PM conference programme_2016.04.05_concise_Clean(Latest)
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
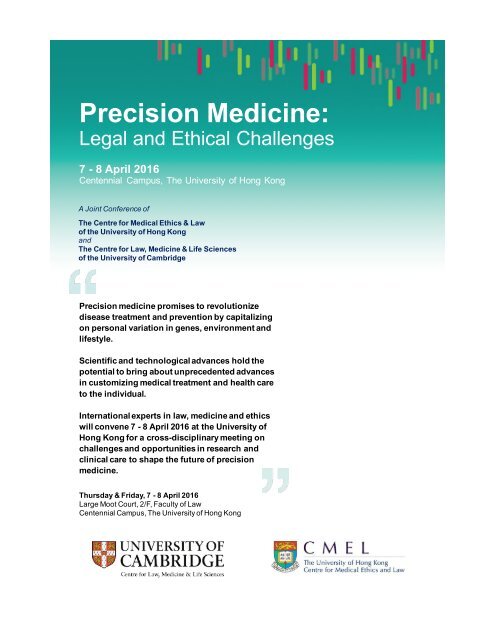
Precision$Medicine:<br />
Legal&and&Ethical&Challenges<br />
7$C 8$April$2016<br />
Centennial& Campus,&The&University&of&Hong&Kong<br />
A"Joint"Conference"of<br />
The$Centre$for$Medical$Ethics$&$Law<br />
of$the$University$of$Hong$Kong<br />
and<br />
The$Centre$for$Law,$Medicine$&$Life$Sciences<br />
of$the$University$of$Cambridge<br />
Precision$medicine$promises$to$revolutionize$<br />
disease$treatment$and$prevention$by$capitalizing$<br />
on$personal$variation$in$genes,$environment$and$<br />
lifestyle.$$<br />
Scientific$and$technological$advances$hold$the$<br />
potential$to$bring$about$unprecedented$advances$<br />
in$customizing$medical$treatment$and$health$care$<br />
to$the$individual.<br />
International$experts$in$law,$medicine$and$ethics$<br />
will$convene$7$C 8$April$2016$at$the$University$of$<br />
Hong$Kong$for$a$crossCdisciplinary$meeting$on$<br />
challenges$and$opportunities$in$research$and$<br />
clinical$care$to$shape$the$future$of$precision$<br />
medicine.<br />
Thursday$&$Friday,$7$C 8$April$2016<br />
Large&Moot&Court,&2/F,&Faculty&of&Law<br />
Centennial&Campus,&The&University&of&Hong&Kong
Programme<br />
Thursday, 7 April, 2016<br />
8:00am – 9:00am Registration<br />
9:00am – 9:10am Welcome<br />
Terry Kaan & Kathy Liddell<br />
9:10am – 9:40am Opening Address<br />
Ron Zimmern: “Health Systems and the Future of Personalized Medicine:<br />
A Population Health Perspective”<br />
I. CHALLENGES IN THE IMPLEMENTATION OF PRECISION MEDICINE<br />
►► PART 1: THE HEALTH CARE SYSTEM<br />
9:40am – 10:20am Keynote<br />
Henry T. Greely: “Precision Medicine: The Ethical, Legal, and Practical<br />
Challenges Ahead”<br />
10:20am – 10:50am Morning Break<br />
10:50am – 11:30am Presentations<br />
Jeffrey M. Skopek: “Personalized Rationing: The Law and Ethics of<br />
Differentiation”<br />
Ock-Joo Kim and Yoon-Jung Chang: “Precision Medicine Ethics:<br />
Prospects on Clinical Application and Ethical Issues”<br />
11:30am – 1:00pm Roundtable<br />
Chair: Hilary Burton<br />
1:00pm – 2:00pm Lunch [1/F Podium, Cheung Yu Tung Tower, Centennial Campus, The<br />
University of Hong Kong]<br />
►► PART 2: MEDICAL TREATMENT<br />
2:00pm – 2:40pm<br />
2:40pm – 4:30pm<br />
4:30pm – 6:00pm<br />
7:00pm –<br />
Keynote<br />
I. Glenn Cohen: “Legal and Ethical Issues in Using Big Data for Predictive<br />
Analytics in Health Care”<br />
Presentations<br />
Terry Kaan: “Genetic Information and the Family: the Future of the Duty<br />
of Disclosure and the Limits of Confidentiality”<br />
Tracey Evans Chan: “Regulatory Challenges of Innovative Therapeutics<br />
and Diagnostics in Medical Practice”<br />
Afternoon Break<br />
Colm McGrath: “Liability for failure to disclose and the challenge of<br />
precision medicine”<br />
Darrell Rowbottom: “On Probabilities in Personalized Medicine”<br />
Roundtable<br />
Chair: Ron Zimmern<br />
Private Dinner<br />
Speakers and Invited Guests<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 1
Friday, 8 April, 2016<br />
II. CHALLENGES IN THE DEVELO<strong>PM</strong>ENT OF PRECISION MEDICINE<br />
►► PART 1: FOUNDATIONAL RESEARCH<br />
9:00am – 9:40am<br />
9:40am – 11:30am<br />
11:30am – 1:00pm<br />
1:00pm – 2:00pm<br />
Keynote<br />
Bartha Maria Knoppers: “Activating the Right of Citizens to Benefit from<br />
Scientific Advances”<br />
Presentations<br />
Kazuto Kato: “Genomic Medicine in Japan: Recent Changes in the<br />
Government Policy, and New Ethical and Legal Challenge”<br />
Yann Joly: “Controlled Data Access for Precision Medicine: An Acceptable<br />
Trade-off?”<br />
Morning Break<br />
Alison Hall: “Harm, Discretion or Duty: The Changing Nature of the<br />
Return of Individualized Results in Genomics Research”<br />
Janice Tsang: “Precision Medicine for Cancer Care - Prime Time versus<br />
Provocation Threat?”<br />
Roundtable<br />
Chair: Henry T. Greely<br />
Lunch<br />
►► PART 2: TRANSLATIONAL MEDICINE<br />
2:00pm – 2:40pm<br />
2:40pm – 4:30pm<br />
4:30pm – 6:00pm<br />
6:00pm – 6:10pm<br />
7:00pm –<br />
Keynote<br />
Donald Chalmers: “Has the Biobank Bubble Burst: A Translational<br />
Challenge”<br />
Presentations<br />
Kathy Liddell & John Liddicoat: “The Changing IP Landscape for<br />
Precision Medicine”<br />
Chih-Hsing Ho: “From Bench to Bedside: Secondary Use of Health Data<br />
for Precision Medicine”<br />
Afternoon Break<br />
Stuart Hogarth: “Lost on Planet Biomarker? Standards, Pathways, Carrots<br />
and Sticks for Diagnostic Development in the Post-genomic Era”<br />
Timo Minssen: “Lost in Translation? Opportunities & Risks of Increased<br />
Research & Clinical Trials Data Transparency”<br />
Roundtable<br />
Chair: I. Glenn Cohen<br />
Closing Remarks & Acknowledgements<br />
Jeffrey M. Skopek<br />
Official Conference Dinner<br />
Speakers, Delegates, and Invited Guests<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 2
Abstracts<br />
Thursday, 7 April, 2016<br />
I. CHALLENGES IN THE IMPLEMENTATION OF PRECISION MEDICINE<br />
►► PART 1: THE HEALTH CARE SYSTEM<br />
Dr Ron Zimmern, Chairman, PHG Foundation<br />
Health Systems and the Future of Personalized Medicine: A Population Health Perspective<br />
Personalized or precision medicine places patients at the centre of health care. It emphasizes their individuality as<br />
persons with both unique biology and personal values and beliefs. This focus is no means new, but in recent<br />
decades has been overshadowed by evidence based medicine which uses results from clinical trials and population<br />
based studies to provide a more standardized system of patient management. Because of ageing populations,<br />
increasing patient expectations and technological advances health systems all over the world have also been faced<br />
with rising costs. In this talk I will (a) outline the essential characteristics of personalized medicine (b) emphasize<br />
the biological heterogeneity of populations using insights from modern genomic science (c) discuss how a refocus<br />
on the individual and placing the patient at the centre of a health system may provide one way of reducing health<br />
care costs and (d) show how these considerations will require much by way of philosophical and legal analysis and<br />
insights from the social sciences.<br />
Professor Henry T. Greely, Deane F. and Kate Edelman Johnson Professor of Law and Professor, by<br />
courtesy, of Genetics, Stanford University; Director, Stanford Center for Law and the Biosciences<br />
Precision Medicine: The Ethical, Legal, and Practical Challenges Ahead<br />
The goal of precision medicine, of course, is not research but medicine, the delivery of health care in ways that<br />
improve the wellbeing of people and of their societies. The potential for improving healthcare through precision<br />
medicine is vast, although perhaps somewhat more limited and somewhat slower in arriving, than in the most<br />
expansive hopes. But, as with any good new technology, precision medicine will also raise challenges as we try to<br />
incorporate it in ways that maximize its benefits and minimize any risks or harms. These include complex issues of<br />
