Caring - Dartmouth-Hitchcock
Caring - Dartmouth-Hitchcock
Caring - Dartmouth-Hitchcock
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
12<br />
<strong>Caring</strong> for patients with spinal injuries is a<br />
high-risk endeavor. Injuries to the spine<br />
can be difficult to rule out, and they<br />
carry the risk of potentially devastating<br />
neurological complications.<br />
“That means we have to prove nothing<br />
is wrong with patients before removing<br />
devices that immobilize their neck<br />
and spine,” says JoElla McCarragher,<br />
RN, MSN, a clinical nurse specialist in<br />
DHMC’s Level 1 Trauma Center.<br />
Prolonged cervical immobilization<br />
has its own set of complications. “For<br />
starters, it’s uncomfortable for those<br />
patients who are conscious,” says<br />
McCarragher. “It affects how we can<br />
position patients—if we can’t sit them up<br />
in a natural position for breathing or<br />
coughing, they may have to be intubated<br />
longer which leaves them more at<br />
risk for respiratory difficulties and potential<br />
pneumonias.”<br />
Other complications include delayed<br />
mobilization and its associated risks. “The<br />
longer they are bedridden, the higher the<br />
chance they may develop complications<br />
such as blood clots in their legs,” she<br />
explains. “It also delays our ability to get<br />
them into physical or occupational therapy,<br />
and they become more susceptible<br />
to skin breakdowns and pressure ulcers.”<br />
Identifying Areas for Improvement<br />
To better manage this dilemma, McCarragher<br />
and her colleague Ingrid Mroz,<br />
RN, MSN, a clinical nurse specialist in the<br />
Intensive Care Unit (ICU), spearheaded a<br />
collaborative effort—utilizing an evidence-based<br />
nursing model—to improve<br />
the care of patients with spinal injuries.<br />
“We recognized early on that we<br />
couldn’t just focus on the ICU—we<br />
needed to look at the whole spectrum of<br />
care for these patients,” says McCarragher.<br />
“So we pulled together a diverse<br />
group of clinicians from the emergency<br />
department (ED), neuroscience, pediatrics,<br />
the ICU, the surgical floor, the<br />
trauma program, orthopedics, physical<br />
therapy, and discharge planning.”<br />
The multidisciplinary task force began<br />
meeting monthly in February 2002.<br />
Evidence-Based Practices Improve Trauma Care<br />
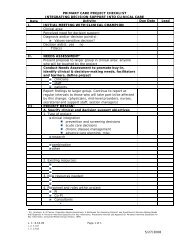
The next steps for the task<br />
force will be measuring<br />
post-implementation<br />
outcomes which will<br />
include tracking the time<br />
patients spend on<br />
backboards, examining<br />
the thoroughness of<br />
orders, and measuring<br />
the timeframe for<br />
replacing extrication<br />
collars with in-house<br />
collars.<br />
Several areas were targeted for improvement.<br />
“One of our biggest challenges<br />
was we had multiple services managing<br />
patients,” she says. “This led to problems<br />
like inconsistent precautions, prolonged<br />
backboard time for patients, and care<br />
issues associated with cervical collars.”<br />
A Standardized Approach<br />
To address the inconsistencies, the task<br />
force developed a standardized order set<br />
for spine injury management. “We<br />
agreed that the orders should be written<br />
the same way, whether the patient was in<br />
general surgery, trauma, neurology, or<br />
orthopedics,” McCarragher says. “We<br />
implemented it in December 2002,<br />
revised it after six months, and continue to<br />
monitor it monthly—it’s been very helpful.”<br />
In conjunction with the group’s efforts,<br />
the ED initiated a project to reduce the<br />
time some patients were spending immobilized<br />
on backboards. “They developed<br />
a policy and procedure that allows nurses<br />
to make the assessments—the result is lowrisk<br />
patients are now removed from backboards<br />
more quickly.”<br />
McCarragher also felt that an assessment<br />
of cervical collars needed to be<br />
done. “We looked at the literature and<br />
had the two leading companies come in<br />
and present their products,” she says.