LMITransactions&Report2014-15
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
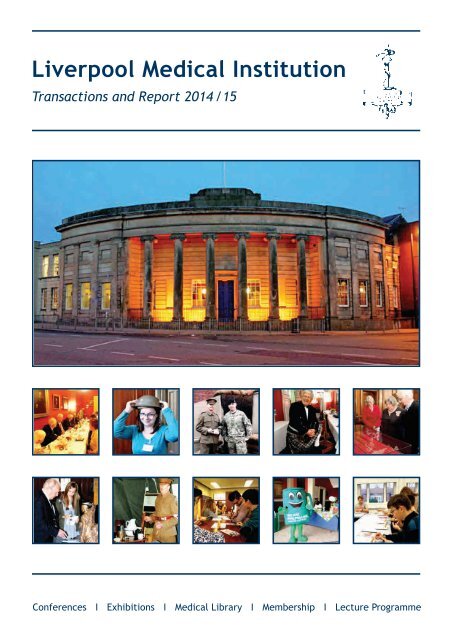
Liverpool Medical Institut ion<br />
Transactions and Report 2014 /<strong>15</strong><br />
Conferences I Exhibitions I Medical Library I Membership I Lecture Programme
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Order of Contents<br />
Frontispiece, Mr Max McCormick 2<br />
List of SMC Members 3<br />
List of MEC Members 4<br />
The Liverpool Medical Institution Staff 5<br />
Editorial 6<br />
Inaugural Address of the President<br />
Held on Thursday 16th October 2014 8<br />
Henry Cohen Memorial Lecture 11<br />
Annual Healthcare Service <strong>15</strong><br />
Minutes of the Ordinary Meetings of the 176th Session<br />
including details of social events and Admission of Life Members 16<br />
Edith Cavell – WWI Heroine 52<br />
Retired Members’ Group 54<br />
Report of Council 57<br />
Report of the Honorary Librarian 59<br />
Obituary Notices 60<br />
Members Joined since last Transactions 65<br />
Auditor’s Report 66<br />
List of Presidents 67<br />
Charitable Donations 68<br />
Cover Illustrations<br />
Upper Row, Left to Right:<br />
1. LMI members and guests dining after Professor TM Jones’ lecture in November 2014<br />
2. LMI manager Sam Pickup tries on a WWI helmet during the military medicine exhibition October 2014<br />
3. 208 Field Hospital personnel in modern and WWI uniform outside a simulated WWI trench October 2014<br />
4. Professor Richard Ramsden posing in his kilt before speaking at the Annual Dinner on February 20<strong>15</strong><br />
5. LMI librarian Adrienne Mayers admiring Capt. Noel Chavasse’s sword with Dame Lorna Muirhead, October 2014<br />
Lower Row, Left to Right:<br />
1. A visitor and a volunteer inspect the prototype cast for Liverpool Heroes Memorial on display at LMI during the military medicine exhibition October 2014<br />
2. 208 Field Hospital personnel giving a lecture on living conditions and medicine in the trenches<br />
3. Students at a Clinical Skills teaching session held at the LMI in November 2014<br />
4. Macmillan mascot at the Macmillan World’s Biggest Coffee Morning event at the LMI in September 2014<br />
5. Year 12 students attending a surgical skills taster session at Broadgreen Hospital during the Year 12 Medical Conference, December 2014
Liverpool Medical Institution<br />
Registered Charity No: 210112<br />
Transactions<br />
and Report<br />
The Institution book plate, reproduced on the front cover, was designed and engraved by Stephen<br />
Gooden, C.B.E., R.A.<br />
The basis of the design is the staff and serpent of Asklepios, bearing the date when the Library was<br />
opened to the profession in Liverpool and neighbourhood.<br />
On the shield is the emblem of Liverpool and it is supported by two fleams or lancets of a design<br />
once used for blood-letting.<br />
The Institution crest, reproduced above, can be seen in the library, the lecture theatre and as a<br />
mosaic in the main hall. It also shows the Staff and Serpent, with the opening words of the<br />
Aphorisms of Hippocrates:<br />
(Life is short, and Art long; the crisis fleeting; experience<br />
perilous and decision difficult).<br />
Trans. FRANCIS ADAMS<br />
114 Mount Pleasant, Liverpool L3 5SR<br />
Telephone: 0<strong>15</strong>1-709 9125 Fax: 0<strong>15</strong>1-707 2810<br />
Email: admin@lmi.org.uk Web Address: www.lmi.org.uk Twitter: @LMI114<br />
1
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Mr. Max McCormick<br />
President 2014-<strong>15</strong><br />
2
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Strategic Management Council (SMC) 2014-20<strong>15</strong><br />
Chairman:<br />
A SWIFT<br />
President:<br />
M McCORMICK<br />
President-Elect:<br />
G LAMONT<br />
Treasurer:<br />
A ELLIS<br />
Secretary:<br />
A McCORMICK<br />
Librarian:<br />
A LARNER<br />
D ANTONIA<br />
L DE COSSART<br />
E DJABATEY<br />
A ELLIS<br />
S EVANS<br />
Members of SMC:<br />
R FARQUHARSON<br />
N GILMOUR<br />
W KENYON<br />
A LARNER<br />
G LAMONT<br />
A McCORMICK<br />
M McCORMICK<br />
S SHEARD<br />
A SWIFT<br />
Auditors:<br />
BAKER TILLY<br />
David Antonia<br />
Linda de Cossart<br />
Edwin Djabatey<br />
Anthony Ellis<br />
Susan Evans<br />
Roy Farquharson<br />
Nigel Gilmour<br />
William Kenyon<br />
Andrew Larner<br />
Graham Lamont<br />
Austin McCormick Max McCormick Sally Sheard Andrew Swift<br />
3
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Membership and Education Committee (MEC) 2014-20<strong>15</strong><br />
President:<br />
M McCORMICK<br />
President-Elect:<br />
G LAMONT<br />
Vice Presidents:<br />
V JHA J CURTIS<br />
Treasurer:<br />
A ELLIS<br />
Secretary:<br />
A McCORMICK<br />
Librarian:<br />
A LARNER<br />
Members of MEC:<br />
J CURTIS<br />
P D O DAVIES<br />
L DE COSSART<br />
A ELLIS<br />
R C EVANS<br />
V JHA<br />
G LAMONT<br />
A LARNER<br />
A McCORMICK<br />
M McCORMICK<br />
I RYLAND<br />
Additional Honorary Officers:<br />
Secretary of Ordinary Meetings: VACANT<br />
Editor of Transactions: R C EVANS<br />
(Assistant Editors: N R CLITHEROW, SHARON HUNT AND LYNNE SMITH)<br />
John Curtis<br />
Peter Davies<br />
Linda de Cossart<br />
Anthony Ellis<br />
Richard Evans<br />
Vikram Jha<br />
Graham Lamont<br />
Andrew Larner<br />
Austin McCormick<br />
Max McCormick<br />
Ida Ryland<br />
Samantha Dolan<br />
Peter Skellorn<br />
4
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
The Staff of the Liverpool Medical Institution<br />
Sue Curbishley<br />
(Library Assistant)<br />
Samantha Pickup (Manager) Audrey Roberts (Admin) Jim Penwill (Finance Officer)<br />
Sharon Hunt (Admin)<br />
Tom Spearitt (Security)<br />
Lynne Smith (Admin)<br />
Joyce Williams (Bar)<br />
Karen Alsop<br />
(Finance Manager & Project Manager)<br />
Adrienne Mayers (Librarian)<br />
Other Team Members<br />
Deborah & Dennis Holden<br />
(Catering)<br />
Mark Ross<br />
(AV Technician)<br />
Jeremy Blades<br />
(AV Technician)<br />
Anna Reid<br />
(RCGP Mersey Faculty)<br />
Sarah Adams<br />
(RCGP Mersey Faculty)<br />
Christopher Mayers<br />
(RCP Mersey Regional Office)<br />
5
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Editorial<br />
It was a rather exciting Tour-de-France this year with British rider Chris Froome<br />
winning the maillot jaune. Controversies that embroiled Chris Froome perhaps seem<br />
to have arisen from our historical relationship with our neighbour across la manche.<br />
It was also remarkable seeing Chris Froome’s story on television and the way in which<br />
he lived across the inherent borders that are still present in South Africa.<br />
It was the use of modern technology that enabled me to catch snippets of Le tour on<br />
my i-Phone, connected to the now widely available hospital Wi-Fi system, even in our<br />
small community unit. After a long slog through a busy clinic, it was a relief that I<br />
was able to finish the day early just after 3pm, so that I could catch up with family<br />
before my wife started notorious Saturday night duty. Like most other days of the<br />
week, we continue to hunt for time together to be with our 1 year-old daughter.<br />
That evening I took the opportunity to look at my wife’s paediatric rota which was remarkably over-complicated,<br />
but not surprising given the current difficulties with recruitment of doctors. This led me to think about the<br />
problems that we still have, some increasingly so, in borders across medicine. I find it quite difficult as someone<br />
who had such a broad training in general medicine to see that specialities appear to be not only metaphorically<br />
segregated but also geographically.<br />
I am currently in practice on the other side of our own regional border named after King Offa. I notice how<br />
relationships have changed in medicine across the North West now that the rotations from Liverpool and<br />
elsewhere are significantly diminished. One gets the feeling that any mention of migration locally seems to<br />
have a response almost akin to that suffered by poor Edith Cavell [see the feature article in this Transactions].<br />
In the LMI, I find it interesting to see how many people cross the corridors to attend meetings other than their<br />
own speciality. I admit on occasions my only reason is often to have a necessary biscuit after a long journey.<br />
When I was a student my flat mates and I decided to see if we could manage to eat for free for two weeks by<br />
attending clinical meetings alone! Thankfully I shared a flat with students from other medical schools across<br />
London, so we had a wide variety from which to choose. We succeeded in attending, learning and eating<br />
breakfast, lunch and dinner in some of the most wide-ranging speciality meetings one can imagine. I am pretty<br />
sure that, apart from the fact that this enabled me to have enough energy to cycle in and out of Central London,<br />
I learned plenty. I do remember, however, a lecture on child psychiatry being beyond my comprehension, not<br />
withstanding it started at 6am.<br />
I have recently been asked to take over the Merseyside and North Wales Association of Physicians meetings,<br />
which have lapsed for some time now (making note of the fact that the acronym of MANSWOP is not only<br />
incorrect but potentially disappointing).<br />
I find it challenging to work out how to try and recruit new members to this group, combining common interest<br />
and enthusiasm about medicine across boarders, particularly when the old connections of training fellows are<br />
slowly disappearing. It almost feels rather akin to the still delayed stability of the French fusion reactor.<br />
Perhaps I will have to go back to the attraction that worked when I was a student: “let food be thy medicine and<br />
medicine be thy food”<br />
Mangez bien!<br />
Richard Evans<br />
6
7<br />
LMI Transactions and Report 2014 - 20<strong>15</strong>
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
‘The Missing Chapter’<br />
The Inaugural Address of the 176th Session of the Liverpool Medical Institution<br />
Thursday 16th October 2014<br />
By: The President - Mr Max S McCormick<br />
Prof Linda de Cossart and Mr Max McCormick<br />
Introduction<br />
Members, colleagues and guests; first of all I would<br />
like to thank you all for attending tonight and giving<br />
me the honour of being your President for this 176th<br />
session. Thanks especially to the management<br />
committee for putting their faith in me to do this.<br />
My talk will cover various aspects of my schooling,<br />
training and passage through Medical School, Junior<br />
Doctor training, Senior Doctor training and finally this<br />
appointment. The title of my talk ‘The Missing<br />
Chapter’ relates to my work as a Consultant Surgeon,<br />
whose main interests are in training new doctors and<br />
senior doctors as apprentices and hopefully making a<br />
difference to my trainees as to how they practise<br />
medicine.<br />
Born in Belfast to George and Jessie, my background<br />
was fairly humble. I attended State primary school<br />
and subsequently Methodist College Belfast, a State<br />
grammar school. There was a strong history of<br />
working with ships and indeed my grandfather won<br />
many trophies building model yachts sailed at a local<br />
reservoir. We still retain one cup, larger than the FA<br />
Cup. He was a shipwright and worked on the building<br />
of the Titanic. Having achieved success in the 11-plus,<br />
I entered Methodist College Belfast, a large mixed<br />
school of almost 2,000 people with two prep schools<br />
and fairly large sporting grounds. Achieving some<br />
success in sports activities, mainly in cricket, I managed<br />
to achieve sufficient ‘A levels’ to enter medical school.<br />
The choice of medical school was not straightforward<br />
in that had I chosen Queen’s University Belfast, I would<br />
have had an offer from them and nowhere else. As it<br />
was I chose Edinburgh, Liverpool and various others<br />
and ended up without an offer. Eventually Liverpool<br />
agreed to interview me and after a short meeting<br />
with the then Dean, Jack Leggate, an offer was made.<br />
The grades were achieved and I entered medical<br />
school in 1968. I really enjoyed medical school in all<br />
aspects, academic, social and artistic, taking part in<br />
many activities including being President of the<br />
Medical Students’ Society in 1971-72. Marriage and a<br />
young family commenced shortly after this. Early jobs<br />
as a House Officer and Senior House Officer in<br />
Whiston were followed by periods of plastic surgery,<br />
gynaecology and eventually time in the<br />
demonstrating room, time well spent to obtain<br />
primary FRCS.<br />
8
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
It was at this point I entered training in ENT as an SHO<br />
under the guidance of Philip Stell. Six months into this<br />
training I was able to get a Registrar’s post in Oxford<br />
at the Radcliffe Infirmary (the old Radcliffe in the<br />
centre of town) working with Bernard Coleman, Bill<br />
Lund and Andrew Freeland. This was a great time for<br />
my academic career working with likeminded<br />
individuals, both my level and senior to me, and also<br />
the 3 Consultants with a tertiary referral practice.<br />
Having obtained my Fellowship in Surgery I was able<br />
to then take advantage of an offer of a Registrar’s<br />
post in the Groote Schuur Hospital, Cape Town, under<br />
the guidance of Professor Sean Sellers. This was a very<br />
productive period of my life where I was able to utilise<br />
what knowledge I had along with some surgical skills<br />
but under good tutorship and supervision. On<br />
completion of this contract and following a three<br />
month locum in Bulawayo to cover expenses, I<br />
returned initially to Oxford and subsequently to a<br />
Senior Registrar’s job in Liverpool. In January 1986 I<br />
commenced my full time post as a Consultant<br />
Otolaryngologist, with sessions both at the Royal<br />
Liverpool and Arrowe Park Hospitals. It was at this<br />
point that I noticed that the Royal Liverpool Hospital<br />
building was eleven stories high and the length of two<br />
football pitches i.e. exactly the same dimensions as the<br />
Titanic.<br />
Subsequently I dropped my sessions at Arrowe Park<br />
and took up sessions at Alder Hey Children’s Hospital.<br />
During this time I had worked with approximately 20<br />
Consultant colleagues from whom I learnt a lot about<br />
surgery, patient management, differing health care<br />
systems and it gave me an ability to analyse and assess<br />
treatment modalities.<br />
The Missing Chapter<br />
As indicated earlier, this is the bit of all textbooks<br />
which is missing i.e. how to interpret facts and<br />
translate them into patient management. Most of this<br />
can only be taught by the bedside or in theatre or in<br />
relaxed frank discussion. I don’t think there is<br />
anything didactic in this method of teaching:<br />
textbooks are full of facts and whilst accurate, are<br />
themselves pretty lifeless. It is the job of the surgical<br />
tutor to enable trainees to elicit and recognise<br />
physical signs and then with all the other relevant<br />
details relating to a patient, formulate a management<br />
strategy and a plan for treatment. I have estimated<br />
that I have perhaps worked with almost 300 trainees<br />
in my 29-year surgical career and hope that many of<br />
these have been influenced in a positive way about<br />
my thoughts in relation to management.<br />
It is accepted by all of us that today’s trainees are not<br />
as experienced as their predecessors. We now<br />
produce emergency safe surgeons and only with<br />
fellowships and subspecialisation post CCST<br />
accreditation would a specialist be regarded as fully<br />
trained. This of course means that the general<br />
training that I gained has now devolved into otology,<br />
rhinology, head and neck cancer, facial plastics,<br />
paediatric ENT and audiology i.e. the same sort of<br />
subspecialisation which has happened in General<br />
Surgery.<br />
A lot of the conditions covered in otolaryngology are<br />
not surgical at all and need to be managed in the<br />
clinic for ex<strong>amp</strong>le tinnitus and dizziness.<br />
Surgery, like virtually everything in medicine, is<br />
individualised to each patient, but the same steps<br />
must be included in each case. This of course is learnt<br />
by repeated practice in a similar way to the same basic<br />
golf swing being used for every shot but then adapted<br />
to special circumstances.<br />
I do feel however that the surgical training needs<br />
focus and guidance in particular areas, and I<br />
understand that the undergraduate medical<br />
curriculum is being altered to provide some more<br />
focus and guidance in this respect.<br />
I was fortunate in that I was able to travel to South<br />
Africa and subsequently Zimbabwe using my medical<br />
degree almost as a passport. I would recommend this<br />
to any trainee as a method of broadening your<br />
outlook on life and experiencing different values in<br />
healthcare systems.<br />
The “Whenwees”<br />
A displaced group of ex-pats from Rhodesia are often<br />
referred to as The “Whenwees”, due to the way that<br />
when they meet to discuss the good old days it nearly<br />
always starts with ‘when we …’. Perhaps I feel a little<br />
like that on looking back at my career, and asking<br />
what in fact was wrong with selection and<br />
competition? What is the benefit that the<br />
introduction of university fees has given apart from<br />
shifting the burden of debt from the State to the<br />
student? What was wrong with providing the<br />
underprivileged and underfunded student with a<br />
student grant as opposed to encouraging to take out<br />
even more loans on top of the university fees?<br />
9
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
The NHS<br />
I work in a system where there appears to be<br />
continual change and it certainly feels like a top-down<br />
managed structure. Not only is there continual<br />
change in management, there are continual changes<br />
in ideas, often at the behest of politicians, with<br />
nothing longer than a short to medium term<br />
management plan. As clinicians, we often feel<br />
disenfranchised offering advice about management.<br />
I have often wondered whether the NHS might<br />
benefit from a similar structure to the Bank of<br />
England, who have an independent Board which<br />
makes recommendations to the Government.<br />
Acknowledgements<br />
I would like to thank all those that have supported me<br />
in my career and particularly the State education<br />
system, the NHS for supporting my apprenticeship,<br />
friends who have shared my professional<br />
development and other providers of opportunities.<br />
Finally I would like to thank my wife, Siobhan, who<br />
has been an unerring supporter whether it be pushing<br />
from behind, supporting me by my side or indeed<br />
leading from the front. We have shared this passage<br />
through medical school, junior doctor, senior doctor<br />
and now entering the twilight of my career, I am still<br />
very glad of her presence.<br />
10
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
The Henry Cohen History of Medicine Lecture<br />
Delivered on Thursday 30th October 2014<br />
By Professor Mark Harrison, Professor of the History of Medicine and Director of the<br />
Wellcome Unit for the History of Medicine at Oxford University<br />
‘Britain’s Medical War: Health and Medicine in the British Army, 1914-18’<br />
Prof Vikram Jha, Prof Mark Harrison & Mr Max McCormick<br />
In some ways, World War I represented a turning point<br />
in medical care during conflict. In major wars up until<br />
then, more soldiers had died of disease than from<br />
battle injuries. The disease:combat fatality ratio had<br />
been 5:1 in the Crimean and American Civil Wars and<br />
2:1 in the South African War. Compare this to the<br />
ratios in WWI and WWII which were 0.7:1 and 0.1:1<br />
respectively and the contrast is clear. However, when<br />
hospital admissions were included as well as deaths,<br />
there were major variations in the disease:combat<br />
ratio in different theatres.<br />
brought in casualties from the battlefield and they<br />
then passed down a chain from regimental aid post to<br />
collecting post, dressing station, casualty clearing<br />
station and hospital. Long ambulance trains ferried<br />
the wounded to the hospitals, hospital ships carried<br />
wounded over the Channel and hospital trains were<br />
available on both sides of the Channel.<br />
Professor Harrison set out to examine the explanations<br />
for these differences in 3 WWI theatres. Among British<br />
and Empire forces on the Western Front in France and<br />
Flanders, 56% of deaths and hospital admissions were<br />
‘non-battle’, in the Dardanelles this figure was 68%<br />
and in Mesopotamia (modern Iraq) 91%.<br />
In all theatres, 85-90% of non-battle casualties were<br />
from disease. On the Western Front, where battle lines<br />
were relatively static for much of the war, the numbers<br />
were enormous and a vast ‘medical machine’ was<br />
established. Over 5.5 million were admitted to<br />
hospital, 183,454 died of wounds and disease, almost<br />
3 million returned to duty in theatre and 2.3 million<br />
were evacuated out of the theatre. Stretcher bearers<br />
A convoy of Red Cross Ford Ambulances (built to order<br />
of the French Relief Fund) en route from Liverpool to<br />
London. The convoy reached the Metropolis without<br />
mishap, proceeding via Lichfield, Coventry and St<br />
Albans.<br />
Ford Times September 19<strong>15</strong>.<br />
11
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
generated lack of supplies and prolonged casualty<br />