safety regulation, reimbursement, physician duties, and patient privacy and other rights. Effort spent now<br />
considering how to manage foreseeable challenges (and how to spot and respond to unexpected problems) should<br />
prove very useful. My talk will try both to highlight some of the difficulties and suggest some possibly useful<br />
responses.<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 3
Dr Jeffrey M. Skopek, Lecturer in Medical Law, Ethics, and Policy, Faculty of Law, University of<br />
Cambridge; Deputy Director, Centre for Law, Medicine and Life Sciences<br />
Personalized Rationing: The Law and Ethics of Differentiation<br />
Some of the greatest challenges that we will face in implementing precision medicine will arise from the ways in<br />
which increased precision destabilizes foundational categories and concepts in our law and ethics. This can be seen<br />
in the pharmacogenomic stratification of patient populations, which will give rise to new and difficult questions<br />
about the conditions in which an individual patient should be able to differentiate himself from a group of similar<br />
patients in order to gain access to a treatment that is not available to the group—and conversely, the conditions in<br />
which a patient should be able to resist being differentiated from a group in order to avoid losing access to a<br />
treatment. In this presentation, I will identify and analyze some previously unrecognized challenges concerning the<br />
law and ethics of differentiation in this area. In doing so, I will highlight the fact that advances precision medicine<br />
will both benefit and harm patients, moving us closer not only to personalized treatment, but also to personalized<br />
rationing.<br />
Professor Ock-Joo Kim, Professor and Chair in the Department of Medical History and Medical<br />
Humanities, Seoul National University College of Medicine<br />
Dr Yoon-Jung Chang, Associate Professor of Department of Cancer Control and Policy, Graduate<br />
School of Cancer Science and Policy, National Cancer Center; Associate scientist, Hospice &<br />
Palliative Care Branch, National Cancer Center; Expert secretory, Team of legislation, ethics &<br />
policy, Precision Medicine Working Group, Ministry of Health & Welfare, South Korea<br />
Precision Medicine Ethics: Prospects on Clinical Application and Ethical Issues<br />
Precision medicine is one of the programs that follow-up human genome project, in the hope of developing clinical<br />
applications from the personalized genome information. Individual patient's sequence data in comparison with the<br />
database from a larger population is expected to identify specific variations that contribute to personalized<br />
treatment. This effort depends on the availability of biobanks for general population and for particular disease<br />
groups, such as cancer, for which genomic variations exert large enough influence on the prognosis. Various<br />
treatment regimens must be developed unique to the patterns of variations. Ethical and legal issues also need to be<br />
resolved toward these developments. In South Korea, discussion on the possibility of personalized medicine<br />
became active since 2010, including forums and grants supported by Ministry of Health. Korea has several strengths<br />
in the infrastructure toward the development of precision medicine. Korea Center for Disease Control has<br />
established large biobanks for population-based cohorts and patient cohorts. Korean National Health Insurance<br />
Service maintains health care data for all Koreans that can be used for research. There is a strong infrastructure for<br />
clinical trials including cancer treatment. Capacity for developing new drugs and diagnostic technologies has also<br />
significantly increased. This paper overviews the prospects on precision medicine in Korean contexts, particularly<br />
focusing on ethical and legal issues.<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 4
►► PART 2: MEDICAL TREATMENT<br />
Professor I. Glenn Cohen, Professor of Law, Harvard Law School; Director, Petrie-Flom Center for<br />
Health Law Policy, Biotechnology, and Bioethics<br />
Legal and Ethical Issues in Using Big Data for Predictive Analytics in Health Care<br />
This talk will discuss a series of legal and ethical issues in using big data for predictive analytics in health care — the<br />
use of electronic algorithms that forecast clinical events in real time to improve patient outcomes and reduce costs.<br />
The talk will cover the 4 phases of such projects — collection of data to build a model, building a model, testing<br />
the model in real world settings, and wide scale deployment of the model.<br />
Mr Terry Kaan, Associate Professor of Law, The University of Hong Kong; Co-Director, Centre for<br />
Medical Ethics and Law<br />
Genetic Information and the Family: the Future of the Duty of Disclosure and the Limits of<br />
Confidentiality<br />
Current paradigms of the legal and ethical relationship between physicians and patients are largely focused on the<br />
rights (and obligations) of the individual patient. What are the implications for current legal and ethical paradigms<br />
with the advent of precision medicine, and in particular, if and when whole genome sequencing becomes an<br />
ubiquitous and standard procedure? What legal and moral implcations are raised for clinicians in the acquisition<br />
and holding of such genetic information, not only at the time of the acquisition of the data, but also for the future<br />
as as medical and informational technology advances to make possible and reliable what was not at the time of<br />
sequencing? This presentation focuses in particular on the legal and ethical burdens which may be unwittingly<br />
assumed by clinicians (and researchers) for the future when genetic data acquired many years ago may potentially<br />
give rise to unanticipated liability in the future. Clinicians may not be under a legal or ethical obligation to test for<br />
conditions for which no reliable test (both as to test methodology as well as to the predictive value of the result)<br />
currently exists. But as technology and genetic knowledge advances, do the same clinicians and data holders acquire<br />
an unanticipated burden and obligation if and when technology makes genetic analysis for these conditions cheap<br />
and reliable, to the extent that they become standard professional practice? Is the current focus of the common<br />
law on individual rights justified (particularly in the context of the duty of confidentiality, and in the duty to give<br />
full disclosure of risks) in the context of heritable genetic data shared by closely related family members tenable for<br />
the future, particularly where wishes (and interests) of individual family members are in conflict?<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 5
Mr Tracey Evans Chan, Associate Professor, Faculty of Law, National University of Singapore<br />
Regulatory Challenges of Innovative Therapeutics and Diagnostics in Medical Practice<br />
The advent of new technologies in precision medicine raises the challenge of preparing the healthcare regulatory<br />
framework for the potential wave of new therapeutics and associated diagnostics. This presentation will examine<br />
