,74, 102].Central Nervous System <strong>Stem</strong> <strong>Cells</strong> in the VentricularZone. Another group of potential CNS stem cells inthe adult rodent brain may consist of the ependymalcells themselves [47]. Ependymal cells, which areciliated, line the lateral ventricles. They have beendescribed as non-dividing cells [24] that function aspart of the blood-brain barrier [22]. The suggestionthat ependymal cells from the ventricular zone of theadult rodent CNS may be stem cells is thereforeunexpected. However, in a recent study, in which twomolecular tags—the fluorescent marker Dil, and anadenovirus vector carrying lacZ tags—were used tolabel the ependymal cells that line the entire CNSventricular system of adult rats, it was shown thatthese cells could, indeed, act as stem cells. A few29
The Adult <strong>Stem</strong> Celldays after labeling, fluorescent or lacZ + cells wereobserved in the rostral migratory stream (which leadsfrom the lateral ventricle to the olfactory bulb), andthen in the olfactory bulb itself. The labeled cells inthe olfactory bulb also stained for the neuronalmarkers III tubulin and Map2, which indicated thatependymal cells from the ventricular zone of theadult rat brain had migrated along the rostralmigratory stream to generate olfactory bulb neuronsin vivo [47].To show that Dil + cells were neural stem cells andcould generate astrocytes and oligodendrocytes aswell as neurons, a neurosphere assay was performedin vitro. Dil-labeled cells were dissociated from theventricular system and cultured in the presence ofmitogen to generate neurospheres. Most of theneurospheres were Dil + ; they could self-renew andgenerate neurons, astrocytes, and oligodendrocyteswhen induced to differentiate. Single, Dil + ependymalcells isolated from the ventricular zone could alsogenerate self-renewing neurospheres and differentiateinto neurons and glia.To show that ependymal cells can also divide in vivo,bromodeoxyuridine (BrdU) was administered in thedrinking water to rats for a 2- to 6-week period.Bromodeoxyuridine (BrdU) is a DNA precursor that isonly incorporated into dividing cells. Through a seriesof experiments, it was shown that ependymal cellsdivide slowly in vivo and give rise to a population ofprogenitor cells in the subventricular zone [47]. Adifferent pattern of scattered BrdU-labeled cells wasobserved in the spinal cord, which suggested thatependymal cells along the central canal of the cordoccasionally divide and give rise to nearby ependymalcells, but do not migrate away from the canal.Collectively, the data suggest that CNS ependymalcells in adult rodents can function as stem cells. Thecells can self-renew, and most proliferate via asymmetricaldivision. Many of the CNS ependymal cellsare not actively dividing (quiescent), but they can bestimulated to do so in vitro (with mitogens) or in vivo(in response to injury). After injury, the ependymal cellsin the spinal cord only give rise to astrocytes, not toneurons. How and whether ependymal cells from theventricular zone are related to other candidate populationsof CNS stem cells, such as those identified inthe hippocampus [34], is not known.Are ventricular and subventricular zone CNS stemcells the same population? These studies and otherleave open the question of whether cells that directlyline the ventricles—those in the ventricular zone—orcells that are at least a layer removed from thiszone—in the subventricular zone are the same populationof CNS stem cells. A new study, based on thefinding that they express different genes, confirmsearlier reports that the ventricular and subventricularzone cell populations are distinct. The new researchutilizes a technique called representational differenceanalysis, together with cDNA microarray analysis, tomonitor the patterns of gene expression in the complextissue of the developing and postnatal mousebrain. The study revealed the expression of a panel ofgenes known to be important in CNS development,such as L3-PSP (which encodes a phosphoserinephosphatase important in cell signaling), cyclin D2 (acell cycle gene), and ERCC-1 (which is important inDNA excision repair). All of these genes in the recentstudy were expressed in cultured neurospheres, aswell as the ventricular zone, the subventricular zone,and a brain area outside those germinal zones. Thisanalysis also revealed the expression of novel genessuch as A16F10, which is similar to a gene in anembryonic cancer cell line. A16F10 was expressed inneurospheres and at high levels in the subventricularzone, but not significantly in the ventricular zone.Interestingly, several of the genes identified in culturedneurospheres were also expressed in hematopoieticcells, suggesting that neural stem cells and bloodformingcells may share aspects of their geneticprograms or signaling systems [38]. This finding mayhelp explain recent reports that CNS stem cellsderived from mouse brain can give rise tohematopoietic cells after injection into irradiatedmice [13].Central Nervous System <strong>Stem</strong> <strong>Cells</strong> in theHippocampus. The hippocampus is one of the oldestparts of the cerebral cortex, in evolutionary terms,and is thought to play an important role in certainforms of memory. The region of the hippocampus inwhich stem cells apparently exist in mouse andhuman brains is the subgranular zone of the dentategyrus. In mice, when BrdU is used to label dividingcells in this region, about 50% of the labeled cellsdifferentiate into cells that appear to be dentate30
The Adult <strong>Stem</strong> Cellgyrus granule neurons, and 15% become glial cells.The rest of the BrdU-labeled cells do not have arecognizable phenotype [90]. Interestingly, many, ifnot all the BrdU-labeled cells in the adult rodenthippocampus occur next to blood vessels [33].In the human dentate gyrus, some BrdU-labeled cellsexpress NeuN, neuron-specific enolase, or calbindin,all of which are neuronal markers. The labeledneuron-like cells resemble dentate gyrus granulecells, in terms of their morphology (as they did inmice). Other BrdU-labeled cells express glial fibrillaryacidic protein (GFAP) an astrocyte marker. The studyinvolved autopsy material, obtained with familyconsent, from five cancer patients who had beeninjected with BrdU dissolved in saline prior to theirdeath for diagnostic purposes. The patients ranged inage from 57 to 72 years. The greatest number ofBrdU-labeled cells were identified in the oldestpatient, suggesting that new neuron formation in thehippocampus can continue late in life [27].Fetal Central Nervous System <strong>Stem</strong> <strong>Cells</strong>. Notsurprisingly, fetal stem cells are numerous in fetaltissues, where they are assumed to play an importantrole in the expansion and differentiation of all tissuesof the developing organism. Depending on thedevelopmental stage of an animal, fetal stem cellsand precursor cells—which arise from stem cells—may make up the bulk of a tissue. This is certainly truein the brain [48], although it has not been demonstratedexperimentally in many tissues.It may seem obvious that the fetal brain containsstem cells that can generate all the types of neuronsin the brain as well as astrocytes and oligodendrocytes,but it was not until fairly recently that the conceptwas proven experimentally. There has been along-standing question as to whether or not the samecell type gives rise to both neurons and glia. In studiesof the developing rodent brain, it has now beenshown that all the major cell types in the fetal brainarise from a common population of progenitor cells[20, 34, 48, 80, 108].Neural stem cells in the mammalian fetal brain areconcentrated in seven major areas: olfactory bulb,ependymal (ventricular) zone of the lateral ventricles(which lie in the forebrain), subventricular zone (nextto the ependymal zone), hippocampus, spinal cord,cerebellum (part of the hindbrain), and the cerebralcortex. Their number and pattern of developmentvary in different species. These cells appear torepresent different stem cell populations, rather thana single population of stem cells that is dispersed inmultiple sites. The normal development of the braindepends not only on the proliferation and differentiationof these fetal stem cells, but also on agenetically programmed process of selective celldeath called apoptosis [76].Little is known about stem cells in the human fetalbrain. In one study, however, investigators derivedclonal cell lines from CNS stem cells isolated from thediencephalon and cortex of human fetuses, 10.5weeks post-conception [103]. The study is unusual,not only because it involves human CNS stem cellsobtained from fetal tissue, but also because the cellswere used to generate clonal cell lines of CNS stemcells that generated neurons, astrocytes, andoligodendrocytes, as determined on the basis ofexpressed markers. In a few experiments describedas “preliminary,” the human CNS stem cells wereinjected into the brains of immunosuppressed ratswhere they apparently differentiated into neuron-likecells or glial cells.In a 1999 study, a serum-free growth medium thatincluded EGF and FGF2 was devised to grow thehuman fetal CNS stem cells. Although most of thecells died, occasionally, single CNS stem cells survived,divided, and ultimately formed neurospheresafter one to two weeks in culture. The neurospherescould be dissociated and individual cells replated.The cells resumed proliferation and formed new neurospheres,thus establishing an in vitro system that (likethe system established for mouse CNS neurospheres)could be maintained up to 2 years. Depending onthe culture conditions, the cells in the neurospherescould be maintained in an undifferentiated dividingstate (in the presence of mitogen), or dissociatedand induced to differentiate (after the removal ofmitogen and the addition of specific growth factorsto the culture medium). The differentiated cells consistedmostly of astrocytes (75%), some neurons (13%)and rare oligodendrocytes (1.2%). The neurons generatedunder these conditions expressed markersindicating they were GABAergic, [the major type ofinhibitory neuron in the mammalian CNS responsiveto the amino acid neurotransmitter, gammaaminobutyricacid (GABA)]. However, catecholaminelikecells that express tyrosine hydroxylase (TH, acritical enzyme in the dopamine-synthesis pathway)31
The Adult <strong>Stem</strong> Cellcould be generated, if the culture conditions werealtered to include different medium conditioned by arat glioma line (BB49). Thus, the report indicates thathuman CNS stem cells obtained from early fetusescan be maintained in vitro for a long time withoutdifferentiating, induced to differentiate into the threemajor lineages of the CNS (and possibly two kinds ofneurons, GABAergic and TH-positive), and engraft (inrats) in vivo [103].Central Nervous System Neural Crest <strong>Stem</strong> <strong>Cells</strong>.Neural crest cells differ markedly from fetal or adultneural stem cells. During fetal development, neuralcrest cells migrate from the sides of the neural tubeas it closes. The cells differentiate into a range oftissues, not all of which are part of the nervous system[56, 57, 91]. Neural crest cells form the sympatheticand parasympathetic components of the peripheralnervous system (PNS), including the network of nervesthat innervate the heart and the gut, all the sensoryganglia (groups of neurons that occur in pairs alongthe dorsal surface of the spinal cord), and Schwanncells, which (like oligodendrocytes in the CNS) makemyelin in the PNS. The non-neural tissues that arisefrom the neural crest are diverse. They populatecertain hormone-secreting glands—including theadrenal medulla and Type I cells in the carotidbody—pigment cells of the skin (melanocytes),cartilage and bone in the face and skull, andconnective tissue in many parts of the body [76].Thus, neural crest cells migrate far more extensivelythan other fetal neural stem cells during development,form mesenchymal tissues, most of whichdevelop from embryonic mesoderm as well as thecomponents of the CNS and PNS which arises fromembryonic ectoderm. This close link, in neural crestdevelopment, between ectodermally derived tissuesand mesodermally derived tissues accounts in partfor the interest in neural crest cells as a kind of stemcell. In fact, neural crest cells meet several criteria ofstem cells. They can self-renew (at least in the fetus)and can differentiate into multiple cells types, whichinclude cells derived from two of the three embryonicgerm layers [76].Recent studies indicate that neural crest cells persistlate into gestation and can be isolated from E14.5 ratsciatic nerve, a peripheral nerve in the hindlimb. Thecells incorporate BrdU, indicating that they are dividingin vivo. When transplanted into chick embryos, therat neural crest cells develop into neurons and glia,an indication of their stem cell-like properties [67].However, the ability of rat E14.5 neural crest cellstaken from sciatic nerve to generate nerve and glialcells in chick is more limited than neural crest cellsderived from younger, E10.5 rat embryos. At theearlier stage of development, the neural tube hasformed, but neural crest cells have not yet migratedto their final destinations. Neural crest cells fromearly developmental stages are more sensitive tobone morphogenetic protein 2 (BMP2) signaling,which may help explain their greater differentiationpotential [106].<strong>Stem</strong> <strong>Cells</strong> in the Bone Marrow and BloodThe notion that the bone marrow contains stem cellsis not new. One population of bone marrow cells, thehematopoietic stem cells (HSCs), is responsible forforming all of the types of blood cells in the body.HSCs were recognized as a stem cells more than 40years ago [9, 99]. Bone marrow stromal cells—amixed cell population that generates bone, cartilage,fat, fibrous connective tissue, and the reticular networkthat supports blood cell formation—weredescribed shortly after the discovery of HSCs [30, 32,73]. The mesenchymal stem cells of the bonemarrow also give rise to these tissues, and mayconstitute the same population of cells as the bonemarrow stromal cells [78]. Recently, a population ofprogenitor cells that differentiates into endothelialcells, a type of cell that lines the blood vessels, wasisolated from circulating blood [8] and identified asoriginating in bone marrow [89]. Whether theseendothelial progenitor cells, which resemble theangioblasts that give rise to blood vessels duringembryonic development, represent a bona fidepopulation of adult bone marrow stem cells remainsuncertain. Thus, the bone marrow appears to containthree stem cell populations—hematopoietic stemcells, stromal cells, and (possibly) endothelialprogenitor cells (see Figure 4.3. Hematopoietic andStromal <strong>Stem</strong> Cell Differentiation).Two more apparent stem cell types have beenreported in circulating blood, but have not beenshown to originate from the bone marrow. Onepopulation, called pericytes, may be closely relatedto bone marrow stromal cells, although their originremains elusive [12]. The second population of bloodbornstem cells, which occur in four species of32
The Adult <strong>Stem</strong> CellBoneNatural killer(NK) cellLymphoidprogenitorcellT lymphocytesNeutrophilBasophilEosinophilB lymphocyteHematopoieticstem cellMultipotentialstem cellMyeloidprogenitorcellMonocyte/macrophagePlateletsRed blood cells© 2001 Terese Winslow, Lydia KibiukBonematrixOsteoclastPericyteBloodvesselStromalcellAdipocyteStromalstem cellBone (or cartilage)OsteoblastPre-osteoblastSkeletal muscle stem cell?Hepatocyte stem cell?Lining cellOsteocyteHematopoieticsupportive stromaHematopoieticstem cellMarrowadipocyteFigure 4.3. Hematopoietic and Stromal <strong>Stem</strong> Cell Differentiation.animals tested—guinea pigs, mice, rabbits, andhumans—resemble stromal cells in that they cangenerate bone and fat [53].Hematopoietic <strong>Stem</strong> <strong>Cells</strong>. Of all the cell types in thebody, those that survive for the shortest period of timeare blood cells and certain kinds of epithelial cells.For example, red blood cells (erythrocytes), whichlack a nucleus, live for approximately 120 days in thebloodstream. The life of an animal literally dependson the ability of these and other blood cells to bereplenished continuously. This replenishment processoccurs largely in the bone marrow, where HSCsreside, divide, and differentiate into all the blood celltypes. Both HSCs and differentiated blood cells cyclefrom the bone marrow to the blood and back again,under the influence of a barrage of secreted factorsthat regulate cell proliferation, differentiation, andmigration (see Chapter 5. Hematopoietic <strong>Stem</strong> <strong>Cells</strong>).HSCs can reconstitute the hematopoietic system ofmice that have been subjected to lethal doses ofradiation to destroy their own hematopoietic systems.This test, the rescue of lethally irradiated mice, hasbecome a standard by which other candidate stemcells are measured because it shows, withoutquestion, that HSCs can regenerate an entire tissuesystem—in this case, the blood [9, 99]. HSCs were firstproven to be blood-forming stem cells in a series ofexperiments in mice; similar blood-forming stem cellsoccur in humans. HSCs are defined by their ability toself-renew and to give rise to all the kinds of bloodcells in the body. This means that a single HSC iscapable of regenerating the entire hematopoieticsystem, although this has been demonstrated only afew times in mice [72].Over the years, many combinations of surface markershave been used to identify, isolate, and purifyHSCs derived from bone marrow and blood.Undifferentiated HSCs and hematopoietic progenitorcells express c-kit, CD34, and H-2K. These cells usuallylack the lineage marker Lin, or express it at very lowlevels (Lin –/low ). And for transplant purposes, cells thatare CD34 + Thy1 + Lin – are most likely to contain stemcells and result in engraftment.33
The Adult <strong>Stem</strong> CellTwo kinds of HSCs have been defined. Long-termHSCs proliferate for the lifetime of an animal. Inyoung adult mice, an estimated 8 to 10 % oflong-term HSCs enter the cell cycle and divide eachday. Short-term HSCs proliferate for a limited time,possibly a few months. Long-term HSCs have highlevels of telomerase activity. Telomerase is an enzymethat helps maintain the length of the ends of chromosomes,called telomeres, by adding on nucleotides.Active telomerase is a characteristic of undifferentiated,dividing cells and cancer cells. Differentiated,human somatic cells do not show telomerase activity.In adult humans, HSCs occur in the bone marrow,blood, liver, and spleen, but are extremely rare in anyof these tissues. In mice, only 1 in 10,000 to 15,000bone marrow cells is a long-term HSC [105].Short-term HSCs differentiate into lymphoid andmyeloid precursors, the two classes of precursors forthe two major lineages of blood cells. Lymphoid precursorsdifferentiate into T cells, B cells, and naturalkiller cells. The mechanisms and pathways that leadto their differentiation are still being investigated [1, 2].Myeloid precursors differentiate into monocytes andmacrophages, neutrophils, eosinophils, basophils,megakaryocytes, and erythrocytes [3]. In vivo, bonemarrow HSCs differentiate into mature, specializedblood cells that cycle constantly from the bonemarrow to the blood, and back to the bone marrow[26]. A recent study showed that short-term HSCs area heterogeneous population that differ significantly interms of their ability to self-renew and repopulate thehematopoietic system [42].Attempts to induce HSC to proliferate in vitro—onmany substrates, including those intended to mimicconditions in the stroma—have frustrated scientists formany years. Although HSCs proliferate readily in vivo,they usually differentiate or die in vitro [26]. Thus,much of the research on HSCs has been focused onunderstanding the factors, cell-cell interactions, andcell-matrix interactions that control their proliferationand differentiation in vivo, with the hope that similarconditions could be replicated in vitro. Many of thesoluble factors that regulate HSC differentiation in vivoare cytokines, which are made by different cell typesand are then concentrated in the bone marrow bythe extracellular matrix of stromal cells—the sites ofblood formation [45, 107]. Two of the most-studiedcytokines are granulocyte-macrophage colony-stimulatingfactor (GM-CSF) and interleukin-3 (IL-3) [40, 81].Also important to HSC proliferation and differentiationare interactions of the cells with adhesion moleculesin the extracellular matrix of the bone marrow stroma[83, 101, 110].Bone Marrow Stromal <strong>Cells</strong>. Bone marrow (BM) stromalcells have long been recognized for playing animportant role in the differentiation of mature bloodcells from HSCs (see Figure 4.3. Hematopoietic andStromal <strong>Stem</strong> Cell Differentiation). But stromal cellsalso have other important functions [30, 31]. In additionto providing the physical environment in whichHSCs differentiate, BM stromal cells generate cartilage,bone, and fat. Whether stromal cells are bestclassified as stem cells or progenitor cells for these tissuesis still in question. There is also a question as towhether BM stromal cells and so-called mesenchymalstem cells are the same population [78].BM stromal cells have many features that distinguishthem from HSCs. The two cell types are easy to separatein vitro. When bone marrow is dissociated, andthe mixture of cells it contains is plated at low density,the stromal cells adhere to the surface of the culturedish, and the HSCs do not. Given specific in vitro conditions,BM stromal cells form colonies from a singlecell called the colony forming unit-F (CFU-F). Thesecolonies may then differentiate as adipocytes ormyelosupportive stroma, a clonal assay that indicatesthe stem cell-like nature of stromal cells. Unlike HSCs,which do not divide in vitro (or proliferate only to alimited extent), BM stromal cells can proliferate for upto 35 population doublings in vitro [16]. They growrapidly under the influence of such mitogens asplatelet-derived growth factor (PDGF), epidermalgrowth factor (EGF), basic fibroblast growth factor(bFGF), and insulin-like growth factor-1 (IGF-1) [12].To date, it has not been possible to isolate a populationof pure stromal cells from bone marrow. Panels ofmarkers used to identify the cells include receptors forcertain cytokines (interleukin-1, 3, 4, 6, and 7) receptorsfor proteins in the extracellular matrix, (ICAM-1and 2, VCAM-1, the alpha-1, 2, and 3 integrins, andthe beta-1, 2, 3 and 4 integrins), etc. [64]. Despite theuse of these markers and another stromal cell markercalled Stro-1, the origin and specific identity of stromalcells have remained elusive. Like HSCs, BMstromal cells arise from embryonic mesoderm duringdevelopment, although no specific precursor or stemcell for stromal cells has been isolated and identified.34
The Adult <strong>Stem</strong> CellOne theory about their origin is that a common kindof progenitor cell—perhaps a primordial endothelialcell that lines embryonic blood vessels—gives rise toboth HSCs and to mesodermal precursors. The lattermay then differentiate into myogenic precursors (thesatellite cells that are thought to function as stemcells in skeletal muscle), and the BM stromal cells[10].In vivo, the differentiation of stromal cells into fat andbone is not straightforward. Bone marrow adipocytesand myelosupportive stromal cells—both of whichare derived from BM stromal cells—may be regardedas interchangeable phenotypes [10, 11]. Adipocytesdo not develop until postnatal life, as the bonesenlarge and the marrow space increases to accommodateenhanced hematopoiesis. When the skeletonstops growing, and the mass of HSCs decreasesin a normal, age-dependent fashion, BM stromal cellsdifferentiate into adipocytes, which fill the extraspace. New bone formation is obviously greaterduring skeletal growth, although bone “turns over”throughout life. Bone forming cells are osteoblasts,but their relationship to BM stromal cells is not clear.New trabecular bone, which is the inner region ofbone next to the marrow, could logically developfrom the action of BM stromal cells. But the outsidesurface of bone also turns over, as does bone next tothe Haversian system (small canals that form concentricrings within bone). And neither of these surfaces isin contact with BM stromal cells [10, 11].Adult <strong>Stem</strong> <strong>Cells</strong> in Other TissuesIt is often difficult—if not impossible—to distinguishadult, tissue-specific stem cells from progenitor cells.With that caveat in mind, the following summaryidentifies reports of stem cells in various adult tissues.Endothelial Progenitor <strong>Cells</strong>. Endothelial cells line theinner surfaces of blood vessels throughout the body,and it has been difficult to identify specific endothelialstem cells in either the embryonic or the adultmammal. During embryonic development, just aftergastrulation, a kind of cell called the hemangioblast,which is derived from mesoderm, is presumed to bethe precursor of both the hematopoietic andendothelial cell lineages. The embryonic vasculatureformed at this stage is transient and consists of bloodislands in the yolk sac. But hemangioblasts, per se,have not been isolated from the embryo and theirexistence remains in question. The process of formingnew blood vessels in the embryo is called vasculogenesis.In the adult, the process of forming blood vesselsfrom pre-existing blood vessels is called angiogenesis[50].Evidence that hemangioblasts do exist comes fromstudies of mouse embryonic stem cells that aredirected to differentiate in vitro. These studies haveshown that a precursor cell derived from mouse EScells that express Flk-1 [the receptor for vascularendothelial growth factor (VEGF) in mice] can giverise to both blood cells and blood vessel cells [88,109]. Both VEGF and fibroblast growth factor-2 (FGF-2)play critical roles in endothelial cell differentiationin vivo [79].Several recent reports indicate that the bone marrowcontains cells that can give rise to new blood vesselsin tissues that are ischemic (damaged due to thedeprivation of blood and oxygen) [8, 29, 49, 94]. Butit is unclear from these studies what cell type(s) in thebone marrow induced angiogenesis. In a study whichsought to address that question, researchers foundthat adult human bone marrow contains cells thatresemble embryonic hemangioblasts, and maytherefore be called endothelial stem cells.In more recent experiments, human bone marrowderivedcells were injected into the tail veins of ratswith induced cardiac ischemia. The human cellsmigrated to the rat heart where they generated newblood vessels in the infarcted muscle (a process akinto vasculogenesis), and also induced angiogenesis.The candidate endothelial stem cells are CD34 + (amarker for HSCs), and they express the transcriptionfactor GATA-2 [51]. A similar study using transgenicmice that express the gene for enhanced green fluorescentprotein (which allows the cells to be tracked),showed that bone-marrow-derived cells could repopulatean area of infarcted heart muscle in mice, andgenerate not only blood vessels, but also cardiomyocytesthat integrated into the host tissue [71] (seeChapter 9. Can <strong>Stem</strong> <strong>Cells</strong> Repair a Damaged Heart?).And, in a series of experiments in adult mammals,progenitor endothelial cells were isolated fromperipheral blood (of mice and humans) by using antibodiesagainst CD34 and Flk-1, the receptor for VEGF.The cells were mononuclear blood cells (meaningthey have a nucleus) and are referred to as MB CD34+cells and MB Flk1+ cells. When plated in tissue-culture35
The Adult <strong>Stem</strong> Celldishes, the cells attached to the substrate, becamespindle-shaped, and formed tube-like structures thatresemble blood vessels. When transplanted into miceof the same species (autologous transplants) withinduced ischemia in one limb, the MB CD34+ cellspromoted the formation of new blood vessels [8].Although the adult MB CD34+ and MB Flk1+ cells functionin some ways like stem cells, they are usuallyregarded as progenitor cells.Skeletal Muscle <strong>Stem</strong> <strong>Cells</strong>. Skeletal muscle, like thecardiac muscle of the heart and the smooth musclein the walls of blood vessels, the digestive system,and the respiratory system, is derived from embryonicmesoderm. To date, at least three populations ofskeletal muscle stem cells have been identified:satellite cells, cells in the wall of the dorsal aorta, andso-called “side population” cells.Satellite cells in skeletal muscle were identified 40years ago in frogs by electron microscopy [62], andthereafter in mammals [84]. Satellite cells occur onthe surface of the basal lamina of a mature musclecell, or myofiber. In adult mammals, satellite cellsmediate muscle growth [85]. Although satellite cellsare normally non-dividing, they can be triggered toproliferate as a result of injury, or weight-bearingexercise. Under either of these circumstances, musclesatellite cells give rise to myogenic precursor cells,which then differentiate into the myofibrils that typifyskeletal muscle. A group of transcription factorscalled myogenic regulatory factors (MRFs) playimportant roles in these differentiation events. The socalledprimary MRFs, MyoD and Myf5, help regulatemyoblast formation during embryogenesis. The secondaryMRFs, myogenin and MRF4, regulate the terminaldifferentiation of myofibrils [86].With regard to satellite cells, scientists have beenaddressing two questions. Are skeletal muscle satellitecells true adult stem cells or are they instead precursorcells? Are satellite cells the only cell type that canregenerate skeletal muscle. For example, a recentreport indicates that muscle stem cells may alsooccur in the dorsal aorta of mouse embryos, andconstitute a cell type that gives rise both to musclesatellite cells and endothelial cells. Whether the dorsalaorta cells meet the criteria of a self-renewing musclestem cell is a matter of debate [21].Another report indicates that a different kind of stemcell, called an SP cell, can also regenerate skeletalmuscle may be present in muscle and bone marrow.SP stands for a side population of cells that can beseparated by fluorescence-activated cell sortinganalysis. Intravenously injecting these muscle-derivedstem cells restored the expression of dystrophin inmdx mice. Dystrophin is the protein that is defectivein people with Duchenne’s muscular dystrophy; mdxmice provide a model for the human disease.Dystrophin expression in the SP cell-treated mice waslower than would be needed for clinical benefit.Injection of bone marrow- or muscle-derived SP cellsinto the dystrophic muscle of the mice yieldedequivocal results that the transplanted cells had integratedinto the host tissue. The authors conclude thata similar population of SP stem cells can be derivedfrom either adult mouse bone marrow or skeletalmuscle, and suggest “there may be some directrelationship between bone marrow-derived stem cellsand other tissue- or organ-specific cells” [43]. Thus,stem cell or progenitor cell types from variousmesodermally-derived tissues may be able to generateskeletal muscle.Epithelial Cell Precursors in the Skin and DigestiveSystem. Epithelial cells, which constitute 60 percent ofthe differentiated cells in the body are responsible forcovering the internal and external surfaces of thebody, including the lining of vessels and other cavities.The epithelial cells in skin and the digestive tractare replaced constantly. Other epithelial cell populations—inthe ducts of the liver or pancreas, forexample—turn over more slowly. The cell populationthat renews the epithelium of the small intestineoccurs in the intestinal crypts, deep invaginations inthe lining of the gut. The crypt cells are oftenregarded as stem cells; one of them can give riseto an organized cluster of cells called a structuralproliferativeunit [93].The skin of mammals contains at least three populationsof epithelial cells: epidermal cells, hair folliclecells, and glandular epithelial cells, such as those thatmake up the sweat glands. The replacement patternsfor epithelial cells in these three compartments differ,and in all the compartments, a stem cell populationhas been postulated. For example, stem cells in thebulge region of the hair follicle appear to give rise tomultiple cell types. Their progeny can migrate downto the base of the follicle where they become matrixcells, which may then give rise to different cell typesin the hair follicle, of which there are seven [39]. The36
The Adult <strong>Stem</strong> Cellbulge stem cells of the follicle may also give rise tothe epidermis of the skin [95].Another population of stem cells in skin occurs in thebasal layer of the epidermis. These stem cells proliferatein the basal region, and then differentiate as theymove toward the outer surface of the skin. The keratinocytesin the outermost layer lack nuclei and actas a protective barrier. A dividing skin stem cell candivide asymmetrically to produce two kinds of daughtercells. One is another self-renewing stem cell. Thesecond kind of daughter cell is an intermediate precursorcell which is then committed to replicate a fewtimes before differentiating into keratinocytes. Selfrenewingstem cells can be distinguished from thisintermediate precusor cell by their higher level of 1integrin expression, which signals keratinocytes to proliferatevia a mitogen-activated protein (MAP) kinase[112]. Other signaling pathways include that triggeredby -catenin, which helps maintain the stem-cellstate [111], and the pathway regulated by the oncoproteinc-Myc, which triggers stem cells to give rise totransit amplifying cells [36].<strong>Stem</strong> <strong>Cells</strong> in the Pancreas and Liver. The status ofstem cells in the adult pancreas and liver is unclear.During embryonic development, both tissues arisefrom endoderm. A recent study indicates that asingle precursor cell derived from embryonic endodermmay generate both the ventral pancreas andthe liver [23]. In adult mammals, however, both thepancreas and the liver contain multiple kinds ofdifferentiated cells that may be repopulated orregenerated by multiple types of stem cells. In thepancreas, endocrine (hormone-producing) cellsoccur in the islets of Langerhans. They include thebeta cells (which produce insulin), the alpha cells(which secrete glucagon), and cells that release thepeptide hormones somatostatin and pancreaticpolypeptide. <strong>Stem</strong> cells in the adult pancreas arepostulated to occur in the pancreatic ducts or in theislets themselves. Several recent reports indicate thatstem cells that express nestin—which is usuallyregarded as a marker of neural stem cells—cangenerate all of the cell types in the islets [60, 113](see Chapter 7. <strong>Stem</strong> <strong>Cells</strong> and Diabetes).The identity of stem cells that can repopulate the liverof adult mammals is also in question. Recent studiesin rodents indicate that HSCs (derived frommesoderm) may be able to home to liver after it isdamaged, and demonstrate plasticity in becominginto hepatocytes (usually derived from endoderm)[54, 77, 97]. But the question remains as to whethercells from the bone marrow normally generate hepatocytesin vivo. It is not known whether this kind ofplasticity occurs without severe damage to the liver orwhether HSCs from the bone marrow generate ovalcells of the liver [18]. Although hepatic oval cells existin the liver, it is not clear whether they actually generatenew hepatocytes [87, 98]. Oval cells may arisefrom the portal tracts in liver and may give rise toeither hepatocytes [19, 55] and to the epithelium ofthe bile ducts [37, 92]. Indeed, hepatocytes themselves,may be responsible for the well-know regenerativecapacity of liver.SUMMARYWhat Do We Know About Adult <strong>Stem</strong> <strong>Cells</strong>?• Adult stem cells can proliferate without differentiatingfor a long period (a characteristic referredto as long-term self-renewal), and they can giverise to mature cell types that have characteristicshapes and specialized functions.• Some adult stem cells have the capability todifferentiate into tissues other than the ones fromwhich they originated; this is referred to asplasticity.• Adult stem cells are rare. Often they are difficultto identify and their origins are not known.Current methods for characterizing adult stemcells are dependent on determining cell surfacemarkers and observations about their differentiationpatterns in test tubes and culture dishes.• To date, published scientific literature indicatesthat adult stem cells have been derived frombrain, bone marrow, peripheral blood, dentalpulp, spinal cord, blood vessels, skeletal muscle,epithelia of the skin and digestive system,cornea, retina, liver, and pancreas; thus, adultstem cells have been found in tissues thatdevelop from all three embryonic germ layers.• Hematopoietic stem cells from bone marrow arethe most studied and used for clinical applicationsin restoring various blood and immunecomponents to the bone marrow via transplantation.There are at least two other populations ofadult stem cells that have been identified frombone marrow and blood.37
The Adult <strong>Stem</strong> Cell• Several populations of adult stem cells havebeen identified in the brain, particularly thehippocampus. Their function is unknown.Proliferation and differentiation of brain stem cellsare influenced by various growth factors.• There are now several reports of adult stem cellsin other tissues (muscle, blood, and fat) thatdemonstrate plasticity. Very few publishedresearch reports on plasticity of adult stem cellshave, however, included clonality studies. That is,there is limited evidence that a single adult stemcell or genetically identical line of adult stemcells demonstrates plasticity.• Rarely have experiments that claim plasticitydemonstrated that the adult stem cells havegenerated mature, fully functional cells or thatthe cells have restored lost function in vivo.What Do We Need to Know About Adult <strong>Stem</strong> <strong>Cells</strong>?• What are the sources of adult stem cells in thebody? Are they “leftover” embryonic stem cells,or do they arise in some other way? And if thelatter is true—which seems to be the case—exactly how do adult stem cells arise, andwhy do they remain in an undifferentiatedstate, when all the cells around them havedifferentiated?• Is it possible to manipulate adult stem cells toincrease their ability to proliferate in vitro, so thatadult stem cells can be used as a sufficientsource of tissue for transplants?• How many kinds of adult stem cells exist, and inwhich tissues do they exist? Evidence is accumulatingthat, although they occur in smallnumbers, adult stem cells are present in manydifferentiated tissues.• What is the best evidence that adult stem cellsshow plasticity and generate cell types of othertissues?• Is it possible to manipulate adult stem cells toincrease their ability to proliferate in vitro so thatadult stem cells can be used as a sufficientsource of tissue for transplants?• Is there a universal stem cell? An emergingconcept is that, in adult mammals, there maybe a population of “universal” stem cells.Although largely theoretical, the concept hassome experimental basis. A candidate, universaladult stem cell may be one that circulates inthe blood stream, can escape from the blood,and populate various adult tissues. In more thanone experimental system, researchers havenoted that dividing cells in adult tissues oftenappear near a blood vessel, such as candidatestem cells in the hippocampus, a region of thebrain [75].• Do adult stem cells exhibit plasticity as a normalevent in vivo? If so, is this true of all adult stemcells? What are the signals that regulate theproliferation and differentiation of stem cells thatdemonstrate plasticity?REFERENCES1. Akashi, K., Traver, D., Kondo, M., and Weissman, I.L. (1999).Lymphoid development from hematopoietic stem cells. Int.J. Hematol. 69, 217-226.2. Akashi, K., Kondo, M., Cheshier, S., Shizuru, J., Gandy, K.,Domen, J., Mebius, R., Traver, D., and Weissman, I.L. (1999).Lymphoid development from stem cells and the commonlymphocyte progenitors. Cold Spring Harb. Symp. Quant.Biol. 64, 1-12.3. Akashi, K., Traver, D., Miyamoto, T., and Weissman, I.L.(2000). A clonogenic common myeloid progenitor thatgives rise to all myeloid lineages. Nature. 404, 193-197.4. Alison, M.R., Poulsom, R., Jeffery, R., Dhillon, A.P., Quaglia,A., Jacob, J., Novelli, M., Prentice, G., Williamson, J., andWright, N.A. (2000). Hepatocytes from non-hepatic adultstem cells. Nature. 406, 257.5. Altman, J. and Das, G.D. (1965). Autoradiographic and histologicalevidence of postnatal hippocampal neurogenesisin rats. J. Comp. Neurol. 124, 319-335.6. Altman, J. (1969). Autoradiographic and histological studiesof postnatal neurogenesis. IV. Cell proliferation and migrationin the anterior forebrain, with special reference to persistingneurogenesis in the olfactory bulb. J. Comp. Neurol.137, 433-457.7. Anderson, D.J., Gage, F.H., and Weissman, I.L. (2001). Canstem cells cross lineage boundaries? Nat. Med. 7, 393-395.8. Asahara, T., Murohara, T., Sullivan, A., Silver, M., van der ZeeR., Li, T., Witzenbichler, B., Schatteman, G., and Isner, J.M.(1997). Isolation of putative progenitor endothelial cells forangiogenesis. Science. 275, 964-967.9. Becker, A.J., McCullough, E.A., and Till, J.E. (1963).Cytological demonstration of the clonal nature of spleencolonies derived from transplanted mouse marrow cells.Nature. 197, 452-454.10. Bianco, P. and Cossu, G. (1999). Uno, nessuno e centomila:searching for the identity of mesodermal progenitors. Exp.Cell Res. 251, 257-263.38
The Adult <strong>Stem</strong> Cell11. Bianco, P., Riminucci, M., Kuznetsov, S., and Robey, P.G.(1999). Multipotential cells in the bone marrow stroma:regulation in the context of organ physiology. Crit. Rev.Eukaryotic. Gene Expr. 9, 159-173.12. Bianco, P., Riminucci, M., Gronthos, S., and Robey, P.G.(2001). Bone marrow stromal stem cells: nature, biology,and potential applications. <strong>Stem</strong> <strong>Cells</strong>. 19, 180-192.13. Bjornson, C.R., Rietze, R.L., Reynolds, B.A., Magli, M.C., andVescovi, A.L. (1999). Turning brain into blood: a hematopoieticfate adopted by adult neural stem cells in vivo.Science. 283, 534-537.14. Blau, H., personal communication.15. Brazelton, T.R., Rossi, F.M., Keshet, G.I., and Blau, H.M.(2000). From marrow to brain: expression of neuronalphenotypes in adult mice. Science. 290, 1775-1779.16. Bruder, S.P., Jaiswal, N., and Haynesworth, S.E. (1997).Growth kinetics, self-renewal, and the osteogenic potentialof purified human mesenchymal stem cells during extensivesubcultivation and following cryopreservation. J. Cell.Biochem. 64, 278-294.17. Clarke, D.L., Johansson, C.B., Wilbertz, J., Veress, B., Nilsson,E., Karlström, H., Lendahl, U., and Frisen, J. (2000).Generalized potential of adult neural stem cells. Science.288, 1660-1663.18. Crosby, H.A. and Strain, A.J. (2001). Adult liver stem cells:bone marrow, blood, or liver derived? Gut. 48, 153-154.19. Dabeva, M.D. and Shafritz, D.A. (1993). Activation, proliferation,and differentiation of progenitor cells into hepatocytesin the D-galactosamine model of liver regeneration. Am. J.Pathol. 143, 1606-1620.20. Davis, A.A. and Temple, S. (1994). A self-renewing multipotentialstem cell in embryonic rat cerebral cortex. Nature.372, 263-266.21. De Angelis, L., Berghella, L., Coletta, M., Lattanzi, L., Zanchi,M., Cusella-De Angelis, M.G., Ponzetto, C., and Cossu, G.(1999). Skeletal myogenic progenitors originating fromembryonic dorsal aorta coexpress endothelial and myogenicmarkers and contribute to postnatal muscle growthand regeneration. J. Cell Biol. 147, 869-877.22. Del Bigio, M.R. (1995). The ependyma: a protective barrierbetween brain and cerebrospinal fluid. Glia. 14, 1-13.23. Deutsch, G., Jung, J., Zheng, M., Lora, J., and Zaret, K.S.(2001). A bipotential precursor population for pancreas andliver within the embryonic endoderm. Development. 128,871-881.24. Doetsch, F., Garcia-Verdugo, J.M., and Alvarez-Buylla, A.(1997). Cellular composition and three-dimensional organizationof the subventricular germinal zone in the adultmammalian brain. J. Neurosci. 17, 5046-5061.25. Doetsch, F., Caille, I., Lim, D.A., Garcia-Verdugo, J.M., andAlvarez-Buylla, A. (1999). Subventricular zone astrocytes areneural stem cells in the adult mammalian brain. Cell. 97,703-716.26. Domen, J. and Weissman, I.L. (1999). Self-renewal, differentiationor death: regulation and manipulation ofhematopoietic stem cell fate. Mol. Med. Today. 5, 201-208.27. Eriksson, P.S., Perfilieva, E., Bjork-Eriksson, T., Alborn, A.M.,Nordborg, C., Peterson, D.A., and Gage, F.H. (1998).Neurogenesis in the adult human hippocampus. Nat. Med.4, 1313-1317.28. Ferrari, G., Cusella-De Angelis, G., Coletta, M., Paolucci, E.,Stornaiuolo, A., Cossu, G., and Mavilio, F. (1998). Muscleregeneration by bone marrow-derived myogenic progenitors.Science. 279, 1528-1530.29. Folkman, J. (1998). Therapeutic angiogenesis in ischemiclimbs. Circulation. 97, 1108-1110.30. Friedenstein, A.J., Piatetzky-Shapiro, I.I., and Petrakova, K.V.(1966). Osteogenesis in transplants of bone marrow cells.J. Embryol. Exp. Morphol. 16, 381-390.31. Friedenstein, A.J., Petrakova, K.V., Kurolesova, A.I., andFrolova, G.P. (1968). Heterotopic of bone marrow. Analysisof precursor cells for osteogenic and hematopoietictissues. Transplantation. 6, 230-247.32. Friedenstein, A.J., Chailakhjan, R.K., and Lalykina, K.S.(1970). The development of fibroblast colonies in monolayercultures of guinea-pig bone marrow and spleen cells.Cell Tissue Kinet. 3, 393-403.33. Gage, F., personal communication.34. Gage, F.H., Ray, J., and Fisher, L.J. (1995). Isolation, characterization,and use of stem cells from the CNS. Annu. Rev.Neurosci. 18, 159-192.35. Gage, F.H., Coates, P.W., Palmer, T.D., Kuhn, H.G., Fisher,L.J., Suhonen, J.O., Peterson, D.A., Suhr, S.T., and Ray, J.(1995). Survival and differentiation of adult neuronalprogenitor cells transplanted to the adult brain. Proc. Natl.Acad. Sci. U. S. A. 92, 11879-11883.36. Gandarillas, A. and Watt, F.M. (1997). c-Myc promotesdifferentiation of human epidermal stem cells. Genes Dev.11, 2869-2882.37. Germain, L., Noel, M., Gourdeau, H., and Marceau, N.(1988). Promotion of growth and differentiation of rat ductularoval cells in primary culture. Cancer Res. 48, 368-378.38. Geschwind, D.H., Ou, J., Easterday, M.C., Dougherty, J.D.,Jackson, R.L., Chen, Z., Antoine, H., Terskikh, A., Weissman,I.L., Nelson, S.F., and Kornblum, H.I. (2001). A genetic analysisof neural progenitor differentiation. Neuron. 29, 325-339.39. Ghazizadeh, S. and Taichman, L.B. (2001). Multiple classesof stem cells in cutaneous epithelium: a lineage analysis ofadult mouse skin. EMBO J. 20, 1215-1222.40. Gordon, M.Y., Riley, G.P., Watt, S.M., and Greaves, M.F.(1987). Compartmentalization of a haematopoietic growthfactor (GM-CSF) by glycosaminoglycans in the bonemarrow microenvironment. Nature. 326, 403-405.39
The Adult <strong>Stem</strong> Cell41. Gritti, A., Parati, E.A., Cova, L., Frolichsthal, P., Galli, R.,Wanke, E., Faravelli, L., Morassutti, D.J., Roisen, F., Nickel,D.D., and Vescovi, A.L. (1996). Multipotential stem cells fromthe adult mouse brain proliferate and self-renew inresponse to basic fibroblast growth factor. J. Neurosci. 16,1091-1100.42. Guenechea, G., Gan, O.I., Dorrell, C., and Dick, J.E. (2001).Distinct classes of human stem cells that differ in proliferativeand self-renewal potential. Nat. Immunol. 2, 75-82.43. Gussoni, E., Soneoka, Y., Strickland, C.D., Buzney, E.A., Khan,M.K., Flint, A.F., Kunkel, L.M., and Mulligan, R.C. (1999).Dystrophin expression in the mdx mouse restored by stemcell transplantation. Nature. 401, 390-394.44. Holtzer. H. (1978). Cell lineages, stem cells and the‘quantal’ cell cycle concept. In: <strong>Stem</strong> cells and tissuehomeostasis. Eds: B.I. Lord, C.S. Potten, and R.J. Cole.(Cambridge, New York: Cambridge University Press). 1-28.45. Hunt, P., Robertson, D., Weiss, D., Rennick, D., Lee, F., andWitte, O.N. (1987). A single bone marrow-derived stromalcell type supports the in vitro growth of early lymphoid andmyeloid cells. Cell. 48, 997-1007.46. Jackson, K., Majka SM, Wang H, Pocius J, Hartley CJ,Majesky MW, Entman ML, Michael LH, Hirschi KK, andGoodell MA (2001). Regeneration of ischemic cardiacmuscle and vascular endothelium by adult stem cells.J. Clin. Invest. 107, 1-8.47. Johansson, C.B., Momma, S., Clarke, D.L., Risling, M.,Lendahl, U., and Frisen, J. (1999). Identification of a neuralstem cell in the adult mammalian central nervous system.Cell. 96, 25-34.48. Johe, K.K., Hazel, T.G., Muller, T., Dugich-Djordjevic, M.M.,and McKay, R.D. (1996). Single factors direct the differentiationof stem cells from the fetal and adult central nervoussystem. Genes Dev. 10, 3129-3140.49. Kalka, C., Masuda, H., Takahashi, T., Kalka-Moll, W.M., Silver,M., Kearney, M., Li, T., Isner, J.M., and Asahara, T. (2000).Transplantation of ex vivo expanded endothelial progenitorcells for therapeutic neovascularization. Proc. Natl. Acad.Sci. U. S. A. 97, 3422-3427.50. Keller, G. (2001). The hemangioblast. Marshak, D.R.,Gardner, D.K., and Gottlieb, D. eds. (Cold Spring Harbor,New York: Cold Spring Harbor Laboratory Press). 329-348.51. Kocher, A.A., Schuster, M.D., Szabolcs, M.J., Takuma, S.,Burkhoff, D., Wang, J., Homma, S., Edwards, N.M., andItescu, S. (2001). Neovascularization of ischemic myocardiumby human bone-marrow-derived angioblastsprevents cardiomyocyte apoptosis, reduces remodelingand improves cardiac function. Nat. Med. 7, 430-436.52. Krause, D.S., Theise, N.D., Collector, M.I., Henegariu, O.,Hwang, S., Gardner, R., Neutzel, S., and Sharkis, S.J. (2001).Multi-organ, multi-lineage engraftment by a single bonemarrow-derived stem cell. Cell. 105, 369-377.53. Kuznetsov, S.A., Mankani, M.H., Gronthos, S., Satomura, K.,Bianco, P., and Robey P.G. (2001). Circulating skeletal stemcells. J. Cell Biol. 153, 1133-1140.54. Lagasse, E., Connors, H., Al Dhalimy, M., Reitsma, M.,Dohse, M., Osborne, L., Wang, X., Finegold, M., Weissman,I.L., and Grompe, M. (2000). Purified hematopoietic stemcells can differentiate into hepatocytes in vivo. Nat. Med. 6,1229-1234.55. Lazaro, C.A., Rhim, J.A., Yamada, Y., and Fausto, N. (1998).Generation of hepatocytes from oval cell precursors in culture.Cancer Res. 58, 5514-5522.56. Le Douarin, N.M. (1980). The ontogeny of the neural crest inavian embryo chimaeras. Nature. 286, 663-669.57. Le Douarin, N.M. and Kalcheim, C. (1999). The migration ofneural crest cells. In: The neural crest. (Cambridge, NewYork: Cambridge University Press). 23-59.58. Leblond, C.P. (1964). Classification of cell populations onthe basis of their proliferative behavior. National CancerInstitute. 14, 119-150.59. Lois, C. and Alvarez-Buylla, A. (1994). Long-distanceneuronal migration in the adult mammalian brain.Science. 264, 1145-1148.60. Lumelsky, N., Blondel, O., Laeng, P., Velasco, I., Ravin, R.,and McKay, R. (2001). Differentiation of Embryonic <strong>Stem</strong><strong>Cells</strong> to Insulin-Secreting Structures Similiar to PancreaticIslets. Science. 292, 1309-1599.61. Luskin, M.B. (1993). Restricted proliferation and migration ofpostnatally generated neurons derived from the forebrainsubventricular zone. Neuron. 11, 173-189.62. Mauro, A. (1961). Satellite cell of skeletal muscle fibers.J. Biophys. Biochem. Cytol. 9, 493-495.63. McKay, R. (1997). <strong>Stem</strong> cells in the central nervous system.Science. 276, 66-71.64. McKay, R., personal communication.65. Mezey, E., Chandross, K.J., Harta, G., Maki, R.A., andMcKercher, S.R. (2000). Turning blood into brain: cells bearingneuronal antigens generated in vivo from bone marrow.Science. 290, 1779-1782.66. Momma, S., Johansson, C.B., and Frisen, J. (2000). Get toknow your stem cells. Curr. Opin. Neurobiol. 10, 45-49.67. Morrison, S.J., White, P.M., Zock, C., and Anderson, D.J.(1999). Prospective identification, isolation by flow cytometry,and in vivo self-renewal of multipotent mammalianneural crest stem cells. Cell. 96, 737-749.68. Morrison, S.J. (2001). Neuronal differentiation: Proneuralgenes inhibit gliogenesis. Curr. Biol. 11, R349-R351.69. Morshead, C.M., Reynolds, B.A., Craig, C.G., McBurney,M.W., Staines, W.A., Morassutti, D., Weiss, S., and van der,K.D. (1994). Neural stem cells in the adult mammalianforebrain: a relatively quiescent subpopulation ofsubependymal cells. Neuron. 13, 1071-1082.70. Morshead, C.M. and van der Kooy, K.D. (2001). A new ‘spin’on neural stem cells? Curr. Opin. Neurobiol. 11, 59-65.40
The Adult <strong>Stem</strong> Cell102. Vescovi, A.L., Reynolds, B.A., Fraser, D.D., and Weiss, S.(1993). bFGF regulates the proliferative fate of unipotent(neuronal) and bipotent (neuronal/astroglial) EGFgeneratedCNS progenitor cells. Neuron. 11, 951-966.103. Vescovi, A.L., Gritti, A., Galli, R., and Parati, E.A. (1999).Isolation and intracerebral grafting of nontransformedmultipotential embryonic human CNS stem cells. J.Neurotrauma. 16, 689-693.104. Weiss, S. and van der Kooy D. (1998). CNS stem cells:where’s the biology (a.k.a. beef)? J. Neurobiol. 36,307-314.105. Weissman, I.L. (2000). <strong>Stem</strong> cells: units of development,units of regeneration, and units in evolution. Cell. 100,157-168.106. White, P.M., Morrison, S.J., Orimoto, K., Kubu, C.J., Verdi,J.M., and Anderson, D.J. (2001). Neural crest stem cellsundergo cell-intrinsic developmental changes in sensitivityto instructive differentiation signals. Neuron. 29, 57-71.107. Whitlock, C.A., Tidmarsh, G.F., Muller-Sieburg, C., andWeissman, I.L. (1987). Bone marrow stromal cell lines withlymphopoietic activity express high levels of a pre-B neoplasia-associatedmolecule. Cell. 48, 1009-1021.108. Williams, B.P., Read, J., and Price, J. (1991). The generationof neurons and oligodendrocytes from a common precursorcell. Neuron. 7, 685-693.109. Yamashita, J., Itoh, H., Hirashima, M., Ogawa, M.,Nishikawa, S., Yurugi, T., Naito, M., Nakao, K., andNishikawa, S. (2000). Flk1-positive cells derived fromembryonic stem cells serve as vascular progenitors.Nature. 408, 92-96.110. Zandstra, P.W., Lauffenburger, D.A., and Eaves, C.J. (2000).A ligand-receptor signaling threshold model of stem celldifferentiation control: a biologically conserved mechanismapplicable to hematopoiesis. Blood. 96, 1215-1222.111. Zhu, A.J. and Watt, F.M. (1999). beta-catenin signallingmodulates proliferative potential of human epidermal keratinocytesindependently of intercellular adhesion.Development. 126, 2285-2298.112. Zhu, A.J., Haase, I., and Watt, F.M. (1999). Signaling viabeta1 integrins and mitogen-activated protein kinasedetermines human epidermal stem cell fate in vitro. Proc.Natl. Acad. Sci. U. S. A. 96, 6728-6733.113. Zulewski, H., Abraham, E.J., Gerlach, M.J., Daniel, P.B.,Moritz, W., Muller, B., Vallejo, M., Thomas, M.K., andHabener, J.F. (2001). Multipotential nestin-positive stemcells isolated from adult pancreatic islets differentiate exvivo into pancreatic endocrine, exocrine, and hepaticphenotypes. Diabetes. 50, 521-533.42
5.HEMATOPOIETICSTEM CELLSWith more than 50 years of experience studyingblood-forming stem cells called hematopoietic stemcells, scientists have developed sufficient understandingto actually use them as a therapy. Currently, noother type of stem cell, adult, fetal or embryonic,has attained such status. Hematopoietic stem celltransplants are now routinely used to treat patientswith cancers and other disorders of the blood andimmune systems. Recently, researchers haveobserved in animal studies that hematopoietic stemcells appear to be able to form other kinds of cells,such as muscle, blood vessels, and bone. If this canbe applied to human cells, it may eventually bepossible to use hematopoietic stem cells to replacea wider array of cells and tissues than once thought.Despite the vast experience with hematopoietic stemcells, scientists face major roadblocks in expandingtheir use beyond the replacement of blood andimmune cells. First, hematopoietic stem cells areunable to proliferate (replicate themselves) anddifferentiate (become specialized to other cell types) invitro (in the test tube or culture dish). Second, scientistsdo not yet have an accurate method to distinguishstem cells from other cells recovered from the bloodor bone marrow. Until scientists overcome thesetechnical barriers, they believe it is unlikely thathematopoietic stem cells will be applied as cellreplacement therapy in diseases such as diabetes,Parkinson’s Disease, spinal cord injury, and many others.INTRODUCTIONBlood cells are responsible for constant maintenanceand immune protection of every cell type of thebody. This relentless and brutal work requires thatblood cells, along with skin cells, have the greatestpowers of self-renewal of any adult tissue.The stem cells that form blood and immune cells areknown as hematopoietic stem cells (HSCs). They areultimately responsible for the constant renewal ofblood—the production of billions of new blood cellseach day. Physicians and basic researchers haveknown and capitalized on this fact for more than 50years in treating many diseases. The first evidenceand definition of blood-forming stem cells camefrom studies of people exposed to lethal doses ofradiation in 1945.Basic research soon followed. After duplicatingradiation sickness in mice, scientists found they couldrescue the mice from death with bone marrowtransplants from healthy donor animals. In the early1960s, Till and McCulloch began analyzing the bonemarrow to find out which components were responsiblefor regenerating blood [56]. They defined whatremain the two hallmarks of an HSC: it can renewitself and it can produce cells that give rise to all thedifferent types of blood cells (see Chapter 4. TheAdult <strong>Stem</strong> Cell).WHAT IS A HEMATOPOIETICSTEM CELL?A hematopoietic stem cell is a cell isolated from theblood or bone marrow that can renew itself, candifferentiate to a variety of specialized cells, canmobilize out of the bone marrow into circulatingblood, and can undergo programmed cell death,called apoptosis—a process by which cells that aredetrimental or unneeded self-destruct.A major thrust of basic HSC research since the 1960shas been identifying and characterizing these stemcells. Because HSCs look and behave in culture likeordinary white blood cells, this has been a difficultchallenge and this makes them difficult to identify bymorphology (size and shape). Even today, scientistsmust rely on cell surface proteins, which serve, onlyroughly, as markers of white blood cells.43
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>Identifying and characterizing properties of HSCsbegan with studies in mice, which laid the groundworkfor human studies. The challenge is formidableas about 1 in every 10,000 to 15,000 bone marrowcells is thought to be a stem cell. In the blood streamthe proportion falls to 1 in 100,000 blood cells. To thisend, scientists began to develop tests for proving theself-renewal and the plasticity of HSCs.The “gold standard” for proving that a cell derivedfrom mouse bone marrow is indeed an HSC is stillbased on the same proof described above andused in mice many years ago. That is, the cells areinjected into a mouse that has received a dose ofirradiation sufficient to kill its own blood-producingcells. If the mouse recovers and all types of bloodcells reappear (bearing a genetic marker from thedonor animal), the transplanted cells are deemed tohave included stem cells.These studies have revealed that there appear to betwo kinds of HSCs. If bone marrow cells from thetransplanted mouse can, in turn, be transplanted toanother lethally irradiated mouse and restore itshematopoietic system over some months, they areconsidered to be long-term stem cells that arecapable of self-renewal. Other cells from bonemarrow can immediately regenerate all the differenttypes of blood cells, but under normal circumstancescannot renew themselves over the long term, andthese are referred to as short-term progenitor orprecursor cells. Progenitor or precursor cells are relativelyimmature cells that are precursors to a fullydifferentiated cell of the same tissue type. They arecapable of proliferating, but they have a limitedcapacity to differentiate into more than one cell typeas HSCs do. For example, a blood progenitor cellmay only be able to make a red blood cell (seeFigure 5.1. Hematopoietic and Stromal <strong>Stem</strong> CellDifferentiation).Harrison et al. write that short-term blood-progenitorcells in a mouse may restore hematopoiesis for threeto four months [36]. The longevity of short-term stemcells for humans is not firmly established. A true stemcell, capable of self-renewal, must be able to renewitself for the entire lifespan of an organism. It is theseBoneNatural killer(NK) cellLymphoidprogenitorcellT lymphocytesNeutrophilBasophilEosinophilB lymphocyteHematopoieticstem cellMultipotentialstem cellMyeloidprogenitorcellMonocyte/macrophagePlateletsRed blood cells© 2001 Terese Winslow, Lydia KibiukBonematrixOsteoclastPericyteBloodvesselStromalcellAdipocyteStromalstem cellBone (or cartilage)OsteoblastPre-osteoblastSkeletal muscle stem cell?Hepatocyte stem cell?Lining cellOsteocyteHematopoieticsupportive stromaHematopoieticstem cellMarrowadipocyteFigure 5.1. Hematopoietic and Stromal <strong>Stem</strong> Cell Differentiation.44
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>long-term replicating HSCs that are most importantfor developing HSC-based cell therapies. Unfortunately,to date, researchers cannot distinguish thelong-term from the short-term cells when they areremoved from the bloodstream or bone marrow.The central problem of the assays used to identifylong-term stem cells and short-term progenitor cells isthat they are difficult, expensive, and time-consumingand cannot be done in humans. A few assays arenow available that test cells in culture for their abilityto form primitive and long-lasting colonies of cells,but these tests are not accepted as proof that a cellis a long-term stem cell. Some genetically alteredmice can receive transplanted human HSCs to testthe cells’ self-renewal and hematopoietic capabilitiesduring the life of a mouse, but the relevance of thistest for the cells in humans—who may live fordecades—is open to question.The difficulty of HSC assays has contributed to twomutually confounding research problems: definitivelyidentifying the HSC and getting it to proliferate, orincrease its numbers, in a culture dish. More rapidresearch progress on characterizing and using HSCswould be possible if they could be readily grown inthe laboratory. Conversely, progress in identifyinggrowth conditions suitable for HSCs and getting thecells to multiply would move more quickly if scientistscould reliably and readily identify true HSCs.CAN CELL MARKERS BE USEDTO IDENTIFY HEMATOPOIETICSTEM CELLS?HSCs have an identity problem. First, the ones withlong-term replicating ability are rare. Second, thereare multiple types of stem cells. And, third, the stemcells look like many other blood or bone marrow cells.So how do researchers find the desired cell populations?The most common approach is throughmarkers that appear on the surface of cells. (For amore detailed discussion, see Appendix E.i. Markers:How Do Researchers Use Them to Identify <strong>Stem</strong> <strong>Cells</strong>?)These are useful, but not perfect tools for theresearch laboratory.In 1988, in an effort to develop a reliable means ofidentifying these cells, Irving Weissman and hiscollaborators focused attention on a set of proteinmarkers on the surface of mouse blood cells thatwere associated with increased likelihood that thecell was a long-term HSC [50]. Four years later, thelaboratory proposed a comparable set of markers forthe human stem cell [3]. Weissman proposes themarkers shown in Table 5.1 as the closest markers formouse and human HSCs [62].Table 5.1. Proposed cell-surface markers ofundifferentiated hematopoietic stem cells.Listed here are cell surface markers found on mouseand human hematopoietic stem cells as they exist intheir undifferentiated state in vivo and in vitro. As thesecells begin to develop as distinct cell lineages the cellsurface markers are no longer identified.MouseHumanCD34 low/- CD 34 +SCA-1 + CD59 +*Thy1 +/low Thy1 +CD38 +C-kit +CD38 low/-C-kit -/lowlin -* lin -*** Only one of a family of CD59 markers has thus far beenevaluated.** Lin- cells lack 13 to 14 different mature blood-lineagemarkers.Such cell markers can be tagged with monoclonalantibodies bearing a fluorescent label and culled outof bone marrow with fluorescence-activated cellsorting (FACS).The groups of cells thus sorted by surface markers areheterogeneous and include some cells that are true,long-term self-renewing stem cells, some shorter-termprogenitors, and some non-stem cells. Weissman’sgroup showed that as few as five genetically taggedcells, injected along with larger doses of stem cellsinto lethally irradiated mice, could establish themselvesand produce marked donor cells in all bloodcell lineages for the lifetime of the mouse. A singletagged cell could produce all lineages for as manyas seven weeks, and 30 purified cells were sufficientto rescue mice and fully repopulate the bone marrowwithout extra doses of backup cells to rescue themice [49]. Despite these efforts, researchers remaindivided on the most consistently expressed set of HSCmarkers [27, 32]. Connie Eaves of the University ofBritish Columbia says none of the markers are tied tounique stem cell functions or truly define the stemcell [14]. “Almost every marker I am aware of hasbeen shown to be fickle,” she says.45
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>More recently, Diane Krause and her colleagues atYale University, New York University, and Johns HopkinsUniversity, used a new technique to home in on a singlecell capable of reconstituting all blood cell lineagesof an irradiated mouse [27]. After marking bonemarrow cells from donor male mice with a nontoxicdye, they injected the cells into female recipientmice that had been given a lethal dose of radiation.Over the next two days, some of the injected cellsmigrated, or homed, to the bone marrow of therecipients and did not divide; when transplanted intoa second set of irradiated female mice, they eventuallyproved to be a concentrated pool of self-renewingstem cells. The cells also reconstituted blood production.The scientists estimate that their techniqueconcentrated the long-term stem cells 500 to 1,000-fold compared with bone marrow.WHAT ARE THE SOURCES OFHEMATOPOIETIC STEM CELLS?Bone MarrowThe classic source of hematopoietic stem cells (HSCs)is bone marrow. For more than 40 years, doctorsperformed bone marrow transplants by anesthetizingthe stem cell donor, puncturing a bone—typically ahipbone—and drawing out the bone marrow cellswith a syringe. About 1 in every 100,000 cells in themarrow is a long-term, blood-forming stem cell; othercells present include stromal cells, stromal stem cells,blood progenitor cells, and mature and maturingwhite and red blood cells.Peripheral BloodAs a source of HSCs for medical treatments, bonemarrow retrieval directly from bone is quickly fadinginto history. For clinical transplantation of humanHSCs, doctors now prefer to harvest donor cells fromperipheral, circulating blood. It has been known fordecades that a small number of stem and progenitorcells circulate in the bloodstream, but in the past 10years, researchers have found that they can coax thecells to migrate from marrow to blood in greaternumbers by injecting the donor with a cytokine, suchas granulocyte-colony stimulating factor (GCSF). Thedonor is injected with GCSF a few days before thecell harvest. To collect the cells, doctors insert anintravenous tube into the donor’s vein and pass hisblood through a filtering system that pulls out CD34 +white blood cells and returns the red blood cells tothe donor. Of the cells collected, just 5 to 20 percentwill be true HSCs. Thus, when medical researcherscommonly refer to peripherally harvested “stemcells,” this is something of a misnomer. As is true forbone marrow, the CD34 + cells are a mixture of stemcells, progenitors, and white blood cells of variousdegrees of maturity.In the past three years, the majority of autologous(where the donor and recipient are the same person)and allogeneic (where the donor and recipient aredifferent individuals) “bone marrow” transplants haveactually been white blood cells drawn from peripheralcirculation, not bone marrow. Richard Childs, an intramuralinvestigator at the NIH, says peripheral harvestof cells is easier on the donor—with minimal pain, noanesthesia, and no hospital stay—but also yieldsbetter cells for transplants [6]. Childs points to evidencethat patients receiving peripherally harvestedcells have higher survival rates than bone marrowrecipients do. The peripherally harvested cells containtwice as many HSCs as stem cells taken from bonemarrow and engraft more quickly. This meanspatients may recover white blood cells, platelets, andtheir immune and clotting protection several daysfaster than they would with a bone marrow graft.Scientists at Stanford report that highly purified,mobilized peripheral cells that have CD34 + andThy-1 + surface markers engraft swiftly and withoutcomplication in breast cancer patients receiving anautologous transplant of the cells after intensivechemotherapy [41].Umbilical Cord BloodIn the late 1980s and early 1990s, physicians beganto recognize that blood from the human umbilicalcord and placenta was a rich source of HSCs. Thistissue supports the developing fetus during pregnancy,is delivered along with the baby, and, is usually discarded.Since the first successful umbilical cordblood transplants in children with Fanconi anemia,the collection and therapeutic use of these cells hasgrown quickly. The New York Blood Center’s PlacentalBlood Program, supported by NIH, is the largest U.S.public umbilical cord blood bank and now has13,000 donations available for transplantation intosmall patients who need HSCs. Since it began collectingumbilical cord blood in 1992, the center hasprovided thousands of cord blood units to patients.Umbilical cord blood recipients—typically children—have now lived in excess of eight years, relying on theHSCs from an umbilical cord blood transplant [31, 57].46