evacuation to base facilities, with the added risk of<br />
interruption by enemy action. Casualty evacuation<br />
was more difficult during advances or retreats.<br />
Operations also generated new varieties of medical<br />
problems such as shell-shock and gas poisoning on the<br />
Western Front. There was little shell-shock in<br />
Mesopotamia. Relationships with the local population<br />
could be hostile in Mesopotamia and it was always<br />
important to negotiate with the locals.<br />
Geographical factors played a major role. The<br />
prevalence of diseases such as typhoid in the local<br />
civilian population and in animal reservoirs would<br />
influence the likelihood of infecting the soldiers.<br />
There were problems of heat stroke in the Dardanelles<br />
and Mesopotamia, and of frost bite in France. The<br />
terrain in France was flat and there was a pre-existing<br />
infrastructure of roads and railways, although<br />
flooding, wind, snow and ice could be problems.<br />
Casualties in the Dardanelles were evacuated under<br />
fire to poorly-organised medical facilities. Although<br />
these improved compared with the second wave of<br />
landings, there was no space in the bridgeheads and a<br />
lack of resources for anything like what was available<br />
on the Western Front. In Mesopotamia there were no<br />
railways and few roads. Transport was by horse- or<br />
donkey-drawn vehicles over very long distances, until<br />
a river could be reached.<br />
To some extent, technology played a part in ironing<br />
out the differences between the 3 theatres. In<br />
particular, immunisation against typhoid and tetanus<br />
was available in all 3 areas, but immunisation against<br />
cholera was only 50% effective. Each theatre<br />
presented its own unique challenges, but the<br />
difficulties remained greatest outside Europe.<br />
Geographical difficulties could be partly overcome<br />
given sufficient planning and resources.<br />
Operational factors always played a major role. For<br />
the medical services, the relatively static theatre on the<br />
Western Front carried major advantages, allowing<br />
facilities to be built up over a period. Combined<br />
operations such as in the Dardanelles added problems,<br />
with poor communications and rivalry between the<br />
army and navy. When warfare was more widespread,<br />
such as in Mesopotamia, the extended lines of<br />
communication stretching over thousands of miles<br />
With the rising tide of nationhood in the British Empire<br />
it was important that Imperial troops were seen to be<br />
treated fairly. On each side of the conflict, nations<br />
accused each other of poor treatment of prisoners.<br />
Relationships between commanding officers and<br />
medical officers was crucial. The Medical Act of 1858<br />
increased the professionalisation of medicine and the<br />
Royal Army Medical Corps was founded in 1898, giving<br />
medical officers the same ranks as the rest of the army.<br />
However, relations remained strained in the later part<br />
of the Victorian era. In the Boer War the senior<br />
commanders such as Lord Roberts and Sir Garnet<br />
Wolseley had a poor opinion of medical officers and<br />
this view appeared to pass down the chain of<br />
command. There was a great gulf between combatant<br />
officers and medical officers and operational plans<br />
were drawn up without consultation with medical<br />
officers. Advice on water purification, sanitation and<br />
rations was ignored, resulting in 8000 deaths from<br />
typhoid. Consequently public support for the war<br />
declined.<br />
After the Boer War, lessons were learnt. There was<br />
better training of commanding officers in the<br />
importance of hygiene and sanitation. It was thought<br />
that better Japanese medical services had contributed<br />
to their victory in the Russo-Japanese War. The<br />
efficiency and status of the army medical services were<br />
built up by Lieutenant General Sir Alfred Keogh, who<br />
was Director General 1904-1910 and 1914-1918. He<br />
worked well with Lieutenant General Sir Arthur<br />
Sloggett who was in charge of medical services on the<br />
Western Front. Although the rapid expansion of the<br />
army diluted knowledge and caused a relative lack of<br />
training, every effort was made to overcome this. The<br />
High Command on the Western Front was acutely<br />
aware of the connection between good medical<br />
services and morale and the need to provide good<br />
facilities to get soldiers back to their units as soon as<br />
possible.<br />
12
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
In the Dardanelles, the situation was quite different.<br />
General Sir Ian Hamilton excluded the senior medical<br />
staff from his Headquarters before and during the<br />
c<strong>amp</strong>aign. The senior medical officer, Colonel Keble,<br />
was not provided with a boat to take him ashore and<br />
was thus confined to his ship. Estimates of the number<br />
of casualties and the means of evacuating them were<br />
unrealistic and there was poor coordination between<br />
commanding officers and medical officers. The navy<br />
was poorly equipped for <strong>amp</strong>hibious operation and its<br />
ships poorly equipped to deal with casualties. Facilities<br />
and attitudes improved with the second wave of<br />
landings but always lagged behind those on the<br />
Western Front.<br />
Mesopotamia was largely the responsibility of the<br />
Indian Army, with its culture of deference to authority.<br />
Medical officers were excluded from Lt. Gen. Sir John<br />
Nixon’s HQ and little thought was given to logistics or<br />
sanitation. The c<strong>amp</strong>aign was very poorly resourced<br />
until the handover to control by the War Office in<br />
1916. General Nixon would withhold information<br />
from the Viceroy in Delhi and the Viceroy would<br />
withhold information from London. The distances<br />
were enormous and casualty evacuation was held up<br />
by lack of boats. Nixon was eventually replaced by Lt<br />
Gen Sir Frederick Maude in 1916 and there was a slow<br />
but steady improvement. Less deferential civilian<br />
doctors who had volunteered to serve such as Colonel<br />
Sir Victor Horsley 1 also played a role in improving<br />
facilities. Horsley unfortunately died in Mesopotamia<br />
in 1916. Apart from the first period of the war in 1914,<br />
the Western Front was well resourced medically. The<br />
Dardanelles theatre was under-resourced but things<br />
improved with the second wave of landings.<br />
Scrutiny of events by war reporters was surprisingly less<br />
important in informing the population at home than<br />
the return of casualties, visits by dignitaries and<br />
politicians and the presence of civilian volunteers and<br />
experts in the army. The sister of Sir John French, head<br />
of the British Expeditionary Force in 1914, was a VAD<br />
nurse who had no hesitation in informing influential<br />
friends at home of any deficiencies she came across.<br />
Sir Frederick Treves on the other hand was guilty of<br />
concealing evidence both in the Boer War and in WWI.<br />
The High Command was acutely conscious of the need<br />
to maintain public support at home.<br />
Hospital ship No. 1, bearing sick and wounded from Kut,<br />
coming alongside the bank of Tigris at the British lines<br />
at Flalhiyah.<br />
In conclusion, the differences between the three<br />
theatres of war were not simply due to geographical<br />
or operational factors. In general, sanitary and<br />
medical conditions improved even in unpromising<br />
conditions and the main reasons for this were external<br />
scrutiny, better resources and better relationships<br />
between commanding officers and medical officers.<br />
The need for manpower economy and the morale of<br />
troops and families stimulated improvements in the<br />
medical arrangements. The medical and sanitary<br />
advances which were occurring at home diminished<br />
13
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
fatalism in the armed forces and increasing<br />
democratisation increased politicians’ awareness of<br />
their responsibilities to the nation.<br />
During subsequent discussions, Dr John Goldsmith<br />
pointed out the different stress-related conditions of<br />
the two world wars in the 20th century: in WWI<br />
hysterical reactions such as paralysis were common<br />
while in WWII peptic ulcers were more prominent. Dr<br />
Sally Sheard asked if soldiers in WWI had ever been<br />
ordered not to pass on details of conditions as had<br />
happened with returning Far East Prisoners of War in<br />
WWII. Professor Harrison had found no evidence of<br />
this and in any case did not believe that such<br />
prohibitions would have worked.<br />
Dr John Rowlands 2 pointed out that two of the<br />
fourteen medical officers whose names are on the<br />
LMI’s WWI war memorial took their own lives and<br />
wondered how common this was. Professor Harrison<br />
was unable to throw any light on this but considered<br />
that the combination of unrealistic expectations and<br />
appalling conditions was very conducive to severe<br />
mental stress. A further questioner wondered if<br />
conditions in the enemies’ medical services were any<br />
different from ours. Professor Harrison thought that<br />
conditions often depended on how well the war was<br />
going for them. At the time of any defeat, conditions<br />
in enemy hospitals would always tend to be poor.<br />
The meeting closed with a vote of thanks by Professor<br />
Dangerfield and the reading of the University’s<br />
formula of dismissal by Professor Jha.<br />
1<br />
Professor Sir Victor Horsley’s name is on the WWI Roll of Honour in the entrance hall of the Medical Institution.<br />
He was a pioneer neurosurgeon, a Fellow of the Royal Society, member of the Pathological Society and Founder<br />
of the Journal of Pathology. He was elected an Honorary Member of the LMI in 1894. He held many international<br />
distinctions. He died of heatstroke on active service in Mesopotamia on 16th July, 1916 at the age of 59 and is<br />
buried in the Commonwealth War Cemetery in Amarah. The Intensive Care Unit in the Walton Centre for<br />
Neurology and Neurosurgery is named after him.<br />
2<br />
Dr Rowlands is the author of a booklet listing the histories of these fourteen medical officers. There is a copy<br />
in the LMI Library.<br />
14
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Merseyside Annual Healthcare Service 20<strong>15</strong><br />
The Annual Healthcare Service took place at the Liverpool Metropolitan Cathedral in the form of choral evening<br />
prayer on Sunday, 10th May at 3pm. The speaker was Archbishop Malcolm McMahon and the celebrant Canon<br />
Tony O’Brien. The Epistle was read by Mr Graham Lamont, President Elect of the Liverpool Medical Institution<br />
and the Gospel was read by Father Dominic Curran. Also in attendance was Councillor Erica Kemp, Lord Mayor<br />
of Liverpool. The theme was Child Health to celebrate the opening of the newly built Alder Hey Hospital.<br />
In his homily, Archbishop Malcolm McMahon spoke of the faith that leads to help as illustrated in the Gospel<br />
reading. The passage described the healing of the Centurion’s servant and also the healing of Peter’s mother in<br />
law. He pointed out that it was the faith of the Centurion that essentially supplied the cure that Jesus provided.<br />
Jesus’s dying opened a path of cure for all for entry in to the Kingdom of Heaven. The suffering of Jesus was of<br />
value. As the topic of the service was child health, Archbishop McMahon alluded to the faith of the sick child.<br />
This would often provide resilience, hope and joy and energy to the carers. The heart of a child was the gift of<br />
love both from the parents and the Father God. Just as in the same way, Jesus restored the Centurion’s servant<br />
and Peter’s mother in law to perform the task to worship in the service of God. So healing provides us with the<br />
ability to provide our worship in our daily lives through performing the works that God has given us to do.<br />
As healthcare workers we would be contributing to God’s healing creation and this was the time to give thanks<br />
to God for healthcare work.<br />
The first address was given by Dr Alan Fryer, Geneticist at Alder Hey Hospital. He pointed out that 75% of all<br />
serious childhood illness came from genetic disorders. It was important for parents that the condition is<br />
diagnosed so that they would know what to expect and how best to provide support for the suffering child. As<br />
a Clinician, Dr Fryer said that prayer was important to give him wisdom as he set out on his daily tasks. Prayer<br />
should not be seen as an alternative therapy but as part of the care plan that God has for all people, who are<br />
disabled or in any way unwell. The Health Care Service was a time to thank God for the expertise and the science<br />
of medicine and to pray for the needs of the region.<br />
The second address was given by Dr Janine Arnott, a Social Scientist working at Alder Hey. She spoke of the need<br />
to talk to the families directly, helping them through their personal journey of helping a disabled or ill child. It<br />
was her job to make the journey more positive for the parents. Just the simple actions of a child were important<br />
in detecting improvements in the abilities. However it was difficult to quantify such things when applying to<br />
grant-giving bodies to provide funds for further research. She spoke of servant leadership which was the new<br />
buzzword in the health service. She pointed out that it is over 2000 years old, and initiated by Our Lord himself.<br />
Followers of Jesus were in the ministry of providing support, care and cure to those who suffered. There was<br />
no conflict between faith and reason.<br />
The bidding prayers were composed by Reverend David Williams, Chaplain to Alder Hey Hospital and read by<br />
Professor Linda de Cossart CBE, Past President of the Liverpool Medical Institution.<br />
The blessing dismissal was given by Dean Anthony O’Brien. I would like to stress my thanks to all those on the<br />
Committee and in the Liverpool Metropolitan Cathedral for enabling the service to take place.<br />
Professor Peter Davies<br />
Chair, Merseyside Healthcare Service Committee<br />
<strong>15</strong>
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Minutes of the First Ordinary Meeting<br />
Held on Thursday 13th November 2014<br />
‘The GMC in 2014. What Is It (Good) For?’<br />
Professor Anthony Narula, FRCS. Treasurer, Royal College of Surgeons (England)<br />
Mr M McCormick, Prof A Narula and Prof L de Cossart<br />
The President, Mr Max McCormick welcomed<br />
Professor Narula to the first ordinary meeting of the<br />
LMI Academic sessions. Max went on to tell the<br />
audience that he was delighted that Tony had<br />
accepted his invitation to Liverpool explaining that<br />
they had met many years ago as ENT Trainees and<br />
progressed through their careers contemporaneously.<br />
Professor Narula was welcomed to the podium with a<br />
round of applause.<br />
Professor Narula replied that he was enormously<br />
pleased to be at the LMI. He offered a short<br />
biography of himself saying that he had just recently,<br />
at the age of 59 years, retired from the NHS, he said<br />
'to avoid bare below the elbows'. He was born in<br />
South Asia in Burma and came with his family to<br />
Britain as a refugee. He suggested that he was<br />
probably the first asylum seeker to speak at the LMI!<br />
Following school education at a 'Victorian boarding<br />
school in the South East’ he went on to study medicine<br />
at Trinity Hall Cambridge and The Middlesex Hospital<br />
in London. He explained that he managed to<br />
graduate with a minimum of work but not without a<br />
concentrated cramming just before examinations! He<br />
went on to say that he had spent the first twelve years<br />
of his consultant career working as a busy NHS<br />
consultant in Leicester. He was called to the lofty<br />
spires of London to take up a post at St Mary's<br />
Hospital in London just over ten years ago.<br />
He began his talk by setting the scene of what is<br />
regarded as the 'typical consultant' by showing the<br />
entry of 'Sir Lancelot Spratt' (actor James Robinson<br />
Justice) into an early NHS hospital in a flurry of action<br />
and paying little attention to the patients. He went<br />
on to begin his talk ‘The GMC in 2014. What is it good<br />
for?’<br />
The General Medical Council, he said, was responsible<br />
for many regulatory functions with respect to<br />
practising doctors. He showed the complexity of the<br />
various committees and processes, reassuring us that<br />
his talk tonight would focus on ‘Fitness to Practise’<br />
and ‘Revalidation’ but offering a quote from a well<br />
respected psychiatric colleague “All of these bodies<br />
eventually become self-serving”. He proffered that<br />
the GMC is probably at this point right now.<br />
16
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
He continued with a slide showing the photographs<br />
of the medical members of the Council of the GMC.<br />
He invited the audience to name those in the<br />
photographs. Not many could be named. He then<br />
showed photographs of the lay members of Council<br />
and again few if any could be identified. He pointed<br />
out Dame Suzie Leather, former head of the Charity<br />
Commission who is now a lay member of the Council.<br />
He reminded us that not only were these people<br />
responsible for overseeing the annual GMC spend of<br />
100 million pounds but were also our leaders in<br />
medical regulation.<br />
Fitness to Practice<br />
Professor Narula went on to say that as a practising<br />
doctor, you may one day receive a letter from the<br />
GMC, and as time goes on the number of people<br />
receiving these will go up. He asked if any in the<br />
audience had received one. None had. Currently he<br />
said, each year about 1 in 25 will receive such a letter.<br />
It is probably the most awful heart sink moment in a<br />
doctor's professional career.<br />
The letter will inform you of the complainant and you<br />
will be asked to fill in the form to include all the places<br />
that you have ever worked. The name of the<br />
complainant may be a very disgruntled patient and<br />
well known to you. The GMC will follow this up by<br />
writing to every medical institution at which you have<br />
worked asking 'Is any thing known about this doctor?’<br />
The chief of that organisation will have to consider<br />
their position when they reply.<br />
There are about 250,000 doctors on the register and in<br />
2012 there were 10,000 such complaints (4%). This<br />
figure has gone up by almost 20% on the previous<br />
year and by 50% on the previous five years. Following<br />
review of the complaint 6000 will be dismissed but the<br />
rest will trigger some sort of investigation. That<br />
translates into investigations being instituted by the<br />
GMC on 4000 doctors in one year. Approximately 60%<br />
of these are likely to undergo a fuller investigation.<br />
This is an enormous workload, but perhaps more<br />
worryingly it is a chance for sensationalists and<br />
journalists to misuse the statistics and predict that in<br />
time every doctor will be investigated. All of this<br />
neatly missing the fact this already causes huge pain<br />
and agony to doctors and their families, in some cases<br />
destroying careers of innocent doctors.<br />
If the complaint is not dismissed, you may be called to<br />
the Interim Orders panel. This will happen very<br />
quickly, within a month of the first letter. In 2012, 800<br />
doctors were referred here and eventually 216 went<br />
to full panel hearings with a further one hundred<br />
doctors agreeing 'undertakings' related to the<br />
complaint. Panel hearings were 208 down from<br />
previous year and there were 55 erasures and 64<br />
suspensions.<br />
Professor Narula continued, saying that until late 2013<br />
he was chief of neurosciences (ENT, Maxillo-Facial,<br />
Head and Neck and Neuro) at Imperial and responsible<br />
for nearly 100 consultants. The following two casestudies<br />
illustrated what happens to individual<br />
practitioners when things go wrong.<br />
Case Study One: Doctor has an affair with his<br />
secretary.<br />
A respected surgeon, who was under Narula's care as<br />
a manager, received a letter from the GMC with the<br />
criticism that he had taken advantage of a woman<br />
colleague, started an affair with her and then dumped<br />
her.<br />
As the chief of the department Narula had received<br />
all the paper work and having read it, felt the GMC<br />
complaint was without foundation.<br />
The surgeon told Professor Narula his version of the<br />
story. He had had an affair and this had broken down<br />
when he had declared to his lover that he was not<br />
going to divorce his wife. The investigation of the<br />
case uncovered the fact that during this affair the<br />
surgeon had done two things which caused concern:<br />
a) he had arranged for the lover to have an MRI scan<br />
of her knee at the hospital at which they both<br />
worked, and b) he wrote her a prescription, for a drug<br />
she was already prescribed by her GP (thyroxine) as<br />
there had been a delay in getting it from the GP. The<br />
GMC wrote demanding that he appear before them<br />
within the next thirty days. A date was set.<br />
Professor Narula said that he was so concerned about<br />
this doctor that he had visions of him getting onto a<br />
railway station platform and throwing himself under<br />
a train at Manchester Piccadilly on the way to the<br />
hearing. He took a day off and went with him to the<br />