some of the issues that arise in ensuring that these new treatments/diagnostics are safe and effective.<br />
Mr Colm McGrath, WYNG Research Fellow in Medical Law and Ethics, Trinity Hall, University of<br />
Cambridge<br />
Liability for failure to disclose and the challenge of precision medicine<br />
This paper examines the role of personalised medicine in medical intervention and treatment. It does so by focusing<br />
on the law surrounding risk disclosure and securing the patient's consent to treatment in the UK. This is an area of<br />
law which has undergone significant change in the last year following the decision of the UK Supreme Court in<br />
Montgomery v Lanarkshire Health Board. That decision, which has introduced uncertainty as to when a clinician<br />
ought to offer a particular treatment as an alternative to other suggested treatments, has the potential to greatly<br />
influence the availability of some precision treatments in practice in the UK.<br />
Professor Darrell Rowbottom, Head of Philosophy & Professor, Lingnan University<br />
On Probabilities in Personalized Medicine<br />
Personalised medicine may involve personalised, ‘one off’, treatments. But how might we arrive at reasonable<br />
probability estimates for the success of such treatments? Imagine, for example, that a new drug is synthesised in<br />
order to treat a patient. This drug has never been tested before. Moreover, in so far as it is ’tailor made', it is not<br />
possible to test it satisfactorily on anyone other than the patient. So how could a doctor have reasonable grounds<br />
for prescribing the drug? Call this ‘the problem of the untestable drug'. In this talk, I’ll propose a solution to it.<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 6
Friday, 8 April, 2016<br />
II. CHALLENGES IN THE DEVELO<strong>PM</strong>ENT OF PRECISION MEDICINE<br />
►► PART 1: FOUNDATIONAL RESEARCH<br />
Professor Bartha Maria Knoppers, Director, Centre of Genomics and Policy, Faculty of Medicine,<br />
Department of Human Genetics, McGill University<br />
Activating the Right of Citizens to Benefit from Scientific Advances<br />
The Framework for Responsible Sharing of Genomic and Health Related Data of the GA4GH is founded on<br />
article 27 of the Universal Declaration of Human Rights. Article 27 maintains the right of citizens to benefit from<br />
scientific progress and was enshrined in later binding international legal instruments. How has this right been<br />
interpreted? What does it (or could it) mean? The position that we need to "activate " this right will create<br />
obligations on governments to facilitate and promote data sharing. Supporting this positive obligation may serve<br />
to change the imbalance of power between citizens and health researchers, data stewards and physicians as we<br />
move more towards translational medicine.<br />
Professor Kazuto Kato, Professor of Biomedical Ethics and Public Policy, Graduate School of<br />
Medicine, Osaka University, Japan<br />
Genomic Medicine in Japan: Recent Changes in the Government Policy, and New Ethical<br />
and Legal Challenge<br />
Dr Yann Joly, Associate Professor, Faculty of Medicine, Department of Human Genetics, McGill<br />
University; Research Director, Centre of Genomics and Policy<br />
Controlled Data Access for Precision Medicine: An Acceptable Trade-Off?<br />
The major goal of translational research in precision medicine will be to link genomic information to personal<br />
information collected periodically, including the patient’s lifestyle, clinical history, and response to treatment. These<br />
rich datasets will need to be securely shared between researchers from both the private and public sectors to<br />
promote rapid scientific advancement and the development of new diagnostics and treatments. ‘’Controlled<br />
access’’, a process where researchers requesting access to the data must complete an access agreement for personal<br />
and institutional identification, can substantially improve the security of such data sharing initiatives. This<br />
presentation will highlight the main component of the controlled access approach to data sharing focussing on its<br />
potential for research in personalized medicine. The legal, ethical and social challenges and opportunities of using<br />
such an approach will be critically assessed.<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 7
Ms Alison Hall, Head of Humanities, PHG Foundation<br />
Harm, Discretion or Duty: The Changing Nature of the Return of Individualized Results in<br />
Genomics Research<br />
The advent of genomic sequencing has generated a rich debate about the potential for generating, interpreting,<br />
validating and reporting incidental and secondary findings. The view that it is desirable to ‘actively look’ for well<br />
characterised clinically actionable secondary findings is gaining traction, provided that this can be justified in the<br />
participant’s or patient’s best interests. There is less clarity about how these developments might impact on<br />
researchers undertaking genetics and genomics research and how these might change the nature of the duties and<br />
responsibilities that researchers owe to research participants and the liabilities that might result. This presentation<br />
assesses these developments and the extent to which adopting personalised approaches within genomic research<br />
might change the nature of the relationship between the researcher and research participant. It also explores some<br />
wider consequences for research design, management and funding.<br />
Dr Janice Tsang, Specialist in Medical Oncology, Clinical Assistant Professor Department of Medicine, The<br />
University of Hong KongFounding Convenor, Hong Kong Breast Oncology Group<br />
Precision Medicine for Cancer Care - Prime Time versus Provocation Threat"?<br />
Cancer is an aging disease and a public health issue. With the emerging aging population, cancer has become an<br />
complex health threat with various unmet needs of patients living with the disease. Over the past 2 decades, there<br />
have been great breakthroughs in the changing landscape of the management of cancer - from the advent of<br />
targeted therapy to personalized treatment to the current second wave of personalized medicine with “Precision<br />
Medicine” which involves the increasing visibility of molecular genomic profiling and the potential added value of<br />
next generation sequencing which is now moving towards to the clinic at a fast tempo.<br />
While cancer patients and family members are having high expectation on the holistic cancer care and their<br />
mindfulness with “Precision Medicine” and the easy access to new information of research and development, this<br />
presentation is going to give a bird’s eye view of the current status of Precision Medicine in oncology with updates<br />
of the potential clinical application, yet the attempt to comment whether this is the prime time for all cancer<br />
patients, or this is just the end of another beginning and the emerging potential ethical challenge with some of the<br />
controversies coming from the harvest of translational research.<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 8
►► PART 2: TRANSLATIONAL MEDICINE<br />