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>There is a substantial amount of research being conductedon umbilical cord blood to search for ways toexpand the number of HSCs and compare and contrastthe biological properties of cord blood with adultbone marrow stem cells. There have been suggestionsthat umbilical cord blood contains stem cellsthat have the capability of developing cells of multiplegerm layers (multipotent) or even all germ layers,e.g., endoderm, ectoderm, and mesoderm(pluripotent). To date, there is no published scientificevidence to support this claim. While umbilical cordblood represents a valuable resource for HSCs,research data have not conclusively shown qualitativedifferences in the differentiated cells producedbetween this source of HSCs and peripheral bloodand bone marrow.Fetal Hematopoietic SystemAn important source of HSCs in research, but not inclinical use, is the developing blood-producing tissuesof fetal animals. Hematopoietic cells appear early inthe development of all vertebrates. Most extensivelystudied in the mouse, HSC production sweepsthrough the developing embryo and fetus in waves.Beginning at about day 7 in the life of the mouseembryo, the earliest hematopoietic activity is indicatedby the appearance of blood islands in the yolksac (see Appendix A. Early Development). The point isdisputed, but some scientists contend that yolk sacblood production is transient and will generate someblood cells for the embryo, but probably not the bulkof the HSCs for the adult animal [12, 26, 44].According to this proposed scenario, most stem cellsthat will be found in the adult bone marrow andcirculation are derived from cells that appear slightlylater and in a different location. This other wave ofhematopoietic stem cell production occurs in theAGM—the region where the aorta, gonads, and fetalkidney (mesonephros) begin to develop. The cellsthat give rise to the HSCs in the AGM may also giverise to endothelial cells that line blood vessels. [13].These HSCs arise at around days 10 to 11 in themouse embryo (weeks 4 to 6 in human gestation),divide, and within a couple of days, migrate to theliver [11]. The HSCs in the liver continue to divide andmigrate, spreading to the spleen, thymus, and—nearthe time of birth—to the bone marrow.Whereas an increasing body of fetal HSC research isemerging from mice and other animals, there ismuch less information about human fetal andembryonic HSCs. Scientists in Europe, includingCoulombel, Peault, and colleagues, first describedhematopoietic precursors in human embryos only afew years ago [20, 53]. Most recently, Gallacher andothers reported finding HSCs circulating in the bloodof 12- to 18-week aborted human fetuses [16, 28, 54]that was rich in HSCs. These circulating cells haddifferent markers than did cells from fetal liver, fetalbone marrow, or umbilical cord blood.Embryonic <strong>Stem</strong> <strong>Cells</strong> and Embryonic Germ <strong>Cells</strong>In 1985, it was shown that it is possible to obtainprecursors to many different blood cells from mouseembryonic stem cells [9]. Perkins was able to obtainall the major lineages of progenitor cells from mouseembryoid bodies, even without adding hematopoieticgrowth factors [45].Mouse embryonic stem cells in culture, given the rightgrowth factors, can generate most, if not all, thedifferent blood cell types [19], but no one has yetachieved the “gold standard” of proof that they canproduce long-term HSCs from these sources—namelyby obtaining cells that can be transplanted intolethally irradiated mice to reconstitute long-termhematopoiesis [32].The picture for human embryonic stem and germcells is even less clear. Scientists from JamesThomson’s laboratory reported in 1999 that they wereable to direct human embryonic stem cells—whichcan now be cultured in the lab—to produce bloodprogenitor cells [23]. Israeli scientists reported thatthey had induced human ES cells to producehematopoietic cells, as evidenced by their productionof a blood protein, gamma-globin [21]. Cell linesderived from human embryonic germ cells (culturedcells derived originally from cells in the embryo thatwould ultimately give rise to eggs or sperm) that arecultured under certain conditions will produce CD34 +cells [47]. The blood-producing cells derived fromhuman ES and embryonic germ (EG) cells have notbeen rigorously tested for long-term self-renewal orthe ability to give rise to all the different blood cells.As sketchy as data may be on the hematopoieticpowers of human ES and EG cells, blood experts areintrigued by their clinical potential and their potentialto answer basic questions on renewal and differentiationof HSCs [19]. Connie Eaves, who has madecomparisons of HSCs from fetal liver, cord blood,47
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>The <strong>Stem</strong> Cell Databasehttp://stemcell.princeton.eduIhor Lemischka and colleagues at Princeton Universityand the Computational Biology and InformaticsLaboratory at the University of Pennsylvania are collaboratingto record all the findings about hematopoieticstem cell (HSC) genes and markers in the <strong>Stem</strong> CellDatabase.The collaborators started the database five years ago.Its goal is listing and annotating all the genes that aredifferentially expressed in mouse liver HSCs and theircellular progeny. The database is growing to includehuman HSCs from different blood sources, and arelated database, constructed in collaboration withKateri A. Moore, also at Princeton University, will documentall genes active in stromal cells, which provide themicroenvironment in which stem cells are maintained.The combined power of the two databases, along withnew tools and methods for studying molecular biology,will help researchers put together a complete portrait ofthe hematopoietic stem cell and how it works. Thedatabases will continue to grow and take advantageof other efforts, such as those to complete the genesequences of mammals. Data will be publicly availableto researchers around the world.and adult bone marrow, expects cells derived fromembryonic tissues to have some interesting traits. Shesays actively dividing blood-producing cells from EScell culture—if they are like other dividing cells—willnot themselves engraft or rescue hematopoiesis in ananimal whose bone marrow has been destroyed.However, they may play a critical role in developingan abundant supply of HSCs grown in the lab.Indications are that the dividing cells will also morereadily lend themselves to gene manipulations thando adult HSCs. Eaves anticipates that HSCs derivedfrom early embryo sources will be developmentallymore “plastic” than later HSCs, and more capable ofself-renewal [14].HOW DO HSCs FROM VARYINGSOURCES DIFFER?Scientists in the laboratory and clinic are beginning tomeasure the differences among HSCs from differentsources. In general, they find that HSCs taken fromtissues at earlier developmental stages have agreater ability to self-replicate, show different homingand surface characteristics, and are less likely to berejected by the immune system—making thempotentially more useful for therapeutic transplantation.<strong>Stem</strong> cell populations of the bone marrowWhen do HSCs move from the early locations in thedeveloping fetus to their adult “home” in the bonemarrow? European scientists have found that the relativenumber of CD34 + cells in the collections of cordblood declined with gestational age, but expressionof cell-adhesion molecules on these cells increased.The authors believe these changes reflect preparationsfor the cells to relocate—from homing in fetalliver to homing in bone marrow [52].The point is controversial, but a paper by Chen et al.provides evidence that at least in some strains ofmice, HSCs from old mice are less able to repopulatebone marrow after transplantation than are cellsfrom young adult mice [5]. <strong>Cells</strong> from fetal mice were50 to 100 percent better at repopulating marrowthan were cells from young adult mice were. Thespecific potential for repopulating marrow appears tobe strain-specific, but the scientists found this potentialdeclined with age for both strains. Other scientistsfind no decreases or sometimes increases in numbersof HSCs with age [51]. Because of the difficultyin identifying a long-term stem cell, it remains difficultto quantify changes in numbers of HSCs as aperson ages.Effectiveness of Transplants of Adult versus UmbilicalCord Blood <strong>Stem</strong> <strong>Cells</strong>A practical and important difference between HSCscollected from adult human donors and from umbilicalcord blood is simply quantitative. Doctors arerarely able to extract more than a few million HSCsfrom a placenta and umbilical cord—too few to usein a transplant for an adult, who would ideally get 7 to10 million CD34 + cells per kilogram body weight, butoften adequate for a transplant for a child [33, 48].Leonard Zon says that HSCs from cord blood are lesslikely to cause a transplantation complication calledgraft-versus-host disease, in which white blood cells48
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>from a donor attack tissues of the recipient [65]. In arecent review of umbilical cord blood transplantation,Laughlin cites evidence that cord blood causes lessgraft-versus-host disease [31]. Laughlin writes that it isyet to be determined whether umbilical cord bloodHSCs are, in fact, longer lived in a transplant recipient.In lab and mouse-model tests comparing CD34 +cells from human cord with CD34 + cells derived fromadult bone marrow, researchers found cord bloodhad greater proliferation capacity [24]. White bloodcells from cord blood engrafted better in a mousemodel, which was genetically altered to tolerate thehuman cells, than did their adult counterparts.Effectiveness in Transplants of Peripheral VersusBone Marrow <strong>Stem</strong> <strong>Cells</strong>In addition to being far easier to collect, peripherallyharvested white blood cells have other advantagesover bone marrow. Cutler and Antin’s review says thatperipherally harvested cells engraft more quickly, butare more likely to cause graft-versus-host disease [8].Prospecting for the most receptive HSCs for genetherapy, Orlic and colleagues found that mouse HSCsmobilized with cytokines were more likely to take upgenes from a viral vector than were non-mobilizedbone marrow HSCs [43].WHAT DO HEMATOPOIETIC STEMCELLS DO AND WHAT FACTORS AREINVOLVED IN THESE ACTIVITIES?As stated earlier, an HSC in the bone marrow has fouractions in its repertoire: 1) it can renew itself, 2) it candifferentiate, 3) it can mobilize out of the bonemarrow into circulation (or the reverse), or 4) it canundergo programmed cell death, or apoptosis.Understanding the how, when, where, which, and whyof this simple repertoire will allow researchers tomanipulate and use HSCs for tissue and organ repair.Self-renewal of Hematopoietic <strong>Stem</strong> <strong>Cells</strong>Scientists have had a tough time trying to grow—or even maintain—true stem cells in culture. This is animportant goal because cultures of HSCs that couldmaintain their characteristic properties of self-renewaland lack of differentiation could provide an unlimitedsource of cells for therapeutic transplantation andstudy. When bone marrow or blood cells are observedin culture, one often observes large increases in thenumber of cells. This usually reflects an increase indifferentiation of cells to progenitor cells that can giverise to different lineages of blood cells but cannotrenew themselves. True stem cells divide and replacethemselves slowly in adult bone marrow.New tools for gene-expression analysis will now allowscientists to study developmental changes in telomeraseactivity and telomeres. Telomeres are regionsof DNA found at the end of chromosomes that areextended by the enzyme telomerase. Telomeraseactivity is necessary for cells to proliferate and activitydecreases with age leading to shortened telomeres.Scientists hypothesize that declines in stem cellrenewal will be associated with declines in telomerelength and telomerase activity. Telomerase activity inhematopoietic cells is associated with self-renewalpotential [40].Because self-renewal divisions are rare, hard toinduce in culture, and difficult to prove, scientists donot have a definitive answer to the burning question:what puts—or perhaps keeps—HSCs in a self-renewaldivision mode? HSCs injected into an anemic patientor mouse—or one whose HSCs have otherwise beensuppressed or killed—will home to the bone marrowand undergo active division to both replenish all thedifferent types of blood cells and yield additional selfrenewingHSCs. But exactly how this happens remainsa mystery that scientists are struggling to solve bymanipulating cultures of HSCs in the laboratory.Two recent examples of progress in the culturingstudies of mouse HSCs are by Ema and coworkersand Audet and colleagues [2, 15]. Ema et al. foundthat two cytokines—stem cell factor and thrombopoietin—efficientlyinduced an unequal first celldivision in which one daughter cell gave rise torepopulating cells with self-renewal potential. Audetet al. found that activation of the signaling moleculegp130 is critical to survival and proliferation of mouseHSCs in culture.Work with specific cytokines and signaling moleculesbuilds on several earlier studies demonstrating modestincreases in the numbers of stem cells that couldbe induced briefly in culture. For example, Van Zantand colleagues used continuous-perfusion cultureand bioreactors in an attempt to boost human HSCnumbers in single cord blood samples incubated forone to two weeks [58]. They obtained a 20-foldincrease in “long-term culture initiating cells.”49
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>More clues on how to increase numbers of stem cellsmay come from looking at other animals and variousdevelopmental stages. During early developmentalstages—in the fetal liver, for example—HSCs mayundergo more active cell division to increase theirnumbers, but later in life, they divide far less often [30,42]. Culturing HSCs from 10- and 11-day-old mouseembryos, Elaine Dzierzak at Erasmus University in theNetherlands finds she can get a 15-fold increase inHSCs within the first 2 or 3 days after she removes theAGM from the embryos [38]. Dzierzak recognizes thatthis is dramatically different from anything seen withadult stem cells and suggests it is a difference withpractical importance. She suspects that the increaseis not so much a response to what is going on in theculture but rather, it represents the developmentalmomentum of this specific embryonic tissue. That is, itis the inevitable consequence of divisions that werecued by that specific embryonic microenvironment.After five days, the number of HSCs plateaus and canbe maintained for up to a month. Dzierzak says thatthe key to understanding how adult-derived HSCs canbe expanded and manipulated for clinical purposesmay very well be found by defining the cellular compositionand complex molecular signals in the AGMregion during development [13].In another approach, Lemischka and coworkers havebeen able to maintain mouse HSCs for four to sevenweeks when they are grown on a clonal line of cells(AFT024) derived from the stroma, the other majorcellular constituent of bone marrow [39]. No oneknows which specific factors secreted by the stromalcells maintain the stem cells. He says ongoing genecloning is rapidly zeroing in on novel molecules fromthe stromal cells that may “talk” to the stem cells andpersuade them to remain stem cells—that is,continue to divide and not differentiate.If stromal factors provide the key to stem cell selfrenewal,research on maintaining stromal cells maybe an important prerequisite. In 1999, researchers atOsiris Therapeutics and Johns Hopkins Universityreported culturing and expanding the numbers ofmesenchymal stem cells, which produce the stromalenvironment [46]. Whereas cultured HSCs rush todifferentiate and fail to retain primitive, self-renewingcells, the mesenchymal stem cells could beincreased in numbers and still retained their powers togenerate the full repertoire of descendant lineages.Differentiation of HSCs into Components of theBlood and Immune SystemProducing differentiated white and red blood cells isthe real work of HSCs and progenitor cells. M.C.MacKey calculates that in the course of producinga mature, circulating blood cell, the originalhematopoietic stem cell will undergo between 17and 19.5 divisions, “giving a net amplification ofbetween ~170,000 and ~720,000” [35].Through a series of careful studies of cultured cells—often cells with mutations found in leukemia patientsor cells that have been genetically altered—investigators have discovered many key growthfactors and cytokines that induce progenitor cells tomake different types of blood cells. These factorsinteract with one another in complex ways to createa system of exquisite genetic control and coordinationof blood cell production.Migration of Hematopoietic <strong>Stem</strong> <strong>Cells</strong> Into andOut of Marrow and TissuesScientists know that much of the time, HSCs live inintimate connection with the stroma of bone marrowin adults (see Chapter 4. The Adult <strong>Stem</strong> Cell). ButHSCs may also be found in the spleen, in peripheralblood circulation, and other tissues. Connection tothe interstices of bone marrow is important to boththe engraftment of transplanted cells and to themaintenance of stem cells as a self-renewing population.Connection to stroma is also important to theorderly proliferation, differentiation, and maturation ofblood cells [63].Weissman says HSCs appear to make brief forays outof the marrow into tissues, then duck back into marrow[62]. At this time, scientists do not understand whyor how HSCs leave bone marrow or return to it [59].Scientists find that HSCs that have been mobilizedinto peripheral circulation are mostly non-dividingcells [64]. They report that adhesion molecules on thestroma, play a role in mobilization, in attachment tothe stroma, and in transmitting signals that regulateHSC self-renewal and progenitor differentiation [61].Apoptosis and Regulation of Hematopoietic <strong>Stem</strong>Cell PopulationsThe number of blood cells in the bone marrow andblood is regulated by genetic and molecularmechanisms. How do hematopoietic stem cells know50
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>when to stop proliferating? Apoptosis is the processof programmed cell death that leads cells to selfdestructwhen they are unneeded or detrimental. Ifthere are too few HSCs in the body, more cells divideand boost the numbers. If excess stem cells wereinjected into an animal, they simply wouldn’t divideor would undergo apoptosis and be eliminated [62].Excess numbers of stem cells in an HSC transplantactually seem to improve the likelihood and speed ofengraftment, though there seems to be no rigorousidentification of a mechanism for this empiricalobservation.The particular signals that trigger apoptosis in HSCsare as yet unknown. One possible signal for apoptosismight be the absence of life-sustaining signals frombone marrow stroma. Michael Wang and othersfound that when they used antibodies to disrupt theadhesion of HSCs to the stroma via VLA-4/VCAM-1,the cells were predisposed to apoptosis [61].Understanding the forces at play in HSC apoptosis isimportant to maintaining or increasing their numbersin culture. For example, without growth factors, suppliedin the medium or through serum or other feederlayers of cells, HSCs undergo apoptosis. Domen andWeissman found that stem cells need to get twogrowth factor signals to continue life and avoidapoptosis: one via a protein called BCL-2, the otherfrom steel factor, which, by itself, induces HSCs toproduce progenitor cells but not to self-renew [10].WHAT ARE THE CLINICAL USES OFHEMATOPOIETIC STEM CELLS?Leukemia and LymphomaAmong the first clinical uses of HSCs were thetreatment of cancers of the blood—leukemia andlymphoma, which result from the uncontrolledproliferation of white blood cells. In these applications,the patient’s own cancerous hematopoieticcells were destroyed via radiation or chemotherapy,then replaced with a bone marrow transplant, or, as isdone now, with a transplant of HSCs collected fromthe peripheral circulation of a matched donor. Amatched donor is typically a sister or brother of thepatient who has inherited similar human leukocyteantigens (HLAs) on the surface of their cells. Cancersof the blood include acute lymphoblastic leukemia,acute myeloblastic leukemia, chronic myelogenousleukemia (CML), Hodgkin’s disease, multiplemyeloma, and non-Hodgkin’s lymphoma.Thomas and Clift describe the history of treatment forchronic myeloid leukemia as it moved from largelyineffective chemotherapy to modestly successfuluse of a cytokine, interferon, to bone marrow transplants—firstin identical twins, then in HLA-matchedsiblings [55]. Although there was significant risk ofpatient death soon after the transplant either frominfection or from graft-versus-host disease, for the firsttime, many patients survived this immediate challengeand had survival times measured in years oreven decades, rather than months. The authors write,“In the space of 20 years, marrow transplantationhas contributed to the transformation of [chronicmyelogenous leukemia] CML from a fatal diseaseto one that is frequently curable. At the same time,experience acquired in this setting has improved ourunderstanding of many transplant-related problems.It is now clear that morbidity and mortality are notinevitable consequences of allogeneic transplantation,[and] that an allogeneic effect can add to theanti-leukemic power of conditioning regimens…”In a recent development, CML researchers havetaken their knowledge of hematopoietic regulationone step farther. On May 10, 2001, the Food andDrug Administration approved Gleevec (imatinibmesylate), a new, rationally designed oral drug fortreatment of CML. The new drug specifically targets amutant protein, produced in CML cancer cells, thatsabotages the cell signals controlling orderly divisionof progenitor cells. By silencing this protein, the newdrug turns off cancerous overproduction of whiteblood cells, so doctors do not have to resort to bonemarrow transplantation. At this time, it is unknownwhether the new drug will provide sustained remissionor will prolong life for CML patients.Inherited Blood DisordersAnother use of allogeneic bone marrow transplants isin the treatment of hereditary blood disorders, suchas different types of inherited anemia (failure to produceblood cells), and inborn errors of metabolism(genetic disorders characterized by defects in keyenzymes need to produce essential body componentsor degrade chemical byproducts). The blooddisorders include aplastic anemia, beta-thalassemia,Blackfan-Diamond syndrome, globoid cell leukodystrophy,sickle-cell anemia, severe combinedimmunodeficiency, X-linked lymphoproliferativesyndrome, and Wiskott-Aldrich syndrome. Inborn errorsof metabolism that are treated with bone marrow51
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>The National Marrow Donor Programhttp://www.marrow.orgLaunched in 1987, the National Marrow Donor Program(NMDP) was created to connect patients who needblood-forming stem cells or bone marrow with potentialnonrelated donors. About 70 percent of patients whoneed a life-saving HSC transplant cannot find a matchin their own family.The NMDP is made up of an international network ofcenters and banks that collect cord blood, bonemarrow, and peripherally harvested stem cells and thatrecruit potential donors. As of February 28, 2001, theNMDP listed 4,291,434 potential donors. Since its start,the Minneapolis-based group has facilitated almost12,000 transplants—75 percent of them for leukemia.Major recruiting efforts have led to substantial increasesin the number of donations from minorities, but thechance that African Americans, Native Americans,Asian/Pacific Islanders, or Hispanics will find a match isstill lower than it is for Caucasians.transplants include: Hunter’s syndrome, Hurler’s syndrome,Lesch Nyhan syndrome, and osteopetrosis.Because bone marrow transplantation has carried asignificant risk of death, this is usually a treatment oflast resort for otherwise fatal diseases.Hematopoietic <strong>Stem</strong> Cell Rescue in CancerChemotherapyChemotherapy aimed at rapidly dividing cancer cellsinevitably hits another target—rapidly dividinghematopoietic cells. Doctors may give cancerpatients an autologous stem cell transplant toreplace the cells destroyed by chemotherapy. Theydo this by mobilizing HSCs and collecting them fromperipheral blood. The cells are stored while thepatient undergoes intensive chemotherapy or radiotherapyto destroy the cancer cells. Once the drugshave washed out of a patient’s body, the patientreceives a transfusion of his or her stored HSCs.Because patients get their own cells back, there is nochance of immune mismatch or graft-versus-hostdisease. One problem with the use of autologousHSC transplants in cancer therapy has been thatcancer cells are sometimes inadvertently collectedand reinfused back into the patient along with thestem cells. One team of investigators finds that theycan prevent reintroducing cancer cells by purifyingthe cells and preserving only the cells that areCD34 + , Thy-1 + [41].Graft-Versus-Tumor Treatment of CancerOne of the most exciting new uses of HSCtransplantation puts the cells to work attacking otherwiseuntreatable tumors. A group of researchers inNIH’s intramural research program recently describedthis approach to treating metastatic kidney cancer[7]. Just under half of the 38 patients treated sofar have had their tumors reduced. The researchprotocol is now expanding to treatment of other solidtumors that resist standard therapy, including cancerof the lung, prostate, ovary, colon, esophagus, liver,and pancreas.This experimental treatment relies on an allogeneicstem cell transplant from an HLA-matched siblingwhose HSCs are collected peripherally. The patient’sown immune system is suppressed, but not totallydestroyed. The donor’s cells are transfused into thepatient, and for the next three months, doctorsclosely monitor the patient’s immune cells, using DNAfingerprinting to follow the engraftment of the donor’scells and regrowth of the patient’s own blood cells.They must also judiciously suppress the patient’simmune system as needed to deter his/her T cellsfrom attacking the graft and to reduce graft-versushostdisease.A study by Joshi et al. shows that umbilical cordblood and peripherally harvested human HSCs showantitumor activity in the test tube against leukemiacells and breast cancer cells [22]. Grafted into amouse model that tolerates human cells, HSCs attackhuman leukemia and breast cancer cells. Althoughuntreated cord blood lacks natural killer (NK) lymphocytescapable of killing tumor cells, researchers havefound that at least in the test tube and in mice, theycan greatly enhance the activity and numbers ofthese cells with cytokines IL-15 [22, 34].Other Applications of Hematopoietic <strong>Stem</strong> <strong>Cells</strong>Substantial basic and limited clinical research exploringthe experimental uses of HSCs for other diseasesis underway. Among the primary applications areautoimmune diseases, such as diabetes, rheumatoid52
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>arthritis, and system lupus erythematosis. Here, thebody’s immune system turns to destroying bodytissues. Experimental approaches similar to thoseapplied above for cancer therapies are being conductedto see if the immune system can bereconstituted or reprogrammed. More detailed discussionon this application is provided in Chapter 6.Autoimmune Diseases and the Promise of <strong>Stem</strong> Cell-Based Therapies. The use of HSCs as a means todeliver genes to repair damaged cells is anotherapplication being explored. The use of HSCs for genetherapies is discussed in detail in Chapter 11. Use ofGenetically Modified <strong>Stem</strong> <strong>Cells</strong> in ExperimentalGene Therapies.PLASTICITY OF HEMATOPOIETICSTEM CELLSA few recent reports indicate that scientists havebeen able to induce bone marrow or HSCs todifferentiate into other types of tissue, such as brain,muscle, and liver cells. These concepts and theexperimental evidence supporting this concept arediscussed in Chapter 4. The Adult <strong>Stem</strong> Cell.Research in a mouse model indicates that cells fromgrafts of bone marrow or selected HSCs may hometo damaged skeletal and cardiac muscle or liver andregenerate those tissues [4, 29]. One recent advancehas been in the study of muscular dystrophy, agenetic disease that occurs in young people andleads to progressive weakness of the skeletal muscles.Bittner and colleagues used mdx mice, a geneticallymodified mouse with muscle cell defects similar tothose in human muscular dystrophy. Bone marrowfrom non-mdx male mice was transplanted intofemale mdx mice with chronic muscle damage;after 70 days, researchers found that nuclei from themales had taken up residence in skeletal and cardiacmuscle cells.Lagasse and colleagues’ demonstration of liver repairby purified HSCs is a similarly encouraging sign thatHSCs may have the potential to integrate into andgrow in some non-blood tissues. These scientistslethally irradiated female mice that had an unusualgenetic liver disease that could be halted with adrug. The mice were given transplants of geneticallymarked, purified HSCs from male mice that did nothave the liver disease. The transplants were given achance to engraft for a couple of months while themice were on the liver-protective drug. The drug wasthen removed, launching deterioration of the liver—and a test to see whether cells from the transplantwould be recruited and rescue the liver. The scientistsfound that transplants of as few as 50 cells led toabundant growth of marked, donor-derived liver cellsin the female mice.Recently, Krause has shown in mice that a singleselected donor hematopoietic stem cell could domore than just repopulate the marrow andhematopoietic system of the recipient [27]. Theseinvestigators also found epithelial cells derived fromthe donors in the lungs, gut, and skin of the recipientmice. This suggests that HSCs may have grown in theother tissues in response to infection or damage fromthe irradiation the mice received.In humans, observations of male liver cells in femalepatients who have received bone marrow grafts frommales, and in male patients who have received livertransplants from female donors, also suggest thepossibility that some cells in bone marrow have thecapacity to integrate into the liver and formhepatocytes [1].WHAT ARE THE BARRIERS TO THEDEVELOPMENT OF NEW ANDIMPROVED TREATMENTS USINGHEMATOPOIETIC STEM CELLS?Boosting the Numbers of Hematopoietic <strong>Stem</strong> <strong>Cells</strong>Clinical investigators share the same fundamentalproblem as basic investigators—limited ability to growand expand the numbers of human HSCs. Cliniciansrepeatedly see that larger numbers of cells in stemcell grafts have a better chance of survival in apatient than do smaller numbers of cells. The limitednumber of cells available from a placenta andumbilical cord blood transplant currently means thatcord blood banks are useful to pediatric but not adultpatients. Investigators believe that the main cause offailure of HSCs to engraft is host-versus-graft disease,and larger grafts permit at least some donor cellsto escape initial waves of attack from a patient’sresidual or suppressed immune system [6]. Ability toexpand numbers of human HSCs in vivo or in vitrowould clearly be an enormous boost to all currentand future medical uses of HSC transplantation.53
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>Once stem cells and their progeny can be multipliedin culture, gene therapists and blood experts couldcombine their talents to grow limitless quantities of“universal donor” stem cells, as well as progenitorsand specific types of red and white blood cells. If thecells were engineered to be free of markers thatprovoke rejection, these could be transfused to anyrecipient to treat any of the diseases that are nowaddressed with marrow, peripheral, cord, or othertransfused blood. If gene therapy and studies of theplasticity of HSCs succeed, the cells could also begrown to repair other tissues and treat non-bloodrelateddisorders [32].Several research groups in the United States, Canada,and abroad have been striving to find the key factoror factors for boosting HSC production. Typicalapproaches include comparing genes expressed inprimitive HSCs versus progenitor cells; comparinggenes in actively dividing fetal HSCs versus adultHSCs; genetic screening of hematopoieticallymutated zebrafish; studying dysregulated genes incancerous hematopoietic cells; analyzing stromal orfeeder-layer factors that appear to boost HSCdivision; and analyzing factors promoting homingand attachment to the stroma. Promising candidatefactors have been tried singly and in combination,and researchers claim they can now increase thenumber of long-term stem cells 20-fold, albeit briefly,in culture.The specific assays researchers use to prove that theirexpanded cells are stem cells vary, which makes itdifficult to compare the claims of different researchgroups. To date, there is only a modest ability toexpand true, long-term, self-renewing human HSCs.Numbers of progenitor cells are, however, morereadily increased. Kobari et al., for example, canincrease progenitor cells for granulocytes andmacrophages 278-fold in culture [25].Some investigators are now evaluating whether thesecomparatively modest increases in HSCs are clinicallyuseful. At this time, the increases in cell numbers arenot sustainable over periods beyond a few months,and the yield is far too low for mass production. Inaddition, the cells produced are often not rigorouslycharacterized. A host of other questions remain—from how well the multiplied cells can be altered forgene therapy to their potential longevity, immunogenicity,ability to home correctly, and susceptibility tocancerous transformation. Glimm et al. [17] highlightsome of these problems, for example, with theirconfirmation that human stem cells lose their abilityto repopulate the bone marrow as they enter andprogress through the cell cycleælike mouse stemcells that have been stimulated to divide lose theirtransplantability [18]. Observations on the inverserelationship between progenitor cell division rate andlongevity in strains of mice raise an additional concernthat culture tricks or selection of cells thatexpand rapidly may doom the cells to a short life.Pragmatically, some scientists say it may not benecessary to be able to induce the true, long-termHSC to divide in the lab. If they can manipulateprogenitors and coax them into division on command,gene uptake, and differentiation into keyblood cells and other tissues, that may be sufficientto accomplish clinical goals. It might be sufficient toboost HSCs or subpopulations of hematopoietic cellswithin the body by chemically prodding the bonemarrow to supply the as-yet-elusive factors torejuvenate cell division.Outfoxing the Immune System in Host, Graft, andPathogen AttacksCurrently, the risks of bone marrow transplants—graftrejection, host-versus-graft disease, and infectionduring the period before HSCs have engrafted andresumed full blood cell production—restrict their useto patients with serious or fatal illnesses. Allogeneicgrafts must come from donors with a close HLAmatch to the patient (see Chapter 6. AutoimmuneDiseases and the Promise of <strong>Stem</strong> Cell-BasedTherapies). If doctors could precisely manipulateimmune reactions and protect patients frompathogens before their transplants begin to function,HSC transplants could be extended to less ill patientsand patients for whom the HLA match was not asclose as it must now be. Physicians might usetransplants with greater impunity in gene therapy,autoimmune disease, HIV/AIDS treatment, and thepreconditioning of patients to accept a major organtransplant.Scientists are zeroing in on subpopulations of T cellsthat may cause or suppress potentially lethal hostversus-graftrejection and graft-versus-host disease inallogeneic-transplant recipients. T cells in a graft area two-edged sword. They fight infections and help54
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>the graft become established, but they also cancause graft-versus-host disease. Identifying subpopulationsof T cells responsible for deleterious andbeneficial effects—in the graft, but also in residualcells surviving or returning in the host—could allowclinicians to make grafts safer and to ratchet upgraft-versus-tumor effects [48]. Understanding thepresentation of antigens to the immune system andthe immune system’s healthy and unhealthyresponses to these antigens and maturation andprogrammed cell death of T cells is crucial.The approach taken by investigators at Stanford—purifying peripheral blood—may also help eliminatethe cells causing graft-versus-host disease. Transplantsin mouse models support the idea that purified HSCs,cleansed of mature lymphocytes, engraft readily andavoid graft-versus-host disease [60].Knowledge of the key cellular actors in autoimmunedisease, immune grafting, and graft rejection couldalso permit scientists to design gentler “minitransplants.”Rather than obliterating and replacing thepatient’s entire hematopoietic system, they couldreplace just the faulty components with a selection ofcells custom tailored to the patient’s needs. Cliniciansare currently experimenting with deletion of T cellsfrom transplants in some diseases, for example,thereby reducing graft-versus-host disease.Researchers are also experimenting with the possibilityof knocking down the patient’s immune system—butnot knocking it out. A blow that is sublethal to thepatient’s hematopoietic cells given before an allogeneictransplant can be enough to give the graft achance to take up residence in the bone marrow.The cells replace some or all of the patient’s originalstem cells, often making their blood a mix of donorand original cells. For some patients, this mix of cellswill be enough to accomplish treatment objectivesbut without subjecting them to the vicious sideeffects and infection hazards of the most powerfultreatments used for total destruction of their hematopoieticsystems [37].Understanding the Differentiating Environment andDevelopmental PlasticityAt some point in embryonic development, all cellsare plastic, or developmentally flexible enough togrow into a variety of different tissues. Exactly what isit about the cell or the embryonic environment thatinstructs cells to grow into one organ and not another?Could there be embryological underpinnings to theapparent plasticity of adult cells? Researchers havesuggested that a lot of the tissues that are showingplasticity are adjacent to one another after gastrulationin the sheet of mesodermal tissue that will goon to form blood—muscle, blood vessels, kidney,mesenchyme, and notochord. Plasticity may reflectderivation from the mesoderm, rather than being afixed trait of hematopoietic cells. One lab is nowstudying the adjacency of embryonic cells and howthe developing embryo makes the decision to makeone tissue instead of another—and whether thedecision is reversible [65].In vivo studies of the plasticity of bone marrow orpurified stem cells injected into mice are in theirinfancy. Even if follow-up studies confirm and moreprecisely characterize and quantify plasticity potentialof HSCs in mice, there is no guarantee that it willoccur or can be induced in humans.SUMMARYGrounded in half a century of research, the study ofhematopoietic stem cells is one of the most excitingand rapidly advancing disciplines in biomedicinetoday. Breakthrough discoveries in both the laboratoryand clinic have sharply expanded the use andsupply of life-saving stem cells. Yet even morepromising applications are on the horizon andscientists’ current inability to grow HSCs outside thebody could delay or thwart progress with these newtherapies. New treatments include graft-versus-tumortherapy for currently incurable cancers, autologoustransplants for autoimmune diseases, and genetherapy and tissue repair for a host of other problems.The techniques, cells, and knowledge thatresearchers have now are inadequate to realize thefull promise of HSC-based therapy.Key issues for tapping the potential of hematopoieticstem cells will be finding ways to safely and efficientlyexpand the numbers of transplantable human HSCsin vitro or in vivo. It will also be important to gain abetter understanding of the fundamentals of howimmune cells work—in fighting infections, in causingtransplant rejection, and in graft-versus-host disease aswell as master the basics of HSC differentiation.Concomitant advances in gene therapy techniquesand the understanding of cellular plasticity could makeHSCs one of the most powerful tools for healing.55
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>REFERENCES1. Alison, M.R., Poulsom, R., Jeffery, R., Dhillon, A.P., Quaglia,A., Jacob, J., Novelli, M., Prentice, G., Williamson, J., andWright, N.A. (2000). Hepatocytes from non-hepatic adultstem cells. Nature. 406, 257.2. Audet, J., Miller, C.L., Rose-John, S., Piret, J.M., and Eaves,C.J. (2001). Distinct role of gp130 activation in promotingself-renewal divisions by mitogenically stimulated murinehematopoietic stem cells. Proc. Natl. Acad. Sci. U. S. A. 98,1757-1762.3. Baum, C.M., Weissman, I.L., Tsukamoto, A.S., Buckle, A.M.,and Peault, B. (1992). Isolation of a candidate humanhematopoietic stem-cell population. Proc. Natl. Acad. Sci.U. S. A. 89, 2804-2808.4. Bittner, R.E., Schofer, C., Weipoltshammer, K., Ivanova, S.,Streubel, B., Hauser, E., Freilinger, M., Hoger, H., Elbe-Burger,A., and Wachtler, F. (1999). Recruitment of bone-marrowderivedcells by skeletal and cardiac muscle in adultdystrophic mdx mice. Anat. Embryol. (Berl) 199, 391-396.5. Chen, J., Astle, C.M., and Harrison, D.E. (1999).Development and aging of primitive hematopoietic stemcells in BALB/cBy mice. Exp. Hematol. 27, 928-935.6. Childs, R., personal communication.7. Childs, R., Chernoff, A., Contentin, N., Bahceci, E., Schrump,D., Leitman, S., Read, E.J., Tisdale, J., Dunbar, C., Linehan,W.M., Young, N.S., and Barrett, A.J. (2000). Regression ofmetastatic renal-cell carcinoma after nonmyeloablativeallogeneic peripheral-blood stem-cell transplantation.N. Engl. J. Med. 343, 750-758.8. Cutler, C. and Antin, J.H. (2001). Peripheral blood stem cellsfor allogeneic transplantation: a review. <strong>Stem</strong> <strong>Cells</strong>. 19,108-117.9. Doetschman, T., Eistetter, H., Katz, M., Schmit, W., andKemler, R. (1985). The in vitro development of blastocystderivedembryonic stem cell lines: formation of visceralyolk sac, blood islands and myocardium. J. Embryol. Exp.Morph. 87, 27-45.10. Domen, J. and Weissman, I.L. (2000). Hematopoietic stemcells need two signals to prevent apoptosis; BCL-2 canprovide one of these, Kitl/c-Kit signaling the other. J. Exp.Med. 192, 1707-1718.11. Dzierzak, E., Medvinsky, A., and de Bruijn, M. (1998).Qualitative and quantitative aspects of haematopoieticcell development in the mammalian embryo. Immunol.Today. 19, 228-236.12. Dzierzak, E. (1999). Embryonic beginnings of definitivehematopoietic stem cells. Ann. N. Y. Acad. Sci. 872,256-262.13. Dzierzak, E., personal communication.14. Eaves, C. J., personal communication.16. Gallacher, L., Murdoch, B., Wu, D., Karanu, F., Fellows, F.,and Bhatia, M. (2000). Identification of novel circulatinghuman embryonic blood stem cells. Blood. 96, 1740-1747.17. Glimm, H., Oh, I.H., and Eaves, C.J. (2000). Humanhematopoietic stem cells stimulated to proliferate in vitrolose engraftment potential during their S/G(2)/M transit anddo not reenter G(0). Blood. 96, 4185-4193.18. Gothot, A., van der Loo, J.C., Clapp, D.W., and Srour, E.F.(1998). Cell cycle-related changes in repopulating capacityof human mobilized peripheral blood CD34 + cells innon-obese diabetic/severe combined immune-deficientmice. Blood. 92, 2641-2649.19. Hole, N. (1999). Embryonic stem cell-derivedhaematopoiesis. <strong>Cells</strong> Tissues Organs. 165, 181-189.20. Huyhn, A., Dommergues, M., Izac, B., Croisille, L., Katz, A.,Vainchenker, W., and Coulombel, L. (1995).Characterization of hematopoietic progenitors from humanyolk sacs and embryos. Blood. 86, 4474-4485.21. Itskovitz-Eldor, J., Schuldiner, M., Karsenti, D., Eden, A.,Yanuka, O., Amit, M., Soreq, H., and Benvenisty, N. (2000).Differentiation of human embryonic stem cells into embryoidbodies comprising the three embryonic germ layers.Mol. Med. 6, 88-95.22. Joshi, S.S., Tarantolo, S.R., Kuszynski, C.A., and Kessinger, A.(2000). Antitumor therapeutic potential of activated humanumbilical cord blood cells against leukemia and breastcancer. Clin. Cancer Res. 6, 4351-4358.23. Kaufman, D.S., Lewis, R.L., Auerbach, R., and Thomson, J.A.(1999). Directed differentiation of human embryonic stemcells into hematopoietic colony forming cells. Blood. 94(Supplement part 1), 34a.24. Kim, D.K., Fujiki, Y., Fukushima, T., Ema, H., Shibuya, A., andNakauchi, H. (1999). Comparison of hematopoietic activitiesof human bone marrow and umbilical cord bloodCD34 positive and negative cells. <strong>Stem</strong> <strong>Cells</strong>. 17, 286-294.25. Kobari, L., Pflumio, F., Giarratana, M., Li, X., Titeux, M., Izac,B., Leteurtre, F., Coulombel, L., and Douay, L. (2000). In vitroand in vivo evidence for the long-term multilineage(myeloid, B, NK, and T) reconstitution capacity of ex vivoexpanded human CD34+ cord blood cells. Exp. Hematol.28, 1470-1480.26. Koichi, T., Akashi, K., and Weissman, I.L. (2001). <strong>Stem</strong> cellsand hematolymphoic development. Zon, L.I. ed. OxfordPress.27. Krause, D.S., Theise, N.D., Collector, M.I., Henegariu, O.,Hwang, S., Gardner, R., Neutzel, S., and Sharkis, S.J. (2001).Multi-organ, multi-lineage engraftment by a single bonemarrow-derived stem cell. Cell. 105, 369-377.28. Labastie, M.C., Cortes, F., Romeo, P.H., Dulac, C., andPeault, B. (1998). Molecular identity of hematopoietic precursorcells emerging in the human embryo. Blood. 92,3624-3635.15. Ema, H., Takano, H., Sudo, K., and Nakauchi, H. (2000).In vitro self-renewal division of hematopoietic stem cells.J. Exp. Med. 192, 1281-1288.56
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>29. Lagasse, E., Connors, H., Al Dhalimy, M., Reitsma, M.,Dohse, M., Osborne, L., Wang, X., Finegold, M., Weissman,I.L., and Grompe, M. (2000). Purified hematopoietic stemcells can differentiate into hepatocytes in vivo. Nat. Med. 6,1229-1234.30. Lansdorp, P.M., Dragowska, W., and Mayani, H. (1993).Ontogeny-related changes in proliferative potential ofhuman hematopoietic cells. J. Exp. Med. 178, 787-791.31. Laughlin, M.J. (2001). Umbilical cord blood for allogeneictransplantation in children and adults. Bone MarrowTransplant. 27, 1-6.32. Lemischka, I. R., personal communication.33. Lickliter, J.D., McGlave, P.B., DeFor, T.E., Miller, J.S., Ramsay,N.K., Verfaillie, C.M., Burns, L.J., Wagner, J.E., Eastlund, T.,Dusenbery, K., and Weisdorf, D.J. (2000). Matched-pairanalysis of peripheral blood stem cells compared to marrowfor allogeneic transplantation. Bone Marrow Transplant.26, 723-728.34. Lin, S.J., Yang, M.H., Chao, H.C., Kuo, M.L., and Huang, J.L.(2000). Effect of interleukin-15 and Flt3-ligand on naturalkiller cell expansion and activation: umbilical cord vs. adultperipheral blood mononuclear cells. Pediatr. AllergyImmunol. 11, 168-174.35. MacKey, M.C. (2001). Cell kinetic status of haematopoieticstem cells. Cell. Prolif. 34, 71-83.36. Marshak, D.R., Gottlieb, D., Kiger, A.A., Fuller, M.T., Kunath, T.,Hogan, B., Gardner, R.L., Smith, A., Klar, A.J.S., Henrique, D.,D’Urso, G., Datta, S., Holliday, R., Astle, C.M., Chen, J.,Harrison, D.E., Xie, T., Spradling, A., Andrews, P.W., Przyborski,S.A., Thomson, J.A., Kunath, T., Strumpf, D., Rossant, J.,Tanaka, S., Orkin, S.H., Melchers, F., Rolink, A., Keller, G.,Pittenger, M.F., Marshak, D.R., Flake, A.W., Panicker, M.M.,Rao, M., Watt, F.M., Grompe, M., Finegold, M.J., Kritzik, M.R.,Sarvetnick, N., and Winton, D.J. (2001). <strong>Stem</strong> cell biology,Marshak, D.R., Gardner, R.L., and Gottlieb, D. eds. (ColdSpring Harbor, New York: Cold Spring Harbor LaboratoryPress).37. McSweeney, P.A. and Storb, R. (1999). Mixed chimerism:preclinical studies and clinical applications. Biol. BloodMarrow Transplant. 5, 192-203.38. Medvinsky, A. and Dzierzak, E. (1996). Definitivehematopoiesis is autonomously initiated by the AGMregion. Cell. 86, 897-906.39. Moore, K.A., Ema, H., and Lemischka, I.R. (1997). In vitromaintenance of highly purified, transplantable hematopoieticstem cells. Blood. 89, 4337-4347.40. Morrison, S.J., Prowse, K.R., Ho, P., and Weissman, I.L. (1996).Telomerase activity in hematopoietic cells is associatedwith self- renewal potential. Immunity. 5, 207-216.41. Negrin, R.S., Atkinson, K., Leemhuis, T., Hanania, E., Juttner,C., Tierney, K., Hu, W.W., Johnston, L.J., Shizurn, J.A., Stockerl-Goldstein, K.E., Blume, K.G., Weissman, I.L., Bower, S.,Baynes, R., Dansey, R., Karanes, C., Peters, W., and Klein, J.(2000). Transplantation of highly purified CD34 + Thy-1 +hematopoietic stem cells in patients with metastatic breastcancer. Biol. Blood Marrow Transplant. 6, 262-271.42. Oh, I.H., Lau, A., and Eaves, C.J. (2000). During ontogenyprimitive (CD34 + CD38 - ) hematopoietic cells show alteredexpression of a subset of genes associated with earlycytokine and differentiation responses of their adult counterparts.Blood. 96, 4160-4168.43. Orlic, D., Girard, L.J., Anderson, S.M., Pyle, L.C., Yoder, M.C.,Broxmeyer, H.E., and Bodine, D.M. (1998). Identification ofhuman and mouse hematopoietic stem cell populationsexpressing high levels of mRNA encoding retrovirus receptors.Blood. 91, 3247-3254.44. Orlic, D., Bock, T.A., and Kanz, L. (1999). Hematopoieticstem cells biology and transplantation. Annals of The NewYork Academy of Sciences (New York, NY).45. Perkins, A.C. (1998). Enrichment of blood from embryonicstem cells in vitro. Reprod. Fertil. Dev. 10, 563-572.46. Pittenger, M.F., Mackay, A.M., Beck, S.C., Jaiswal, R.K.,Douglas, R., Mosca, J.D., Moorman, M.A., Simonetti, D.W.,Craig, S., and Marshak, D.R. (1999). Multilineage potentialof adult human mesenchymal stem cells. Science. 284,143-147.47. Shamblott, M.J., Axelman, J., Littlefield, J.W., Blumenthal,P.D., Huggins, G.R., Cui, Y., Cheng, L., and Gearhart, J.D.(2001). Human embryonic germ cell derivatives express abroad range of developmentally distinct markers and proliferateextensively in vitro. Proc. Natl. Acad. Sci. U. S. A. 98,113-118.48. Sharp, J.G., Kessinger, A., Lynch, J.C., Pavletic, Z.S., andJoshi, S.S. (2000). Blood stem cell transplantation: factorsinfluencing cellular immunological reconstitution. J.Hematother. <strong>Stem</strong> Cell Res. 9, 971-981.49. Smith, L.G., Weissman, I.L., and Heimfeld, S. (1991). Clonalanalysis of hematopoietic stem-cell differentiation in vivo.Proc. Natl. Acad. Sci. U. S. A. 88, 2788-2792.50. Spangrude, G.J., Heimfeld, S., and Weissman, I.L. (1988).Purification and characterization of mouse hematopoieticstem cells. Science. 241, 58-62.51. Sudo, K., Ema, H., Morita, Y., and Nakauchi, H. (2000). Ageassociatedcharacteristics of murine hematopoietic stemcells. J. Exp. Med. 192, 1273-1280.52. Surbek, D.V., Steinmann, C., Burk, M., Hahn, S., Tichelli, A.,and Holzgreve, W. (2000). Developmental changes inadhesion molecule expressions in umbilical cord bloodCD34 + hematopoietic progenitor and stem cells. Am. J.Obstet. Gynecol. 183, 1152-1157.53. Tavian, M., Coulombel, L., Luton, D., Clemente, H.S.,Dieterlen-Lievre, F., and Peault, B. (1996). Aorta-associatedCD34 + hematopoietic cells in the early human embryo.Blood. 87, 67-72.54. Tavian, M., Hallais, M.F., and Peault, B. (1999). Emergenceof intraembryonic hematopoietic precursors in the pre-liverhuman embryo. Development. 126, 793-803.55. Thomas, E.D. and Clift, R.A. (1999). Allogenic transplantationfor chronic myeloid leukemia. Thomas, E.D., Blume, K.G.,and Forman, S.J. eds. Blackwell Sci., 807-815.57
Hematopoietic <strong>Stem</strong> <strong>Cells</strong>56. Till, J.E. and McCullough, E.A. (1961). A direct measurementof the radiation sensitivity of normal mouse bone marrowcells. Radiat. Res. 14, 213-222.57. U.S. Department of Health and Human Services. (2000).Report to Congress on the Status of Umbilical Cord BloodTransplantation.58. Van Zant, G., Rummel, S.A., Koller, M.R., Larson, D.B.,Drubachevsky, I., Palsson, M., and Emerson, S.G. (1994).Expansion in bioreactors of human progenitor populationsfrom cord blood and mobilized peripheral blood. Blood<strong>Cells</strong>. 20, 482-490.59. Verfaillie, C. M., personal communication.60. Verlinden, S.F., Mulder, A.H., de Leeuw, J.P., and vanBekkum, D.W. (1998). T lymphocytes determine the developmentof xeno GVHD and of human hemopoiesis inNOD/SCID mice following human umbilical cord bloodtransplantation. <strong>Stem</strong> <strong>Cells</strong>. 16, Suppl. 1, 205-217.stromal cells. Cell Growth Differ. 9, 105-112.62. Weissman, I. L., personal communication.63. Whetton, A.D. and Graham, G.J. (1999). Homing andmobilization in the stem cell niche. Trends Cell. Biol. 9,233-238.64. Wright, D.E., Cheshier, S.H., Wagers, A.J., Randall, T.D.,Christensen, J.L., and Weissman, I.L. (2001).Cyclophosphamide/granulocyte colony-stimulating factorcauses selective mobilization of bone marrow hematopoieticstem cells into the blood after M-phase of the cellcycle.65. Zon, L. I., personal communication.61. Wang, M.W., Consoli, U., Lane, C.M., Durett, A., Lauppe,M.J., Champlin, R., Andreeff, M., and Deisseroth, A.B.(1998). Rescue from apoptosis in early (CD34-selected)versus late (non-CD34- selected) human hematopoieticcells by very late antigen 4- and vascular cell adhesionmolecule (VCAM) 1-dependent adhesion to bone marrow58
6.AUTOIMMUNE DISEASES AND THEPROMISE OF STEM CELL-BASED THERAPIESOne of the more perplexing questions in biomedicalresearch is—why does the body’s protective shieldagainst infections, the immune system, attack its ownvital cells, organs, and tissues? The answer to thisquestion is central to understanding an array ofautoimmune diseases, such as rheumatoid arthritis,type 1 diabetes, systemic lupus erythematosus, andSjogren’s syndrome. When some of the body's cellularproteins are recognized as “foreign” by immune cellscalled T lymphocytes, a destructive cascade ofinflammation is set in place. Current therapies tocombat these cases of cellular mistaken identitydampen the body’s immune response and leavepatients vulnerable to life-threatening infections.Research on stem cells is now providing newapproaches to strategically remove the misguidedimmune cells and restore normal immune cells tothe body. Presented here are some of the basicresearch investigations that are being guided byadult and embryonic stem cell discoveries.INTRODUCTIONThe body’s main line of defense against invasion byinfectious organisms is the immune system. To succeed,an immune system must distinguish the manycellular components of its own body (self) from thecells or components of invading organisms (nonself).“Nonself” should be attacked while “self” should not.Therefore, two general types of errors can be madeby the immune system. If the immune system fails toquickly detect and destroy an invading organism, aninfection will result. However, if the immune systemfails to recognize self cells or components andmistakenly attacks them, the result is known as anautoimmune disease. Common autoimmunediseases include rheumatoid arthritis, systemic lupuserythematosis (lupus), type 1 diabetes, multiplesclerosis, Sjogren’s syndrome and inflammatory boweldisease. Although each of these diseases hasdifferent symptoms, they share the unfortunate realitythat, for some reason, the body’s immune system hasturned against itself (see Box 6.1. Immune SystemComponents: Common Terms and Definitions).HOW DOES THE IMMUNE SYSTEMNORMALLY KEEP US HEALTHY?The “soldiers” of the immune system are white bloodcells, including T and B lymphocytes, which originatein the bone marrow from hematopoietic stem cells.Every day the body comes into contact with manyorganisms such as bacteria, viruses, and parasites.Unopposed, these organisms have the potential tocause serious infections, such as pneumonia or AIDS.When a healthy individual is infected, the bodyresponds by activating a variety of immune cells.Initially, invading bacteria or viruses are engulfed byan antigen presenting cell (APC), and their componentproteins (antigens) are cut into pieces and displayedon the cell’s surface. Pieces of the foreignprotein (antigen) bind to the major histocompatibilitycomplex (MHC) proteins, also known as human leukocyteantigen (HLA) molecules, on the surface of theAPCs (see Figure 6.1 Immune Response to Self orForeign Antigens). This complex, formed by a foreignprotein and an MHC protein, then binds to a T cellreceptor on the surface of another type of immunecell, the CD4 helper T cell. They are so namedbecause they “help” immune responses proceedand have a protein called CD4 on their surface. Thiscomplex enables these T cells to focus the immuneresponse to a specific invading organism. The antigen-specificCD4 helper T cells divide and multiplywhile secreting substances called cytokines, whichcause inflammation and help activate other immunecells. The particular cytokines secreted by the CD4helper T cells act on cells known as the CD8 “cytotoxic”T cells (because they can kill the cells that areinfected by the invading organism and have the CD859
Autoimmune Diseases and the Promise of <strong>Stem</strong> Cell-Based TherapiesFree pathogenclearance byspecific antibodyAntibodiesB CellProduction ofpathogenicself-reactiveantibodiesForeign (or self)antigenCytokinesCD8cytotoxicT cellWhole selfantigenAntigenPresentingCell (APC)Antigen-specificT cell receptorCD4helperT cellCD4helperT cellInfected cells (displaysforeign T cell epitopeon its surface) or self(i.e., loss of selftolerance)Cell death© 2001 Terese WinslowMHC/antigencomplexFigure 6.1. Immune Response to Self or Foreign Antigens.protein on their surface). The helper T cells can alsoactivate antigen-specific B cells to produce antibodies,which can neutralize and help eliminate bacteriaand viruses from the body. Some of the antigen-specificT and B cells that are activated to rid the body ofinfectious organisms become long-lived “memory”cells. Memory cells have the capacity to act quicklywhen confronted with the same infectious organism atlater times. It is the memory cells that cause us tobecome “immune” from later reinfections with thesame organism.HOW DO THE IMMUNE CELLS OFTHE BODY KNOW WHAT TO ATTACKAND WHAT NOT TO?All immune and blood cells develop from multipotenthematopoietic stem cells that originate in the bonemarrow. Upon their departure from the bone marrow,immature T cells undergo a final maturation processin the thymus, a small organ located in the upperchest, before being dispersed to the body with therest of the immune cells (e.g., B cells). Within thethymus, T cells undergo an important process that“educates” them to distinguish between self (theproteins of their own body) and nonself (the invadingorganism’s) antigens. Here, the T cells are selected fortheir ability to bind to the particular MHC proteinsexpressed by the individual. The particular array ofMHCs varies slightly between individuals, and thisvariation is the basis of the immune response when atransplanted organ is rejected. MHCs and other lesseasily characterized molecules called minor histocompatibilityantigens are genetically determinedand this is the reason why donor organs from relativesof the recipient are preferred over unrelated donors.60
Autoimmune Diseases and the Promise of <strong>Stem</strong> Cell-Based TherapiesBox 6.1Immune System Components: Common Terms and DefinitionsAntibody — A Y-shaped protein secreted by B cells inresponse to an antigen. An antibody binds specificallyto the antigen that induced its production. Antibodiesdirected against antigens on the surface of infectiousorganisms help eliminate those organisms from thebody.Antigen — A substance (often a protein) that inducesthe formation of an antibody. Antigens are commonlyfound on the surface of infectious organisms, transfusedblood cells, and organ transplants.Antigen presenting cells (APC) — One of a variety ofcells within the body that can process antigens anddisplay them on their surface in a form recognizableby T cells.Autoantibody — An antibody that reacts with antigensfound on the cells and tissues of an individual’s ownbody. Autoantibodies can cause autoimmune diseases.Autoimmune disease — A condition that results fromthe formation of antibodies that attack the cells ortissues of an individual’s own body.B cells — Also known as B lymphocytes. Each B cellis capable of making one specific antibody. Whenstimulated by antigen and helper T cells, B cells matureinto plasma cells that secrete large amounts of theirspecific antibodyBone marrow — The soft, living tissue that fills mostbone cavities and contains hematopoietic stem cells,from which all red and white blood cells evolve. Thebone marrow also contains mesenchymal stem cellsthat a number of cell types come from, includingchondrocytes, which produce cartilage.Cytokines — A generic term for a large variety ofregulatory proteins produced and secreted by cellsand used to communicate with other cells. One classof cytokines is the interleukins, which act as intercellularmediators during the generation of an immune response.Immune system cells — White blood cells or leukocytesthat originate from the bone marrow. They includeantigen presenting cells, such as dendritic cells, T and Blymphocytes, and neutrophils, among many others.Lymphatic system — A network of lymph vessels andnodes that drain and filter antigens from tissue fluidsbefore returning lymphocytes to the blood.Memory cells — A subset of antigen-specific T or Bcells that “recall” prior exposure to an antigen andrespond quickly without the need to be activatedagain by CD4 helper T cells.Major histocompatibility complex (MHC) — A groupof genes that code for cell-surface histocompatibilityantigens. These antigens are the primary reason whyorgan and tissue transplants from incompatibledonors fail.T cells — Also known as T lymphocytes. There are twoprimary subsets of T cells. CD4 helper T cells (identifiedby the presence of the CD4 protein on their surfaces)are instrumental in initiating an immune response bysupplying special cytokines. CD8 cytotoxic (killer) T cells(identified by the presence of the CD8 protein on theirsurfaces), after being activated by the CD4 helper cells,are capable of killing infected cells in the body. CD4helper T cells are destroyed by the HIV virus in AIDSpatients, resulting in an ineffective immune system.Thymus — A lymphoid organ located in the upperchest cavity. Maturing T cells leave the bone marrowand go directly to the thymus, where they are educatedto discriminate between self and nonself proteins.(See tolerance.)Tolerance — A state of specific immunologicunresponsiveness. Individuals should normally betolerant of the cells and tissues that make up our ownbodies. Should tolerance fail, an autoimmune diseasemay result.In the bone marrow, a highly diverse and randomarray of T cells is produced. Collectively, these T cellsare capable of recognizing an almost unlimitednumber of antigens. Because the process ofgenerating a T cell’s antigen specificity is a randomone, many immature T cells have the potential toreact with the body’s own (self) proteins. To avoid thispotential disaster, the thymus provides an environmentwhere T cells that recognize self-antigens(autoreactive or self-reactive T cells) are deleted orinactivated in a process called tolerance induction.Tolerance usually ensures that T cells do not attackthe “autoantigens” (self-proteins) of the body. Giventhe importance of this task, it is not surprising thatthere are multiple checkpoints for destroying orinactivating T cells that might react to auto-antigens.Autoimmune diseases arise when this intricate systemfor the induction and maintenance of immunetolerance fails. These diseases result in cell and tissuedestruction by antigen-specific CD8 cytotoxic T cellsor autoantibodies (antibodies to self-proteins) and the61
Autoimmune Diseases and the Promise of <strong>Stem</strong> Cell-Based Therapiesaccompanying inflammatory process. Thesemechanisms can lead to the destruction of the jointsin rheumatoid arthritis, the destruction of the insulinproducingbeta cells of the pancreas in type 1diabetes, or damage to the kidneys in lupus. The reasonsfor the failure to induce or maintain toleranceare enigmatic. However, genetic factors, along withenvironmental and hormonal influences and certaininfections, may contribute to tolerance and thedevelopment of autoimmune disease [4, 7].HEMATOPOIETIC STEM CELLTHERAPY FOR AUTOIMMUNEDISEASESThe current treatments for many autoimmune diseasesinclude the systemic use of anti-inflammatory drugsand potent immunosuppressive and immunomodulatoryagents (i.e., steroids and inhibitor proteins thatblock the action of inflammatory cytokines). However,despite their profound effect on immune responses,these therapies are unable to induce clinically significantremissions in certain patients. In recent years,researchers have contemplated the use of stem cellsto treat autoimmune disorders. Discussed here issome of the rationale for this approach, with a focuson experimental stem cell therapies for lupus,rheumatoid arthritis, and type 1 diabetes.The immune-mediated injury in autoimmune diseasescan be organ-specific, such as type 1 diabeteswhich is the consequence of the destruction of thepancreatic beta islet cells or multiple sclerosis whichresults from the breakdown of the myelin covering ofnerves. These autoimmune diseases are amenableto treatments involving the repair or replacement ofdamaged or destroyed cells or tissue (see Chapter 7.<strong>Stem</strong> <strong>Cells</strong> and Diabetes and Chapter 11. Use ofGenetically Modified <strong>Stem</strong> <strong>Cells</strong> in ExperimentalGene Therapies). In contrast, non-organ-specificautoimmune diseases, such as lupus, are characterizedby widespread injury due to immune reactionsagainst many different organs and tissues.One approach is being evaluated in early clinicaltrials of patients with poorly responsive, life-threateninglupus. This is a severe disease affecting multipleorgans in the body including muscles, skin, joints, andkidneys as well as the brain and nerves. Over 239,000Americans, of which more than 90 percent arewomen, suffer from lupus. In addition, lupusdisproportionately afflicts African-American andHispanic women [11]. A major obstacle in the treatmentof non-organ-specific autoimmune diseasessuch as lupus is the lack of a single specific target forthe application of therapy.The objective of hematopoietic stem cell therapy forlupus is to destroy the mature, long-lived, and autoreactiveimmune cells and to generate a new,properly functioning immune system. In most of thesetrials, the patient’s own stem cells have been used ina procedure known as autologous (from “one’s self”)hematopoietic stem cell transplantation. First, patientsreceive injections of a growth factor, which coaxeslarge numbers of hematopoietic stem cells to bereleased from the bone marrow into the blood stream.These cells are harvested from the blood, purifiedaway from mature immune cells, and stored. Aftersufficient quantities of these cells are obtained, thepatient undergoes a regimen of cytotoxic (cell-killing)drug and/or radiation therapy, which eliminates themature immune cells. Then, the hematopoietic stemcells are returned to the patient via a blood transfusioninto the circulation where they migrate to the bonemarrow and begin to differentiate to become matureimmune cells. The body’s immune system is thenrestored. Nonetheless, the recovery phase, until theimmune system is reconstituted represents a period ofdramatically increased susceptibility to bacterial, fungal,and viral infection, making this a high-risk therapy.Recent reports suggest that this replacement therapymay fundamentally alter the patient’s immune system.Richard Burt and his colleagues [18] conducteda long-term follow-up (one to three years) of sevenlupus patients who underwent this procedure andfound that they remained free from active lupus andimproved continuously after transplantation, withoutthe need for immunosuppressive medications. Oneof the hallmarks of lupus is that during the natural progressionof disease, the normally diverse repertoire ofT cells become limited in the number of different antigensthey recognize, suggesting that an increasingproportion of the patient’s T cells are autoreactive.Burt and colleagues found that following hematopoieticstem cell transplantation, levels of T celldiversity were restored to those of healthy individuals.This finding provides evidence that stem cell replacementmay be beneficial in reestablishing tolerance inT cells, thereby decreasing the likelihood of diseasereoccurrence.62