hearing.<br />
The legal costs for the doctor for that day amounted<br />
to £<strong>15</strong>,000. Narula said that he imagined that the<br />
GMC would have been paying a similar amount for<br />
their barrister. The final deliberation of the GMC was<br />
17
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
that there was no risk to the public, no action to take<br />
and no reason to proceed. However, it took just under<br />
two years before the letter saying this arrived on desk<br />
of the surgeon. During that time his revalidation date<br />
was due and because the GMC file was still open, the<br />
Revalidation Responsible Officer at the Trust could not<br />
action his revalidation process.<br />
Case Study Two<br />
A consultant surgeon in his mid sixties, nationally and<br />
internationally well known, received a GMC letter.<br />
The complainant was the private hospital at which he<br />
worked and where he had complained that the<br />
facilities fell short of the required standards. The<br />
complaint indicated 10 cases where his practice had<br />
been found wanting and threatened the safe care of<br />
patients.<br />
Within 9 to 10 months of receiving this letter all of the<br />
criticisms raised had been dismissed. However, 18<br />
months later he got another letter from the GMC<br />
saying it was now going to a fitness to practise<br />
hearing. The ultimate outcome of this hearing was<br />
that there was no case to answer. The effect on this<br />
man's life has been considerable both personally and<br />
professionally as a practising surgeon as well as to his<br />
family.<br />
Our speaker went on to say that the Medical<br />
Protection Society have said that 93% of doctors who<br />
go through fitness to practise processes report severe<br />
anxiety and stress. Whistle-blowing brings with it<br />
considerable personal risks.<br />
Revalidation<br />
Professor Narula changed to the subject of Medical<br />
Revalidation. He said that in the early 2000s the GMC<br />
was all set to institute new and improved<br />
recertification processes and procedures for doctors in<br />
medical practice in the United Kingdom. However,<br />
Dame Janet Smith, the High Court judge who chaired<br />
the Shipman enquiry, heavily criticised the ideas<br />
behind these proposals in her third and final report.<br />
Many lawyers criticised her for going outside of her<br />
remit in the enquiry by making these comments but<br />
her intervention led to a revisiting by the GMC of this<br />
whole process.<br />
Thus a whole new bureaucracy was designed to<br />
respond to the criticism but in fact the only real<br />
difference that came forth was the introduction of<br />
processes of feedback from patients and doctors. The<br />
main thrust of this process was to prevent another<br />
Shipman. But, our speaker went on to say, we all<br />
know Shipman's patients loved him so, even as a mass<br />
murderer, he was unlikely to be picked up by this new<br />
process. There was majority agreement for this from<br />
the audience.<br />
We are now in year two of the era of Revalidation. A<br />
phased process has been introduced and it is<br />
anticipated that all doctors in practice will have been<br />
revalidated by March 2016. There is still much<br />
sceptism abroad in the profession about the process<br />
and some believe that if approximately five per cent<br />
of doctors refused to engage, the whole system would<br />
collapse.<br />
Our speaker went on to say that the underpinning to<br />
Revalidation is annual appraisal. The annual appraisal<br />
process is meant to review the evidence of your<br />
practice as a doctor and the evidence to support the<br />
quality of that practice both in private practice and<br />
NHS practice. It is meant to be both formative and<br />
summative in supporting the continuing professional<br />
development of you, the doctor. “In my experience”,<br />
said our speaker, “I have been appraised since 2003<br />
but never been asked about my private practice.”<br />
The process of appraisal is that the doctor submits a<br />
portfolio of evidence in line with the four domains of<br />
the GMC standards for Knowledge Skills and<br />
Performance; Safety and Quality; Communications,<br />
Partnership and Team work and Maintaining Trust.<br />
Nowadays this is an electronic repository, which can<br />
be supplemented at the time of appraisal by paper<br />
records and evidence. Following a successful appraisal<br />
meeting, a summary is agreed by appraiser and<br />
appraisee and a professional development plan (PDP)<br />
is drawn up and this will form the framework for the<br />
next appraisal. Our speaker went on to say that there<br />
is a requirement in the portfolio for Reflection. He<br />
admitted that he was not sure what this was really<br />
about and that many felt the same way.<br />
One of the key things for appraisal, he offered, is the<br />
inclusion of national registry data about outcomes for<br />
index surgical operations. This is particularly true for<br />
surgeons. He said with considerable feeling that he<br />
had resisted the recent desire by government for<br />
publication of such data before individual clinicians<br />
had had time to see their own results. He went on:<br />
“There are in my opinion a whole lot of potential and<br />
18
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
real risks of poorly collected data. The Team and the<br />
environment of surgical procedures plays a huge role<br />
and is often not accounted for within the data and the<br />
reported results are often to the detriment of an<br />
individual until things are investigated in more<br />
detail.”<br />
He continued by saying that the electronic portfolio<br />
systems are awful and there are many companies<br />
learning how to construct the database 'on the job'<br />
and making money out of healthcare providers in<br />
doing so. As the King's Fund has said “it [appraisal]<br />
will become a box ticking exercise because you have to<br />
have ticked the boxes to be allowed to proceed”. The<br />
well-meaning purposes of doing these things have<br />
been lost in this awful process. The system is unlikely<br />
to pick up those doing locums and in independent<br />
practice who may fall short of the standards.<br />
This bureaucratic monster has been set up by the<br />
Department of Health and the GMC. Locum and<br />
retired doctors have problems in ensuring that they<br />
can account for their practice and remediation for<br />
those falling short of the standards is also very<br />
difficult. He said his experience of managing such<br />
processes left him very concerned about how<br />
meaningful remediation could be achieved.<br />
Remediation is a massive problem he said because<br />
many complaints fall into the domain of psychological<br />
problems and few in managerial positions have the<br />
range of skills to respond to this.<br />
Many of these things suggest, he said, that the GMC<br />
has many unanswered questions. Medical<br />
practitioners especially outside of London need to<br />
remain vigilant and be able to voice critique on what<br />
the GMC and government is doing in particular taking<br />
note of the many unregulated healthcare providers<br />
on the high street.<br />
Professor Narula concluded with some amusing videos<br />
that in a comic and ironic way emphasised some of<br />
these points. He finished by thanking the LMI for<br />
inviting to him to speak and he paid warm tribute to<br />
his wife for putting up with him and his mad working<br />
ways. As a final point he offered the caption defining<br />
the difference between complete and finished:<br />
“If you marry the right person your life is complete if<br />
you marry the wrong person your life is finished, but<br />
if you marry the right person and get caught with the<br />
wrong person you are completely finished.”<br />
The audience responded with applause and there was<br />
the usual time for questions. The meeting concluded<br />
with supper.<br />
Linda de Cossart CBE<br />
He went on to say that the GMC has commissioned a<br />
report from Collaboration for Education and Research<br />
Assessment in Plymouth. He explained that he was of<br />
the opinion that it will find that the profession is<br />
spending a lot of energy and money on ticking boxes<br />
and not getting on with the job in hand. There is<br />
other unfinished business: there is no quality<br />
assurance of the appraisal system between Healthcare<br />
Trusts and this will lead to inconsistencies if and when<br />
doctors move between Trusts.<br />
19
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Minutes of the Second Ordinary Meeting<br />
Held on Tuesday 18th November 2014<br />
Joint Meeting with Liverpool Medical History Society<br />
The Tenth Annual History of Medicine Medical Students’ Prize Evening<br />
Back (left to right): Dr Nick Beeching, Mr Max McCormick, Dr Stephen Kenny, and Dr Christopher Evans<br />
Middle (left to right): Shane D’Souza, Alexander Boone,<br />
Professor Sally Sheard, Dr Susan Evans and Dr Peter Dangerfield<br />
Front (left to right): Kitty Worthing, Siân Elsby and Sophie Gealy-Evans<br />
Kitty Worthing - Winner<br />
‘Crazy to be sane - whatever happened to RD Laing?’<br />
R D Laing was a well-known figure in the 1960s both<br />
in the medical community and amongst sections of the<br />
wider public. He became an important, and for a<br />
while, influential figure in redefining and treating<br />
mental illness - in particular Schizophrenia. However<br />
his ideas and influence were apparently short-lived.<br />
Given criticisms of the style of psychiatric diagnosis<br />
currently employed, this presentation examines<br />
different historical constructions of mental illness and<br />
how it is treated. Opposition to psychiatry has taken<br />
many forms, all of which could not be covered by this<br />
presentation. Therefore I have chosen to focus on<br />
outlining the ideas of RD Laing and the 'antipsychiatry<br />
movement' and to consider the<br />
contribution that he, and they, made to the<br />
understanding and treatment of mental illness. Firstly<br />
I will reflect upon the attitudes and treatments<br />
prevalent in the 1950s and ‘60s and the critique of<br />
these made by Laing and others. I will then examine<br />
some of the possible reasons for the backlash against<br />
Laing and his ideas before finally looking at the extent<br />
to which Laing's ideas are in fact an influence on<br />
modern day attitudes to defining and treating mental<br />
illness - an influence which it argues can be seen in,<br />
for ex<strong>amp</strong>le, the 'user movement' and in the<br />
popularity of 'self-help' groups. I will conclude that<br />
although much of Laing's work lacked scientific<br />
validity, his contribution to making 'madness'<br />
comprehensible and encouraging people to consider<br />
mental illness from an empathic and humanistic point<br />
of view is of great value to contemporary medical<br />
practice and wider society. It also highlights that there<br />
is a lack of historical analysis concerning the antipsychiatry<br />
movement; especially in regards to its<br />
demise.<br />
Shane D'Souza - Second Place<br />
‘Gertrude Elion and Her Drug Discoveries’<br />
Gertrude Elion made significant discoveries of drugs<br />
in the treatment of leukaemia, herpes and antirejection<br />
drugs for kidney transplants. Her hard work,<br />
commitment and attitude led to revolutionary<br />
20
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
developments in the medical world, for which she was<br />
awarded the 1988 Nobel Prize in Physiology or<br />
Medicine. Not only did Gertrude Elion work on drugs<br />
to fight HIV and malaria, she remains an inspirational<br />
figure and a role model of a woman who persevered<br />
in science at a time when there was unfair<br />
discrimination towards women in science.<br />
During the presentation, I discuss the knowledge and<br />
ideas presented before Gertrude’s discoveries, and<br />
how her discoveries have since changed the ideologies<br />
in drug treatment since up to the modern day. I<br />
consider previous ideologies of male dominance in<br />
science and how Gertrude Elion acted as a<br />
distinguishing ex<strong>amp</strong>le as someone who has broken<br />
these barriers.<br />
The presentation discusses her background, career<br />
struggles, women in STEM; science pre-1954 (specifics<br />
regarding knowledge on Malaria/Leukaemia/Antirejection<br />
medicines); science post-1954 (the above<br />
topics and how Elion’s contribution has affected<br />
modern day medicine); the way forward in Medicine.<br />
Alexander Boone - Third Place<br />
‘The Exile of Paracelsus’<br />
‘The art of healing comes from nature, not from the<br />
physician. Therefore the physician must start from<br />
nature, with an open mind’ – Paracelsus.<br />
In <strong>15</strong>26, Philippus Aureolus Theophrastus Bombastus<br />
von Hohenheim, otherwise known as ‘Paracelsus’, was<br />
appointed Professor of Medicine at the University of<br />
Basel, Switzerland. In <strong>15</strong>38 he was exiled from Basel<br />
and died just three years later in Austria.<br />
Paracelsus is commonly regarded as one of the most<br />
influential medical scientists of the Renaissance era.<br />
His methods revolutionised medicine in early modern<br />
Europe. Paracelsus rejected the ancient texts from key<br />
authorities such as Galen and Celsus and insisted upon<br />
using observations of nature to guide his own medical<br />
practice. He specifically rejected Galen’s claim that<br />
health and disease were controlled by the ‘four<br />
humours’. Paracelsus encouraged the study of nature<br />
and pioneered an experimental approach. He also<br />
believed in the existence of gnomes, spirits and fairies.<br />
Public burning of books by Ibn Sina and Galen,<br />
inviting non-academics and lay-people to his lectures<br />
and rejecting much of university-taught medicine<br />
gained Paracelsus much notoriety. His actions<br />
ultimately led to his exile. Paracelsus argued that the<br />
body operated as a chemical system subject to internal<br />
and external influences. This premise led Paracelsus<br />
to introduce chemical substances into medicine.<br />
Mercury, for ex<strong>amp</strong>le, was used for the treatment of<br />
Syphilis. Paracelsus is therefore often termed the<br />
‘Father of Toxicology’.<br />
I propose to discuss the modern day relevance of<br />
Paracelsus and also Paracelsian theory in terms of its<br />
medical, philosophical, socio-political and religious<br />
connotations. I hope to convey the pugnacious<br />
temperament of the man and define exactly how he<br />
defied medicine in his day!<br />
Siân Elsby - Runner-Up<br />
‘Medical Ethics and the Third Reich’<br />
The atrocities perpetrated during World War II are<br />
well documented. The Nazi eugenics movement<br />
persecuted ‘sub-human’ non-Aryans: labelled as<br />
'genetically unfit', these people were rounded into<br />
concentration c<strong>amp</strong>s and routinely sterilized, used as<br />
subjects in human experimentation, and killed. The<br />
scale was unprecedented: after war broke out in<br />
September 1939, so-called 'mercy deaths' became<br />
commonplace at mental hospitals - between January<br />
1940 and September 1942, some 70,723 mental<br />
patients were gassed. The total number of Jews<br />
murdered during the war is estimated to be between<br />
5.5 and 6 million.<br />
Much of this torture was given pseudo-scientific<br />
justification and perpetrated by willing medical<br />
professionals. When war ended in 1945, one of the<br />
Allies' priorities was bringing war criminals to justice.<br />
Between December 1946 and August 1947, a trial was<br />
held in Nuremberg - commonly called 'The Doctors'<br />
Trial', the defendants included twenty medical doctors<br />
and three Nazi officials accused of human<br />
experimentation and mass murder under the guise of<br />
euthanasia. A defence offered by many was that no<br />
ethical guidelines governing human experimentation<br />
existed at the time - so no laws were breached.<br />
The Nuremberg Trials gave rise to the Nuremberg<br />
Code in 1947 - it was 'a catalogue of ten principles<br />
which would protect the rights of experimental<br />
subjects and other vulnerable groups in the future’.<br />
This led to the Declaration of Geneva in 1948, which<br />
shaped the Declaration of Helsinki in 1964 - a set of<br />
21
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
ethical principles regarding human experimentation<br />
developed for the medical community by the World<br />
Medical Association.<br />
The presentation will seek to inform the audience<br />
about what led to the Nuremberg Trials - and invite<br />
them to reflect on whether it is unethical to use<br />
information gained from Nazi experiments, or if to<br />
ignore it would mean millions of people ‘died for<br />
nothing’.<br />
Sophie Gealy-Evans - Runner-Up<br />
‘Anaesthesia in the First World War’<br />
Anaesthetics is now considered an essential part of<br />
medicine, but in 1914 it was a game of trial and error.<br />
The First World War was a brutal massacre of life, for<br />
which both soldiers and medical professionals were<br />
severely unprepared. There was a sudden<br />
advancement in anaesthetic techniques in this period<br />
(1914-1918), during which a massive need for pain<br />
relief and emergency treatment resulted in the<br />
established role of the anaesthetist. Out of the<br />
desperation came innovative new ways to deal with<br />
casualties and poor facilities.<br />
I believe there were three key elements that were<br />
outcomes of the harsh conditions of war - the role of<br />
the anaesthetist, the development of anaesthetic<br />
agents and their administration and the better<br />
understanding of the physiology behind them. In this<br />
presentation, I would like first to give some<br />
background on what was already known about<br />
anaesthetics at the time, and then consider how each<br />
of these three aspects developed, and why the War<br />
was so integral in their progression.<br />
On the year of its centenary, it is especially important<br />
that we recall how this war shaped and moulded<br />
these three elements, and I will consider how the<br />
setting of World War I was both a catalyst, and<br />
limiting factor, to the advancements of anaesthetics,<br />
which shaped the course of new advancements. It<br />
should be remembered whilst looking at new<br />
developments in the war zone that these must be fully<br />
explored and adapted to civilian life, away from the<br />
limitations of combat, so that positives can be taken<br />
from the horrific situations from where they came. I<br />
believe it is a topical subject, and an educational way<br />
to pay respect to those who died during the First<br />
World War.<br />
22
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Minutes of the Third Ordinary Meeting<br />
Held on Thursday 20th November 2014<br />
‘Catheter Ablation for Cardiac Arrhythmias: What’s New?’<br />
Dr Dhiraj Gupta, Consultant Cardiologist and Electrophysiologist,<br />
Liverpool Heart and Chest Hospital<br />
‘Device Therapy for Heart Failure’<br />
Dr Richard Snowdon, Consultant Cardiologist and Electrophysiologist,<br />
Liverpool Heart and Chest Hospital<br />
The President introduced Dr Dhiraj Gupta and Dr<br />
Richard Snowdon from the Liverpool Heart and Chest<br />
Hospital. In his introduction he reflected on his own<br />
memories of cardiology and how things have changed<br />
in the intervening years.<br />
Dr Gupta introduced his subject of arrhythmia<br />
ablation, explaining that the Liverpool Heart and<br />
Chest Hospital served a population of 2.8 million and<br />
carried out around 1200 procedures per year. The<br />
ablation of cardiac arrhythmias relies on mapping the<br />
focus generating the arrhythmia and then delivering<br />
either heat or cold to that area. Intravascular<br />
catheters are able to locate the focus of the<br />
generation of the arrhythmia to deliver an electrical<br />
burn and to measure the temperature, or as an<br />
alternative, to deliver cold. The technique may be<br />
used to treat supraventricular tachycardias, atrial<br />
flutter, Wolff-Parkinson-White syndrome and re-entry<br />
tachycardias, atrial fibrillation being increasingly<br />
common. Paroxysmal atrial fibrillation is the most<br />
common arrhythmia treated, and untreated can result<br />
in serious disability with shortness of breath and<br />
stroke, symptomatic spells and may reduce life<br />
expectancy significantly.<br />
In around 2000 it had been determined by intracardiac<br />
electrical mapping that the commonest position was<br />
around the origins of the pulmonary veins and<br />
creating a circular scar around this area had an 80%<br />
success rate in suppression of such arrhythmias. A cryo<br />
generating balloon was also very effective and could<br />
reduce the symptomatic rate by 80-90%. In the last<br />
decade of the 20th century, a surgical approach had<br />
been adopted using basket electrodes in the atrium<br />
to map arrhythmia origins followed by surgical<br />
burning. This technique sometimes involved 2 or 3<br />
procedures but had an 80% success rate. The ability to<br />
carry out this procedure by intracardiac catheter had<br />
now superseded the surgical approach. The<br />
procedures were not without some complications, but<br />
these were increasingly uncommon with increasing<br />
experience. Bleeding from the catheter entry site,<br />
usually in the groin, t<strong>amp</strong>onade from perforation and<br />
the accumulation of intrapericardial fluid were not<br />
unknown but were increasingly uncommon,<br />
particularly with the advent of ultrasound guidance<br />