Professor Donald Chalmers, Distinguished Professor, University of Tasmania; Deputy-Director,<br />
Centre for Law and Genetics<br />
Has the Biobank Bubble Burst: A Translational Challenge<br />
Biobanks have been heralded as essential tools for translating biomedical research into practice and for driving<br />
precision medicine towards improved pathways for healthcare treatment and services. Biobanking has made<br />
significant progress in relation to their ethical, legal and social governance, however, operational, sustainability and<br />
funding challenges have emerged. There are questions about their overall viability and value in light of the<br />
significant resources, particularly funding, required to keep them running. This is largely influenced by, although<br />
not in the least limited to, pressures. This talk reviews four waves of challenges for biobanks since their recognition<br />
in the early 2000s, with reference to six countries, and considers some future challenges. This talk had its genesis<br />
in a discussion and later joint paper on biobanks during the Centre for Health, Law and Emerging Technologies<br />
(HeLEX) <strong>conference</strong> in Oxford UK, co-sponsored by the Centre for Law and Genetics (University of Tasmania)<br />
in 2015.<br />
Dr Kathy Liddell, Herschel Smith Lecturer in Intellectual Property Law; Director, Centre for Law,<br />
Medicine and Life Sciences, University of Cambridge<br />
Dr John Liddicoat, Philomathia Post-Doctoral Research Associate in Intellectual Property Law and<br />
Genetics, Faculty of Law, University of Cambridge<br />
The Changing IP Landscape for Precision Medicine<br />
A difficult, but crucial, challenge for the future of precision medicine is to improve the translation of basic genomic<br />
science into affordable and widely adopted new treatments. This is essential if genomics is to become, as is widely<br />
hoped, an everyday reality in healthcare. One issue is how to raise or recoup funding to meet the significant costs<br />
associated with understanding how genetic correlations work in particular individuals in a clinically useful way. This<br />
is particularly complex in light of the changing landscape of intellectual property incentives for precision medicine.<br />
This presentation focuses on two recent IP developments: (1) the dramatic decrease in the economic strength of<br />
DNA-related patents following several landmark rulings by the US Supreme Court (for example, Alice Corp, Myriad<br />
and Prometheus); and (2) increasing public attention on the IP and access policies for major biobanks, and associated<br />
calls for ‘open innovation’. We will also outline some of the new research questions raised by this changing<br />
landscape. For example, in what ways have the patent strategies and business models of precision medicine<br />
innovators changed? Are other IP rights taking on greater significance?<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 9
Dr Chih-Hsing Ho, Assistant Professor, Academia Sinica, Taiwan<br />
From Bench to Bedside: Secondary Use of Health Data for Precision Medicine<br />
Many biomedical projects have been relying on large consortia of repositories, such as networks of biobanks, to<br />
increase the overall size of bio-samples and data for statistical significance. Nevertheless, the increasing need for<br />
transmission and linkage of health data for secondary usage has brought new challenges to translational research.<br />
The current models and privacy frameworks for the secondary use of health data focus predominately on<br />
techniques and rules of anonymization or de-identification. These data-centric perspectives fail to adequately<br />
address issues such as data control, access and sharing, all of which are imperative to data subjects in terms of<br />
deciding how they would like their health information to be used for future research. This talk will investigate these<br />
challenges, especially with regards to the secondary use of health data in precision medicine. It aims at proposing a<br />
transparent and community-based data sharing model to improve the pitfalls of data-centric models for the<br />
secondary use of health data in translational research.<br />
Dr Stuart Hogarth, Senior Research Fellow, Department of Social Science, Health and Medicine,<br />
King's College London<br />
Lost on Planet Biomarker? Standards, Pathways, Carrots and Sticks for Diagnostic<br />
Development in the Post-genomic Era<br />
In this talk I will situate current debates about the development and regulation of molecular diagnostics in the<br />
broader historical context of longstanding efforts to provide greater conceptual clarity and scientific rigour to<br />
diagnostic research. I will offer some suggestions as to why repeated complaints of poor scientific standard and<br />
calls for reform have had limited impact, review examples of recent initiatives championed by a variety of<br />
institutional actors, and conclude by proposing that current developments may finally offer some hope of significant<br />
and sustained change.<br />
Dr Timo Minssen, Associate Professor of IP & Innovation Law, University of Copenhagen, Centre for<br />
Information & Innovation Law<br />
Lost in Translation? Opportunities & Risks of Increased Research & Clinical Trials Data<br />
Transparency<br />
Recent US and European initiatives reflect a growing policy consensus favoring greater clinical trials and research<br />
transparency. New legislation, publishers and industry-driven projects promote independent verification of drug<br />
data, which provides a better framework for international collaboration. Greater transparency also increases public<br />
trust in research results, drugs and industry and the possibility of facilitating large cross-border clinical trials. Yet,<br />
the costs and concerns associated with opening up research and clinical trial data are also significant—for patients<br />
(protection of personal data and patient privacy), for research (misuse of clinical trial data) and for technology<br />
transfer and commercialization (obstacles to IP protection and increased exposure to litigation). This presentation<br />
will discuss these issues from an interdisciplinary perspective in order to sketch out legal mechanism that could be<br />
useful for unlocking and safe-guarding the full potential of greater transparency.<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 10
Biographies<br />
Dr Hilary Burton, Director, PHG Foundation<br />
Hilary Burton was the PHG Foundation’s Programme Director before<br />
becoming its Director (CEO) in 2010. She is a highly experienced public health<br />
physician who believes passionately that genomic science can, and should be<br />
used by public health professionals alongside the social and environmental<br />
determinants of health to bring about improvements in population health. Her<br />
special interests include the integration of genomics within mainstream<br />
medicine, genetics education for health professionals, and genomics and the<br />
developing world. Hilary trained at St Hugh’s College and The Radcliffe<br />
Hospital, Oxford and became a consultant in public health medicine in 1993.<br />
She was a member of the Department of Health’s Human Genomics Strategy<br />
