FERTILITY GENETICS
TCqTZH
TCqTZH
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
THE FEATURED ARTICLE<br />
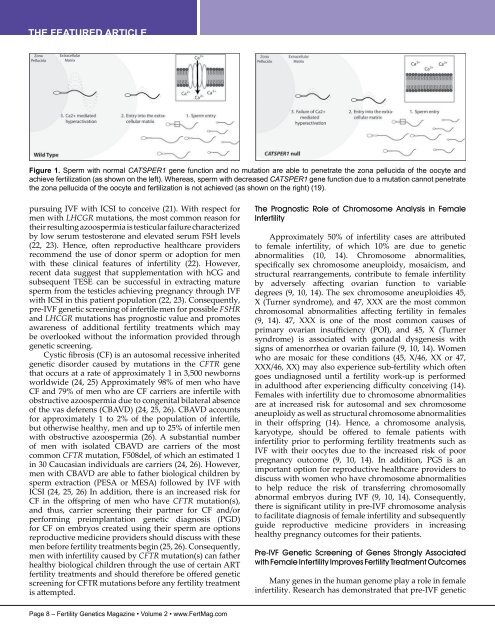
Figure 1. Sperm with normal CATSPER1 gene function and no mutation are able to penetrate the zona pellucida of the oocyte and<br />
achieve fertilization (as shown on the left). Whereas, sperm with decreased CATSPER1 gene function due to a mutation cannot penetrate<br />
the zona pellucida of the oocyte and fertilization is not achieved (as shown on the right) (19).<br />
pursuing IVF with ICSI to conceive (21). With respect for<br />
men with LHCGR mutations, the most common reason for<br />
their resulting azoospermia is testicular failure characterized<br />
by low serum testosterone and elevated serum FSH levels<br />
(22, 23). Hence, often reproductive healthcare providers<br />
recommend the use of donor sperm or adoption for men<br />
with these clinical features of infertility (22). However,<br />
recent data suggest that supplementation with hCG and<br />
subsequent TESE can be successful in extracting mature<br />
sperm from the testicles achieving pregnancy through IVF<br />
with ICSI in this patient population (22, 23). Consequently,<br />
pre-IVF genetic screening of infertile men for possible FSHR<br />
and LHCGR mutations has prognostic value and promotes<br />
awareness of additional fertility treatments which may<br />
be overlooked without the information provided through<br />
genetic screening.<br />
Cystic fibrosis (CF) is an autosomal recessive inherited<br />
genetic disorder caused by mutations in the CFTR gene<br />
that occurs at a rate of approximately 1 in 3,500 newborns<br />
worldwide (24, 25) Approximately 98% of men who have<br />
CF and 79% of men who are CF carriers are infertile with<br />
obstructive azoospermia due to congenital bilateral absence<br />
of the vas deferens (CBAVD) (24, 25, 26). CBAVD accounts<br />
for approximately 1 to 2% of the population of infertile,<br />
but otherwise healthy, men and up to 25% of infertile men<br />
with obstructive azoospermia (26). A substantial number<br />
of men with isolated CBAVD are carriers of the most<br />
common CFTR mutation, F508del, of which an estimated 1<br />
in 30 Caucasian individuals are carriers (24, 26). However,<br />
men with CBAVD are able to father biological children by<br />
sperm extraction (PESA or MESA) followed by IVF with<br />
ICSI (24, 25, 26) In addition, there is an increased risk for<br />
CF in the offspring of men who have CFTR mutation(s),<br />
and thus, carrier screening their partner for CF and/or<br />
performing preimplantation genetic diagnosis (PGD)<br />
for CF on embryos created using their sperm are options<br />
reproductive medicine providers should discuss with these<br />
men before fertility treatments begin (25, 26). Consequently,<br />
men with infertility caused by CFTR mutation(s) can father<br />
healthy biological children through the use of certain ART<br />
fertility treatments and should therefore be offered genetic<br />
screening for CFTR mutations before any fertility treatment<br />
is attempted.<br />
The Prognostic Role of Chromosome Analysis in Female<br />
Infertility<br />
Approximately 50% of infertility cases are attributed<br />
to female infertility, of which 10% are due to genetic<br />
abnormalities (10, 14). Chromosome abnormalities,<br />
specifically sex chromosome aneuploidy, mosaicism, and<br />
structural rearrangements, contribute to female infertility<br />
by adversely affecting ovarian function to variable<br />
degrees (9, 10, 14). The sex chromosome aneuploidies 45,<br />
X (Turner syndrome), and 47, XXX are the most common<br />
chromosomal abnormalities affecting fertility in females<br />
(9, 14). 47, XXX is one of the most common causes of<br />
primary ovarian insufficiency (POI), and 45, X (Turner<br />
syndrome) is associated with gonadal dysgenesis with<br />
signs of amenorrhea or ovarian failure (9, 10, 14). Women<br />
who are mosaic for these conditions (45, X/46, XX or 47,<br />
XXX/46, XX) may also experience sub-fertility which often<br />
goes undiagnosed until a fertility work-up is performed<br />
in adulthood after experiencing difficulty conceiving (14).<br />
Females with infertility due to chromosome abnormalities<br />
are at increased risk for autosomal and sex chromosome<br />
aneuploidy as well as structural chromosome abnormalities<br />
in their offspring (14). Hence, a chromosome analysis,<br />
karyotype, should be offered to female patients with<br />
infertility prior to performing fertility treatments such as<br />
IVF with their oocytes due to the increased risk of poor<br />
pregnancy outcome (9, 10, 14). In addition, PGS is an<br />
important option for reproductive healthcare providers to<br />
discuss with women who have chromosome abnormalities<br />
to help reduce the risk of transferring chromosomally<br />
abnormal embryos during IVF (9, 10, 14). Consequently,<br />
there is significant utility in pre-IVF chromosome analysis<br />
to facilitate diagnosis of female infertility and subsequently<br />
guide reproductive medicine providers in increasing<br />
healthy pregnancy outcomes for their patients.<br />
Pre-IVF Genetic Screening of Genes Strongly Associated<br />
with Female Infertility Improves Fertility Treatment Outcomes<br />
Many genes in the human genome play a role in female<br />
infertility. Research has demonstrated that pre-IVF genetic<br />
Page 8 – Fertility Genetics Magazine • Volume 2 • www.FertMag.com