to determine accurately the catheter position.<br />
Subsequently pulmonary vein stenosis at the site of<br />
the scar was not unknown but rare.<br />
The starting point for consideration of catheter<br />
ablation of arrhythmias was the failure of drug antiarrhythmic<br />
treatment. There is now approximately<br />
ten years’ experience of catheter ablation with good<br />
long term results gradually accumulating.<br />
Dr Richard Snowdon discussed recent advances in<br />
implanted devices, in particular, pacemakers<br />
for the treatment of heart block and bradicardias,<br />
for the termination of tachyarrhythmias and<br />
resynchronisation of atrial and ventricular<br />
23
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
components of cardiac output to improve heart<br />
failure. Most devices were battery operated with<br />
leads to the appropriate areas of the heart. The leads<br />
were able to sense cardiac electrical impulses and<br />
deliver an appropriate electrical stimulation.<br />
The majority of pacemakers inserted are dual chamber<br />
with leads to both atria and ventricle. Single chamber<br />
pacing is occasionally indicated in the atrium for sinus<br />
node dysfunction with normal atrio-ventricular<br />
conduction or ventricular pacing only for ventricular<br />
rate control resistant atrial fibrillation. Cardiac<br />
function is best maximised by efficient synchronised<br />
atrial and ventricular activity. The existence of an<br />
intraventricular bundle branch block results in<br />
dysfunctional ventricular activity, in particular a left<br />
bundle branch block gives rise to a dysfunctional left<br />
ventricular contraction. In the past, pacing of the<br />
right ventricle mimicked a left bundle branch block<br />
and subsequent inefficient activity. This could be<br />
overcome by pacing the posterolateral wall via the<br />
coronary sinus requiring a 3 lead pacemaker.<br />
Ventricular tachycardia or ventricular fibrillation is<br />
amongst the commonest cause of sudden cardiac<br />
death. Modern devices are able to sense ventricular<br />
tachycardia or ventricular fibrillation to terminate it<br />
and pace the ventricles. Unfortunately this technique<br />
does not work for atrial fibrillation. Ventricular shock<br />
so delivered can be painful but this is a relatively small<br />
price. Dr Snowdon continued by briefly describing the<br />
technique involved in the insertion of such devices.<br />
The heart is approached from the systemic venous side<br />
and a subcutaneous pocket is developed for the device<br />
itself. Leads are of either a corkscrew or a grappling<br />
hook type of end, which engages with the<br />
trabeculations within the heart. Subcutaneous<br />
defibrillation devices for ventricular tachycardia or<br />
ventricular fibrillation have no intracardiac lead.<br />
Intracardiac leads are continually moving and<br />
therefore can become broken or moved from the<br />
implanted position. Such devices will deliver a shock<br />
to revert VT or VF but can only give rescue pacing.<br />
Sudden cardiac death is usually of arrhythmic origin.<br />
Implanted defibrillators do make patients live longer<br />
but the anxiety about such attacks of VT or VF does<br />
remain. In the presence of known episodes the risk of<br />
death in five years, if untreated, is around 50%, and<br />
the chance of surviving cardiac death outside hospital<br />
is around 5%. In the presence of a known chance of<br />
catastrophic arrhythmia implanted defibrillators<br />
present a significant risk improvement. Life<br />
expectancy is improved. Inappropriate shocks are<br />
rare. Battery life of such devices is 5-8 years.<br />
Indications for such devices are a known arrhythmic<br />
problem, either familial or acquired with improved<br />
long term survival following surgery for congenital<br />
heart disease. Right ventricular failure can also present<br />
an arrhythmic risk. The long term outcomes for the<br />
different groups are obviously variable.<br />
In the investigation of arrhythmias and syncope<br />
attacks, external monitoring devices have a limited<br />
use. Implantable loop recorders are capable of<br />
monitoring for up to three years and usually record a<br />
7-10 minute cycle overwritten if no event occurs. They<br />
may be interrogated transcutaneously by telephone<br />
without the necessity for visiting the monitoring<br />
centre.<br />
In recent years there have been significant<br />
advancements in the scope of the use of such devices.<br />
The risk of lead failure is now very low, battery life is<br />
extended considerably and sophisticated electronics<br />
are capable of sophisticated tasks. Although the<br />
presence of an implanted device does improve patient<br />
outlook, it is apparent that not all anxiety from<br />
knowledge of the underlying condition is removed,<br />
and patients continue to need significant<br />
psychological support which at present is ill resourced.<br />
The President thanked the two speakers from the<br />
Liverpool Heart and Chest Hospital.<br />
R Franks<br />
24
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Minutes of the Fourth Ordinary Meeting<br />
Held on Thursday 27th November 2014<br />
‘The Human Papilloma Virus Epidemic – Sex, Science, Cancers, Vaccines and the Media’<br />
Prof T M Jones, Consultant in ENT & Head and Neck Surgery, Aintree University Hospital<br />
And<br />
Dr C O’Mahony, Consultant Physician in Sexual Health, Countess of Chester Hospital<br />
Dr C O’Mahony, Mr M McCormick and Prof T M Jones<br />
Dr O’Mahony opened with some anecdotes before<br />
moving on to some startling genital images. Dr<br />
O’Mahony discussed recent editorials he was involved<br />
in with the BMJ:-<br />
i) HPV Vaccination: Reaping the rewards of the<br />
appliance of Science<br />
(BMJ 2013;346:f2184 doi: 10.1136/bmj.f2184<br />
(Published 19 April 2013)<br />
ii)<br />
HPV Vaccination: What about the boys?<br />
BMJ 2014;349:g4783 doi: 10.1136/bmj.g4783<br />
(Published 29 July 2014)<br />
HPV causes a wide range of conditions and evidence<br />
has accumulated over the last 30 years of its oncogenic<br />
role. From this evening’s point of view it was about<br />
genital warts, laryngeal papillomas, cervical cancer,<br />
vulval cancer, vaginal cancer, anal cancer and<br />
oropharyngeal cancer.<br />
HPV types 6 and 11 cause anogenital warts, rarely<br />
oropharyngeal warts and occasionally laryngeal<br />
papilloma.<br />
HPV vaccine was considered impossible as people can<br />
often be infected again with the strain or simply<br />
develop recurrences. However, Professor Fraser<br />
working in Melbourne isolated the outer capsid<br />
protein, L1, for HPV 16 and remarkably these capsids<br />
self-assembled to create the perfect scientific vaccine,<br />
ie; a protein coat with absolutely no nucleic material<br />
inside. This virus-like particle (VLP) looks exactly like<br />
the real thing so stimulates an immune response<br />
which is perfect for dealing with the actual agent.<br />
Also, intramuscular injection of this vaccine produced<br />
very high antibody levels and immune response to<br />
HPV of a far greater magnitude than from a real<br />
infection. Remarkably, these vaccine trials show 100%<br />
in many of the trials which was a staggering result.<br />
Two vaccines are available, (i) Cervarix, containing 16<br />
and 18 the predominant oncogenic types and (ii)<br />
Gardasil, which contains 6, 11, 16 and 18. SPMD will<br />
soon produce a nanovalent vaccine containing<br />
additional oncogenic types.<br />
Professor Jones then gave an overview of increasing<br />
incidence of oropharyngeal cancers and, in particular,<br />
the near epidemic increase in human papillomavirus<br />
genotype 16 associated oropharyngeal cancers (HPV+<br />
OPSCC) seen in the developed world in the last four<br />
decades. Whilst sexual contact is a pre-requisite for<br />
developing HPV+ OPSCC, which specific sexual act is<br />
most relevant is not clear from the data. Whilst the<br />
vast majority of sexually active individuals will contract<br />
an HPV infection, the vast majority of us will clear the<br />
25
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
infection whilst a small percentage (
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Minutes of the Fifth Ordinary Meeting<br />
Held on Thursday 8th January 20<strong>15</strong><br />
Joint Meeting with the Liverpool Society of Anaesthetists<br />
‘Improving Outcome for High Risk Surgery’<br />
Prof Rupert Pearse, Royal London Hospital<br />
Mr M McCormick, Prof R Pearse and Dr E Forrest<br />
Professor Pearse opened his talk by declaring two<br />
conflicts of interest; firstly he believed that surgical<br />
outcomes can improve and secondly, despite having<br />
trained as an anaesthetist, he no longer gives<br />
anaesthetics. He quoted the paper by Weiser T.G. et al 1<br />
which estimated that there were 234 million major<br />
surgical procedures worldwide each year. The mortality<br />
rate for all this surgery is not known. If 1% of patients<br />
could be prevented from dying as a result of surgery,<br />
this would result in 2.3 million avoidable deaths each<br />
year. He then showed a slide demonstrating the<br />
international variation in adjusted mortality risk in<br />
comparison with the UK. It appeared that northern<br />
European and in particular Scandinavian countries had<br />
the best results with eastern and southern European<br />
countries having the worst. He looked at the work of<br />
Ghaferi 2 which showed that although surgical death<br />
rates vary widely across hospitals, the rate of<br />
complications seems to be similar.<br />
To understand post-operative complications, Professor<br />
Pearse thought that you had to consider three things.<br />
Firstly the surgery, which technically had greatly<br />
improved, for ex<strong>amp</strong>le, with significantly lower rates<br />
of anastomotic leaks. Therefore these major surgical<br />
complications had reduced in incidence. However the<br />
medical conditions with which patients present had<br />
changed. Those with significantly greater<br />
comorbidities were now undergoing major surgery for<br />
which, in the past, they would be deemed unsuitable.<br />
Finally the perioperative care of these patients was<br />
becoming increasingly important with the recognition<br />
and early treatment of worsening medical conditions<br />
becoming vital. He looked at the consequences of<br />
anaesthesia and surgery where an inevitable<br />
consequence, such as wound inflammation, develops<br />
into a wound infection: a complication. This could also<br />
be respiratory impairment becoming a pneumonia,<br />
immobility resulting in pulmonary embolism and<br />
organ dysfunction becoming acute kidney injury. This<br />
was far more likely in the increasingly frail and<br />
comorbid population undergoing surgery.<br />
Professor Pearse spoke about his vision of<br />
perioperative medicine, of which there are many<br />
definitions. He offered one which was the prevention<br />
and treatment of harm resulting from the tissue injury<br />
of surgery (and anaesthesia). He thought that the<br />
27
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
battle for safety in anaesthesia had now been largely<br />
won and thought that is was time to take this further<br />
outside the operating theatre. He discussed preoperative<br />
assessment which tried to predict patients<br />
who may have poor surgical outcomes. He highlighted<br />
cardiopulmonary exercise testing, one area in which he<br />
was currently researching. He quoted a paper by<br />
Musallam K et al 3 which highlighted the incremental<br />
risk of anaemia with other comorbidities such as<br />
cardiac disease, COPD, renal impairment, all being<br />
associated with a higher mortality. Therefore, as<br />
Shander A et al 4 had highlighted, perioperative patient<br />
blood management is vital for good outcomes. This<br />
includes optimising haemopoiesis, minimising blood<br />
loss and bleeding and the improvement of tolerance<br />
of anaemia. He wondered how many of us have been<br />
presented with a patient on the day of surgery who<br />
had been inadequately optimised but we all felt the<br />
pressure to continue. Almost always we manage to<br />
get the patient through anaesthesia and surgery but<br />
the real problems seem to start a couple of days<br />
afterwards where inevitable consequences often<br />
become complications. Therefore individualised care<br />
must be the aim of pre-operative assessment.<br />
Professor Pearse then looked at the surgical event and<br />
highlighted the importance of checklists and the<br />
variable use of the WHO checklist across Europe. He<br />
spoke about other factors that may help to improve<br />
outcomes such as minimally invasive cardiac output<br />
measurements and the use of epidural anaesthesia. He<br />
thought that these were very important and<br />
anaesthetists in general were not very good at<br />
highlighting the necessity of putting their case across<br />
strongly for pieces of equipment or better nursing<br />
care.<br />
Professor Pearse discussed events occurring early after<br />
surgery and reminded the audience that acute organ<br />
injury can be a cause of long-term harm. This can<br />
include acute lung injury, sepsis-related myocardial<br />
injury and loss of muscle function. He quoted a paper<br />
Squadrone V et al 5 which showed that the early use of<br />
CPAP (Continuous Positive Airway Pressure) for the<br />
treatment of post-operative hypoxaemia can<br />
significantly reduce post-operative respiratory<br />
complications. He also highlighted the association<br />
between post-operative troponin levels and mortality.<br />
Post-operative rises in troponin were associated with<br />
a much higher mortality than similarly raised levels<br />
found in patients admitted through A&E.<br />
Professor Pearse went on to look at events later after<br />
surgery and showed a paper by Khuri et al 6 which<br />
demonstrated those with either pulmonary or wound<br />
complications had a significantly lower 5 and 10 year<br />
survival after surgery. This was again demonstrated for<br />
acute kidney injury after cardiac surgery 7 . Acute<br />
kidney injury was a key cause of chronic kidney disease<br />
as a result of loss of nephrons during each episode. He<br />
reminded the audience that the serum creatinine<br />
actually falls after surgery and therefore if it is raised,<br />
this is evidence of a much bigger injury than a rise<br />
associated with no surgery. Finally, he thought that<br />
anaesthetists should see some patients in postoperative<br />
clinics because they tend to be better at<br />
looking at the whole patient rather than just the<br />
outcome of surgery. They can then refer patients to<br />
relevant specialists if organ dysfunction has worsened<br />
as a result of these surgical episodes.<br />
Professor Pearse thought that surgery could often be a<br />
sentinel event with this being the first contact that<br />
many patients will have with a doctor. This can lead to<br />
the unmasking of many co-morbidities which often<br />
need to be treated prior to surgery and anaesthesia.<br />
He highlighted a number of quality improvement<br />
initiatives, such as the publication of performance data<br />
for individual surgeons and the way that cardiological<br />
services have been reorganised over the last 10 years<br />
showing a major improvement in 30 day survival<br />
following STEMI. He spoke about the EPOCH trial<br />
(Enhanced Perioperative Care for High Risk Patients)<br />
which is a project to implement an integrated care<br />
pathway for patients scheduled for emergency<br />
laparotomy. He described how healthcare can learn<br />
lessons from other industries and highlighted the way<br />
that the building of Crossrail in central London had<br />
changed building culture to greatly improve the safety<br />
of workers on the project.<br />
Finally he thought that the Royal College of<br />
Anaesthetists should be renamed that Royal College of<br />
Perioperative Medicine and reminded the audience<br />
that the College was soon to roll out its initiative in this<br />
area.<br />
1 Lancet 2008;372:139-44<br />
2 NEJM 2009;361:1368-75<br />
3 Lancet 2011;378:1396-407<br />
4 BJA 2012;109:55-68<br />
5 JAMA 2005:293;589-95<br />
6 Ann Surg 2005:242;326-343<br />
7 Hobson C et al, Circulation 2009:119;2444<br />
Ewen Forrest<br />
28
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Minutes of the Sixth Ordinary Meeting<br />
Held on Thursday 22nd January 20<strong>15</strong><br />
‘What I’ve Learnt from Cleveland’<br />
Dr G P Wyatt, The James Cook University Hospital, Department of Paediatrics,<br />
Middlesborough<br />
Dr G Wyatt and Mr M McCormick<br />
The meeting started with the President of LMI, Mr<br />
Max McCormick, introducing our guest speaker Dr G P<br />
Wyatt who was in fact a Liverpool Medical Graduate.<br />
He had graduated in 1973 the same year as our<br />
President and several other LMI members.<br />
Dr Wyatt was one of the two paediatricians involved<br />
in the 1980s child abuse scandal in Cleveland. He gave<br />
a very emotional and somewhat disturbing account of<br />
his involvement in the matter. Indeed he told us that<br />
it was the first time in the ensuing 17 years that he<br />
had spoken openly in public about it.<br />
He summed up his talk in his first slide. “After<br />
Discovery comes Discredit, then Discipline, then<br />
Discussion, then Delay, then Denial, then Damage,<br />
then Defiance, then Dismissal.”<br />
Dr Wyatt used the Cleveland report to illustrate his<br />
talk and went through it in fine detail. He was a<br />
newly appointed consultant paediatrician in 1987 and<br />
wanted to improve his knowledge of managing sexual<br />
abuse in children. He therefore discussed the topic<br />
with his colleague Dr Marietta Higgs. One of the<br />
clinical signs they relied upon was ‘Reflex Anal<br />
Dilatation’. The first wave of admissions of children<br />
was in May 1987. In all some 121 children were taken<br />
into temporary local authority care. This led to<br />
widespread media coverage and the local MP Stuart<br />
Bell made a statement in the House of Commons.<br />
The Tory government set up an inquiry under Lord<br />
Justice (Elizabeth) Butler-Sloss which sat for a year and<br />
published its report in 1988. Dr Wyatt pointed out<br />
that at NO time did the inquiry look into the accuracy<br />
of the doctors’ diagnoses.<br />
Dr Wyatt gave evidence to the inquiry in December<br />
1987. He returned to work in March 1988 with a<br />
restriction on his practice which he described as a loss<br />
of his clinical freedom. Points about this were raised<br />
by members of the audience.<br />
The two paediatricians were accused of compromising<br />
the work of social workers and demands for action<br />
were made in July 1988. Dr Wyatt read an extract<br />
from the minutes of a meeting held at The Royal<br />
Society of Medicine at which Lord Justice Butler-Sloss<br />
was asked whether the inquiry should have<br />
considered the individual cases to see if abuse had<br />
29
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
occurred. He also pointed out that there was NO<br />
recommendation of a restriction of clinical practice<br />
made in the Cleveland Report. Despite this he was<br />
sent a letter about disciplinary action on 18th October<br />
1988 and his severe reprimand was made public!<br />
At this point Dr Wyatt donned a striped prison hat and<br />
vest! He then told us that it was later found that there<br />
was no wide scale error of diagnosis made by Drs<br />
Wyatt and Higgs and a significant number of the<br />
children were subsequently found to be victims of<br />
serious abuse. He said their accuracy of diagnosis was<br />
70-75% which is as high if not higher than other<br />
branches of medicine!<br />
In December 1988 the Regional Health Authority<br />
issued the following to Dr Wyatt:<br />
- a severe reprimand<br />
- a warning as to his future conduct<br />
- a restriction of clinical freedom in that he would<br />
have no further involvement in child abuse matters.<br />
Dr Wyatt made the point that he was not reported to<br />
the GMC by his employers at any time. He felt that if<br />
that had happened he would have been subject to<br />
regular review but would not have had to endure the<br />
20 year restriction on his clinical practice that the RHA<br />
had imposed. Did that restriction amount to a breach<br />
of his human rights?<br />
His contract was eventually terminated in 2010. He<br />
then undertook forensic training and he is now<br />
working as an independent expert writing reports and<br />
assisting the courts by giving evidence.<br />
The meeting concluded with a lively question and<br />
answer session between Dr Wyatt and the audience.<br />
It was quite clear to all who attended that Dr Wyatt<br />
had been through a very traumatic emotional ride<br />
throughout the whole of the Cleveland affair and that<br />
it still affected him deeply. He was thanked by Dr J<br />
Tappin on behalf of the members for sharing his<br />
experiences with us.<br />
John Dorgan<br />
30
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Minutes of the Seventh Ordinary Meeting<br />
Held on Thursday 29th January 20<strong>15</strong><br />
Joint Meeting with Merseyside Medico-Legal Society<br />
‘Contemporary Themes in Whistle-blowing’<br />
Dr Peter Wilmshurst, Consultant Cardiologist & Ethicist, University of North Staffs<br />
Mr N Gilmour, Mr M McCormick, Dr P Wilmshurst and Dr C Evans<br />
Over sixty members and guests attended the lecture<br />
given by Dr Peter Wilmshurst, a retired cardiologist<br />
from Shrewsbury who formerley worked in Stoke at<br />
the North Staffordshire Hospitals, recently rebranded<br />