Group and currently serves on the Joint Committee of Medical Genetics of the<br />
Royal Colleges and the Council for the British Society of Human Genetics. She<br />
is a Fellow of Hughes Hall, Cambridge, and holds an Honorary Lectureship at<br />
the University of Cambridge.<br />
Professor Donald Chalmers, Distinguished Professor, University of<br />
Tasmania; Deputy-Director, Centre for Law and Genetics<br />
Donald Chalmers is Distinguished Professor at the University of Tasmania and<br />
in the Centre for Law and Genetics. He is a Foundation Fellow of the Australian<br />
Academy of Law and a Fellow of the Australian Academy of Health and Medical<br />
Sciences. In 2010, he received the NHMRC Ethics Award, the Distinguished<br />
Service Medal, University of Tasmania and the Australian Red Cross<br />
Distinguished Service Award. His major research interests focus on medical<br />
research ethics and the regulatory aspects of human genetics. He has been chief<br />
investigator on Australian Research Council discovery grants, with colleagues on<br />
the legal, ethical and governance implications of genetics, particularly<br />
commercialisation, biobanking and personalised medicine and on an NHMRC<br />
program grant on cancer genetics, He has published in health law and genetics,<br />
research ethics and law reform criminal law, legal studies trusts, authored a<br />
number of government and Law Reform Commissioner reports and made regular<br />
submissions to government enquiries. Throughout his career, he has been<br />
involved in teaching, administration and served on many State, national and<br />
international committees.<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 11
Mr Tracey Evans Chan, Associate Professor, Faculty of Law, National<br />
University of Singapore<br />
Tracey Evans Chan is an Associate Professor in the Faculty of Law, NUS, and<br />
specializes in biomedical law and ethics. He has published in the field both locally<br />
and internationally, and served in a number of Singapore expert committees on<br />
matters such as surrogacy, transplant ethics, human-animal combinations in<br />
biomedical research and mitochondrial germline modification. Professionally, he<br />
was called to the Singapore Bar in 1998 and then spent two years clerking for the<br />
Supreme Court of Singapore before joining academia. He recently concluded a<br />
year-long secondment to the Singapore Ministry of Health as a Deputy Director<br />
in the Regulatory Policy and Legislation Division, where he assisted in the policy<br />
work for the recently enacted Human Biomedical Research Act 2015.<br />
Dr Yoon-Jung Chang, Associate Professor of Department of Cancer<br />
Control and Policy, Graduate School of Cancer Science and Policy,<br />
National Cancer Center; Associate scientist, Hospice & Palliative Care<br />
Branch, National Cancer Center; Expert secretory, Team of legislation,<br />
ethics & policy, Precision Medicine Working Group, Ministry of Health &<br />
Welfare, South Korea<br />
Yoon-Jung Chang, M.D., Ph.D, is actively participated in policy development in<br />
hospice & palliative care (HPC) in South Korea. She was a representative<br />
interviewee of South Korea for ‘the 2015 Quality of Death Index: Ranking<br />
palliative care across the world’ a report by the Economist Intelligence Unit. Her<br />
major research interests focus on HPC policy, and risk communication and<br />
biomedical ethics in cancer care & Cancer research. Recently she joined the<br />
Precision Medicine Working Group, Ministry of Health & Welfare as an expert<br />
secretory.<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 12
Professor I. Glenn Cohen, Professor of Law, Harvard Law School;<br />
Director, Petrie-Flom Center for Health Law Policy, Biotechnology &<br />
Bioethics<br />
Glenn Cohen is a Professor of Law at Harvard Law School and Director of the<br />
Petrie-Flom Center for Health Law Policy, Biotechnology & Bioethics. He is<br />
one of the world's leading experts on the intersection of bioethics and the law, as<br />
well as health law. He was the youngest professor on the faculty at Harvard Law<br />
School both when he joined the faculty in 2008 (at age 29) and when he was<br />
tenured as a full professor in 2013 (at age 34). His current research projects relate<br />
to health information technologies, mobile health, reproductive technology,<br />
research ethics, rationing in law and medicine, health policy, FDA law and medical<br />
tourism. He is the author of more than 70 articles and chapters and his awardwinning<br />
work has appeared in leading legal medical, bioethics, and public health<br />
journals. Prior to becoming a professor he served as a law clerk to Judge Michael<br />
Boudin of the U.S. Court of Appeals for the First Circuit and as a lawyer for U.S.<br />
Department of Justice, Civil Division, Appellate Staff, where he handled litigation<br />
in the Courts of Appeals and (in conjunction with the Solicitor General’s Office)<br />
in the U.S. Supreme Court. In his spare time, he still litigates, most recently having<br />
authored an amicus brief in the U.S. Supreme Court for leading gene scientist Eric<br />
Lander in Association of Molecular Pathology v. Myriad, concerning whether human<br />
genes are patent eligible subject matter, a brief that was extensively discussed by<br />
the Justices at oral argument.<br />
Professor Henry T. Greely, Deane F. and Kate Edelman Johnson<br />
Professor of Law and Professor, by courtesy, of Genetics, Stanford<br />
University; Director, Stanford Center for Law and the Biosciences<br />
Hank Greely is the Deane F. and Kate Edelman Johnson Professor of Law and<br />
Professor, by courtesy, of Genetics at Stanford University. He specializes in<br />
ethical, legal, and social issues arising from advances in the biosciences,<br />
particularly from genetics, neuroscience, and human stem cell research. He<br />
directs the Stanford Center for Law and the Biosciences and the Stanford<br />
Program on Neuroscience in Society; chairs the California Advisory Committee<br />
on Human Stem Cell Research; and serves on the Neuroscience Forum of the<br />
Institute of Medicine, the Advisory Council for the National Institute for General<br />
Medical Sciences of NIH, the Committee on Science, Technology, and Law of<br />
the National Academy of Sciences, and the NIH Multi-Council Working Group<br />
on the BRAIN Initiative. He was elected a fellow of the American Association<br />
for the Advancement of Science in 2007. He graduated from Stanford in 1974<br />
and from Yale Law School in 1977. He served as a law clerk for Judge John Minor<br />
Wisdom on the United States Court of Appeals and for Justice Potter Stewart of<br />
the United States Supreme Court. After working during the Carter<br />
Administration in the Departments of Defense and Energy, he entered private<br />
practice in Los Angeles in 1981 as a litigator with the law firm of Tuttle & Taylor,<br />
Inc. He began teaching at Stanford in 1985.<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 13
Ms Alison Hall, Head of Humanities, PHG Foundation<br />
As Head of Humanities at the PHG Foundation, Alison is actively involved in<br />
policy analysis, evaluation and implementation. Professionally qualified as a lawyer<br />
