TUBERCULOSIS
2dnCECj
2dnCECj
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
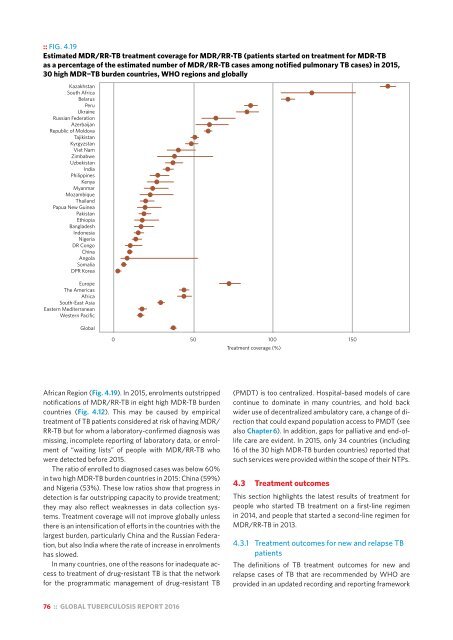
:: FIG. 4.19<br />
Estimated MDR/RR-TB treatment coverage for MDR/RR-TB (patients started on treatment for MDR-TB<br />
as a percentage of the estimated number of MDR/RR-TB cases among notified pulmonary TB cases) in 2015,<br />
30 high MDR−TB burden countries, WHO regions and globally<br />
Kazakhstan<br />
South Africa<br />
Belarus<br />
Peru<br />
Ukraine<br />
Russian Federation<br />
Azerbaijan<br />
Republic of Moldova<br />
Tajikistan<br />
Kyrgyzstan<br />
Viet Nam<br />
Zimbabwe<br />
Uzbekistan<br />
India<br />
Philippines<br />
Kenya<br />
Myanmar<br />
Mozambique<br />
Thailand<br />
Papua New Guinea<br />
Pakistan<br />
Ethiopia<br />
Bangladesh<br />
Indonesia<br />
Nigeria<br />
DR Congo<br />
China<br />
Angola<br />
Somalia<br />
DPR Korea<br />
Europe<br />
The Americas<br />
Africa<br />
South-East Asia<br />
Eastern Mediterranean<br />
Western Pacific<br />
Global<br />
0 50 100 150<br />
Treatment coverage (%)<br />
African Region (Fig. 4.19). In 2015, enrolments outstripped<br />
notifications of MDR/RR-TB in eight high MDR-TB burden<br />
countries (Fig. 4.12). This may be caused by empirical<br />
treatment of TB patients considered at risk of having MDR/<br />
RR-TB but for whom a laboratory-confirmed diagnosis was<br />
missing, incomplete reporting of laboratory data, or enrolment<br />
of “waiting lists” of people with MDR/RR-TB who<br />
were detected before 2015.<br />
The ratio of enrolled to diagnosed cases was below 60%<br />
in two high MDR-TB burden countries in 2015: China (59%)<br />
and Nigeria (53%). These low ratios show that progress in<br />
detection is far outstripping capacity to provide treatment;<br />
they may also reflect weaknesses in data collection systems.<br />
Treatment coverage will not improve globally unless<br />
there is an intensification of efforts in the countries with the<br />
largest burden, particularly China and the Russian Federation,<br />
but also India where the rate of increase in enrolments<br />
has slowed.<br />
In many countries, one of the reasons for inadequate access<br />
to treatment of drug-resistant TB is that the network<br />
for the programmatic management of drug-resistant TB<br />
(PMDT) is too centralized. Hospital-based models of care<br />
continue to dominate in many countries, and hold back<br />
wider use of decentralized ambulatory care, a change of direction<br />
that could expand population access to PMDT (see<br />
also Chapter 6). In addition, gaps for palliative and end-oflife<br />
care are evident. In 2015, only 34 countries (including<br />
16 of the 30 high MDR-TB burden countries) reported that<br />
such services were provided within the scope of their NTPs.<br />
4.3 Treatment outcomes<br />
This section highlights the latest results of treatment for<br />
people who started TB treatment on a first-line regimen<br />
in 2014, and people that started a second-line regimen for<br />
MDR/RR-TB in 2013.<br />
4.3.1 Treatment outcomes for new and relapse TB<br />
patients<br />
The definitions of TB treatment outcomes for new and<br />
relapse cases of TB that are recommended by WHO are<br />
provided in an updated recording and reporting framework<br />
76 :: GLOBAL <strong>TUBERCULOSIS</strong> REPORT 2016