Autoimmune Diseases and the Promise of <strong>Stem</strong> Cell-Based TherapiesDEVELOPMENT OF HEMATOPOIETICSTEM CELL LINES FORTRANSPLANTATIONThe ability to generate and propagate unlimitednumbers of hematopoietic stem cells outside thebody—whether from adult, umbilical cord blood,fetal, or embryonic sources—would have a majorimpact on the safety, cost, and availability of stemcells for transplantation. The current approach ofisolating hematopoietic stem cells from a patient’sown peripheral blood places the patient at risk for aflare-up of their autoimmune disease. This is a potentialconsequence of repeated administration of thestem cell growth factors needed to mobilizehematopoietic stem cells from the bone marrow tothe blood stream in numbers sufficient for transplantation.In addition, contamination of the purifiedhematopoietic stem cells with the patient’s matureautoreactive T and B cells could affect the success ofthe treatment in some patients. Propagation of purecell lines in the laboratory would avoid these potentialdrawbacks and increase the numbers of stem cellsavailable to each patient, thus shortening the at-riskinterval before full immune reconstitution.Whether embryonic stem cells will provide advantagesover stem cells derived from cord blood oradult bone marrow hematopoietic stem cells remainsto be determined. However, hematopoietic stemcells, whether from umbilical cord blood or bonemarrow, have a more limited potential for selfrenewalthan do pluripotent embryonic stem cells.Although new information will be needed to directthe differentiation of embryonic stem cells intohematopoietic stem cells, hematopoietic cells arepresent in differentiated cultures from human embryonicstem cells [9] and from human fetal-derivedembryonic germ stem cells [17].One potential advantage of using hematopoieticstem cell lines for transplantation in patients withautoimmune diseases is that these cells could begenerated from unaffected individuals or, as predisposinggenetic factors are defined, from embryonicstem cells lacking these genetic influences. In addition,use of genetically selected or genetically engineeredcell types may further limit the possibility of diseaseprogression or reemergence.One risk of using nonself hematopoietic stem cells isof immune rejection of the transplanted cells.Immune rejection is caused by MHC protein differencesbetween the donor and the patient (recipient).In this scenario, the transplanted hematopoietic stemcells and their progeny are rejected by the patient’sown T cells, which are originating from the patient’ssurviving bone marrow hematopoietic stem cells. Inthis regard, embryonic stem cell-derived hematopoieticstem cells may offer distinct advantages overcord blood and bone marrow hematopoietic stemcell lines in avoiding rejection of the transplant.Theoretically, banks of embryonic stem cells expressingvarious combinations of the three most criticalMHC proteins could be generated to allow closematching to the recipient’s MHC composition.Additionally, there is evidence that embryonic stemcells are considerably more receptive to geneticmanipulation than are hematopoietic stem cells (seeChapter 11. Use of Genetically Modified <strong>Stem</strong> <strong>Cells</strong> inExperimental Gene Therapies).This characteristic means that embryonic stem cellscould be useful in strategies that could prevent theirrecognition by the patient’s surviving immune cells.For example, it may be possible to introduce therecipient’s MHC proteins into embryonic stem cellsthrough targeted gene transfer. Alternatively, it istheoretically possible to generate a universal donorembryonic stem cell line by genetic alteration orremoval of the MHC proteins. Researchers haveaccomplished this by genetically altering a mouseso that it has little or no surface expression of MHCmolecules on any of the cells or tissues. There is norejection of pancreatic beta islet cells from thesegenetically altered mice when the cells are transplantedinto completely MHC-mismatched mice [13].Additional research will be needed to determine thefeasibility of these alternative strategies for preventionof graft rejection in humans [6].Jon Odorico and colleagues have shown that expressionof MHC proteins on mouse embryonic stem cellsand differentiated embryonic stem cell progeny iseither absent or greatly decreased compared withMHC expression on adult cells [8]. These preliminaryfindings raise the intriguing possibility that lines derivedfrom embryonic stem cells may be inherently lesssusceptible to rejection by the recipient’s immune63
Autoimmune Diseases and the Promise of <strong>Stem</strong> Cell-Based Therapiessystem than lines derived from adult cells. This couldhave important implications for the transplantation ofcells other than hematopoietic stem cells.Another potential advantage of using pure populationsof donor hematopoietic stem cells achievedthrough stem cell technologies would be a lowerincidence and severity of graft-versus-host disease, apotentially fatal complication of bone marrow transplantation.Graft-versus-host disease results from theimmune-mediated injury to recipient tissues thatoccurs when mature organ-donor T cells remain withinthe organ at the time of transplant. Such maturedonor alloreactive T cells would be absent from purepopulations of multipotent hematopoietic stem cells,and under ideal conditions of immune toleranceinduction in the recipient’s thymus, the donor-derivedmature T cell population would be tolerant to the host.GENE THERAPY AND STEM CELLAPPROACHES FOR THE TREATMENTOF AUTOIMMUNE DISEASESGene therapy is the genetic modification of cells toproduce a therapeutic effect (see Chapter 11. Use ofGenetically Modified <strong>Stem</strong> <strong>Cells</strong> in ExperimentalGene Therapies). In most investigational protocols,DNA containing the therapeutic gene is transferredinto cultured cells, and these cells are subsequentlyadministered to the animal or patient. DNA can alsobe injected directly, entering cells at the site of theinjection or in the circulation. Under ideal conditions,cells take up the DNA and produce the therapeuticprotein encoded by the gene.Currently, there is an extensive amount of genetherapy research being conducted in animal modelsof autoimmune disease. The goal is to modify theaberrant, inflammatory immune response that ischaracteristic of autoimmune diseases [15, 19].Researchers most often use one of two generalstrategies to modulate the immune system. The firststrategy is to block the actions of an inflammatorycytokine (secreted by certain activated immune cellsand inflamed tissues) by transferring a gene into cellsthat encodes a “decoy” receptor for that cytokine.Alternatively, a gene is transferred that encodes ananti-inflammatory cytokine, redirecting the autoinflammatoryimmune response to a more “tolerant”state. In many animal studies, promising results havebeen achieved by using these approaches, and thestudies have advanced understanding of the diseaseprocesses and the particular inflammatory cytokinesinvolved in disease progression [15, 19].Serious obstacles to the development of effectivegene therapies for humans remain, however.Foremost among these are the difficulty of reliablytransferring genetic material into adult and slowlydividing cells (including hematopoietic stem cells)and of producing long-lasting expression of theintended protein at levels that can be tightly controlledin response to disease activity. Importantly,embryonic stem cells are substantially more permissiveto gene transfer compared with adult cells, andembryonic cells sustain protein expression duringextensive self-renewal. Whether adult-derived stemcells, other than hematopoietic stem cells, aresimilarly amenable to gene transfer has not yetbeen determined.Ultimately, stem cell gene therapy should allow thedevelopment of novel methods for immune modulationin autoimmune diseases. One example is thegenetic modification of hematopoietic stem cells ordifferentiated tissue cells with a “decoy” receptor forthe inflammatory cytokine interferon gamma to treatlupus. For example, in a lupus mouse model, genetransfer of the decoy receptor, via DNA injection,arrested disease progression [12]. Other investigatorshave used a related but distinct approach in amouse model of type 1 diabetes. Interleukin-12(IL-12), an inflammatory cytokine, plays a prominentrole in the development of diabetes in these mice.The investigators transferred the gene for a modifiedform of IL-12, which blocks the activity of the naturalIL-12, into pancreatic beta islet cells (the target ofautoimmune injury in type 1 diabetes). The islet cellgene therapy prevented the onset of diabetes inthese mice [20]. Theoretically, embryonic stem cellsor adult stem cells could be genetically modifiedbefore or during differentiation into pancreatic betaislet cells to be used for transplantation. The resultingimmune-modulating islet cells might diminish theoccurrence of ongoing autoimmunity, increase thelikelihood of long-term function of the transplantedcells, and eliminate the need for immunosuppressivetherapy following transplantation.Researchers are exploring similar genetic approachesto prevent progressive joint destruction and loss ofcartilage and to repair damaged joints in animal64
Autoimmune Diseases and the Promise of <strong>Stem</strong> Cell-Based Therapiesmodels of rheumatoid arthritis. Rheumatoid arthritis isa debilitating autoimmune disease characterized byacute and chronic inflammation, in which theimmune system primarily attacks the joints of thebody. In a recent study, investigators geneticallytransferred an anti-inflammatory cytokine, interleukin-4(IL-4), into a specialized, highly efficient antigenpresentingcell called a dendritic cell, and theninjected these IL-4-secreting cells into mice that canbe induced to develop a form of arthritis similar torheumatoid arthritis in humans. These IL-4-secretingdendritic cells are presumed to act on the CD4helper T cells to reintroduce tolerance to self-proteins.Treated mice showed complete suppression of theirdisease and, in addition to its immune-modulatoryproperties, IL-4 blocked bone resorption (a seriouscomplication of rheumatoid arthritis), making it aparticularly attractive cytokine for this therapy [10].However, one obstacle to this approach is that humandendritic cells are difficult to isolate in large numbers.Investigators have also directed the differentiation ofdendritic cells from mouse embryonic stem cells,indicating that a stem cell-based approach mightwork in patients with rheumatoid arthritis [5]. Longertermfollow-up and further characterization will beneeded in animal models before researchersproceed with the development of such an approachin humans. In similar studies, using other inhibitors ofinflammatory cytokines such as a decoy receptor fortumor necrosis factor– (a prominent inflammatorycytokine in inflamed joints), an inhibitor of nuclearfactor– (a protein within cells that turns on theproduction of many inflammatory cytokines), andinterleukin-13 (an anti-inflammatory cytokine),researchers have shown promising results in animalmodels of rheumatoid arthritis [19]. Because of thecomplexity and redundancy of immune systemsignaling networks, it is likely that a multifacetedapproach involving inhibitors of several differentinflammatory cytokines will be successful, whereasapproaches targeting single cytokines might fail orproduce only short-lived responses. In addition, othercell types may prove to be even better vehicles forthe delivery of gene therapy in this disease.Chondrocytes, cells that build cartilage in joints, mayprovide another avenue for stem cell-based treatmentof rheumatoid arthritis. These cells have beenderived from human bone marrow stromal stem cellsderived from human bone marrow [14]. Little is knownabout the intermediate cells that ultimately differentiateinto chondrocytes. In addition to adult bonemarrow as a source for stromal stem cells, humanembryonic stem cells can differentiate into precursorcells believed to lead ultimately to the stromal stemcells [16]. However, extensive research is needed toreliably achieve the directed derivation of the stromalstem cells from embryonic stem cells and, subsequently,the differentiation of chondrocytes fromthese stromal stem cells.The ideal cell for optimum cartilage repair may be amore primitive cell than the chondrocyte, such as thestromal cell, or an intermediate cell in the pathway(e.g., a connective tissue precursor) leading to thechondrocyte. Stromal stem cells can generate newchondrocytes and facilitate cartilage repair in a rabbitmodel [3]. Such cells may also prove to be idealtargets for the delivery of immune-modulatory genetherapy. Like hematopoietic stem cells, stromal stemcells have been used in animal models for delivery ofgene therapy [1]. For example, a recent studydemonstrated that genetically engineered chondrocytes,expressing a growth factor, can enhance thefunction of transplanted chondrocytes [2].Two obstacles to the use of adult stromal stem cellsor chondrocytes are the limited numbers of thesecells that can be harvested and the difficulties inpropagating them in the laboratory. Embryonic stemcells, genetically modified and expanded beforedirected differentiation to a connective tissue stemcell, may be an attractive alternative.Collectively, these results illustrate the tremendouspotential these cells may offer for the treatment ofrheumatoid arthritis and other autoimmune diseases.CONCLUSION<strong>Stem</strong> cell-based therapies offer many excitingpossibilities for the development of novel treatments,and perhaps even cures, for autoimmune diseases.A challenging research effort remains to fully realizethis potential and to address the many remainingquestions, which include how best to direct the differentiationof specific cell types and determine whichparticular type of stem cell will be optimum for eachtherapeutic approach. Gene therapy with cytokinesor their inhibitors is still in its infancy, but stem cells or65
Autoimmune Diseases and the Promise of <strong>Stem</strong> Cell-Based Therapiestheir progeny may provide one of the better avenuesfor future delivery of immune-based therapies.Ultimately, the potential to alleviate these devastatingchronic diseases with the use of stem cell-basedtechnologies is enormous.REFERENCES1. Allay, J.A., Dennis, J.E., Haynesworth, S.E., Majumdar, M.K.,Clapp, D.W., Shultz, L.D., Caplan, A.I., and Gerson, S.L.(1997). LacZ and interleukin-3 expression in vivo after retroviraltransduction of marrow-derived human osteogenicmesenchymal progenitors. Hum. Gene Ther. 8, 1417-1427.2. Brower-Toland, B.D., Saxer, R.A., Goodrich, L.R., Mi, Z.,Robbins, P.D., Evans, C.H., and Nixon, A.J. (2001). Directadenovirus-mediated insulin-like growth factor I genetransfer enhances transplant chondrocyte function. Hum.Gene Ther. 12, 117-129.3. Caplan, A.I., Elyaderani, M., Mochizuki, Y., Wakitani, S., andGoldberg, V.M. (1997). Principles of cartilage repair andregeneration. Clin. Orthop. 342, 254-269.4. Cooper, G.S., Dooley, M.A., Treadwell, E.L., St Clair, E.W.,Parks, C.G., and Gilkeson, G.S. (1998). Hormonal, environmental,and infectious risk factors for developing systemiclupus erythematosus. Arthritis Rheum. 41, 1714-1724.5. Fairchild, P.J., Brook, F.A., Gardner, R.L., Graca, L., Strong, V.,Tone, Y., Tone, M., Nolan, K.F., and Waldmann, H. (2000).Directed differentiation of dendritic cells from mouseembryonic stem cells. Curr. Biol. 10, 1515-1518.6. Gearhart, J. (1998). New potential for human embryonicstem cells. Science. 282, 1061-1062.7. Grossman, J.M. and Tsao, B.P. (2000). Genetics and systemiclupus erythematosus. Curr. Rheumatol. Rep. 2, 13-18.8. Harley, C.B., Gearhart, J., Jaenisch, R., Rossant, J., andThomson, J. (2001). Keystone Symposia. Pluripotent stemcells: biology and applications. Durango, CO.9. Itskovitz-Eldor, J., Schuldiner, M., Karsenti, D., Eden, A.,Yanuka, O., Amit, M., Soreq, H., and Benvenisty, N. (2000).Differentiation of human embryonic stem cells into embryoidbodies comprising the three embryonic germ layers.Mol. Med. 6, 88-95.10. Kim, S.H., Kim, S., Evans, C.H., Ghivizzani, S.C., Oligino, T.,and Robbins, P.D. (2001). Effective treatment of establishedmurine collagen-induced arthritis by systemic administrationof dendritic cells genetically modified to express IL-4.J. Immunol. 166, 3499-3505.11. Lawrence, R.C., Helmick, C.G., Arnett, F.C., Deyo, R.A.,Felson, D.T., Giannini, E.H., Heyse, S.P., Hirsch, R., Hochberg,M.C., Hunder, G.G., Liang, M.H., Pillemer, S.R., Steen, V.D.,and Wolfe, F. (1998). Estimates of the prevalence of arthritisand selected musculoskeletal disorders in the United States.Arthritis Rheum. 41, 778-799.12. Lawson, B.R., Prud’homme, G.J., Chang, Y., Gardner, H.A.,Kuan, J., Kono, D.H., and Theofilopoulos, A.N. (2000).Treatment of murine lupus with cDNA encoding IFNgammaR/Fc.J. Clin. Invest. 106, 207-215.13. Osorio, R.W., Ascher, N.L., Jaenisch, R., Freise, C.E., Roberts,J.P., and Stock, P.G. (1993). Major histocompatibility complexclass I deficiency prolongs islet allograft survival.Diabetes. 42, 1520-1527.14. Pittenger, M.F., Mackay, A.M., Beck, S.C., Jaiswal, R.K.,Douglas, R., Mosca, J.D., Moorman, M.A., Simonetti, D.W.,Craig, S., and Marshak, D.R. (1999). Multilineage potentialof adult human mesenchymal stem cells. Science. 284,143-147.15. Prud’homme, G.J. (2000). Gene therapy of autoimmunediseases with vectors encoding regulatory cytokines orinflammatory cytokine inhibitors. J. Gene. Med. 2, 222-232.16. Schuldiner, M., Yanuka, O., Itskovitz-Eldor, J., Melton, D., andBenvenisty, N. (2000). Effects of eight growth factors on thedifferentiation of cells derived from human embryonic stemcells. Proc. Natl. Acad. Sci. U. S. A. 97, 11307-11312.17. Shamblott, M.J., Axelman, J., Littlefield, J.W., Blumenthal,P.D., Huggins, G.R., Cui, Y., Cheng, L., and Gearhart, J.D.(2000). Human embryonic germ cell derivatives express abroad range of develpmentally distinct markers and proliferateextensively in vitro. Proc. Natl. Acad. Sci. U. S. A. 98,113-118.18. Traynor, A.E., Schroeder, J., Rosa, R.M., Cheng, D., Stefka, J.,Mujais, S., Baker, S., and Burt, R.K. (2000). Treatment ofsevere systemic lupus erythematosus with high-dosechemotherapy and haemopoietic stem-cell transplantation:a phase I study. Lancet. 356, 701-707.19. Tsokos, G.C. and Nepom, G.T. (2000). Gene therapy in thetreatment of autoimmune diseases. J. Clin. Invest. 106,181-183.20. Yasuda, H., Nagata, M., Arisawa, K., Yoshida, R., Fujihira, K.,Okamoto, N., Moriyama, H., Miki, M., Saito, I., Hamada, H.,Yokono, K., and Kasuga, M. (1998). Local expression ofimmunoregulatory IL-12p40 gene prolonged syngeneic isletgraft survival in diabetic NOD mice. J. Clin. Invest. 102,1807-1814.66
7.STEM CELLSAND DIABETESDiabetes exacts its toll on many Americans, youngand old. For years, researchers have painstakinglydissected this complicated disease caused by thedestruction of insulin producing islet cells of thepancreas. Despite progress in understanding theunderlying disease mechanisms for diabetes, there isstill a paucity of effective therapies. For years investigatorshave been making slow, but steady, progresson experimental strategies for pancreatic transplantationand islet cell replacement. Now, researchershave turned their attention to adult stem cells thatappear to be precursors to islet cells and embryonicstem cells that produce insulin.INTRODUCTIONFor decades, diabetes researchers have beensearching for ways to replace the insulin-producingcells of the pancreas that are destroyed by apatient’s own immune system. Now it appears thatthis may be possible. Each year, diabetes affectsmore people and causes more deaths than breastcancer and AIDS combined. Diabetes is the seventhleading cause of death in the United States today,with nearly 200,000 deaths reported each year. TheAmerican Diabetes Association estimates that nearly16 million people, or 5.9 percent of the United Statespopulation, currently have diabetes.Diabetes is actually a group of diseases characterizedby abnormally high levels of the sugar glucose inthe bloodstream. This excess glucose is responsiblefor most of the complications of diabetes, whichinclude blindness, kidney failure, heart disease, stroke,neuropathy, and amputations. Type 1 diabetes, alsoknown as juvenile-onset diabetes, typically affectschildren and young adults. Diabetes develops whenthe body’s immune system sees its own cells asforeign and attacks and destroys them. As a result,the islet cells of the pancreas, which normallyproduce insulin, are destroyed. In the absence ofinsulin, glucose cannot enter the cell and glucoseaccumulates in the blood. Type 2 diabetes, alsocalled adult-onset diabetes, tends to affect older,sedentary, and overweight individuals with a familyhistory of diabetes. Type 2 diabetes occurs when thebody cannot use insulin effectively. This is calledinsulin resistance and the result is the same as withtype 1 diabetes—a build up of glucose in the blood.There is currently no cure for diabetes. People withtype 1 diabetes must take insulin several times a dayand test their blood glucose concentration three tofour times a day throughout their entire lives. Frequentmonitoring is important because patients who keeptheir blood glucose concentrations as close tonormal as possible can significantly reduce many ofthe complications of diabetes, such as retinopathy(a disease of the small blood vessels of the eyewhich can lead to blindness) and heart disease,that tend to develop over time. People with type 2diabetes can often control their blood glucoseconcentrations through a combination of diet,exercise, and oral medication. Type 2 diabetesoften progresses to the point where only insulintherapy will control blood glucose concentrations.Each year, approximately 1,300 people with type 1diabetes receive whole-organ pancreas transplants.After a year, 83 percent of these patients, onaverage, have no symptoms of diabetes and donot have to take insulin to maintain normal glucoseconcentrations in the blood. However, the demandfor transplantable pancreases outweighs theiravailability. To prevent the body from rejecting thetransplanted pancreas, patients must take powerfuldrugs that suppress the immune system for their entirelives, a regimen that makes them susceptible to a67
<strong>Stem</strong> <strong>Cells</strong> and Diabeteshost of other diseases. Many hospitals will not performa pancreas transplant unless the patient also needs akidney transplant. That is because the risk of infectiondue to immunosuppressant therapy can be a greaterhealth threat than the diabetes itself. But if a patient isalso receiving a new kidney and will require immunosuppressantdrugs anyway, many hospitals willperform the pancreas transplant.Over the past several years, doctors have attemptedto cure diabetes by injecting patients with pancreaticislet cells—the cells of the pancreas that secreteinsulin and other hormones. However, the requirementfor steroid immunosuppressant therapy to preventrejection of the cells increases the metabolicdemand on insulin-producing cells and eventuallythey may exhaust their capacity to produce insulin.The deleterious effect of steroids is greater for isletcell transplants than for whole-organ transplants. Asa result, less than 8 percent of islet cell transplantsperformed before last year had been successful.More recently, James Shapiro and his colleagues inEdmonton, Alberta, Canada, have developed anexperimental protocol for transplanting islet cells thatinvolves using a much larger amount of islet cells anda different type of immunosuppressant therapy. In arecent study, they report that [17], seven of sevenpatients who received islet cell transplants no longerneeded to take insulin, and their blood glucoseconcentrations were normal a year after surgery.The success of the Edmonton protocol is now beingtested at 10 centers around the world.If the success of the Edmonton protocol can beduplicated, many hurdles still remain in using thisapproach on a wide scale to treat diabetes. First,donor tissue is not readily available. Islet cells used intransplants are obtained from cadavers, and the procedurerequires at least two cadavers per transplant.The islet cells must be immunologically compatible,and the tissue must be freshly obtained—within eighthours of death. Because of the shortage of organdonors, these requirements are difficult to meet andthe waiting list is expected to far exceed availabletissue, especially if the procedure becomes widelyaccepted and available. Further, islet cell transplantrecipients face a lifetime of immunosuppressanttherapy, which makes them susceptible to otherserious infections and diseases.DEVELOPMENT OF THE PANCREASBefore discussing cell-based therapies for diabetes,it is important to understand how the pancreasdevelops. In mammals, the pancreas contains threeclasses of cell types: the ductal cells, the acinar cells,and the endocrine cells. The endocrine cells producethe hormones glucagon, somatostatin, pancreaticpolypeptide (PP), and insulin, which are secreted intothe blood stream and help the body regulate sugarmetabolism. The acinar cells are part of the exocrinesystem, which manufactures digestive enzymes, andductal cells from the pancreatic ducts, whichconnect the acinar cells to digestive organs.In humans, the pancreas develops as an outgrowthof the duodenum, a part of the small intestine. Thecells of both the exocrine system—the acinar cells—and of the endocrine system—the islet cells—seemto originate from the ductal cells during development.During development these endocrine cellsemerge from the pancreatic ducts and formaggregates that eventually form what is known asIslets of Langerhans. In humans, there are four typesof islet cells: the insulin-producing beta cells; thealpha cells, which produce glucagon; the delta cells,which secrete somatostatin; and the PP-cells, whichproduce pancreatic polypeptide. The hormonesreleased from each type of islet cell have a role inregulating hormones released from other islet cells. Inthe human pancreas, 65 to 90 percent of islet cellsare beta cells, 15 to 20 percent are alpha-cells, 3 to10 percent are delta cells, and one percent is PPcells. Acinar cells form small lobules contiguous withthe ducts (see Figure 7.1. Insulin Production in theHuman Pancreas). The resulting pancreas is acombination of a lobulated, branched acinar glandthat forms the exocrine pancreas, and, embeddedin the acinar gland, the Islets of Langerhans, whichconstitute the endocrine pancreas.During fetal development, new endocrine cellsappear to arise from progenitor cells in the pancreaticducts. Many researchers maintain that somesort of islet stem cell can be found intermingled withductal cells during fetal development and that thesestem cells give rise to new endocrine cells as thefetus develops. Ductal cells can be distinguishedfrom endocrine cells by their structure and by thegenes they express. For example, ductal cellstypically express a gene known as cytokeratin-968
<strong>Stem</strong> <strong>Cells</strong> and DiabetesHuman pancreasIslet ofLangerhansBeta cellMuscle fiberBloodvesselInsulin© 2001 Terese Winslow, Lydia KibiukGlucoseFigure 7.1. Insulin Production in the Human Pancreas.The pancreas is located in the abdomen, adjacent to the duodenum (the first portion of the small intestine). A cross-sectionof the pancreas shows the islet of Langerhans which is the functional unit of the endocrine pancreas. Encircled is the betacell that synthesizes and secretes insulin. Beta cells are located adjacent to blood vessels and can easily respond tochanges in blood glucose concentration by adjusting insulin production. Insulin facilitates uptake of glucose, the main fuelsource, into cells of tissues such as muscle.69
<strong>Stem</strong> <strong>Cells</strong> and Diabetes(CK-9), which encodes a structural protein. Beta isletcells, on the other hand, express a gene calledPDX-1, which encodes a protein that initiatestranscription from the insulin gene. These genes,called cell markers, are useful in identifying particularcell types.Following birth and into adulthood, the source of newislet cells is not clear, and some controversy existsover whether adult stem cells exist in the pancreas.Some researchers believe that islet stem cell-like cellscan be found in the pancreatic ducts and even inthe islets themselves. Others maintain that the ductalcells can differentiate into islet precursor cells, whileothers hold that new islet cells arise from stem cells inthe blood. Researchers are using several approachesfor isolating and cultivating stem cells or islet precursorcells from fetal and adult pancreatic tissue. Inaddition, several new promising studies indicate thatinsulin-producing cells can be cultivated from embryonicstem cell lines.DEVELOPMENT OF CELL-BASEDTHERAPIES FOR DIABETESIn developing a potential therapy for patients withdiabetes, researchers hope to develop a system thatmeets several criteria. Ideally, stem cells should beable to multiply in culture and reproduce themselvesexactly. That is, the cells should be self-renewing.<strong>Stem</strong> cells should also be able to differentiate invivo to produce the desired kind of cell. For diabetestherapy, it is not clear whether it will be desirable toproduce only beta cells—the islet cells that manufactureinsulin—or whether other types of pancreatic isletcells are also necessary. Studies by Bernat Soria andcolleagues, for example, indicate that isolated betacells—those cultured in the absence of the othertypes of islet cells—are less responsive to changes inglucose concentration than intact islet clusters madeup of all islet cell types. Islet cell clusters typicallyrespond to higher-than-normal concentrations ofglucose by releasing insulin in two phases: a quickrelease of high concentrations of insulin and a slowerrelease of lower concentrations of insulin. In thismanner the beta cells can fine-tune their responseto glucose. Extremely high concentrations of glucosemay require that more insulin be released quickly,while intermediate concentrations of glucose can behandled by a balance of quickly and slowlyreleased insulin.Isolated beta cells, as well as islet clusters withlower-than-normal amounts of non-beta cells, do notrelease insulin in this biphasic manner. Instead insulinis released in an all-or-nothing manner, with nofine-tuning for intermediate concentrations of glucosein the blood [5, 18]. Therefore, many researchersbelieve that it will be preferable to develop a systemin which stem or precursor cell types can becultured to produce all the cells of the islet cluster inorder to generate a population of cells that will beable to coordinate the release of the appropriateamount of insulin to the physiologically relevantconcentrations of glucose in the blood.FETAL TISSUE AS SOURCE FORISLET CELLSSeveral groups of researchers are investigating theuse of fetal tissue as a potential source of islet progenitorcells. For example, using mice, researchershave compared the insulin content of implants fromseveral sources of stem cells—fresh human fetalpancreatic tissue, purified human islets, and culturedislet tissue [2]. They found that insulin content wasinitially higher in the fresh tissue and purified islets.However, with time, insulin concentration decreasedin the whole tissue grafts, while it remained the samein the purified islet grafts. When cultured islets wereimplanted, however, their insulin content increasedover the course of three months. The researchersconcluded that precursor cells within the culturedislets were able to proliferate (continue to replicate)and differentiate (specialize) into functioning islettissue, but that the purified islet cells (alreadydifferentiated) could not further proliferate whengrafted. Importantly, the researchers found, however,that it was also difficult to expand cultures of fetal isletprogenitor cells in culture [7].ADULT TISSUE AS SOURCE FORISLET CELLSMany researchers have focused on culturing islet cellsfrom human adult cadavers for use in developingtransplantable material. Although differentiated betacells are difficult to proliferate and culture, someresearchers have had success in engineering suchcells to do this. For example, Fred Levine and hiscolleagues at the University of California, San Diego,have engineered islet cells isolated from humancadavers by adding to the cells’ DNA special genes70
<strong>Stem</strong> <strong>Cells</strong> and Diabetesthat stimulate cell proliferation. However, becauseonce such cell lines that can proliferate in culture areestablished, they no longer produce insulin. The celllines are further engineered to express the beta isletcell gene, PDX-1, which stimulates the expression ofthe insulin gene. Such cell lines have been shown topropagate in culture and can be induced todifferentiate to cells, which produce insulin. Whentransplanted into immune-deficient mice, the cellssecrete insulin in response to glucose. The researchersare currently investigating whether these cells willreverse diabetes in an experimental diabetesmodel in mice [6, 8].These investigators report that these cells do notproduce as much insulin as normal islets, but it iswithin an order of magnitude. The major problem indealing with these cells is maintaining the delicatebalance between growth and differentiation. <strong>Cells</strong>that proliferate well do not produce insulin efficiently,and those that do produce insulin do not proliferatewell. According to the researchers, the major issue isdeveloping the technology to be able to grow largenumbers of these cells that will reproducibly producenormal amounts of insulin [9].Another promising source of islet progenitor cells liesin the cells that line the pancreatic ducts. Someresearchers believe that multipotent (capable offorming cells from more than one germ layer) stemcells are intermingled with mature, differentiated ductcells, while others believe that the duct cellsthemselves can undergo a differentiation, or areversal to a less mature type of cell, which can thendifferentiate into an insulin-producing islet cell.Susan Bonner-Weir and her colleagues reported lastyear that when ductal cells isolated from adulthuman pancreatic tissue were cultured, they couldbe induced to differentiate into clusters thatcontained both ductal and endocrine cells. Overthe course of three to four weeks in culture, the cellssecreted low amounts of insulin when exposed tolow concentrations of glucose, and higher amountsof insulin when exposed to higher glucoseconcentrations. The researchers have determinedby immunochemistry and ultrastructural analysis thatthese clusters contain all of the endocrine cells ofthe islet [4].Bonner-Weir and her colleagues are working withprimary cell cultures from duct cells and have notestablished cells lines that can grow indefinitely.However the cells can be expanded. According tothe researchers, it might be possible in principle to doa biopsy and remove duct cells from a patient andthen proliferate the cells in culture and give thepatient back his or her own islets. This would work withpatients who have type 1 diabetes and who lackfunctioning beta cells, but their duct cells remainintact. However, the autoimmune destruction wouldstill be a problem and potentially lead to destructionof these transplanted cells [3]. Type 2 diabetespatients might benefit from the transplantation ofcells expanded from their own duct cells since theywould not need any immunosuppression. However,many researchers believe that if there is a geneticcomponent to the death of beta cells, then betacells derived from ductal cells of the same individualwould also be susceptible to autoimmune attack.Some researchers question whether the ductal cellsare indeed undergoing a dedifferentiation or whethera subset of stem-like or islet progenitors populate thepancreatic ducts and may be co-cultured alongwith the ductal cells. If ductal cells die off but isletprecursors proliferate, it is possible that the isletprecursor cells may overtake the ductal cells inculture and make it appear that the ductal cellsare dedifferentiating into stem cells. According toBonner-Weir, both dedifferentiated ductal cells andislet progenitor cells may occur in pancreatic ducts.Ammon Peck of the University of Florida, VijayakumarRamiya of Ixion Biotechnology in Alachua, FL, andtheir colleagues [13, 14] have also cultured cells fromthe pancreatic ducts from both humans and mice.Last year, they reported that pancreatic ductalepithelial cells from adult mice could be cultured toyield islet-like structures similar to the cluster of cellsfound by Bonner-Weir. Using a host of islet-cell markersthey identified cells that produced insulin, glucagon,somatostatin, and pancreatic polypeptide. When thecells were implanted into diabetic mice, the diabeteswas reversed.Joel Habener has also looked for islet-like stem cellsfrom adult pancreatic tissue. He and his colleagueshave discovered a population of stem-like cells withinboth the adult pancreas islets and pancreatic ducts.These cells do not express the marker typical ofductal cells, so they are unlikely to be ductal cells,according to Habener. Instead, they express a markercalled nestin, which is typically found in developing71
<strong>Stem</strong> <strong>Cells</strong> and Diabetesneural cells. The nestin-positive cells do not expressmarkers typically found in mature islet cells. However,depending upon the growth factors added, the cellscan differentiate into different types of cells, includingliver, neural, exocrine pancreas, and endocrine pancreas,judged by the markers they express, and canbe maintained in culture for up to eight months [20].EMBRYONIC STEM CELLSThe discovery of methods to isolate and grow humanembryonic stem cells in 1998 renewed the hopes ofdoctors, researchers, and diabetes patients and theirfamilies that a cure for type 1 diabetes, and perhapstype 2 diabetes as well, may be within strikingdistance. In theory, embryonic stem cells could becultivated and coaxed into developing into theinsulin-producing islet cells of the pancreas. With aready supply of cultured stem cells at hand, thetheory is that a line of embryonic stem cells couldbe grown up as needed for anyone requiring atransplant. The cells could be engineered to avoidimmune rejection. Before transplantation, they couldbe placed into nonimmunogenic material so thatthey would not be rejected and the patient wouldavoid the devastating effects of immunosuppressantdrugs. There is also some evidence that differentiatedcells derived from embryonic stem cells might beless likely to cause immune rejection (see Chapter10. Assessing Human <strong>Stem</strong> Cell Safety). Althoughhaving a replenishable supply of insulin-producingcells for transplant into humans may be a long wayoff, researchers have been making remarkableprogress in their quest for it. While some researchershave pursued the research on embryonic stem cells,other researchers have focused on insulin-producingprecursor cells that occur naturally in adult andfetal tissues.Since their discovery three years ago, several teamsof researchers have been investigating the possibilitythat human embryonic stem cells could bedeveloped as a therapy for treating diabetes.Recent studies in mice show that embryonic stemcells can be coaxed into differentiating intoinsulin-producing beta cells, and new reports indicatethat this strategy may be possible using humanembryonic cells as well.Last year, researchers in Spain reported using mouseembryonic stem cells that were engineered to allowresearchers to select for cells that were differentiatinginto insulin-producing cells [19]. Bernat Soria and hiscolleagues at the Universidad Miguel Hernandez inSan Juan, Alicante, Spain, added DNA containingpart of the insulin gene to embryonic cells from mice.The insulin gene was linked to another gene thatrendered the mice resistant to an antibiotic drug. Bygrowing the cells in the presence of an antibiotic,only those cells that were activating the insulinpromoter were able to survive. The cells were clonedand then cultured under varying conditions. <strong>Cells</strong>cultured in the presence of low concentrations ofglucose differentiated and were able to respond tochanges in glucose concentration by increasinginsulin secretion nearly sevenfold. The researchersthen implanted the cells into the spleens ofdiabetic mice and found that symptoms ofdiabetes were reversed.Manfred Ruediger of Cardion, Inc., in Erkrath,Germany, is using the approach developed by Soriaand his colleagues to develop insulin-producinghuman cells derived from embryonic stem cells. Byusing this method, the non-insulin-producing cells willbe killed off and only insulin-producing cells shouldsurvive. This is important in ensuring that undifferentiatedcells are not implanted that could give rise totumors [15]. However, some researchers believe thatit will be important to engineer systems in which allthe components of a functioning pancreatic islet areallowed to develop.Recently Ron McKay and his colleagues described aseries of experiments in which they induced mouseembryonic cells to differentiate into insulin-secretingstructures that resembled pancreatic islets [10].McKay and his colleagues started with embryonicstem cells and let them form embryoid bodies—anaggregate of cells containing all three embryonicgerm layers. They then selected a population of cellsfrom the embryoid bodies that expressed the neuralmarker nestin (see Appendix B. Mouse Embryonic<strong>Stem</strong> <strong>Cells</strong>). Using a sophisticated five-stage culturingtechnique, the researchers were able to induce thecells to form islet-like clusters that resembled thosefound in native pancreatic islets. The cells respondedto normal glucose concentrations by secreting insulin,although insulin amounts were lower than thosesecreted by normal islet cells (see Figure 7.2.Development of Insulin-Secreting Pancreatic-Like<strong>Cells</strong> From Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>). Whenthe cells were injected into diabetic mice, they72
<strong>Stem</strong> <strong>Cells</strong> and DiabetesMouse blastocystInner cell massMouse embryoniccellsPancreaticislet-likecells secreteinsulinDifferentiationDiabetic mousePancreaticislet-like cells© 2001 Terese Winslow, Lydia KibiukInsulin secretedFigure 7.2. Development of Insulin-Secreting Pancreatic-Like <strong>Cells</strong> From Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>.Mouse embryonic stem cells were derived from the inner cell mass of the early embryo (blastocyst) and cultured underspecific conditions. The embryonic stem cells (in blue) were then expanded and differentiated. <strong>Cells</strong> with markers consistentwith islet cells were selected for further differentiation and characterization. When these cells (in purple) were grown in culture,they spontaneously formed three-dimentional clusters similar in structure to normal pancreatic islets. The cells produced andsecreted insulin. As depicted in the chart, the pancreatic islet-like cells showed an increase in release of insulin as the glucoseconcentration of the culture media was increased. When the pancreatic islet-like cells were implanted in the shoulder of diabeticmice, the cells became vascularized, synthesized insulin, and maintained physical characteristics similar to pancreatic islets.73
<strong>Stem</strong> <strong>Cells</strong> and Diabetessurvived, although they did not reverse the symptomsof diabetes.According to McKay, this system is unique in that theembryonic cells form a functioning pancreatic islet,complete with all the major cell types. The cellsassemble into islet-like structures that contain anotherlayer, which contains neurons and is similar to intactislets from the pancreas [11]. Several research groupsare trying to apply McKay’s results with mice toinduce human embryonic stem cells to differentiateinto insulin-producing islets.Recent research has also provided more evidencethat human embryonic cells can develop into cellsthat can and do produce insulin. Last year, Melton,Nissim Benvinisty of the Hebrew University inJerusalem, and Josef Itskovitz-Eldor of the Technion inHaifa, Israel, reported that human embryonic stemcells could be manipulated in culture to express thePDX-1 gene, a gene that controls insulin transcription[16]. In these experiments, researchers culturedhuman embryonic stem cells and allowed them tospontaneously form embryoid bodies (clumps ofembryonic stem cells composed of many types ofcells from all three germ layers). The embryoid bodieswere then treated with various growth factors, includingnerve growth factor. The researchers found thatboth untreated embryoid bodies and those treatedwith nerve growth factor expressed PDX-1. Embryonicstem cells prior to formation of the aggregatedembryoid bodies did not express PDX-1. Becauseexpression of the PDX-1 gene is associated with theformation of beta islet cells, these results suggest thatbeta islet cells may be one of the cell types thatspontaneously differentiate in the embryoid bodies.The researchers now think that nerve growthfactor may be one of the key signals for inducingthe differentiation of beta islet cells and can beexploited to direct differentiation in the laboratory.Complementing these findings is work done by JonOdorico of the University of Wisconsin in Madisonusing human embryonic cells of the same source.In preliminary findings, he has shown that humanembryonic stem cells can differentiate and expressthe insulin gene [12].More recently, Itskovitz-Eldor and his Technioncolleagues further characterized insulin-producingcells in embryoid bodies [1]. The researchers foundthat embryonic stem cells that were allowed tospontaneously form embryoid bodies contained asignificant percentage of cells that express insulin.Based on the binding of antibodies to the insulinprotein, Itskovitz-Eldor estimates that 1 to 3 percentof the cells in embryoid bodies are insulin-producingbeta-islet cells. The researchers also found that cellsin the embryoid bodies express glut-2 and islet-specificglucokinase, genes important for beta cell functionand insulin secretion. Although the researchers didnot measure a time-dependent response to glucose,they did find that cells cultured in the presence ofglucose secrete insulin into the culture medium. Theresearchers concluded that embryoid bodies containa subset of cells that appear to function as beta cellsand that the refining of culture conditions may soonyield a viable method for inducing the differentiationof beta cells and, possibly, pancreatic islets.Taken together, these results indicate that the developmentof a human embryonic stem cell system thatcan be coaxed into differentiating into functioninginsulin-producing islets may soon be possible.FUTURE DIRECTIONSUltimately, type 1 diabetes may prove to beespecially difficult to cure, because the cells aredestroyed when the body’s own immune systemattacks and destroys them. This autoimmunity mustbe overcome if researchers hope to use transplantedcells to replace the damaged ones. Manyresearchers believe that at least initially, immunosuppressivetherapy similar to that used in the Edmontonprotocol will be beneficial. A potential advantage ofembryonic cells is that, in theory, they could beengineered to express the appropriate genes thatwould allow them to escape or reduce detection bythe immune system. Others have suggested that atechnology should be developed to encapsulate orembed islet cells derived from islet stem or progenitorcells in a material that would allow small moleculessuch as insulin to pass through freely, but would notallow interactions between the islet cells and cells ofthe immune system. Such encapsulated cells couldsecrete insulin into the blood stream, but remaininaccessible to the immune system.Before any cell-based therapy to treat diabetesmakes it to the clinic, many safety issues must beaddressed (see Chapter 10. Assessing Human <strong>Stem</strong>Cell Safety). A major consideration is whether any74
<strong>Stem</strong> <strong>Cells</strong> and Diabetesprecursor or stem-like cells transplanted into the bodymight revert to a more pluripotent state and inducethe formation of tumors. These risks would seeminglybe lessened if fully differentiated cells are used intransplantation.But before any kind of human islet-precursor cellscan be used therapeutically, a renewable source ofhuman stem cells must be developed. Althoughmany progenitor cells have been identified in adulttissue, few of these cells can be cultured for multiplegenerations. Embryonic stem cells show the greatestpromise for generating cell lines that will be free ofcontaminants and that can self renew. However,most researchers agree that until a therapeuticallyuseful source of human islet cells is developed, allavenues of research should be exhaustivelyinvestigated, including both adult and embryonicsources of tissue.REFERENCES1. Assady, S., Maor, G., Amit, M., Itskovitz-Eldor, J., Skorecki,K.L., and Tzukerman, M. (2001). Insulin production byhuman embryonic stem cells. Diabetes. 50.http://www.diabetes.org/Diabetes_Rapids/Suheir_Assady_06282001.pdf2. Beattie, G.M., Otonkoski, T., Lopez, A.D., and Hayek, A.(1997). Functional beta-cell mass after transplantation ofhuman fetal pancreatic cells: differentiation or proliferation?Diabetes. 46, 244-248.3. Bonner-Weir, S., personal communication.4. Bonner-Weir, S., Taneja, M., Weir, G.C., Tatarkiewicz, K., Song,K.H., Sharma, A., and O'Neil, J.J. (2000). In vitro cultivationof human islets from expanded ductal tissue. Proc. Natl.Acad. Sci. U. S. A. 97, 7999-8004.5. Bosco, D. and Meda, P. (1997). Reconstructing islet functionin vitro. Adv. Exp. Med. Biol. 426, 285-298.6. Dufayet de la Tour, D., Halvorsen, T., Demeterco, C.,Tyrberg, B., Itkin-Ansari, P., Loy, M., Yoo, S.J., Hao, S., Bossie,S., and Levine, F. (2001). b-cell differentiation from ahuman pancreatic cell line in vitro and in vivo. Mol.Endocrinol. 15, 476-483.7. Hayek, A., personal communication.8. Itkin-Ansari, P., Demeterco, C., Bossie, S., Dufayet de la Tour,D., Beattie, G.M., Movassat, J., Mally, M.I., Hayek, A., andLevine, F. (2001). PDX-1 and cell-cell contact act in synergyto promote d-cell development in a human pancreaticendocrine precursor cell line. Mol. Endocrinol. 14, 814-822.9. Levine, F., personal communication.10. Lumelsky, N., Blondel, O., Laeng, P., Velasco, I., Ravin, R.,and McKay, R. (2001). Differentiation of Embryonic <strong>Stem</strong><strong>Cells</strong> to Insulin-Secreting Structures Similiar to PancreaticIslets. Science. 292, 1389-1394.11. McKay, R., personal communication12. Odorico, J. S., personal communication.13. Peck, A., personal communication.14. Ramiya, V. K., personal communication.15. Ruediger, M., personal communication.16. Schuldiner, M., Yanuka, O., Itskovitz-Eldor, J., Melton, D., andBenvenisty, N. (2000). Effects of eight growth factors on thedifferentiation of cells derived from human embryonic stemcells. Proc. Natl. Acad. Sci. U. S. A. 97, 11307-11312.17. Shapiro, J., Lakey, J.R.T., Ryan, E.A., Korbutt, G.S., Toth, E.,Warnock, G.L., Kneteman, N.M., and Rajotte, R.V. (2000).Islet transplantation in seven patients with type 1 diabetesmellitus using a glucocorticoid-free immunosuppressiveregimen. N. Engl. J. Med. 343, 230-238.18. Soria, B., Martin, F., Andreu, E., Sanchez-Andrés, J.V.,Nacher, V., and Montana, E. (1996). Diminished fraction ofblockable ATP-sensitive K+ channels in islets transplantedinto diabetic mice. Diabetes. 45, 1755-1760.19. Soria, B., Roche, E., Berná, G., Leon-Quinto, T., Reig, J.A.,and Martin, F. (2000). Insulin-secreting cells derived fromembryonic stem cells normalize glycemia in streptozotocininduceddiabetic mice. Diabetes. 49, 157-162.20. Zulewski, H., Abraham, E.J., Gerlach, M.J., Daniel, P.B.,Moritz, W., Muller, B., Vallejo, M., Thomas, M.K., andHabener, J.F. (2001). Multipotential nestin-positive stem cellsisolated from adult pancreatic islets differentiate ex vivointo pancreatic endocrine, exocrine, and hepatic phenotypes.Diabetes. 50, 521-533.75
<strong>Stem</strong> <strong>Cells</strong> and DiabetesThis page intentionally left blank76
8.REBUILDING THE NERVOUSSYSTEM WITH STEM CELLSToday, most treatments for damage to the brain orspinal cord aim to relieve symptoms and limit furtherdamage. But recent research into the regenerationmechanisms of the central nervous system, includingthe discovery of stem cells in the adult brain that cangive rise to new neurons and neural support cells,has raised hopes that researchers can find ways toactually repair central nervous system damage.Research on stem cells in nervous system disorders isone of the few areas in which there is evidence thatcell-replacement therapy can restore lost function.STEM CELLS BRING NEWSTRATEGIES FOR DEVELOPINGREPLACEMENT NEURONSJust a decade ago, neuroscience textbooks heldthat neurons in the adult human brain and spinalcord could not regenerate. Once dead, it wasthought, central nervous system neurons were gonefor good. Because rebuilding nervous tissue seemedout of the question, research focused almost entirelyon therapeutic approaches to limiting further damage.That dogma that brain tissue could not be regeneratedis history. In the mid-1990s, neuroscientists learned thatsome parts of the adult human brain do, in fact, generatenew neurons, at least under certain circumstances.Moreover, they found that the new neurons arise from"neural stem cells” in the fetal as well as the adult brain(see Chapter 4. The Adult <strong>Stem</strong> Cell). These undifferentiatedcells resemble cells in a developing fetus that giverise to the brain and spinal cord. The researchers alsofound that these neural stem cells could generatemany, if not all, types of cells found in the brain. Thisincludes neurons—the main message carriers in thenervous system, which use long, thin projections calledaxons to transmit signals over long distances—as wellas crucial neural-support cells called oligodendrocytesand astrocytes (see Figure 8.1. The Neuron).The discovery of a regenerative capacity in the adultcentral nervous system holds out the promise that itmay eventually be possible to repair damage fromterrible degenerative diseases such as Parkinson’sDisease and amyotrophic lateral sclerosis (ALS, alsoknown as Lou Gehrig’s disease), as well as from brainand spinal cord injuries resulting from stroke or trauma(see Box 8.1. Early Research Shows <strong>Stem</strong> <strong>Cells</strong> CanImprove Movement in Paralyzed Mice).Researchers are pursuing two fundamental strategiesto exploit this discovery. One is to grow differentiatedcells in a laboratory dish that are suitable for implantationinto a patient by starting with undifferentiatedneural cells. The idea is either to treat the cells in cultureto nudge them toward the desired differentiatedneuronal cell type before implantation, or to implantthem directly and rely on signals inside the body todirect their maturation into the right kind of brain cell.A variety of stem cells might be used for this task,including so-called “neural precursor cells” that areinwardly committed to differentiating into a particularcell type but are outwardly not yet changed orpluripotent embryonic stem cells—cells derived froma very early stage human embryo that retain thecapacity to become any cell type in the body andthat can be maintained in culture for a very longtime without differentiating.The other repair strategy relies on finding growthhormones and other “trophic factors”—growth factors,hormones, and other signaling molecules thathelp cells survive and grow—that can fire up apatient’s own stem cells and endogenous repairmechanisms, to allow the body to cope with damagefrom disease or injury. Researchers are vigorouslypursuing both strategies to find therapies for centralnervous system disorders that involve cell death, buta great deal more basic research must be carriedout before effective new therapies emerge.77
Rebuilding the Nervous System with <strong>Stem</strong> <strong>Cells</strong>DendritesCell BodyAxonOligodendrocyteMyelin sheathSynapticterminalReceptorPostsynapticmembraneNeurotransmitterreleaseSynapse© 2001 Terese WinslowFigure 8.1. The Neuron.When sufficient neurotransmitters cross synapses and bind receptors on the neuronal cell body and dendrites, the neuronsends an electrical signal down its axon to synaptic terminals, which in turn release neurotransmitters into the synapse thataffects the following neuron. The brain neurons that die in Parkinson's Disease release the transmitter dopamine.Oligodendrocytes supply the axon with an insulating myelin sheath.78
Rebuilding the Nervous System with <strong>Stem</strong> <strong>Cells</strong>Researchers at Johns Hopkins University recently reportedpreliminary evidence that cells derived from embryonicstem cells can restore movement in an animal modelof amyotrophic lateral sclerosis (ALS) [1]. This degenerativedisorder, also called as Lou Gehrig’s disease, progressivelydestroys special nerves found in the spinalcord, known as motor neurons, that control movement.Patients with ALS develop increasing muscle weaknessover months to years, which ultimately leads to paralysisand death. The cause is largely unknown, and there areno effective treatments.In this new study, the researchers used a rat model ofALS to test for possible nerve cell- restoring properties ofstem cells. The rats were exposed to Sindbis virus, whichinfects the central nervous system and destroys themotor neurons in the spinal cord. Rats that survive areleft with paralyzed muscles in their hindquarters andweakened back limbs. Scientists assess the degree ofimpairment by measuring the rats’ movement, quantifyingelectrical activity in the nerves serving the backlimbs, and visually judging the extent of nerve damagethrough a microscope.The researchers wanted to see whether stem cells couldrestore nerves and improve mobility in rats. Because scientistshave had difficulty sustaining stem cell linesderived from rat embryos, the investigators conductedtheir experiments with embryonic germ cells that JohnGearhart and colleagues isolated from human fetal tissuein 1998. These cells can produce unchangedcopies of themselves when maintained in culture, andthey form into clumps called embryoid bodies. Undercertain conditions, research has shown that the cells inthe embryoid bodies begin to look and function likeneurons when subjected to specific laboratory conditions[2]. The researchers had an idea that these embryoidbody cells in their nonspecialized state mightbecome specialized as replacement neurons if placedinto the area of the damaged spinal cord. So theycarefully prepared cells from the embryoid bodies andinjected them into the fluid surrounding the spinal cordof the paralyzed rats that had their motor neuronsdestroyed by the Sindbis virus.Box 8.1Early Research Shows <strong>Stem</strong> <strong>Cells</strong>Can Improve Movement in Paralyzed MiceTo test this idea, the researchers selected from laboratoryculture dishes barely differentiated embryonic germscells that displayed the molecular markers of neuralstem cells, including the proteins nestin and neuron specificenolase. They grew these cells in large quantitiesand injected them into the fluid surrounding the spinalcords of partially paralyzed, Sindbis-virus-treated rats.The response was impressive. Three months after theinjections, many of the treated rats were able to movetheir hind limbs and walk, albeit clumsily, while the ratsthat did not receive cell injections remained paralyzed.Moreover, at autopsy the researchers found that cellsderived from human embryonic germ cells had migratedthroughout the spinal fluid and continued to develop,displaying both the shape and molecular markerscharacteristic of mature motor neurons. The researchersare quick to caution that their results are preliminary,and that they do not know for certain whether the treatmenthelped the paralyzed rats because new neuronstook the place of the old, or because trophic factorsfrom the injected cells facilitated the recovery of therats’ remaining nerve cells and helped the rats improvein their ability to use their hind limbs. Nor do they knowhow well this strategy will translate into a therapy forhuman neurodegenerative diseases like ALS. And theyemphasize that there are many hurdles to cross beforethe use of stem cells to repair damaged motor neuronsin patients can be considered. Nevertheless, researchersare excited about these results, which, if confirmed,would represent a major step toward using specializedstem cells from embryonic and fetal tissue sources torestore nervous system function.REFERENCES1. Kerr, D.A., Llado, J., Shamblott, M., Maragakis, N., Irani, D.N.,Dike, S., Sappington, A., Gearhart, J., and Rothstein, J. (2001).Human embryonic germ cell derivatives facillitate motorrecovery of rats with diffuse motor neuron injury.2. Shamblott, M.J., Axelman, J., Wang, S., Bugg, E.M., Littlefield,J.W., Donovan, P.J., Blumenthal, P.D., Huggins, G.R., andGearhart, J.D. (1998). Derivation of pluripotent stem cellsfrom cultured human primordial germ cells. Proc. Natl. Acad.Sci. U. S. A. 95, 13726-13731.MULTIPLE APPROACHES FOR USINGSTEM CELLS IN PARKINSON’SDISEASE RESEARCHEfforts to develop stem cell based therapies forParkinson’s Disease provide a good example ofresearch aimed at rebuilding the central nervous system.As is the case with other disorders, both the cellimplantationand the trophic-factor strategies areunder active development. Both approaches arepromising. This is especially true of cell implantation,which involves using primary tissue transplanteddirectly form developing fetal brain tissue. Parkinson’sis a progressive movement disorder that usually strikes79
Rebuilding the Nervous System with <strong>Stem</strong> <strong>Cells</strong>after age 50. Symptoms often begin with an uncontrollablehand tremor, followed by increasing rigidity,difficulty walking, and trouble initiating voluntarymovement. The symptoms result from the death of aparticular set of neurons deep in the brain.The neurons that die in Parkinson’s Disease connect astructure in the brain called the substantia nigra toanother structure called the striatum, composedof the caudate nucleus and the putamen(see Figure 8.2. Neuronal Pathways that Degeneratein Parkinson’s Disease). These “nigro-striatal” neuronsrelease the chemical transmitter dopamine onto theirtarget neurons in the striatum. One of dopamine’smajor roles is to regulate the nerves that control bodymovement. As these cells die, there is less dopamineproduced, leading to the movement difficulties characteristicof Parkinson’s. At this point, no one knows forcertain why the neurons die.Lateral ventriclesStriatum}CaudatenucleusPutamenNigro-striatalneuronsSubstantianigra© 2001 Terese Winslow, Lydia KibiukFigure 8.2. Neuronal Pathways that Degenerate in Parkinson's Disease.Signals that control body movements travel along neurons that project from the substantia nigra to the caudate nucleus andputamen (collectively called the striatum). These “nigro-striatal” neurons release dopamine at their stargets in the striatum.In Parkinson's patients, dopamine neurons in the nigro-striatal pathway degenerate for unknown reasons.80
Rebuilding the Nervous System with <strong>Stem</strong> <strong>Cells</strong>Most patients suffering from Parkinson’s Disease aretreated with a drug called levodopa, which the brainconverts into dopamine. It initially helps most patients,but unfortunately, side effects of the drug increaseover time and its effectiveness wanes. This leavesParkinson’s patients and their doctors fighting a long,uphill battle to balance medication with side effectsto maintain function. In the end, many patients areutterly helpless.FETAL TISSUE TRANSPLANTS INPARKINSON’S DISEASE RESEARCHThe idea of growing dopamine cells in the laboratoryto treat Parkinson’s is the most recent step in the longhistory of cell or tissue transplantation to reverse thisdevastating disease. The concept was, and still is,straightforward: implant cells into the brain that canreplace the lost dopamine-releasing neurons.Although conceptually straightforward, this is not aneasy task. Fully developed and differentiateddopamine neurons do not survive transplantation, sodirect transplantation of fully developed brain tissuefrom cadavers, for example, is not an option.Moreover, full functional recovery depends on morethan cell survival and dopamine release; transplantedcells must also make appropriate connectionswith their normal target neurons in the striatum.One of the first attempts at using cell transplantationin humans was tried in the 1980s. This surgicalapproach involved the transplantation of dopamineproducingcells found in the adrenal glands, which sitatop the kidneys in the abdomen. Neurosurgeons inMexico reported that they had achieved dramaticimprovement in Parkinson’s patients by transplantingdopamine-producing chromaffin cells from severalpatients’ own adrenal glands to the nigro-striatal areaof their brains. Surgeons in the United States, however,observed only very modest and inconsistent improvementin their patients’ symptoms, and any gains disappearedwithin a year after surgery. Furthermore, itbecame clear that the risks associated with the procedure—whichrequired both brain and abdominalsurgery on patients who are often frail and elderly—outweigh the benefits [13].Another strategy, based on transplanting developingdopamine neurons from fetal brain tissue, hasfared better, however. Lars Olsen and his colleaguesshowed in the early 1970s that fetal tissuetransplanted directly from the developing nigro-striatalpathways of embryonic mice into the anterior chamberof an adult rat’s eye continues to mature into fullydeveloped dopamine neurons [3]. By the early 1980sAnders Bjorkland and others had shown that transplantationof fetal tissue into the damaged areas ofthe brains of rats and monkeys used as models of thedisease could reverse their Parkinson’s-like symptoms.Subsequently, researchers refined their surgical techniquesand showed that functional recovery dependson the implanted neurons growing and making functionalconnections at the appropriate brain locations—essentiallyfinishing their maturation by integratinginto the adult host brain [3].The promising animal results led to human trials inseveral centers worldwide, starting in the mid-1980s.Using tissue removed from a fetus electively abortedseven to nine weeks after conception, these earlyhuman transplantation studies showed encouraging,but inconsistent, benefit to patients. Although not allpatients improved, in the best cases patients receivingfetal tissue transplants showed a clear reductionin the severity of their symptoms. Also, researcherscould measure an increase in dopamine neuronfunction in the striatum of these patients by using abrain-imaging method called positron emissiontomography (PET) (see Figure 8.3. Positron EmissionTomography [PET] images from a Parkinson’s patientbefore and after fetal tissue transplantation). Also,autopsies done on the few patients who died fromcauses unrelated to either Parkinson’s or the surgeryrevealed a robust survival of the grafted neurons.Moreover, the grafted neurons sent outgrowths fromthe cell body that integrated well into the normaltarget areas in the striatum.A major weakness in these initial studies was that theywere all done “open label,” meaning that bothresearchers and patients knew which patientsreceived the transplanted tissue. When appropriate,the best test of a new therapy is a placebo controlled,double-blind trial, in which neither researchernor patient knows who has received the experimentaltreatment. In the mid-1990s, NIH approved fundingfor two rigorous clinical trials of fetal tissue transplantationfor Parkinson’s patients. Both studiesprovided for placebo control, in the form of shamsurgery conducted on half the study patients, andthey were done double blind—neither the81