and a nurse, with a master’s qualification in health care ethics, her work focuses<br />
on ethical, legal and social issues (ELSI) in biomedical technologies, and includes<br />
regulatory and legal policy analysis and briefings on the governance of human<br />
tissue, data protection and in vitro-diagnostic devices reform. Recent work<br />
includes leading a two year policy development project working with stakeholders<br />
on the ethical, legal and societal implications of implementing genomic<br />
sequencing into clinical practice (Hall A, Finnegan T, Alberg C, PHG Foundation<br />
(2014) Realising Genomics in Clinical Practice. ISBN 978-1-907198-15-1) and<br />
contributing legal and regulatory analysis to a report on data sharing to support<br />
clinical genetics and genomics practice (Data sharing to support UK clinical<br />
genetics and genomics services, PHG Foundation (2015) ISBN 978-1-907198-20-<br />
5). At EU policy level, with the Wellcome Trust, she has led advocacy on the<br />
genetic testing provisions in the proposed EU in vitro diagnostic devices<br />
regulation. Internationally, she has chaired a group developing a Data Sharing<br />
Lexicon as part of the regulatory and ethics activities of the Global Alliance for<br />
Genomics and Health. She has also co-authored PHG Foundation reports on<br />
ethical, legal and societal impacts of biotechnological advances including genomic<br />
stratification in cancer prevention and non-invasive prenatal diagnosis, and has<br />
over 20 peer-reviewed publications. Nationally, she has contributed to<br />
professional guidance including ‘Consent and Confidentiality in Clinical Genetic<br />
Practice’ published by the UK Joint Committee on Genomics in Medicine. She<br />
is currently on the UK Data Access Committee for METADAC, on the ethics<br />
and policy committee of the British Society for Genetic Medicine, and is a lay<br />
member of an NHS research ethics committee.<br />
Dr Chih-Hsing Ho, Assistant Professor/Assistant Research Fellow,<br />
Academia Sinica, Taiwan<br />
Chih-hsing Ho is Assistant Professor/Assistant Research Fellow at Academia<br />
Sinica, Taiwan. Her research focuses on the nexus of law and medicine in general,<br />
with particular attention to the governance of genomics and newly emerging<br />
biotechnologies, such as big data and biobanks. She is currently a Co-Principal<br />
Investigator for a health cloud project in Taiwan, and is responsible for designing<br />
an adequate regulatory framework for the secondary use of personal data and<br />
health-related data linkage. She holds a Ph.D. in law from the London School of<br />
Economics (LSE) where she was an Olive Stone Scholar. She obtained her first<br />
law degree from Taiwan, and later received her LLM from Columbia Law School<br />
and a JSM from Stanford University. Before moving back to Taipei in 2014, she<br />
had been working at the Centre for Medical Ethics and Law (CMEL) at the<br />
University of Hong Kong.<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 14
Dr Stuart Hogarth, Senior Research Fellow in the Department of Social<br />
Science, Health and Medicine at King's College London<br />
Stuart Hogarth is a Senior Research Fellow in the Department of Social Science,<br />
Health and Medicine at King's College London. His research focuses on the<br />
political economy of diagnostic innovation. His work combines empirical research<br />
on the development, assessment and adoption of diagnostic technologies, with<br />
normative analysis of public policy and commercial strategy. He has produced<br />
reports on intellectual property rights and regulatory frameworks in personalized<br />
medicine for the European Commission, Health Canada and the Human Genetics<br />
Commission.<br />
Dr Yann Joly, Associate Professor, Faculty of Medicine, Department of<br />
Human Genetics, McGill University; Research Director, Centre of<br />
Genomics and Policy<br />
Yann Joly, Ph.D. (DCL), Ad.E. is a Lawyer Emeritus from the Quebec Bar and<br />
the Research Director of the Centre of Genomics and Policies(CGP). He is a<br />
research fellow from the Fonds de recherche du Québec- Santé (FRQS) and an<br />
associate researcher at the Centre de recherche en droit public (Université de<br />
Montréal). He also works as an ethics and legal consultant in the private sector<br />
and serves as the Data Access Officer of the International Cancer Genome<br />
Consortium (ICGC). His research activities lie at the interface of the fields of<br />
intellectual property, health law (biotechnology and other emerging health<br />
technologies) and bioethics. He has served as a legal advisor on several ethics<br />
committees in the public and private sectors. Prof. Joly is a member of the<br />
Scientific Committee of the legal journal Lex Elextronica and an Advisory Board<br />
member of the Current Pharmacogenomics and Personalized Medicine Journal.<br />
He recently received the Quebec Bar Award of Merit (Innovation) for his work<br />
on the right to privacy in the biomedical field.<br />
Mr Terry Kaan, Associate Professor of Law, The University of Hong<br />
Kong; Co-Director, Centre for Medical Ethics and Law<br />
Terry Kaan’s research interests span from tort law to medical ethics and law. He<br />
has published articles and book chapters with regard to the issues of traditional,<br />
contemporary and alternative medicine, and genetic privacy. His current research<br />
is on how genetic testing impacts doctor-patient relationship.<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 15
Professor Kazuto Kato, Professor of Biomedical Ethics and Public<br />
Policy, Graduate School of Medicine, Osaka University, Japan<br />
Kazuto Kato, PhD is Professor of Biomedical Ethics and Public Policy at the<br />
Graduate School of Medicine, Osaka University, Japan. He is also Project<br />
Professor of the Institute for Integrated Cell-Material Sciences (iCeMS) at Kyoto<br />
University. He has a PhD degree in developmental biology from Kyoto<br />
University. After finishing postdoctoral research at the University of Cambridge<br />
with Sir John Gurdon, he started to work on the ethical and social issues of<br />
genomics and stem cell research. He has been serving as members of various<br />
international projects/academic societies such as Ethics Committee of Human<br />
Genome Organization (HUGO) (Currently, HUGO Committee on Ethics, Law<br />
and Society), ELSI group of the International HapMap Project. In 2010, he was<br />
appointed as a member of the Expert Panel on Bioethics of the Council for<br />
Science, Technology and Innovation Policy (CSTP) of the Cabinet Office, Japan.<br />
Professor Ock-Joo Kim, Professor and Chair in the Department of<br />
Medical History and Medical Humanities, Seoul National University<br />
College of Medicine<br />
Ock-Joo Kim, M.D., Ph. D., a graduate from Seoul National University College<br />
of Medicine, trained in biomedical ethics and medical history at University of<br />
Minnesota, Harvard University and Western IRB. Since 2002 she has worked in<br />
research governance systems including establishment of the KAIRB (Korean<br />
Association of IRBs). After the Hwang Scandal, she collaborated with various<br />
governmental agencies and academia to rebuild research ethics systems and<br />