after the mid Staffs debacle. The meeting was opened<br />
by our President, Mr Max McCormick, who noted that<br />
whistle-blowing was following a series of related<br />
topics concerning the GMC. Dr Wilmshurst was<br />
introduced by HH Judge Nigel Gilmour, a past<br />
president of the MMLS, deputising for Miss Wendy<br />
Owen who was ill.<br />
We were told that in general, whistleblowers were<br />
treated worse than those about whom they<br />
complained. Dr Wilmshurst cited the former Bristol<br />
anaesthetist, who, following the Bristol Kennedy<br />
enquiry had been obliged to seek employment in<br />
Australia, only to be invited back to the UK to deliver<br />
a prestigious lecture to the Royal College of<br />
Anaesthetists some fifteen years later. High profile<br />
cases involving doctors, radiographers and nurses who<br />
had been the subject of professional and physical<br />
intimidation by managers were discussed in clinical<br />
detail and included Baby P, gagging clauses, duty of<br />
candour and child protection issues. Such suspensions<br />
and special leave offered to whistleblowers had cost<br />
the NHS millions of pounds.<br />
A special area of concern was research fraud in which<br />
multinational companies attempted to influence<br />
results and findings of individual doctors, who in turn<br />
came under intense pressure from high ranking<br />
colleagues, Trust managers and, shockingly, academic<br />
institutions and their heads of departments.<br />
Dr Wilmshurst related the long saga of a doctor who<br />
had fabricated results, was awarded academic<br />
distinction, subsequently admonished by the GMC,<br />
then re-employed, dismissed as clinically dangerous,<br />
only to be appointed as a consultant elsewhere. He<br />
then went on to be awarded Fellowships of Royal<br />
Colleges, and unbelievably, a national clinical<br />
excellence award. Most recently, and utterly<br />
astonishingly, he was awarded a national honour in<br />
recognition of patient safety.<br />
By now the audience would have believed almost<br />
anything about the "Club Culture" influencing<br />
decisions of regulators and that similar double<br />
standards affected the judiciary.<br />
31
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
In vigorous discussion Dr Wilmshurst highlighted the<br />
international parallels in Europe, America as well as<br />
the third world and the low probity ranking of the UK.<br />
Our president gave the vote of thanks and members<br />
left the institution into the freezing snowy conditions<br />
bewildered after learning of such a catalogue of cases.<br />
Chris Evans<br />
32
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Minutes of the Eighth Ordinary Meeting<br />
Held on Thursday 5th February 20<strong>15</strong><br />
Joint Meeting with the Institute of Physics<br />
‘Stimulating the Parts that Other Treatments Can’t Reach: The Use of Functional<br />
Electrical Stimulation in Neurological Rehabilitation’<br />
Professor Ian Swain, Clinical Director, Odstock Medical Limited. Professor of Clinical<br />
Engineering, Bournemouth University<br />
Dr H Stockdale, Prof I Swain and Mr M McCormick<br />
Professor Swain studied Electronic Engineering at<br />
South<strong>amp</strong>ton University and went on to complete a<br />
PhD at the same institution. He was, until the end of<br />
2014, the Director of Clinical Science and Engineering<br />
at Salisbury NHS Foundation Trust, a role which he<br />
combined with that of Clinical Director of Odstock<br />
Medical Limited (OML) and Professor of Clinical<br />
Engineering at Bournemouth University. He continues<br />
in his role with OML as well as his Chair at<br />
Bournemouth.<br />
Professor Swain’s talk concentrated on three aspects of<br />
his work:<br />
(i) The basis of Functional Electrical Stimulation (FES)<br />
and its history in Salisbury. He outlined the clinical uses<br />
of FES in patients with Dropped Foot due to upper<br />
motor neuron lesions (pointing out that FES was not<br />
indicated in the rehabilitation of patients with<br />
Dropped Foot due to lower motor neurone damage).<br />
(ii) The setting up of a commercial company in<br />
conjunction with the NHS Trust to manufacture and<br />
market the devices used in FES.<br />
(iii) Clinical results for the application of FES to patients<br />
with neurological disorders. At the end of his talk, he<br />
gave ex<strong>amp</strong>les of other clinical uses of FES.<br />
(i) The basis of FES and its history in Salisbury<br />
Stimulating muscles with electrical currents has a long<br />
history. The ancient Greeks used the technique on<br />
torpedo fish by rubbing amber (clearly, not knowing<br />
what was happening) through to the work of Volta<br />
and Galvani in the 1790s who demonstrated muscle<br />
contraction when starting and stopping electrical<br />
current. More recent work involved the development<br />
of external and implanted pacemakers in the 1950s.<br />
The essential point of the application is to apply an<br />
active electrode to send a current through a nerve<br />
which causes adjacent muscle contraction with the<br />
33
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
current looped to an indifferent electrode.<br />
FES has a role in the rehabilitation of patients with<br />
Dropped Foot due to upper motor neurone lesions due<br />
to stroke, MS, head injury, cerebral palsy, HSP,<br />
Parkinson’s disease and spinal cord injury (but only<br />
above T12). FES has no role in the rehabilitation in<br />
patients with lower motor neurone damage due to<br />
polio, motor neurone disease, peripheral nerve<br />
damage, Guillain-Barre syndrome or spinal cord injury<br />
below T12.<br />
It was in the 1970s that Nightingale and Glanville set<br />
up FES research in South<strong>amp</strong>ton and, in 1984, the<br />
Spinal Unit at Salisbury began work with FES using a<br />
modified Slendertone machine. The service developed<br />
and an in-house design for FES was introduced<br />
culminating in 37 patients with a variety of<br />
neurological conditions causing a Dropped Foot being<br />
treated between 1988 & 1992. The FES clinical service<br />
started in 1992 coinciding with an article in the<br />
Independent newspaper.<br />
Initially, all the equipment was made in-house for<br />
research work. In 1996, the clinical success of FES was<br />
evident and other centres were asking for the<br />
equipment so the Salisbury unit started manufacturing<br />
to a view to commercial development. In 1998, the<br />
Medical Devices Directive came into force and the<br />
Salisbury unit applied for ISO 9000 accreditation which<br />
was granted in October of that year. Patents were<br />
granted in the UK, US and Canada during the period<br />
2002 – 2004.<br />
(ii) The setting up of a commercial company<br />
It became clear that trying to manufacture and sell<br />
products from within an NHS Department would be<br />
fraught with problems. The sales income distorted the<br />
financial position of the NHS department with issues<br />
such as income not being ring fenced, money not<br />
rolling over from one financial year to the next, lack<br />
of funding for long term investment, not being able<br />
to advertise and difficulties with overseas accounts<br />
being just some of the problems.<br />
However, in 2004, the regulations within the NHS were<br />
changed to allow NHS 3 Star Trusts to set up spin-off<br />
companies to capitalise on R&D work carried out<br />
within these NHS Trusts. A business plan was<br />
submitted in 2005 and Odstock Medical Limited started<br />
trading in April, 2006.<br />
Setting up a spin-off company had its initial problems<br />
(such as separating the company and NHS budgets,<br />
seconding staff between the two entities, appointing<br />
an MD with commercial experience and shareholder<br />
agreements.) The company was set up successfully<br />
with 68% owned by the NHS Trust, 18% by Trustees,<br />
12% by staff and 2% by Bournemouth University. The<br />
company appointed its first directly appointed<br />
employee in December 2006 by taking on its Managing<br />
Director. The company turnover in 2006/07 was £820k.<br />
OML went from strength to strength such that in 20<strong>15</strong>,<br />
3.5 wte NHS staff were seconded to OML, 16.6 staff<br />
were directly employed by OML, there was a separate<br />
accounts system established and the company was<br />
profitable with a projected turnover in 2014/<strong>15</strong> of ~<br />
£1.8m.<br />
(iii) Clinical results for the application of FES<br />
Professor Swain described several clinical cases where<br />
patients experienced significant improvements in<br />
walking following the onset of Dropped Foot. Patients<br />
measured their improvement either in increased<br />
walking speed or increased walking confidence, often<br />
accompanied with a significant decrease in fear of<br />
falling and a consequent increase in stability. Patients<br />
frequently reported a reduced (self-rated) effort in<br />
walking.<br />
As an ex<strong>amp</strong>le, he cited results from a group (n = 144)<br />
of patients with Dropped Foot following Multiple<br />
Sclerosis during the period 2008 - 2013. From that set<br />
of results, 91% of patients were still using FES after 18<br />
weeks, there was a significant increase in walking<br />
speed (p
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
He also commented on the opinion of the National<br />
Institute for Health and Care Excellence (NICE) which<br />
considered the treatment of Dropped Foot using<br />
electrical stimulation (www.nice.org.uk/IPG278) and<br />
which supported the use of FES for patients with<br />
Dropped Foot of central neurological origin.<br />
He also briefly reported on the use of FES to improve<br />
hand function, orthopaedic muscle strengthening,<br />
spasticity reduction and facial stimulation among other<br />
clinical applications.<br />
To indicate the level of workload by staff and the<br />
commitment required for the patients, he gave details<br />
of the standard treatment packages, namely:<br />
For walking stimulation:<br />
- Initial assessment<br />
- Set up<br />
- Follow up at: 2 set ups in the first week; 6 weeks; 3<br />
months; 6 months; thence annually.<br />
For upper limb and facial:<br />
- Initial assessment<br />
- Set up<br />
- Follow up at: 2 weeks; 6 weeks; 10 weeks; 18 weeks<br />
and 26 weeks.<br />
In conclusion, Professor Swain stated that FES enables:<br />
(i) a significant increase in walking speed, (ii) clinically<br />
manageable changes in a patient’s functional walking<br />
category, (iii) a significant reduction in the effort of<br />
walking, (iv) a significant reduction in fear of falling,<br />
and (v) a greater likelihood of achieving personal<br />
goals.<br />
At the end of Professor Swain’s presentation, Mr<br />
McCormick invited questions and Professor Swain<br />
responded to several questions from the audience.<br />
Dr Harold Stockdale (IOP Branch member and IOP link<br />
to the LMI) thanked Professor Swain for this<br />
entertaining and informative talk. That the question<br />
session lasted for twenty minutes (and had to be<br />
ended because of time constraints!) in itself indicated<br />
the degree of interest generated by the talk. The<br />
audience showed its appreciation of Professor Swain’s<br />
talk in the usual manner.<br />
Dr H Stockdale<br />
35
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Minutes of the Ninth Ordinary Meeting<br />
Held on Thursday 12th February 20<strong>15</strong><br />
‘Reasons Why Average Life Expectancy is Set to Fall in Developed Countries’<br />
Professor C Vyvyan Howard, Nano Systems Biology, Centre for Molecular Bioscience,<br />
University of Ulster<br />
Mr M McCormick and Prof C V Howard<br />
Prof Howard started by saying that the possibility of<br />
falls in life expectancy was topical at the moment in<br />
view of the ‘epidemic’ of obesity, diabetes and cancer<br />
and displayed graphs which confirmed the increase in<br />
these conditions in recent years. He then suggested<br />
that there might be a common thread linking them.<br />
The average person’s body contains hundreds of<br />
chemicals in minute quantities none of which was in<br />
existence sixty years ago. There are persistent<br />
chemical pollutants which, when recognised, may be<br />
banned; e.g. DDT. There are also transient chemicals,<br />
rapidly eliminated, previously thought to be safe<br />
which are now regarded as toxic even in miniscule<br />
amounts.<br />
An ex<strong>amp</strong>le of a dangerous chemical in plastic bottles<br />
used for a long time is Bisphenol A. This predisposes<br />
to obesity, reduces sperm count and stimulates<br />
production of prostate cancer cells. It is no longer in<br />
use but there are numerous chemicals in the food we<br />
eat, in our drinks and even possibly in our clothes.<br />
These chemicals cross the placenta and may have a<br />
huge effect later in life causing, at least in part, the<br />
conditions mentioned above.<br />
Prof Howard then discussed the increase in cancer in<br />
children and young adults which he suggested may be<br />
due to the effect of chemicals in utero. We must be<br />
more aware of this and strenuous efforts must be<br />
made to identify possible chemical pollutants.<br />
A lively discussion took place involving many<br />
comments and questions, after which we proceeded<br />
to supper terrified at the prospect of ingesting all the<br />
dangerous chemicals in the seemingly innocent food<br />
put before us.<br />
R S Ahearn<br />
36
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Annual Dinner<br />
Held on Thursday 19th February 20<strong>15</strong><br />
Guest Speaker: Professor Richard Ramsden, Department of Ear Nose and Throat<br />
Surgery, Manchester Royal Infirmary<br />
Mr M McCormick, Dame L Muirhead<br />
and Lord Mayor Erica Kemp<br />
Prof R Ramsden<br />
Prof R Ramsden<br />
and Mr M McCormick<br />
At the well attended Annual Dinner of the Liverpool<br />
Medical Institution, the President, Mr Max McCormick,<br />
introduced Professor Richard Ramsden, Emeritus<br />
Professor of Otorhinolaryngology, who, as a<br />
consultant and then professor at Manchester, had<br />
pioneered the development of cochlear implant<br />
surgery in the United Kingdom, for which he was<br />
awarded the MBE in 2014.<br />
Professor Ramsden is a Scot. He graduated from St<br />
Andrews in 1968 and was drawn to the speciality of<br />
ENT whilst a house officer in Scotland. He was a<br />
registrar and senior registrar at the Royal National<br />
Throat Nose and Ear Hospital, London, and was<br />
appointed Consultant in ENT surgery at the<br />
Manchester Royal Infirmary in 1977.<br />
This was an auspicious time for treatment of cochlear<br />
disease. In Australia, in the 1980s, Graham Clarke<br />
pioneered the use of multi-channelled cochlear<br />
implants that allowed the treatment of cochlear<br />
deafness. Professor Ramsden learned of the<br />
technique and developed the use of cochlear implants<br />
in his department in Manchester. It was a technique<br />
which could cure cochlear deafness but it was very<br />
complicated and expensive.<br />
The early treatments cost between £<strong>15</strong>,000 and<br />
£20,000 each.<br />
Professor Ramsden had obtained MRC funding for his<br />
research, and when it was shown to be successful,<br />
other departments in the United Kingdom started to<br />
offer the technique.<br />
A further Australian development had been made by<br />
W Gibson in the 1990s, who showed that deafness<br />
could be diagnosed in infants, and where suitable,<br />
they could be offered cochlear surgery so that their<br />
deafness could be cured in childhood and they could<br />
receive mainstream education.<br />
The Manchester Cochlear Implant Programme,<br />
established in 1988, was recognised as the leading<br />
centre of research in its field in the UK. The<br />
procedures are now available to patients in centres<br />
throughout the United Kingdom. For Professor<br />
Ramsden, these developments are an ex<strong>amp</strong>le of the<br />
NHS working at its best. A discovery was made, the<br />
United Kingdom research had been funded by the<br />
MRC, and a technique, initially available only at a few<br />
centres, had been developed so that it is now widely<br />
available to NHS patients, improving their quality of<br />
life immeasurably.<br />
Professor Ramsden concluded by inviting us to toast<br />
the health of the Liverpool Medical Institution.<br />
John Sprigge<br />
37
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Minutes of the Tenth Ordinary Meeting<br />
Held on Thursday 5th March 20<strong>15</strong><br />
Joint Meeting with Manchester Medical Society (held at MANDEC)<br />
‘Public Health from the Front Line’<br />
Professor John Ashton, CBE<br />
President, Faculty of Public Health Medicine, UK<br />
Prof J Ashton<br />
Professor Ashton was introduced by the Liverpool<br />
Medical Institution President, Max McCormick. He<br />
gave a brief pen picture of his career.<br />
John Ashton was a scholar at Quarry Bank High School<br />
in Liverpool and Newcastle University Medical School.<br />
He then did postgraduate training at the London<br />
School of Hygiene and Tropical Medicine.<br />
He became a Lecturer and Professor of Public Health in<br />
South<strong>amp</strong>ton and subsequently the London School of<br />
Hygiene and Tropical Medicine and University of<br />
Liverpool Medical School. He was a Regional Director<br />
of Public Health for North West England for thirteen<br />
years and the Director of Public Health County<br />
Medical Officer for six years.<br />
He was appointed President of the Faculty of Public<br />
Health, a position he holds until 2016.<br />
John’s approach to public health is acknowledged by<br />
many to be radical and he himself remains outspoken<br />
about his positions and we looked forward to hearing<br />
about his involvements in many of the controversial<br />
areas about which he speaks.<br />
Professor Ashton began his talk by going through<br />
some of his earlier career building moments and<br />
influences and then discussed his early involvement<br />
with controversial programmes. He was involved in<br />
managing the high incidence of teenage pregnancy<br />
in the Liverpool population. He also worked on the<br />
introduction of a controversial syringe exchange<br />
programme seen by many traditionalists as an<br />
encouragement to drug taking but ultimately<br />
acknowledged as saving more lives than many other<br />
health initiatives by helping prevent the spread of HIV<br />
and hepatitis.<br />
John spoke emotively about his attendance at the<br />
Hillsborough football disaster and his part in<br />
managing casualties and his subsequent statements<br />
and assistance to the Court in clarifying the sequence<br />
of events.<br />
He then went on to talk about the establishment of<br />
38
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
the Liverpool Public Health Observatory which has<br />
subsequently expanded into a network monitoring<br />
the effects of health policy on the public.<br />
He spoke stridently about the introduction of<br />
Foundation Trusts - he felt this was a change which<br />
was a step too far, and it had contributed to his<br />
resignation as the Medical Director in Liverpool.<br />
He described his appointment as President of the<br />
Faculty of Public Health Medicine from 2013 to date<br />
and outlined some of the areas where he is involved<br />
including age of consent, the scrapping of warm<br />
homes, the healthy people fund and more noticeably<br />
his involvement in the active management of those<br />
terminally ill.<br />
His wide ranging talk covered other areas, including<br />
conversations with Bill Clinton and other dignitaries<br />
engaged in the health of the nation.<br />
John Ashton’s talk was indeed a tour de force about<br />
his view of public health as being health of the public<br />
as opposed to the traditional view of public health, a<br />
form of catechism of behaviour by health bodies.<br />
The LMI offers its grateful thanks to Manchester<br />
Medical Society for their customary hospitality in<br />
extending a warm welcome and an excellent venue to<br />
visiting guests and speakers.<br />
Max McCormick<br />
39
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Minutes of the Eleventh Ordinary Meeting<br />
Held on Thursday 12th March 20<strong>15</strong><br />
Joint Meeting with the BMA<br />
‘Where Next for the NHS?’<br />
Dr David Wrigley, GP, Carnforth<br />
Mr M McCormick, Dr D Wrigley and Dr P Dangerfield<br />
Dr Wrigley is a GP in Carnforth, north Lancashire. He<br />
sits on the British Medical Association UK Council and<br />
the BMA General Practice Committee and also a<br />
member of the Medical Practitioners Union. He is a<br />
member of the Labour party. He is also a<br />
spokesperson for Keep Our NHS Public – a non<br />
partisan c<strong>amp</strong>aigning group that seeks to bring about<br />
an NHS that is publicly funded, publicly provided and<br />
publicly accountable. He has written numerous<br />
articles and spoken widely on the marketisation of the<br />
English NHS and contributed to the 2013 book ‘NHS<br />
SOS’. A new book has just been published that he has<br />
co-authored with Dr Jacky Davis and John Lister titled<br />
‘NHS for Sale – myths, lies and deceptions’.<br />
While he is a graduate of Sheffield Medical School, he<br />
did apply to Liverpool but was rejected and eventually<br />
entered medicine as a mature student through<br />
clearing! This is not so likely to happen today!<br />
In opening his talk, David introduced the audience to<br />
some key statistics related to the NHS, noting the<br />
colossal rise in costs from £33.5b in 1997 to £113b<br />