Rebuilding the Nervous System with <strong>Stem</strong> <strong>Cells</strong>Dopamine-Neuron TransplantationBefore SurgeryAfter SurgeryFigure 8.3. Positron Emission Tomography (PET) images from a Parkinson’s patientbefore and after fetal tissue transplantation. The image taken before surgery (left)shows uptake of a radioactive form of dopamine (red) only in the caudate nucleus,indicating that dopamine neurons have degenerated. Twelve months after surgery, animage from the same patient (right) reveals increased dopamine function, especiallyin the putamen. (Reprinted with permission from N Eng J Med 2001;344 (10) p. 710.)researchers evaluating the effects of the surgery northe patients themselves knew who got tissue implants.The results of one of these trials, led by Curt Freed,were published recently [5]. Compared with control,patients who received the fetal-tissue transplantshowed no significant benefit in a subjective assessmentof the patient’s quality of life, which was thestudy’s primary endpoint. Moreover, two years aftersurgery, 5 out of 33 treated patients developed persistentdyskinesia—uncontrolled flailing movements—that had not been observed in the open-label workdescribed above.The Freed study results, nonetheless, provide importantinformation about the ability of dopamineneurons to survive in humans. Moreover, PET-scanningdata from the treated patients, as well as autopsiesof two patients who died of unrelated causes severalmonths after the surgery, showed that many of thedopamine neurons survived and grew. Researchersare now awaiting the results of the second NIHsponsoreddouble-blind trial, led by Warren Olanow[12]. The procedures used in this study differ substantiallyfrom those of Freed and his colleagues—including the tissue-handling method, the number ofcells implanted, the use of immunosuppressive drugsto limit rejection of the implanted tissue, and the testsused to assess patient response—and are closer tothose used in the most successful of the early openlabelexperiments.Most Parkinson’s researchers are still hopeful that thecell-implantation approach will one day lead to auseful and widely used therapy for Parkinson’sDisease. At the same time, however, mostresearchers are also convinced they must find adifferent source of cells for transplant. The logisticaland technical problems involved in recoveringenough developing dopamine neurons from fetaltissue are very great. Moreover, it is virtually impossibleto standardize the tissue collected from differentfetuses and to fully characterize the cells implanted.This absence of tissue standardization makes it verydifficult to determine the most important factors thatlead to a good patient response and may add risk(see Chapter 10. Assessing Human <strong>Stem</strong> Cell Safety).One alternative to cell implantation with human fetaltissue is to use fetal cells and tissues from animals.Researchers at Diacrin and Genzyme, twobiotechnology companies, recently announcedpreliminary results from a clinical trial in which 10Parkinson’s patients received neural cells from the82
Rebuilding the Nervous System with <strong>Stem</strong> <strong>Cells</strong>brains of fetal pigs. Eighteen months after the surgery,treated patients did not improve enough to show astatistically significant difference from eight controlpatients who received a sham immunosuppressionregimen and underwent sham surgery. Autopsy ofone treated patient who died of a pulmonaryembolism eight months after surgery revealed that asmall portion of the transplanted pig cells had survived[2], but PET studies looking for improvement indopamine uptake in all treated patients did not showclear improvement. The researchers are still analyzingtheir data [15].RAISING NEURONS FORREPLACEMENT IN PATIENTS WITHPARKINSON’S DISEASEWhat Parkinson’s researchers ultimately want is arenewable source of cells that can differentiate intofunctional dopamine neurons when placed in thestriatum. Laboratory-grown cells derived from a stemcell may be the best potential alternative source fortransplantable material. One way to get these is tofind the right combination of growth factors and cellcultureconditions to bring undifferentiated cells alongin a culture dish to a point where they are committedto becoming dopamine neurons, then implant themto finish growth and differentiation in the host brain.Another possibility is to put less-committed cells into adamaged brain and rely on “environmental” signalsin the brain to guide them into becoming the rightkind of replacement cell. These developmental signalsmay be expressed in the brain transiently followingneural degeneration or acute damage.Whether the cells ultimately implanted are halfdifferentiatedor completely immature, however,researchers need a reliable source. To that end, theyhave identified a whole host of different immaturecells that may have the potential to become,among other things, dopamine neurons, and theyare now in the process of sorting out how best tomake them do so. Neural stem cells isolated fromanimals and humans cannot be grown efficiently inthe lab without changing them in some way, such asby engineering them to express a gene normallyturned on only early in development. Embryonic stemcells—derived from the inner cell mass of an embryoat the blastocyst stage, when only a few hundredcells are present—can be kept in culture in a completelyundifferentiated state. They are still capable ofbecoming not just nervous system cells but every celltype in the body. If researchers want to be able toimplant cells derived from undifferentiated embryonicstem cells, they must take care that no cells in themix give rise to unwanted cell types, such as muscleor bone, within the nervous system. <strong>Stem</strong> cells fromother tissues—including umbilical cord blood andhuman bone marrow—can also be coaxed todisplay many of the surface-protein “markers” characteristicof nervous system cells. It is not yet clear,however, whether these cells are capable of givingrise to fully functional neurons.A great deal of basic research remains to be done tofind which of these cells provides the best way to geta workable therapy for Parkinson’s Disease. For example,although researchers have shown for certain thatboth primary human fetal cells and mouse embryonicstem cells can become fully functional dopamineneurons, they do not yet know if adult neural stemcells have the same potential. Also, no one has yetpublished evidence that cells from any renewablesource that are laboratory-directed to differentiateinto dopamine neurons can eliminate symptoms inanimal models of Parkinson’s when implanted.Researchers are making rapid progress, however. Forexample, Ron McKay and his colleagues at NIHreported in 1998 that they were able to expand apopulation of neurons from embryonic mouse brainin culture, and that these cells relieved Parkinson’s-likesymptoms in a rat model [16]. And last year, McKay’slab also described a procedure for efficiently convertingmouse pluripotent embryonic stem cells intoneurons that have all the characteristics of dopamineneurons, including the ability to form synapses [17].McKay and other researchers say they have encouragingunpublished results that dopamine precursorsderived from mouse embryonic stem cells can eliminatesymptoms in rat models of Parkinson’s Disease[7, 10].Privately funded researchers are following an analogouspath using pluripotent human embryonic stemcells. Thomas Okarma of Geron Corporation confirmsthat his company is testing the potential of humanembryonic stem cells in animal models of Parkinson’sDisease, but the results are not yet complete [11]. Inabstracts presented at a recent conference, Geronreports having succeeded in directing humanembryonic stem cells to become mature neural cells83
Rebuilding the Nervous System with <strong>Stem</strong> <strong>Cells</strong>in laboratory culture, including cells that have thestructural and chemical characteristics of dopamineneurons [6].TURNING ON THE BRAIN’S OWNSTEM CELLS AS A REPAIRMECHANISMParkinson’s researchers are also looking for ways tospark the repair mechanisms already in a patient’sbrain to fix damage that these mechanisms couldnot otherwise manage. This strategy is less developedthan cell implantation, but it also holds promise [1].In the future, researchers may use stem cells fromembryonic or adult sources not to replace lost cellsdirectly, but rather to turn on the body’s own repairmechanisms. Alternatively, researchers may findeffective drug treatments that help a patient’s ownstem cells and repair mechanisms work moreeffectively.<strong>Stem</strong> cells in the adult primate brain occur in twolocations. One, the subventricular zone, is an areaunder fluid-filled spaces called ventricles. The other isthe dentate gyrus of the hippocampus. In primates,very few new neurons normally appear in eitherplace, which is why the phenomenon escapednotice until recently. Researchers showed in the mid-1990s that when the brain is injured, stem cells inthese two areas proliferate and migrate toward thesite of the damage. The researchers are now trying todiscover how far this kind of response can go towardameliorating certain kinds of damage.Recent research shows the direction that this may beheading for Parkinson’s Disease. James Fallon andcolleagues studied the effects on rat brain of a proteincalled transforming growth factor alpha (TGF)—a natural peptide found in the body from the veryearliest stages of embryonic development onwardthat is important in activating normal repair processesin several organs, including liver and skin. Fallon'sstudies suggest that the brain’s normal repair processmay never be adequately triggered in a slowly developingdegenerative disease like Parkinson's and thatproviding more TGF can turn it on. Specifically,Fallon found that TGF injected into healthy rat braincauses stem cells in the subventricular zone to proliferatefor several days, after which they disappear. Butif the researchers make similar injections into rats inwhich they first damage the nigro-striatal neurons witha toxin called 6-hydroxydopamine—a frequently usedanimal model for Parkinson’s Disease—two thingshappen. After several days of cell proliferation, Fallonobserves what he calls a “wave of migration” of thestem cells to the damaged areas, where they differentiateinto dopamine neurons. Most importantly, thetreated rats do not show the behavioral abnormalitiesassociated with the loss of the neurons. Whether thebeneficial effect on symptoms is the result of thenewly formed cells or some other trophic effect is notyet entirely clear [4].STEM CELLS’ FUTURE ROLE INSPINAL CORD INJURY REPAIRParkinson’s Disease is only one of many nervoussystem disorders that researchers are trying to solveby regenerating damaged tissue. But Parkinson’s,difficult as it is to reverse, is a relatively easy targetbecause a regenerative therapy need only replaceone particular cell type in one part of the brain.Therapies for other disorders face much biggerhurdles. Complete restoration after severe spinal cordinjury, for example, is probably far in the future, if itcan ever be done at all. Many cell types aredestroyed in these injuries, including neurons thatcarry messages between the brain and the rest ofthe body. Getting these neurons to grow past aninjury site and connect appropriately with their targetsis extraordinarily difficult. But spinal cord injury patientswould benefit greatly from an even limited restorationof lost functions—gaining partial use of a limb insteadof none, or restoring bladder control, or being freedfrom pain. Such limited restoration of part of apatient’s lost functions is, for some less severe types ofinjury, perhaps a more achievable goal.In many spinal injuries, the spinal cord is not actuallycut and at least some of the signal-carrying neuronalaxons are intact. But the surviving axons no longercarry messages because cells called oligodendrocytes,which make the axons’ insulating myelinsheath, are lost. Researchers have recently made thefirst steps in learning to replace these lost myelin-producingcells [14]. For example, researchers haveshown that stem cells can aid remyelination inrodents [8, 9]. Specifically, they found that injection ofoligodendrocytes derived from mouse embryonicstem cells could remyelinate axons in chemicallydemyelinated rat spinal cord and that the treated84
Rebuilding the Nervous System with <strong>Stem</strong> <strong>Cells</strong>rats regained limited use of their hind limbs comparedwith the controls. They are not certain, however,whether the limited increase in function theyobserved in rats is actually due to the remyelinationor an unidentified trophic effect of the treatment.Spinal injury researchers emphasize that much morebasic and preclinical research must be done beforeattempting human trials using stem cell therapies torepair the damaged nervous system. Despite the factthat there is much basic work left to do and manyfundamental questions still to be answered,researchers are hopeful that effective repair for oncehopelessnervous system damage may eventually beachieved. Whether through developing replacementcells or activating the body’s own stem cells in vivo,research on the use of stem cells for nervous systemdisorders is a rapidly advancing field. This researchpromises to answer key questions about how to repairnervous system damage and how to restore keybody functions damaged by disease or disability.REFERENCES1. Bjorklund, A. and Lindvall, O. (2000). Self-repair in the brain.Nature. 405, 892-895.2. Deacon, T., Schumacher, J., Dinsmore, J., Thomas, C.,Palmer, P., Kott, S., Edge, A., Penney, D., Kassissieh, S.,Dempsey, P., and Isacson, O. (1997). Histological evidenceof fetal pig neural cell survival after transplantation into apatient with Parkinson's disease. Nat. Med. 3, 350-353.3. Dunnett, S.B., Bjorklund, A., and Lindvall, O. (2001). Cell therapyin Parkinson's disease—stop or go? Nat. Rev. Neurosci. 2,365-369.4. Fallon, J., Reid, S., Kinyamu, R., Opole, I., Opole, R., Baratta,J., Korc, M., Endo, T.L., Duong, A., Nguyen, G., Karkehabadhi,M., Twardzik, D., and Loughlin, S. (2000). In vivo induction ofmassive proliferation, directed migration, and differentiationof neural cells in the adult mammalian brain. Proc. Natl.Acad. Sci. U. S. A. 97, 14686-14691.6. Harley, C.B., Gearhart, J., Jaenisch, R., Rossant, J., andThomson, J. (2001). Pluripotent stem cells: biology andapplications. Durango, CO.7. Isacson, O., personal communication.8. Liu, S., Qu, Y., Stewart, T.J., Howard, M.J., Chakrabortty, S.,Holekamp, T.F., and McDonald, J.W. (2000). Embryonicstem cells differentiate into oligodendrocytes and myelinatein culture and after spinal cord transplantation. Proc.Natl. Acad. Sci. U. S. A. 97, 6126-6131.9. McDonald, J.W., Liu, X.Z., Qu, Y., Liu, S., Mickey, S.K., Turetsky,D., Gottlieb, D.I., and Choi, D.W. (1999). Transplantedembryonic stem cells survive, differentiate and promoterecovery in injured rat spinal cord. Nat. Med. 5, 1410-1412.10. McKay, R., personal communication.11. Okarma, T., personal communication.12. Olanow, C. W., personal communication.13. Quinn, N.P. (1990). The clinical application of cell graftingtechniques in patients with Parkinson's disease. Prog. BrainRes. 82, 619-625.14. Raisman, G. (2001). Olfactory ensheathing cells—anothermiracle cure for spinal cord injury? Nat. Rev. Neurosci. 2,369-374.15. Schumacher, J.M., Ellias, S.A., Palmer, E.P., Kott, H.S.,Dinsmore, J., Dempsey, P.K., Fischman, A.J., Thomas, C.,Feldman, R.G., Kassissieh, S., Raineri, R., Manhart, C.,Penney, D., Fink, J.S., and Isacson, O. (2000).Transplantation of embryonic porcine mesencephalictissue in patients with PD. Neurology. 54, 1042-1050.16. Studer, L., Csete, M., Lee, S.H., Kabbani, N., Walikonis, J.,Wold, B., and McKay, R. (2000). Enhanced proliferation,survival, and dopaminergic differentiation of CNS precursorsin lowered oxygen. J. Neurosci. 20, 7377-7383.17. Studer, L., Tabar, V., and McKay, R.D. (1998). Transplantationof expanded mesencephalic precursors leads to recoveryin parkinsonian rats. Nat. Neurosci. 1, 290-295.5. Freed, C.R., Greene, P.E., Breeze, R.E., Tsai, W.Y.,DuMouchel, W., Kao, R., Dillon, S., Winfield, H., Culver, S.,Trojanowski, J.Q., Eidelberg, D., and Fahn, S. (2001).Transplantation of embryonic dopamine neurons for severeParkinson's disease. N. Engl. J. Med. 344, 710-719.85
Rebuilding the Nervous System with <strong>Stem</strong> <strong>Cells</strong>This page intentionally left blank86
9.CAN STEM CELLS REPAIRA DAMAGED HEART?Heart attacks and congestive heart failure remainamong the Nation’s most prominent healthchallenges despite many breakthroughs in cardiovascularmedicine. In fact, despite successfulapproaches to prevent or limit cardiovasculardisease, the restoration of function to the damagedheart remains a formidable challenge. Recentresearch is providing early evidence that adult andembryonic stem cells may be able to replacedamaged heart muscle cells and establish newblood vessels to supply them. Discussed here aresome of the recent discoveries that feature stem cellreplacement and muscle regeneration strategies forrepairing the damaged heart.INTRODUCTIONFor those suffering from common, but deadly, heartdiseases, stem cell biology represents a new medicalfrontier. Researchers are working toward using stemcells to replace damaged heart cells and literallyrestore cardiac function.Today in the United States, congestive heart failure—the ineffective pumping of the heart caused by theloss or dysfunction of heart muscle cells—afflicts 4.8million people, with 400,000 new cases each year.One of the major contributors to the development ofthis condition is a heart attack, known medically as amyocardial infarction, which occurs in nearly 1.1 millionAmericans each year. It is easy to recognize thatimpairments of the heart and circulatory system representa major cause of death and disability in theUnited States [5].What leads to these devastating effects? The destructionof heart muscle cells, known as cardiomyocytes,can be the result of hypertension, chronic insufficiencyin the blood supply to the heart muscle caused bycoronary artery disease, or a heart attack, the suddenclosing of a blood vessel supplying oxygen tothe heart. Despite advances in surgical procedures,mechanical assistance devices, drug therapy, andorgan transplantation, more than half of patients withcongestive heart failure die within five years of initialdiagnosis. Research has shown that therapies such asclot-busting medications can reestablish blood flowto the damaged regions of the heart and limit thedeath of cardiomyocytes. Researchers are nowexploring ways to save additional lives by usingreplacement cells for dead or impaired cells sothat the weakened heart muscle can regain itspumping power.How might stem cells play a part in repairing theheart? To answer this question, researchers are buildingtheir knowledge base about how stem cells aredirected to become specialized cells. One importanttype of cell that can be developed is the cardiomyocyte,the heart muscle cell that contracts to ejectthe blood out of the heart’s main pumping chamber(the ventricle). Two other cell types are important to aproperly functioning heart are the vascular endothelialcell, which forms the inner lining of new blood vessels,and the smooth muscle cell, which forms thewall of blood vessels. The heart has a large demandfor blood flow, and these specialized cells are importantfor developing a new network of arteries to bringnutrients and oxygen to the cardiomyocytes after aheart has been damaged. The potential capability ofboth embryonic and adult stem cells to develop intothese cells types in the damaged heart is now beingexplored as part of a strategy to restore heart functionto people who have had heart attacks or havecongestive heart failure. It is important that work withstem cells is not confused with recent reports thathuman cardiac myocytes may undergo cell divisionafter myocardial infarction [1]. This work suggests thatinjured heart cells can shift from a quiescent stateinto active cell division. This is not different from the87
Can <strong>Stem</strong> <strong>Cells</strong> Repair a Damaged Heart?Coronary arteryligated inducingan infarctInfarct© 2001 Terese Winslow, Lydia KibiukFigure 9.1. Rodent Model of Myocardial Infarction.ability of a host of other cells in the body that beginto divide after injury. There is still no evidence thatthere are true stem cells in the heart which canproliferate and differentiate.Researchers now know that under highly specificgrowth conditions in laboratory culture dishes, stemcells can be coaxed into developing as new cardiomyocytesand vascular endothelial cells. Scientistsare interested in exploiting this ability to providereplacement tissue for the damaged heart. Thisapproach has immense advantages over hearttransplant, particularly in light of the paucity of donorhearts available to meet current transplantationneeds.What is the evidence that such an approach torestoring cardiac function might work? In the researchlaboratory, investigators often use a mouse or ratmodel of a heart attack to study new therapies(see Figure 9.1. Rodent Model of MyocardialInfarction). To create a heart attack in a mouse or rat,88
Can <strong>Stem</strong> <strong>Cells</strong> Repair a Damaged Heart?a ligature is placed around a major blood vesselserving the heart muscle, thereby depriving the cardiomyocytesof their oxygen and nutrient supplies.During the past year, researchers using such modelshave made several key discoveries that kindled interestin the application of adult stem cells to heartmuscle repair in animal models of heart disease.Recently, Orlic and colleagues [9] reported on anexperimental application of hematopoietic stem cellsfor the regeneration of the tissues in the heart. In thisstudy, a heart attack was induced in mice by tying offa major blood vessel, the left main coronary artery.Through the identification of unique cellular surfacemarkers, the investigators then isolated a select groupof adult primitive bone marrow cells with a highcapacity to develop into cells of multiple types. Wheninjected into the damaged wall of the ventricle, thesecells led to the formation of new cardiomyocytes,vascular endothelium, and smooth muscle cells, thusgenerating de novo myocardium, including coronaryarteries, arterioles, and capillaries. The newly formedmyocardium occupied 68 percent of the damagedportion of the ventricle nine days after the bone marrowcells were transplanted, in effect replacing thedead myocardium with living, functioning tissue. Theresearchers found that mice that received the transplantedcells survived in greater numbers than micewith heart attacks that did not receive the mousestem cells. Follow-up experiments are now beingconducted to extend the posttransplantation analysistime to determine the longer-range effects of suchtherapy [8]. The partial repair of the damaged heartmuscle suggests that the transplanted mousehematopoietic stem cells responded to signals in theenvironment near the injured myocardium. The cellsmigrated to the damaged region of the ventricle,where they multiplied and became “specialized”cells that appeared to be cardiomyocytes.A second study, by Jackson et al. [3], demonstratedthat cardiac tissue can be regenerated in the mouseheart attack model through the introduction of adultstem cells from mouse bone marrow. In this model,investigators purified a “side population” ofhematopoietic stem cells from a genetically alteredmouse strain. These cells were then transplanted intothe marrow of lethally irradiated mice approximately10 weeks before the recipient mice were subjectedto heart attack via the tying off of a different majorheart blood vessel, the left anterior descending (LAD)coronary artery. At two to four weeks after theinduced cardiac injury, the survival rate was 26 percent.As with the study by Orlic et al., analysis of theregion surrounding the damaged tissue in survivingmice showed the presence of donor-derived cardiomyocytesand endothelial cells. Thus, the mousehematopoietic stem cells transplanted into the bonemarrow had responded to signals in the injured heart,migrated to the border region of the damaged area,and differentiated into several types of tissue neededfor cardiac repair. This study suggests that mousehematopoietic stem cells may be delivered to theheart through bone marrow transplantation as well asthrough direct injection into the cardiac tissue, thusproviding another possible therapeutic strategy forregenerating injured cardiac tissue.More evidence for potential stem cell-based therapiesfor heart disease is provided by a study thatshowed that human adult stem cells taken from thebone marrow are capable of giving rise to vascularendothelial cells when transplanted into rats [6]. As inthe Jackson study, these researchers induced a heartattack by tying off the LAD coronary artery. They tookgreat care to identify a population of humanhematopoietic stem cells that give rise to new bloodvessels. These stem cells demonstrate plasticitymeaning that they become cell types that theywould not normally be. The cells were used to formnew blood vessels in the damaged area of the rats’hearts and to encourage proliferation of preexistingvasculature following the experimental heart attack.Like the mouse stem cells, these human hematopoieticstem cells can be induced under the appropriateculture conditions to differentiate into numeroustissue types, including cardiac muscle [10] (see Figure9.2. Heart Muscle Repair with Adult <strong>Stem</strong> <strong>Cells</strong>). Wheninjected into the bloodstream leading to the damagedrat heart, these cells prevented the death ofhypertrophied or thickened but otherwise viablemyocardial cells and reduced progressive formationof collagen fibers and scars. Control rats that underwentsurgery with an intact LAD coronary artery, aswell as LAD-ligated rats injected with saline or controlcells, did not demonstrate an increase in the numberof blood vessels. Furthermore, the hematopoieticcells could be identified on the basis of highly specificcell markers that differentiate them from cardiomyocyteprecursor cells, enabling the cells to be usedalone or in conjunction with myocyte-regenerationstrategies or pharmacological therapies. (For more89
Can <strong>Stem</strong> <strong>Cells</strong> Repair a Damaged Heart?Mouse adult stem cells areinjected into the muscle ofthe damaged left ventricularwall of the mouse heart.Human adult bone marrowstem cells are injected intothe tail vasculature of a rat.MouseheartAdult stem cellsThe stem cells induce new blood vesselformation in the damaged heart muscleand proliferation of existing vasculature.Adult stemcells<strong>Stem</strong> cells helpregeneratedamagedheart muscle.New bloodvessels© 2001 Terese Winslow, Lydia KibiukDamagedheart musclecellsFigure 9.2. Heart Muscle Repair with Adult <strong>Stem</strong> <strong>Cells</strong>.Damagedheart musclecellsabout stem cell markers see Appendix E.i. How DoResearchers Use Markers to Identify <strong>Stem</strong> <strong>Cells</strong>?)Exciting new advances in cardiomyocyte regenerationare being made in human embryonic stem cellresearch. Because of their ability to differentiate intoany cell type in the adult body, embryonic stem cellsare another possible source population for cardiacrepaircells. The first step in this application was takenby Itskovitz-Eldor et al. [2] who demonstrated thathuman embryonic stem cells can reproducibly differentiatein culture into embryoid bodies made up ofcell types from the body’s three embryonic germlayers. Among the various cell types noted were cellsthat had the physical appearance of cardiomyocytes,showed cellular markers consistent with heartcells, and demonstrated contractile activity similar tocardiomyocytes when observed under the microscope.In a continuation of this early work, Kehat et al. [4]displayed structural and functional properties of earlystage cardiomyocytes in the cells that develop fromthe embryoid bodies. The cells that have spontaneouslycontracting activity are positively identified byusing markers with antibodies to myosin heavy chain,alpha-actinin, desmin, antinaturietic protein, and cardiactroponin—all proteins found in heart tissue. Theseinvestigators have done genetic analysis of thesecells and found that the transcription-factor genesexpressed are consistent with early stage cardiomyocytes.Electrical recordings from these cells,changes in calcium-ion movement within the cells,and contractile responsiveness to catecholaminehormone stimulation by the cells were similar to therecordings, changes, and responsiveness seen inearly cardiomyocytes observed during mammalian90
Can <strong>Stem</strong> <strong>Cells</strong> Repair a Damaged Heart?development. A next step in this research is to seewhether the experimental evidence of improvementin outcome from heart attack in rodents can bereproduced using embryonic stem cells.These breakthrough discoveries in rodent modelspresent new opportunities for using stem cells torepair damaged heart muscle. The results of thestudies discussed above are growing evidence thatadult stem cells may develop into more cell typesthan first thought. In those studies, hematopoieticstem cells appear to be able to develop not only intoblood, but also into cardiac muscle and endothelialtissue. This capacity of adult stem cells, increasinglyreferred to as “plasticity,” may make such adult stemcells a viable candidate for heart repair. But thisevidence is not complete; the mouse hematopoieticstem cell populations that give rise to these replacementcells are not homogenous. Rather, they areenriched for the cells of interest through specific andselective stimulating factors that promote cell growth.Thus, the originating cell population for these injectedcells has not been identified, and the possibility existsfor inclusion of other cell populations that couldcause the recipient to reject the transplanted cells.This is a major issue to contend with in clinical applications,but it is not as relevant in the experimentalmodels described here because the rodents havebeen bred to be genetically similar.What are the implications for extending the researchon differentiated growth of replacement tissues fordamaged hearts? There are some practical aspectsof producing a sufficient number of cells for clinicalapplication. The repair of one damaged humanheart would likely require millions of cells. The uniquecapacity for embryonic stem cells to replicate inculture may give them an advantage over adultstem cells by providing large numbers of replacementcells in tissue culture for transplantation purposes.Given the current state of the science, it is unclearhow adult stem cells could be used to generatesufficient heart muscle outside the body to meetpatients’ demand [7].Although there is much excitement becauseresearchers now know that adult and embryonicstem cells can repair damaged heart tissue, manyquestions remain to be answered before clinicalapplications can be made. For example, how longwill the replacement cells continue to function? Dothe rodent research models accurately reflect humanheart conditions and transplantation responses? Dothese new replacement cardiomyocytes derivedfrom stem cells have the electrical-signal-conductingcapabilities of native cardiac muscle cells?<strong>Stem</strong> cells may well serve as the foundation uponwhich a future form of “cellular therapy” is constructed.In the current animal models, the time betweenthe injury to the heart and the application of stemcells affects the degree to which regeneration takesplace, and this has real implications for the patientwho is rushed unprepared to the emergency room inthe wake of a heart attack. In the future, could thepatient’s cells be harvested and expanded for use inan efficient manner? Alternatively, can at-risk patientsdonate their cells in advance, thus minimizing thepreparation necessary for the cells’ administration?Moreover, can these stem cells be genetically“programmed” to migrate directly to the site of injuryand to synthesize immediately the heart proteinsnecessary for the regeneration process? Investigatorsare currently using stem cells from all sources toaddress these questions, thus providing a promisingfuture for therapies for repairing or replacing thedamaged heart and addressing the Nation’s leadingcauses of death.REFERENCES1. Beltrami, A.P., Urbanek, K., Kajstura, J., Yan, S.M., Finato, N.,Bussani, R., Nadal-Ginard, B., Silvestri, F., Leri, A., Beltrami,C.A., and Anversa, P. (2001). Evidence that human cardiacmyocytes divide after myocardial infarction. N. Engl. J.Med. 344, 1750-1757.2. Itskovitz-Eldor, J., Schuldiner, M., Karsenti, D., Eden, A.,Yanuka, O., Amit, M., Soreq, H., and Benvenisty, N. (2000).Differentiation of human embryonic stem cells intoembryoid bodies comprising the three embryonic germlayers. Mol. Med. 6, 88-95.3. Jackson, K.A., Majka, S.M., Wang, H., Pocius, J., Hartley,C.J., Majesky, M.W., Entman, M.L., Michael, L.H., Hirschi,K.K., and Goodell, M.A. (2001). Regeneration of ischemiccardiac muscle and vascular endothelium by adult stemcells. J. Clin. Invest. 107, 1-8.4. Kehat, I., Kenyagin-Karsenti, D., Druckmann, M., Segev, H.,Amit, M., Gepstein, A., Livne, E., Binah, O., Itskovitz-Eldor, J.,and Gepstein, L. (2001). Human embryonic stem cells candifferentiate into myocytes portraying cardiomyocyticstructural and functional properties. J. Clin. Invest. (in press)5. Kessler, P.D. and Byrne, B.J. (1999). Myoblast cell graftinginto heart muscle: cellular biology and potential applications.Annu. Rev. Physiol. 61, 219-242.91
Can <strong>Stem</strong> <strong>Cells</strong> Repair a Damaged Heart?6. Kocher, A.A., Schuster, M.D., Szabolcs, M.J., Takuma, S.,Burkhoff, D., Wang, J., Homma, S., Edwards, N.M., andItescu, S. (2001). Neovascularization of ischemic myocardiumby human bone-marrow-derived angioblasts preventscardiomyocyte apoptosis, reduces remodeling andimproves cardiac function. Nat. Med. 7, 430-436.7. Lanza, R., personal communication.8. Orlic, D., personal communication.9. Orlic, D., Kajstura, J., Chimenti, S., Jakoniuk, I., Anderson,S.M., Li, B., Pickel, J., McKay, R., Nadal-Ginard, B., Bodine,D.M., Leri, A., and Anversa, P. (2001). Bone marrow cellsregenerate infarcted myocardium. Nature. 410, 701-705.10. Pittenger, M.F., Mackay, A.M., Beck, S.C., Jaiswal, R.K.,Douglas, R., Mosca, J.D., Moorman, M.A., Simonetti, D.W.,Craig, S., and Marshak, D.R. (1999). Multilineage potentialof adult human mesenchymal stem cells. Science. 284,143-147.92
10.ASSESSING HUMANSTEM CELL SAFETYThe isolation of human stem cells offers the promiseof a remarkable array of novel therapeutics. Biologictherapies derived from such cells—through tissueregeneration and repair as well as through thetargeted delivery of genetic material—are expectedto be effective in the treatment of a wide range ofmedical conditions. Efforts to analyze and assess thesafety of using human stem cells in the clinical settingare vitally important to this endeavor.Transplanted human stem cells are dynamic biologicalentities that interact intimately with—and areinfluenced by—the physiology of the recipient. Beforethey are transplanted, cultured human stem cells aremaintained under conditions that promote either theself-renewing expansion of undifferentiated progenitorsor the acquisition of differentiated propertiesindicative of the phenotype the cells will assume.After incompletely differentiated human stem cellsare transplanted, additional fine-tuning occurs as aconsequence of instructions received from the cells’physiologic microenvironments within the recipient.The capabilities to self-renew and differentiate thatare inherent to human stem cells point simultaneouslyto their perceived therapeutic potential and to thechallenge of assessing their safety.Assessing human stem cell safety requires the implementationof a comprehensive strategy. Each step inthe human stem cell development process—beginningwith identifying and evaluating suitable humanstem cell sources—must be carefully scrutinized.Included in this global assessment are the derivation,expansion, manipulation, and characterization ofhuman stem cell lines, as well as preclinical efficacyand toxicity testing in appropriate animal models.Being able to trace back from the cell populationprepared for transplantation to the source of thefounder human stem cells also allows each safetycheckpoint to be connected, one to the other.WEAVING A STEM CELL SAFETY NETA diversity of opinion exists among researchers aboutthe feasibility of initiating pilot clinical studies usinghuman stem cells. Some are of the view that it isreasonable to expect within the next five years thathuman stem cells will be used in transplantationsettings to replace dead or dying cells within organssuch as the failing heart or that genetically modifiedhuman stem cells will be created for delivery oftherapeutic genes. Others argue that a good dealmore information about the basic biology of humanstem cells needs to be accumulated before theirtherapeutic potential in humans can be assessed.Clinical studies involving the transplantation of bloodrestoring,or hematopoietic, stem cells have beenunder way for a number of years. Reconstituting theblood and immune systems through stem cell transplantationis an established practice for treatinghematological malignancies such as leukemia andlymphoma. Transplanting hematopoietic stem cellsresident in the bone marrow or isolated from cordblood or circulating peripheral blood is used tocounter the destruction of certain bone marrow cellscaused by high-intensity chemotherapeutic regimensused to battle various solid tumors. Moreover, clinicaltrials are being conducted to assess the safety andefficacy of using hematopoietic stem cell transplantationto treat various autoimmune conditions includingmultiple sclerosis, lupus, and rheumatoid arthritis.Although precedents exist for the clinical use ofhuman stem cells, there is considerable reluctanceto proceed with clinical trials involving human stemcells derived from embryonic and fetal sources. Thishesitancy extends to adult human stem cells of nonhematopoieticorigin, even though, by contrast, theirplasticity is generally considered to be lower than thatof their embryo- and fetus-derived counterparts. For93
Assessing Human <strong>Stem</strong> Cell Safetyhuman stem cells to advance to the stage of clinicalinvestigation, a virtual safety net composed of acore set of safeguards is required (see Table 10.1.Safeguards for clinical applications of human stemcells, by source of cell).Safety Assurance Begins with AdequateDonor ScreeningWhether human stem cells are of embryonic, fetal,or adult origin, donor sources must be carefullyscreened. Routine testing should be done to guardagainst the inadvertent transmission of infectiousdiseases. Additionally, pedigree assessment andmolecular genetic testing appear to be warranted.This is arguably the case when human stem cellsintended for transplantation are derived from anallogeneic donor—that is, someone other that therecipient—and especially if the cells are obtainedfrom a master cell bank that has been establishedusing human embryonic stem or human embryonicgerm cells.The purpose of pedigree evaluation and/or genetictesting is to establish whether the human stem cellsin question are suitable for use in the context of aparticular clinical situation. For example, embryosderived from a donor with a family history of cardiovasculardiseases may not be the best suited for thederivation of cardiac muscle cells intended to repairdamaged heart tissue. Similarly, the use of molecularTable 10.1. Safeguards for clinical applications of human stem cells, by source of cell*SafeguardEmbryoFetusAdult:Autologous(self)Adult:Allogeneic(nonself)Screen donors• Infectious-agent testing• Pedigree assessment• Molecular genetic testing+++++++Use controlled, standardized practices andprocedures for establishing stem cell lines++++++++Develop alternatives to culturing on cell-feederlayer++++NANAPerform detailed characterization oftem cell lines• Morphology• Cell-surface antigens• Biochemical markers• Gene expression• Karyotype analysis• Biologic activity++++++++Conduct preclinical animal testing• Proof of concept: disease models– Cell integration– Cell migration• Comprehensive toxicity• Proliferative potential++++++++++++++++++++++Monitor patient and do long-term follow-up ++++++++++= more important; +=less important; NA=not applicable.94
Assessing Human <strong>Stem</strong> Cell Safetygenetic analysis could detect a mutation in the genefor alpha-synuclein. This gene is known to be responsiblefor the rare occurrence of early onset Parkinson’sDisease. Detecting such a genetic abnormality inneuronal progenitor cells derived from an establishedembryonic germ cell line could block the use ofthose cells as a treatment for a number of neurodegenerativeconditions, including Parkinson’s Disease.The number of genes known to be directly responsiblefor causing disease or anomalous physiologicfunction is relatively small. Advances in techniques foridentifying, isolating, and analyzing genes, coupledwith the wealth of information destined to becomeavailable as one outcome of the human genomesequencing projects, will raise this number.Considerably more will also be learned about howmultiple gene products, each contributing an incrementalquantity to the overall sum, predispose anindividual to develop particular diseases. Clearly, itwill eventually not be possible, or even necessary, toscreen every source of human stem cells for theentire panoply of disease-associated genes. Thescreening of targeted genes will be conducted withinthe context of the relevant clinical population.Using Controlled, Standardized Practices andProcedures for Establishing Cultured Human <strong>Stem</strong>Cell Lines Enhances SafetyTo ensure the integrity, uniformity, and reliability ofhuman stem cell preparations intended for clinicaluse, it is essential to demonstrate that rigorouslycontrolled, standardized practices and proceduresare being followed in establishing and maintaininghuman stem cell lines in culture.Human stem cells from virtually every source otherthan blood-derived hematopoietic stem cells aremaintained in tissue culture for some defined periodof time. This is necessary to obtain a sufficient numberof cells for use in clinical studies involving transplantation.Culturing human stem cells requires theuse of formulated liquid media supplemented withgrowth factors and other chemical substances thatpromote cellular replication and govern the differentiationof the cultured human stem cells. Since humanstem cells are a dynamic, biological entity, failure tostandardize procedures for maintaining and expandingcells in culture could result in unintended alterationsin the intrinsic properties of the cells. The initialseeding density of the cells, the frequency with whichthe culture medium is replenished, and the densitycells are permitted to achieve before subdividing willall affect the characteristics of human stem cellsmaintained in culture. Altering the concentrations ofsupplemental growth factors and chemical substances,even switching from one supplier to another,may lead to changes in cell growth rate, expressionof defining cell markers, and differentiation potential.Alterations in stem cell properties caused by the useof nonstandardized culture practices are likely toaffect the behavior and effectiveness of the cellsonce transplanted.One particular concern is how safe it is to use serumderived from cows as a supplement to culturemedia. Due to the outbreak of bovine spongiformencephalopathy (BSE) in cattle herds, primarily thoseraised in the United Kingdom, only serum producedfrom cows reared in countries certified to be free ofBSE should be used. Consumption of beef contaminatedwith the agent responsible for causing BSE haslead to the limited emergence of new variantCreutzfeldt-Jakob disease (nvCJD) in humans. This diseaseresults in the relentless destruction of brain tissueand is invariably fatal. Placing neural stem cells contaminatedwith the BSE infectious agent in a patient’snervous system to investigate cellular-replacementtherapies for neurological disorders would be bothirresponsible and devastating. Researchers areengaged in a vigorous effort to develop serum-free,chemically defined media that obviate risks associatedwith the use of bovine serum.Alternatives to Culturing on a Feeder Layer ofAnimal <strong>Cells</strong> Improve SafetyAn issue unique to the culturing of human embryonicstem and embryonic germ cells involves the use ofmouse embryonic fibroblast feeder cells to keep theembryonic cells in a proliferating, undifferentiatedcondition. Human embryonic stem and embryonicgerm cells are seeded directly onto a bed of irradiatedmouse feeder cells. Transplanting into humans stemcell preparations derived from founder cells that havebeen in direct, intimate contact with nonhumananimal cells constitutes xenotransplantation—the useof organs, tissues, and cells derived from animals totreat human disease. The principal concern of xenotransplantationis the unintended transfer of animalviruses into humans.Researchers are devoting considerable attention todeveloping culture conditions that do not use mousefeeder cells. In February of this year, scientists from95
Assessing Human <strong>Stem</strong> Cell SafetyGeron Corporation, a biotech company focusing onthe development of embryonic stem cell technologyfor treating disease, presented findings at a scientificconference demonstrating that human embryonicstem cells can be maintained without mouse feedercells. Human embryonic stem cells seeded on acommercially available basement membrane matrixin media conditioned by feeder cells retain theirproliferative potential and capacity to form all threeembryonic germ layers (mesoderm, endoderm, andectoderm). This suggests that human embryonicstem cells maintained in the absence of directculture on a mouse feeder cell layer are comparableto human embryonic stem cells co-cultured withmouse feeder cells.Detailed Characterization of Human <strong>Stem</strong> CellPopulations Reinforces the Safety NetDetailed characterization of cell preparations intendedfor transplantation is critical to the development ofhuman stem cells for clinical use. Identifying the cellsthat make up an human stem cell population intendedfor clinical study requires identifying cells exhibitingthe desired phenotype within the preparation, as wellas those that do not. This poses considerable challengesbecause human embryonic stem and embryonicgerm cells have the capacity to give rise to alldifferentiated cell types, while adult human stemcells, though generally more restricted in their plasticity,are capable of generating all cell types thatmake up the tissue from which they were derived.On the basis of the complex biological properties ofhuman stem cells, including their potential to differentiatealong multiple lineages and give rise to a varietyof cell types, it is expected that the characterizationof stem cell preparations will require a panel oforthogonal assessments. Parameters that will proveuseful in establishing identity include 1) cell morphology(visual microscopic inspection of cells to assess theirappearance), 2) expression of unique cell-surfaceantigens (as is the case for CD34 + hematopoieticstem cells), 3) characterization of biochemicalmarkers such as a tissue-specific enzymatic activity(e.g., enzymes that produce neurotransmitters fornerve cells), and 4) expression of genes that areunique to a particular cell type. Further, analysis of thenuclear chromosomal karyotype may be used toassess genetic stability of established human embryonicstem and embryonic germ cell lines maintainedin culture for extended periods of time. Continueddevelopment and standardization of DNA microarrayanalysis (simultaneous screening for many genes)and proteomics (protein profiling) technologies willsignificantly enhance stem cell characterization.Rigorous and quantitative identification of cell typeswithin a heterogeneous population of differentiatinghuman stem cells provides the means to gaugepurity of a cellular preparation. In turn, this permitsevaluation of the extent to which purity of a humanstem cell preparation predicts efficacy after transplantation.It is not necessarily the case that homogenouspopulations composed of a single cell typewill be more effective as a cell-replacement therapythan mixed populations of cells. It is conceivable thatthe reason differentiation of cultured stem cellsobtained from the brain leads to formation of all thecell types found within the nervous system (namely,neurons, astrocytes, and oligodendrocytes) is thattheir coincidental presence is required to ensuremaximum survival and functional capability. Theinteraction of various phenotypic cell types within apreparation of progenitor cells obtained after thecontrolled differentiation of cultured human embryonicstem cells is being actively investigated.Once the purity profile has been established for apopulation of human stem cells generated usingstandardized procedures, deviations that occur outsidewhat is expected due to normal biologic variationserve as a harbinger that significant, and possiblydeleterious, changes may have occurred. Such alterationscould reflect the introduction of genetic mutationsas a consequence of culture conditions used topromote expansion and to induce differentiation ofthe progenitor cell population.Before clinical studies involving human stem celltransplantation can be done, it is essential to demonstratethat human stem cell preparations possessrelevant biological activity. The bioassay provides aquantitative measure of the potency of a cell preparationand ensures that cells destined for transplantationare not inert. Assays may be based on abiologic activity such as insulin release from pancreaticislet-like cells, glycogen storage by cellsintended for regeneration of liver tissue, or synchronouscontraction in the case of stem cell-derivedcardiomyocytes to be used for repairing damagedheart muscle. When cells that have not acquired fully96
Assessing Human <strong>Stem</strong> Cell Safetydifferentiated functionality are to be transplanted, itmay be appropriate to use surrogate markers thatpredict the acquisition of the intended biologicactivity upon further differentiation. (For example,counting tyrosine hydroxylase-expressing neuralprogenitor cells in a mixed population of cells intendedto provide dopaminergic neurons for treatingParkinson’s Disease could predict the acquisition ofrelevant biologic activity after transplantation.)Proof of Concept, Toxicity Testing, and Evaluationof Proliferative Potential in Animal Models AreImportant to the Assessment of Human <strong>Stem</strong>Cell SafetyA critical element of the safety net is the transplantationof human stem cells into animals to demonstratethat the therapy does what it is supposed to do(“proof of concept”) and to assess toxicity. Admittedly,animal models of human disease are imperfectbecause most human maladies do not spontaneouslyoccur in animals. Chemical, surgical, andimmunologic methods are used to damage neurons;induce diabetes; simulate heart attacks, stroke, andhypertension; or compromise organ function. In situationswhen focal genetic lesions are known to causedisease, the creation of transgenic mouse colonies inwhich the culpable gene is either eliminated or overexpressedresults in disease models that are capableof faithfully reproducing human-disease-specificpathologies.Human stem cells must be transplanted into animalmodels of human disease. Transplantation of neuralstem cells should demonstrate measurable evidenceof efficacy in models of neurodegenerative disease,such as Parkinson’s Disease, Huntington’s disease,and amyotrophic lateral sclerosis (ALS), Alzheimer’sdisease, as well as spinal cord injury and stroke.Improved liver function after transplantation ofhepatocyte precursors should be observed in ananimal model of hepatic failure. Normalization ofblood insulin concentrations and amelioration ofdiabetic disease symptoms should result from thetransplantation of pancreatic islet progenitors in amouse model of diabetes. It is likely that in all cases,immunosuppression will be required due to immunologicincompatibility between humans and theanimal model species (usually mouse or rat).In addition to efficacy, evidence for anatomic andfunctional integration of transplanted human stemcells should be assessed. human stem cells destinedfor transplantation may be tagged with a marker,such as green fluorescent protein, that allows transplantedcells to be readily identified upon histologicalexamination. A similar approach should be used toevaluate the migration of transplanted human stemcells from the site of injection into adjacent and moredistant tissues. The migration of transplanted humanstem cells to a nontarget site and subsequent differentiationinto a tissue type that is inappropriate forthat anatomic location could be problematic.Questions about the use of embryonic comparedwith adult stem cells with respect to robustness anddurability should be addressed in animal-transplantationmodels. Similarly, the issue of whether less-differentiatedcells will be more effective than more-differentiatedcells following transplantation should beinvestigated. Continued advancements in noninvasiveimaging technologies, such as magnetic resonanceimaging (MRI) and positron emission tomography(PET scanning), will allow these events to beobserved in real time with reasonable resolution andwithout having to use large numbers of animals.From the perspective of toxicology, the proliferativepotential of undifferentiated human embryonic andembryonic germ cells evokes the greatest level ofconcern. A characteristic of human embryonic stemcells is their capacity to generate teratomas whentransplanted into immunologically incompetentstrains of mice. Undifferentiated embryonic stem cellsare not considered as suitable for transplantation dueto the risk of unregulated growth. The question thatremains is, at what point during differentiation doesthis risk become insignificant, if ever? Identifying thestage at which the risk for tumor formation is minimizedwill depend on whether the process of stemcell differentiation occurs only in a forward directionor is reversible. Before clinical trials are begun inhumans, the issue of unregulated growth potentialand its relationship to stem cell differentiation mustbe evaluated. It is essential that careful toxicologystudies are performed that are of the appropriateduration and that involve transplantation intoimmunocompromised animals of undifferentiated orpartially differentiated embryonic stem cells, as wellas adult stem cells.97
Assessing Human <strong>Stem</strong> Cell SafetyThis page intentionally left blank98
11 .USE OF GENETICALLY MODIFIEDSTEM CELLS IN EXPERIMENTALGENE THERAPIESTo date, only nonembryonic human stem cells havebeen used in cell-based gene therapy studies. Theinherent limitations of these stem cells, as discussedbelow, have prompted scientists to ponder andexplore whether human embryonic stem cells mightovercome the current barriers to the clinical successof cell-based gene therapies.PRINCIPLES AND PROMISE OF GENETHERAPYGene therapy is a relatively recent, and still highlyexperimental, approach to treating human disease.While traditional drug therapies involve the administrationof chemicals that have been manufacturedoutside the body, gene therapy takes a very differentapproach: directing a patient’s own cells to produceand deliver a therapeutic agent. The instructions forthis are contained in the therapeutic transgene (thenew genetic material introduced into the patient).Gene therapy uses genetic engineering—the introductionor elimination of specific genes by usingmolecular biology techniques to physically manipulategenetic material—to alter or supplement thefunction of an abnormal gene by providing a copyof a normal gene, to directly repair such a gene, orto provide a gene that adds new functions orregulates the activity of other genes.Clinical efforts to apply genetic engineering technologyto the treatment of human diseases date to1989. Initially, gene therapy clinical trials focused oncancer, infectious diseases, or disorders in which onlya single gene is abnormal, such as cystic fibrosis.Increasingly however, efforts are being directedtoward complex, chronic diseases that involve morethan one gene. Prominent examples include heartdisease, inadequate blood flow to the limbs, arthritis,and Alzheimer’s disease.The potential success of gene therapy technologydepends not only on the delivery of the therapeutictransgene into the appropriate human target cells,but also on the ability of the gene to functionproperly in the cell. Both requirements poseconsiderable technical challenges.Gene therapy researchers have employed two majorstrategies for delivering therapeutic transgenes intohuman recipients (see Figure 11.1. Strategies forDelivering Therapeutic Transgenes into Patients). Thefirst is to “directly” infuse the gene into a person.Viruses that have been altered to prevent them fromcausing disease are often used as the vehicle fordelivering the gene into certain human cell types, inmuch the same way as ordinary viruses infect cells.This delivery method is fairly imprecise and limited tothe specific types of human cells that the viral vehiclecan infect. For example, some viruses commonlyused as gene-delivery vehicles can only infect cellsthat are actively dividing. This limits their usefulness intreating diseases of the heart or brain, because theseorgans are largely composed of nondividing cells.Nonviral vehicles for directly delivering genes intocells are also being explored, including the use ofplain DNA and DNA wrapped in a coat of fattymolecules known as liposomes.The second strategy involves the use of living cells todeliver therapeutic transgenes into the body. In thismethod, the delivery cells—often a type of stem cell,a lymphocyte, or a fibroblast—are removed from thebody, and the therapeutic transgene is introducedinto them via the same vehicles used in the previouslydescribed direct-gene-transfer method. Whilestill in the laboratory, the genetically modified cellsare tested and then allowed to grow and multiplyand, finally, are infused back into the patient.99
Use of Genetically Modified <strong>Stem</strong> <strong>Cells</strong> in Experimental Gene TherapiesDIRECT DELIVERYCELL-BASED DELIVERYTherapeutictransgeneThe therapeutictransgene ispackaged into adelivery vehiclesuch as a virus.The therapeutictransgene ispackaged into adelivery vehiclesuch as a virus.Therapeutictransgene…and injectedinto the patient.Target organ(e.g., liver)…and readministeredto the patient.The therapeutictransgene isintroduced into adelivery cell such asa stem cell that isoften derived fromthe patient.The genetically modifiedcells (e.g., stem cells)are multiplied in thelaboratory.© 2001 Terese WinslowFigure 11.1. Strategies for Delivering Therapeutic Transgenes into Patients.Gene therapy using genetically modified cells offersseveral unique advantages over direct gene transferinto the body and over cell therapy, which involvesadministration of cells that have not been geneticallymodified. First, the addition of the therapeutic transgeneto the delivery cells takes place outside thepatient, which allows researchers an important measureof control because they can select and work onlywith those cells that both contain the transgene andproduce the therapeutic agent in sufficient quantity.Second, investigators can genetically engineer, or“program,” the cells’ level and rate of production ofthe therapeutic agent. <strong>Cells</strong> can be programmed tosteadily churn out a given amount of the therapeuticproduct. In some cases, it is desirable to program thecells to make large amounts of the therapeuticagent so that the chances that sufficient quantitiesare secreted and reach the diseased tissue in thepatient are high. In other cases, it may be desirableto program the cells to produce the therapeuticagent in a regulated fashion. In this case, the therapeutictransgene would be active only in response tocertain signals, such as drugs administered to thepatient to turn the therapeutic transgene on and off.WHY STEM CELLS ARE USED INSOME CELL-BASED GENE THERAPIESTo date, about 40 percent of the more than 450gene therapy clinical trials conducted in the UnitedStates have been cell-based. Of these, approximately30 percent have used human stem cells—specifically, blood-forming, or hematopoietic, stemcells—as the means for delivering transgenes intopatients.Several of the early gene therapy studies usingthese stem cells were carried out not for therapeuticpurposes per se, but to track the cells’ fate after theywere infused back into the patient. The studies aimed100
Use of Genetically Modified <strong>Stem</strong> <strong>Cells</strong> in Experimental Gene Therapiesto determine where the stem cells ended up andwhether they were indeed producing the desiredgene product, and if so, in what quantities and forwhat length of time. Of the stem cell-based genetherapy trials that have had a therapeutic goal,approximately one-third have focused on cancers(e.g., ovarian, brain, breast, myeloma, leukemia, andlymphoma), one-third on human immunodeficiencyvirus disease (HIV-1), and one-third on so-calledsingle-gene diseases (e.g., Gaucher’s disease, severecombined immune deficiency (SCID), Fanconianemia, Fabry disease, and leukocyte adherencedeficiency).But why use stem cells for this method of gene therapy,and why hematopoietic stem cells in particular?The major reason for using stem cells in cell-basedgene therapies is that they are a self-renewingpopulation of cells and thus may reduce oreliminate the need for repeated administrations ofthe gene therapy.Since the advent of gene therapy research,hematopoietic stem cells have been a delivery cellof choice for several reasons. First, although small innumber, they are readily removed from the body viathe circulating blood or bone marrow of adults or theumbilical cord blood of newborn infants. In addition,they are easily identified and manipulated in thelaboratory and can be returned to patients relativelyeasily by injection.The ability of hematopoietic stem cells to give rise tomany different types of blood cells means that oncethe engineered stem cells differentiate, the therapeutictransgene will reside in cells such as T and Blymphocytes, natural killer cells, monocytes,macrophages, granulocytes, eosinophils, basophils,and megakaryocytes. The clinical applications ofhematopoietic stem cell-based gene therapies arethus also diverse, extending to organ transplantation,blood and bone marrow disorders, and immunesystem disorders.In addition, hematopoietic stem cells “home,” ormigrate, to a number of different spots in the body—primarily the bone marrow, but also the liver, spleen,and lymph nodes. These may be strategic locationsfor localized delivery of therapeutic agents for disordersunrelated to the blood system, such as liverdiseases and metabolic disorders such asGaucher’s disease.The only type of human stem cell used in genetherapy trials so far is the hematopoietic stem cell.However, several other types of stem cells are beingstudied as gene-delivery-vehicle candidates. Theyinclude muscle-forming stem cells known asmyoblasts, bone-forming stem cells calledosteoblasts, and neural stem cells.Myoblasts appear to be good candidates for use ingene therapy because of an unusual and advantageousbiological property: when injected into muscle,they fuse with nearby muscle fibers and become anintegral part of the muscle tissue. Moreover, sincemuscle tissue is generally well supplied with nervesand blood, the therapeutic agents produced by thetransgene are also accessible to nerves and thecirculatory system. Thus, myoblasts may not only beuseful for treating muscle disorders such as musculardystrophy, but also possibly nonmuscle disorders suchas neurodegenerative diseases, inherited hormonedeficiencies, hemophilia, and cancers.Several promising animal studies of myoblastmediatedgene therapy have been reported [17]. Forinstance, this approach was successful in correctingliver and spleen abnormalities associated with alysosomal storage disease in mice. Investigators havealso achieved stable production of the human clottingfactor IX deficient in hemophilia at therapeuticconcentrations in mice for at least eight months.Myoblasts engineered to secrete erythropoietin (ahormone that stimulates red blood cell production)were successful in reversing a type of anemiaassociated with end-stage renal disease in a mousemodel of renal failure.Another animal study of myoblast-mediated genetransfer involved a mouse model of familial amyotrophiclateral sclerosis (ALS, also known as LouGehrig’s disease), a fatal disorder characterized byprogressive degeneration of the brain and spinalcord nerves that control muscle activity. Investigatorsinjected myoblasts containing the transgene for ahuman nerve growth factor into the muscles of theALS mice before the onset of disease symptoms andmotor neuron degeneration. The transgene remainedactive in the muscle for up to 12 weeks, and, mostimportantly, the gene therapy successfully delayedthe onset of disease symptoms, slowed muscle atrophy,and delayed the deterioration of motor skills [16].101
Use of Genetically Modified <strong>Stem</strong> <strong>Cells</strong> in Experimental Gene TherapiesIn a series of experiments in rodents, a team of investigatorshas been testing neural stem cells as vehiclesfor cell-based gene therapy for brain tumors knownas gliomas. Gliomas are virtually impossible to treatbecause the tumor cells readily invade the surroundingtissue and migrate extensively into the normalbrain. The researchers genetically modified humanneural stem cells to produce a protein—cytosinedeaminase—that converts a nontoxic precursor druginto an active form that kills cancer cells. The engineeredneural stem cells were then injected into thebrains of mice with human-derived gliomas. Withintwo weeks of the gene therapy and systemic treatmentwith the precursor drug, the tumors had shrunkby 80 percent. The animal studies also revealed thatneural stem cells were able to quickly and accurately“find” glioma cells, regardless of whether the stemcells were implanted directly into the tumors, implantedfar from the tumors (but still within the brain), orinjected into circulating blood outside the brain [1].Another cell-based gene therapy system underinvestigation involves the use of osteoblasts, or boneformingstem cells. In a recent preliminary studyexamining a gene therapy approach to bone repairand regeneration, researchers genetically engineeredosteoblasts to produce a bone growth factor. Theosteoblasts were added to a biodegradable matrixthat could act as a “scaffold” for new bone formation.Within a month after the cell-impregnatedscaffold was implanted into mice, new bone formationwas detectable. Although this work is in the veryearly stages, it offers hope of an effective alternativeto conventional bone-grafting techniques [14].HOW EMBRYONIC STEM CELLSMIGHT PLAY A ROLE IN GENETHERAPY RESEARCHWith one notable exception, no therapeutic effectshave been achieved in gene therapy trials to date.The first successful gene therapy occurred in a recentFrench study in which a therapeutic transgene forcorrecting X-linked severe combined immunedeficiency was introduced into the bone marrowcells of children, resulting in improved function of theirimmune systems and correction of the disease [5].This encouraging success aside, the generally disappointingresults are due, in part, to the inherent limitationsof adult and cord blood stem cells. In principleat least, the use of human embryonic stem cellsmight overcome some of these limitations, but furtherresearch will be needed to determine whetherembryonic stem cells are better suited to meet theneeds of gene therapy applications than are adultstem cells.One important feature of the optimal cell for deliveringa therapeutic transgene would be its ability toretain the therapeutic transgene even as it proliferatesor differentiates into specialized cells. Most of thecell-based gene therapies attempted so far haveused viral vehicles to introduce the transgene into thehematopoietic stem cell. One way to accomplish thisis to insert the therapeutic transgene into the one ofthe chromosomes of the stem cell. Retroviruses areable to do this, and for this reason, they are oftenused as the vehicle for infecting the stem cell andintroducing the therapeutic transgene into thechromosomal DNA. However, mouse retroviruses areonly efficient at infecting cells that are actively dividing.Unfortunately, hematopoietic stem cells are quiescentand seldom divide. The percentage of stemcells that actually receive the therapeutic transgenehas usually been too low to attain a therapeuticeffect. Because of this problem, investigators havebeen exploring the use of viral vehicles that caninfect nondividing cells, such as lentiviruses (e.g., HIV)or adeno-associated viruses. This approach has notbeen entirely successful, however, because ofproblems relating to the fact that the cells themselvesare not in an active state [13, 19].One approach to improving the introduction of transgenesinto hematopoietic stem cells has been tostimulate the cells to divide so that the viral vehiclescan infect them and insert the therapeutic transgene.Inder Verma of the Salk Institute has noted, however,that this manipulation can change other importantproperties of the hematopoietic stem cells, such asplasticity, self-renewal, and the ability to survive andgrow when introduced into the patient [23]. This possibilitymight be overcome with the use of embryonicstem cells if they require less manipulation. And infact, some preliminary data suggest that retroviralvectors may work more efficiently with embryonicstem cells than with the more mature adult stemcells. For example, researchers have noted that retroviralvectors introduce transgenes into human fetalcord blood stem cells more efficiently than into cordblood stem cells from newborns, and that the fetalcord blood stem cells also had a higher proliferative102