promote research ethics education in Korea. As an expert in biomedical research<br />
ethics, she was involved in the total revision of the Bioethics and Safety Act and<br />
the operation of the National Bioethics Policy Institute. She is currently director<br />
of the Center for Human Research Protection at the Seoul National University<br />
Hospital and a member of IRBs in university and hospitals. She serves as a<br />
member of various government committees in bioethics including Central<br />
Advisory Committee of Korean Ministry of Food and Drug Administration, and<br />
Expert Committee under National Bioethics Review Boards. As a member of the<br />
Board of Trustees of the Korean Bioethics Association and the Korean Society<br />
for Medical Ethics, she played major roles in publishing biomedical ethics<br />
textbooks in Korea, including Clinical Ethics (2014) and Medical Ethics (2015). Her<br />
main research areas are clinical ethics, research ethics, and public health ethics and<br />
she has published many articles including recently “Ethical considerations of<br />
MERS-CoV outbreaks in Korea.”<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 16
Professor Bartha Maria Knoppers, Director, Centre of Genomics and<br />
Policy, Faculty of Medicine, Department of Human Genetics, McGill<br />
University<br />
Bartha Maria Knoppers, PhD (Comparative Medical Law), holds the Canada<br />
Research Chair in Law and Medicine (Tier 1: 2001 - ). In 2007, she founded the<br />
international Population Project in Genomics and Society (P3G) and<br />
CARTaGENE Quebec’s population biobank (20,000 indiv.). Former holder of<br />
the Chair d’excellence Pierre Fermat (France: 2006 - 2008), she was named<br />
Distinguished Visiting Scientist (Netherlands Genomics Initiative) (2009 - 2012)<br />
and received the ACFAS prize for multidisciplinarity (2011). She is Chair of the<br />
Ethics Working Party of the International Stem Cell Forum (2005 - ); Co-Chair<br />
of the Sampling/ELSI Committee of the 1000 Genomes Project (2007 - 2013);<br />
Member of the Scientific Steering Committee of the International Cancer<br />
Genome Consortium (ICGC) (2009- ); Chair, Regulatory and Ethics Working<br />
Group - Co-Founder and Member, Transitional Steering Committee (TSC) of the<br />
Global Alliance for Genomics and Health. She holds four Doctorates Honoris<br />
Causa, is Fellow of the American Association for the Advancement of Science, of<br />
The Hastings Center (Bioethics) and of the Canadian Academy of Health Sciences<br />
(CAHS) and Officer of the Order of Canada and of Quebec. She also received an<br />
award “Prix Montreal In Vivo: Secteur des sciences de la vie et des technologies<br />
de la santé” in 2012 and in 2013 was named “Champion of Genetics” by the<br />
Canadian Gene Cure Foundation.<br />
Dr Kathy Liddell, Herschel Smith Lecturer in Intellectual Property Law;<br />
Director, Centre for Law, Medicine and Life Sciences, University of<br />
Cambridge<br />
Kathy Liddell is Herschel Smith Lecturer in Intellectual Property Law and<br />
Director of the Centre for Law, Medicine and Life Sciences in the University of<br />
Cambridge. Her research focuses on a variety of issues such as patent protection<br />
in the field of pharmaceuticals and medical diagnostics, and the regulation of<br />
medical research and complex technologies such as genetic testing and stem cell<br />
products. She is the author of a wide range of articles in leading academic journals,<br />
a number of reports and briefing papers, and is co-editor of The Limits of Consent<br />
(OUP 2009).<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 17
Dr John Liddicoat, Philomathia Post-Doctoral Research Associate in<br />
Intellectual Property Law and Genetics, Faculty of Law, University of<br />
Cambridge<br />
Conference Rapporteur<br />
John Liddicoat joined the University of Cambridge in October 2015 after<br />
submitting his PhD at the University of Tasmania; he also holds a BSc(Hons) and<br />
LLB(Hons) from the University of Melbourne. His research interests lie in the<br />
development and use of new technology. John has published work on various<br />
intellectual property law issues, and enjoys commentating on doctrinal issues as<br />
well as emergent scientific issues – he is particularly interested in genomic and<br />
biotechnology related developments. John has a keen interest in the design of<br />
legal research and uses a broad range of qualitative and quantitative methods. His<br />
two current primary areas of research are: 1. Investigating the role of intellectual<br />
property rights in genomic medicine; and 2. Examining innovation policies<br />
adopted by biobanks. John has also contributed to law reform in Australia. He<br />
has co-authored submissions to various law reform enquiries and has also been<br />
invited to give oral evidence to a legislative committee.<br />
Mr Colm McGrath, WYNG Research Fellow in Medical Law and<br />
Ethics, Trinity Hall, University of Cambridge<br />
Colm McGrath is a member of the Cambridge Centre for Law, Medicine and Life<br />
Sciences based at the Faculty of Law, where he has taught Tort Law, Contract<br />
Law, Comparative Law, European Legal History and Roman law. Between 2009<br />
and 2014 he was a scientific assistant at the Institute for European Tort Law in<br />
Vienna and a lecturer at the University of Graz where he taught private law and<br />
healthcare law. His research focuses on the comparative analysis of private law<br />
and the nature of professional liability, in particular the liability and regulation of<br />
the medical profession. He is the Co-General Editor of the long-running Journal<br />
of Professional Negligence and the Book Reviews Editor for the Journal of<br />
European Tort Law.<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 18
Dr Timo Minssen, Associate Professor of IP & Innovation Law, University<br />
of Copenhagen, Centre for Information & Innovation Law<br />
Timo Minssen’s research concentrates on Intellectual Property, Competition- &<br />
Regulatory Law with a special focus on the pharma, life science & biotech sectors.<br />
His studies comprise a broad variety of legal issues that emerge during the lifecycle<br />
of related products and processes—from the regulation of research and incentives<br />
for innovation to technology transfer and commercialization. Timo is also<br />
scientific advisory board member of the Copenhagen Centre for Regulatory<br />
Sciences (CORS) and co-heads the Copenhagen Biotech & Pharma Forum<br />
(CBPF). He is a frequent lecturer on a variety of biotech and pharma related topics<br />
with many publications in leading international journals. In 2012 he published the<br />
comprehensive study “Assessing the Inventiveness of Biopharmaceutical<br />
Technology under European and US Patent Law,” which was awarded with the<br />
Swedish King Oscar stipendium. He is also a regular contributor on Harvard Law<br />
School’s “Bill of Health” blog. At present he is collaborating with Oxford<br />
University Press on a book in pharmaceutical competition law.<br />
Professor Darrell Rowbottom, Head of Philosophy & Professor,<br />
Lingnan University<br />
Darrell P. Rowbottom is Professor and Head of Philosophy at Lingnan<br />