today, with millions treated by 147,000 doctors and<br />
371,000 nurses. It was also noted that there are some<br />
36,000 managers employed in the Service.<br />
For the population as a whole, the UK has 2.8 doctors<br />
per 1000 patients compared with Germany 4.0 or<br />
France 3.0, so is relatively under doctored. The NHS<br />
copes with <strong>15</strong>.1m hospital admissions per year. To<br />
meet the demand, Medical Schools Intake has risen to<br />
6262 in 2012. Overall, life expectancy varies in the<br />
country, but is still lowest in areas of denser<br />
population. Comparing the life expectancy to health<br />
spending per capita, David noted that the USA spends<br />
more on health care but overall has a lower life<br />
expectancy.<br />
In the launch of the NHS in 1948, the Evening<br />
Standard proclaimed “Free for all at a cost of £<strong>15</strong>2m”.<br />
Every household got a leaflet about the new service<br />
explaining that “….everyone can use it for free, but it<br />
is not a charity so be responsible in its use. You are<br />
paying through your taxes…” There were charges for<br />
Spectacles though.<br />
40
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
The political consensus in England in the 1990s<br />
supported the concept of a market, and this was<br />
introduced by the Conservatives in 1991. BMA<br />
opposed the plans and were highly critical but were<br />
effectively frozen out of discussion.<br />
Following this new NHS structure, the parties such as<br />
New Labour, with Blair, Milburn and Stevens, were pro<br />
market. So were the Liberals with the Orange Book in<br />
2004 and the latest legislation is very much more promarket,<br />
yet the devolved nations oppose it. Other<br />
aspects of the new NHS include private contribution<br />
through Labour’s PFI scheme. Milburn signed the<br />
concordat 2000 due to waiting lists and Labour put<br />
more money in to the NHS, thus allowing private<br />
hospitals to treat NHS patients. A purchaser/provider<br />
split was introduced together with new contracts.<br />
Patient choice was seen as helpful but did not mean<br />
more providers in the market. Payment by results also<br />
meant increased competition to get income by getting<br />
more work into the day. Any willing provider policy<br />
and the new Trusts allowed hospitals to be more in<br />
charge of their income.<br />
However, patient budgets have not really taken off,<br />
even though the concept was supposed to give more<br />
to a patient to look after their care. These changes<br />
were backed by provision of new insurance schemes<br />
to offer a policy to cope if your money ran out.<br />
Current policies have introduced the CCGs, choice is<br />
creating competition and plurality of provision<br />
allowing more choice.<br />
A 2010 Select Committee looked at the<br />
purchaser/provider split and concluded it offered no<br />
real benefit.<br />
The Commonwealth Fund looked at health care<br />
systems and found the NHS produced the best results<br />
compared with the rest of the world. For world<br />
health, comparing life expectancy with cost, showed<br />
highest cost in USA with the UK performing very well<br />
in spite of every negative comment made about it.<br />
Effectively, this demonstrated a market failure in<br />
practice in the USA. The USA system is a $2.3 trillion<br />
medical industrial complex but there are 50m people<br />
uninsured, and 62% personal bankrupts due to health<br />
care costs. ObamaCare came up against the lobby of<br />
industry opposition, using phrases like “socialised<br />
health care” and “look at the mess of the UK NHS”.<br />
The pressure for change was of course poor outcomes<br />
from life expectancies and infant mortality.<br />
As a case study, David noted that a North Carolina<br />
man got arrested for theft of $1 so he could get free<br />
health care, demonstrating a situation of desperation.<br />
Changes to the structure of NHS came from legislation<br />
in Parliament, setting up Strategic Health Authorities<br />
with Primary Care Trusts and NHS Trusts in the 1990s.<br />
The current 2013 structure is highly complex with<br />
different bodies.<br />
Dr Wrigley asserted that there were numerous myths<br />
circulating about the NHS. The first is that it is<br />
unaffordable. However, he pointed out that as a<br />
percentage of GDP, the cost is actually stable, running<br />
at about 30% up to 2007. David Nicholson, in 2008,<br />
met McKinsey secretly and a £20b cost saving<br />
challenge was introduced. Cuts from the budget of<br />
NHS quality, innovation, productivity and prevention<br />
challenges were viewed from a position of surplus in<br />
2001. The politicians are not very open and honest<br />
either in their pronouncements. Spending was<br />
increased during 1970 to 2010 but the Coalition is<br />
presently only keeping income just above inflation.<br />
PFI keeps debt off the Government’s balance sheet but<br />
gives big returns to the private sector. It was<br />
introduced by Labour under Tony Blair, and now has<br />
costs of £180m per year. The deals are rock solid,<br />
government backed and can be traded on the open<br />
market. Deals are being sold overseas as they are seen<br />
as a very good investment deal. £12.2 billion could be<br />
£17.4 billion if Government borrowed the money on<br />
the markets, but the real cost is actually more like £80<br />
billion. Interestingly, NHS logo guidelines allow<br />
private companies use the NHS logo, as it is seen as<br />
safe. In context of public opinion, YouGov polls<br />
looked at NHS, Rail, Energy and Mail and showed they<br />
were felt best in national ownership.<br />
The Health and Social Care Act was opposed by all the<br />
medical Colleges, Midwives and the BMA but was<br />
nonetheless adopted. The view is widely held that the<br />
present NHS reforms are the worst mistake by this<br />
Coalition Government. The speaker also pointed out<br />
that there were links between MPs who often ended<br />
up working for the private sector, giving rise to the<br />
‘Revolving doors’ concept.<br />
The speaker then gave a number of quotes, including:<br />
“In the future the NHS will be a state insurance<br />
provider not a state deliverer…” and “…NHS will not<br />
41
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
exist is 5 years…”, quoting Oliver Letwin.<br />
The talk then considered the new concept of<br />
Manchester devolution. The Treasury deal, signed<br />
with councils in Manchester, covers 1.7 million people.<br />
The deal was secretive and there was no consultation<br />
whatsoever with anyone. The devolved budget is £6<br />
billion, to cover health and social care. There are<br />
mixed feelings about the plans but it is clear that<br />
Government will not be involved. Is this the end of<br />
the NHS with the new MHS? Is the money enough to<br />
sustain the service demands? Dr Wrigley noted that<br />
social care alone is a significant cost and members of<br />
the audience raised the point that this move might<br />
risk a blurring between health care and social support.<br />
On a positive note, this devolution takes healthcare<br />
away from Government into the powers of the local<br />
population. However, is it undermining Labour<br />
signing up with Labour councils?<br />
After the election, the outcome is uncertain. Health<br />
policy differs between the contenders but the<br />
Conservatives will continue the same way. Labour will<br />
repeal some of the Health and Social Care Act, such as<br />
market mechanisms, giving us the NHS first option.<br />
Monitor will go and Health and Well-being Boards will<br />
be run with local councils.<br />
LibDems will continue as before while the Greens have<br />
a policy making the NHS entirely publicly provided.<br />
The SNP are anti-market anti-PFI, anti-Trident and<br />
UKIP are difficult to assess.<br />
In concluding, the speaker raised the issues for the<br />
election and what can be done in the lead up to it. He<br />
encouraged the audience to talk to MPs about the<br />
NHS and health policies and write to local papers as it<br />
can have an impact. The BMA is c<strong>amp</strong>aigning to try to<br />
get political interference away from the NHS. But it<br />
was also noted that the Lobbying Act is effectively a<br />
way to stop anyone c<strong>amp</strong>aigning on government<br />
policy and is effectively a gagging bill.<br />
The Pollock Roderick NHS reinstatement bill is laid<br />
before parliament and it will be interesting to see<br />
where this leads to. 38 degrees and Keep NHS Public<br />
are active as well.<br />
Dr Wrigley concluded by saying “Power to the<br />
people!” A range of questions were raised from the<br />
floor.<br />
Issues discussed included the merits of a national<br />
service for providing healthcare as opposed to private<br />
provisions – namely that a national service is joined up<br />
and talks to itself, and private provisions are risky,<br />
inconsistent and driven by profitability, with the profit<br />
not necessarily being re-invested in the health service.<br />
Market contracting is complex, bureaucratic and<br />
secretive, covered by commercial confidentiality. The<br />
role of CCGs was further explored, with some noting<br />
that CCGs could be very difficult to access from a<br />
doctor’s perspective, and lack of transparency and<br />
consultation could lead to inappropriate decision<br />
making and poor direction for patients.<br />
The group pondered the future for education and<br />
training, which is not covered by the private sectors<br />
and is something the NHS does quite well. Where<br />
training has suffered following a takeover, such as in<br />
Nottingham, consultants have resigned in protest!<br />
However, social reform is also needed to achieve<br />
anything.<br />
Some regretted the trend of disappearing GP<br />
partnerships, and the emergence of short term APMS<br />
contracts which offer little security, and would have<br />
liked to have seen more action from the BMA and GPs<br />
to help keep partnerships alive. Also, patients<br />
favoured continuity and would not get it out-with a<br />
partnership agreement.<br />
The conversation turned to the role of managerial<br />
staff and whether it was justifiable to say there was<br />
an over-provision of managers in the NHS. It was<br />
noted that more are needed as complexity develops,<br />
with the appointment of supporting staff, and the<br />
figures bear this out. The NHS is efficient for its size,<br />
and the number of managers is relatively low.<br />
The vote of thanks was given by the President, who<br />
alluded to the excellent content and illuminating<br />
delivery.<br />
Peter Dangerfield<br />
42
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Minutes of the Twelfth Ordinary Meeting<br />
Held on Thursday 19th March 20<strong>15</strong><br />
Joint Meeting with the Athenaeum Club<br />
‘The Flying Doctor’<br />
Dr A A Gilbertson, MD, RAF (retired)<br />
Sir D Maddison, Dr A A Gilbertson, Dr W Taylor and Mr M McCormick<br />
Members of the Medical Institution and their guests<br />
were welcomed to the Athenaeum Club by Sir David<br />
Maddison who then introduced the speaker for the<br />
evening, Dr Alfred Anthony Gilbertson (known to us<br />
as Tony).<br />
Tony told us that he had attended St Edwards College<br />
and Liverpool University Medical School, qualifying in<br />
1956. Although he officially retired from his NHS<br />
consultant post in anaesthetics and intensive care in<br />
1997, he continued with research, gaining his MD in<br />
2013. However, his illustrated talk confined itself to<br />
the period between his conscription into the RAF in<br />
October 1959 and his last sorties during the 1st Gulf<br />
War in 1991. He described how he was initially sent to<br />
Derbyshire as an MO but after eight months, on the<br />
closure of that unit he was able to choose his<br />
subsequent posting; MO to RAF Newton where the<br />
Nottingham University Air Squadron was based.<br />
Learning to fly there was the origin of an amazing<br />
career combining the skills of a pilot and squadron<br />
leader with those of an anaesthetist (he gained FFA<br />
FRCS whilst at RAF Wroughton).<br />
During the five years that he remained in the RAF he<br />
flew high (taking Canberras to 56,000 feet) and far<br />
(for a period he was the only anaesthetist at a military<br />
hospital in Ghana). He regaled us with incidents and<br />
highlights of this period.<br />
In September 1964 he left the RAF, but didn’t stop<br />
flying. He returned to Liverpool, firstly as senior<br />
registrar then consultant in the Cardiothoracic Unit at<br />
Broadgreen Hospital. He continued as an Authorised<br />
Medical Examiner for the Board of Trade,<br />
relinquishing this in 1981.<br />
Dr Bill Taylor thanked Tony for his tales of a misspent<br />
youth and cold-war warrior. The meeting concluded<br />
with an excellent two course meal enhanced by<br />
convivial companions from both the Athenaeum and<br />
Medical Institution.<br />
Christine Brace<br />
43
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Admission of Life Members<br />
The following members were admitted to Life Membership of the Institution at the<br />
Celebration and Admission of Life Members on Thursday 11th December 2014.<br />
Three Public Orators presented these citations.<br />
Back row (left to right): Mr A McCormick, Mr C Faux, Dr W Taylor, Dr J Ridyard, Mr P Rostron and Dr C Evans<br />
Front row (left to right): Dr J Seager, Mr G McLoughlin, Mr M McCormick, Dr E Preston and Mr J Drakeley<br />
EILEEN MARY BELL (in absentia)<br />
Eileen Bell is a retired<br />
Consultant Psychiatrist. She<br />
now lives in Abergele in<br />
retirement.<br />
She initially trained as<br />
a pharmacist at Leeds<br />
University then did her preclinicals<br />
at the College of<br />
Surgeons in Dublin and<br />
qualified from the Royal Free<br />
Hospital School of Medicine in 1963.<br />
After house jobs in London and New York, she came to<br />
Liverpool and trained in psychiatry in various hospitals<br />
including Walton, Rainhill, Newsham and Winwick.<br />
She eventually took a medical assistant post at Rainhill<br />
and later became a Consultant at Rainhill.<br />
In 1977 she moved to Moss Side Hospital which<br />
subsequently became Ashworth Hospital. She retired<br />
in 1992.<br />
She regards her greatest achievement was “just to<br />
qualify at all” at a time when many women struggled<br />
to enter medical school and especially to qualify in<br />
psychiatry which she felt at the time was somewhat of<br />
a Cinderella specialty.<br />
She continues to be interested in ornithology and<br />
photography.<br />
Max McCormick<br />
JOHN RICHARD CLAYDEN (in absentia)<br />
John Clayden is a retired<br />
General Practitioner and<br />
lives in Holmfirth, West<br />
Yorkshire. He was educated<br />
in Royds Hall Grammar<br />
School, Huddersfield and<br />
qualified from Liverpool<br />
Medical School in 1969.<br />
He also shared digs with<br />
John Drakeley.<br />
44
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
After house jobs and SHO job in obstetrics and<br />
gynaecology he entered general practice in<br />
Huddersfield in 1971. He moved to a single handed<br />
dispensing practice in Holmfirth in 1980 and then into<br />
partnership in 1993. He retired from full-time practice<br />
in 2007 but continued working as a locum.<br />
An enthusiastic trainer, he has been involved with over<br />
seventy GP trainees. Unfortunately the demands of<br />
revalidation meant that he was no longer able to<br />
continue working and retired fully in May 2014.<br />
He is married to Marie and has two children and two<br />
grandchildren.<br />
His outside interests include music, theatre, drawing<br />
and painting and he has travelled extensively in the<br />
Caribbean.<br />
Max McCormick<br />
MICHAEL JOHN DRAKELEY<br />
John was educated at the<br />
King Edward VI School<br />
Nuneaton and graduated<br />
from Liverpool Medical<br />
School in 1963. He was<br />
involved in the general<br />
surgical rotation training<br />
scheme at its inception in<br />
Liverpool and this included<br />
time on the Chest Unit at<br />
Broadgreen Hospital.<br />
He did a Fellowship in Aukland for twelve months and<br />
thereafter trained in cardiothoracic surgery and<br />
obtained a Consultant post in 1977 until his<br />
retirement in October 2003.<br />
John was Regional Specialty Advisor for cardiothoracic<br />
surgery and Programme Director for higher surgical<br />
training and an examiner for the Intercollegiate<br />
Board.<br />
Although originally qualified FRCS in Edinburgh he<br />
was awarded an Honorary English Fellowship in 1998<br />
for his contribution to education.<br />
John’s medical legacy continues with Andrew, who is<br />
now in charge of the John Hewitt IVF Unit at the<br />
Liverpool Women’s Hospital.<br />
He and his wife Irene, a marriage of 44 years, have<br />
seven grandchildren. John has a big interest in<br />
ornithology and wildlife photography and is still<br />
involved with various clubs including the Brandreth<br />
Club and the Harlech Club for cardiothoracic surgeons.<br />
He regards his greatest achievement as playing a<br />
significant role in training surgeons in the USA,<br />
Europe and Malaysia.<br />
Max McCormick<br />
JAMES CHRISTOPHER FAUX<br />
Chris Faux and I were<br />
interviewed for entry to the<br />
Liverpool Medical School<br />
consecutively in the autumn<br />
of 1957. I was the last of the<br />
E's and he was the first of<br />
the F's.<br />
This tall, elegant blond<br />
Adonis told me in the<br />
waiting room, that he<br />
attended Fettes College, sang in the choir, played in<br />
an undefeated rugby <strong>15</strong> and had even met the Queen<br />
and Prince Philip when the Royals were choosing a<br />
school for Prince Charles. His father was a GPgynaecologist<br />
from Bolton. To say that I was<br />
intimidated was an understatement.<br />
Chris didn't tell me that his A level choices were for<br />
mechanical engineering rather than the human<br />
variety, so it was perhaps foreseeable that it would be<br />
ten years later before he graduated. In that decade<br />
Faux had been a spectacular President of MSS and a<br />
medical school legend, in the manner of Richard<br />
Gordon's ‘Doctor in the House’.<br />
As an aspiring orthopaedic surgeon, his mechanical<br />
engineering based postgraduate career was meteoric,<br />
such that in ten years he was appointed as a<br />
Consultant Orthopaedic Surgeon to Preston and<br />
Chorley hospitals. By then he had passed first time<br />
and for the first time an examination - FRCS and whilst<br />
training on the Manchester rotation had worked for<br />
John Charnley at Wrightington.<br />
In Preston, he revolutionised orthopaedic services,<br />
waiting lists and trauma and fracture clinics, and<br />
appreciated the stimulus of teaching medical students,<br />
with whom he had a natural affinity. Private practice<br />
also included being MO to Preston Grasshoppers<br />
Rugby Club and British Leyland trucks and busses.<br />
45
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
When Charnley died in 1982, Chris became a trustee of<br />
the trust bearing Charnley's name and subsequently<br />
its chairman for which he edited essays "After<br />
Charnley" for the Robert Jones Series.<br />
Later he returned to work at Wrightington<br />
performing hip and knee revision surgery until he<br />
suffered a mild heart attack in 2003, described by his<br />
wife Patti as “his first attention seeking illness”,<br />
causing Chris to stop water skiing and surgery.<br />
He and Patti, a Consultant Radiologist, have three<br />
children, none medical, and seven grandchildren.<br />
Faux continues to encourage research on behalf of the<br />
trust and nowadays he is a rugby spectator but<br />
regrettably continues to enjoy gun sports.<br />
In conclusion Mr President, our honorary member’s<br />
successful career was only interrupted by a decade at<br />
medical school where he enjoyed himself and met his<br />
wife. I have the honour to present James Christopher<br />
Faux for Life Membership of our Institution.<br />
GERARD ANTHONY McLOUGHLIN<br />
Chris Evans<br />
Gerry is a retired vascular<br />
surgeon who worked at the<br />
Royal Liverpool Hospital.<br />
He was born in the Scottish<br />
borders and exiled from<br />
Newcastle by German<br />
bombers. His mother’s<br />
family was from Scotland,<br />
his father’s from the west of<br />
Ireland. Both had settled in<br />
Newcastle Upon Tyne. Six months after Gerry was<br />
born, his Father was tragically killed in action in Sicily.<br />
His Mother trained to become a school teacher to<br />
support their only child.<br />
He boarded at Austin Friars School Carlisle and studied<br />
Classics. Inspired by the school’s GP he studied sciences<br />
and entered medical school. In 1966 he qualified from<br />
Durham Medical School with a First Class medical<br />
honors degree. House jobs in Newcastle were<br />
followed by registrar jobs in general surgery, initially<br />
on the Brewer and Helsby firm at the Liverpool Royal<br />
Infirmary.<br />
In 1971 he married Liz McSweeney and he has three<br />
children, Claire, Anthony and Terence.<br />
He obtained Fellowships from the Edinburgh and<br />
London Colleges and then obtained senior jobs<br />
working with Professor Robert Shields and Robert<br />
Sells and then senior registrar with John McFarland.<br />
He was a vascular Fellow in Boston and Harvard for<br />
several years and obtained an MD and MS.<br />
He was appointed as Consultant Vascular Surgeon at<br />
the Royal Liverpool Hospital, initially working with<br />
Raymond Helsby until he retired in 1980 and then<br />
Gerry was in single-handed practice providing vascular<br />