Use of Genetically Modified <strong>Stem</strong> <strong>Cells</strong> in Experimental Gene Therapiescapacity (i.e., they underwent more subsequent celldivisions). This suggests that fetal cord blood stem cellsmight be useful in cell-based in utero gene therapyto correct hematopoietic disorders before birth [15, 21].In some cases—such as a treatment of a chronicdisease—achieving continued production of the therapeutictransgene over the life of the patient will bevery important. Generally, however, gene therapiesusing hematopoietic stem cells have encountered aphenomenon known as “gene silencing,” where, overtime, the therapeutic transgene gets “turned off” dueto cellular mechanisms that alter the structure of thearea of the chromosome where the therapeuticgene has been inserted [6, 7, 11, 22, 24]. Whetherthe use of embryonic stem cells in gene therapycould overcome this problem is unknown, althoughpreliminary evidence suggests that this phenomenonmay occur in these cells as well [8,18].Persistence of the cell containing the therapeutictransgene is equally important for ensuring continuedavailability of the therapeutic agent. Verma notedthat the optimal cells for cell-mediated gene transferwould be cells that will persist for “the rest of thepatient’s life; they can proliferate and they wouldmake the missing protein constantly and forever” [23].Persistence, or longevity, of the cells can come aboutin two ways: a long life span for an individual cell, ora self-renewal process whereby a short-lived cellundergoes successive cell divisions while maintainingthe therapeutic transgene. Ideally, then, the geneticallymodified cell for use in cell-based gene therapyshould be able to self-renew (in a controlled mannerso tumors are not formed) so that the therapeuticagent is available on a long-term basis. This is one ofthe reasons why stem cells are used, but adult stemcells seem to be much more limited in the numberof times they can divide compared with embryonicstem cells. The difference between the ability of adultand embryonic stem cells to self-renew has beendocumented in the mouse, where embryonic stemscells were shown to have a much higher proliferativecapacity than do adult hematopoietic stem cells [25].Researchers are beginning to understand the biologicalbasis of the difference in proliferative capacitybetween adult and embryonic stem cells. Persistenceof cells and the ability to undergo successive celldivisions are in part, at least, a function of the lengthof structures at the tips of chromosomes calledtelomeres. Telomere length is, in turn, maintained byan enzyme known as telomerase. Low levels oftelomerase activity result in short telomeres and, thus,fewer rounds of cell division—in other words, shorterlongevity. Higher levels of telomerase activity result inlonger telomeres, more possible cell divisions, andoverall longer persistence. Mouse embryonic stemcells have been found to have longer telomeres andhigher levels of telomerase activity compared withadult stem cells and other more specialized cells inthe body. As mouse embryonic stem cells give rise tohematopoietic stem cells, telomerase activity levelsdrop, suggesting a decrease in the self-renewingpotential of the hematopoietic stem cells [3,4]. (Formore detailed information regarding telomeres andtelomerase, see Figure C.2. Telomeres andTelomerase.)Human embryonic stem cells have also been shownto maintain pluripotency (the ability to give rise toother, more specialized cell types) and the ability toproliferate for long periods in cell culture in the laboratory[2]. Adult stem cells appear capable of only alimited number of cell divisions, which would preventlong-term expression of the therapeutic gene neededto correct chronic diseases. “Embryonic stem cellscan be maintained in culture, whereas that is nearlyimpossible with cord blood stem cells,” says RobertHawley of the American Red Cross Jerome H. HollandLaboratory for Biomedical Sciences, who is developinggene therapy vectors for insertion into humanhematopoietic cells [12]. “So with embryonic stemcells, you have the possibility of long-term maintenanceand expansion of cell lines, which has notbeen possible with hematopoietic stem cells.”The patient’s immune system response can beanother significant challenge in gene therapy. Mostcells have specific proteins on their surface that allowthe immune system to recognize them as either “self”or “nonself.” These proteins are known as major histocompatibilityproteins, or MHC proteins. If adult stemcells for use in gene therapy cannot be isolated fromthe patient, donor cells can be used. But because ofthe differences in MHC proteins among individuals,the donor stem cells may be recognized as nonselfby the patient’s immune system and be rejected.John Gearhart of Johns Hopkins University and PeterRathjen at the University of Adelaide speculate thatembryonic stem cells may be useful for avoidingsuch immune reactions [10, 20]. For instance, it maybe possible to establish an extensive “bank” of103
Use of Genetically Modified <strong>Stem</strong> <strong>Cells</strong> in Experimental Gene Therapiesembryonic stem cell lines, each with a different setof MHC genes. Then, an embryonic stem cell that isimmunologically compatible for a patient could beselected, genetically modified, and triggered todevelop into the appropriate type of adult stem cellthat could be administered to the patient. By geneticallymodifying the MHC genes of an embryonicstem cell, it may also be possible to create a “universal”cell that would be compatible with all patients.Another approach might be to “customize” embryonicstem cells such that cells derived from themhave a patient’s specific MHC proteins on theirsurface and then to genetically modify them for usein gene therapy. Such approaches are hypotheticalat this point, however, and research is needed toassess their feasibility.Ironically, the very qualities that make embryonicstem cells potential candidates for gene therapy (i.e.,pluripotency and unlimited proliferative capacity) alsoraise safety concerns. In particular, undifferentiatedembryonic stem cells can give rise to teratomas,tumors composed of a number of different tissuetypes (see Chapter 10. Assessing Human <strong>Stem</strong> CellSafety). It may thus be preferable to use a differentiatedderivative of genetically modified embryonicstem cells that can still give rise to a limited numberof cell types (akin to an adult stem cell). CautionsEsmail Zanjani of the University of Nevada, “We coulddifferentiate embryonic stem cells into, say, liver cells,and then use them, but I don’t see how we can takeembryonic stem cells per se and put genes intothem to use therapeutically” [26].Further research is needed to determine whether thedifferentiated stem cells retain the advantages, suchas longer life span, of the embryonic stem cells fromwhich they were derived. Because of the difficulty inisolating and purifying many of the types of adultstem cells, embryonic stem cells may still be bettertargets for gene transfer. The versatile embryonicstem cell could be genetically modified, and then, intheory, it could be induced to give rise to all varietiesof adult stem cells. Also, since the genetically modifiedstem cells can be easily expanded, large, purepopulations of the differentiated cells could be producedand saved. Even if the differentiated cellswere not as long-lived as the embryonic stem cells,there would still be sufficient genetically modifiedcells to give to the patient whenever the needarises again.Achieving clinical success with cell-based genetherapy will require new knowledge and advances inseveral key areas, including the design of viral andnonviral vehicles for introducing transgenes into cells,the ability to direct where in a cell the transgene isintroduced, the ability to direct the genetically modifiedstem cells or the secreted therapeutic agent todiseased tissues, optimization and regulation of theproduction of the therapeutic agent within the stemcell, and management of immune reactions to thegene therapy process. The ability of embryonic stemcells to generate a wide variety of specialized celltypes and being able to maintain them in the laboratorywould make embryonic stem cells a promisingmodel for exploring critical questions in many ofthese areas.“There are possibilities of long-term maintenance andexpansion of embryonic stem cells and of differentiationalong specific lineages that have not beenpossible with hematopoietic stem cells,” Zanjani says.“And if they [embryonic stem cells] could be used [inthe laboratory] as a model for differentiation, youcould evaluate … vectors for gene delivery and getan idea of how genes are translated in patients.”Cynthia Dunbar, a gene therapy researcher at theNational Institutes of Health, similarly notes thatembryonic stem cells could be useful not only inscreening new viral and nonviral vectors designed tointroduce therapeutic transgenes into cells, but especiallyfor testing levels of production of the therapeuticagent after the embryonic stem cells differentiatein culture [9]. Explains Dunbar, “These behaviors arehard to predict for human cells based on animalstudies … so this would be a very useful laboratorytool.” Indeed, the major contribution of embryonicstem cells to gene therapy may be to advance thegeneral scientific knowledge needed to overcomemany of the current technical hurdles to successfultherapeutic gene transfer.REFERENCES1. Aboody, K.S., Brown, A., Rainov, N.G., Bower, K.A., Liu, S.,Yang, W., Small, J.E., Herrlinger, U., Ourednik, V., Black, P.M.,Breakefield, X.O., and Snyder, E.Y. (2000). Neural stem cellsdisplay extensive tropism for pathology in adult brain:evidence from intracranial gliomas. Proc. Natl. Acad. Sci.U. S. A. 97, 12846-12851.104
Use of Genetically Modified <strong>Stem</strong> <strong>Cells</strong> in Experimental Gene Therapies2. Amit, M., Carpenter, M.K., Inokuma, M.S., Chiu, C.P., Harris,C.P., Waknitz, M.A., Itskovitz-Eldor, J., and Thomson, J.A.(2000). Clonally derived human embryonic stem cell linesmaintain pluripotency and proliferative potential forprolonged periods of culture. Dev. Biol. 227, 271-278.3. Armstrong, L., Lako, M., Lincoln, J., Cairns, P.M., and Hole, N.(2000). mTert expression correlates with telomerase activityduring the differentiation of murine embryonic stem cells.Mech. Dev. 97, 109-116.4. Betts, D.H., Bordignon, V., Hill, J.R., Winger, Q., Westhusin,M.E., Smith, L.C., and King, W.A. (2001). Reprogramming oftelomerase activity and rebuilding of telomere length incloned cattle. Proc. Natl. Acad. Sci. U. S. A. 98, 1077-1082.5. Cavazzana-Calvo, M., Hacein-Bey, S., de Saint, B.G., Gross,F., Yvon, E., Nusbaum, P., Selz, F., Hue, C., Certain, S.,Casanova, J.L., Bousso, P., Deist, F.L., and Fischer, A. (2000).Gene therapy of human severe combined immunodeficiency(SCID)-X1 disease. Science. 288, 669-672.6. Challita, P.M. and Kohn, D.B. (1994). Lack of expression froma retroviral vector after transduction of murine hematopoieticstem cells is associated with methylation in vivo.Proc. Natl. Acad. Sci. U. S. A. 91, 2567-2571.7. Chen, W.Y. and Townes, T.M. (2000). Molecular mechanismfor silencing virally transduced genes involves histonedeacetylation and chromatin condensation. Proc. Natl.Acad. Sci. U. S. A. 97, 377-382.8. Cherry, S.R., Biniszkiewicz, D., van Parijs, L., Baltimore, D., andJaenisch, R. (2000). Retroviral expression in embryonic stemcells and hematopoietic stem cells. Mol. Cell. Biol. 20,7419-7426.9. Dunbar, C., personal communication.10. Gearhart, J. (1998). New potential for human embryonicstem cells. Science. 282, 1061-1062.11. Halene, S. and Kohn, D.B. (2000). Gene therapy usinghematopoietic stem cells: Sisyphus approaches the crest.Hum. Gene Ther. 11, 1259-1267.12. Hawley, R., personal communication.13. Korin, Y.D. and Zack, J.A. (1998). Progression to the G(1)bphase of the cell cycle is required for completion ofhuman immunodeficiency virus type 1 reverse transcriptionin T cells. J. Virol. 72, 3161-3168.14. Laurencin, C.T., Attawia, M.A., Lu, L.Q., Borden, M.D., Lu,H.H., Gorum, W.J., and Lieberman, J.R. (2001). Poly(lactide-coglycolide)/hydroxyapatitedelivery of BMP-2-producing cells:a regional gene therapy approach to bone regeneration.Biomaterials. 22, 1271-1277.15. Luther-Wyrsch, A., Costello, E., Thali, M., Buetti, E., Nissen, C.,Surbek, D., Holzgreve, W., Gratwohl, A., Tichelli, A., andWodnar-Filipowicz, A. (2001). Stable transduction with lentiviralvectors and amplification of immature hematopoieticprogenitors from cord blood of preterm human fetuses.Hum. Gene. Ther. 12, 377-389.16. Mohajeri, M.H., Figlewicz, D.A., and Bohn, M.C. (1999).Intramuscular grafts of myoblasts genetically modified tosecrete glial cell line-derived neurotrophic factor preventmotoneuron loss and disease progression in a mousemodel of familial amyotrophic lateral sclerosis. Hum. GeneTher. 10, 1853-1866.17. Ozawa, C.R., Springer, M.L., and Blau, H.M. (2000). A novelmeans of drug delivery: myoblast-mediated gene therapyand regulatable retroviral vectors. Annu. Rev. Pharmacol.Toxicol. 40, 295-317.18. Pannell, D., Osborne, C.S., Yao, S., Sukonnik, T., Pasceri, P.,Karaiskakis, A., Okano, M., Li, E., Lipshitz, H.D., and Ellis, J.(2000). Retrovirus vector silencing is de novo methylaseindependent and marked by a repressive histone code.EMBO J. 19, 5884-5894.19. Park, F., Ohashi, K., Chiu, W., Naldini, L., and Kay, M.A.(2000). Efficient lentiviral transduction of liver requires cellcycling in vivo. Nat. Genet. 24, 49-52.20. Rathjen, P.D., Lake, J., Whyatt, L.M., Bettess, M.D., andRathjen, J. (1998). Properties and uses of embryonic stemcells: prospects for application to human biology andgene therapy. Reprod. Fertil. Dev. 10, 31-47.21. Shields, L.E., Kiem, H.P., and Andrews, R.G. (2000). Highlyefficient gene transfer into preterm CD34 + hematopoieticprogenitor cells. Am. J. Obstet. Gynecol. 183, 732-737.22. Struhl, K. (1998). Histone acetylation and transcriptionalregulatory mechanisms. Genes. Dev. 12, 599-606.23. Verma, I., personal communication.24. Wade, P.A., Pruss, D., and Wolffe, A.P. (1997). Histoneacetylation: chromatin in action. Trends Biochem. Sci. 22,128-132.25. Yoder, M.C. and Hiatt, K. (1999). Murine yolk sac and bonemarrow hematopoietic cells with high proliferative potentialdisplay different capacities for producing colony-formingcells ex vivo. J. Hemato. <strong>Stem</strong> Cell Res. 8, 421-430.26. Zanjani, E., personal communication.105
Use of Genetically Modified <strong>Stem</strong> <strong>Cells</strong> in Experimental Gene TherapiesThis page intentionally left blank106
APPENDIX A:EARLY DEVELOPMENTHow does a single cell—the fertilized egg—give riseto a complex, multicellular organism? The questionreflects one of the greatest mysteries of life, and representsa fundamental challenge in developmentalbiology. As yet, knowledge about the processes bywhich a fertilized egg divides (cleavage), forms a ballof cells (morula), develops a cavity (blastocyst stage),forms the three primary germ layers of cells that willultimately give rise to all the cell types of the body(gastrula stage), and ultimately generates all thespecialized tissues and organs of a mature organismis far from complete. Little is known about the specificgenes that regulate these early events or how interactionsamong cells or how cellular interactions withother factors in the three-dimensional environment ofthe early embryo affect development. The processesby which a fertilized egg becomes an embryo,called embryogenesis, include coordinated celldivision, cell specialization, cell migration, andgenetically programmed cell death [24, 35].A description of the stages of early embryogenesis inhumans and mice follows. It includes an explanationof some of the more technical terms and conceptsthat are used throughout the document. It alsoincludes a selective discussion of some of the genes,molecules, signaling pathways, and other influenceson early embryonic development in the living organism(in vivo) that are used in experiments with stemcells maintained in the laboratory (in vitro).EXPERIMENTAL SYSTEMS USED TOUNDERSTAND EMBRYOGENESISMany kinds of experimental systems have been usedto understand how a fertilized egg produces a blastocyst,the first structure in which any cell specializationoccurs, and a gastrula, in which the three embryonicgerm layers—endoderm, mesoderm, andectoderm—first appear. They include experimentswith yeast cells; invertebrates such as tiny, jellyfish-likehydra, the microscopic roundworm Caenorhabditiselegans, and the fruit fly Drosophila melanogaster;and vertebrates such as amphibians, chick embryosand more recently, zebrafish Danio rerio, which aretransparent as embryos and allow the detailedmonitoring of cell differentiation and migration duringdevelopment. The vast majority of studies on embryogenesisin mammals has been conducted in mice.For obvious ethical reasons, detailed research onhuman embryos has been limited. But the study ofembryogenesis in all of these systems yields as manyquestions as answers.For example, what signals the earliest cell differentiationevents in the embryo? What regulates theactivity of genes that are important for embryonicdevelopment? How and when are the axes of theembryo’s body—anterior-posterior (head-tail), dorsalventral(back-belly), left-right—determined? What roledoes genetically controlled cell death, also known asapoptosis, play in embryogenesis? What influencesthe cell cycle, the controlled series of molecularevents that leads to cell division or the cessation ofcell division?Much of the information about human embryonicdevelopment comes from studies of embryogenesisin the mouse. Like mammalian embryonic developmentin general, many aspects of embryogenesis inmice resembles that of humans, but development inmice also differs in several important respects fromhuman development. For example, embryonic andfetal development in mice takes 18 to 20 days; inhumans, the process takes nine months. The placentaforms and functions differently in the two species. Inhumans, an embryonic disk develops after theembryo implants in the uterine wall, whereas in micean egg cylinder forms. The yolk sac of a mouseembryo persists and functions throughout gestation;in humans, the yolk sac functions only in earlyembryogenesis [28]. The primary roles of the humanA-1
Appendix A: Early Developmentembryonic yolk sac are to initiate hematopoiesis andhelp in the formation of the primary germ cells, whichwill ultimately differentiate into eggs and sperm in theadult. And even for mice, knowledge about the genes,factors, and signal-transduction pathways that controlembryonic development is limited. Signal transductionis a series of molecular events triggered by a signal atthe surface of the cell and leading to a response bythe cell—the secretion of a hormone, or a change inthe activity of a particular gene, for instance [20].Other sources of information about human developmentinclude studies of human embryonal carcinoma(EC) cells maintained in vitro and of histologicalsections of human embryos. (EC cells are derivedfrom unusual tumors called teratocarcinomas, whichmay form spontaneously in the human testis orovary.) Also, within the past 20 years, clinics andresearch institutes in many countries have developedin vitro conditions that allow fertilization and blastocystformation. Thus, the study of methods to improvepregnancy rates following in vitro fertilization (IVF) hasyielded important information about early humanembryogenesis.A FERTILIZED EGG FORMS ABLASTOCYSTPrior to fertilization in humans and mice, the egg(oocyte) enlarges, divides by meiosis, and matures inits ovarian follicle until it reaches a stage of meioticdivision called metaphase II (see Figure A.1. CellCycle). At this point, the follicle releases the oocyteinto the oviduct, one of two tube-like structures thatlead from the ovaries to the uterus. The matureoocyte, a haploid cell that contains half the normalnumber of chromosomes, is surrounded by a protectivecoat of noncellular material (made of extracellularmatrix and glycoproteins), called the zonapellucida. For fertilization to occur, a haploid spermcell must bind to and penetrate the zona pellucida,fuse with the cell membrane of the oocyte, enter theoocyte cytoplasm, and fuse its pronucleus with theoocyte pronucleus. Fusion of the sperm and eggpronuclei restores the number of chromosomes thatis typical of a given species. In humans, the normaldiploid number of chromosomes for all the cells ofthe body (somatic cells) is 46 (23 pairs of chromosomes).Mature sperm and egg cells (germ cells)Cdk1/CycA,CycBCdk 2,3,4/CycD(Gap 2) G2S(Mitosis)MG1 (Gap 1)© 2001 Terese Winslow, Lydia KibiukCdk2/CycACdk2/CycEFigure A.1. Cell Cycle.A-2
Appendix A: Early Developmentin contrast, carry only 23 chromosomes, the haploidnumber [1].Under normal conditions, fertilization of the humanoocyte occurs in the oviduct, near the ovary. Ahuman egg is many times larger than a sperm cell,which means the oocyte contributes most of thecytoplasm of the zygote, another name for the fertilizedegg. As a result, any maternal gene products inthe zygote cytoplasm influence its first few divisions,called cleavages. Within several days, and afterseveral cleavages, the genome (all the DNA orhereditary information in the cell’s chromosomes) ofthe zygote becomes activated and controls subsequentembryonic development [19, 28]. Also, duringthese initial cleavages, the resulting daughter cells donot increase in size. Rather, as early cell division proceeds,the amount of cytoplasm of each daughtercell is reduced by half, and the total volume of theearly embryo remains unchanged from that of thefertilized egg [30, 35].After fertilization, the zygote makes its way to theuterus, a journey that takes three to four days in miceand five to seven days in humans. As it travels, thezygote divides. The first cleavage produces twoidentical cells and then divides again to produce fourcells. If these cells separate, genetically identicalembryos result, the basis of identical twinning. Usually,however, the cells remain together, dividing asynchronouslyto produce 8 cells, 16 cells, and so on [19].Each early round of cell division takes approximately36 hours, according to information gleaned from thestudy of human embryos in vitro [34]. In humans andmice, at about the eight-cell stage, the embryocompacts, meaning that the formerly “loose” ball ofcells comes together in a tight array that is interconnectedby gap junctions. These specializedmembrane structures consist of an array of six proteinmolecules called connexins, which form a pore thatallows the exchange of ions and small moleculesbetween cells [27].Recent information from studies of mouse embryosindicates that even at this early stage of embryogenesis,the anterior-posterior axis of the embryo hasbeen established, a point of some concern for invitro fertilization techniques, which disrupt earlypatterning events. The establishment of the anteriorposterioraxis is critical to normal fetal development,because it helps determine the overall body plan ofthe embryo [3, 15, 18].By the 16-cell stage, the compacted embryo istermed a morula. In mice, the first evidence that cellshave become specialized occurs when the outercells of the 16-cell morula divide to produce an outerrim of cells—the trophectoderm—and an inner coreof cells, the inner cell mass [19]. Although the signalswithin the 16-cell morula that regulate the differentiationof the trophectoderm are largely unknown, it isclear that the outer cells of the morula are polarized.That is, one side of the cell differs from the other side.Thus, in the first differentiation event of embryogenesis,the outer, polar cells give rise to trophectodermand the inner, apolar cells become the inner cellmass. This suggests that individual cells of the earlyembryo exhibit more intrinsic polarity than hadbeen thought [27].Ultimately, the cells of the inner cell mass will give riseto all the tissues of the embryo’s body, as well as tothe nontrophoblast tissues that support the developingembryo. The latter are referred to as extraembryonictissues and include the yolk sac, allantois,and amnion. The trophectoderm, in turn, will generatethe trophoblast cells of the chorion, the embryo’scontribution to the extraembryonic tissue known asthe placenta [19, 28].The cells of the inner cell mass and trophectodermcontinue to divide. Information gained from the studyof mouse embryos suggests that the two tissues needto interact; the inner cell mass helps maintain theability of trophectoderm cells to divide, and thetrophectoderm appears to support the continueddevelopment of the inner cell mass [32]. Secretedparacrine factors (molecular signals that affect othercell types), including fibroblast growth factor-4(FGF-4), which is released from inner cell mass cells[46], help direct embryogenesis at this stage. FGF-4signaling also helps regulate the division and differentiationof trophectoderm cells [29].By embryonic day 3 (E3.0) in the mouse and days 5to 6 in human development [14], the embryo developsa cavity called the blastocoel. It fills with a wateryfluid secreted by trophectodermal cells and transportedin from the exterior. As a result of cavitationand the physical separation and differentiation of thetrophectoderm from the inner cell mass, the morulabecomes a blastocyst. Its chief structural features arethe outer sphere of flattened trophectoderm cells(which become the trophoblast), the small, roundA-3
Appendix A: Early DevelopmentDAY 1DAY 0FirstcleavageFertilized egg(zygote)FertilizationDAY 22-cellstageOvary4-cellstageDAY 3–48-celluncompactedmorulaDAY 4UterusEarlyblastocyst8-cellcompactedmorulaDAY 5TrophectodermBlastocoelInnercell massDAY 6–7ZonapellucidaOocyteOvulationLate-stageblastocyst(hatching)DAY 8–9Epiblast© 2001 Terese WinslowImplantationof theblastocystHypoblastFigure A.2. Development of the Preimplantation Blastocyst in Humans.cells of the inner cell mass, and the fluid-filledblastocoel [3, 19].By E4.0 in mice, and between 5 to 7 days postfertilizationin humans, the blastocyst reaches theuterus. It has not yet implanted into the uterine walland is therefore still a pre-implantation embryo. Whenit arrives in the uterus, the blastocyst “hatches” out ofthe zona pellucida, the structure that originallysurrounded the oocyte and that also prevented theimplantation of the blastocyst into the wall of theoviduct [19]. (An embryo that does implant in theoviduct results in a tubal pregnancy, which can resultin severe hemorrhaging.)The nutritional requirements of the embryo changemarkedly during the time from zygote formation tothe compaction of the morula, to the developmentof the blastocyst. Also, the physiology and biochemistryof the cells change as they increase in numberand begin to differentiate. For example, the primarysources of energy for the cleavage-stage embryoare pyruvate, lactate, and amino acids—simplemolecules that play important roles in various metabolicpathways. But after compaction of the morula,glucose is taken up by the embryo and used as aprimary source of energy [15]. Indeed, mammalianblastocysts may have a unique transporter molecule,GLUT8, that ferries glucose into the blastocyst. GLUT8appears in the blastocyst at the same time as thereceptor for insulin-like growth factor–1 (IGF-1). Thus,the blastocyst, which requires a great deal of energyat this stage of development, is equipped to respondto insulin by taking up glucose [7].These and other observations about the preimplantationblastocyst have led to recommendationsA-4
Appendix A: Early DevelopmentE1.52-cellsE2.04-cellsE2.58-cellsuncompactedE3.0ZonapellucidaInnercell mass E4.0TrophoblastE1.0OvaryOocyte8-cellscompactedEarlyblastocyst(hatching)LateblastocystEpiblastHypoblastE4.5UterusFertilizedegg(zygote)E0OvulationImplantationFertilizationE0.5© 2001 Terese WinslowFigure A.3. Development of the Preimplantation Blastocyst in Mice from Embryonic Day 0 (E0) Through Day 5 (E5.0).about the importance of adapting the cultureconditions to accommodate the changing nutritionalrequirements of the embryo when animal embryosare grown in the laboratory [16].It is at this stage of embryogenesis—near the end ofthe first week of development in humans and aboutE4.0 in mice—that embryonic stem (ES) cells can bederived from the inner cell mass of the blastocyst.Human ES cells are derived from embryos generatedthrough in vitro fertilization procedures and donatedfor research. An embryo at this stage of developmentin vivo would not yet be physically connected to theuterine wall; it would still be a preimplantationembryo.ES cells, per se, may be an in vitro phenomenon.Some scientists argue that the apparent immortalityof ES cells occurs only in a laboratory culture dish[41]. ES cells that are grown in the laboratory mostclosely resemble cells of the epiblast [5], but ES cellsare not identical to epiblast cells [42]. The termepiblast refers to all the pluripotent cell populationsthat follow the formation of the primitive endodermand precede the formation of the gastrula [23]. Likethe epiblast cells of the embryo, ES cells in culturehave the potential to give rise to all the cell typesof the body. However, unlike the epiblast cells ofthe embryo, ES cells in vitro cannot give rise to acomplete organism. They do not have the threedimensionalenvironment that is essential forembryonic development in vivo, and they lack thetrophectoderm and other tissues that support fetaldevelopment in vivo (see Chapter 2. The Embryonic<strong>Stem</strong> Cell).A-5
Appendix A: Early DevelopmentTHE BLASTOCYST IMPLANTS IN THEUTERINE WALLMany of the molecular and cellular events that occurduring the second week of human embryonic development,and at the end of the first week of embryogenesisin the mouse, help establish the placenta.The placenta connects the fetal and maternal bloodstreamsand provides nutrients to the embryothroughout the remainder of gestation.On or about postfertilization days 8 to 9 in humans(and E4.5 in the mouse), the ball-shaped embryoimplants into in the uterine wall (see Figure A.2.Development of the Preimplantation Blastocyst inHumans). The inner cell mass of the human embryoat this stage has split into layers. One is the hypoblast,which lies next to the blastocoel and gives rise to theprimitive endoderm. (Later, the primitive endodermwill give rise to the outer layer of the yolk sac, acurious reminder of reptilian ancestry in mammalianembryos.) The other cell layer that develops from theinner cell mass is the epiblast. It will give rise to all thecells of the embryo’s body [19, 23].The epiblast can be thought of as the group of cellsthat succeeds the inner cell mass. Pluripotent cellsare defined differently in scientific articles and textbooks. In general, however, pluripotent cells arecapable of giving rise to all the kinds of cells thatoccur in the mature organism. So at this stage ofembryogenesis, the only pluripotent cells are theundifferentiated cells of the epiblast.By E6.0 in the mouse, three differentiated cell typesexist: the trophoblast, the epiblast (also called theembryonic ectoderm or primitive ectoderm at thisstage), and the primitive endoderm (see Figure A.3.Development of the Preimplantation Blastocyst inMice). During the next major phase of development,termed gastrulation, the embryonic ectoderm willdifferentiate into the three primary germ layers—endoderm, mesoderm, and ectoderm. Thus, theembryonic ectoderm has succeeded the epiblast asthe tissue that will generate the body of the embryo.The primitive endoderm differentiates into parietaland visceral endoderm, the anterior region of whichwill help regulate the development of the body planduring gastrulation [23].Prior to gastrulation, the majority of cells (approximately75 percent) in the preimplantation blastocystcomprise the trophectoderm and the primitiveendoderm. The preimplantation mouse embryoconsists of approximately 200 cells, approximately 20to 25 of which are inner cell mass or epiblast cells[20, 23]. The day 5, preimplantation human embryocontains 200 to 250 cells, only 30 to 34 of which areinner cell mass cells [4].The extraembryonic cells of both species differentiateinto the tissues that will convey nutrients to theembryo and remove its waste products. For example,some of the trophoblast cells invade the epitheliallining of the uterus (also known as the decidua), andform a multinucleated tissue called a syncitium. Thissyncytiotrophoblast, as it is called, then developslacunae (cavities). By postfertilization day 10 to11 inhumans, the syncytiotrophoblast becomes suppliedwith maternal blood vessels. The fusion of the embryonicchorion and the maternal decidua and vasculartissue generates the placenta [19, 29].The formation of the placenta is a critical process inhuman embryogenesis. Without a healthy placenta,the embryo does not survive; its malformation cantrigger a spontaneous abortion [49]. The placentaanchors the developing embryo to the uterine walland connects it to the maternal bloodstream, thussupplying the embryo with ions and metabolites andproviding a waste-removal mechanism for theembryo [10, 26]. Later, the umbilical cord connectsthe embryo to the chorion portion of the placenta.The cord contains the fetal arteries and veins. Usually,the maternal and fetal blood do not mix directly.Instead, soluble substances pass through fingerlikeprojections called villi that have embedded in theuterine wall, and that have also developed from thetrophoblast of the embryo [19].In mice, some of the genes that regulate the developmentof the placenta have been identified. Oneis the Mash2 gene, which is expressed in the trophoblastcells of the embryo after it implants into theuterine wall. If Mash2 is inactivated, the placentadoes not form and the embryo dies (at E10.5 in themouse) [21, 45]. However, it is not known whether thesame genes that regulate placenta formation in themouse act in humans.Meanwhile, during postfertilization days 7 to 14 ofhuman development, the epiblast splits to form theamnionic cavity. The cavity fills with fluid and cushionsthe embryo throughout gestation.A-6
Appendix A: Early DevelopmentTHE BLASTOCYST BECOMESA GASTRULAAt the start of the third week of human development,and about E6.0 in the mouse (the egg-cylinderstage), the cells of the epiblast begin to differentiate.By the end of the third week, they will have generatedthe three primary germ layers of the embryo—endoderm,mesoderm, and ectoderm. A detailed descriptionof all the events of this critical stage of differentiation—knownas gastrulation—is beyond the scopeof this report. However, the onset of gastrulation istriggered at the posterior end of the embryo with theformation of a structure called the node (fromHensen’s node in chick embryogenesis). The node,together with another important signaling center, theanterior visceral endoderm (AVE), helps regulate theformation of the pattern of the embryo’s body at thisstage of development [19].The process of gastrulation begins between days 14and 16 of human development and at about E6.5 inthe mouse. At that time, a primitive streak forms in aspecific region of the epiblast along the posterior axisof the embryo. Little is known about the signals thatregulate the generation of the primitive streak,although the genes goosecoid, T, Evx-1, and follistatinare expressed [23]. Nevertheless, the forward migrationof the posterior epiblast cells occurs as theircell-cell contacts break down, and they releaseenzymes that digest the basement membrane thatlies underneath. This allows the epiblast cells tomigrate into the space between the epiblast andthe visceral endoderm [6].The forward-moving epiblast cells also spread laterally,a migration that induces the formation of themesoderm and the notochord. The notochord is atemporary, rod-like structure that develops along thedorsal surface of the embryo and will ultimatelyconnect the anterior visceral endoderm (AVE) andthe node. <strong>Cells</strong> at the anterior end of the notochordwill eventually underlie the forebrain [19].At the anterior end of the primitive streak is the node,a two-layered structure and important signalingcenter in the embryo. The ventral layer of cells in thenode comes from the epiblast and generates thenotochordal plate, which then forms the notochord.Endoderm, which will give rise to the gut, also developsnear the node, along the sides of the notochord.Meanwhile, the anterior region of the mesoderm thatdevelops from the primitive streak is preparing to giverise to the heart. The anterior epiblast is generatingthe neuroectoderm and the ectoderm that coversthe surface of the embryo. The ectodermal tissuethat lies dorsal to the notochord will generate theneural plate, which will round up to form the neuraltube, the precursor to the central nervous system(brain and spinal cord) [23].Thus, by the end of the third week of embryonicdevelopment in humans, and by E8.0 in the mouse,the primitive ectoderm of the postimplantationblastocyst has generated the ectoderm, mesoderm,and endoderm of the gastrula (see Figure A.4.Development of Human Embryonic Tissues). Theseand other complex processes result in the formationof the tissues and organs that occur in an adultmammal (see Figure 1.1. Differentiation of HumanTissues). They require the activation and inactivationof specific genes at specific times, highly integratedcell-cell interactions, and interactions between cellsand their noncellular environment, the extracellularmatrix [3, 19].In general, the embryonic “outer” layer, or ectoderm,gives rise to the following tissues: central nervoussystem (brain and spinal cord) and peripheral nervoussystem; outer surface or skin of the organism; corneaand lens of the eye; epithelium that lines the mouthand nasal cavities and the anal canal; epitheliumof the pineal gland, pituitary gland, and adrenalmedulla; and cells of the neural crest (which givesrise to various facial structures, pigmented skin cellscalled melanocytes, and dorsal root ganglia, clustersof nerve cells along the spinal cord). The embryonic“middle” layer, or mesoderm, gives rise to skeletal,smooth, and cardiac muscle; structures of theurogenital system (kidneys, ureters, gonads, andreproductive ducts); bone marrow and blood; fat;bone, and cartilage; other connective tissues; andthe lining of the body cavity. The embryonic “inner”layer, or endoderm, gives rise to the epithelium of theentire digestive tract (excluding the mouth and analcanal); epithelium of the respiratory tract; structuresassociated with the digestive tract (liver and pancreas);thyroid, parathyroid, and thymus glands;epithelium of the reproductive ducts and glands;epithelium of the urethra and bladder [19].A-7
Appendix A: Early DevelopmentDAY0Fertilized eggExtraembryonicTissuesFertilized eggEmbryonicTissuesDAY5BlastocystBlastocystDAY6-7Inner cell massTrophoblastTrophoblastInner cell massDAY8-9EpiblastHypoblastCytotrophoblast Hypoblast EpiblastDAY12SyncytiotrophoblastCytotrophoblastSyncytiotrophoblastExtraembryonicendodermAmnioticectodermPrimitiveectodermDAY14GastrulaYolk sacPrimitive streakDAY15PrimitivestreakEmbryonicectodermExtraembryonicmesodermEmbryonicmesodermEmbryonicendodermEmbryonicectodermDAY16© 2001 Terese WinslowEmbryonicendodermEmbryonicmesodermFigure A.4. Development of Human Embryonic Tissues.A-8
Appendix A: Early DevelopmentPRIMORDIAL GERM CELLS ARE THEPRECURSORS TO EGGS AND SPERMNot to be forgotten in this developmental schemeare the primordial germ (PG) cells, which will give riseto eggs and sperm in the adult organism (see FigureA.5. Development of Mouse Embryonic PrimordialGerm <strong>Cells</strong>). Prior to gastrulation, at about the time ofprimitive streak formation, these precursor cells splitoff from the proximal region of the epiblast andmigrate into the extraembryonic mesoderm (whichgenerates the yolk sac and allantois). It is not until theproximal epiblast cells reach the extraembryonicmesoderm that they are committed to becomingPG cells. Their location in this tissue—which is remotefrom the rest of the embryo’s body, or somatic,cells—may allow PG cells to avoid some of theevents that drive somatic cells through the process ofdifferentiation. One such event is DNA methylation, ameans of silencing genes inherited from oneparent—a process termed genomic imprinting(discussed below).Another feature that distinguishes primordial germcells from somatic cells is their continuous expressionof Oct-4, a transcription factor produced by proliferating,unspecialized cells. Thus, the regulation of PGcell fate in the mammalian embryo is a result of thelocal environment of the cells, a recurring theme inmammalian embryogenesis, and the expression ofgenes in the PG cells [37]. Later in development, thePG cells embark in another migration and ultimatelycome to rest in the genital ridge, the tissue that willgive rise to the gonads: testes in males and ovariesin females [35]. In the testis, the PG cells give rise tospermatagonial stem cells that reside in the testisthroughout the life of the male. They continuouslyrenew themselves and differentiate through theprocess of spermatogenesis into mature, functionalsperm cells. There is no evidence, however, that theyhave pluripotential properties [39].SpermFertilizationBlastocystMaturityOocytePrimordialgerm cellprecursorsE5.5FetalgrowthMigration ofPrimordial germ cellsE7.5© 2001 Terese Winslow, Caitlin DuckwallGenital ridgeE10.5E8.5Primordialgerm cellsPrimordialgerm cellsFigure A.5. Development of Mouse Embryonic Primordial Germ <strong>Cells</strong>.A-9
Appendix A: Early DevelopmentGENES, MOLECULES, AND OTHERSIGNALS ARE IMPORTANT IN EARLYEMBRYOGENESISThis overview of the processes of blastocyst formation,implantation, and gastrulation has ignored most ofthe crucial signals that direct embryonic development.These signals include genes expressed by cellsat different stages of development, molecular factorssecreted by cells, complex molecular signalingsystems that allow cells to respond to secretedfactors, specialized membrane junctions thatconnect cells and allow them to communicate,components of the noncellular environment (knownas the extracellular matrix), and genomic imprinting.These signals—as well as their origins and effects—are the least understood elements of embryonicdevelopment in any organism.GENE TRANSCRIPTION, TRANS-LATION, AND PROTEIN SYNTHESISA gene is a linear segment of a DNA molecule thatencodes one or more proteins. The process occurs inthree major steps (see Figure A.6. Gene Transcription,Translation, and Protein Synthesis). The DNA, which isdouble-stranded, unwinds and copies its triplet code(varying sequences of the four nitrogen bases adenine(A), thymine (T), cytosine (C), and guanine (G))into a messenger RNA (mRNA) molecule. In RNA,uracil (U) is substituted for T. The process is calledtranscription because the triplet code of a DNAmolecule is transcribed into the triplet code of anmRNA molecule. A gene that makes an mRNA transcriptis active; the gene is said to be expressed.The process of initiating transcription is complex.It requires the binding of certain proteins, calledtranscription factors, to regions of the DNA near thesite where transcription begins. Transcription factorsbind at sequences of DNA called the promoterenhancer region. The factors can activate or represstranscription. Although some transcription factors binddirectly to the DNA molecule, many bind to othertranscription factors. Thus, protein-DNA interactionsand protein-protein interactions regulate geneactivity. Their interactions then activate or block theprocess of transcription.Transcription actually begins when the enzyme RNApolymerase II binds to the promoter region of DNA toinitiate the process of making a molecule of messengermRNA. As indicated above, the sequence ofbases in DNA—the order of A, T, C, and G—dictatesthe sequence of the mRNA which will be formed.Thus, an A in DNA can bind only to a U in mRNA. TheDNA base G will bind only to the RNA base C, and soon. RNA polymerase connects these bases togetherin a process called elongation.The second major stage of the process of makingproteins based on the code of DNA is called translation.During translation, the mRNA—which wasgenerated in the nucleus of a cell and now carries itstranscript of the DNA code—moves to the cytoplasm,where it attaches temporarily to tiny structures calledribosomes. There, molecules of mRNA direct theassembly of small molecules called amino acids (ofwhich 20 kinds exist) into proteins. Each amino acid isspecified by a code of three bases. The helpers inthis effort are molecules of transfer RNA (tRNA). EachtRNA molecule contains its own triplet code (tomatch the mRNA code), and each tRNA ferries aparticular kind of amino acid to the mRNA-ladenribosomes.Then, in the third step of protein synthesis, the aminoacids are linked through chemical bonds to createa protein molecule. Proteins typically consist ofhundreds of amino acids. Thus, the sequence ofbases in DNA determines the sequence of mRNA,which then determines the linear sequence of aminoacids in a protein. Depending on its sequence ofamino acids, a protein may fold, twist, bend, pleat,coil, or otherwise contort itself until it assumes thethree-dimensional shape that makes it functional.In the body, proteins make up most of the structuralelements of cells and tissues. They also function asenzymes, which regulate all of the body’s chemicalreactions.Gene Expression and Factors in thePreimplantation BlastocystIt is difficult to identify the genes and factors in vivothat affect the earliest events in mammalian development;maintain the undifferentiated, proliferatingstate of inner cell mass or epiblast cells; regulateimplantation; and direct the differentiation of cellsalong specific developmental pathways, or cell lineages.The embryo itself is very small and, in vivo, isalmost wholly inaccessible to study. Therefore, manyA-10
Appendix A: Early DevelopmentCellNucleusTranscriptionTranslationCytoplasmDNANuclearMembraneNewly formedmessenger RNA (mRNA)mRNABeginningof proteinNearly completedproteinBasesRibosomeDouble helixunwindsCodonNucleotideTHE ROLE OF THE RIBOSOME IN TRANSLATIONAlanineNewly formedprotein chainProlineProline ArginineAmino acid binds togrowing protein chainLeucineIsoleucineAminoacidtRNANucleusmRNAtRNA bindsto codon© 2001 Terese WinslowCytoplasmCompletedproteinRibosomeAlanine Proline Proline Arginine Leucine IsoleucineCodonFigure A.6. Gene Transcription, Translation, and Protein Synthesis.of the genetic and molecular influences that are nowknown to regulate early embryogenesis in vivo wereidentified by studying mouse embryonic stem cellsin vitro.For instance, Oct-4 is a transcription factor that hascome to be recognized as a prototypical marker ofundifferentiated, dividing cells. It is necessary formaintaining the undifferentiated state and proliferationof cells of the inner cell mass and the epiblast.Most of the studies of Oct-4 have been conductedin mouse embryos and ES cells. Oct-4 is expressed inthe mouse oocyte, it disappears during the first cleavageof the zygote, and it reappears in the four-cellmouse embryo as the genome of the zygote beginsto control embryonic development. Oct-4 persists inthe inner cell mass of the blastocyst, but does notoccur in differentiated trophectoderm cells, nor doesit occur other differentiated cell types that arise aftergastrulation in the mouse. The gene for Oct-4,Pou5f1, is expressed in primordial germ cells, however[12, 32].Oct-4 is a member of the class 5 POU (for Pit, Oct,and Unc) family of transcription factors, which bindpromoter or enhancer sites in DNA. These proteinsregulate gene transcription. The transcription factorOct-4 can activate or repress gene expression; itbinds to DNA at a distance from the start of transcription.Hence, depending on the target gene, Oct-4may require the presence of co-activator proteinssuch as the E1A-like transcription factors and theSox2 protein [37].Another target of Oct-4 in mouse embryogenesis isthe Fgf4 gene. It encodes fibroblast growth factor-4(FGF-4), a growth factor protein that is expressedtogether with Oct-4 in the inner cell mass andA-11
Appendix A: Early Developmentepiblast [32]. FGF-4 is a paracrine signal, meaningthat it is released from one cell type and it acts onanother. In this case, FGF-4 is released from proliferatinginner cell mass cells and it affects the surroundingtrophectoderm. FGF-4 may also act as an autocrinesignal, meaning that it may affect the same inner cellmass cells that released it [13].A series of recent experiments indicates that the levelof Oct-4 expression—not simply its presence orabsence in a cell—determines how mouse embryonicstem cells differentiate and whether theycontinue to proliferate [33] (see Appendix B. MouseEmbryonic <strong>Stem</strong> <strong>Cells</strong>).Two proteins, leptin and STAT3, which are producedby maternal granulosa cells that surround the oocyte,are apparently secreted into the oocyte as it maturesin its ovarian follicle. By the time the mouse or humanzygote reaches the four-cell stage, leptin and STAT3are concentrated in what may be the founder cell ofthe embryonic trophectoderm. Later, when the trophectodermdifferentiates and separates from theinner cells mass of the blastocyst, leptin and STAT3 areexpressed only in the trophectoderm, where they playa critical role during implantation [12].Leukemia inhibitory factor (LIF), a cytokine, also playsan important role during implantation. The LIF gene isexpressed in cultured mouse [31] and bovine blastocysts,as is the gene for its receptor. The mRNA for thereceptor for LIF is expressed in human blastocysts [12,47]. LIF, therefore, seems to be important for earlymammalian blastocyst development, as well asimplantation. It is also essential for the survival of theprimordial germ cells, which will become eggs andsperm in the mature organism [22]. And if mouseembryonic stem (ES) cells are cultured from the innercell mass of a blastocyst without the presence of“feeder” layers of cells, they require the addition of LIFto the culture medium in order to survive and proliferate[40]. Curiously, cultures of human ES cells donot respond to LIF [36, 48].Regulation of Body Patterning in the EmbryoAs the embryo forms, its overall body pattern is determinedby the establishment of three clear axes—theanterior-posterior axis (head-tail), the dorsal-ventral(back-belly) axis, and left-right asymmetry. The establishmentof these body axes at the correct time isfundamental to normal embryonic development. Forinstance, the central nervous system develops alongthe dorsal surface, with the largest concentration ofneuronal tissue—the brain—at the anterior end ofthe embryo. The limbs develop symmetrically andbilaterally, whereas the heart—although it begins asa symmetrical structure—ultimately comes to pointtoward the left side of the trunk. Some internal structuresare paired (the kidneys, lungs, adrenal glands,testes, and ovaries), whereas many are not (the heart,gut, pancreas, spleen, liver, and uterus) [19].Information about the establishment of these bodyaxes and their role in development is far from complete.For example, the anterior-posterior axis of themouse blastocyst may be determined before itimplants and is certainly established before gastrulation[15, 17]. An unanswered question, however, iswhether this early embryonic axis helps determine thelater development of the embryo. The early axis mayplay a role in primitive streak formation, and requiresthe expression of Wnt, which helps regulate theformation of one of embryo’s chief signaling centers:the node [38].As indicated above, an important group of cells thatproduces molecular signals that help determine theanterior-posterior axis of the mouse embryo is theanterior visceral endoderm (AVE). The AVE expressesdifferent genes along its length. At E5.0 in the mouse,for example, the Hex gene—a member of the familyof homeobox genes that help regulate body patterningof the mouse embryo—is expressed in the distalvisceral endoderm. These cells migrate to becomethe AVE, which forms on the opposite side of theembryo from the primitive streak, thus establishing theanterior-posterior axis of the fetus [17].Then, between E6.0 and E7.0 in the mouse, theanterior region of the AVE, where the heart will form,expresses Mrg1. The medial region expresses thetranscription factor genes Otx2 and Lim1, as well asother genes. The region of the AVE that lies next to thepart of the epiblast that will give rise to oral ectodermand the forebrain expresses Hesx1, another homeoboxgene. Collectively, the AVE and the genes itexpresses help regulate the development of theanterior end of the embryo [3].Other genes, notably Bmp4, also help shape themouse embryo prior to gastrulation. BMP stands forbone morphogenetic protein, a family of proteinsthat help regulate the differentiation of mesenchymalcells, which are derived from mesoderm, includingA-12
Appendix A: Early Developmentbone-forming osteoblasts, and adipocytes, which arefat cells. They also play a role in CNS development.Bmp4, which is expressed in the extraembryonicectoderm next to the epiblast and also in the innercell mass of the E3.5 and E4.5 mouse blastocyst,may activate genes in epiblast cells that thenmigrate to form the primitive streak. Wnt3 apparentlyhelps induce the formation of both the primitivestreak and the node in mammals, although there isno evidence indicating that Wnt3 expression isrequired for mesoderm induction. However, formationof the embryo’s head region, obviously a key anteriorstructure, seems to require inhibition of the activities ofWnt and Bmp4—a potential role of the AVE [3, 18].Therefore, coordinating the embryo’s “decisions”about its body pattern is a hierarchy of genes.Overall, the Hox genes specify anterior-posterior polarity.Their normal function can be subverted by retinoicacid, which can activate Hox genes in inappropriateplaces. Less is known about the establishment of thedorsal-ventral axis. It may be determined in the blastocyst,or even in the oocyte [16]; it is clearly establishedwhen the notochord develops. Genes such asNodal and Lefty help determine left-right asymmetry.Genes that regulate body patterning in embryonicdevelopment are well conserved throughout evolutionamong both vertebrates and invertebrates [19].Regulation of Cell Differentiation in EarlyEmbryogenesisMyriad other genetic and molecular signals conspireto regulate cell differentiation in the embryo. Factorsin a cell’s environment bind to receptor molecules inits membrane and activate a series of intracellularresponses that may result in gene activation or inactivation.The process by which a cell responds to anexternal signal is called signal transduction, and isitself the subject of many articles and books.One of the earliest genes to be involved in cell differentiationin the preimplantation blastocyst are thosethat encode the GATA class of transcription factors.GATA-6 is expressed in some inner cell mass cells ofthe E3.5 mouse blastocyst; GATA-4 is expressed in theE5.5 parietal and visceral endoderm. GATA-6 expressionis required for the formation of the visceralendoderm; the role of GATA-4 is less clear. Other genessuch as HNF-4, which encodes a transcription factor,and STAT3, which encodes a protein important in acytokine signaling pathway, are expressed later, duringthe early differentiation of the visceral endoderm [18].Other genes are expressed in the pregastrulationepiblast; examples are Brachyury and Cripto, whichencode secreted growth factors. Still others, includingNodal and Otx2, are expressed in both the epiblastand the visceral endoderm [18].A host of genes is expressed along the primitivestreak. These include HNF-3ß in the notochord, node,and floor plate (which will underlie the forebrain);nodal, goosecoid, T, and Lim-1, in the node;Follistatin and T for the remainder of the streak; andFGF-4 just caudal to the node.It is far easier to monitor the expression of particulargenes than it is to identify their function(s) duringdevelopment. One of the most useful kinds of experimentsfor determining the function of a gene involvesits permanent inactivation—to create a knockoutmouse, for example—followed by studies of impairedfunctions in the gene-deficient animal. Similarresearch strategies obviously cannot be used todetermine the functions of specific genes in humanembryogenesis. However, it is possible to identifyhuman genes that are important for development bystudying heritable abnormalities or congenital defectsthat have a genetic basis. Then, the function of thehuman genes—which almost certainly will have similareffects in mice—can be assessed in more detailby generating knockout mice that lack the gene.THE CELL CYCLEMany cells of the early embryo are in a constantstate of dividing or of preparing to divide. The seriesof molecular events that regulate these processes iscalled the cell cycle (see Figure A.1. Cell Cycle).The cell cycle includes four main phases: DNA synthesis(S phase), G2 (a gap phase during which thecell increases in size and prepares to divide), celldivision (also called mitosis, M phase), and G1 (a gapphase of cell growth and replication of the centrioles).When a cell exits the cell cycle, to differentiate, forexample, it is said to be in G0. Progression throughthe cell cycle is regulated by the activation of cyclindependentkinases (Cdks), enzymes that attachphosphate groups onto other proteins. Particular Cdksand their associated cyclins regulate the transitionfrom one phase of the cell cycle to the next. Forexample, in mammalian cells, Cdk2 and cyclin EA-13
Appendix A: Early Developmentregulate the transition from G1 to S, whereas Cdk1and cyclins A and B regulate the transition from S toG2. And recently, it has become clear that the cellcycle has several checkpoint mechanisms, duringwhich the cell stops its progression through the cyclewhile it repairs damaged DNA [11].The activity of the cell cycle varies, depending on thestatus of the cell and the cues—such as cytokinestimulation—the cell receives from its environment.Some cells “cycle” quickly, dividing in a matter ofhours. Others cycle slowly, and some do not cycle atall. The epiblast cells of the postimplantation E5.5 toE6.0 mouse blastocyst, for example, have a meancycle time of 11.5 hours. But a day later, at E6.5 toE7.0, epiblast cells have a mean cell cycle time ofonly 4.4 hours [23]. In contrast, the cycle time for cellsin the cleavage-stage human embryo—a muchearlier developmental stage—is approximately 36hours [34]. And cells that are terminally differentiated—maturenerve cells in the brain, for example—have stopped dividing altogether. What factors regulatethe cell cycle during development, or how thecell cycle alters gene expression or any other eventin embryogenesis, remains largely unknown.CELL DEATH IS A NORMAL PROCESSDURING EMBRYOGENESISIt is a general characteristic of undifferentiated cells—including embryonic cells in vivo or in vitro— thatwhen they stop dividing, they differentiate, becomequiescent or senescent (stop their progress throughthe cell cycle and enter a period of temporary orpermanent “rest”), or die. In vivo or in vitro, theprocess of cell death can occur by necrosis or apoptosis.The latter is a form of genetically controlled celldeath that, in itself, is an important aspect of normalembryonic development in vivo. When the geneticprogram for apoptosis becomes activated, the cellcommits a form of molecular suicide. Its DNA disintegratesin a characteristic manner, blebs (smallpouches) form in the cell membrane, and the celldies. The genetic controls for apoptosis differ,depending on the cell type, but all involve activatingproteases called caspases, enzymes that destroy theprotein components of cells.As the body of an embryo develops, apoptosis helpsshape it. For example, apoptosis helps control thespacing of nerve cells in the brain and spinal cord; ithelps generate the space in the middle ear, and itcauses the death of skin cells between fingers andtoes—the typical “webbing” of fetal digits [19].Many of the genes that regulate apoptosis werediscovered in studies of the microscopic roundworm,C. elegans. The mammalian counterparts of thesegenes are very similar in terms of their DNAsequences, and are called homologues. For example,in C. elegans, the ced-4 and ced-3 genes areactivated (in that order) prior to apoptosis. They, inturn, activate enzymes called caspases, whichactually trigger apoptosis. But the regulatory pathwaythat leads to cell death is complex. Anotherapoptosis-control gene called ced-9 can blockactivation of ced-4 and ced-3, and thereby “rescue”a cell from apoptosis. The mammalian homologuesof ced-9 are members of the BCL-2 gene family,which prevent apoptosis in mammalian cells—and in C. elegans, if they are introduced into cellsfrom the worm [19].Another mammalian apoptosis gene, Apaf-1 workswith caspase-9 to bring about cell death. It is interestingto note that the silencing of the Apaf-1 gene—rather than a mutation in its DNA sequence—wasrecently linked to cancer metastasis [43]. In fact,several of the genes that normally regulate apoptosisinhibit the formation of tumors because they triggerthe death of cells with damaged DNA that mightotherwise replicate to produce a tumor. Because oftheir normal, protective function against the developmentof cancer, such genes are termed tumorsuppressorgenes. Many tumor-suppressor genes,including Apaf-1, are associated with the so-calledp53 tumor-suppressor pathway. If even one of theapoptosis-regulating genes becomes mutated, thetumor-suppressor pathway can fail, a step toward thedevelopment of cancer.SOME COMPARISONS BETWEENEMBRYOGENESIS AND ONCOGENESISThere are many molecular links between the regulationof normal embryogenesis and the induction ofcancer, which is called oncogenesis. A comprehensivereview of the similarities between the twoexceeds the scope of this report. However, it is usefulto point out that at least some of the genes, factors,and cell-cell interactions critical for normal embryonicdevelopment also play a role in—or are alteredin—tumor development. The example cited aboveA-14
Appendix A: Early Developmentindicates that some of the genes that function duringapoptosis in the embryo also protect the matureorganism from developing tumors.A different, and obvious, parallel between embryogenesisand oncogenesis can be observed in thespontaneous formation of tumors in the gonads ofmammals, including humans. These unusual tumors,which include teratomas, embryonal carcinomas,and teratocarcinomas, develop from the germ cellsin the testes or ovaries. The tumors have provoked agreat deal of interest because they often containhighly differentiated cells and tissues such as teeth,hair, neural cells, and epithelial cells. The structuresare disorganized, but often recognizable [2].Although teratomas are benign, embryonal carcinomasand teratocarcinomas are highly malignant. Thelatter contain a kind of stem cell, called an embryonalcarcinoma (EC) cell, which in mice and humansresembles embryonic stem (ES) cells. Human EC cells,unlike ES cells, typically have abnormal chromosomes.The chromosomes in mouse EC cells mayappear to be normal, although they carry geneticdefects. Nevertheless, mouse EC cells can contributeto normal embryonic development if they are introducedinto a mouse blastocyst, which is thenimplanted in the uterus of a pseudopregnant female[2] (see Table A.1. Comparison of Mouse, Monkey,and Human ES, EG, and EC <strong>Cells</strong>).Other genes recently identified as important in thedevelopment of human cancers are also activeduring embryonic development. For instance, thehuman breast cancer genes, BRCA1 and BRCA2,and their counterparts in mice are expressed in thethree primary germ layers during embryogenesis,particularly in cell types undergoing the most rapidproliferation. The expression of these genes isdependent on the stage of the cell cycle, with peakexpression during the G1/S transition and lowestexpression in cells in the G1 or G0 phase. In mouseand nonhuman primate (cynomolgus monkey)embryos, the temporal and spatial patterns of Brca1and Brca2 expression are virtually identical, despitethe fact that the coding sequences for the genesand their promoters differ between the species. Inhumans, BRCA1 and BRCA2 probably function duringthe development of mammary epithelium, althoughlittle is known about their role in this process. Mutantforms of the genes appear to cause breast canceronly if the mutations occur in the germ line. Somaticmutations of BRCA1 and BRCA2 are not linked tobreast cancer [8].DNA METHYLATION AND GENOMICIMPRINTING AFFECT EMBRYONICDEVELOPMENTDNA methylation is the process of adding methylgroups to specific cytosine residues in the promoterregions of DNA. DNA methylation is a genome-widephenomenon; it occurs in many genes dependingon the stage of development and the differentiationstatus of a cell. When the methyl groups are boundat their designated sites in DNA, transcription factorscannot bind to the DNA and gene transcription isturned off. Also, DNA methylation causes a rearrangementof the structure of chromatin, the combinationof DNA and protein that forms the chromosomes.DNA methylation patterns change during development,and their rearrangement in different tissues atdifferent times is an important method for controllinggene expression [19].Also important to embryonic development is theprocess of genomic imprinting, which causes certainto be genes turned on or off, depending on whetherthey are inherited from the mother or the father.Several mechanisms of genomic imprinting exist inmammals. A common method of imprinting is DNAmethylation. Once methylated, or “marked,” a genemay be activated or inactivated. Thus, the process ofmarking a gene as being inherited from either thefather or the mother is genomic imprinting [19].For most of the genes known to undergo imprinting,specific regulatory regions have been identifiedwhere methylation takes place. The methylationmarks are acquired during gametogenesis, theprocess of sperm and egg formation, and theypersist during the development of the pre- and postimplantationembryo [9, 44]. In contrast, the genesof nonimprinted embryos acquire their methylationpatterns after blastocyst implantation, as do EScells in vitro [50].The genomes of germ cells and the zygote are largelydemethylated, although the sites associated withparental-specific imprints remain methylated. In thepreimplantation blastocyst, the nonimprinted genesof undifferentiated cells remain demethylated, whichA-15
Appendix A: Early DevelopmentTable A.1. Comparison of Mouse, Monkey, and Human Pluripotent <strong>Stem</strong> <strong>Cells</strong>MarkerNameMouse EC/ES/EG cellsMonkeyES cellsHumanES cellsHumanEG cellsHumanEC cellsSSEA-1 + – – + –SSEA-3 – + + + +SEA-4 – + + + +TRA-1-60 – + + + +TRA-1-81 – + + + +Alkalinephosphatase+ + + + +Oct-4 + + + Unknown +Telomerase activity + ES, EC Unknown + Unknown +Feeder-celldependentES, EG,some ECYes Yes Yes Some; relatively lowclonal efficiencyFactors which aidin stem cellself-renewalLIF and otherfactors that actthrough gp130receptor and cansubstitute forfeeder layerCo-culture withfeeder cells; otherpromoting factorshave not beenidentifiedFeeder cells +serum; feederlayer +serum-freemedium + bFGFLIF, bFGF,forskolinUnknown;low proliferativecapacityGrowthcharacteristicsin vitroForm tight,rounded,multi-layer clumps;can form EBsForm flat, looseaggregates;can form EBsForm flat, looseaggregates;can form EBsForm rounded,multi-layer clumps;can form EBsForm flat, looseaggregates;can form EBsTeratomaformation in vivoChimeraformation+ + + – ++ Unknown + – +KEYES cell =EG cell =EC cell =SSEA =Embryonic stem cellEmbryonic germ cellEmbryonal carcinoma cellStage-specific embryonic antigenTRA =LIF =bFGF =EB =Tumor rejection antigen-1Leukemia inhibitory factorBasic fibroblast growth factorEmbryoid bodiesmeans that most of their genes are capable of beingexpressed. But before gastrulation, as the three germlayers prepare to differentiate, the DNA of theembryo’s somatic cells becomes remethylated andgenes are selectively turned on or off. The only cellsthat escape this phenomenon are the primordialgerm cells (PGCs). They gradually remove theirgenomic imprinting marks, which exist in the form ofparentally specified DNA methylation patterns. Thisphenomenon of erasing the marks for genomicimprinting occurs as the PGCs migrate to thegonadal ridges, which in the mouse occurs on E13.5[23]. Then, as the germ cells mature, their genomesacquire new imprints due to the activity of a specificDNA methyltransferase, which adds methyl groupsto DNA [50].A-16