University, Hong Kong. His research focuses on general issues in the philosophy<br />
of science (e.g. scientific method, scientific realism, and scientific progress) and<br />
the philosophy of probability (e.g. intersubjective probability and measurement<br />
paradoxes). He also has interests in epistemology, metaphysics, and the<br />
philosophy of education. His textbook Probability was recently published<br />
by Polity Press; an edition in simplified Chinese is set to be published by Shanghai<br />
People’s Publishing House. He is currently completing a research monograph,<br />
The Instrument of Science, which articulates and defends a new form of<br />
instrumentalism about science.<br />
Dr Jeffrey M. Skopek, Lecturer in Medical Law, Ethics, and Policy,<br />
Faculty of Law, University of Cambridge; Deputy Director, Centre for<br />
Law, Medicine and Life Sciences<br />
Jeffrey Skopek’s research interests centre on advances in the biosciences that<br />
destabilize categories and concepts that play a foundational role in our law and<br />
ethics. He is currently working on projects that explore challenges posed by<br />
developments in personalized medicine, biobanking, and big data. He previously<br />
taught at Harvard Law School, where he was a research fellow at the Petrie-Flom<br />
Centre for Health Law Policy, Biotechnology, and Bioethics. Prior to entering<br />
academia, he served as a law clerk to the Chief Judge of the United States Court<br />
of Appeals for the First Circuit. He has been awarded Fulbright, Gates, and<br />
Truman Scholarships and holds a J.D. (magna cum laude) from Harvard Law<br />
School, a Ph.D. and M.Phil. in the History and Philosophy of Science from the<br />
University of Cambridge, and an A.B. in History (with distinction) from Stanford<br />
University.<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 19
Dr Janice Tsang, Specialist in Medical Oncology, Clinical Assistant<br />
Professor Department of Medicine, The University of Hong<br />
KongFounding Convenor, Hong Kong Breast Oncology Group<br />
Janice Tsang is the Clinical Assistant Professor at the Department of Medicine,<br />
and the Assistant Dean (Alumni Relations) at the Li Ka Shing Faculty of Medicine,<br />
The University of Hong Kong. Her research interests lie mainly in breast oncology<br />
including conduction of clinical trials, translational research and psychosocial<br />
oncology. Being the first female academic medical oncologist at The University<br />
of Hong Kong, Dr. Tsang was awarded the 2014 Hong Kong Ten Outstanding<br />
Young Persons Award, and the 2012 Hong Kong City Lady Award (Professional<br />
& Academic Category) as the only medical professional receiving this award for<br />
the year. She was also the winner of the Psychosocial Oncology Young<br />
Investigator Award at the 16th Hong Kong International Cancer Congress & 6th<br />
Annual Meeting of Centre for Cancer Research in 2009 and was bestowed the<br />
Faculty Teaching Medal in 2012, and the Outstanding Teaching Award (Team<br />
Award) for Medical Humanities in 2013 in recognition of her being one of the<br />
pioneers in incorporating Medical Humanities in the formal medical curriculum.<br />
She has conducted over 70 clinical trials including local, regional and international<br />
multi-centred clinical trials, and has been serving as Chairperson for Data<br />
Monitoring Committee, Steering Committee Members for major multi-centred<br />
clinical trials, and various International and Regional Advisory Boards. She is a<br />
key opinion leader in breast oncology both locally and regionally. She is also the<br />
Founding Convenor of the Hong Kong Breast Oncology Group (HKBOG)<br />
which is now a member of the “Breast International Group” (BIG), being the<br />
third Asian member after Japan and Taiwan.<br />
Dr. Tsang is currently the Programme Director for Medical Oncology in the Hong<br />
Kong Island at the Hong Kong College of Physicians, a member of the Coordinating<br />
Committee (CoC) for Medical Oncology at the Hospital Authority, and<br />
the Deputy Chairperson for the Institutional Review Board for the Hong Kong<br />
West Cluster/ HKU, She was the Director of Cancer Centre at the Queen Mary<br />
Hospital (2014-2015), and she has various appointments in different professional<br />
bodies such as the Honorary Advisor for various cancer self-help groups including<br />
the Hong Kong Christian Cancer Care Association, Hong Kong Caner Fund etc.<br />
She is also the Founding Vice President of the Hong Kong Women Doctors<br />
Association, and Warden of the Starr Hall, HKU.<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 20
Dr Ron Zimmern, Chairman, PHG Foundation<br />
Ron Zimmern is a Public Health Physician with a special interest in public health<br />
genomics and personalized medicine. He is Chairman of the Foundation for<br />
Genomics and Population Health, the ‘PHG Foundation’, the successor to the<br />
Public Health Genetics Unit which he established in Cambridge in June 1997 and<br />
on which he served as its Director until 2010.<br />
Ron graduated in 1971 following medical training at Trinity College, Cambridge<br />
and the Middlesex Hospital, London. He specialized initially in neurology, and<br />
was appointed Lecturer at the Clinical School in Cambridge in 1976. He obtained<br />
a law degree at Cambridge in 1983, after which he trained in public health<br />
medicine. He was Director of Public Health for Cambridge and Huntingdon<br />
Health Authority from 1991 to 1998, and of the Institute of Public Health at the<br />
University of Cambridge from 2002 to 2008. He was for many years an Associate<br />
Lecturer at the University of Cambridge and has been an Honorary Consultant in<br />
Public Health Medicine at Addenbrooke's Hospital.<br />
Ron has served on many national committees concerned with genomics in the<br />
UK since 1997. He has an Honorary Professorship in Public Health at the<br />
University of Hong Kong and sits on the Management Committee of its Centre<br />
for Medical Ethics and Law. He is also a member of the External Advisory<br />
Committee of the University of Cambridge’s Centre for Law, Medicine and Life<br />
Sciences within the Law Faculty; and of the Centre for Personalized Medicine at<br />
St Anne’s College, Oxford. He is a Life Fellow of Hughes Hall in Cambridge and<br />
a Fellow of Hong Kong University and of the University of Cardiff. He now<br />
serves as a Non-Executive Director of Papworth Hospital and on the Ethics<br />
Advisory Committee of Genomics England. His special interests and expertise,<br />
in addition to public health genomics and personalized medicine, include strategic<br />
planning, the relationship between clinical services and teaching and research,<br />
priority setting in the NHS, and the law and ethics of medicine.<br />
Note: Abstracts and Biographies are subject to change<br />
Contact Information<br />
Contact LML<br />
Centre for Law, Medicine and Life Sciences<br />
University of Cambridge<br />
lml@law.cam.ac.uk<br />
http://www.lml.law.cam.ac.uk<br />
Contact CMEL<br />
Centre for Medical Ethics and Law<br />
The University of Hong Kong<br />
cmel@hku.hk<br />
www.cmel.hku.hk<br />
PRECISION MEDICINE: LEGAL AND ETHICAL CHALLENGES 21