services to the hospital.<br />
In 1999 following cardiac surgery, he retired from the<br />
NHS but then studied law and became a medically<br />
qualified judge working with the Criminal Injuries<br />
Compensation Tribunal Board. He also undertook<br />
medico-legal work.<br />
When Pope John Paul visited Liverpool in 1982, he was<br />
volunteered by his colleagues to be the on-call<br />
surgeon for papal emergencies. Six months after the<br />
visit Bishop Vincent Malone rang his doorbell. As a<br />
token of gratitude the Pope had sent a medal. Gerry<br />
believes this is the only time a vascular surgeon has<br />
been awarded a papal medal sent by a Bishop.<br />
Outside of medicine and family, his interests are<br />
French language and literature and rugby union. As<br />
well as playing rugby until aged 40 he was the<br />
Liverpool Club doctor for about twenty years. He has<br />
left directions that he is to be buried in his Liverpool<br />
Rugby Club jersey.<br />
Max McCormick<br />
ELIZABETH MARY PRESTON<br />
The eldest of five girls, Dr<br />
Elizabeth Preston was<br />
always busy as a child, a<br />
habit she continued into<br />
her career. She was<br />
educated at The Alice<br />
Ottley School for Girls,<br />
Worcester, which since she<br />
has left has amalgamated<br />
with the adjacent boys<br />
school and a gate has been<br />
inserted into the 30ft wall - no doubt since she left it<br />
was felt the wall wasn’t necessary. She completed her<br />
46
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
medical degree here in Liverpool and after house jobs<br />
worked in most of the hospitals in Liverpool, as they<br />
were then, as an anaesthetic trainee. This included<br />
learning to give open ether from Dr J Beddard.<br />
She was appointed as a Consultant in Anaesthesia<br />
including Neuroanaesthesia at Walton and Fazakerley<br />
Hospitals in 1975, later renamed Aintree University<br />
Hospitals. Her medical career was notable for the<br />
multiple times she had to change her roles and<br />
responsibilities as she worked between the Walton<br />
site and Fazakerley - something we may all be about<br />
to go through again as talks of merging hospitals and<br />
service reconfiguration abound.<br />
She will be remembered as a medical leader in<br />
Liverpool, firstly as Clinical Director in anaesthesia and<br />
latterly as Medical Director for ten years (longer than<br />
most survive in that position) including six months as<br />
acting Chief Executive of Aintree Hospital.<br />
Outside medicine, as a school girl she competed very<br />
successfully at national level in show jumping and<br />
three day eventing, a skill she taught her children. Her<br />
son Nick is a Consultant in Anaesthesia in Bristol<br />
Southmead Hospital and her daughter Caroline has<br />
degrees in both Business and Law. She has two<br />
grandchildren and one more on the way.<br />
Like many in the medical profession she met her<br />
husband at work. Tim, who is known to many of you,<br />
was a registrar for Mr James Cosbie Ross when they<br />
met at the lunch table. 46 years later they are still<br />
enjoying lunch together, thanks partly to Tim’s present<br />
early in their marriage of a 72 edition Cordon Bleu<br />
cookery course.<br />
Austin McCormick<br />
JOHN BOLTON RIDYARD<br />
John Ridyard and I first met<br />
at the Royal Southern<br />
Hospital, when John was<br />
the new house physician<br />
and I the medical registrar<br />
on Dr Gerard Sanderson’s<br />
Firm. The apprenticeship<br />
was to influence both our<br />
careers as regards a<br />
physicianly ethos, student<br />
and junior staff welfare and<br />
training, as well as team work based on the firm<br />
structure.<br />
John’s father was a Methodist minister from the<br />
Yorkshire dales where John went to primary school<br />
prior to attending Rydal in the welsh hills. As an<br />
outstanding A level student he went to Cambridge<br />
and graduated in natural sciences before joining the<br />
Liverpool Medical School from where he graduated in<br />
1968.<br />
His straightforward, conscientious and sympathetic<br />
approach to his professional career was rapidly<br />
rewarded with MRCP and an MD from the Broadgreen<br />
Chest Unit where he utilised the radioactive Xenon<br />
apparatus to study regional lung function in a variety<br />
of medical and musculoskeletal disorders under the<br />
direction of Colin Ogilvie.<br />
As a medical registrar he had a year out, not in the<br />
USA or Europe, but in Nigeria as a lecturer in medicine<br />
at the Ahmadu Bello University Hospital in Zaria. This<br />
established his love of Africa, where he has returned<br />
several times. He has crossed the Sahara desert and<br />
climbed Kilimanjaro to cite but two of many revisits.<br />
John’s hobbies are extensive; choral music - he was a<br />
founder member of the Renaissance Music Group of<br />
Liverpool - fell walking unsurprisingly, cycling, travel<br />
especially railways as a latter day Bradshaw rather<br />
than a Portillo, squash and gardening.<br />
John was appointed as Consultant General Physician<br />
to Whiston Hospital where he enjoyed all medical<br />
disciplines and started undergraduate teaching<br />
rounds in the manner of his mentor. A dedicated full<br />
time physician he developed lung function and<br />
bronchoscopy services as well as cardiac measurement<br />
and the CCU.<br />
When aged 46, this self titled unreconstructed<br />
bachelor married Joyce, a Care of the Elderly<br />
Physician, with immediate results such that there are<br />
two sons, both now junior doctors. John’s latest baby<br />
is their border terrier.<br />
Mr President, I have the honour of presenting to you<br />
for Life Membership of this Institution, John Bolton<br />
Ridyard, a resolute trustworthy Yorkshire physician<br />
who is best described by the phrase “what you see and<br />
hear is what you get”.<br />
Chris Evans<br />
47
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
PETER KENNETH MAKIN ROSTRON<br />
Peter grew up in Southport<br />
where his father was a GP<br />
and was educated at King<br />
George V School. A keen<br />
athlete he represented the<br />
school at rugby and<br />
captained the cricket team<br />
and informs me he once ran<br />
100 yards in 10.2 seconds.<br />
He qualified from Liverpool Medical School in 1967.<br />
After demonstrating anatomy for a year, he started on<br />
his career then had a year out as a ship’s surgeon with<br />
P & O circumnavigating the globe.<br />
He returned to Liverpool, completed his rotational<br />
training in orthopaedics and was appointed as a<br />
General Orthopaedic Surgeon at Whiston and St<br />
Helens in 1979, with particular interest in paediatric<br />
orthopaedics. He provided his expertise to St Helens<br />
and Widnes rugby league clubs as well as Everton for<br />
over twenty years.<br />
He is married to his wife Christine and has three<br />
daughters and five grandchildren.<br />
He resigned from the Health Service in 1995 but<br />
continued in practice until 2007 and still does some<br />
medico-legal work.<br />
He is a keen golfer, captained Birkdale in 1998 and<br />
presented Mark O’Meara with the Claret Jug in 1998.<br />
When not playing golf, he plays bridge, watches birds<br />
and looks after hens and a few sheep on his farm in<br />
Ormskirk.<br />
Max McCormick<br />
JOHN SEAGER<br />
Dr John Seager was educated<br />
at Malvern College before<br />
coming to Liverpool for his<br />
medical degree. He specialised<br />
in paediatrics, training first in<br />
Liverpool, then at Great<br />
Ormond Street Hospital, The<br />
Institute of Child Health and<br />
University Hospital Wales in<br />
Cardiff. His interests included<br />
paediatric immunology and allergy and he was a<br />
Consultant Paediatrician at Arrowe Park Hospital<br />
Wirral, where he became the Clinical Director for<br />
Paediatrics.<br />
One of his happiest achievements at that time was to<br />
move some aspects of paediatric care out of the<br />
hospital environment into the community. This<br />
involved further developing the Hospital at Home<br />
team and setting up a day ward so that more children<br />
could be treated at home with their families. This he<br />
achieved not without some political skill in convincing<br />
local politicians of the need to close a children’s ward<br />
to make this happen. Now in a well earned<br />
retirement with his wife Liz, he enjoys electrical<br />
things, languages and growing things you can eat.<br />
He is most welcome as a Life Member at the LMI, an<br />
Institution his father was President of in 1973 (the year<br />
of my birth).<br />
Austin McCormick<br />
WILLIAM (BILL) TAYLOR<br />
William Taylor, known<br />
when he worked in the<br />
Royal’s pathology<br />
department as “the nice Bill<br />
Taylor”, graduated from<br />
Liverpool Medical School in<br />
1969. He had been<br />
educated at the Liverpool<br />
Collegiate School and his<br />
house jobs were at the<br />
David Lewis Northern<br />
Hospital. It was here that his mind was turned in the<br />
direction of pathology and he was inspired by Dr<br />
Winston Evans. He was unwilling to give up direct<br />
contact with patients so soon after qualifying, but a<br />
year as an SHO in obstetrics at the Liverpool Maternity<br />
Hospital, passing the DObst RCOG examination,<br />
confirmed his view that pathology was the career for<br />
him. As a trainee, Bill recalls the great influence of<br />
such icons as Alan Cruickshank, Charles St Hill, David<br />
Weatherall and Alan Percival.<br />
As a lecturer then senior lecturer in the University<br />
Department of Pathology his interest in pulmonary<br />
pathology was shaped by Donald Heath and in<br />
gastroenterology by Alan Cruickshank.<br />
48
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
In 1983 Bill was appointed to Fazakerley Hospital as a<br />
Consultant Histopathologist where he provided a<br />
regional-wide service on resected and biopsied lung<br />
specimens. With William Kenyon, from the<br />
Broadgreen Laboratory, he attended the regional<br />
combined thoracic meetings at Broadgreen Chest Unit<br />
where their diligent microscopic detailed reports<br />
spawned many papers for the clinical staff. Believing<br />
that pathologists should see patients, he did a weekly<br />
endoscopy list which he regarded as ‘pathology on the<br />
hoof’. This greatly enhanced understanding and<br />
cooperation between the gastroenterologists and the<br />
laboratory. Later in his career he set up and<br />
singlehandedly ran a service for post mortem<br />
examinations on maternal deaths in the North West<br />
and North Wales. Bill also ran the Histology Journal<br />
Club which never failed to meet over twenty years.<br />
This attention to detail came to the fore when Dr<br />
Peter Davies encouraged him to take over the<br />
editorship of LMI Transactions & Report which he<br />
upgraded from a 20th Century black and white A5<br />
publication to a 21st Century glossy A4 journal. Bill<br />
was President of our Institution in 2009/10 and we<br />
well recall his erudite address on Thomas Hardy, who<br />
remains one of his passions.<br />
Bill married Dr Nancy Gibson, a General Practitioner,<br />
whom he had met at the Northern Hospital. Sadly she<br />
died in 2012. They have three children, one of whom<br />
is a GP in London, and one grandchild. He is now<br />
embarking on a biography of Sir Cyril Clarke, who<br />
introduced him to the LMI when Bill was a student on<br />
his firm at the old Royal Infirmary. When he is not<br />
writing, he is walking or flying as he holds a private<br />
pilot’s licence.<br />
PHILIP NICHOLAS WAKE (in absentia)<br />
Phil Wake is a retired General<br />
and Vascular Surgeon. He was<br />
educated at the Aristotle<br />
Secondary Modern School,<br />
Brixton and Norwood Technical<br />
College, London. He qualified<br />
from Liverpool Medical School in<br />
1969.<br />
Following his training in general surgery and some sub<br />
specialty training in vascular surgery, he was<br />
appointed to Warrington and Halton NHS Trust. He<br />
was Regional Adviser for surgery from 1998 to 2004<br />
and Chairman of the STEC. He was Clinical Director of<br />
Surgery at Warrington Hospital from 1993 to 1998 and<br />
became Medical Director from 2004 to 2008. He has<br />
also acted as a member of the independent review<br />
panel and has considerable experience of being a<br />
medical expert in legal cases.<br />
He is married to Margaret and has three children,<br />
Suzanna, an anaesthetist, Peter, a solicitor, and Kate,<br />
a teacher. He has eight grandchildren.<br />
He regards his greatest achievement as actually<br />
getting into medical school from an inner city<br />
secondary modern school.<br />
His outside interests include golf, DIY, walking and<br />
childcare.<br />
Max McCormick<br />
Mr President, in the case of Bill Taylor, we are<br />
admitting to Life Membership of our Institution a<br />
doctor who has served this Institution well and is an<br />
earnest seeker of the truth.<br />
Chris Evans<br />
49
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
President’s Guest Lecture<br />
Held on Thursday 30th March 20<strong>15</strong><br />
‘The Attempt to Destroy the NHS’<br />
Prof Raymond Tallis, Retired Professor of Gerontology, Manchester and Philosopher<br />
Mr M McCormick and Prof R Tallis<br />
The president introduced Professor Tallis by<br />
welcoming him again to the Institution, Professor<br />
Tallis having spoken on several occasions to the<br />
members of the Institution in the past.<br />
Born in Liverpool in 1946, Raymond Tallis attended<br />
Liverpool College and obtained an open scholarship<br />
to Keeble College, Oxford.<br />
After a degree in animal physiology he completed his<br />
medical degree in 1970 and then completed his<br />
training as a Senior Lecturer in Gerontology in<br />
Liverpool University and thereafter moved to<br />
Manchester as Professor of Gerontology.<br />
He has held many prestigious posts as an advisor to<br />
the Government regarding care of the elderly and<br />
became well-known for his views on care of the<br />
elderly and end of life management. He is a humanist,<br />
atheist and a patron of dignity in dying.<br />
As well as being an exceptionally clear-thinking orator,<br />
he commands respect in the philosophical world.<br />
During his talk he applied his clear thinking to the<br />
present problem of structural, philosophical and<br />
financial management of the National Health Service.<br />
The title of his talk, namely “The Attempt to Destroy<br />
the NHS” left the audience in no doubt from the<br />
outset where he stood on the subject of privatisation<br />
of the National Health Service. He explained that the<br />
impetus for his developing a deep concern for the<br />
future of the NHS was the introduction of the Health<br />
and Social Care Act which was passed in 2012. His<br />
chagrin at the failure of the BMA to oppose it was<br />
documented in two books which he contributed called<br />
‘NHS SOS’ and ‘NHS for sale’.<br />
He set the scene for the Act by turning to the run up<br />
to the election of 2010 when Conservative politicians<br />
made three promises, namely: 1) no cutbacks in<br />
funding, 2) no hospital closures and 3) no further<br />
reorganisations. He then proceeded to illustrate the<br />
duplicity of politicians by demonstrating how they<br />
reneged on each of these promises.<br />
Professor Tallis informed the audience that the<br />
underlying policies of the Health and Social Care Act<br />
were deliberately hidden by subterfuge and<br />
propaganda by the propagation of several “myths” to<br />
50
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
conceal the true intentions of the then Conservative<br />
Government, and they were: 1) that the Health and<br />
Social Care Act was not about privatisation, 2) that<br />
privatisation was not happening, 3) that privatisation<br />
was a good thing anyway and 4) that privatisation<br />
cannot be stopped. These myths were buttressed by<br />
misinformation that the Health Service was beyond<br />
repair, that the NHS was about empowerment of<br />
general practitioners by allowing them to be the<br />
budget holders and patient choice, and that it was<br />
about reducing bureaucracy.<br />
He then provided evidence to refute each of these<br />
assertions and subsequently to identify those elements<br />
of the Conservative party and their supporters, some<br />
of whom were doctors, who were responsible, both<br />
openly and surreptitiously, for developing and<br />
railroading this piece of legislation through<br />
Parliament. He expressed his deep concerns about<br />
other developments such as the Transatlantic Trade<br />
and Investment Partnership (TTIP), an agreement<br />
between the American government and the EU,<br />
particularly the clause called the Investment States<br />
Dispute Settlement, which purports to prevent<br />
governments from interfering in the practice of<br />
business.<br />
Professor Tallis followed this up by listing the<br />
numerous ways in which privatisation would actually<br />
worsen the National Health Service such as disruption<br />
of the tendering process, fragmentation of the service,<br />
and cherry-picking. He gave concrete ex<strong>amp</strong>les of<br />
these worrying tendencies. He was particularly<br />
worried about accountability, teaching, ethical, moral<br />
and de-professionalisation issues in the private sector.<br />
In spite of appearances that privatisation was already<br />
a ‘done deal’, he maintained that it was still possible,<br />
even at this late stage, to rally sufficient support to<br />
reverse the Health and Social Care Act, if not<br />
completely, then at least sections 75 and 165. His<br />
frustration that the media had not woken up to what<br />
was happening and the Royal Colleges had not given<br />
more of a lead surfaced several times. His final<br />
message was that although the situation looked<br />
perilous we should continue to fight for the National<br />
Health Service.<br />
The President thanked Professor Tallis for his<br />
stimulating, factual account about the present NHS and<br />
the effect of the “financial management of the NHS”<br />
and other matters such as teaching, education and<br />
quality of patient care which remain dear to most of us.<br />
Anthony Ellis<br />
51
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
WORLD WAR ONE HEROINE<br />
EDITH CAVELL - EXECUTED FOR TREASON DURING WW1<br />
Born 4th December 1865, in Swardeston, Norfolk<br />
Executed on 12th October 19<strong>15</strong> in Brussels<br />
“But this I would say,<br />
standing as I do in view<br />
of God and Eternity, I<br />
realise that patriotism is<br />
not enough, I must have<br />
no hatred or bitterness<br />
toward anyone.”<br />
Edith Cavell<br />
It is difficult to tell<br />
Edith’s story condensed<br />
into two pages but I<br />
have endeavoured to portray her heroism and<br />
devotion to her fellow man. The incredible injustice<br />
of her execution affected many. The shooting of this<br />
brave nurse was not forgotten or forgiven and was<br />
used to sway neutral opinion against Germany and<br />
eventually helped to bring the U.S.A. into the war.<br />
Propaganda about her death caused recruiting to<br />
double for eight weeks after her death was<br />
announced.<br />
As a young girl, she was far from being a little saint;<br />
however it is clear that, as an adult, she held fast to<br />
her Christian faith. Edith's father was a Church of<br />
England Vicar and would want to keep a strict<br />
Sabbath. There was no play on a Sunday; however,<br />
there was laughter in the family. Edith's father was<br />
not dour and could easily be tempted to disguise<br />
himself as a bear and cause the Cavell children to<br />
shriek with delight.<br />
Edith was quite an<br />
accomplished artist. She<br />
loved drawing and<br />
painting the natural<br />
things around her,<br />
flowers, plants, birds<br />
and even other<br />
people enjoying the<br />
countryside. She would<br />
sometimes give one of<br />
her pictures as a gift to a<br />
villager for a special<br />
occasion.<br />
Edith was not just a talented artist; she was also very<br />
good at French. In 1890, Edith took a governess post<br />
with the Francois family in Brussels. She stayed here<br />
for five years and became a firm favourite with the<br />
family, even though she objected to their jokes about<br />
Queen Victoria being a prude. She continued to paint<br />
in her spare time and became fluent in French.<br />
During her summer breaks she is thought to have<br />
formed a romantic fondness for her second cousin,<br />
Eddie. Unfortunately, he had an inherited nervous<br />
condition he did not think he ought to pass on by<br />
marrying and having children. Edith did not forget<br />
him however, and on the day she was executed, she<br />
wrote in her copy of 'The Imitation of Christ' "With<br />
love to E. D. Cavell".<br />
After testing her vocation for a few months at the<br />
Fountains Fever Hospital, Tooting, Edith (aged 30) was<br />
accepted for training at the London Hospital under<br />
Eva Lückes in April 1896.<br />
In the summer of 1897, an epidemic of typhoid fever<br />
broke out in Maidstone. Six of Miss Lückes’ nurses<br />
were seconded to help, including Edith. Of the 1700<br />
that contracted the disease, only 132 died. Edith<br />
received the Maidstone Medal for her work here - the<br />
only medal she was ever to receive from her country.<br />
In September 1906, Edith went to work for the<br />
Manchester and Salford Sick Poor and Private Nursing<br />
Institution as a nurse at one of the Queen's District<br />
Nursing Homes, in a temporary position for 3 months.<br />
However, since the Matron, Miss Hall, became ill, she<br />