Appendix A: Early DevelopmentREFERENCES1. Alberts, B., Bray, D., Lewis, J., Raff, M., Roberts, K., andWatson, J.D. (1994). Molecular biology of the cell,(New York: Garland Publishing, Inc.).2. Andrews, P.W., Przyborski, S.A., and Thomson, J. (2001).Embryonal carcinoma cells as embryonic stem cells.Marshak, D.R., Gardner, D.K., and Gottlieb, D. eds. ColdSpring Harbor Laboratory Press, 231-266.3. Beddington, R.S. and Robertson, E.J. (1999). Axis developmentand early asymmetry in mammals. Cell. 96, 195-209.4. Bongso, A., personal communication.5. Brook, F.A. and Gardner, R.L. (1997). The origin and efficientderivation of embryonic stem cells in the mouse. Proc. Natl.Acad. Sci. U. S. A. 94, 5709-5712.6. Burdsal, C.A., Flannery, M.L., and Pedersen, R.A. (1998).FGF-2 alters the fate of mouse epiblast from ectoderm tomesoderm in vitro. Dev. Biol. 198, 231-244.7. Carayannopoulos, M.O., Chi, M.M., Cui, Y., Pingsterhaus,J.M., McKnight, R.A., Mueckler, M., Devaskar, S.U., andMoley, K.H. (2000). GLUT8 is a glucose transporter responsiblefor insulin-stimulated glucose uptake in the blastocyst.Proc. Natl. Acad. Sci. U. S. A. 97, 7313-7318.8. Chodosh, L.A. (1998). Expression of BRCA1 and BRCA2 innormal and neoplastic cells. J. Mammary Gland Biol.Neoplasia. 3, 389-402.9. Constância, M., Pickard, B., Kelsey, G., and Reik, W. (1998).Imprinting mechanisms. Genome Res. 8, 881-900.10. Cronier, L., Bastide, B., Defamie, N., Niger, C., Pointis, G.,Gasc, J.M., and Malassine, A. (2001). Involvement of gapjunctional communication and connexin expression introphoblast differentiation of the human placenta. Histol.Histopathol. 16, 285-295.11. D’Urso, G. and Datta, S. (2001). Cell cycle control,checkpoints, and stem cell biology. Marshak, D.R., Gardner,D.K., and Gottlieb, D. eds. Cold Spring Harbor LaboratoryPress, 61-94.12. Edwards, R.G. (2000). The role of embryonic polarities inpreimplantation growth and implantation of mammalianembryos. Hum. Reprod. 15 Suppl 6, 1-8.13. Feldman, B., Poueymirou, W., Papaioannou, V.E., DeChiara,T.M., and Goldfarb, M. (1995). Requirement of FGF-4 forpostimplantation mouse development. Science. 267,246-249.14. Fong, C.Y., Bongso, A., Ng, S.C., Kumar, J., Trounson, A.,and Ratnam, S. (1998). Blastocyst transfer after enzymatictreatment of the zona pellucida: improving in-vitro fertilizationand understanding implantation. Hum. Reprod. 13,2926-2932.15. Gardner, R.L. (1997). The early blastocyst is bilaterallysymmetrical and its axis of symmetry is aligned with theanimal-vegetal axis of the zygote in the mouse.Development. 124, 289-301.16. Gardner, D.K. (1998). Changes in requirements andutilization of nutrients during mammalian preimplantationembryo development and their significance in embryoculture. Theriogenology. 49, 83-102.17. Gardner, R.L. (1999). Polarity in early mammalian development.Curr. Opin. Genet. Dev. 9, 417-421.18. Gardner, R.L. (2001). The initial phase of embryonicpatterning in mammals. Int. Rev. Cytol. 203, 233-290.19. Gilbert, S.F. (2000). Developmental biology. (Sunderland,MA: Sinauer Associates).20. Gossler, A. (1992). Early embryonic development ofanimals, Hennig, W., Nover, L., and Scheer, U. eds.(Berlin, New York: Springer-Verlag).21. Guillemot, F., Nagy, A., Auerbach, A., Rossant, J., andJoyner, A.L. (1994). Essential role of Mash-2 in extraembryonicdevelopment. Nature. 371, 333-336.22. Hara, T., Tamura, K., de Miguel, M.P., Mukouyama, Y., Kim,H., Kogo, H., Donovan, P.J., and Miyajima, A. (1998). Distinctroles of oncostatin M and leukemia inhibitory factor in thedevelopment of primordial germ cells and sertoli cells inmice. Dev. Biol. 201, 144-153.23. Hogan, B., Beddington, R., Constantini, F., and Lacy, E.(1994). Manipulating the mouse embryo a laboratorymanual, (Cold Spring Harbor, New York: Cold Spring HarborLaboratory Press).24. Hogan, B.L. (1999). Morphogenesis. Cell. 96, 225-233.25. Hogan, B. (2001). Primordial germ cells as stem cells.Marshak, D.R., Gardner, D.K., and Gottlieb, D. eds. ColdSpring Harbor Laboratory Press, 189-204.26. Janatpour, M.J., Utset, M.F., Cross, J.C., Rossant, J., Dong,J., Israel, M.A., and Fisher, S.J. (1999). A repertoire ofdifferentially expressed transcription factors that offersinsight into mechanisms of human cytotrophoblastdifferentiation. Dev. Genet. 25, 146-157.27. Johnson, M.H., Maro, B., and Takeichi, M. (1986). The roleof cell adhesion in the synchronization and orientation ofpolarization in 8-cell mouse blastomeres. J. Embryol. Exp.Morphol. 93, 239-255.28. Jones, J.M. and Thomson, J.A. (2000). Human embryonicstem cell technology. Semin. Reprod. Med. 18, 219-223.29. Kunath, T., Strumpf, D., Rossant, J., and Tanaka, S. (2001).Trophoblast stem cells. Marshak, D.R., Gardner, D.K., andGottlieb, D. eds. Cold Spring Harbor Laboratory Press, 267-288.30. Marshak, D.R., Gottlieb, D., Kiger, A.A., Fuller, M.T., Kunath, T.,Hogan, B., Gardner, R.L., Smith, A., Klar, A.J.S., Henrique, D.,D’Urso, G., Datta, S., Holliday, R., Astle, C.M., Chen, J., Harrison,D.E., Xie, T., Spradling, A., Andrews, P.W., Przyborski, S.A.,Thomson, J.A., Kunath, T., Strumpf, D., Rossant, J., Tanaka, S.,Orkin, S.H., Melchers, F., Rolink, A., Keller, G., Pittenger, M.F.,Marshak, D.R., Flake, A.W., Panicker, M.M., Rao, M., Watt, F.M.,Grompe, M., Finegold, M.J., Kritzik, M.R., Sarvetnick, N., andWinton, D.J. (2001e). <strong>Stem</strong> cell biology, Marshak, D.R.,Gardner, R.L., and Gottlieb, D. eds. (Cold Spring Harbor,New York: Cold Spring Harbor Laboratory Press).A-17
Appendix A: Early Development31. Nichols, J., Davidson, D., Taga, T., Yoshida, K., Chambers,I., and Smith, A. (1996). Complementary tissue-specificexpression of LIF and LIF-receptor mRNAs in early mouseembryogenesis. Mech. Dev. 57, 123-131.32. Nichols, J., Zevnik, B., Anastassiadis, K., Niwa, H., Klewe-Nebenius, D., Chambers, I., Scholer, H., and Smith, A.(1998). Formation of pluripotent stem cells in themammalian embryo depends on the POU transcriptionfactor Oct4. Cell. 95, 379-391.33. Niwa, H., Miyazaki, J., and Smith, A.G. (2000). Quantitativeexpression of Oct-3/4 defines differentiation, dedifferentiationor self-renewal of ES cells. Nat. Genet. 24, 372-376.34. Odorico, J.S., Kaufman, D.S., and Thomson, J.A. (2001).Multilineage Differentiation from Human Embryonic <strong>Stem</strong>Cell Lines. <strong>Stem</strong> <strong>Cells</strong>. 19, 193-204.35. Pelton, T.A., Bettess, M.D., Lake, J., Rathjen, J., and Rathjen,P.D. (1998). Developmental complexity of early mammalianpluripotent cell populations in vivo and in vitro. Reprod.Fertil. Dev. 10, 535-549.36. Pera, M.F., Reubinoff, B., and Trounson, A. (2000). Humanembryonic stem cells. J. Cell Sci. 113 ( Pt 1), 5-10.37. Pesce, M., Anastassiadis, K., and Scholer, H.R. (1999). Oct-4:lessons of totipotency from embryonic stem cells. <strong>Cells</strong>Tissues Organs. 165, 144-152.38. Rossant, J., personal communication.39. Shinohara, T., Orwig, K.E., Avarbock, M.R., and Brinster, R.L.(2000). Spermatogonial stem cell enrichment by multiparameterselection of mouse testis cells. Proc. Natl. Acad.Sci. U. S. A. 97, 8346-8351.40. Smith, A.G., Heath, J.K., Donaldson, D.D., Wong, G.G.,Moreau, J., Stahl, M., and Rogers, D. (1988). Inhibition ofpluripotential embryonic stem cell differentiation by purifiedpolypeptides. Nature. 336, 688-690.41. Smith, A. (2001). Embryonic stem cells. Marshak, D.R.,Gardner, D.K., and Gottlieb, D. eds. Cold Spring HarborLaboratory Press, 205-230.42. Smith, A.G. (2001). Origins and properties of mouseembryonic stem cells. Annu. Rev. Cell. Dev. Biol. 1-22.43. Soengas, M.S., Capodieci, P., Polsky, D., Mora, J., Esteller,M., Opitz-Araya, X., McCombie, R., Herman, J.G., Gerald,W.L., Lazebnik, Y.A., Cordon-Cardo, C., and Lowe, S.W.(2001). Inactivation of the apoptosis effector Apaf-1 inmalignant melanoma. Nature. 409, 207-211.44. Surani, M.A. (1998). Imprinting and the initiation of genesilencing in the germ line. Cell. 93, 309-312.45. Tanaka, M., Gertsenstein, M., Rossant, J., and Nagy, A.(1997). Mash2 acts cell autonomously in mouse spongiotrophoblastdevelopment. Dev. Biol. 190, 55-65.46. Tanaka, S., Kunath, T., Hadjantonakis, A.K., Nagy, A., andRossant, J. (1998). Promotion of trophoblast stem cellproliferation by FGF4. Science. 282, 2072-2075.47. Teruel, M., Smith, R., and Catalano, R. (2000). Growthfactors and embryo development. Biocell. 24, 107-122.48. Thomson, J.A., Itskovitz-Eldor, J., Shapiro, S.S., Waknitz, M.A.,Swiergiel, J.J., Marshall, V.S., and Jones, J.M. (1998).Embryonic stem cell lines derived from human blastocysts.Science. 282, 1145-1147.49. Trounson, A.O., Gardner, D.K., Baker, G., Barnes, F.L.,Bongso, A., Bourne, H., Calderon, I., Cohen, J., Dawson, K.,Eldar-Geve, T., Gardner, D.K., Graves, G., Healy, D., Lane,M., Leese, H.J., Leeton, J., Levron, J., Liu, D.Y., MacLachlan,V., Munné, S., Oranratnachai, A., Rogers, P., Rombauts, L.,Sakkas, D., Sathananthan, A.H., Schimmel, T., Shaw, J.,Trounson, A.O., Van Steirteghem, A., Willadsen, S., andWood, C. (2000). Handbook of in vitro fertilization, (BocaRaton, London, New York, Washington, D.C.: CRC Press).50. Tucker, K.L., Beard, C., Dausmann, J., Jackson-Grusby, L.,Laird, P.W., Lei, H., Li, E., and Jaenisch, R. (1996). Germ-linepassage is required for establishment of methylation andexpression patterns of imprinted but not of nonimprintedgenes. Genes Dev. 10, 1008-1020.A-18
APPENDIX B:MOUSE EMBRYONICSTEM CELLSMOUSE EMBRYONIC STEMCELL CULTURESThe techniques for culturing mouse embryonic stem(ES) cells from the inner cell mass of the preimplantationblastocyst were first reported 20 years ago [6,11], and versions of these standard procedures areused today in laboratories throughout the world.Additionally, studies of embryonal carcinoma (EC)cells from mice and humans [2, 30] have helpedestablish parameters for growing and assessing EScells. It is striking that, to date, only three species ofmammals have yielded long-term cultures of selfrenewingES cells: mice, monkeys, and humans [21,34, 35, 36] (see Figure B.1. Origins of MousePluripotent <strong>Stem</strong> <strong>Cells</strong>).In mice, the efficiency of generating ES cells is influencedby the genetic strain of laboratory mice andindividual factors that affect pregnant females. Onlya few strains of laboratory mice—notably 129,C57BL/6, and a hybrid strain—yield cultures of EScells. Even then, ES cells derived from C57BL/6 blastocystsdo not behave as reliably as do ES cells fromthe 129 strain of mice. The former are more difficultto propagate in vitro, generate chimeras less efficientlythan do ES cells from the 129 strain of mice,and infrequently contribute to the germ line [4].Another influence on the efficiency with which ES cellscan be cultured from mouse blastocysts is the pregnancystatus of the female. Pregnant mice that are indiapause tend to yield ES cells with greater success.Diapause occurs in female mice that have producedone litter and are still nursing when they becomepregnant again. Diapause is a naturally occurringdelay in the process of blastocyst implantation, whichcauses an arrest in embryonic development and asmall increase in the number of epiblast cells [28].These findings have led to the notion that geneticfactors that are peculiar to specific strains of inbredmice, and other in vivo influences such as diapause,determine, to a great extent, whether mouse ES cellscan be derived from a given blastocyst.Generating cultures of mouse or human ES cells thatremain in a proliferating, undifferentiated state is amultistep process that typically includes the following.First, the inner cell mass of a preimplantation blastocystis removed from the trophectoderm that surroundsit. (For cultures of human ES cells, blastocystsare generated by in vitro fertilization and donated forresearch.) The small plastic culture dishes used togrow the cells contain growth medium supplementedwith fetal calf serum, and are sometimes coated witha “feeder” layer of nondividing cells. The feeder cellsare often mouse embryonic fibroblast (MEF) cells thathave been chemically inactivated so they will notdivide. Mouse ES cells can be grown in vitro withoutfeeder layers if the cytokine leukemia inhibitory factor(LIF) is added to the culture medium (see below).Human ES cells, however do not respond to LIF.Second, after several days to a week, proliferatingcolonies of cells are removed and dispersed into newculture dishes, each of which also contains an MEFfeeder layer. Under these in vitro conditions, the EScells aggregate to form colonies. Some coloniesconsist of dividing, nondifferentiated cells; in othercolonies, cells may be differentiating. It is difficult tomaintain human ES cells in dispersed cultures wherecells do not aggregate, although mouse ES cells canbe cultured this way. Depending on the culture conditions,it may also be difficult to prevent the spontaneousdifferentiation of mouse or human ES cells.In the third major step required to generate ES celllines, the individual, nondifferentiating colonies aredissociated and replated into new dishes, a stepcalled passage. This replating process establishes a“line” of ES cells. The line of cells is “clonal” if a singleES cell generates it. Following some version of thisfundamental procedure, human and mouse ES cellscan be grown and passaged for two or more years,B-1
Appendix B: Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>Embryonic <strong>Stem</strong> <strong>Cells</strong> Embryonic Germ <strong>Cells</strong> Embryonic Carcinoma <strong>Cells</strong>InnercellmassMouseblastocystE10.5mouseembryoPrimordialgerm cellsTesticularteratocarcinomaTransfer ofstem cellsto mouseblastocystNormalblastocystNormalblastocystNormalblastocyst© 2001 Terese WinslowFigure B.1. Origins of Mouse Pluripotent <strong>Stem</strong> <strong>Cells</strong>.through hundreds of population doublings, and stillmaintain a normal complement of chromosomes,called a karyotype [31, 35].MAINTAINING MOUSE EMBRYONICSTEM CELLS IN THEIRUNDIFFERENTIATED STATELeukemia Inhibitory Factor and STAT3 ActivationMouse ES cells can be maintained in a proliferative,undifferentiated state in vitro by growing them onfeeder layers of MEF cells. An alternative to culture onfeeder layers is the addition of leukemia inhibitoryfactor (LIF) to the growth medium [31, 39]. LIF is producedby feeder cells and, in their absence, allowsmouse ES cells in vitro to continue proliferating withoutdifferentiating [20]. LIF exerts its effects by binding toa two-part receptor complex that consists of the LIFreceptor and the gp130 receptor. The binding of LIFtriggers the activation of the latent transcription factorSTAT3, a necessary event in vitro for the continuedproliferation of mouse ES cells [5, 12, 14]. RecentB-2
Appendix B: Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>evidence indicates that two transcription factors,STAT3 and Oct-4, may interact and perhaps affectthe function of a common set of target genes [15].In vivo, signaling through the gp130 receptor is notnecessary for normal, early embryonic developmentbut is required to maintain the epiblast duringdiapause. After gastrulation, LIF signaling and STAT3activation promote the differentiation of specific celllineages such as the myeloid cells of the hematopoieticsystem or the astrocyte precursor cells in thecentral nervous system [9].The self-renewal of mouse ES cells also appears tobe influenced by SHP-2 and ERK activity. SHP-2 is atyrosine phosphatase, an enzyme that removesphosphate groups to the tyrosine residues of variousproteins. SHP-2 interacts with the intracellular (aminoterminus) domain of the gp130 receptor. ERK (whichstands for extracellular regulated kinase) is one of severalkinds of enzymes that becomes activated whenthe gp130 receptor and other cell-surface receptorsare stimulated. Both ERK and SHP-2 are componentsof a signal-transduction pathway that counteracts theproliferative effects of STAT3 activation. Therefore, ifERK and SHP-2 are active, they inhibit ES cell selfrenewal[5] (see Figure B.2. The LIF-STAT3 SignalingPathway Promotes Embryonic <strong>Stem</strong> Cell Self-Renewal).It is possible that some of the components of signalingpathways in cultured mouse ES cells are uniqueto these cells. For example, mouse ES cells in vitroexpress high amounts of a modified version of anadapter protein, Gab1. The unusual form of Gab1that occurs in ES cells may suppress interactions ofspecific receptors to the Ras-ERK signaling pathway[31]. Further, the expression of this altered form ofGab1 may be promoted by the transcription factorOct-4. In mouse ES cells, Oct-4 expression andincreased synthesis of Gab1 may help suppressinduction of differentiation [30].Thus, the emerging picture is that the effects ofvarious signaling pathways must be balanced in aparticular way for ES cells to remain in a self-renewingstate. If the balance shifts, ES cells begin to differentiate[29, 30].Expression of Oct-4 in Undifferentiated,Pluripotent <strong>Cells</strong>One of the hallmarks of an undifferentiated, pluripotentcell is the expression of the Pou5f1 gene,which encodes the transcription factor Oct-4 (also© 2001 Terese Winslow, Lydia KibiukPlasmamembraneTranscriptionfactorSTAT3LIFRJAKSTATactivationSelf-RenewalSTAT3STAT3Embryonicstem cellsCell receptorsgp130BlastocystInner cellmassFigure B.2. The LIF-STAT3 Signaling Pathway PromotesEmbryonic <strong>Stem</strong> Cell Self-Renewal.called Oct-3 or Oct-3/4). Oct-4 is present in themouse zygote, and is required throughout blastocystdevelopment to establish [13] and maintain [15] thepluripotency of the inner cell mass and the epiblast.Oct-4 is also expressed in the primordial germ cells ofmice and in mature germ cells [19, 23, 26].Mouse ES cells in vitro can replicate indefinitely andproduce 10 9 to 10 10 (1 to 10 billion) cells withoutdifferentiating. In vitro, undifferentiated, proliferatingmouse [18] and human [21] ES cells express Oct-4.Studies of Oct-4 expression and function in humancells are incomplete, however, and most of theinformation about Oct-4 comes from the study ofmouse ES cells in vitro.JAKSHP2GabERKactivationSignalTransductionPathwayERK 1/2Blocks Self-RenewalB-3
Appendix B: Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>As is the case with inner cell mass and epiblast cellsin vivo, Oct-4 expression in vitro is required to maintainthe pluripotent, undifferentiated state of ES cells.If Oct-4 expression is inhibited in cultured mouse EScells, the cells generate trophectoderm. If Oct-4expression is artificially increased, mouse ES cells differentiateinto primitive endoderm and mesoderm.Therefore, the level of Oct-4 expression dictates asignificant aspect of the developmental program ofmouse ES cells, making the protein a candidate“master regulator” of ES cell pluripotency [15].How and why the Oct-4 transcription factor plays suchan important role in early embryogenesis depend onthe genes it regulates. Seven to eight target genes forOct-4 have been identified to date; it activates someand represses others. In fact, the overall impact ofOct-4 may be to prevent the expression of genes thatare required for differentiation [19].The Cell Cycle of Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>: ItsRole in Preventing DifferentiationLike the cells of the epiblast in the preimplantationmouse embryo, mouse ES cells in vitro have anunusual cell cycle. Specifically, the G1 checkpointdoes not appear to operate in proliferating epiblastand ES cells [25, 38]. This may explain why it has notbeen possible to induce quiescence—withdrawalfrom the cell cycle to a G1 or G0 state—inundifferentiated ES cells [29].However, if ES cells begin to differentiate by formingembryoid bodies, cyclin D expression increases, theG1 phase of the cell cycle becomes longer, and therate of cell division slows [25]. This can occur if LIF orfeeder layers are withdrawn from mouse ES cell cultures.Then, cell division continues for only a few daysas the process of differentiation begins [29]. Perhapsconstant cell proliferation somehow inhibits celldifferentiation, and once the signals for cell divisionare removed, differentiation can occur [37].Markers of Undifferentiated Embryonic <strong>Stem</strong> <strong>Cells</strong>ES and EC cells, as well as cells of the inner cell massof mouse blastocysts, express a panel of surfacemarkers that are used to characterize undifferentiated,pluripotent embryonic cells. (see Table B.1.Comparison of Mouse, Monkey, and HumanPluripotent <strong>Stem</strong> <strong>Cells</strong>). The markers also distinguishmouse ES and EC cells from human ES and EC cells.For example mouse ES and EC cells express thestage-specific embryonic antigen SSEA-1, whereashuman ES and EC cells do not. But human ES and ECcells express SSEA-3 and SSEA-4, whereas mouse ESand EC cells do not [21, 35].Human EG cells, which are derived from primordialgerm cells, express all three markers: SSEA-1, SSEA-3,and SSEA-4. The biological significance of the expressionpatterns of these surface antigens is unclear, butSSEA-1 expression may be related to the growth characteristicof the cells in vitro. Undifferentiated humanES and EC cells tend to grow in flat, relatively loosecolonies. In contrast, mouse ES and EC colonies tendto be multilayered and compact [27]. Alternatively, thesurface expression of various SSEAs may reflect a differencein the developmental stages of the cells [17].Other markers used to identify ES cells are the surfaceantigens TRA1-60, TRA1-81, and the enzyme alkalinephosphatase. All occur in human ES [3, 27, 35], asthey do in their mouse counterparts.Genomic Imprinting in Embryonic <strong>Stem</strong> <strong>Cells</strong>It is known that if genomic imprinting patterns aredisturbed before blastocyst implantation in vivo, fetalabnormalities may result. In genomic imprinting,DNA methylation marks certain genes, depending onwhether they are inherited from the mother or thefather. The marked genes are turned on or off in anon-random pattern that is determined by parentalorigin. Imprinting marks are erased in the primordialgerm cells and then reestablished during theformation of eggs and sperm.However, when embryonic development occursin vitro or when ES cells are grown in tissue culture,normal patterns of genomic imprinting may bedisturbed. For example, mouse embryos that weregrown in vitro in the presence of fetal calf serum—a very different environment than the oviduct—andthen allowed to develop in vivo, showed abnormalgenomic imprinting patterns and abnormal development.Apparently, the presence of fetal calf serum,a common ingredient in mouse and human EScultures, decreases the expression of certainimprinted genes [8].How or whether the use of fetal calf serum forculturing mouse or human ES cells affects genomicimprinting and the behavior of ES cells in vitro is notknown. But for mouse ES cells, the parental imprintingpattern apparently persists in vitro [16, 22]. Theimprinting pattern of human ES cells in vitro has notyet been determined.B-4
Appendix B: Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>Table B.1. Comparison of Mouse, Monkey, and Human Pluripotent <strong>Stem</strong> <strong>Cells</strong>MarkerNameMouse EC/ES/EG cellsMonkeyES cellsHumanES cellsHumanEG cellsHumanEC cellsSSEA-1 + – – + –SSEA-3 – + + + +SEA-4 – + + + +TRA-1-60 – + + + +TRA-1-81 – + + + +Alkalinephosphatase+ + + + +Oct-4 + + + Unknown +Telomerase activity + ES, EC Unknown + Unknown +Feeder-celldependentES, EG,some ECYes Yes Yes Some; relatively lowclonal efficiencyFactors which aidin stem cellself-renewalLIF and otherfactors that actthrough gp130receptor and cansubstitute forfeeder layerCo-culture withfeeder cells; otherpromoting factorshave not beenidentifiedFeeder cells +serum; feederlayer +serum-freemedium + bFGFLIF, bFGF,forskolinUnknown;low proliferativecapacityGrowthcharacteristicsin vitroForm tight,rounded,multi-layer clumps;can form EBsForm flat, looseaggregates;can form EBsForm flat, looseaggregates;can form EBsForm rounded,multi-layer clumps;can form EBsForm flat, looseaggregates;can form EBsTeratomaformation in vivoChimeraformation+ + + – ++ Unknown + – +KEYES cell =Embryonic stem cellTRA =Tumor rejection antigen-1EG cell =Embryonic germ cellLIF =Leukemia inhibitory factorEC cell =Embryonal carcinoma cellbFGF =Basic fibroblast growth factorSSEA =Stage-specific embryonic antigenEB =Embryoid bodiesTargeted Differentiation of Mouse Embryonic<strong>Stem</strong> <strong>Cells</strong>.Outlined here are three different ways to directmouse ES cell differentiation in vitro. In the first example,mouse ES cells are directed to generate primitiveblood vessels. In the second, mouse ES cells aredirected to become neurons that release the transmittersdopamine and serotonin. And in the third—a series of experiments conducted by the same labgroup that generated dopamine neurons—verysimilar conditions are used to direct the differentiationof mouse ES cells to yield pancreatic islet cells thatsecrete insulin.Making Vascular Progenitors from Mouse Embryonic<strong>Stem</strong> <strong>Cells</strong>In the mouse embryo, blood cells and blood vesselsare formed at roughly the same time, when bloodislands first appear in the wall of the yolk sac. A prevailingidea is that blood cells and blood vessels ariseB-5
Appendix B: Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>from a common precursor cell derived frommesoderm, the hemangioblast. After hemangioblastsdifferentiate from the mesoderm, they aggregate toform blood islands. The inner cells of the blood islandsbecome hematopoietic stem cells, or blood-formingcells. The outer cells of the blood islands becomeangioblasts, which give rise to the blood vessels.A recent study showed that mouse ES cells in vitrocould be induced to follow this in vivo developmentalpathway.In vivo, blood vessel formation occurs in two ways:by vasculogenesis and angiogenesis. Vasculogenesishelps establish the blood islands and the capillarynetwork that connects them. During angiogenesis,new blood vessels form by remodeling or adding toexisting vessels. Both vasculogenesis and angiogenesisare regulated by the actions of a series ofparacrine growth factors, which include fibroblastgrowth factor–2 (FGF-2), vascular endothelial growthfactor (VEGF), and later (in the adult) platelet-derivedgrowth factor (PDGF) and transforming growth factorbeta (TGFß). Each of these growth factors binds tospecific receptors. VEGF, for instance, binds to twodifferent receptors: VEGF-R1, also known as Flt1, andVEGF-R2, also known as Flk1 [7].To make vascular progenitors from mouse ES cells,Shin-Ichi Nishikawa of Kyoto University GraduateSchool of Medicine in Japan and his colleagues triedto mimic this in vivo pathway for blood vessel formation[40]. They grew undifferentiated ES cells oncollagen-coated dishes in medium containing fetalcalf serum but no leukemia inhibitory factor (LIF). Thisinduced the generation of cells that express Flk1, areceptor for VEGF. Several days later, the cells beganto differentiate. Nearly all the mouse ES cellsexpressed -smooth muscle actin (SMA), a marker formural cells. (Mural cells, which include pericytes andsmooth muscle cells, normally interact in vivo withendothelial cells to make blood vessels.) When VEGFwas added to the culture medium, sheets ofendothelial cells formed that expressed plateletendothelialcell adhesion molecule (PECAM1) andother endothelial cell markers. At this point, the culturecontained two differentiating cell types, endothelialcells and mural cells.Therefore, it appeared that the mouse ES cells haddifferentiated into Flk1 + precursor cells, which thengave rise to both mural cells and endothelial cellsin vitro. To test that hypothesis, single Flk1 + cells werecultured. The individual ES cells generated three kindsof colonies: pure mural cells (SMA + ), pure endothelialcells (PECAM1 + ), and mixed mural and endothelialcells. That result indicated that ES cells can give riseto Flk1 + cells that are precursors for both mural andendothelial cells.The next test was to see whether the mural cells andendothelial cells generated from Flk1 + precursorscould assemble into primitive blood vessels in vitro.They did. By growing hundreds of Flk1 + cells in collagengel suspensions with fetal calf serum and VEGF,tube-like structures formed within three to five days.This change in the culture conditions allowed the EScells to grow in suspension and interact with eachother. As a result, the cells spontaneously organizedthemselves into tube-like structures that resembleblood vessels in vivo. The tubes were composed ofendothelial (PECAM1 + ) cells and mural (SMA + ) cells.Occasionally, they formed branching structures,which is typical of the organization of blood vesselsin vivo. Also, blood cells (bearing the markers CD45and Ter119) formed inside the tubes, which alsomimicked the organization of blood islands in theearly embryo in vivo.The final test was to see whether the Flk1 + cells generatedfrom mouse ES cells in vitro would differentiateinto endothelial cells and mural cells in vivo. Again,they did. Flk1 + cells were engineered to express LacZ(which allows the cells to be tracked visually) andinjected into the developing hearts of stage 16-17chick embryos. The donor mouse cells populatedblood vessels in the chicks’ head, yolk sac, heart, andregions between the somites, forming endothelialcells and mural cells in those regions.Thus, undifferentiated mouse ES cells can bedirected to differentiate into Flk1 + precursors thatgive rise to endothelial cells and mural cells in vitroand in vivo. Further, the differentiated cells can formtube-like vascular structures in vitro. The experimentsnot only demonstrate the power of directed differentiationof ES cells into individual cell types, they alsoshow that ES cells can generate multiple cell typesthat then spontaneously organize themselves intotissues that resemble those in vivo. In addition, theexperiments by Nishikawa and his co-workers [40]reveal that Flk1 + cells are important for generatingblood vessels in vivo.B-6
Appendix B: Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>Making Dopamine Neurons from MouseEmbryonic <strong>Stem</strong> <strong>Cells</strong>A second example of the directed differentiation ofmouse ES cells in vitro yielded the formation ofparticular kinds of neurons that normally occur in themammalian midbrain and hindbrain. For a long time,the goal of efficiently inducing the formation of theseneurons—which release the neurotransmittersdopamine and serotonin, respectively— was highlydesired, but elusive. In Parkinson’s Disease, a keypopulation of midbrain neurons that releasesdopamine dies. So finding a way to grow largequantities of nerve cells in vitro that might be ableto replace lost dopamine neurons in vivo is a clinicalpriority (see Chapter 8. Rebuilding the Nervous Systemwith <strong>Stem</strong> <strong>Cells</strong>).Last year, Ron McKay and his colleagues reported anefficient technique for inducing mouse ES cells in vitroto differentiate into dopamine neurons of the midbrainand serotonin neurons, which normally populatethe hindbrain. Like Nishikawa and his colleagues [40],McKay and his collaborators [10] triggered the differentiationof mouse ES cells in vitro at various stagesby changing the growth conditions to mimic, in part,those that occur during embryogenesis in vivo. Theresulting differentiated nerve cells look and functionlike their in vivo counterparts.During embryogenesis, central nervous system (CNS)development is a long, complex process thatdepends on a highly coordinated series of cellularand molecular events. Different signals direct theformation of the neurectoderm from the epiblast, aprocess that ultimately results in the formation of theCNS, the brain and spinal cord. Later, other signalsregulate the development of different parts of thebrain. For example, early in the formation of thebrain, the homeobox genes OTX1 and OTX2 areexpressed [28]. <strong>Cells</strong> of the epiblast express OTX2before the onset of gastrulation. Then, during gastrulation,OTX2 is expressed in the anterior neurectoderm,where it is necessary for the formation of themidbrain and forebrain. Meanwhile, OTX1 expressionoccurs in the region of the neurectoderm that givesrise to the dorsal forebrain. Interactions between OTX1and OTX2 are thought to help shape the midbrainand hindbrain [1].Once these major brain structures form, variousgenes control the development of individual nervecell types. For example, the genes Pax2, Pax5, Wnt1,En1, and Nurr1 help control the differentiation ofneurons that release the transmitters dopamine andserotonin [24, 33]. Furthermore, when the proteinssonic hedgehog (SHH) and fibroblast growth factor-8(FGF-8) are added to explant cultures (small chunksof tissue maintained in vitro) of neural plate, thedevelopment of midbrain neurons is enhanced [41].Taking into account these and other findings, McKayand his coworkers devised an in vitro system forcontrolling the differentiation of mouse ES cells intomidbrain neurons that release dopamine and hindbrainneurons that release serotonin [11]. The cultureconditions they used differ from those devised byNishikawa and his colleagues (described above), butthe starting material—undifferentiated, proliferatingmouse ES cells—was the same in both experiments.McKay and his colleagues cultured mouse ES cells infive distinct stages, each of which they identified bythe changes in culture conditions and the behaviorof the cells (see Figure B.3. Directed Differentiation ofMouse Embryonic <strong>Stem</strong> <strong>Cells</strong> Into Neurons orPancreatic Islet-Like Clusters).In stage 1, undifferentiated mouse ES cells were dissociatedinto single cells and plated at low density.They proliferated in plastic culture dishes coated withgelatin. The growth media contained LIF and fetalcalf serum and was supplemented with amino acids,conditions that promoted the proliferation of undifferentiatedES cells. In stage 2, the cells were inducedto form embryoid bodies by dissociating them andreplating at a higher density on a nonadherent surface.These conditions allowed the cells to aggregateand begin the process of differentiation. Afterfour days, the cells were replated on an adherentsubstrate in the original (stage 1) growth medium.Twenty-four hours later, the growth medium wasreplaced with serum-free insulin/transferrin/selenium/fibronectin (ITSFn) medium. This switch to a serum-freemedium (one lacking fetal calf serum) caused manycells to die but allowed the survival of cells thatexpress nestin. This intermediate filament protein isused as a marker to identify CNS stem cells in vivoand in vitro, although it is also expressed by other celltypes. Stage 1 neurons expressed high levels of OXT2,which decreased in stages 2 and 3. OXT1 was notexpressed until the cells reached stage 3.Guiding the mouse ES cells through stages 4 and 5of in vitro development yielded fully differentiateddopaminergic and serotoninergic neurons. After 6 toB-7
Appendix B: Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>Inner cellmass ofblastocystUndifferentiatedembryonic stem cellsEMBRYOID BODIESITFSn medium (insulin/transferrin/fibronectin/selenium)Adherent substrateSELECTION OF NESTIN-POSITIVE CELLSN2 medium/bFGF/lamininN2 medium/bFGF/B27 media supplementNESTIN-POSITIVE NEURONALPRECURSOR CELLSExpansionPhaseNESTIN-POSITIVE PANCREATICPROGENITOR CELLSRemove bFGFDifferentiationPhaseRemove bFGFAdd nicotinamideDOPAMINE- AND SEROTONIN-SECRETING NEURONSTYROSINE HYDROXYLASE/SEROTONININSULIN-SECRETING PANCREATICISLET-LIKE CLUSTERSINSULIN/GLUCAGON© 2001 Terese Winslow, Caitlin DuckwallReproduced with permissionfrom Nature BiotechnologyReproduced with permissionfrom ScienceFigure B.3. Directed Differentiation of Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong> Into Neurons or Pancreatic Islet-Like Clusters.B-8
Appendix B: Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>10 days in the medium that selects for cells thatexpress nestin, the cells were dissociated andinduced to divide in another medium, N2, supplementedwith laminin and basic FGF, a growth factorthat induces proliferation. Other critical additives toyield stage 4 cells were SHH and FGF-8. <strong>Cells</strong> atstages 3 and 4 express genes that, in vivo, trigger thedevelopment of dopaminergic and serotinergicneurons—namely, Pax2, Pax5, Wnt1, En1, and Nurr1.Stage 5, the final stage of differentiation, wasachieved by removing basic FGF from the growthmedium (which made the cells stop dividing) andgrowing the cells for 6 to 15 days in N2 mediumsupplemented with laminin and ascorbic acid, acombination of additives that induces the differentiationof serotonin neurons.This complex, multistage differentiation process yieldeda higher percentage (30 percent) of neurons thatexpress tyrosine hydroxylase (TH, the rate-limitingenzyme in the synthesis of dopamine) than any otherreported in vivo or in vitro technique. The cells wereconfirmed to be true dopamine neurons by severalfunctional assays. The neurons secreted dopamineinto the culture medium, showed the electricalactivity typical of neurons, and responded to theaddition of a high concentration of potassium ions(via the addition of potassium chloride) by releasingmore dopamine, much as they would in vivo. A separatepopulation of neurons in the mouse ES cell culturesstained positive for serotonin. The differentiationof serotoninergic neurons could be induced by addingonly SHH to the culture medium; addition of FGF-8was not required. Thus, mouse ES cells in vitro can bedirected to differentiate at a high efficiency intoneurons that release either dopamine or serotonin.Making Pancreatic Islet <strong>Cells</strong> from MouseEmbryonic <strong>Stem</strong> <strong>Cells</strong>The experimental strategy is similar to that describedabove [10] and is based on a five-stage, in vitrosystem. As before (to differentiate neurons that producedopamine), undifferentiated mouse ES cells areinduced to proliferate in LIF-supplemented medium(stage 1). Then, the cells are induced to form embryoidbodies (EBs) in serum-free ITSFn medium withoutLIF (stage 2). ES stage 1 cells expressed Oct-4, a transcriptionfactor that characterizes undifferentiated,proliferating, pluripotent cells. Again, cells that expressnestin survive in serum-free medium, whereas othercell types do not, thus creating an environment that“selects” for nestin-positive cells (stage 3). As before,cells that express nestin are expanded by adding themitogen basic FGF to the serum-free medium (stage4). When basic FGF is withdrawn, the cells stopdividing and begin their final stages of differentiation.It is at this point that the techniques for generatingneurons that release dopamine and pancreatic isletcells that release insulin diverge.To generate neurons that release dopamine, ESderivedcells were cultured in medium that containedSHH and FGF-8 and later, an N2 medium supplementedwith laminin and ascorbic acid [10]. Togenerate pancreatic islet cells, however, B27 culturemedium was used for stage 4, and nicotinamide wasadded to stage 5 cultures. Another change in thepancreatic islet culture system was to co-cultureindividual stage 4 or 5 ES cells, which were taggedwith the marker green fluorescent protein (GFP), withnontagged ES cells. This meant that an individual,tagged ES cell could be followed so its developmentalfate could be traced, a technique that madepossible the clonal analysis of the labeled ES cell andits progeny. Tagged, GFP-expressing ES cells gave riseto both pancreatic islet cells and neurons, indicatingthat the same cell acted as the precursor for bothdifferentiated cell types (see Figure B.3. DirectedDifferentiation of Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong> IntoNeurons or Pancreatic Islet-Like Clusters).The tests that identified the differentiated cells typesas pancreatic islet cells and neurons included assaysof various markers. The ES cells at stages 1 and 5expressed GATA-4 and HNFb, markers for embryonicendoderm and extra-embryonic endoderm. This indicatesthat endodermal markers are present in undifferentiatedES cells. But stage 5 cells express additionalmarkers that are characteristic of endocrine pancreaticislet cells: mouse insulin I and II, islet amyloidpolypeptide, and the glucose transporter GLUT-2.Other cells stained positive for glucagon, a hormoneproduced by the alpha cells of the pancreas, andsomatostatin, a peptide hormone produced by pancreaticendocrine cells in vivo. Nerve cells that surroundedthe clusters of islet cells—a spontaneouslyforming, in vitro arrangement of cell types that mimickedtheir arrangement in vivo—stained positive forneuron-specific tubulin. No cells stained positive forboth pancreatic islet markers and neuronal markers,indicating that the two cell types had differentiatedcompletely from a common precursor cell.B-9
Appendix B: Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>Other tests demonstrated the functional properties ofthe pancreatic islet cells differentiated from mouseES cells. Adding glucose to the culture mediumtriggered the release of insulin in a dose-dependentmanner. Agonists and antagonists of insulin releasein vivo stimulated or blocked insulin release in vitro,indicating that the pharmacological responses of theES-derived islet cells in vitro mirrored in vivo responses.Finally, when cell clusters of the cultured pancreaticislets were grafted under the skin of diabetic mice(whose diabetes was induced by treatment withstreptozocin), the grafts survived and became infiltratedwith blood vessels. The ES-derived pancreaticislets released only one-fiftieth the amount of insulinthey released as islet cells in vivo, however, thediabetic mice experienced no correction of theirhyperglycemia (see Chapter 7. <strong>Stem</strong> <strong>Cells</strong> andDiabetes; and Figure 7.2. Development of InsulinSecreting Pancreatic-Like <strong>Cells</strong> from MouseEmbryonic <strong>Stem</strong> <strong>Cells</strong>).Taken together, the three studies show that the differentiationof lines of mouse ES cells can be directedin vitro to yield vascular structures [40], neurons thatrelease dopamine and serotonin [10], and endocrinepancreatic islet cells. In all three cases, proliferating,undifferentiated mouse ES cells provided the startingmaterial and functional, differentiated cells were theresult. Also, in all three experiments, the onset ofmouse ES cell differentiation was triggered by withdrawingthe cytokine LIF, which promotes the divisionof undifferentiated mouse ES cells, but — inexplicably— does not have the same effect on human ES cells.In addition, the ES cells in all three examples citedwere induced to aggregate, a change in theirthree-dimensional environment that presumablyallowed some of the cell-cell interactions to occur invitro that would occur in vivo during normal embryonicdevelopment.Collectively, these three studies provide some of thebest examples of directed differentiation of mouseES cells in vitro. Two of them showed that a single precursorcell can give rise to multiple, differentiated celltypes[10, 40], and all of three studies demonstratedthat the resulting differentiated cells function as theirin vivo counterparts do.These two criteria – demonstrating that a single cellcan give rise to multiple cells types (clonal analysis),and that the functional properties of the differentiatedcells – form the basis of an acid test for all claims ofdirected differentiation of either ES cells or of adultstem cells. Unfortunately, very few experiments meetthese criteria, which too often makes it impossible toassess whether a differentiated cell type resulted fromthe experimental manipulation that was reported.REFERENCES1. Acampora, D. and Simeone, A. (1999). The TINS Lecture.Understanding the roles of Otx1 and Otx2 in the control ofbrain morphogenesis. Trends. Neurosci. 22, 116-122.2. Andrews, P.W., Casper, J., Damjanov, I., Duggan-Keen, M.,Giwercman, A., Hata, J., von Keitz, A., Looijenga, L.H.,Millan, J.L., Oosterhuis, J.W., Pera, M., Sawada, M., Schmoll,H.J., Skakkebaek, N.E., van Putten, W., and Stern, P. (1996).Comparative analysis of cell surface antigens expressed bycell lines derived from human germ cell tumours. Int. J.Cancer. 66, 806-816.3. Andrews, P.W., Damjanov, I., Simon, D., Banting, G.S., Carlin,C., Dracopoli, N.C., and Fogh, J. (1984). Pluripotentembryonal carcinoma clones derived from the humanteratocarcinoma cell line Tera-2. Differentiation in vivo andin vitro. Lab. Invest. 50, 147-162.4. Brook, F.A. and Gardner, R.L. (1997). The origin and efficientderivation of embryonic stem cells in the mouse. Proc. Natl.Acad. Sci. U. S. A. 94, 5709-5712.5. Burdon, T., Chambers, I., Stracey, C., Niwa, H., and Smith,A. (1999). Signaling mechanisms regulating self-renewaland differentiation of pluripotent embryonic stem cells.<strong>Cells</strong> Tissues Organs. 165, 131-143.6. Evans, M.J. and Kaufman, M.H. (1981). Establishment inculture of pluripotential cells from mouse embryos. Nature.292, 154-156.7. Gilbert, S.F. (2000). Developmental biology. (Sunderland,MA: Sinauer Associates).8. Khosla, S., Dean, W., Brown, D., Reik, W., and Feil, R. (2001).Culture of preimplantation mouse embryos affects fetaldevelopment and the expression of imprinted genes. Biol.Reprod. 64, 918-926.9. Kishimoto, T., Taga, T., and Akira, S. (1994). Cytokine signaltransduction. Cell. 76, 253-262.10. Lee, S.H., Lumelsky, N., Studer, L., Auerbach, J.M., andMcKay, R.D. (2000). Efficient generation of midbrain andhindbrain neurons from mouse embryonic stem cells. Nat.Biotechnol. 18, 675-679.11. Martin, G.R. (1981). Isolation of a pluripotent cell line fromearly mouse embryos cultured in medium conditioned byteratocarcinoma stem cells. Proc. Natl. Acad. Sci. U. S. A.78, 7634-7638.12. Matsuda, T., Nakamura, T., Nakao, K., Arai, T., Katsuki, M.,Heike, T., and Yokota, T. (1999). STAT3 activation is sufficientto maintain an undifferentiated state of mouse embryonicstem cells. EMBO J. 18, 4261-4269.B-10
Appendix B: Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>13. Nichols, J., Zevnik, B., Anastassiadis, K., Niwa, H., Klewe-Nebenius, D., Chambers, I., Scholer, H., and Smith, A.(1998). Formation of pluripotent stem cells in themammalian embryo depends on the POU transcriptionfactor Oct4. Cell. 95, 379-391.14. Niwa, H., Burdon, T., Chambers, I., and Smith, A. (1998).Self-renewal of pluripotent embryonic stem cells is mediatedvia activation of STAT3. Genes Dev. 12, 2048-2060.15. Niwa, H., Miyazaki, J., and Smith, A.G. (2000). Quantitativeexpression of Oct-3/4 defines differentiation, dedifferentiationor self-renewal of ES cells. Nat. Genet. 24, 372-376.16. O’Shea, K.S. (1999). Embryonic stem cell models ofdevelopment. Anat. Rec. 257, 32-41.17. Pera, M., personal communication.18. Pesce, M., Gross, M.K., and Scholer, H.R. (1998). In line withour ancestors: Oct-4 and the mammalian germ. Bioessays.20, 722-732.19. Pesce, M., Wang, X., Wolgemuth, D.J., and Scholer, H.(1998). Differential expression of the Oct-4 transcriptionfactor during mouse germ cell differentiation. Mech. Dev.71, 89-98.20. Rathjen, P.D., Toth, S., Willis, A., Heath, J.K., and Smith, A.G.(1990). Differentiation inhibiting activity is produced inmatrix-associated and diffusible forms that are generatedby alternate promoter usage. Cell. 62, 1105-1114.21. Reubinoff, B.E., Pera, M.F., Fong, C.Y., Trounson, A., andBongso, A. (2000). Embryonic stem cell lines from humanblastocysts: somatic differentiation in vitro. Nat. Biotechnol.18, 399-404.22. Rohwedel, j., Sehlmeyer, U., Shan, J., Meister, A., andWobus, A.M. (1996). Primordial germ cell-derived mouseembryonic germ (EG) cells in vitro resemble undifferentiatedstem cells with respect to differentiation capacityand cell cycle distribution. Cell. Biol. Int. 20, 279-587.23. Rosner, J.L. (1990). Reflections of science as a product.Nature. 345, 108.24. Rowitch, D.H. and McMahon, A.P. (1995). Pax-2 expressionin the murine neural plate precedes and encompasses theexpression domains of Wnt-1 and En-1. Mech. Dev. 52, 3-8.25. Savatier, P., Lapillonne, H., van Grunsven, L.A., Rudkin, B.B.,and Samarut, J. (1996). Withdrawal of differentiationinhibitory activity/leukemia inhibitory factor up-regulatesD-type cyclins and cyclin-dependent kinase inhibitors inmouse embryonic stem cells. Oncogene. 12, 309-322.26. Schöler, H.R., Ruppert, S., Suzuki, N., Chowdhury, K., andGruss, P. (1990). New type of POU domain in germ linespecificprotein Oct-4. Nature. 344, 435-439.28. Simeone, A. (1998). Otx1 and Otx2 in the developmentand evolution of the mammalian brain. EMBO J. 17,6790-6798.29. Smith, A.G. (2001). Embryonic stem cells. Marshak, D.R.,Gardner, D.K., and Gottlieb, D. eds. (Cold Spring Harbor,New York: Cold Spring Harbor Laboratory Press). 205-230.30. Smith, A., personal communication.31. Smith, A.G. (2001). Origins and properties of mouseembryonic stem cells. Annu. Rev. Cell. Dev. Biol.32. Stevens, L.C. (1970). The development of transplantableteratocarcinomas from intratesticular grafts of pre-andpostimplantation mouse embryos. Dev. Biol. 21, 364-382.33. Stoykova, A. and Gruss, P. (1994). Roles of Pax-genes indeveloping and adult brain as suggested by expressionpatterns. J. Neurosci. 14, 1395-1412.34. Thomson, J.A., Kalishman, J., Golos, T.G., Durning, M., Harris,C.P., Becker, R.A., and Hearn, J.P. (1995). Isolation of aprimate embryonic stem cell line. Proc. Natl. Acad. Sci.U. S. A. 92, 7844-7848.35. Thomson, J.A., Itskovitz-Eldor, J., Shapiro, S.S., Waknitz, M.A.,Swiergiel, J.J., Marshall, V.S., and Jones, J.M. (1998).Embryonic stem cell lines derived from human blastocysts.Science. 282, 1145-1147.36. Thomson, J.A. and Marshall, V.S. (1998). Primate embryonicstem cells. Curr. Top. Dev. Biol. 38, 133-165.37. Weissman, I.L. (2000). <strong>Stem</strong> cells: units of development,units of regeneration, and units in evolution. Cell. 100,157-168.38. Wianny, F., Real, F.X., Mummery, C.L., van Rooijen, M., Lahti,J., Samarut, J., and Savatier, P. (1998). G1-phase regulators,Cyclin D1, Cyclin D2, and Cyclin D3: up-regulation at gastrulationand dynamic expression during neurolation. Dev.Dyn. 212, 49-62.39. Williams, R.L., Hilton, D.J., Pease, S., Willson, T.A., Stewart,C.L., Gearing, D.P., Wagner, E.F., Metcalf, D., Nicola, N.A.,and Gough, N.M. (1988). Myeloid leukaemia inhibitoryfactor maintains the developmental potential ofembryonic stem cells. Nature. 336, 684-687.40. Yamashita, J., Itoh, H., Hirashima, M., Ogawa, M.,Nishikawa, S., Yurugi, T., Naito, M., Nakao, K., and Nishikawa,S. (2000). Flk1-positive cells derived from embryonic stemcells serve as vascular progenitors. Nature. 408, 92-96.41. Ye, W., Shimamura, K., Rubenstein, J.L., Hynes, M.A.,and Rosenthal, A. (1998). FGF and Shh signals controldopaminergic and serotonergic cell fate in the anteriorneural plate. Cell. 93, 755-766.27. Shamblott, M.J., Axelman, J., Wang, S., Bugg, E.M.,Littlefield, J.W., Donovan, P.J., Blumenthal, P.D., Huggins,G.R., and Gearhart, J.D. (1998). Derivation of pluripotentstem cells from cultured human primordial germ cells.Proc. Natl. Acad. Sci. U. S. A. 95, 13726-13731.B-11
Appendix B: Mouse Embryonic <strong>Stem</strong> <strong>Cells</strong>This page intentionally left blankB-12
APPENDIX C:HUMAN EMBRYONIC STEM CELLSAND HUMAN EMBRYONIC GERM CELLSMETHODS FOR GROWING HUMANEMBRYONIC STEM CELLS IN VITROTo grow cultures of human ES cells, Thomson and hiscollaborators used 36 fresh or frozen embryos generatedin IVF laboratories from couples undergoingtreatment for infertility. From the 14 embryos thatdeveloped to the blastocyst stage, they established5 human ES cell lines—H1, H7, H9, H13 and H14 [35].Four of the 5 lines were derived from frozen embryosprovided to Thomson’s laboratory by Josef Itskovitz-Eldor, of the Rambam Medical Center in Haifa, Israel.The ES cell line from the fifth, fresh embryo wasderived from an embryo donated in Wisconsin.To generate human ES cell cultures, cells from theinner cell mass of a human blastocyst were culturedin a multi-step process. The pluripotent cells of theinner cell mass were separated from the surroundingtrophectoderm by immunosurgery, the antibodymediateddissolution of the trophectoderm. The innercell masses were plated in culture dishes containinggrowth medium supplemented with fetal bovineserum on feeder layers of mouse embryonic fibroblaststhat had been gamma-irradiated to preventtheir replication. After 9 to 15 days, when inner cellmasses had divided and formed clumps of cells,cells from the periphery of the clumps were chemicallyor mechanically dissociated and replated inthe same culture conditions. Colonies of apparentlyhomogeneous cells were selectively removed,mechanically dissociated, and replated. These wereexpanded and passaged, thus creating a cell line.None of the initial 5 human ES cell lines generated inthis manner was derived clonally (cloned from asingle cell and are, therefore, genetically identical)[35] (see Figure C.1. Techniques for GeneratingEmbryonic <strong>Stem</strong> Cell Cultures).The five original human ES cell lines continued todivide without differentiating for 5 to 6 months [35].Since then, the H9 line has divided for nearly twoyears in vitro, for more than 300 population doublingsand has yielded two subclones, H9.1 and H9.2 [1] 1 .All the ES cell lines express high levels of telomerase[1, 36], the enzyme that helps maintain telomereswhich protect the ends of chromosomes. Telomeraseactivity and long telomeres are characteristic ofproliferating cells in embryonic tissues and of germcells. Human somatic cells, however, do not showtelomerase activity and their telomeres are considerablyshorter. Unlike ES cells, differentiated somaticcells also stop dividing in culture—a phenomenoncalled replicative senescence (see Figure C.2.Telomeres and Telomerase).Three of the human ES cell lines generated byThomson were XY (male) and two were XX (female);all maintained a normal karyotype. Like monkey EScells [34], human ES cells express a panel of surfacemakers that include the stage-specific embryonicantigens SSEA-3 and SSEA-4, as well as TRA-1-60,TRA-1-81, and alkaline phosphatase [14, 25, 26, 35].Mouse ES cells do not express SSEA-3 or SSEA-4; theyexpress SSEA-1, which human and monkey ES cellsdo not. Human ES cells also express the transcriptionfactor Oct-4 [26], as mouse ES cells do.A somewhat different technique for deriving andculturing human ES cells has now been reported by1The H9.1 and H9.2 clonal cell lines were produced by first plating 105 of the parent H9 cells per well in tissue-culture plates. The culture mediumcontained KnockOut Dulbecco’s modified minimal essential medium (a serum-free substitute for the 20% fetal bovine serum used in the 1998experiments), and basic FGF, which is necessary to maintain cell proliferation and prevent differentiation. To generate clonal cell lines from individualH9 ES cells, 384 single cells were removed from these cultures and transferred individually to the wells of larger plates that contained non-dividingmouse embryonic fibroblasts (MEF) as feeder layers. The single ES cells proliferated and, every 7 days, were dissociated and replated, a process thatgenerate two clonal cell lines, H9.1 and H9.2.C-1
Appendix C: Human Embryonic <strong>Stem</strong> <strong>Cells</strong> and Human Embryonic Germ <strong>Cells</strong>Cleavagestage embryoCulturedblastocystIsolatedinner cell mass<strong>Cells</strong> dissociatedand replatedIrradiated mousefibroblast feeder cellsNew feeder cells© 2001 Terese Winslow, Caitlin DuckwallEstablished embryonic stem cell cell culturesFigure C.1. Techniques for Generating Embryonic <strong>Stem</strong> Cell Cultures.C-2
Appendix C: Human Embryonic <strong>Stem</strong> <strong>Cells</strong> and Human Embryonic Germ <strong>Cells</strong>TELOMERESEmbryonic<strong>Stem</strong><strong>Cells</strong>Adult<strong>Stem</strong><strong>Cells</strong>EXTENDING THE LENGTH OF A TELOMEREChromosomeBeforeNucleusShort endof DNATelomeraseRNA templateTelomerelongTelomereshortNew DNATelomeraseactiveTelomeraseinactiveor absentDNApolymeraseTelomere is arepeatingDNAsequenceAfter© 2001 Terese WinslowFigure C.2. Telomeres and Telomerase.A telomere is a repeating sequence of double-stranded DNA located at the ends of chromosomes. Greater telomere lengthis associated with immortalized cell lines such as embryonic stem cells and cancer cells. As cells divide and differentiatethroughout the lifespan of an organism or cell line, the telomeres become progressively shortened and lose the ability tomaintain their length. Telomerase is an enzyme that lengthens telomeres by adding on repeating sequences of DNA.Telomerase binds to the ends of the telomere via an RNA template that is used for the attachment of a new strand of DNA.Telomerase adds several repeated DNA sequences then releases and a second enzyme, DNA Polymerase, attaches theopposite or complementary strand of DNA completing the double stranded extension of the chromosome ends. High levelsof telomerase activity are detected in embryonic stem cells and cancer cells, whereas little or no telomerase activity ispresent in most mature, differentiated cell types. The functions of telomeres and telomerase appear to be important in celldivision, normal development, and aging.C-3
Appendix C: Human Embryonic <strong>Stem</strong> <strong>Cells</strong> and Human Embryonic Germ <strong>Cells</strong>investigators in Singapore and Australia. The humanblastocysts are cultured in Singapore, where monolayercultures of human ES cells growing on feederlayers are prepared. The primary cultures are shippedto Australia, where the colonies of growing cells aredissociated mechanically and replated. LIF and fetalbovine serum are added to the growth medium. Thecells do not grow well without serum, although it is notclear that LIF has any effect. Under these in vitro conditions,the ES cells tend to clump and differentiatespontaneously as they are passaged. In vivo, afterinjection into the testes of immunocompromised mice,the ES cells differentiate into bone, cartilage, squamousand cuboidal epithelium, neural cells, glandularepithelium, and striated muscle [25, 26]. Six human EScell lines have been generated from 12 blastocysts, ahigh yield by any standard. The original two cell lineswere generated from fresh embryos; the other fourcells lines were generated from frozen embryos [23].Recent reports have identified additional human EScell lines that have been developed. New derivationshave been conducted from the blastocyst of frozenembryos at two centers in India (National Centre forBiological Sciences, University of Agriculture Sciences,Bangalore; Harkishondas Hospital in collaboration withReliance Biotechnology, Bombay). They used derivationtechniques that differ from those of the Thomsonlaboratory including the use of laser ablation for theremoval of the inner cell mass [22, 24, 33, 36]. Anadditional preparation of human ES cell lines hasbeen conducted in San Francisco [10]. There are nopublications to date on these cell lines and theextent of the research being conducted is not known.By several criteria, all of the human ES cell lines generatedto date are pluripotent. When injected underthe skin or into the testes of immunocompromisedmice—an in vivo method of determining pluripotency—the human ES cells form teratomas that containderivatives of all three primary germ layers. Whenallowed to differentiate in vitro (by culturing the cellsin the absence of MEF feeder layers), the human EScells differentiate spontaneously. Subsequent studiesindicate that in vitro differentiation of these human EScell lines is extensive; the cells can generate manycell types that are derived from all three primarygerm layers [1, 14, 25, 26]. However, the extent towhich these human ES cell lines will differentiate invitro does not match their more extensive differentiationcapability in vivo (in teratomas) [19].METHODS FOR THE DERIVATION ANDCULTURE OF HUMAN EMBRYONICGERM CELLSTo derive cultures of human embryonic germ (EG)-likecells, Gearhart and his colleagues grew cells from 38initial cultures of primordial germ cells (PGC), whichwere obtained from the gonadal ridge and mesenteryof 5 to 9-week gestation fetal tissue. (PGCs giverise to the germ cells, eggs and sperm, in the adult.)The PGCs were mechanically and chemically dissociated,then plated on a feeder layer of non-dividing,mouse STO fibroblasts in growth medium supplementedwith fetal bovine serum [31]. Unlike thegrowth conditions initially reported for human ES cells[35], the medium for human PGCs cells also containedthe cytokine, leukemia inhibitory factor (LIF),a mitogen (basic fibroblast growth factor, bFGF),and forskolin.After one to three weeks in vitro, the human PGCshad formed dense, multilayered colonies of cellsthat resembled mouse ES or EG cells. <strong>Cells</strong> in thesecolonies expressed SSEA-1, SSEA-3, SSEA-4, TRA1-60,TRA-1-81, and alkaline phosphatase. A small, variablepercentage (1 to 20 %) of the PGC-derived cellcolonies spontaneously formed embryoid bodies. Thegrowth medium for embryoid body cultures lackedLIF, bFGF, and forskolin. The embryoid bodies werecollected from the cultures and either examined forthe cell types they contained, or replated into singlewells of a tissue culture plate for 14 days. The rangeof cell types in the human PGC-derived embryoidbodies included derivatives of all three embryonicgerm layers—endoderm, mesoderm, and ectoderm—basedon the appearance of the cells andthe surface markers they expressed. This result wasinterpreted to mean that the PGC-derived cells werepluripotent, however, it was not possible to demonstratepluripotency in vivo by generating the formationof teratomas in mice [31].In their next series of experiments, Gearhart and hiscollaborators devised methods for growing stem cellsderived from human EG cells. The process requiresthe generation of embryoid bodies, which form spontaneouslyfrom EG cells that remain attached to thesubstrate. The embryoid bodies then float freely in theculture medium. Each embryoid body consists of anunpredictable mix of partially differentiated cell types,but allowing the embryoid bodies to form is the mostC-4
Appendix C: Human Embryonic <strong>Stem</strong> <strong>Cells</strong> and Human Embryonic Germ <strong>Cells</strong>consistent way of allowing EG-derived cells to differentiate[11]. The process involves several stages ofcell derivation in a different kinds of growth media.<strong>Cells</strong> from low-serum cultures were passaged, chemicallydissociated, and resuspended in a culturemedia that contains 50% fetal bovine serum, andfrozen in this state. To measure proliferation, culturesare derived from the frozen embryoid bodies andgrown in the same media used to grow the dissociatedcells. Clonal cell lines are then derived fromthe embryoid body-derived cultures [32].The embryoid body-derived cells resulting from thisprocess have high proliferative capacity and geneexpression patterns that are representative of multiplecell lineages. This suggests that the embryoid bodyderivedcells are progenitor or precursor cells for avariety of differentiated cell types [11].Recently, Neil Hanley and David Wilson from theUniversity of Southampton, United Kingdom, havederived EG cells from the primordial germ cells of thefetal gonadal ridge. Using material at 8 -10 weeksgestation, cells were derived slightly differently formthe methods of Shamblott et al using a combinationof irradiated fibroblast feeder layers and gelatincoated tissue culture dishes [12]. This method andthe further characterization of the alkaline phosphatase/SSEA1-positive EG cells currently remains unpublished.DIRECTED DIFFERENTIATION OFHUMAN EMBRYONIC STEM CELLS ANDEMBRYONIC GERM CELLS IN VITROAs with cultures of mouse ES cells, human ES cellsbegin to differentiate if they are removed from feederlayers and grown in suspension culture on a nonadherentsurface. The human ES cells form embryoidbodies which, in the early stages, may be simple orcystic and filled with fluid. Although human embryoidbodies vary in their cellular content, many includecells that look like neurons and heart muscle cells[14, 25, 26].After the human embryoid bodies form, they can bedissociated and replated in monolayer cultures whichare then exposed to specific growth factors thatinfluence further cell differentiation. Some growthfactors induce cell types that would normally bederived from ectoderm in the embryo; these includeretinoic acid, epidermal growth factor (EGF), bonemorphogenic protein 4 (BMP4), and basic fibroblastgrowth factor (bFGF). Other growth factors, such asactivin-A and transforming growth factor–beta 1(TGF-ß1) trigger the differentiation of mesodermallyderivedcells. Two other factors, hepatocyte growthfactor (HGF) and nerve growth factor (NGF), promotedifferentiation into all three germ layers, includingendoderm. When these eight growth factors wereadded individually to cell cultures derived fromembryoid bodies (generated from the H9 line fromThomson’s laboratory), the cells differentiated into 11cell types that represented all three germ layers. Theidentify of the differentiated human embryoid bodyderivedcells was determined by their morphology,growth characteristics and expression of messengerRNA (mRNA) for specific markers [30] (see Figure A.6Gene Transcription, Translation, and Protein Synthesis).Human embryoid body-derived cells will differentiatespontaneously into many kinds of cells, without theaddition of growth factors. However, the addition ofone of a number of growth factors resulted in culturesthat were more likely to be populated by only one ortwo types of differentiated cells, as measured bymRNA transcripts expressed by the cells. Humanembryoid body-derived cultures treated with bFGFdifferentiated largely into epidermal epithelial cellsthat express keratin, a protein in skin. <strong>Cells</strong> in activin-A–treated cultures formed muscle cell-like syncytium—fused, multinucleated populations of similar cells—that express the enzyme muscle-specific enolase.And cultures treated with retinoic acid differentiatedinto cells that resemble neurons and express neurofilamentH. However, the same growth factor typicallyinduced the expression of multiple markers; none ofthe resulting cell populations was homogeneous [30].Spontaneous differentiation of human ES cells intohematopoietic cells, which form all the lineages ofblood cells, is rare in vitro. However, by co-culturinghuman ES cells with mouse bone marrow stromalcells (irradiated to prevent their replication) in growthmedium that contains fetal bovine serum, but noadded growth factors, the cells differentiate to formwhat appear to be hematopoietic precursor cells.The partly differentiated cells express CD34, a markerfor blood cell precursors. If these partly differentiatedhuman ES cells are replated under conditions thatallow them to form colonies of hematopoietic cells,they differentiate into erythroid cells, macrophages,granulocytes, and megakaryocytes [19] (see Chapter5. Hematopoietic <strong>Stem</strong> <strong>Cells</strong>).C-5
Appendix C: Human Embryonic <strong>Stem</strong> <strong>Cells</strong> and Human Embryonic Germ <strong>Cells</strong>As indicated, human ES cells maintained in vitro havetendency to differentiate spontaneously, a characteristicthat may not always be desirable. Thus, it maybe necessary to devise methods that allow undifferentiatedES cells be selected from a culture that containsa mixture of differentiated, partially differentiated,and undifferentiated cells types. The undifferentiatedES cells could then be used for the purposesof directed differentiation, or they could be removedfrom cultures in which the differentiated cell types arethe desired product. In either case, a suggestedmethod for identifying undifferentiated ES cells is tointroduce a marker gene—such as that encodinggreen fluorescence protein (GFP)—whose expressionis driven by a gene that is specifically expressed inproliferating, undifferentiated cells, such as Rex1.Then, undifferentiated cells that express GFP can beselectively removed from human ES cultures by usinga fluorescence activated cells sorter (FACS) [9] (seeAppendix E.i. Markers: How Do Researchers Use Themto Identify <strong>Stem</strong> <strong>Cells</strong>?).Joseph Itskovitz-Eldor and his colleagues are trying todirect the differentiation of human ES cells into cardiacmyocytes. They use several of the human ESlines generated in James Thomson’s laboratory. Theyreport a number of cells in embryoid bodies thathave contractile activity and express genetic markersconsistent commonly found in cardiac myocytes [16](see Chapter 9. Can <strong>Stem</strong> <strong>Cells</strong> Repair a DamagedHeart?). Karl Skorecki and his collaborators have hadsuccess in directing the differentiation of human EScell lines (originating from the Thomson laboratoryderivation) into pancreatic islet-like cells that secreteinsulin. They have also reported the expression ofinsulin genes found in islet-like cells of the pancreas[6] (see Chapter 7. <strong>Stem</strong> <strong>Cells</strong> and Diabetes).A new report indicates that it may be possible todirect the differentiation of human EG cells intoneuronal cells that may play a role in restoring somefunction to paralyzed animals. The SDEC human cellline in this study was generated from embryoidbodies that formed in culture by the aggregation ofhuman EG cells, and is referred to as an embryoidderivedcell line. SDEC cells express a panel ofneuronal markers that include nestin, neurofilament,tau protein, neuron-specific enolase; the cells alsoexpress the glial cells markers glial fibrillary acidicprotein, galactocerebroside, and CNPase. No in vitroassays that indicate cell function have been reportedfor SDEC cell assays. However, when SDEC cells wereinjected into the central canal of the spinal cord ofrats—whose hind limbs were paralyzed by aninduced form of amytrophic lateral sclerosis (ALS,also known as Lou Gehrig’s disease)—the majority ofanimals showed some functional recovery. It is notclear whether the human embryoid body-derivedcells replaced some of the spinal motor neuronsdamaged by the experimental ALS, or whether theinjected cells triggered neurons in the recipientanimals to recover lost function [17] (see Chapter 8.Rebuilding the Nervous System with <strong>Stem</strong> <strong>Cells</strong>).Several groups of investigators are trying to direct thedifferentiation of human ES cell lines, but their work isnot yet published. They reported their findings ininterviews with the NIH or during presentations atscientific meetings. They include, but are not limitedto, the following:• Martin Pera, Alan Trounson, and their coworkersare trying to direct the differentiation of humanES cells along a neural lineage using the BMPantagonist noggin. They generate an apparentlyhomogenous population of cells, but have notyet characterized it [23].• Brenda Kahan, Jon Odorico, and their coworkersare trying to direct the differentiation of thehuman ES lines H1 and H9 into pancreatic isletcells, which are endodermal derivatives. Theyinduce the formation of embryoid bodies inmedium lacking bFGF and assay cultures for theexpression of transcripts for the endodermalmarkers hnf3, lfabp, ifabp, and villin 1. Differentiatedprogeny from these cells express thegenes for insulin, glucagon, and somatostatin,which are normally expressed in pancreaticislet cells [15].• Micha Drukker, Nissim Benvenisty, and theircolleagues are trying to direct the differentiationof human ES cells into neurons by addingretinoic acid or ß-NGF to the growth medium.They report that about 80% of embryoid bodiesexposed to these factors contain differentiatedneuronal cells, as determined by morphologyand the expression of receptors for dopamine orserotonin [8].• Su-Chang Zhang, James Thomson, and theircollaborators are trying to direct the differentiationof human ES cells into neural epithelial cells, byC-6
Appendix C: Human Embryonic <strong>Stem</strong> <strong>Cells</strong> and Human Embryonic Germ <strong>Cells</strong>selecting cells from embryoid bodies thatexpress nestin, glial fibrillary acidic protein (GFAP,an astrocyte marker), neural cell adhesion molecule(NCAM), and Musashi-1. The differentiatedcell types express (as yet unidentified) markers ofneurons and glial cells. After transplantation intothe mouse brain, the cells aggregated intoclusters and migrate into the brain parenchymawhere they express (unidentified) neural and glialmarkers. By 10 weeks after transplantation, thehuman embryoid-derived cells had not formedteratomas [38].• Margaret Inokuma, Melissa Carpenter, and theircolleagues are trying to direct the differentiationof human ES cells into neural cells using neurotrophin3 (NT3) and brain-derived neurotrophicfactor (BNDF). Some of the resulting cells stainpositive for tyrosine hydroxylase (TH, the ratelimitingenzyme in dopamine synthesis) orgamma-amino butyric acid (GABA), an inhibitoryneurotransmitter [13].• Chunhui Xu, Melissa Carpenter, and theircolleagues report preliminary data on growinghuman ES cells in vitro in serum-free mediumwithout feeder layers. The details of their methodhave not been published but apparently includeMatrigel or laminin as a substrate, basic FGF, andconditioned medium from cultures of mouseembryo fibroblasts [39].• J.S. Lebkowski and Margaret Inokuma et al.report methods for using genetic modificationand changes in culture conditions to direct thedifferentiation of the human ES cell lines H1 andH7 in vitro. They grow undifferentiated human EScells in serum-free medium on Matrigel orlaminin, and then add 20% serum replacementmedium plus DMSO to direct the first stage ofdifferentiation. The second stage is induced byadding sodium butyrate to the medium. Cellmaturation occurs in a third medium (notdescribed). To induce differentiation into neuralcells, they allow the human ES cells to formembryoid bodies, which are then expanded,and plated in B27 medium (not described), withFGF and EGF. The resulting cells express theneural progenitor markers psNCAM and A2B5.Some differentiated cells express the glial markerGFAP. Other cells express the neuronal markersß-tubulin III and synaptophysin, or stain for theneurotransmitters GABA, tyrosine hydroxylase, orglutamate. No quantitative data, electrophysiologicaldata, or responses to neurotransmitterapplication are reported [18].HUMAN EMBRYONIC CARCINOMACELLSEmbryonal carcinoma (EC) cells are the “stem cells”that occur in unusual germ cell tumors, also calledteratocarcinomas. As such, they give rise to the differentiatedcell types that also occur in the tumors. Thetumors probably arise from a malignant form of aprimordial germ cell. In humans, germ cell tumorsoccur most often in the testis of young men; theseare always malignant, but usually treatable. Benigngerm tumors called ovarian cysts can occur in theovary; malignant ovarian germ cell tumors are muchrarer (malignant ovarian tumors – usually referred toas ovarian cancer – are not germ cell tumors).Germ cell tumors have been studied extensively inhumans and mice. They contain an aberrant mix ofdifferentiated cell types, rather than a single kind oftumor cell. Small groups of the cells may appearorganized, but overall, the tissue in the tumor is disorganized.Teratocarcinomas are of particular interestbecause they contain EC cells, which in many waysresemble normal ES cells [4].Like human ES cells, human EC cells proliferate extensivelyin vitro and in teratomas formed in vivo afterinjection into immunocompromised mice. Becauseresearch on human ES cells is so recent, a directcomparison of cultured human EC cells and humanES cells has just begun. 2 Both cell types express apanel of surface markers, including the embryonicstage-specific antigens SSEA-3 and SSEA-4. Neitherhuman ES cells nor human EC cells expresses SSEA-1,as mouse ES and EC cells do [5, 26, 35]. Conversely,mouse EC and ES cells do not express SSEA-3 orSSEA-4. Human EC and ES cells also carry on their surfaceskeratin sulfate proteoglycans that can belabeled with specific antibodies, TRA-1-60 andTRA-1-81 [3, 7]. Also, unlike their mouse counterparts,2As of May 9, 2001, the comparisons between human ES cells and EC cells have been made only in Peter Andrews’ laboratory at the University ofSheffield, United Kingdom. James Thomson, of the University of Wisconsin at Madison, supplied Andrews with four lines of human ES cells [3, 32].C-7
Appendix C: Human Embryonic <strong>Stem</strong> <strong>Cells</strong> and Human Embryonic Germ <strong>Cells</strong>human ES and EC cells express MHC Class I antigens,which are responsible for immunogenicity (seeChapter 6. Autoimmune Diseases and the Promise of<strong>Stem</strong> Cell-Based Therapies). Like mouse ES and ECcells, undifferentiated human ES and EC cells stronglyexpress the transcription factor Oct-4 [26, 4], which iswidely regarded as a hallmark of pluripotent embryoniccells [20, 28, 29] (see Table C.1. Comparison ofMouse, Monkey, and Human Pluripotent <strong>Stem</strong> <strong>Cells</strong>).Human ES and EC cells differ in important ways.Human ES cells are euploid, meaning they carry thenormal complement of chromosomes. In contrast,human EC cells are aneuploid; their chromosomesare distinctly abnormal. (Interestingly, the chromosomesin mouse EC cells do not appear as abnormal,although they do carry subtle chromosomalabnormalities.) The ability of both cell types todifferentiate into various tissue types has beenexplored by injecting human ES and EC cells intoTable C.1. Comparison of Mouse, Monkey, and Human Pluripotent <strong>Stem</strong> <strong>Cells</strong>MarkerNameMouse EC/ES/EG cellsMonkeyES cellsHumanES cellsHumanEG cellsHumanEC cellsSSEA-1 + – – + –SSEA-3 – + + + +SEA-4 – + + + +TRA-1-60 – + + + +TRA-1-81 – + + + +Alkalinephosphatase+ + + + +Oct-4 + + + Unknown +Telomerase activity + ES, EC Unknown + Unknown +Feeder-celldependentES, EG,some ECYes Yes Yes Some; relatively lowclonal efficiencyFactors which aidin stem cellself-renewalLIF and otherfactors that actthrough gp130receptor and cansubstitute forfeeder layerCo-culture withfeeder cells; otherpromoting factorshave not beenidentifiedFeeder cells +serum; feederlayer +serum-freemedium + bFGFLIF, bFGF,forskolinUnknown;low proliferativecapacityGrowthcharacteristicsin vitroForm tight,rounded,multi-layer clumps;can form EBsForm flat, looseaggregates;can form EBsForm flat, looseaggregates;can form EBsForm rounded,multi-layer clumps;can form EBsForm flat, looseaggregates;can form EBsTeratomaformation in vivoChimeraformation+ + + – ++ Unknown + – +KEYES cell =EG cell =EC cell =SSEA =Embryonic stem cellEmbryonic germ cellEmbryonal carcinoma cellStage-specific embryonic antigenTRA =LIF =bFGF =EB =Tumor rejection antigen-1Leukemia inhibitory factorBasic fibroblast growth factorEmbryoid bodiesC-8
Appendix C: Human Embryonic <strong>Stem</strong> <strong>Cells</strong> and Human Embryonic Germ <strong>Cells</strong>immunocompromised mice. Injected human ES cellswill form embryonic stem cell teratomas in mice, andthe tumors consist of cells derived from all threeprimary germ layers [36]. In contrast, human EC celllines vary in their ability to differentiate in vivo, but ingeneral are more limited than are ES cells. Forexample, NTERA2 cl.D1 cells (which are derived fromhuman TERA2 EC cells) generate only a few kinds oftissues, including primitive gut-like structures, andneural tissue after injection into immunocompromisedmice [2].The in vitro growth characteristics of human ES andEC cells are also being compared. Both cell typesgrow well in serum-containing medium on feederlayers of mouse embryonic fibroblasts that havebeen treated to block their proliferation. It is difficultto induce human ES cells to proliferate in theabsence of feeder layers, unless conditioned mediumfrom feeder cells cultures is added. However,many human EC cells lines, such as the NTERA2 line,are not dependent on feeder layers [2].If human ES cells are removed from their feederlayers, they differentiate spontaneously into manycell types. Mouse ES cells, after removal from feederlayers, can be stimulated to divide and preventedfrom differentiating by adding LIF (leukemia inhibitoryfactor); neither human ES nor EC cells show thisresponse to LIF. Instead, if human ES cells grow toconfluence (where the cells grow to completelycover the culture plates), the cells aggregate andbegin to differentiate spontaneously [26, 35]. Also,human ES cells grown in suspension cultures at highdensity will form embryoid bodies. Embryoid bodiesare clumps or groupings of cells that form whencultured in plates or media and do not occur innature. Embryoid bodies contain undifferentiated andpartially differentiated cells [14]. However, human ECcells remain undifferentiated when grown at highdensity [4]. Whether these apparent differences in thein vitro growth characteristics of human ES and ECcells are meaningful or real is subject to debate [5].The pluripotency of human EC cells does not equalthat of human ES cells. Human ES cells can differentiateinto a wide range of cell types in vitro, and canform teratomas with many cell types after injectioninto immune-deficient mice. The differentiationpotential of most lines of human EC cells is morelimited, both in vitro and in vivo. One human EC cellline, however, TERA2, differentiates easily in vitro. Thewell-studied morphogen, retinoic acid, induces TERA2cells (and the subline NTERA2) to differentiate intoneural precursors, which can then become matureneurons [4]. But when human ES cells are exposed toretinoic acid, they differentiate into a wider array ofcell types than do human EC cells. As yet, it is notclear how the mechanism of action of retinoic aciddiffers in human ES cells versus human EC cells. Itmay be that, because of their tumor origin, humanEC cells carry genetic variations linked to tumorigenesisthat restrict their capacity for differentiation [5].Thus, the in vitro and in vivo characteristics of humanEC cells resembles that of human ES cells in certainrespects, but not in others. Although ES cells will likelyprove to be a better model for understanding humandevelopment than will EC cells [27], there may besome aspects of development that EC cells willreveal that ES cells will not [5].REFERENCES1. Amit, M., Carpenter, M.K., Inokuma, M.S., Chiu, C.P., Harris,C.P., Waknitz, M.A., Itskovitz-Eldor, J., and Thomson, J.A.(2000). Clonally derived human embryonic stem cell linesmaintain pluripotency and proliferative potential forprolonged periods of culture. Dev. Biol. 227, 271-278.2. Andrews, P.W., Damjanov, I., Simon, D., Banting, G.S., Carlin,C., Dracopoli, N.C., and Fogh, J. (1984). Pluripotent embryonalcarcinoma clones derived from the human teratocarcinomacell line Tera-2. Differentiation in vivo and in vitro.Lab. Invest. 50, 147-162.3. Andrews, P.W., Casper, J., Damjanov, I., Duggan-Keen,M., Giwercman, A., Hata, J., von Keitz, A., Looijenga, L.H.,Millan, J.L., Oosterhuis, J.W., Pera, M., Sawada, M., Schmoll,H.J., Skakkebaek, N.E., van Putten, W., and Stern, P. (1996).Comparative analysis of cell surface antigens expressed bycell lines derived from human germ cell tumours. Int. J.Cancer. 66, 806-816.4. Andrews, P.W. (1998). Teratocarcinomas and humanembryology: pluripotent human EC cell lines. Reviewarticle. APMIS. 106, 158-167.5. Andrews, P.W., personal communication.6. Assady, S., Maor, G., Amit, M., Itskovitz-Eldor, J., Skorecki, K.L.,and Tzukerman, M. (2001). Insulin production by humanembryonic stem cells. Diabetes. 50.7. Badcock, G., Pigott, C., Goepel, J., and Andrews, P.W.(1999). The human embryonal carcinoma marker antigenTRA-1-60 is a sialylated keratan sulfate proteoglycan.Cancer Res. 59, 4715-4719.8. Drukker, M., Schuldiner, M., Eiges, R., Eden, A., Yanuka, O.,Itskovitz-Eldor, J., and Benvenisty, N. Keystone symposia.Pluripotent stem cells: biology and applications. Inducedneuronal differentiation of human embryonic stem cells.Poster abstracts. 207.C-9
Appendix C: Human Embryonic <strong>Stem</strong> <strong>Cells</strong> and Human Embryonic Germ <strong>Cells</strong>9. Eiges, R., Schuldiner, M., Drukker, M., Yanuka, O., Itskovitz-Eldor, J., and Benvenisty, N. (2001). Establishment of humanembryonic stem cell-transduced clones carrying a markerof undifferentiated cells. Curr. Biol. 11, 514-518.10. Firpo, M., personal communication.11. Gearhart, J., personal communication.12. Hanley, N., personal communication.13. Inokuma, M.S., Denham, J., Mujtaba, T., Rao, M., andCarpenter, M.K. Keystone symposia. Pluripotent stem cells:biology and applications. Human embryonic stem cellsdifferentiate into neural cells in vitro. Poster abstracts. 312.14. Itskovitz-Eldor, J., Schuldiner, M., Karsenti, D., Eden, A.,Yanuka, O., Amit, M., Soreq, H., and Benvenisty, N. (2000).Differentiation of human embryonic stem cells into embryoidbodies comprising the three embryonic germ layers.Mol. Med. 6, 88-95.15. Kahan, B.W., Jacobson, L.M., Hullett, D.A., Thomson, J.,and Odorico, J.S. Keystone symposia. Pluripotent stem cells:biology and applications. In vitro differentiation of humanembryonic stem (ES) cell lines: expression of endodermandpancreatic islet-specific genes. Poster abstract. 117.16. Kehat, I., Kenyagin-Karsenti, D., Druckmann, M., Segev, H.,Amit, M., Gepstein, A., Livne, E., Binah, O., Itskovitz-Eldor, J.,and Gepstein, L. (2001). Human embryonic stem cellscan differentiate into myocytes portraying cardiomyocyticstructural and functional properties. J. Clin. Invest. (In press)17. Kerr, D.A., Llado, J., Shamblott, M., Maragakis, N., Irani,D.N., Dike, S., Sappington, A., Gearhart, J., and Rothstein, J.(2001). Human embryonic germ cell derivatives facillitatemotor recovery of rats with diffuse motor neuron injury.18. Lebkowski, J.S., Gold, J., Chiu, C.P., Xu, C., Inokuma, M.,Hassanipour, M., Denham, J., Piderit, A., Rosler, E., Golds,K., and Carpenter, M. ASGT Meeting. Targeted GeneExpression I. Human Embryonic <strong>Stem</strong> <strong>Cells</strong>: GeneticModification and Differentiation into Cell Types for PotentialTransplantation Applications. Poster Abstract. 205.19. Odorico, J.S., Kaufman, D.S., and Thomson, J.A. (2001).Multilineage Differentiation from Human Embryonic <strong>Stem</strong>Cell Lines. <strong>Stem</strong> <strong>Cells</strong>. 19, 193-204.20. Okamoto, K., Okazawa, H., Okuda, A., Sakai, M.,Muramatsu, M., and Hamada, H. (1990). A novel octamerbinding transcription factor is differentially expressed inmouse embryonic cells. Cell. 60, 461-472.21. Panicker, M., personal communication.22. Pera, M., personal communication.23. Rao, M., personal communication.24. Reubinoff BE, Pera, M., Fong, C.Y., and Trounson, A. (2000).Research Errata. Nat. Biotechnol. 18, 559.25. Reubinoff, B.E., Pera, M.F., Fong, C.Y., Trounson, A., andBongso, A. (2000). Embryonic stem cell lines from humanblastocysts: somatic differentiation in vitro. Nat. Biotechnol.18, 399-404.26. Roach, S., Cooper, S., Bennett, W., and Pera, M.F. (1993).Cultured cell lines from human teratomas: windows intotumour growth and differentiation and early humandevelopment. Eur. Urol. 23, 82-87.27. Rosner, J.L. (1990). Reflections of science as a product.Nature. 345, 108.28. Schöler, H.R., Ruppert, S., Suzuki, N., Chowdhury, K., andGruss, P. (1990). New type of POU domain in germ linespecificprotein Oct-4. Nature. 344, 435-439.29. Schuldiner, M., Yanuka, O., Itskovitz-Eldor, J., Melton, D., andBenvenisty, N. (2000). Effects of eight growth factors on thedifferentiation of cells derived from human embryonic stemcells. Proc. Natl. Acad. Sci. U. S. A. 97, 11307-11312.30. Shamblott, M.J., Axelman, J., Wang, S., Bugg, E.M.,Littlefield, J.W., Donovan, P.J., Blumenthal, P.D., Huggins,G.R., and Gearhart, J.D. (1998). Derivation of pluripotentstem cells from cultured human primordial germ cells.Proc. Natl. Acad. Sci. U. S. A. 95, 13726-13731.31. Shamblott, M.J., Axelman, J., Littlefield, J.W., Blumenthal,P.D., Huggins, G.R., Cui, Y., Cheng, L., and Gearhart, J.D.(2001). Human embryonic germ cell derivatives expressa broad range of develpmentally distinct markers andproliferate extensively in vitro. Proc. Natl. Acad. Sci. U. S. A.98, 113-118.32. Thomson, J., personal communication.33. Thomson, J.A., Kalishman, J., Golos, T.G., Durning, M., Harris,C.P., Becker, R.A., and Hearn, J.P. (1995). Isolation of aprimate embryonic stem cell line. Proc. Natl. Acad. Sci. U.S. A. 92, 7844-7848.34. Thomson, J.A., Itskovitz-Eldor, J., Shapiro, S.S., Waknitz, M.A.,Swiergiel, J.J., Marshall, V.S., and Jones, J.M. (1998).Embryonic stem cell lines derived from human blastocysts.Science. 282, 1145-1147.35. Thomson, J.A. and Odorico, J.S. (2000). Human embryonicstem cell and embryonic germ cell lines. Trends.Biotechnol. 18, 53-57.36. Totey, S., personal communication.37. Xu, C., Inokuma, M.S., Denham, J., Golds, K., Kundu, P.,Gold, J.D., and Carpenter, M.K. Keystone symposia.Pluripotent stem cells: biology and applications. Growth ofundifferentiated human embryonic stem cells on definedmatrices with conditioned medium. Poster abstract. 133.38. Zhang, S.U., Wernig, M., Duncan, I.D., Brüstle, O., andThomson, J. Keystone symposia. Pluripotent stem cells:biology and applications. Directed differentiation of humanES cells to neural epithelia. Poster abstracts. 235.C-10
APPENDIX D:STEM CELL TABLESCOMPENDIUM OF SCIENTIFIC PUBLICATIONS REGARDING THEISOLATION AND CHARACTERIZATION OF STEM CELLSThe following tables provide an overview of informationabout stem cells that have been derived frommice and humans. The tables summarize publishedresearch that characterizes cells that are capable ofdeveloping into cells of multiple germ layers (i.e.,multipotent or pluripotent) or that can generate thedifferentiated cell types of another tissue (i.e., plasticity)such as a bone marrow cell becoming a neuronalcell. The tables do not include information about cellsconsidered progenitor ore precursor cells or thosethat can proliferate without the demonstrated abilityto generate cell types of other tissues.The tables list the tissue from which the cells werederived, the types of cells that developed, theconditions under which differentiation occurred, themethods by which the cells were characterized, andthe primary references for the information.D-1
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.i.Published Reports Adult on Isolation Human and Differentiation <strong>Stem</strong> <strong>Cells</strong> of Mouse <strong>Stem</strong> <strong>Cells</strong>Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceBonemarrowHematopoieticstem cell (HSC)Cardiac muscleCardiac injury induced inmiceInjected labeled HSCsinto injured heartMeasurement of greenfluorescent protein(GFP) in regeneratingcardiac cellsMeasurement ofcardiac-specific proteinand gene expressionCardiac-function testsOrlic et al.,2001HSCEpithelial cells ofthe liver, skin, lung,esophagus,stomach, smalland large intestineTransplantation of HSCsinto lethally irradiatedfemale miceDetection of antibodiesto cellular and cellsurfaceproteinsCell stainingProbing for Y chromosome-positivecellsKrause et al.,2001HSCCholangiocyteHepatocytePurification of HSCs frombone marrowTransplantation of HSCsinto mice with liverenzymedeficiencyObservation of normalizedliver function andregenerating hepatocytesMeasurement ofexpression of hematopoieticand hepaticcell-surface proteinsLagasse et al.,2000HSCPlateletRed blood cellWhite blood cellHematopoietic growthfactors: interleukin-3,interleukin-6,granulocyte-colonystimulating factor,erythropoietin, andthrombopoietinDetection of antibodiesto cell-surface proteinsColony-forming assaysImmunophenotypingSpangrudeet al., 1991Morrison et al.,1995HSCSide population(SP)Skeletal muscleLethal irradiation offemale miceInduced muscle injuryPurified bone marrowtransplanted into miceMeasurement ofdystrophin expression inregenerating muscle cellsFluorescence-activatedcell sorting (FACS)Probing for Y chromosome-positivecellsGussoni et al.,1999Mesenchymalstem cell (MSC)AdipocyteChondrocyteOsteoblastTenocyteDexamethasoneVitamin D3Bone morphogeneticprotein-2 (BMP-2)Detection of antibodybinding to cell-surfaceproteinsImmunofluorescenceFriedenstein etal., 1976Pereira et al.,1995Prockop, 1997D-2
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.i. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceBonemarrow(cont.)MSCAstrocyteNeuronInjection of MSCinto brain ofimmunocompromisedneonatal miceDetection of cell-surfacemarkers by usingantibodies andimmunofluorescenceKopen et al.,1999MSCAstrocyteNeuronEpidermal growth factorBrain-derivedneurotrophic factorß-mercaptoethanolRetinoic acidImmunofluorescenceCell sortingSanchez-Ramoset al., 2000MSC Neuron Stromal cells expandedas undifferentiated cellsß-mercaptoethanolButylated hydroxyanisoleDetection of numerousneuron-specific proteinsvia stainingWoodbury etal., 2000MSC Skeletal muscle 5-azacytidine andamphotericin BObservation of myotubesStaining for myocytesWakitani et al.,1995MSC and/orHSCAstrocyteMicrogliaOligodendrocyteInduced injury to neuraltissueBone marrowtransplantationDetection of antibodiesto cell-surface proteinsEglitis andMezey, 1997MSC and/orHSCCardiac muscleBone marrow transplantationof 5-azacytidinetreatedcells into micewith induced cardiacmuscle injuryCell staining for cardiacmuscle proteinsMeasurement of bloodpressureElectron microscopyObservation of beatingcells in vitroMeasurement of atrialnatriuretic peptideStaining cells for muscleproteinsTomita et al.,1999Makino et al.,1999MSC and/orHSCHepatocyteSuppression of liver cellproliferationInduced injury to liverBone marrowtransplantationStaining cellsAntibody labeling of cellsurfacemarkersTaniguchi et al.,1996Petersen et al.,1999Theise et al.,2000D-3
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.i. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceBonemarrow(cont.)MSC and/orHSCNeuronInduced neural tissueinjuryBone marrowtransplantation intofemale miceDetection of antibodiesto cell-surface proteinsProbing for Ychromosome-containingneuronsMezey et al.,2000Brazelton et al.,2000MSC, HSC, orside population(SP)Cardiac muscleSkeletal muscleLethal irradiation of miceBone marrowtransplantation fromnormal male donor miceinto mice with inducedmuscle degenerationProbing for Ychromosome-containingmuscle cellsDetection of expressionof myoregulatory proteinsBittner et al.,1999MSC, HSC, or SP Skeletal muscle Induced muscle tissueinjuryTransplantation ofgenetically marked bonemarrow intoimmunodeficient miceHistologic observation ofmuscle regenerationDetection of antibodiesto cell-surface proteinsMyogenic differentiationfactor transcriptexpressionFerrari et al.,1998SPCardiomyocyteVascularendotheliaTransplanted into lethallyirradiated mice withischemic damage tocardiac tissueImmunohistochemistryStaining forcardiomyocte marker(alpha-actin) andendothelial marker (flt-1)Jackson et al.,2001BrainNeural stemcell (NSC)AstrocyteNeuronOligodendrocyteBasic fibroblast growthfactorEpidermal growth factorDetection of antibodiesto neural cell-specificproteinsReynolds et al.,1996Doetsch et al.,1999Johansson etal., 1999NSCRed blood cellWhite blood cellTransplantation of NSCinto irradiated miceFlow cytometry analysisGenetic labeling assayDetection of antibodiesto cell surface proteinsBjornson et al.,1999D-4
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.i. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceBrain(cont.)NSC Skeletal muscle Transplantation of NSCsinto miceIn vitro co-culture withmyogenic cellsObservation ofdifferentiated skeletalmuscle cellsAnalysis of muscle cellspecificproteins andgene expressionGalli et al.,2000Embryoblastocystinner-cellmassEmbryonicstem (ES)AdipocyteRetinoic acidInsulin, T3 (thyroidhormone), and Leukemiainhibitory factor (LIF)Observation ofadipocyte differentiationMeasurement ofadipocyte enzymeactivityMeasurement ofadipocyte-specific geneexpressionDani et al.,1997ESAstrocyteGlial precursorOligodendrocyte<strong>Cells</strong> cultured inneurogenic medium withbasic fibroblast growthfactorEpidermal growth factorPlatelet-derived growthfactorTransplanted glialprecursor cells intomyelin-deficient miceObservation of spinalcord remyelinationElectron microscopyAntibodies to neural cellspecificproteinsBrustle et al.,1999ESAstrocyteMidbrain neuronNeural precursorNeuronOligodendrocyteRetinoic acidCell selection throughtransgene conferringdrug resistanceCo-culture with stromalcellsExamination of cellmorphology and neuronspecificmarkersCell-specific markersDetection of dopamineproductionBain et al.,1995Strubing et al.,1995Li et al., 1998Lee et al., 2000Kawasaki et al.,2000ESAstrocyteNeuronOligodendrocyteRetinoic acidObservation of functionalsynapsesMeasurement ofneurotransmittersSlager, et al.,1993Gottlieb, et al.,1999ESAstrocyteOligodendrocyteRetinoic acidFetal calf serum (10%)ß-mercaptoethanolAntibodies to neural cellspecificproteinsCytochemistryFraichard et al.,1995D-5
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.i. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceEmbryoblastocystinner-cellmass(cont.)ESCardiac muscleSkeletal muscleSmooth muscleRetinoic acidDimethyl sulfoxideTransplantation of musclecells into miceHistologyDetection of cell-specificproteinsCytochemistryDinsmore et al.,1996ES Cardiomyocyte LIF, retinoic acidFibroblast feeder cellsHistology andobservation of beatingcardiomyocyteDetection of specificcardiac cell-geneexpression andcardiomyocyte surfaceproteinsDoetschman etal., 1985Maltsev et al.,1993Wobus et al.,1995ES Cardiomyocyte LIFCell selection throughgenetic labeling of ESInjection of ES intomouse heartDetection of geneticallylabeled cardiomyocytesElectrophysiologicalstudiesBader et al.,2000ES Cardiomyocyte LIFPurification ofcardiomyocytes from ESculture by geneticlabeling and selectionObservation of functionalcardiomyocyte grafts inheartImmunohistologyKlug et al.,1996ES Cardiomyocyte Culture of ES with LIFSelection ofcardiomyocytes throughgenetic labelingInjection ofcardiomyocytes intomouse heartMicroscopy and cellreceptorstudiesObservation ofcardiomyocytedifferentiation andcontractilityAnalysis ofcardiomyocyte geneexpressionWestfall et al.,1997ESChondrocyte(cartilage-formingcell)BMP-2 and BMP-4Staining of maturechondrocytesMeasurement ofchondrocyte-specificgene expression andproteinsKramer et al.,2000D-6
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.i. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceEmbryoblastocystinner-cellmass(cont.)ESDendritic (immunecell)Culture on stromal celllayerInterleukin-3GranulocytemacrophagestimulatingfactorImmune-function assaysImmunophenotypingFairchild et al.,2000ESEmbryoid bodies(EBs) consisting ofstructures thatcontain tissues ofthe threeembryonic germlayers: endoderm,mesoderm, andectodermTeratocarcinomaES cultured in suspensionwithout feeder cell layerAbsence of LIFInjection of ESs into miceObservation ofdifferentiation intomultiple tissue types ofthe germ layers of blood,skeletal and cardiacmuscle, primitive gastrointestinaland neuraltissueGrowth of tumorcontaining tissues fromembryonic germ layerEvans andKaufman, 1981ES ES self–renewal LIFCulture on feeder celllayerObservation of extensiveES proliferation and selfrenewalEvans andKaufman, 1981ES Endothelial Culture on collagensubstrateHematopoietic growthfactorsSemisolid mediaEB implanted peritonealcavityObservation of capillaryformationRisau et al.,1988ESEndothelialSmooth muscleVascular progenitorCulture over collagen-IVmatrixAbsence of LIFVascular endothelialgrowth factorElectron microscopy:observation ofendothelial and smoothmuscle vascularstructuresDetection of endothelialcell marker byimmunochemistryDetection of smoothmuscle markers byimmunochemistryYamashita etal., 2000D-7
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.i. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceEmbryoblastocystinner-cellmass(cont.)ES HSC and erythroid Interleukin-6Absence of LIF and cellfeeder layerCulture on collagensubstrateHematopoietic growthfactorsSemisolid mediaBMP-4Antibodies againstsurface markersFACSImmunophenotypingWiles and Keller,1991Johansson andWiles, 1995Perkins et al.,1998ES Keratinocyte (skin) ß-mercaptoethanolImplantation of ES cellsin miceMicroscopyImmunofluorescenceObservation of skin tissuedifferentiationMeasurement of keratinBagutti et al.,1996ESLymphoidprecursorLymphocyteCulture of ES in lowoxygen concentration(5%) withouthematopoietic growthfactorsAntibodies to lymphoidcell-surface proteinsAnalysis of antibodyproduction andlymphocyte receptorsPotocnik et al.,1994ES Macrophage Interleukin-3 andmacrophage colonystimulating factorImmunophenotypingImmune-function assaysLieschke andDunn, 1995ES Mast Lethal mutations in EScellsCulture of EBs in mediacontaining interleukin-3,stem cell factorTransplantation of cellsinto mast cell-deficientmiceImmunologic- andinflammation-functiontestsAnalysis of geneexpressionJohansson andWiles, 1995Tsai et al., 2000ES Melanocyte DexamethasoneStromal cell layerSteel factorMorphology studiesReactivity to growthfactorsExpression ofmelanogenic markersYamane et al.,1999D-8
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.i. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceEmbryoblastocystinner-cellmass(cont.)ES Neuron Expression of noggincDNA in ESExpression of neuronaldetermination geneEB exposed to retinoicacidDetection of antibodiesto neuronal proteinsO’Shea, 1999ES Oligodendrocyte Retinoic acidInduced spinal cordinjuryTransplantation of ESderivedcells into spinalcord of miceDetection ofremyelination in spinalcordAntibodies tooligodendrocyte-specificproteinsLiu et al., 2000ESOsteoblast (bonecell)Co-cultured with fetalmouse osteoblastsDexamethasone, retinoicacid, ascorbic acid,ß-glycerophosphateMicroscopy; observationof mineralized bonenodulesHistochemistryButtery et al.,2001ES Pancreatic Insertion of insulin-genepromoter into ESAntibodies to cellularproteinsMeasurement of insulin,glucagon, somatostatinObservation of islet-likeorganization of cellsTransplantation of cellsinto diabetic mice withresultant lowering ofblood glucoseSoria et al.,2000ES Pancreatic islet-like Serum-free mediaAbsence of feeder-celllayerBasic fibroblast growthfactorNicotinamideDetection of antibodiesto cellular and cellsurfaceproteinsLumelsky et al.,2001ES Skeletal muscle Overexpression of insulinlikegrowth factor-2 in ESthrough gene insertionDimethyl sulfoxideObservation of myocytedifferentiationMeasurement ofmyocyte-specific geneexpression and proteinsPrelle et al.,2000D-9
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.i. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceEmbryoblastocystinner-cellmass(cont.)ES Skeletal muscle Transforming growthfactor-beta and retinoicacidES co-culture with stromalcellsFetal calf serumß-mercaptoethanolObservation of myocytedifferentiationDetection of functionalmuscle cell receptorsMeasurement ofmyocyte-specific geneexpressionSlager et al.,1993Rohwedel et al.,1994ES Smooth muscle Retinoic acid and dbcAMPCulture over collagen IVmatrixVascular endothelialgrowth factorPlatelet-derived growthfactor-BBElectron microscopyobservation of vascularstructuresDetection of smoothmuscle markers: SMA,CGA7Drab et al.,1997Yamashita etal., 2000ES Smooth muscle Platelet-derived growthfactorFACSDetection of smoothmuscle cell proteinsHirashima et al.,1999ES White blood cell Interleukin-3Transplantation of ESsinto lymphocytedeficientmiceMeasurement oflymphocyte-specificgene expressionRadioimmunoassayWiles and Keller,1991ES White blood cell Transplantation of ES cellsinto lymphocytedeficientmiceHistologyImmunophenotypingAntibodies to cellspecificproteinsRathjen et al.,1998Gonadalridge(fetal)Embryonicprimordial germcellEndodermMesodermEctoderm“Reprogramming”primordial germ cells:culture of primordialgerm cell with LIF, basicfibroblast growth factorandSteel factorHistologyImmunocytochemistryMatsui et al.,1992D-10
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.i. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceLiver HSC HSCAll blood celllineagesEnrichment of cellpopulations throughimmunoselectionPurification of CD45 +liver cellsSelection of cells withHSC markersTransplantation of HSCsinto lethally irradiatedmiceColony-forming assaysDetection of in vitrogrowth of hematopoieticcolonies by flowcytometry and cellsortingLiver-derived cellsreconstituted from bonemarrow of transplantedmiceFACSTaniguchi et al.,199PancreasPancreaticductal epithelialcellAlpha, beta, anddelta pancreaticislet<strong>Stem</strong> cells isolated fromprediabetic adult,nonobese mice<strong>Cells</strong> cultured for anextensive periodPancreatic cellstransplanted intodiabetic miceAnalysis of pancreaticcell gene expression anddifferentiation markersGlucose challenge testin vitroObservation of reversalof insulin-dependentdiabetes in mice withtransplantsRamiya et al.,2000Unselectedpancreatic cellsHepatocytePancreatic cellstransplanted into micewith liver-enzymedeficiencyDetection of normalizedliver function in miceHistological evidence ofdonor-derivedhepatocytesWang et al.,2001SkeletalmuscleMuscle Adipocyte Long-chain fatty acidsThiazolidinedionesAssays of adipocyteenzyme functionObservation ofadipocyte differentiationDetection of adipocytespecificgene expressionGrimaldi et al.,1997MuscleOsteoclast andosteocyteOsteoprogenitorExposure of donor cellsto BMP-2Retroviral transfection ofcells with vector andtransplantation intosevere combinedimmunodeficient mice(SCID)Detection of ectopicbone formationDetection of musclederivedcellsCo-localization withosteocalcin-producingcells in newly formedbone matrixBosch et al.,2000D-11
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.i. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceSkeletalmuscle(cont.)MuscleSatelliteHSCMyocyte precursorIsolation of transcriptionfactor Pax7 as a geneexpressed specifically insatellite cell-derivedmyoblastsDetection of Pax7 –/– andPax7 + muscle cells inhematopoietic andmyogenic cellsSeale et al.,2000MuscleSatellite orSPAll blood celllineagesHSCTransplant of musclederivedcells into lethallyirradiated miceObservation ofengraftment of musclecells in bone marrowAntibodies tohematopoietic cellmarkersFACSJackson et al.,1999Gussoni et al.,1999SatelliteMyocyteMyocyte precursorInduced tissue injury;mechanical anddenervation stressTranscription factorexpressionDetection of myocyteprogenitor and myocytespecificproteins andmRNA transcriptsMegeney et al.,199SpinalcordNSCAstrocyteNeuronOligodendrocyteBasic fibroblast growthfactorEpidermal growth factorDetection of antibodiesto neural cell proteinsWeiss et al.,1996D-12
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.ii.Published Reports on Isolation and Differentiation of Human Fetal Tissue Germ <strong>Cells</strong>Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceGonadalridgePrimordial germcellEmbryoid bodiesSDEC line of embryoidbody derived cellstransplanted into ratsparalyzed with a virusinduced motor neurondegenerationFunctional assessment ofrat locomotion andrighting ability (turningfrom supine to prone)Histopathologicexamination of motoraxonsImmunohistochemistry ofmature neurons: NeuN +and 68-kilodaltonneurofilamentKerr et al., 2001Primordial germcellEmbryoid bodieswith neural cells,vascularendothelium,muscle cells,endodermalderivativesLeukemia inhibitoryfactor,Basic fibroblast growthfactorClonal expression,polymerase chainreactionEthidium bromidefluorescence detectionSurface markers: 68-kilodalton neurofilament,neuron-specific enolase,tau, vimentin, humannestin,galactocerebroside, O4,SMI32Shamblott etal., 2001Primordial germcellEmbryoid bodieswith three germlayers: endoderm,mesoderm,ectodermLeukemia inhibitoryfactor,Basic fibroblast growthfactorDetection of surfacemarkers: SSEA-1, SSEA-3,SSEA-4, TRA-1-60, TRA-1-81Shamblott etal., 1998D-13
AppendicesAppendix D.iii.Published Reports on Isolation and Differentiation of Human Embryonic <strong>Stem</strong> <strong>Cells</strong>Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceHumanembryo(fromin vitrofertilization(IVF))Blastocyst innercellmassEctodermEndodermMesodermNeuronalprogenitor cellLeukemia inhibitoryfactorInjection into severecombinedimmunodeficient (SCID)miceDeveloped two lines(HES-1, HES-2)Clonal expressionPolymerase chainreactionSurface markers: SSEA-1,SSEA-4, TRA-1-60,GTCM-2Reubinoff et al.,2000Blastocyst innercellmass (H9clone line fromThomson et al.,1998)CardiomyocyteEmbryoid bodyformation(See Itskovitz-Eldor et al.,2000)Visualization ofcontracting areas inembryoid bodiesImmunohistochemistryfor cardiac myosin heavychain, alpha-actinin,desmin, cardiac troponinI, and antinatureticprotein.Assady et al.,2001Blastocyst innercellmass (H9clone line fromThomson et al.,1998)CardiomyocyteEmbryoid bodyformationPolymerase chainreaction for cardiacspecificgenes andtranscription factorsKehat et al.,2001Blastocyst innercellmass (H9clone line fromThomson et al.,1998)CardiomyocyteEndodermHematopoieticNeuronLeukemia inhibitoryfactorBasic fibroblast growthfactorCollagenase ortrypsin/EDTA to induceembryoid bodyClonal expressionPolymerase chainreactionSurface markers:gamma-globin, 68-kilodalton neurofilament,alpha-fetoprotein,albuminItskovitz-Eldor etal., 2000Blastocyst innercellmass (H9clone line fromThomson et al.,1998)Ectoderm: brain,skin, adrenalEndoderm: liver,pancreasMesoderm:muscle, bone,kidney, urogenital,heart,hematopoietic,hematopoieticBasic fibroblast growthfactor, transforminggrowth factor beta 1,activin-A, bonemorphogenic protein 4hepatocyte growthfactor, epidermal growthfactor, beta nerve growthfactor, retinoic acidClonal expressionPolymerase chainreactionSurface markersSchuldiner etal., 2000D-14
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.iii. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceHumanembryo(fromin vitrofertilization(IVF)(cont.)Blastocyst innercellmass (H9clone line fromThomson et al.,1998)Ectoderm: neuralepithelium,embryonicganglia, stratifiedsquamousepitheliumEndoderm: gutepitheliumMesoderm:cartilage, bone,smooth muscle,striated muscleInjection of cell lines intosevere combinedimmunodeficient miceLeukemia inhibitoryfactorType IV collagenaseSurface markers: SSEA-3,SSEA-4, TRA-160, TRA-181,alkaline phosphataseRadioimmunoassaydetection: alphafetoproteinand humanchorionic gonadotropinThomson et al.,1998Blastocyst innercellmass (H9clone line fromThomson et al.,1998)Pancreatic betacellEmbryoid bodyformation(See Itskovitz-Eldor et al.,2000)No leukemia inhibitoryfactor or basic fibroblastgrowth factorImmunohistochemistryfor insulinPolymerase chainreaction for insulin,IPF1/PDX1, Ngn3, betaactin,Glut-1, Glut-2,glucokinase, and Oct 4Assady et al.,2001D-15
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.iv.Published Reports on Adult Isolation and Human Differentiation of <strong>Stem</strong> Human Embryonic <strong>Cells</strong>Carcinoma <strong>Stem</strong> <strong>Cells</strong>Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceTeratocarcinomaEmbryoniccarcinoma (EC)Endodermalprogenitor cellAbsence of feeder celllayerBone morphogeneticprotein-2Retinoic acidAnalysis of stem cellmarker-gene transcriptionImmunochemistryImmunofluorescenceRoach et al.,1994Pera andHerszfeld, 1998EC Neuron EC transplanted intomouse brainObservation of functionalsynapsesImmunochemistryTrojanowski etal., 1993ECGlialNeuronRetinoic acidMeasurement of mRNAfor GABA(A) receptorchloridecomplexRecording of whole-cellvoltage-clampmeasurements indifferentiated cells in thepresence of GABA(A)receptor antagonists andactivators (bicucullineand flurazepam,respectively)Reynolds et al.,1994ECGlialNeuronRetinoic acidDetection of neurons withHNK-1 antibodyMeasurement ofacetylcholine synthesisand detection of highaffinityuptake sites forGABAMcBurney et al.,1988EC Neuron Retinoic acid Morphology andhistologyAnalysis of neuronspecificproteinsAndrews, 1984D-16
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.iv. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceTeratocarcinomaorteratomaECTumors containingtissue types fromendoderm,mesoderm, andectodermBone morphogeneticprotein-7EC cells cultured withoutfeeder cell layerTransplantation of ECcells into miceMorphology, histology,and cell stainingObservation of tissuetypes from endoderm,mesoderm, andectodermObservation of extendedself-renewal of EC cellsAnalysis of chromosomesand specific genesDetection of cell-specificproteinsCytochemical assayAndrews et al.,1984Thompson etal., 1984Pera, 1989D-17
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.v.Published Reports Adult on Isolation Human and Differentiation <strong>Stem</strong> of <strong>Cells</strong> Human Adult <strong>Stem</strong> <strong>Cells</strong>Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceBloodCirculatorySkeletalAdipocyteOsteocyteLeukemia inhibitoryfactor (LIF)Transplantation of stemcells into bg-nu-xidimmunocompromisedmiceAntibody labelingPolymerase chainreactionKuznetsov, 2001BonemarrowAngioblast(endothelialprecursor)Mature endotheliaand newly formedblood vesselsAngioblasts isolated bymobilizing peripheralblood with granulocytecolonystimulating factorAngioblasts injected intorats with experimentalmyocardial infarctionObservation ofneovascularization withinmyocardium fromtransplanted cellsDetection of improvedcardiac function inexperimental animalsKocher et al.,2001Hematopoieticstem cell (HSC)HepatocyteCholangiocyteBone marrowtransplantationProbed for presence andfunction of Ychromosome-containingliver cellsMeasured expression ofliver-specific proteinsImmunochemistryAlison et al.,2000Theise et al.,2000Human marrowstromalStromal-derivedcell engrafted inrat brainIsolation of marrowstromal cell from humanvolunteers; injection ofstromal cell into rat brainObservation ofengraftment, migration,and survival of stromalderivedcell in rat brainObservation of loss ofstromal cell functionsAntibodies to cell-surfaceproteinsAzizi et al., 1998Mesenchymalstem cell(MSC)AdipocyteChondrocyteOsteocyteFetal bovine serum,dexamethasone,isobutylxanthine, insulin,ascorbate,indomethacin,transforming growthfactor-B3, and glycerolphosphateHistology andimmunofluorescenceDetection of lipids andspecific enzyme activityof adipocytes andosteocytesSpecific staining forchondrocytesPittenger et al.,1999D-18
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.v. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceBonemarrow(cont.)MSC Neuron Prolonged expansion ofMSCs as undifferentiatedcells-mercaptoethanol(BME)Butylated hydroxyanisole(BHA)HistologyDetection of numerousneuron-specific proteinsvia staining and antibodybindingWoodbury etal., 2000MSC Neuron MSCs cultured with fetalrat brain cellsEpidermal growth factorBrain-derivedneurotrophic factorDetection of nestin andnestin-gene expressionDetection of neuronspecificproteinsSanchez-Ramoset al., 2000MSCAdipocyteBone marrowstromal cellCardiomyocyteChondrocyteMyocyteThymic stromal cellMSCs isolated from bonemarrowTransplantation of MSCsinto fetal sheepAnalysis of human geneexpression in sheeptissuesConfirmed presence ofhuman cells byimmunohistochemistryLiechty et al.,2000Bonemarrow(fetal)HSCHSCRed blood celllineagesWhite blood celllineagesEnrichment ofhematopoietic cellpopulations by cellselectionTransplantation of bonemarrow and thymus cellsinto miceEstablishment of longtermmultilineagecultures ofhematopoietic coloniesFluorescence-activatedcell sorting (FACS)Engraftment ofhematopoietic cells inmiceBaum et al.,1992BrainNeural stemcell (NSC)Muscle cellExposure of NSCs tomyoblastsDissociation of NSCclustersTransplantation of humanNSCs into mice withinduced muscle injuryObservation ofdifferentiated skeletalmuscle cells fromprimary and culturederivedNSCsDemonstration of NSCengraftment in mice bydetection of expressionof specific genesGalli et al.,2000D-19
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.v. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceBrain(adultandneonatal)Neuralprogenitor cell(NPC)AstrocyteNeuronOligodendrocyteNPCs cultured inmedium containingglutamine, amphotericin-B, antibiotics, fetal calfserum, basic fibroblastgrowth factor, epidermalgrowth factor, andplatelet-derived growthfactor ABTransplantation of humancentral nervous systemstem cells (hCNS-SCs)into miceObservation of functionalengraftment of NPCs intomouse brainAntibody labeling ofneuronal cell-surfaceproteinsPalmer et al.,2001Brain(fetal)Human centralnervous systemstem cell(hCNS-SC)AstrocyteNeuronOligodendrocyteFibroblast growth factor-2, epidermal growthfactor, lymphocyteinhibitory factor, neuralsurvival factor-1, brainderivedand glial-derivedneurotrophic factorsObservation ofneurosphere formationand self-renewal ofhCNS-SCsDemonstration ofengraftment,proliferation, migration,and neural differentiationof hCNS-SCsFACSUchida et al.,2000FatStromalvascular cellfraction ofprocessedlipoaspirateAdipocyteprecursorOsteocyteprecursorChondrocyteprecursorMyocyte precursorCo-cultured with mouseadipocytes,isobutylmethylxanthine,dexamethasoneCo-cultured with humanosteoblasts, insulin,indomethacin,antibiotic/antimycoticdexamethasone,ascorbate, b-glycerophosphate,antibiotic/antimycoticCo-cultured with humanskeletal myocytes, insulin,transforming growthfactor-B, ascorbate,antibiotic/antimycoticdexamethasone,hydrocortisone,antibiotic/antimycoticStaining for lipidaccumulationStaining for alkalinephosphatase activityStaining for boneformationStaining forproteoglycan-rich matrixAntibody binding tocollagen IIVisualization ofmultinucleationStaining for muscleprotein: myosinAntibody binding toMyoD1Zuk et al., 2001D-20
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.v. (cont.)Origin Cell Types Differentiation Methods ofTissue Cell Type Developed Conditions Characterization ReferenceLiver(fetal)HSCHematopoieticprogenitor cell(HPC)Red blood celllineagesWhite blood celllineagesCo-culture of HSCs withmouse stromal cellsImplantation of fetalhematopoietic liver cellsinto immunocompromisedmiceDemonstration ofdifferentiation into redand white blood celllineages through colonyformingassays anddetection of surfacemarkers characteristic ofthe hematopoieticsystemMcCune et al.,1988Namikawa etal., 1990PancreasNestin-positiveislet-derivedprogenitor cell(NIP)PancreaticHepaticNIPs obtained frompancreatic islets andcultured for extendedperiodsObservation of extendedproliferative, selfrenewing,andmultipotent capacityExpression of hepaticand exocrine pancreaticmarkersDemonstration of ductaland endocrinepancreatic featuresProduction of insulin andglucagonsZulewski et al.,2000UmbilicalcordbloodHPCMost red and whiteblood cell lineagesCollection and sortingStimulation with colonystimulatingfactors andinterleukin-3Demonstration ofmultipotent progenitor,granulocytemacrophage,anderythroid cell linesBroxmeyer etal., 1989HSCMesenchymalprogenitor cell(MPC)Most red and whiteblood cell lineagesOsteoblastsAdipocytesMixtures ofdexamethasone, ß-glycerol, ascorbate,insulin, isobutylmethylxanthine,andindomethacinCell morphologyCytochemical analysis ofosteoblast andadipocyte productsImmunophenotypingErices et al.,1999D-21
Appendix D: <strong>Stem</strong> Cell TablesAppendix D.vi.REFERENCES1. Alison, M.R., Poulsom, R., Jeffery, R., Dhillon, A.P., Quaglia,A., Jacob, J., Novelli, M., Prentice, G., Williamson, J., andWright, N.A. (2000). Hepatocytes from non-hepatic adultstem cells. Nature. 406, 257.2. Andrews, P.W., Damjanov, I., Simon, D., Banting, G.S., Carlin,C., Dracopoli, N.C., and Fogh, J. (1984). Pluripotent embryonalcarcinoma clones derived from the human teratocarcinomacell line Tera-2. Differentiation in vivo and in vitro.Lab. Invest. 50, 147-162.3. Assady, S., Maor, G., Amit, M., Itskovitz-Eldor, J., Skorecki, K.L.,and Tzukerman, M. (2001). Insulin production by humanembryonic stem cells. Diabetes, 50,http://www.diabetes.org/Diabetes_Rapids/Suheir_Assady_06282001.pdf.4. Azizi, S.A., Stokes, D., Augelli, B.J., DiGirolamo, C., andProckop, D.J. (1998). Engraftment and migration of humanbone marrow stromal cells implanted in the brains of albinorats—similarities to astrocyte grafts. Proc. Natl. Acad. Sci.U. S. A. 95, 3908-3913.5. Bader, A., Al Dubai, H., and Weitzer, G. (2000). Leukemiainhibitory factor modulates cardiogenesis in embryoid bodiesin opposite fashions. Circ. Res. 86, 787-794.6. Bagutti, C., Wobus, A.M., Fassler, R., and Watt, F.M. (1996).Differentiation of embryonal stem cells into keratinocytes:comparison of wild-type and ß(1) integrin-deficient cells.Dev. Biol. 179, 184-196.7. Bain, G., Kitchens, D., Yao, M., Huettner, J.E., and Gottlieb,D.I. (1995). Embryonic stem cells express neuronal propertiesin vitro. Dev. Biol. 168, 342-357.8. Baum, C.M., Weissman, I.L., Tsukamoto, A.S., Buckle, A.M.,and Peault, B. (1992). Isolation of a candidate humanhematopoietic stem-cell population. Proc. Natl. Acad. Sci.U. S. A. 89, 2804-2808.9. Bittner, R.E., Schofer, C., Weipoltshammer, K., Ivanova, S.,Streubel, B., Hauser, E., Freilinger, M., Hoger, H., Elbe-Burger,A., and Wachtler, F. (1999). Recruitment of bone-marrowderivedcells by skeletal and cardiac muscle in adult dystrophicmdx mice. Anat. Embryol. (Berl) 199, 391-396.10. Bjornson, C.R., Rietze, R.L., Reynolds, B.A., Magli, M.C., andVescovi, A.L. (1999). Turning brain into blood: a hematopoieticfate adopted by adult neural stem cells in vivo.Science. 283, 534-537.11. Bosch, P., Musgrave, D.S., Lee, J.Y., Cummins, J., Shuler, F.,Ghivizzani, S.C., Evans, C., Robbins, P.D., and Huard, J.(2000). Osteoprogenitor cells within skeletal muscle. J.Orthop. Res. 18, 933-944.12. Brazelton, T.R., Rossi, F.M., Keshet, G.I., and Blau, H.M.(2000). From marrow to brain: expression of neuronal phenotypesin adult mice. Science. 290, 1775-1779.13. Broxmeyer, H.E., Douglas, G.W., Hangoc, G., Cooper, S.,Bard, J., English, D., Arny, M., Thomas, L., and Boyse, E.A.(1989). Human umbilical cord blood as a potential sourceof transplantable hematopoietic stem/progenitor cells.Proc. Natl. Acad. Sci. U. S. A. 86, 3828-3832.14. Brustle, O., Jones, K.N., Learish, R.D., Karram, K., Choudhary,K., Wiestler, O.D., Duncan, I.D., and McKay, R.D. (1999).Embryonic stem cell-derived glial precursors: a source ofmyelinating transplants. Science. 285, 754-756.15. Buttery, L.D., Bourne, S., Xynos, J.D., Wood, H., Hughes, F.J.,Hughes, S.P., Episkopou, V., and Polak, J.M. (2001).Differentiation of osteoblasts and in vitro bone formationfrom murine embryonic stem cells. Tissue Eng. 7, 89-99.16. Dani, C., Smith, A.G., Dessolin, S., Leroy, P., Staccini, L.,Villageois, P., Darimont, C., and Ailhaud, G. (1997).Differentiation of embryonic stem cells into adipocytes invitro. J. Cell Sci. 110, 1279-1285.17. Dinsmore, J., Ratliff, J., Deacon, T., Pakzaban, P., Jacoby, D.,Galpern, W., and Isacson, O. (1996). Embryonic stem cellsdifferentiated in vitro as a novel source of cells for transplantation.Cell Transplant. 5, 131-143.18. Doetsch, F., Caille, I., Lim, D.A., Garcia-Verdugo, J.M., andAlvarez-Buylla, A. (1999). Subventricular zone astrocytes areneural stem cells in the adult mammalian brain. Cell. 97,703-716.19. Doetschman, T., Eistetter, H., Katz, M., Schmit, W., andKemler, R. (1985). The in vitro development of blastocystderivedembryonic stem cell lines: formation of visceralyolk sac, blood islands and myocardium. J. Embryol. Exp.Morph. 87, 27-45.20. Drab, M., Haller, H., Bychkov, R., Erdmann, B., Lindschau, C.,Haase, H., Morano, I., Luft, F.C., and Wobus, A.M. (1997).From totipotent embryonic stem cells to spontaneouslycontracting smooth muscle cells: a retinoic acid and dbcAMPin vitro differentiation model. FASEB J. 11, 905-915.21. Eglitis, M.A. and Mezey, E. (1997). Hematopoietic cells differentiateinto both microglia and macroglia in the brainsof adult mice. Proc. Natl. Acad. Sci. U. S. A. 94, 4080-4085.22. Erices, A., Conget, P., and Minguell, J.J. (1999).Mesenchymal progenitor cells in human umbilical cordblood. Br. J. Haematol. 109, 235-242.23. Evans, M.J. and Kaufman, M.H. (1981). Establishment in cultureof pluripotential cells from mouse embryos. Nature.292, 154-156.24. Fairchild, P.J., Brook, F.A., Gardner, R.L., Graca, L., Strong, V.,Tone, Y., Tone, M., Nolan, K.F., and Waldmann, H. (2000).Directed differentiation of dendritic cells from mouseembryonic stem cells. Curr. Biol. 10, 1515-1518.25. Ferrari, G., Cusella-De Angelis, G., Coletta, M., Paolucci, E.,Stornaiuolo, A., Cossu, G., and Mavilio, F. (1998). Muscleregeneration by bone marrow-derived myogenic progenitors.Science. 279, 1528-1530.D-22
Appendix D: <strong>Stem</strong> Cell Tables26. Fraichard, A., Chassande, O., Bilbaut, G., Dehay, C.,Savatier, P., and Samarut, J. (1995). In vitro differentiation ofembryonic stem cells into glial cells and functional neurons.J. Cell Sci. 108, 3181-3188.27. Friedenstein, A.J., Gorskaja, U.F., and Kulagina, N.N. (1976).Fibroblast precursors in normal and irradiated mousehematopoietic organs. Exp. Hematol. 4, 267-274.28. Galli, R., Borello, U., Gritti, A., Minasi, M.G., Bjornson, C.,Coletta, M., Mora, M., De Angelis, M.G., Fiocco, R., Cossu,G., and Vescovi, A.L. (2000). Skeletal myogenic potential ofhuman and mouse neural stem cells. Nat. Neurosci. 3,986-991.29. Gottlieb, D.I. and Huettner, J.E. (1999). An in vitro pathwayfrom embryonic stem cells to neurons and glia. <strong>Cells</strong>Tissues Organs. 165, 165-172.30. Grimaldi, P.A., Teboul, L., Inadera, H., Gaillard, D., and Amri,E.Z. (1997). Trans-differentiation of myoblasts to adipoblasts:triggering effects of fatty acids and thiazolidinediones.Prostaglandins. Leukot. Essent. Fatty. Acids. 57, 71-75.31. Gussoni, E., Soneoka, Y., Strickland, C.D., Buzney, E.A., Khan,M.K., Flint, A.F., Kunkel, L.M., and Mulligan, R.C. (1999).Dystrophin expression in the mdx mouse restored by stemcell transplantation. Nature. 401, 390-394.32. Hirashima, M., Kataoka, H., Nishikawa, S., Matsuyoshi, N.,and Nishikawa, S. (1999). Maturation of embryonic stemcells into endothelial cells in an in vitro model of vasculogenesis.Blood. 93, 1253-1263.33. Itskovitz-Eldor, J., Schuldiner, M., Karsenti, D., Eden, A.,Yanuka, O., Amit, M., Soreq, H., and Benvenisty, N. (2000).Differentiation of human embryonic stem cells into embryoidbodies comprising the three embryonic germ layers.Mol. Med. 6, 88-95.34. Jackson, K.A., Mi, T., and Goodell, M.A. (1999).Hematopoietic potential of stem cells isolated from murineskeletal muscle. Proc. Natl. Acad. Sci. U. S. A. 96, 14482-14486.35. Jackson, K., Majka SM, Wang H, Pocius J, Hartley CJ,Majesky MW, Entman ML, Michael LH, Hirschi KK, and andGoodell MA (2001). Regeneration of ischemic cardiacmuscle and vascular endothelium by adult stem cells. J.Clin. Invest. 107, 1-8.36. Johansson, B.M. and Wiles, M.V. (1995). Evidence forinvolvement of activin A and bone morphogenetic protein4 in mammalian mesoderm and hematopoietic development.Mol. Cell Biol. 15, 141-151.37. Johansson, C.B., Momma, S., Clarke, D.L., Risling, M.,Lendahl, U., and Frisen, J. (1999). Identification of a neuralstem cell in the adult mammalian central nervous system.Cell. 96, 25-34.38. Kawasaki, H., Mizuseki, K., Nishikawa, S., Kaneko, S., Kuwana,Y., Nakanishi, S., Nishikawa, S.I., and Sasai, Y. (2000).Induction of midbrain dopaminergic neurons from ES cellsby stromal cell-derived inducing activity. Neuron. 28, 31-40.39. Kehat, I., Kenyagin-Karsenti, D., Druckmann, M., Segev, H.,Amit, M., Gepstein, A., Livne, E., Binah, O., Itskovitz-Eldor, J.,and Gepstein, L. (2001). Human embryonic stem cells candifferentiate into myocytes portraying cardiomyocytic structuraland functional properties. J. Clin. Invest. (in press).40. Kerr, D.A., Llado, J., Shamblott, M., Maragakis, N., Irani, D.N.,Dike, S., Sappington, A., Gearhart, J., and Rothstein, J.(2001). Human embryonic germ cell derivatives facillitatemotor recovery of rats with diffuse motor neuron injury.41. Klug, M.G., Soonpaa, M.H., Koh, G.Y., and Field, L.J. (1996).Genetically selected cardiomyocytes from differentiatingembryonic stem cells form stable intracardiac grafts. J.Clin. Invest. 98, 216-224.42. Kocher, A.A., Schuster, M.D., Szabolcs, M.J., Takuma, S.,Burkhoff, D., Wang, J., Homma, S., Edwards, N.M., andItescu, S. (2001). Neovascularization of ischemic myocardiumby human bone-marrow-derived angioblasts preventscardiomyocyte apoptosis, reduces remodeling andimproves cardiac function. Nat. Med. 7, 430-436.43. Kopen, G.C., Prockop, D.J., and Phinney, D.G. (1999).Marrow stromal cells migrate throughout forebrain andcerebellum, and they differentiate into astrocytes afterinjection into neonatal mouse brains. Proc. Natl. Acad.Sci. U. S. A. 96, 10711-10716.44. Kramer, J., Hegert, C., Guan, K., Wobus, A.M., Muller, P.K.,and Rohwedel, J. (2000). Embryonic stem cell-derivedchondrogenic differentiation in vitro: activation by BMP-2and BMP-4. Mech. Dev. 92, 193-205.45. Krause, D.S., Theise, N.D., Collector, M.I., Henegariu, O.,Hwang, S., Gardner, R., Neutzel, S., and Sharkis, S.J. (2001).Multi-organ, multi-lineage engraftment by a single bonemarrow-derived stem cell. Cell. 105, 369-377.46. Kuznetsov, S.A., Mankani, M.H., Gronthos, S., Satomura, K.,Bianco, P., and Robey P.G. (2001). Circulating skeletal stemcells. J. Cell Biol. 153, 1133-40.47. Lagasse, E., Connors, H., Al Dhalimy, M., Reitsma, M.,Dohse, M., Osborne, L., Wang, X., Finegold, M., Weissman,I.L., and Grompe, M. (2000). Purified hematopoietic stemcells can differentiate into hepatocytes in vivo. Nat. Med.6, 1229-1234.48. Lee, S.H., Lumelsky, N., Studer, L., Auerbach, J.M., andMcKay, R.D. (2000). Efficient generation of midbrain andhindbrain neurons from mouse embryonic stem cells. Nat.Biotechnol. 18, 675-679.49. Li, M., Pevny, L., Lovell-Badge, R., and Smith, A. (1998).Generation of purified neural precursors from embryonicstem cells by lineage selection. Curr. Biol. 8, 971-974.50. Liechty, K.W., MacKenzie, T.C., Shaaban, A.F., Radu, A.,Moseley, A.B., Deans, R., Marshak, D.R., and Flake, A.W.(2000). Human mesenchymal stem cells engraft anddemonstrate site-specific differentiation after in utero transplantationin sheep. Nat. Med. 6, 1282-1286.D-23
Appendix D: <strong>Stem</strong> Cell Tables51. Lieschke, G.J. and Dunn, A.R. (1995). Development of functionalmacrophages from embryonal stem cells in vitro.Exp. Hematol. 23, 328-334.52. Liu, S., Qu, Y., Stewart, T.J., Howard, M.J., Chakrabortty, S.,Holekamp, T.F., and McDonald, J.W. (2000). Embryonicstem cells differentiate into oligodendrocytes and myelinatein culture and after spinal cord transplantation. Proc.Natl. Acad. Sci. U. S. A. 97, 6126-6131.53. Lumelsky, N., Blondel, O., Laeng, P., Velasco, I., Ravin, R.,and McKay, R. (2001). Differentiation of Embryonic <strong>Stem</strong><strong>Cells</strong> to Insulin-Secreting Structures Similiar to PancreaticIslets. Science. 292, 1389-1394.54. Makino, S., Fukuda, K., Miyoshi, S., Konishi, F., Kodama, H.,Pan, J., Sano, M., Takahashi, T., Hori, S., Abe, H., Hata, J.,Umezawa, A., and Ogawa, S. (1999). Cardiomyocytes canbe generated from marrow stromal cells in vitro. J. Clin.Invest. 103, 697-705.55. Maltsev, V.A., Rohwedel, J., Hescheler, J., and Wobus, A.M.(1993). Embryonic stem cells differentiate in vitro into cardiomyocytesrepresenting sinusnodal, atrial and ventricularcell types. Mech. Dev. 44, 41-50.56. Matsui, Y., Zsebo, K., and Hogan, B.L. (1992). Derivation ofpluripotential embryonic stem cells from murine primordialgerm cells in culture. Cell. 70, 841-847.57. McBurney, M.W., Reuhl, K.R., Ally, A.I., Nasipuri, S., Bell, J.C.,and Craig, J. (1988). Differentiation and maturation ofembryonal carcinoma-derived neurons in cell culture. J.Neurosci. 8, 1063-1073.58. McCune, J.M., Namikawa, R., Kaneshima, H., Shultz, L.D.,Lieberman, M., and Weissman, I.L. (1988). The SCID-humouse: murine model for the analysis of human hematolymphoiddifferentiation and function. Science. 241,1632-1639.59. Megeney, L.A., Kablar, B., Garrett, K., Anderson, J.E., andRudnicki, M.A. (1996). MyoD is required for myogenic stemcell function in adult skeletal muscle. Genes Dev. 10, 1173-1183.60. Mezey, E., Chandross, K.J., Harta, G., Maki, R.A., andMcKercher, S.R. (2000). Turning blood into brain: cellsbearing neuronal antigens generated in vivo from bonemarrow. Science. 290, 1779-1782.61. Morrison, S.J., Uchida, N., and Weissman, I.L. (1995). Thebiology of hematopoietic stem cells. Annu. Rev. Cell. Dev.Biol. 11, 35-71.62 Namikawa, R., Weilbaecher, K.N., Kaneshima, H., Yee, E.J.,and McCune, J.M. (1990). Long-term human hematopoiesisin the SCID-hu mouse. J. Exp. Med. 172, 1055-1063.63. O’Shea, K.S. (1999). Embryonic stem cell models of development.Anat. Rec. 257, 32-41.64. Orlic, D., Kajstura, J., Chimenti, S., Jakoniuk, I., Anderson,S.M., Li, B., Pickel, J., McKay, R., Nadal-Ginard, B., Bodine,D.M., Leri, A., and Anversa, P. (2001). Bone marrow cellsregenerate infarcted myocardium. Nature. 410, 701-705.65. Palmer, T.D., Schwartz, P.H., Taupin, P., Kaspar, B., Stein, S.A.,and Gage, F.H. (2001). Progenitor cells from human brainafter death. Nature. 411, 42-43.66. Pera, M.F., Cooper, S., Mills, J., and Parrington, J.M. (1989).Isolation and characterization of a multipotent clone ofhuman embryonal carcinoma cells. Differentiation. 42,10-23.67. Pera, M.F. and Herszfeld, D. (1998). Differentiation of humanpluripotent teratocarcinoma stem cells induced by bonemorphogenetic protein-2. Reprod. Fertil. Dev. 10, 551-555.68. Pereira, R.F., Halford, K.W., O’Hara, M.D., Leeper, D.B.,Sokolov, B.P., Pollard, M.D., Bagasra, O., and Prockop, D.J.(1995). Cultured adherent cells from marrow can serve aslong-lasting precursor cells for bone, cartilage, and lungin irradiated mice. Proc. Natl. Acad. Sci. U. S. A. 92,4857-4861.69. Perkins, A.C. (1998). Enrichment of blood from embryonicstem cells in vitro. Reprod. Fertil. Dev. 10, 563-572.70. Petersen, B.E., Bowen, W.C., Patrene, K.D., Mars, W.M.,Sullivan, A.K., Murase, N., Boggs, S.S., Greenberger, J.S., andGoff, J.P. (1999). Bone marrow as a potential source ofhepatic oval cells. Science. 284, 1168-1170.71. Pittenger, M.F., Mackay, A.M., Beck, S.C., Jaiswal, R.K.,Douglas, R., Mosca, J.D., Moorman, M.A., Simonetti, D.W.,Craig, S., and Marshak, D.R. (1999). Multilineage potentialof adult human mesenchymal stem cells. Science.284, 143-147.72. Potocnik, A.J., Nielsen, P.J., and Eichmann, K. (1994). In vitrogeneration of lymphoid precursors from embryonic stemcells. EMBO J. 13, 5274-5283.73. Prelle, K., Wobus, A.M., Krebs, O., Blum, W.F., and Wolf, E.(2000). Overexpression of insulin-like growth factor-II inmouse embryonic stem cells promotes myogenic differentiation.Biochem. Biophys. Res. Commun. 277, 631-638.74. Prockop, D.J. (1997). Marrow stromal cells as stem cells fornonhematopoietic tissues. Science. 276, 71-74.75. Ramiya, V.K., Maraist, M., Arfors, K.E., Schatz, D.A., Peck,A.B., and Cornelius, J.G. (2000). Reversal of insulin-dependentdiabetes using islets generated in vitro from pancreaticstem cells. Nat. Med. 6, 278-282.76. Rathjen, P.D., Lake, J., Whyatt, L.M., Bettess, M.D., andRathjen, J. (1998). Properties and uses of embryonic stemcells: prospects for application to human biology andgene therapy. Reprod. Fertil. Dev. 10, 31-47.77. Reubinoff, B.E., Pera, M.F., Fong, C.Y., Trounson, A., andBongso, A. (2000). Embryonic stem cell lines from humanblastocysts: somatic differentiation in vitro. Nat. Biotechnol.18, 399-404.78. Reynolds, B.A. and Weiss, S. (1996). Clonal and populationanalyses demonstrate that an EGF-responsive mammalianembryonic CNS precursor is a stem cell. Dev. Biol. 175,1-13.D-24
Appendix D: <strong>Stem</strong> Cell Tables79. Reynolds, J.N., Ryan, P.J., Prasad, A., and Paterno, G.D.(1994). Neurons derived from embryonal carcinoma (P19)cells express multiple GABA(A) receptor subunits and fullyfunctional GABA(A) receptors. Neurosci. Lett. 165, 129-132.80. Risau, W., Sariola, H., Zerwes, H.G., Sasse, J., Ekblom, P.,Kemler, R., and Doetschman, T. (1988). Vasculogenesis andangiogenesis in embryonic-stem-cell-derived embryoidbodies. Development. 102, 471-478.81. Roach, S., Schmid, W., and Pera, M.F. (1994). Hepatocytictranscription factor expression in human embryonal carcinomaand yolk sac carcinoma cell lines: expression ofHNF-3 in models of early endodermal cell differentiation.Exp. Cell. Res. 215, 189-198.82. Rohwedel, J., Maltsev, V., Bober, E., Arnold, H.H., Hescheler,J., and Wobus, A.M. (1994). Muscle cell differentiation ofembryonic stem cells reflects myogenesis in vivo: developmentallyregulated expression of myogenic determinationgenes and functional expression of ionic currents. Dev. Biol.164, 87-101.83. Sanchez-Ramos, J., Song, S., Cardozo-Pelaez, F., Hazzi, C.,Stedeford, T., Willing, A., Freeman, T.B., Saporta, S., Janssen,W., Patel, N., Cooper, D.R., and Sanberg, P.R. (2000). Adultbone marrow stromal cells differentiate into neural cells invitro. Exp. Neurol. 164, 247-256.84. Schuldiner, M., Yanuka, O., Itskovitz-Eldor, J., Melton, D., andBenvenisty, N. (2000). Effects of eight growth factors on thedifferentiation of cells derived from human embryonic stemcells. Proc. Natl. Acad. Sci. U. S. A. 97, 11307-11312.85. Seale, P., Sabourin, L.A., Girgis-Gabardo, A., Mansouri, A.,Gruss, P., and Rudnicki, M.A. (2000). Pax7 is required for thespecification of myogenic satellite cells. Cell. 102, 777-786.86. Shamblott, M.J., Axelman, J., Littlefield, J.W., Blumenthal,P.D., Huggins, G.R., Cui, Y., Cheng, L., and Gearhart, J.D.(2001). Human embryonic germ cell derivatives express abroad range of develpmentally distinct markers and proliferateextensively in vitro. Proc. Natl. Acad. Sci. U. S. A.98, 13-118.87. Shamblott, M.J., Axelman, J., Wang, S., Bugg, E.M.,Littlefield, J.W., Donovan, P.J., Blumenthal, P.D., Huggins,G.R., and Gearhart, J.D. (1998). Derivation of pluripotentstem cells from cultured human primordial germ cells.Proc. Natl. Acad. Sci. U. S. A. 95, 13726-13731.88. Slager, H.G., Van Inzen, W., Freund, E., Van den Eijnden-VanRaaij A.J.M., and Mummery, C.L. (1993). Transforminggrowth factor-beta in the early mouse embryo: implicationsfor the regulation of muscle formation and implantation.Dev. Genet. 14, 212-224.89. Soria, B., Roche, E., Berna, G., Leon-Quinto, T., Reig, J.A.,and Martin, F. (2000). Insulin-secreting cells derived fromembryonic stem cells normalize glycemia in streptozotocininduceddiabetic mice. Diabetes. 49, 157-162.90. Spangrude, G.J., Smith, L., Uchida, N., Ikuta, K., Heimfeld,S., Friedman, J., and Weissman, I.L. (1991). Mousehematopoietic stem cells. Blood. 78, 1395-1402.91. Strubing, C., Ahnert-Hilger, G., Shan, J., Wiedenmann, B.,Hescheler, J., and Wobus, A.M. (1995). Differentiation ofpluripotent embryonic stem cells into the neuronal lineagein vitro gives rise to mature inhibitory and excitatoryneurons. Mech. Dev. 53, 275-287.92. Taniguchi, H., Toyoshima, T., Fukao, K., and Nakauchi, H.(1996). Presence of hematopoietic stem cells in the adultliver. Nat. Med. 2, 198-203.93. Theise, N.D., Nimmakayalu, M., Gardner, R., Illei, P.B.,Morgan, G., Teperman, L., Henegariu, O., and Krause, D.S.(2000). Liver from bone marrow in humans. Hepatology.32, 11-16.94. Thompson, S., Stern, P.L., Webb, M., Walsh, F.S., Engstrom,W., Evans, E.P., Shi, W.K., Hopkins, B., and Graham, C.F.(1984). Cloned human teratoma cells differentiate intoneuron-like cells and other cell types in retinoic acid. J.Cell. Sci. 72, 37-64.95. Thomson, J.A., Itskovitz-Eldor, J., Shapiro, S.S., Waknitz, M.A.,Swiergiel, J.J., Marshall, V.S., and Jones, J.M. (1998).Embryonic stem cell lines derived from human blastocysts.Science. 282, 1145-1147.96. Tomita, S., Li, R.K., Weisel, R.D., Mickle, D.A., Kim, E.J., Sakai,T., and Jia, Z.Q. (1999). Autologous transplantation ofbone marrow cells improves damaged heart function672. Circulation. 100 (Suppl. II), 11247-11256.97. Trojanowski, J.Q., Mantione, J.R., Lee, J.H., Seid, D.P., You,T., Inge, L.J., and Lee, V.M. (1993). Neurons derived from ahuman teratocarcinoma cell line establish molecular andstructural polarity following transplantation into the rodentbrain. Exp. Neurol. 122, 283-294.98. Tsai, M., Wedemeyer, J., Ganiatsas, S., Tam, S.Y., Zon, L.I.,and Galli, S.J. (2000). In vivo immunological function ofmast cells derived from embryonic stem cells: anapproach for the rapid analysis of even embryonic lethalmutations in adult mice in vivo. Proc. Natl. Acad. Sci.U. S. A. 97, 9186-9190.99. Uchida, N., Buck, D.W., He, D., Reitsma, M.J., Masek, M.,Phan, T.V., Tsukamoto, A.S., Gage, F.H., and Weissman, I.L.(2000). Direct isolation of human central nervous systemstem cells. Proc. Natl. Acad. Sci. U. S. A. 97, 14720-14725.100. Wakitani, S., Saito, T., and Caplan, A.I. (1995). Myogeniccells derived from rat bone marrow mesenchymal stemcells exposed to 5-azacytidine 754. Muscle. Nerve. 18,1417-1426.101. Wang, X., Al-Dhalimy, M., Lagasse, E., Finegold, M., andGrompe, M. (2001). Liver repopulation and correction ofmetabolic liver disease by transplanted adult mouse pancreaticcells. Am. J. Pathol. 158, 571-579.102. Weiss, S., Dunne, C., Hewson, J., Wohl, C., Wheatley, M.,Peterson, A.C., and Reynolds, B.A. (1996). Multipotent CNSstem cells are present in the adult mammalian spinalcord and ventricular neuroaxis. J. Neurosci. 16,7599-7609.D-25
Appendix D: <strong>Stem</strong> Cell Tables103. Westfall, M.V., Pasyk, K.A., Yule, D.I., Samuelson, L.C., andMetzger, J.M. (1997). Ultrastructure and cell-cell couplingof cardiac myocytes differentiating in embryonic stemcell cultures. Cell. Motil. Cytoskeleton. 36, 43-54.104. Wiles, M.V. and Keller, G. (1991). Multiple hematopoieticlineages develop from embryonic stem (ES) cells in culture.Development. 111, 259-267.105. Wobus, A.M., Rohwedel, J., Maltsev, V., and Hescheler, J.(1995). Development of cardiomyocytes expressing cardiac-specificgenes, action potentials, and ionic channelsduring embryonic stem cell-derived cardiogenesis. Ann.N. Y. Acad. Sci. 752, 460-469.106. Woodbury, D., Schwarz, E.J., Prockop, D.J., and Black, I.B.(2000). Adult rat and human bone marrow stromal cellsdifferentiate into neurons. J. Neurosci. Res. 61, 364-370.108. Yamashita, J., Itoh, H., Hirashima, M., Ogawa, M.,Nishikawa, S., Yurugi, T., Naito, M., Nakao, K., andNishikawa, S. (2000). Flk1-positive cells derived fromembryonic stem cells serve as vascular progenitors.Nature. 408, 92-96.109. Zuk, P.A., Zhu, M., Mizuno, H., Huang, J., Futrell, J.W., Katz,A.J., Benhaim, P., Lorenz, H.P., and Hedrick, M.H. (2001).Multilineage cells from human adipose tissue: implicationsfor cell- based therapies. Tissue Eng. 7, 211-228.110. Zulewski, H., Abraham, E.J., Gerlach, M.J., Daniel, P.B.,Moritz, W., Muller, B., Vallejo, M., Thomas, M.K., andHabener, J.F. (2001). Multipotential nestin-positive stemcells isolated from adult pancreatic islets differentiate exvivo into pancreatic endocrine, exocrine, and hepaticphenotypes. Diabetes. 50, 521-533.107. Yamane, T., Hayashi, H., Mizoguchi, M., Yamazaki, H., andKunisada, T. (1999). Derivation of melanocytes fromembryonic stem cells in culture. Dev. Dyn. 216, 450-458.D-26
APPENDIX E:STEM CELL MARKERSAppendix E.i.HOW DO RESEARCHERS USEMARKERS TO IDENTIFY STEM CELLS?In recent years, scientists have discovered a widearray of stem cells that have unique capabilities toself-renew, grow indefinitely, and differentiate ordevelop into multiple types of cells and tissues.Researchers now know that many different types ofstem cells exist but they all are found in very smallpopulations in the human body, in some cases 1stem cell in 100,000 cells in circulating blood. And,when scientists examine these cells under a microscope,they look just like any other cell in the tissuewhere they are found. So, how do scientists identifythese rare type of cells found in many different cellsand tissues—a process that is much akin to finding aneedle in a haystack? The answer is rather simplethanks to stem cell “markers.” This feature describesstem cell marker technology and how it is used in theresearch laboratory. Following this is a listing of someof the commonly used stem cell markers (seeAppendix E.ii. Markers Commonly Used to Identify<strong>Stem</strong> <strong>Cells</strong> and to Characterize DifferentiatedCell Types).What are stem cell markers? Coating the surface ofevery cell in the body are specialized proteins, calledreceptors, that have the capability of selectively bindingor adhering to other “signaling” molecules. Thereare many different types of receptors that differ intheir structure and affinity for the signaling molecules.Normally, cells use these receptors and the moleculesthat bind to them as a way of communicatingwith other cells and to carry out their proper functionsin the body. These same cell surface receptors arethe stem cell markers. Each cell type, for example aliver cell, has a certain combination of receptors ontheir surface that makes them distinguishable fromother kinds of cells. Scientists have taken advantageof the biological uniqueness of stem cell receptorsand chemical properties of certain compounds totag or “mark” cells. Researchers owe much of thepast success in finding and characterizing stem cellsto the use of markers.<strong>Stem</strong> cell markers are given short-hand names basedon the molecules that bind to the stem cell surfacereceptors. For example, a cell that has the receptorstem cell antigen – 1, on its surface, is identified asSca-1. In many cases, a combination of multiplemarkers is used to identify a particular stem cell type.So now, researchers often identify stem cells in shorthandby a combination of marker names reflectingthe presence (+) or absence (–) of them. For example,a special type of hematopoietic stem cell fromblood and bone marrow called “side population” or“SP” is described as (CD34 –/low , c-Kit + , Sca-1 + ) [4].Researchers use the signaling molecules that selectivelyadhere to the receptors on the surface of thecell as a tool that allows them to identify stem cells.Many years ago, a technique was developed toattach to the signaling molecule another molecule(or the tag) that has the ability to fluoresce or emitlight energy when activated by an energy sourcesuch as an ultraviolet light or laser beam (see FigureE.i.1. Identifying Cell Surface Markers UsingFluorescent Tags). At the researchers’ disposal aremultiple fluorescent tags with emitted light that differin color and intensity.Described here are two approaches of howresearchers use the combination of the chemicalproperties of fluorescence and unique receptor patternson cell surfaces to identify specific populationsof stem cells. One approach for using markers as aresearch tool is with a technique known as fluorescence-activatedcell sorting (FACS) (see Figure E.i.2.E-1
Appendix E: <strong>Stem</strong> Cell Markers© 2001 Terese WinslowFluorescent tagattached to surfacemarkerFluorescenttagCell receptor<strong>Cells</strong>urface<strong>Stem</strong> cellFigure E.i.1. Identifying Cell Surface Markers UsingFluorescent Tags.Looking for a Needle in a Haystack: How ResearchersFind <strong>Stem</strong> <strong>Cells</strong>) [1, 3, 5]. Researchers often use aFACS instrument to sort out the rare stem cells fromthe millions of other cells. With this technique, a suspensionof tagged cells (i.e., bound to the cell surfacemarkers are fluorescent tags) is sent under pressurethrough a very narrow nozzle—so narrow thatcells must pass through one at a time. Upon exitingthe nozzle, cells then pass, one-by-one, through alight source, usually a laser, and then through anelectric field. The fluorescent cells become negativelycharged, while nonfluorescent cells become positivelycharged. The charge difference allows stem cellsto be separated from other cells. The researchersnow have a population of cells that have all of thesame marker characteristics, and with these cells theycan conduct their research.A second method uses stem cell markers and theirfluorescent tags to visually assess cells as they exist intissues. Often researchers want to assess how stemcells appear in tissues and in doing so they use amicroscope to evaluate them rather than the FACSinstrument. In this case, a thin slice of tissue is prepared,and the stem cell markers are tagged by thesignaling molecule that has the fluorescent tagattached. The fluorescent tags are then activatedeither by special light energy or a chemical reaction.The stem cells will emit a fluorescent light that caneasily be seen under the microscope.Genetic and molecular biology techniques areextensively used to study how cells become specializedin the organism’s development. In doing so,researchers have identified genes and transcriptionfactors (proteins found within cells that regulate agene’s activity) that are unique in stem cells. Scientistsuse techniques such as polymerase chain reaction(PCR) to detect the presence of genes that are“active” and play a role guiding the specialization ofa cell. This technique has is helpful to researchers toidentify “genetic markers” that are characteristic ofstem cells. For example, a gene marker called PDX-1is specific for a transcription factor protein that initiatesactivation of the insulin gene. Researchers usethis marker to identify cells that are able to developislet cells in the pancreas.Recently, researchers have applied a genetic engineeringapproach that uses fluorescence, but isn’tdependent on cell surface markers. The importanceof this new technique is that it allows the tracking ofstem cells as they differentiate or become specialized.Scientists have inserted into a stem cell a“reporter gene” called green fluorescent protein orGFP [2]. The gene is only activated or “reports” whencells are undifferentiated and is turned off once theybecome specialized. Once activated, the genedirects the stem cells to produce a protein that fluorescesin a brilliant green color (see Figure Ei.3.Microscopic Image of Fluorescent-Labeled <strong>Stem</strong>Cell). Researchers are now coupling this reportingmethod with the FACS and microscopic methodsdescribed earlier to sort cells, identify them in tissues,and now, track them as they differentiate or becomespecialized.These discovery tools are commonly used in researchlaboratories and clinics today, and will likely playimportant roles in advancing stem cell research.There are limitations, however. One of them is that asingle marker identifying pluripotent stem cells, thosestem cells that can make any other cell, has yet tobe found. As new types of stem cells are identifiedand research applications of them becomeincreasingly complex, more sophisticated tools will bedeveloped to meet investigators’ needs. For the foreseeablefuture, markers will continue to play a majorrole in the rapidly evolving world of stem cell biology.E-2
Appendix E: <strong>Stem</strong> Cell Markers<strong>Stem</strong> cell<strong>Cells</strong> in suspensionare tagged withfluorescent markersspecific for undifferentiatedstem cells.FLUORESCENTACTIVATED CELLSORTING (FACS)Laser beam passesthrough one cellLabeled cells are sentunder pressure througha small nozzle and passthrough an electric field.GRAPHIC DISPLAY OF FACSA cell generates anegative charge if itfluoresces and apositive charge if itdoes not.Fluorescence intensity© 2001 Terese Winslow, Lydia Kibiuk, Caitlin Duckwall<strong>Stem</strong> cell foundFigure E.i.2. Looking for a Needle in a Haystack: How Researchers Find <strong>Stem</strong> <strong>Cells</strong>.E-3
Appendix E: <strong>Stem</strong> Cell MarkersREFERENCES© 2001 Terese WinslowDifferentiated<strong>Cells</strong>Undifferentiatedstem cellsFigure E.i.3. Microscopic Image of Fluorescent-Labeled<strong>Stem</strong> Cell.1. Bonner, W.A., Hulett, H.R., Sweet, R.G., and Herzenberg, L.A.(1972). Fluorescence activated cell sorting. Rev. Sci.Instrum. 43, 404-409.2. Eiges, R., Schuldiner, M., Drukker, M., Yanuka, O., Itskovitz-Eldor, J., and Benvenisty, N. (2001). Establishment of humanembryonic sten cell-transduced clones carrying a markerof undifferentiated cells. Curr. Biol. 11, 514-518.3. Herzenberg, L.A. and De Rosa, S.C. (2000). Monoclonalantibodies and the FACS: complementary tools forimmunobiology and medicine. Immunol. Today. 21, 383-390.4. Jackson, K., Majka SM, Wang H, Pocius J, Hartley CJ,Majesky MW, Entman ML, Michael LH, Hirschi KK, andGoodell MA (2001). Regeneration of ischemic cardiacmuscle and vascular endothelium by adult stem cells. J.Clin. Invest. 107, 1-8.5. Julius, M.H., Masuda, T., and Herzenberg, L.A. (1972).Demonstration that antigen-binding cells are precursors ofantibody- producing cells after purification with a fluorescence-activatedcell sorter. Proc. Natl. Acad. Sci. U. S. A.69, 1934-1938.E-4
Appendix E: <strong>Stem</strong> Cell MarkersAppendix E.ii.Markers Commonly Used to Identify <strong>Stem</strong> <strong>Cells</strong>and to Characterize Differentiated Cell TypesMarker Name Cell Type SignificanceBlood VesselFetal liver kinase-1(Flk1)EndothelialCell-surface receptor protein that identifies endothelial cellprogenitor; marker of cell-cell contactsSmooth muscle cell-specificmyosin heavy chainSmooth muscleIdentifies smooth muscle cells in the wall of blood vesselsVascular endothelial cellcadherinSmooth muscleIdentifies smooth muscle cells in the wall of blood vesselsBone-specific alkalinephosphatase(BAP)OsteoblastBoneEnzyme expressed in osteoblast; activity indicates bone formationHydroxyapatite Osteoblast Minerlized bone matrix that provides structural integrity; marker ofbone formationOsteocalcin(OC)OsteoblastMineral-binding protein uniquely synthesized by osteoblast; marker ofbone formationBone Marrow and BloodBone morphogenetic proteinreceptor(BMPR)Mesenchymal stemand progenitor cellsImportant for the differentiation of committed mesenchymal celltypes from mesenchymal stem and progenitor cells; BMPR identifiesearly mesenchymal lineages (stem and progenitor cells)CD4 and CD8 White blood cell (WBC) Cell-surface protein markers specific for mature T lymphocyte(WBC subtype)CD34Hematopoietic stemcell (HSC), satellite,endothelial progenitorCell-surface protein on bone marrow cell, indicative of a HSC andendothelial progenitor; CD34 also identifies muscle satellite, amuscle stem cellCD34 + Sca1 + Lin – profileMesencyhmal stemcell (MSC)Identifies MSCs, which can differentiate into adipocyte, osteocyte,chondrocyte, and myocyteE-5
Appendix E: <strong>Stem</strong> Cell MarkersAppendix E.ii. (cont.)Marker Name Cell Type SignificanceBone Marrow and Blood cont.CD38Absent on HSCPresent on WBClineagesCell-surface molecule that identifies WBC lineages. Selection ofCD34 + /CD38 – cells allows for purification of HSC populationsCD44 Mesenchymal A type of cell-adhesion molecule used to identify specific types ofmesenchymal cellsc-Kit HSC, MSC Cell-surface receptor on BM cell types that identifies HSC and MSC;binding by fetal calf serum (FCS) enhances proliferation of ES cells,HSCs, MSCs, and hematopoietic progenitor cellsColony-forming unit(CFU)HSC, MSC progenitorCFU assay detects the ability of a single stem cell or progenitor cellto give rise to one or more cell lineages, such as red blood cell(RBC) and/or white blood cell (WBC) lineagesFibroblast colony-forming unit(CFU-F)Bone marrow fibroblastAn individual bone marrow cell that has given rise to a colony ofmultipotent fibroblastic cells; such identified cells are precursors ofdifferentiated mesenchymal lineagesHoechst dye Absent on HSC Fluorescent dye that binds DNA; HSC extrudes the dye and stainslightly compared with other cell typesLeukocyte common antigen(CD45)WBCCell-surface protein on WBC progenitorLineage surface antigen(Lin)HSC, MSCDifferentiated RBC andWBC lineagesThirteen to 14 different cell-surface proteins that are markers ofmature blood cell lineages; detection of Lin-negative cells assists inthe purification of HSC and hematopoietic progenitor populationsMac-1 WBC Cell-surface protein specific for mature granulocyte andmacrophage (WBC subtypes)Muc-18 (CD146)Bone marrowfibroblasts, endothelialCell-surface protein (immunoglobulin superfamily) found on bonemarrow fibroblasts, which may be important in hematopoiesis; asubpopulation of Muc-18+ cells are mesenchymal precursorsE-6
Appendix E: <strong>Stem</strong> Cell MarkersAppendix E.ii. (cont.)Marker Name Cell Type SignificanceBone Marrow and Blood cont.<strong>Stem</strong> cell antigen(Sca-1)HSC, MSCCell-surface protein on bone marrow (BM) cell, indicative of HSCand MSCStro-1 antigenStromal(mesenchymal)precursor cells,hematopoietic cellsCell-surface glycoprotein on subsets of bone marrow stromal(mesenchymal) cells; selection of Stro-1 + cells assists in isolatingmesenchymal precursor cells, which are multipotent cells that giverise to adipocytes, osteocytes, smooth myocytes, fibroblasts,chondrocytes, and blood cellsThy-1 HSC, MSC Cell-surface protein; negative or low detection is suggestive of HSCCartilageCollagen types II and IV Chondrocyte Structural proteins produced specifically by chondrocyteKeratin Keratinocyte Principal protein of skin; identifies differentiated keratinocyteSulfated proteoglycan Chondrocyte Molecule found in connective tissues; synthesized by chondrocyteFatAdipocyte lipid-binding protein(ALBP)AdipocyteLipid-binding protein located specifically in adipocyteFatty acid transporter(FAT)AdipocyteTransport molecule located specifically in adipocyteAdipocyte lipid-binding protein(ALBP)AdipocyteLipid-binding protein located specifically in adipocyteGeneralY chromosome Male cells Male-specific chromosome used in labeling and detecting donorcells in female transplant recipientsKaryotype Most cell types Analysis of chromosome structure and number in a cellE-7
Appendix E: <strong>Stem</strong> Cell MarkersAppendix E.ii. (cont.)Marker Name Cell Type SignificanceAlbumin Hepatocyte Principal protein produced by the liver; indicates functioning ofmaturing and fully differentiated hepatocytesLiverB-1 integrin Hepatocyte Cell-adhesion molecule important in cell-cell interactions; markerexpressed during development of liverNervous SystemCD133 Neural stem cell, HSC Cell-surface protein that identifies neural stem cells, which give riseto neurons and glial cellsGlial fibrillary acidic protein(GFAP)AstrocyteProtein specifically produced by astrocyteMicrotubule-associatedprotein-2(MAP-2)NeuronDendrite-specific MAP; protein found specifically in dendriticbranching of neuronMyelin basic protein(MPB)OligodendrocyteProtein produced by mature oligodendrocytes; located in the myelinsheath surrounding neuronal structuresNestin Neural progenitor Intermediate filament structural protein expressed in primitiveneural tissueNeural tubulin Neuron Important structural protein for neuron; identifies differentiated neuronNeurofilament(NF)NeuronImportant structural protein for neuron; identifies differentiated neuronNeurosphere Embryoid body (EB), ES Cluster of primitive neural cells in culture of differentiating ES cells;indicates presence of early neurons and gliaNoggin Neuron A neuron-specific gene expressed during the developmentof neuronsO4 Oligodendrocyte Cell-surface marker on immature, developing oligodendrocyteO1 Oligodendrocyte Cell-surface marker that characterizes mature oligodendrocyteE-8
Appendix E: <strong>Stem</strong> Cell MarkersAppendix E.ii. (cont.)Marker Name Cell Type SignificanceNervous System cont.Synaptophysin Neuron Neuronal protein located in synapses; indicates connectionsbetween neuronsTau Neuron Type of MAP; helps maintain structure of the axonPancreasCytokeratin 19(CK19)Pancreatic epitheliumCK19 identifies specific pancreatic epithelial cells that areprogenitors for islet cells and ductal cellsGlucagon Pancreatic islet Expressed by alpha-islet cell of pancreasInsulin Pancreatic islet Expressed by beta-islet cell of pancreasInsulin-promoting factor-1(PDX-1)Pancreatic isletTranscription factor expressed by beta-islet cell of pancreasNestin Pancreatic progenitor Structural filament protein indicative of progenitor cell linesincluding pancreaticPancreatic polypeptide Pancreatic islet Expressed by gamma-islet cell of pancreasSomatostatin Pancreatic islet Expressed by delta-islet cell of pancreasPluripotent <strong>Stem</strong> <strong>Cells</strong>Alkaline phosphataseEmbryonic stem (ES),embryonal carcinoma(EC)Elevated expression of this enzyme is associated with undifferentiatedpluripotent stem cell (PSC)Alpha-fetoprotein (AFP) Endoderm Protein expressed during development of primitive endoderm;reflects endodermal differentiationBone morphogenetic protein-4 Mesoderm Growth and differentiation factor expressed during early mesodermformation and differentiationBrachyury Mesoderm Transcription factor important in the earliest phases of mesodermformation and differentiation; used as the earliest indicator ofmesoderm formationE-9
Appendix E: <strong>Stem</strong> Cell MarkersAppendix E.ii. (cont.)Marker Name Cell Type SignificancePluripotent <strong>Stem</strong> <strong>Cells</strong> cont.Cluster designation 30(CD30)ES, ECSurface receptor molecule found specifically on PSCCripto(TDGF-1)ES, cardiomyocyteGene for growth factor expressed by ES cells, primitive ectoderm,and developing cardiomyocyteGATA-4 gene Endoderm Expression increases as ES differentiates into endodermGCTM-2 ES, EC Antibody to a specific extracellular-matrix molecule that issynthesized by undifferentiated PSCsGenesis ES, EC Transcription factor uniquely expressed by ES cells either in or duringthe undifferentiated state of PSCsGerm cell nuclear factor ES, EC Transcription factor expressed by PSCsHepatocyte nuclear factor-4(HNF-4)EndodermTranscription factor expressed early in endoderm formationNestinEctoderm, neural andpancreatic progenitorIntermediate filaments within cells; characteristic of primitiveneuroectoderm formationNeuronal cell-adhesionmolecule(N-CAM)EctodermCell-surface molecule that promotes cell-cell interaction; indicatesprimitive neuroectoderm formationOct-4 ES, EC Transcription factor unique to PSCs; essential for establishment andmaintenance of undifferentiated PSCsPax6 Ectoderm Transcription factor expressed as ES cell differentiates intoneuroepitheliumStage-specific embryonicantigen-3 (SSEA-3)ES, ECGlycoprotein specifically expressed in early embryonic developmentand by undifferentiated PSCsStage-specific embryonicantigen-4 (SSEA-4)ES, ECGlycoprotein specifically expressed in early embryonic developmentand by undifferentiated PSCsE-10
Appendix E: <strong>Stem</strong> Cell MarkersAppendix E.ii. (cont.)Marker Name Cell Type SignificancePluripotent <strong>Stem</strong> <strong>Cells</strong> cont.<strong>Stem</strong> cell factor(SCF or c-Kit ligand)ES, EC, HSC, MSCMembrane protein that enhances proliferation of ES and EC cells,hematopoietic stem cell (HSCs), and mesenchymal stem cells(MSCs); binds the receptor c-KitTelomerase ES, EC An enzyme uniquely associated with immortal cell lines; useful foridentifying undifferentiated PSCsTRA-1-60 ES, EC Antibody to a specific extracellular matrix molecule is synthesized byundifferentiated PSCsTRA-1-81 ES, EC Antibody to a specific extracellular matrix molecule normallysynthesized by undifferentiated PSCsVimentinEctoderm, neural andpancreatic progenitorIntermediate filaments within cells; characteristic of primitiveneuroectoderm formationSkeletal Muscle/Cardiac/Smooth MuscleMyoD and Pax7 Myoblast, myocyte Transcription factors that direct differentiation of myoblasts intomature myocytesMyogenin and MR4 Skeletal myocyte Secondary transcription factors required for differentiation ofmyoblasts from muscle stem cellsMyosin heavy chain Cardiomyocyte A component of structural and contractile protein foundin cardiomyocyteMyosin light chain Skeletal myocyte A component of structural and contractile protein found inskeletal myocyteE-11
Appendix E: <strong>Stem</strong> Cell MarkersThis page intentionally left blankE-12
APPENDIX F:GLOSSARY AND TERMSAppendix F.i.GLOSSARYAdipocyte – Fat cell.Adult stem cell – An undifferentiated cell found in adifferentiated tissue that can renew itself and (withcertain limitations) differentiate to yield all the specializedcell types of the tissue from which it originated.Allogenic – Two or more individuals (or cell lines) arestated to be allogeneic to one another when thegenes at one or more loci are not identical insequence in each organism.Amnion – The innermost intrauterine membranearound the fetus and the amniotic fluid.Anterior visceral endoderm (AVE) – Specific tissuestructure arising in the early embryo that helpsestablish the anterior-posterior axis of the organism.Antibody – A Y-shaped protein secreted by B cells inresponse to an antigen. An antibody binds specificallyto the antigen that induced its production.Antibodies directed against antigens on the surfaceof infectious organisms help eliminate those organismsfrom the body.Antigen – A substance (often a protein) that inducesthe formation of an antibody. Antigens are commonlyfound on the surface of infectious organisms, transfusedblood cells, and transplanted organs.Antigen presenting cells (APCs) – One of a variety ofcells within the body that can process antigens anddisplay them on their surface in a form recognizableby T cells.Apoptosis – Genetically programmed cell death.Astrocyte – One of the large neuroglia cells ofnervous tissue.Autoantibody – An antibody that reacts with antigensfound on the cells and tissues of an individual’sownbody. Autoantibodies can cause autoimmunediseases.Autoimmune disease – A condition that results fromT cells and/or antibodies that attack the cells ortissues of an individual’s own body.Autologous transplant – Transplanted tissue derivedfrom the intended recipient of the transplant. Such atransplant helps avoid complications of immunerejection.Axis – A straight line passing through a spherical bodybetween its two poles. The central line of the body orany of its parts. The vertebral column. The centralnervous system. An artery that when created, immediatelydivides into a number of branches.B cells – Also known as B lymphocytes. Each B cell iscapable of making one specific antibody. Whenstimulated by antigen and helper T cells, B cellsmature into plasma cells that secrete large amountsof their specific antibody.Blastocoel – The cavity in the blastula of thedeveloping embryo.Blastocyst – A preimplantation embryo of 30-150cells. The blastocyst consists of a sphere made up ofan outer layer of cells (the trophectoderm), a fluidfilledcavity (the blastocoel), and a cluster of cellson the interior (the inner cell mass).Blastula – An early stage in the development of anovum consisting of a hollow sphere of cells enclosinga cavity called the blastocoel.F-1
Appendix F: Glossary and TermsBone marrow – The soft, living tissue that fills mostbone cavities and contains hematopoietic stemcells, from which all red and white blood cells evolve.The bone marrow also contains mesenchymal stemcells that a number of cells types come from,including chondrocytes, which produce cartilage.Bone marrow (BM) cell – Refers to bothhematopoietic and mesenchymal (stromal) cells.Bone marrow stem cell (BMSC) – One of at least twotypes of multipotient stem cells: hematopoietic stemcell and mesenchymal stem cell.Bone marrow transplantation (BMTx) – Trans-plantationof bone marrow from one individual to another.Autologous BMTx is a process in which a patient’shealthy bone marrow is withdrawn and preserved,then injected back into the patient to restore the productionof healthy blood and immune cells by thebone marrow. This strategy is often used in patientswith certain types of cancer who have undergoneradiation therapy or chemotherapy that destroys thebone marrow cells.Bone morphogenetic proteins (BMPs) – Proteinsthatare involved in the formation of embryonic bone.BMPs operate at several stages in this formation ofbone, beginning with the early stages of morphogenesisand continuing to late postnatal life. BMPsalso play a critical role in the development of thecentral nervous system.Brain-derived neurotrophic factor (BDNF) – A growthfactor synthesized in the brain that stimulates neuriteoutgrowth and supports survival of neurons.Cavitation – A process that occurs during the formationof the blastocyst and establishes the polarity ofembryonic cells.Cell cycle – The orderly sequence of events by whichthe cell duplicates its contents and divides into two.Chimera – An organism composed of cells derivedfrom at least two genetically different zygotes.Theoretically, the zygote could be from separatespecies.Chondrocytes – Cartilage cells.Chorion – The multilayered, outermost fetalmembrane. As pregnancy progresses, part of thechorion becomes the placenta.Chromosomes – Nucleic acid-protein structures inthe nucleus of a cell. Chromosomes are composedchiefly of DNA, the carrier of hereditary information.Chromosomes contain genes, working subunits ofDNA that carry the genetic code for specific proteins,interspersed with large amounts of DNA of unknownfunction. A normal human body cell contains 46chromosomes; a normal human gamete, 23chromosomes.Cleavage – The process of cell division in the veryearly embryo before it becomes a blastocyst.Clonality – A line of cells that is genetically identicalto the originating cell; in this case, a stem cell.Cluster differentiation (CD) – Cell membranemolecules used to classify leukocytes into subsets.Colony-forming cells – Groups of cells growing on asolid nutrient surface with each group being createdfrom the multiplication of an individual cell.Colony-stimulating factors – Diffusible proteins thatstimulate the proliferation of hematopoietic stemcells.Cripto – Transcription factor expressed by pluripotentstem cells and early embryos.Cyclin-dependent kinase (Cdk protein) – Proteinkinase that has to be complexed with a cyclin proteinin order to act; different Cdk-cyclin complexes arethought to trigger different steps in the cell-divisioncycle by phosphorylating specific target proteins.Cytokines – A generic term for a large variety ofregulatory proteins produced and secreted by cellsand used to communicate with other cells. One classofcytokines is the interleukins, which act as intercellularmediators during the generation of animmune response.Cytoplasm – The contents of a cell other than thenucleus; cytoplasm consists of a fluid containingnumerous structures, known as organelles, that carryout essential cell functions.Decidual cells – A cellular matrix that first surroundsan implanted embryo and later occupies most of theendometrium.Dendrite – Extension of a nerve cell, typicallybranched and relatively short, that receives stimulifrom other nerve cells.F-2
Appendix F: Glossary and TermsDifferentiation – The process whereby an unspecializedearly embryonic cell acquires the features of aspecialized cell such as a heart, liver, or muscle cell.Diploid – A cell or tissue having two chromosomesets, as opposed to the haploid situation of gametes,which have only one chromosome set.DNA – Deoxyribonucleic acid, a chemical foundprimarily in the nucleus of cells. DNA carries theinstructions for making all the structures and materialsthe body needs to function.DNA methylation – A type of chemical modificationof DNA that regulates gene expression.Ectoderm – The upper, outermost of the threeprimitive germ layers of the embryo; it gives rise toskin, nerves, and brain.Egg cylinder – An asymmetric embryonic structurethat helps to determine the body plan of the mouse.Embryo – In humans, the developing organism fromthe time of fertilization until the end of the eighthweek of gestation, when it becomes known as afetus.Embryoid bodies (EBs) – Clumps of cellular structuresthat arise when embryonic stem cells are cultured.Embryoid bodies contain tissue from all three of thegerm layers: endoderm, mesoderm, and ectoderm.Embryoid bodies are not part of normal developmentand occur only in in vitro conditions.Embryonal carcinoma (EC) cells – A type of pluripotentstem cell derived from teratocarcinoma(usually a testis tumor).Embryonic disk – A group of cells derived from theinner cell mass of the blastocyst, which later developsinto an embryo. The disc consists of three germ layersknown as the endoderm, mesoderm, and ectoderm.Embryonic germ (EG) cells – <strong>Cells</strong> found in aspecific part of the embryo/fetus called the gonadalridge that normally develop into mature gametes.Embryonic stem (ES) cells – Primitive (undifferentiated)cells from the embryo that have the potentialto become a wide variety of specialized cell types.Endoderm – Lower layer of a group of cells derivedfrom the inner cell mass of the blastocyst; it laterbecomes the lungs and digestive organs.Epiblast – Gives rise to the ectoderm andmesoderm. The mesoderm then displaces thehypoblast cells and forms the entodermal cell layeron its inner surface.Epidermal growth factor (EGF) – A protein that stimulatesepidermal and various other cells to divide.Epithelium – The layer of cells forming the epidermisof the skin. These cells serve the general functions ofprotection, absorption, and secretion, and play aspecialized role in moving substances through ducts,in the production of germ cells, and in the receptionof stimuli. Their ability to regenerate is excellent; theepithelium may replace itself as frequently as every24 hours.Erythroid cell – Red blood cells.Ex vivo – Outside the living body.Extracellular matrix – The microenvironment next to acell that allows for structural support, orientation, andconnections for cell-to-cell interactions and formationof connective tissues.Extraembryonic tissues – Intrauterine tissues thatsupport the embryoís placenta, umbilical cord, andamniotic sac.Feeder cell layer – <strong>Cells</strong> that are utilized in co-cultureto maintain pluripotent stem cells. <strong>Cells</strong> usually consistof mouse embryonic fibroblasts.Fertilization – The process whereby male and femalegametes unite.Fetal calf serum – A type of culture medium oftenused in the culture of stem cells. It provides a numberof growth factors.Fibroblast – <strong>Cells</strong> that give rise to connective tissue.Fluorescence-activated cell sorting (FACS) – Atechnique that can separate and analyze cells,which are labeled with fluorochrome-conjugatedantibody, by their fluorescence and light scatteringpatterns.Follistatin – An inhibitory factor produced duringembryonic development that affects the growth anddifferentiation of the pancreas.Gap junctions – Communicating cell-cell junctionsthat allow ions and small molecules to pass from thecytoplasm of one cell to the cytoplasm of another cell.F-3
Appendix F: Glossary and TermsGastrula – Animal embryo at an early stage of developmentin which cells are enclosed in a sheath toform the beginning of a gut cavity.Gene – A functional unit of heredity that is a segmentof DNA located in a specific site on a chromosome.A gene Directs the formation of an enzyme of otherprotein.Genital Ridge – Formation of a genital ridge requiresat least two genes, WT-1, which is also important inearly kidney formation, and SF-1, required for thedevelopment of both the gonads and adrenalglands.Genome – The complete genetic material of anorganism.Genomic imprinting – A biochemical phenomenonthat determines, for certain specific genes, which oneof the pair of identical genes, the motherís or thefatherís, will be active in that individual.Germ cell – A sperm or egg, or a cell that canbecome a sperm or egg. All other body cells arecalled somatic cells.Gestation – The period of development of anorganism from fertilization of the ovum until birth.Glia – The nonneuronal or supporting tissue(neuroglia) of the brain and spinal cord.Glial cells – Supporting cells of the nervous system,including oligodendrocytes and astrocytes in thevertebrate central nervous system and Schwann cellsin the peripheral nervous system.Glial fibrillary acidic protein (GFAP) – A structuralprotein specifically produced by astrocytes. GFAP isoften used as a marker of astrocytes.Glucagon – A hormone consisting of a straight chainof proteins composed of 29 amino acid residues thatcan be extracted from certain pancreatic cells.Glycoprotein – A compound consisting of acarbohydrate and a protein.Gonadal ridge –Anatomic site in the early fetuswhere primordial germ cells (PGCs) are formed.Gonads – The embryonic sex gland before itbecomes a definitive testis or ovary.Goosecoid – Gene that encodes a transcriptionfactor that is important for determining craniofacialorientation and features in the vertebrate embryo.Graft-versus-host disease (GVHD) – A condition thatoccurs following bone marrow transplantation inwhich the donor-derived T cells attack the host’stissues.Granulocyte – A type of white blood cell filled withmicroscopic granules that are little sacs containingenzymes, compounds that digest microorganisms.Neutrophils, eosinophils and basophils are all types ofgranulocytes. They are named by the stainingfeatures of their granules in the laboratory.Granulose cells – <strong>Cells</strong> surrounding and maintainingthe ovarian follicle.Green fluorescent protein (GFP) – Fluorescent-proteindye used to tag and trace particular genes and cellsof interest.Hanging drop method – A technique used to cultureembryonic stem cells so that they develop intoembryoid bodies.Haploid – Refers to a gamete having one chromosomeset, as opposed to the diploid situation of cellsor tissues, where there are two chromosome sets.hCNS – Human central nervous system stem cell.Hematopoiesis – Generation of blood cells, mainly inthe bone marrow.Hematopoietic stem cell (HSC)– A stem cell fromwhich all red and white blood cells evolve.Hepatic – Relating to the liver.Hepatocyte – Liver cell.hES cell – Human embryonic stem cell; a type ofpluripotent stem cell.Hoechst dye – A dye used to identify hematopoieticstem cells (HSCs).Hox genes – Consists of at least 38 encodednucleotides that contain genes found in four clusterson four different chromosomes. An important functionof hox genes in blood is the regulation of cellproliferation.F-4
Appendix F: Glossary and TermsHSC markers – Cell-surface molecules that are usedto identify hematopoietic stem cells.Hybridoma – A hybrid cell produced by the fusion ofan antibody-producing cell and a multiple myelomacell. The cell has the capability to produce acontinuous supply of identical antibodies.Hydroxyapatite – A natural mineral structure thatcontains calcium and phosphate ions that providethe power for the formation of bones and teeth.Hypoblast – The inner cell layer, or endoderm, whichdevelops during the formation of the embryonicgerm layers.Identical twinning – Process in which geneticallyidentical organisms arise from symmetrical divisionand separation of totipotent cells.Immune-function assay – A general term for anumber of tests based on an immune cell’s ability tocarry out a particular immune function.Immune system cells – White blood cells or leukocytesthat originate from the bone marrow. Theyinclude antigen presenting cells, such as dendriticcells, T and B lymphocytes, and neutrophils, amongmany others.Immunocompromised mice – These geneticallyaltered mice are used for transplantation experimentsbecause they usually do not reject the transplantedtissue.Immunofluorescence – The detection of antibodiesby using special proteins labeled with fluorescein.When present, the specific organism or antibody isobserved as a fluorescent material when examinedmicroscopically while illuminated with a fluorescentlight source.Immunogenic – Relating to or producing an immuneresponse.Immunohistology – Examination of tissues throughspecific immunostaining techniques.Immunophenotyping – Identification of various typesof immune cells by sorting them according to theircell-surface markers.In utero – In the uterus.In vitro – Literally, “in glass;” in a laboratory dish or testtube; an artificial environment.In vitro fertilization (IVF) – An assisted reproductiontechnique in which fertilization is accomplishedoutside the body.In vivo – In the living subject; in a natural environment.Indomethacin – An anti-inflammatory, antipain, andantifever drug. Its primary use is in rheumatoid arthritisand degenerative joint disease when aspirin-basedproducts are ineffective or cannot be tolerated.Inner cell mass – The cluster of cells inside theblastocyst. These cells give rise to the embryonic diskof the later embryo and, ultimately, the fetus.Insulin-promoting factor 1 – A transcription factorexpressed in the pancreas and necessary for theproduction of insulin.Interleukin – Selected peptide or protein thatprimarily mediates local interactions between whiteblood cells.Irradiate – Application of radiation from a source(heat, light, Xrays) to a structure or organism.Karyotype – The full set of chromosomes of a cellarranged with respect to size, shape, and number.Keratin –An extremely tough protein substance foundin hair, nails, skin, and cornea.Keratinocytes – <strong>Cells</strong> that synthesize keratin and arefound in the skin, hair, and nails. A fibrous protein isproduced by keratinocytes and may be hard or soft.The hard keratin is found in hair and nails. The softkeratin is found in the epidermis of the skin in the formof flattened non-nucleated scales that sloughcontinually.Knock-out mouse – A mouse that has had oneor both copies of a specific gene deleted orinactivated.Lacunae – The spaces occupied by cells (e.g.,chondrocytes and osteocytes) of calcified tissues.Lefty – A developmental factor that helps determineright-left asymmetry in vertebrates.Leptin –A hormone produced by the placenta andfetal tissues that acts as a growth factor andmodulator of metabolic and immune functions.Leukemia inhibitory factor (LIF) – A growth factornecessary for maintaining mouse embryonic stemcells in a proliferative, undifferentiated state.F-5
Appendix F: Glossary and TermsLeukocyte – A white blood cell or corpuscle.Leukocytes are formed from undifferentiated stemcells that give rise to all blood cells.Leukocyte common antigen – Cell-surface moleculefound on white blood cells and white blood cellprogenitors. Also referred to as CD45.Lineage surface antigen (Lin) – A mixture of monoclonalantibodies that are directed against antigensfound on mature hematopoietic cells of differentlineages. A usual Lin mix includes eight differentantibodies directed against B and T cells, myeloidcells, and erythroid cells.Lipase – An enzyme produced by many tissues.Lipase is an important regulator of fat in the blood.A deficiency of this enzyme leads to low levels ofhigh-density lipoproteins (HDLs).Lipid – Any one of a group of fats or fatlike substancescharacterized by their insolubility in water andsolubility in fat solvents such as alcohol, ether, andchloroform.Lymph nodes – Widely distributed lymphoid organswithin the lymphatic system where many immunecells are concentrated.Lymphatic system – A network of lymph vessels andnodes that drain and filter antigens from tissue fluidsbefore returning lymphocytes to the blood.Lymphocyte – A cell present in the blood andlymphatic tissue.Lymphoid – A shape or form that resembles lymph orlymph tissue.Macrophage – A monocyte that has left thecirculation and settled and matured in a tissue.Because of their placement in the lymphoid tissues,macrophages serve as the major scavenger of theblood, clearing it of abnormal or old cells andcellular debris as well as pathogenic organisms.Major histocompatibility complex (MHC) – A groupof genes that code for cell-surface histocompatibilityantigens. These antigens are the primary reason whyorgan and tissue transplants from incompatibledonors fail.Marker – See Surface marker.Mast cell – A large tissue cell that does not circulatein the blood. They are also important in producingthe signs and symptoms of hypersensitivity reaction,such as those of an insect sting, and certain forms ofasthma.Maternal gene product – A product in the maleorganism of a gene from the X chromosome.Meiosis – A process where two successive cells divideand produce cells, eggs, or sperm that contain halfthe number of chromosomes in the somaticcells.During fertilization, the nuclei of the sperm andovum fuse and produce a zygote with the fullchromosome complements.Melanocyte – A cell that produces the dark pigmentmelanin; responsible for the pigmentation of skin andhair.Memory – The ability of antigen-specific T or B cellsto“recall” prior exposure to an antigen and respondquickly without the need to be activated again byCD4 helper T cells.Memory cells – A subset of antigen-specific T or Bcells that “recall” prior exposure to an antigen andrespond quickly without the need to be activatedagain by CD4 helper T cells.Mesenchymal stem cells (MSCs) – <strong>Cells</strong> from theimmature embryonic connective tissue. A number ofcell types come from mesenchymal stem cells,including chondrocytes, which produce cartilage.Mesoderm – The middle layer of the embryonic disk,which consists of a group of cells derived from theinner cell mass of the blastocyst. This middle germlayer is known as gastrulation and is the precursor tobone, muscle, and connective tissue.Metaphase– A stage of mitosis where chromosomesare firmly attached to the mitotic spindle at itsequator but have not yet segregated toward oppositepoles.Microtubule – An elongated, hollow tubular structurepresent in the cell. Microtubules help certain cellsmaintain their rigidity, convert chemical energy intowork, and provide a means of transportation ofsubstances in different directions within a cell.Monoclonal – From a single cell.F-6
Appendix F: Glossary and TermsMonoclonal antibody (MoAb) – An exceptionallypure and specific antibody derived from hybridomacells. Because each of the clones is derived from asingle B cell, all of the antibody molecules it makesare identical.Monocyte – A white blood cell derived from myeloidstem cells.Mononucleocyte – A cell containing a singlenucleus. Generally refers to a white blood cell.Morphology – The shape and structural makeup of acell, tissue, or organism.Morula – A solid mass of cells that resembles amulberry and result from the cleavage of an ovum.Mouse embryonic fibroblast (MEF) – Mouseembryonic fibroblast cells are used as feeder cellswhen culturing pluripotent stem cells.Multipotent stem cells – <strong>Stem</strong> cells that have thecapability of developing cells of multiple germ layers.Myelin – A fatty sheath that covers axons of nervecells. It is produced by oligodendrocytes andprovides an insulation for nerve conduction throughthe axons.Myelin basic protein (MPB) –A structural protein withinthe myelin sheath surrounding neurons.Myelin sheath – Insulating layer of specialized cellmembrane wrapped around vertebrate axons. Thissheath is produced by oligodendrocytes in thecentral nervous system and by Schwann cells in theperipheral nervous system.Myeloid – Marrow-like, but not necessarily originatingfrom bone marrow.Myeloid stem cells – Precursors to the other lines ofblood cells: erythrocytes, granulocytes, monocytes,and platelets. The second-generation cells are stillpluripotent but their developmental potency is limitedbecause neither can form an offspring of the othertype.Myocyte – A muscular tissue cell.MyoD1 – A group of four basic myogenic regulatoryfactors (helix-loop-helix transcription) and a newlydiscovered factor called muscle enhancer factor-2which appears to work away from the other threefactors. However, all four of the factors in this MyoDfamily have the capacity of converting nonmuscle cellsinto cells expressing the full range of muscle proteins.Myosin – A protein in muscle fibers.Myosin light chain – There are four light chainsubunits containing complex molecules that formcontractile units in skeletal muscle.Nestin – An intermediate filament protein found incells such as neural and pancreatic precursors.Neural crest – A band of cells that extend lengthwisealong the neural tube of an embryo and give rise tocells that form the cranial, spinal, and autonomicganglia, as well as becoming odontoblasts, whichform the calcified part of the teeth.Neural plate – A thickened band of ectoderm alongthe dorsal surface of an embryo. The nervous systemdevelops from this tissue.Neural stem cell (NSC) – A stem cell found in adultneural tissue that can give rise to neurons, astrocytes,and oligodendrocytes.Neural tube – The embryological forerunner of thecentral nervous system.Neuroectoderm – The central region of the earlyembryonic ectoderm, which later forms the brainand spinal cord, as well as evolving into nerve cells ofthe peripheral nervous systemNeuroepithelium – A specialized epithelial structurethat forms the termination of a nerve of a specialsense, i.e., olfactory cells, hair cells of the inner ear,and the rods and cones of the retina. It is theembryonic layer of the epiblast that develops intothe cerebrospinal axis.Neurofilament (NF) – A type of intermediate filamentfound in nerve cells.F-7
Appendix F: Glossary and TermsNeuron – A nerve cell, the structural and functionalunit of the nervous system. A neuron consists of a cellbody and its processes, an axon, and one or moredendrites. Neurons function by the initiation and conductionof impulses and transmit impulses to otherneurons or cells by releasing neurotransmitters atsynapses.Neurosphere –A primitive neural tissue that ariseswhen embryonic stem cells are grown in certainculture conditions.NMDA receptor – (N-methyl-d-aspartate receptor).A neurotransmitter receptor for excitatory synapses.Nodal – A knob-like protrusion.Node – A knot, knob; a protrusion or swelling; a constrictedregion; a small, rounded organ or structure.Notochord – Forms the axial skeleton in embryos ofall chordates. In vertebrates, it is replaced partially orcompletely by vertebrae.Oligodendrocyte – Cell that provides insulation tonerve cells by forming a myelin sheath around axons.Oocyte – Developing egg; usually a large andimmobile cell.Osteocalcin (OC) – A cytokine produced byosteoblasts that promotes bone formation.Osteoclast – A giant multi-nuclear cell formed in thebone marrow of growing bones.Osteocyte – A cell from the bone tissue.Osteoprogenitor – A cell-type that differentiates intoa mature osteocyte.Ovarian follicle – An external, fluid-filled portion of theovary in which oocytes mature before ovulation.Oviduct – The passage through which the ova travelfrom the ovary into the uterus.Pancreatic polypeptide – An endocrine proteinproduced by islet cells of the pancreas.Paracrine factors – Cytokines or hormones that acton cells or tissues within an extremely limited area.Passage – A round of cell growth and proliferationin culture.Placenta – The oval or discoid spongy structure in theuterus from which the fetus derives its nourishmentand oxygen.Plasticity – The ability of stem cells from one adulttissue to generate the differentiated types of anothertissue.Pluripotent stem cell (PSC) – A single stem cell thathas the capability of developing cells of all germlayers (endoderm, ectoderm, and mesoderm).Polarity – The presence of an axial, non symmetricgradient along a cell or tissue.Population doublings – A doubling in the number ofcells when grown in culture.Precursor <strong>Cells</strong> – In fetal or adult tissues, these arepartly differentiated cells that divide and give rise todifferentiated cells.Also known as progenitor cells.Pre-implantation embryo – The very early, freefloatingEmbryo, from the time the egg is fertilizeduntil implantation in the mother’s womb is complete.Primary germ layers – The three initial embryonicgerm layers–endoderm, mesoderm, andectoderm–from which all other somatic tissue-typesdevelop.Primitive streak – The initial band of cells from whichthe embryo begins to develop. The primitive streakestablishes and reveals the embryo’s head-tail andleft-right orientations.Radioimmunoassay – A sensitive method of determiningthe concentration of a substance, particularlya protein-bound hormone, in blood plasma.Retinoic acid – A metabolite of vitamin A.Ribonucleic acid (RNA) – A chemical that is similar instructure to DNA. One of its main functions is to translatethe genetic code of DNA into structural proteins.Ribosome – Any of the RNA- and protein-rich cytoplasmicorganelles that are sites of protein synthesis.Schwann cell – In the embryo, Schwann cells growaround the nerve fiber, forming concentric layers ofcell membrane (the myelin sheath).F-8
Appendix F: Glossary and TermsSide population (SP) stem cell – Two examples ofmultipotent stem cell populations found in bonemarrow and skeletal muscle. SPs are not yet fullycharacterized. Their significance is their unexpectedability to differentiate into cell types that are distinctfrom their tissue of origin.Signal transduction pathways – Relay of a signal bythe conversion from one physical or chemical formto another. In cell biology, signal transduction is theprocess in which a cell converts an extracellularsignal into a response.Somatic cell nuclear transfer – The transfer of a cellnucleus from a somatic cell into an egg from whichthe nucleus has been removed.Somatic cells – Any cell of a plant or animal otherthan a germ cell or germ cell precursor.Somatostatin – A hormone that inhibits the secretionof insulin and gastrin.Steel factor – See stem cell factor.<strong>Stem</strong> cell – A cell that has the ability to divide forindefinite periods in culture and to give rise tospecialized cells.<strong>Stem</strong> cell antigen 1 (Sca-1) – Cell-surface protein onbone marrow cell, indicative of hematopoietic stemcells and mesenchymal stem cells.<strong>Stem</strong> cell factor (SCF) – Relatively undifferentiatedcell that can continue dividing indefinitely, throwingoff daughter cells that can undergo terminal differentiationinto particular cell types. (Also known assteel factor).Stromal cell – A non-blood cell that is derived fromblood organs, such as bone marrow or fetal liver,which is capable of supporting growth of blood cellsin vitro. Stromal cells that make this matrix within thebone marrow are also derived from mesenchymalstem cells.Sulfated proteoglycan – Molecules found primarily inconnective tissues and joint fluids and that providelubrication.Surface marker – Surface proteins that are unique tocertain cell types capable of detection by antibodiesor other detection methods.Syncytiotrophoblast – A multinucleated cell formedfrom the cells of the trophoblast. Only a small area ofthe syncytiotrophoblast is evident at the start of theformation of the embryo, but this cell tissue is highlyinvasive, quickly expands and soon surrounds theentire embryo.Syncytium – A mass of cytoplasm containing manynuclei that are enclosed by a single plasma membrane.This is usually the result of either cell fusion or aseries of incomplete division cycles in which thenuclei divide but the cell does not.T cells – A type of white blood cell that is of crucialimportance to the immune system. Immature T cellsmigrate to the thymus gland in the upper chestcavity, where they mature and differentiate intovarious types of mature T cells and become active inthe immune system in response to a hormone calledthymosin and other factors. T-cells that are potentiallyactivated against the body’s own tissues are normallykilled or changed (“down-regulated”) during thismaturation process.Telomerase – An enzyme that is composed of acatalytic protein component and an RNA templateand that synthesizes DNA at the ends of chromosomesand confers replicative immortality to cells.Telomere – The end of a chromosome, associatedwith a characteristic DNA sequence that is replicatedin a special way. A telomere counteracts thetendency of the chromosome to shorten with eachround of replication.Tenocyte – Tendon-producing cell.Teratocarcinoma – A tumor that occurs mostly inthe testis.Teratogen – A drug or other agent that raises theincidence of congenital malformations.Teratoma – A tumor composed of tissues from thethree embryonic germ layers. Usually found in ovaryand testis. Produced experimentally in animals byinjecting pluripotent stem cells, in order to determinethe stem cells’ abilities to differentiate into varioustypes of tissues.Thiazolidinediones – A class of antidiabetes drugsthat enhances the activity of insulin.F-9
Appendix F: Glossary and TermsThrombopoietin – Growth factor for the proliferationand differentiation of platelet forming cells calledmegakaryocytes.Thymus – A lymphoid organ located in the upperchest cavity. Maturing T cells go directly to thethymus, where they are “educated” to discriminatebetween self and foreign proteins. (See toleranceinduction.)Tissue culture – Growth of tissue in vitro on an artificialmedium for experimental research.Tolerance – A state of specific immunologic unreponsiveness.Individuals are normally tolerant to theirown cells and tissues. Autoimmune diseases occurwhen tolerance fails.Tolerance induction – The “education” process thatT cells undergo to discriminate between self andforeign proteins. This process takes place primarily inthe thymus. In addition to inactivating or deleting selfreactiveT cells, those T cells that can recognize thebody’s MHC proteins, but not be activated solely bythis recognition, are also selected to leave the thymus(circulate through the body).Totipotent – Having unlimited capability. The totipotentcells of the very early embryo have the capacityto differentiate into extra embryonic membranes andtissues, the embryo, and all postembryonic tissuesand organs.Transaminase – An enzyme that catalyzes chemicalreactions in the body in which an amino group istransferred from a donor molecule to a recipientmolecule.Transcription – Making an RNA copy from asequence of DNA (a gene). Transcription is the firststep in gene expression.Transcription factor – Molecules that bind to RNApolymerase III and aid in transcription.Transgene – A gene that has been incorporatedfrom one cell or organism and passed on tosuccessive generations.Translation – The process of forming a proteinmolecule at a ribosomal site of protein synthesis frominformation contained in messenger RNA.Trophectoderm – The outer layer of the developingblastocyst that will ultimately form the embryonic sideof the placenta.Trophoblast – The extraembryonic tissue responsiblefor negotiating implantation, developing into theplacenta, and controlling the exchange of oxygenand metabolites between mother and embryo.Trypsin – An enzyme that digests proteins. Often usedto separate cells.Undifferentiated – Not having changed to becomea specialized cell type.Unipotent – Refers to a cell that can only develop ina specific way to produce a certain end result.Vascular – Composed of, or having to do with, bloodvessels.Villi – Projections from the surface, especially of amucous membrane. If the projection is minute, as ina cell surface, it is called a microvillus.Vimentin – The major polypeptide that joins withother subunits to form the intermediate filamentcytoskeleton of mesenchymal cells. Vimentin mayalso have a role in maintaining the internalorganization of certain cells.White blood cell (WBC) – The primary effector cellsagainst infection and tissue damage. WBCs areformed from the undifferentiated stem cell that cangive rise to all blood cells. Also known as a leukocyte.X inactivation – The normal inactivation of one of thetwo X chromosomes in females.Y chromosome – The chromosome which determinesmale gender.Yolk sac – Vital to the embryo for the formation ofprimordial and other cells that form the embryo. Inmammals, it is small and devoid of a yolk.Zona pellucida – A thick, transparent noncellularlayer that surrounds and protects the oocyte.Zygote – A cell formed by the union of male andfemale germ cells (sperm and egg, respectively).F-10
Appendix F: Glossary and TermsAppendix F.ii.TERMSAGM – The region where the aorta, gonads, and fetalkidney mesh.ALS – A myotrophic lateral sclerosis. Also known asLou Gehrig’s disease.BME – Beta-mercaptoethanol.BMP-1 to BMP-9 – Bone morphogenetic proteins thatare signaling molecules.BRCA1 – Breast Cancer Gene 1.BRCA2 – Breast Cancer Gene 2.C/EBC – CCAAT/Enhancer binding protein.CD4 – Helper T cells that are instrumental in initiatingan immune response by supplying help in the formof special cytokines to both CD 8 cytotoxic T cellsand B cells.CD8 – Cytotoxic (killer) T cells that are capable ofkilling infected cells once activated by cytokinessecreted by antigen-specific CD4 helper T cells.CMV – Cytomegalovirus.EBs – Embryoid bodies.EG – Embryonic germ cell.ES – Embryonic stem cell.FACS – Fluorescence-activated cell sorting.Fas receptor (CD95) – Fatty acid synthase.FGF-1 to FGF-10 – Fibroblast growth factor 1 to 10.A growth factor molecule.GATA4 – Transcription factor. Important in embryonicstem differentiation into yolk sac endoderm.GATA6 – Important for embryonic stem celldifferentiation into heart smooth muscle.GCSF – Granulocyte-colony stimulating factor.Gdf-5 – Growth/differentiation factor – 5. A growthfactor molecule.GDNF – Glial cell-derived neurotrophic factor. Agrowth factor molecule.GFP – Green fluorescent protein.Gp130 – Glycoprotein. Signal transducing receptorof Cytokines.Gsc – Goosecoid. A signaling molecule.hCNS-SC – Human central nervous system stem cell.Hesx1 – Pituitary transcription factor.Hex – Hexosaminidase. Enzyme for processinglipid (fat).HGF – Hepatic growth factor molecule. Also ascatter factor.HLAs – Human leukocyte antigens.Hoxa-d – Homeobox-containing a to d.A transcription factor.HPC – Hematopoietic progenitor cell.HSC – Hematopoietic stem cell.ICM – Inner Cell Mass.IVF – In vitro fertilization.LIF – Leukemia inhibitory factor. A growth factormolecule.Lim1 – A transcription factor molecule.Mac-1 (CD11b) – Antigen found in blood cells.Indicative of murine and progenitor cells.MPC – Mesenchymal progenitor cell.MR4 – Metabolic regulator. Important for electrontransportand ATP synthesis.MSC – Mesenchymal stem cell.Myf-5 – Myogenic regulatory factor molecule.NK – Natural killer lymphocytes.NSC – Neural stem cell.Oct4 – Octamer binding gene. Important for germcell generation.Otx2 – A transcription factor molecule.Pax-1 to Pax-9 – Paired box 1-9. A transcription factormolecule.PDGF – Platelet-derived growth factor.F-11
Appendix F: Glossary and TermsPDX-1 – A transcription factor molecule.PECAM 1 – Platelet. Endothelial cell adhesionmolecule.SDF-1/CXCR4 – Stromal-derived factor and itsreceptor.SHH – Sonic hedgehog.SMA – Alpha-smooth muscle actin.SP – Side population stem cell.Stat 3 – Signal Transducers and Activators ofTranscription 3.T3 – Triiodothyronine. A thyroid hormone important forhematopietic cells.TGF-1 to TGF-5 – Transforming growth factors.TPO/mpl – Thrombopoietin and receptor.VEGF – Vascular endothelial growth factor.Wnt1 – A signaling molecule.XIST – X-inactive specific transcript. Uncertainfunction.F-12
APPENDIX G:INFORMATIONALRESOURCESAppendix G.i.PERSONS INTERVIEWEDPeter AndrewsUniversity of SheffieldSheffield, UKPiero AnversaNew York Medical CollegeValhalla, NYNissim BenvenistyHebrew UniversityTel Aviv, IsraelChristopher BjornsonUniversity of WashingtonSeattle, WAHelen BlauStanford UniversityPalo Alto, CADavid BodineNational Human GenomeResearch InstituteBethesda, MDAriff BongsoNational University HospitalSingaporeSusan Bonner-WeirHarvard UniversityCambridge, MARichard BurtNorthwestern Medical CenterChicago, ILKaren ChandrossAventis Pharmaceuticals Inc.Bridgewater, NJRichard ChildsNational Heart, Lung, and BloodInstituteBethesda, MDDennis ChoiWashington University School ofMedicineSt. Louis, MOAlan ColmanPPL, LtdBlacksburg, VAJonathan DinsmoreDiacrin, Inc.Charlestown, MACynthia DunbarNational Heart, Lung, and BloodInstituteBethesda, MDStephen DunnettCardiff UniversityCardiff, WalesElaine DzierzakErasmus UniversityRotterdam, HollandConnie EavesUniversity of British ColumbiaVancouver, BC CanadaChris EvansHarvard UniversityCambridge, MAJames FallonUniversity of California, IrvineIrvine, CAGary FathmanStanford UniversityPalo Alto, CAMeri FirpoUniversity of California atSan FranciscoSan Francisco, CAItzhak FischerMCP Hahnemann UniversityPhiladelphia, PACurt FreedUniversity of ColoradoDenver, COFred GageSalk InstituteLa Jolla, CARichard GardnerUniversity of OxfordOxford, UKJohn GearhartJohns Hopkins UniversityBaltimore, MDSteven GoldmanCornell UniversityNew York, NYMargaret GoodellBaylor College of MedicineHouston, TXG-1
Appendix G: Information ResourcesJoel HabenerHarvard UniversityCambridge, MANeil HanleyUniversity of SouthamptonSouthampton, UKAlberto HayekUniversity of California, San DiegoSan Diego, CARobert HawleyAmerican Red CrossRockville, MDThomas HoNeuronyx CorporationMalvern, PARonald HoffmanUniversity of Illinois Cancer CenterChicago, ILOle IsacsonHarvard Medical SchoolBoston, MASilviu ItescuColumbia UniversityNew York, NYJosef Itskovitz-EldorTechnion-Israel Institute ofTechnologyHaifa, IsraelDouglas KerrJohns Hopkins UniversityBaltimore, MDJeffrey KordowerRush Presbyterian Medical CenterChicago, ILKristy KraemerNational Institute of Allergy andInfectious DiseasesBethesda, MDWilliam LangstonParkinsonís InstituteSunnyvale, CARobert LanzaAdvanced Cell TechnologiesCambridge, MAIhor LemischkaPrinceton UniversityPrinceton, NJFred LevineUniversity of California, San DiegoSan Diego, CAJohn McDonaldWashington University School ofMedicineSt. Louis, MORon D. McKayNational Institute of NeurologicalDisorders and StrokeBethesda, MDJeffrey MacklisHarvard Medical SchoolBoston, MADouglas MeltonHarvard UniversityCambridge, MAEva MezeyNational Institute of NeurologicalDisorders and StrokeBethesda, MDShin-Ichi NishikawaKyoto University Medical SchoolKyoto, JapanJon OdoricoUniversity of WisconsinMadison, WIWarren OlanowMt. Sinai School of MedicineNew York, NYThomas OkarmaGeron Inc.Menlo Park, CADonald OrlicNational Human GenomeResearch InstituteBethesda, MDMitradas PanickerNational Centre for BiologicalSciencesBangalore, IndiaAmmon PeckUniversity of FloridaGainesville, FLRoger PedersenUniversity of California at SanFranciscoSan Francisco, CAMartin PeraMonash UniversityMelbourne, AustraliaVijayakumar RamiyaIxion BiotechnologyAlachua, FLMahendra RaoNational Institute on AgingBethesda, MDEugene RedmondYale UniversityNew Haven, CTJuan ReigUniversidad Miguel HernandezAlicante, SpainCamillo RicordiUniversity of MiamiMiami, FLPamela Gehron RobeyNational Institute of Dental andCraniofacial ResearchBethesda, MDJanet RossantUniversity of TorontoOntario, CanadaJeffrey RothsteinJohns Hopkins UniversityBaltimore, MDManfred RuedigerCardion, Inc.Erkrath, GermanyG-2
Appendix G: Information ResourcesHans R. SchölerUniversity of PennsylvaniaKennett Square, PAJames ShapiroUniversity of AlbertaEdmonton, CanadaKarl SkoreckiTechnion ñ Israel Institute ofTechnologyHaifa, IsraelAustin SmithUniversity of EdinburghEdinburgh, ScotlandEvan SnyderHarvard Medical SchoolBoston, MAJames ThomsonUniversity of Wisconsin ñ MadisonMadison, WISatish ToteyNational Institute of ImmunologyNew Delhi, IndiaPantelis TsoulfasUniversity of Miami School ofMedicineMiami, FLAnn Tsukamoto<strong>Stem</strong> <strong>Cells</strong>, Inc.Palo Alto, CAGary Van ZantUniversity of Kentucky MedicalCenterLexington, KYCatherine VerfallieUniversity of MinnesotaMinneapolis, MNInder M. VermaThe Salk InstituteLa Jolla, CAIrving WeissmanStanford University Medical SchoolStanford, CAEsmail ZanjaniUniversity of NevadaReno, NVLeonard ZonHarvard Medical SchoolBoston, MAG-3
Appendix G: Information ResourcesAppendix G.ii.SPECIAL CONTRIBUTIONSJohn GearhartJohns Hopkins UniversityBaltimore, MDRon D. McKayNational Institute of NeurologicalDisorders and StrokeBethesda, MDPamela Gehron RobeyNational Institute of Dental andCraniofacial ResearchBethesda, MDJanet RossantUniversity of TorontoOntario, CanadaJames ThomsonUniversity of Wisconsin – MadisonMadison, WIG-4
Appendix G: Information ResourcesAppendix G.iii.SPECIAL ACKNOWLEDGMENTSCynthia AllenSilver Spring, MDDeborah M. BarnesBethesda, MDMarty BrotemarkleOffice of Science Policy &Planning, NIHBethesda, MDElizabeth Miller DeanOffice of Science Policy &Planning, NIHBethesda, MDGregory J. DowningOffice of Science Policy &Planning, NIHBethesda, MDDonald M. Fink, Jr.U.S. Food and Drug AdministrationBethesda, MDBruce FuchsOffice of Science Education, NIHBethesda, MDCharles Anderson Goldthwaite, Jr.Charlottesville, VAMary GroeschOffice of Biotechnology Activities,NIHBethesda, MDCelia HooperOffice of Intramural Research, NIHBethesda, MDRobin I. KawazoeOffice of Science Policy &Planning, NIHBethesda, MDKristy KraemerNational Institute of Allergy andInfectious DiseasesBethesda, MDRobert LevinOffice of Science Policy &Planning, NIHBethesda, MDMarina O’ReillyOffice of Biotechnology Activities,NIHBethesda, MDAmy P. PattersonOffice of Biotechnology Activities,NIHBethesda, MDPeggy SchnoorOffice of Science Policy &Planning, NIHBethesda, MDRobert TaylorFalls Church, VADat TranOffice of Science Policy &Planning, OSPBethesda, MDNancy TouchetteScience Designs, inc.Monkton, MDJeff WalkerSutter DesignLanham, MDMEDICAL ILLUSTRATIONSTerese WinslowMedical IllustrationAlexandria, VACaitlin DuckwallDuckwall ProductionsBaltimore, MDLydia KibiukBaltimore, MDRob DuckwallDuckwall ProductionsBaltimore, MDG-5
Appendix G: Information ResourcesThis page intentionally left blankG-6
National Institutes of HealthDepartment of Health and Human ServicesJune 2001