filled in as Matron. In a letter dated 12th March 1907,<br />
she wrote to Miss Lückes at London Hospital, saying<br />
that it was a heavy responsibility, and she knew little<br />
of the work of the Queen's District Nurses. She asked<br />
if there were any trained nurses willing to fill in a 3<br />
month post for pay of £30 per annum. Edith's work in<br />
Manchester was commemorated by a splendid brass<br />
plaque, which was found in a Manchester scrap-yard<br />
in April 2002.<br />
In 1907, after a short break, Edith returned to Brussels<br />
to nurse a child patient of Dr Antoine Depage but he<br />
soon transferred her to more important work. Dr<br />
52
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Depage wanted to pioneer the training of nurses in<br />
Belgium along the lines of Florence Nightingale. Until<br />
now, nuns had been responsible for the care of the<br />
sick and, however kind and well intentioned, they had<br />
no training for the work. Edith Cavell, now in her early<br />
forties, was put in charge of a pioneer training school<br />
for lay nurses, 'L'Ecole Belge d'Infirmieres Diplomees',<br />
on the outskirts of Brussels. It was formed out of four<br />
adjoining houses and opened on October 10th, 1907.<br />
By August 1914 she was despatching the Dutch and<br />
German nurses home and impressing on the others<br />
that their first duty was to care for the wounded<br />
irrespective of nationality. The clinic became a Red<br />
Cross Hospital, with German soldiers receiving the<br />
same attention as Belgian. When Brussels fell, the<br />
Germans commandeered the Royal Palace for their<br />
own wounded and 60 English nurses were sent home.<br />
Edith Cavell and her chief assistant, Miss Wilkins<br />
remained. At her establishment, Edith sheltered<br />
British, French and Belgian soldiers, from where they<br />
were helped to escape to Holland. Edith provided<br />
refuge for soldiers in her school whilst they waited for<br />
the necessary documents and guide to get over the<br />
border. She also provided medical care for any who<br />
were wounded. Edith's network managed to help<br />
over 200 Allied soldiers to escape and, thereby, live to<br />
fight another day. Throughout Belgium, thousands<br />
were helped by other networks in similar ways.<br />
Edith’s cell in prison<br />
Edith was not arrested for espionage, as many people<br />
believed, but for treason. The Germans discovered<br />
that she had helped many allies escape and arrested<br />
her. The Americans argued that she could not be tried<br />
or executed for treason, because as a British citizen<br />
she had no allegiance to Germany; however the<br />
American minister in Belgium was not allowed to<br />
attend the trial.<br />
The execution was carried out at dawn by a firing<br />
squad, on October 12th, 19<strong>15</strong>, in Brussels. Edith was<br />
still wearing her nurse's uniform. Until the end of the<br />
war Edith's body was buried where she was executed<br />
and then carried from Dover to London in a passenger<br />
luggage wagon. This same wagon was used for<br />
carrying the body of the Unknown Soldier some time<br />
later. Her family wanted her re-interred at Norfolk<br />
Cathedral and she was re-interred just outside the<br />
Cathedral in a spot called Life’s Green.<br />
Account by Reverend H. Stirling Gahan<br />
on the Execution of Edith Cavell<br />
On Monday evening, October 11th, I was admitted by<br />
special passport from the German authorities to the<br />
prison of St. Gilles, where Miss Edith Cavell had been<br />
confined for ten weeks. The final sentence had been<br />
given early that afternoon. To my astonishment and<br />
relief I found my friend perfectly calm and resigned.<br />
But this could not lessen the tenderness and intensity<br />
of feeling on either part during that last interview of<br />
almost an hour.<br />
Her first words to me were upon a matter concerning<br />
herself personally, but the solemn asseveration which<br />
accompanied them was made expressedly in the light<br />
of God and eternity.<br />
She then added that she wished all her friends to<br />
know that she willingly gave her life for her country,<br />
and said: "I have no fear nor shrinking; I have seen<br />
death so often that it is not strange or fearful to me."<br />
She gave me parting messages for relations and<br />
friends. She spoke of her soul's needs at the moment<br />
and she received the assurance of God's Word as only<br />
the Christian can do. Then I said "Good-by," and she<br />
smiled and said, "We shall meet again." The German<br />
military chaplain was with her at the end and<br />
afterwards gave her Christian burial. He told me: "She<br />
was brave and bright to the last. She professed her<br />
Christian faith and that she was glad to die for her<br />
country." "She died like a heroine."<br />
Lynne Smith<br />
Assistant Editor<br />
53
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Retired Members’ Group<br />
Tuesday 14th October 2014<br />
The Cheshire Salt Industry and Liverpool Connections<br />
Gilmour Stubbs, Former MD, NW Cheshire Salt Works<br />
Ltd<br />
Gilmour’s family company worked about 8% of the<br />
huge Cheshire Salt Industry before being subsumed<br />
into the dominant British Salt Ltd a few years ago.<br />
Quite apart from producing an essential ingredient<br />
for industry and food, the huge underground spaces<br />
of the salt mines are used for safe storage of all<br />
manner of items except those prone to rust.<br />
Tuesday 2nd December 2014<br />
Hidden Gems of Merseyside<br />
Ian Meadows CBE, DL. High Sheriff of Merseyside<br />
2013-4. Executive Chairman RS Clare & Co.<br />
Ian spoke mostly of his family company, RS Clare, who<br />
manufacture lubricants. The company was founded<br />
in 1748 and continues to trade robustly in its second<br />
quarter MILLENIUM! Part of the factory is on the site<br />
of the former Royal Southern Hospital. This was a<br />
point of nostalgia for some members. Ian also told us<br />
some amusing tales arising from his recent tour of<br />
duty as High Sheriff of Merseyside.<br />
Tuesday 10th March 20<strong>15</strong><br />
Fracking<br />
David Millar, MD Heap & Partners, Birkenhead<br />
David’s family business, Heap & Co. has been trading<br />
in Birkenhead for almost <strong>15</strong>0 years. Its main interest<br />
is in control of fluid at high pressure. Fracking is the<br />
process of extracting hidden reserves of gas and oil<br />
from underground stores, previously untapped, using<br />
water under high pressure. The prospect of a bounty<br />
of almost unlimited fossil fuel could prompt a second<br />
industrial revolution. Reserves in the North of<br />
England are very great. So far, the UK has been<br />
reluctant to commit to fracking, largely for fear of<br />
unknown consequences.<br />
Tuesday 19th May 20<strong>15</strong><br />
SUMMER OUTING<br />
Visit to Elthorn’s Farm, Burton, Home of Mark & Tass<br />
Leather<br />
The weather was kind to our group of about 30 when<br />
we were welcomed to this glorious house and garden<br />
by Mark and Tass. Further exploration led us to a trio<br />
of classic cars on display in the yard, two XK Jaguars<br />
and an early model Porsche. The crowning glory (for<br />
the boys at least) was a large shippon laid out with an<br />
amazingly complex model railway. We were dragged<br />
away, almost screaming, to a fine lunch at the Red Fox<br />
pub in Thornton Hough.<br />
ENVOI<br />
About a year ago, I said that after ten years I had run<br />
my course as convenor of these meetings. It was an<br />
honour and delight to do them. I include a list of the<br />
meetings we had. I thank our speakers most of whom<br />
were not doctors and thus relative strangers to the<br />
LMI. I thank members and their guests who took part.<br />
I thank the LMI staff for coping with the chaos which<br />
I often created.<br />
It is a great joy to me that Chris Evans has agreed to<br />
take over now. Please give him your full support.<br />
Austin Carty<br />
Members who have attended the decade of thrice<br />
yearly meetings, which Austin has served up for us,<br />
together with varied summer outings, will be sorry to<br />
lose his innovative, convivial style and panache. In<br />
thanking him on behalf of us all and wishing him well,<br />
I do hope that you will support the programme I am<br />
arranging, the details of which will be circulated in the<br />
usual way. I look forward to you joining me at midday<br />
on October 20th.<br />
Chris Evans<br />
54
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
LMI Retired Members Group<br />
Meeting Schedule 2005-20<strong>15</strong>: Convenor A T Carty<br />
Date Speaker Title<br />
October 2005 Stanley Owens: Guide dogs for the blind<br />
December 2005 Sir David Henshaw Cranes over the City<br />
March 2006 James Carmichael Glyndebourne<br />
Summer Outing Visit to Rydal Hall and Summerdale House, Cumbria: Sheals Family<br />
October 2006 Captain Mick Owen Soldiers of the Queen<br />
December 2006 Michael Groves Fairbridge<br />
March 2007 Howard Beddow British Canals (part 2)<br />
Summer Outing Visit to Aintree Racecourse<br />
October 2007 Bob Muirhead Mechanical Music<br />
December 2007 Don Menzies Aspects of Midwifery in 19th and 20th centuries<br />
March 2008 Kit Jackson Investment in Fine Wine<br />
Summer Outing Visit to Speke Hall<br />
October 2008 Tony Ensor An Indian Summer in Crime<br />
December 2008 David Lloyd Footballs for Fun<br />
March 2009 Arthur Aldcroft Cotton: the Liverpool Connection<br />
Summer Outing Visit to Bryngwyn Hall, Welshpool<br />
October 2009 Austin Carty A Favourite of the King<br />
December 2009 Frank Carlyle Liverpool Unravelled<br />
March 2010 Nick Wainwright Fascinating Gemstones<br />
October 2010 Terry Overill ‘Operatunity’ in Retirement<br />
December 2010 Helen Carty Carving a niche<br />
March 2011 Elizabeth Steele Liverpool Theatres: History and Present<br />
May 2011 Simon Marsh Sods I have cut on the Turf<br />
October 2011 Peter Kennerley What’s so special about Liverpool Cathedral?<br />
December 2011 Sophia Povey The Reader Organisation<br />
March 2012 Bruce Gibson Past Imperfect or Future Perfect<br />
Summer Outing Visit to Hoylake Lifeboat Station<br />
October 2012 Paul Nolan The Mersey Forester<br />
December 2012 Iolo Thomas Pole Dancing at the Bar. (River Mersey Pilot Service)<br />
March 2013 James Carmichael The Arnolfini Portrait<br />
Summer Outing Ian Tracey Organ Recital at Liverpool Cathedral<br />
December 2013 Jane Kennedy Policing Merseyside: Partners in Crime<br />
March 2014 Lesley Dixon PSS in its 94th year<br />
Summer Outing Visit to the new Central Library, William Brown Street<br />
October 2014 Gilmour Stubbs The Cheshire Salt Industry: Liverpool Connections December<br />
2014 Ian Meadows Little Gems of Merseyside<br />
March 20<strong>15</strong> David Millar Fracking<br />
Summer Outing Visit Mark and Tass Leather’s home: Garden, Model Trains and Classic Cars<br />
55
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
56
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Report of the Strategic Management Council (SMC): 2014-20<strong>15</strong><br />
This year’s president for the 176th session of the<br />
Liverpool Medical Institution was Mr Max McCormick.<br />
He presented a very varied and interesting programme<br />
that included medical military history, marking the<br />
centenary of World War I; Whistle Blowing in the NHS;<br />
personal insights into the Cleveland Scandal from Dr<br />
Wyatt and a thought-provoking lecture by Professor<br />
Vyvyan Howard.<br />
If you were unable to attend, recordings of some of this<br />
session’s lectures are available for members to view on<br />
the LMI website at http://www.lmi.org.uk/publicwebcast.aspx.<br />
Events<br />
The undoubted highlight of the year was the military<br />
medicine exhibition organised by the library,<br />
comparing 1914 and 2014 field medicine, which was a<br />
great success. The exhibition took place from the 2nd to<br />
4th October 2014, in partnership with 208 Liverpool<br />
Field Hospital and in association with Liverpool Medical<br />
History Society. It is estimated that LMI received 800<br />
visitors over the duration of the event. 208 Field<br />
Hospital organised 8 lectures, which were all very well<br />
received.<br />
Displays included Captain Noel Chavasse’s sword and<br />
the last letter he is known to have written, military<br />
uniforms and a recreated trench in the LMI car park.<br />
Adrienne, the LMI Librarian, was successful in obtaining<br />
an Heritage Lottery Fund grant which enabled her to<br />
employ a co-ordinator, train 18 volunteer guides and<br />
video the lectures. VIP guests included the Lord<br />
Lieutenant and the High Sheriff of Merseyside. The<br />
event received excellent feedback via email and the<br />
visitors’ book and had strengthened links with 208 Field<br />
Hospital who were very keen to work with LMI again.<br />
Members can see the photographs of the event and<br />
hear recordings of the talks on the LMI’s website.<br />
LMI was also part of the Alder Hey Centenary<br />
Exhibition celebrating 100 years of Alder Hey. Alder Hey<br />
are very interested in working with LMI on future<br />
projects and events. LMI also opened for Liverpool<br />
Light Night on the <strong>15</strong>th May 20<strong>15</strong>, to celebrate<br />
Liverpool’s medical heritage and invite members of the<br />
public to take a fascinating tour through 250 years of<br />
medicine. Light Night is an annual cultural event where<br />
arts places of interest open their doors until late. The<br />
LMI received an estimated 250 visitors over the 3 hour<br />
duration.<br />
The admin team have been working with Liverpool<br />
Heart and Chest Hospital to share resources for<br />
improving pathways into medicine for students<br />
considering applying to study medicine, and widening<br />
the appeal of the ‘Year 12 Conference’. The variety of<br />
external conferences hosted during the year include<br />
the annual LSTM Neurological Infectious Diseases<br />
conference, the Norman Gibbon Urology Meeting,<br />
popular five-day ECG training courses and regular<br />
Essential Stroke and Neuro MRI courses, RSM’s North<br />
West meeting, the bi-annual Final FRCA exam prep<br />
course, student case presentations, Liverpool Biennial<br />
Artists’ Talks and many more. LMI has even played host<br />
to several paranormal investigation teams who<br />
explored the building for signs of ghostly activity.<br />
Membership<br />
The LMI have negotiated with University of Liverpool<br />
Libraries an improvement to membership benefits<br />
whereby walk in access to their library facilities will be<br />
granted on presentation of an LMI Membership Card,<br />
which members will have received in their Christmas<br />
mailing. The LMI has also extended its links with the<br />
Liverpool Philharmonic with access to exclusive behindthe-scenes<br />
events for members.<br />
The Strategic Management Council has discussed<br />
proposals to share the wealth of clinical experience and<br />
knowledge among the LMI’s membership by setting up<br />
a mentoring programme directed at Year 4 and 5<br />
medical students in the University of Liverpool.<br />
Students would derive significant benefits from<br />
forming relationships with experienced clinicians.<br />
Anyone interested in taking part or wanting more<br />
information on this scheme or should make themselves<br />
known to the admin team.<br />
People<br />
The Strategic Management Council wish to thank all<br />
those who help the LMI run on a day-to-day basis. In<br />
particular this year we would like to thank Mrs Claudia<br />
Harding-Mackean and Mr Terry Wardle for their efforts<br />
with the Sixth Form Conference; Dr Tony Ellis for his<br />
work as Honorary Treasurer; Dr Richard Evans for his<br />
role as Editor of the LMI Transactions & Report, Dr<br />
57
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Andrew Larner for his work as Honorary Librarian and<br />
our regular caterers, ‘Real Food’ for their outstanding<br />
offerings.<br />
The staff of the Institution, who work tirelessly behind<br />
the scenes ensuring meetings, lectures and conferences<br />
run smoothly, are also much appreciated. Karen Alsop<br />
has joined us from Save the Family, and has worked<br />
wonders improving the LMI building, planning the<br />
various projects and since March has been keeping a<br />
firm hand on the LMI’s finances. Sadly, our stalwart<br />
Finance Officer, Jim Penwill, retired this year. We wish<br />
him a wonderful retirement and thank him for his years<br />
of support.<br />
Adrienne, Sue, Joy and the many library volunteers<br />
continue to run a most efficient library and have<br />
recently completed a complete reclassification of the<br />
contents. They also ran the extremely popular and wellpublicised<br />
World War I event over several days that<br />
attracted local and national attention. We look forward<br />
to new interest in the LMI and collaborations as a result<br />
of this project.<br />
Managing the membership and conferences could not<br />
be done without the administration team Audrey,<br />
Lynne, Sam and Sharon. Joyce, who manages the bar,<br />
wishes to retire at the end of the 20<strong>15</strong> session. She has<br />
worked at the LMI for over 20 years and we wish her<br />
well, and thank her for her years of service. We also<br />
thank Tom, who looks after the evening meetings.<br />
Last but not least, the support of members in these<br />
challenging economic times is appreciated now more<br />
than ever, and we love to see members using and<br />
enjoying the building.<br />
The Building<br />
Plans to modernize and develop the building have<br />
continued this year, and it is an exciting time in the<br />
development of the LMI. The Gallery, Oak Study and<br />
Dining Room have been redecorated in tasteful<br />
heritage red and are looking fantastic. The stonework<br />
on the Ionic colonnade at the front of the building has<br />
been cleaned and retouched. The Wi-Fi system has<br />
been upgraded to provide a better service; members<br />
and visitors now need only register once and the system<br />
will remember them next time.<br />
The antique grandfather clock fondly known as the<br />
‘Old Doctor’ was featured on the second of two BBC<br />
Antiques Roadshow episodes filmed out of Liverpool<br />
Metropolitan Cathedral. A link to the programme can<br />
be found on the LMI website for those who missed it!<br />
An eight-week programme to renovate and improve<br />
the Back Corridor outside the Lecture Theatre, and<br />
overhaul the windows in the Council Room and Library<br />
has begun over the summer. The new layout will<br />
provide a new accessible facility, ladies facilities on the<br />
ground floor and a larger facility for men. We expect<br />
this to dramatically improve the appearance and<br />
functionality of this area for members and visitors to<br />
the building. We have made a conscious effort to<br />
choose fittings and décor commensurate with the<br />
period in which the building was built, and we are<br />
looking forward to seeing the finished result.<br />
The Year Ahead<br />
The incoming President for the 177th Session (20<strong>15</strong>-<br />
2016) is Mr Graham Lamont, and we look forward to<br />
his programme of events, meanwhile Mr Derek Machin<br />
has been nominated for President of the 178th Session.<br />
Following the modest success of the initial Trainee<br />
Programme, a new LMI Junior Doctors Committee has<br />
been set up to to facilitate long term input from the<br />
trainees and students themselves and provide a regular<br />
programme of meetings and events to interest and<br />
support junior doctors and medical students.<br />
Representatives from each of the Hospital Trusts have<br />
agreed to sit on the committee to suggest ideas for<br />
appropriate and interesting topics and speakers. They<br />
will then bring the message back to their own hospitals<br />
and grand rounds, to help LMI engage better with<br />
junior doctors and promote these evenings. The<br />
programme will begin in August, with an evening for<br />
the new F1 doctors about to begin their first preregistration<br />
year.<br />
The next stage of material redevelopment, for which<br />
proposals have already been received from architects,<br />
involves the ground floor of the 1960s’ extension of the<br />
LMI (the reception area and ‘Reading Room’). The brief<br />
is to maximise the space and flexibility the LMI can<br />
provide for exhibitions and events, whilst providing a<br />
more welcoming entrance befitting the age and<br />
heritage of the building. Once more formal plans have<br />
been shortlisted these concepts will be circulated to<br />
members. We hope members can join us in looking<br />
forward to an exciting future.<br />
Mr Austin McCormick<br />
Honorary Secretary<br />
58
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Report of the Honorary Librarian 2014-<strong>15</strong><br />
The highlight of the 2014-<strong>15</strong> session was the World<br />
War I commemoration event, Then and Now: Military<br />
Medicine 1914-2014, in partnership between the LMI<br />
and 208 Field Hospital (Liverpool) and in association<br />
with the Liverpool Medical History Society, which took<br />
place on 2-4 October. It featured a wide range of<br />
displays, including a 1914 trench re-created in the LMI<br />
car park, a 1914 Casualty Clearing station and a 2014<br />
Field Dressing station, lectures on military medicine by<br />
Army medical personnel, and opportunities to learn<br />
about Liverpool doctors who contributed to the War<br />
effort including Noel Godfrey Chavasse, Frances Ivens,<br />
Mary Birrell Davies and Sir Robert Jones. Much further<br />
information is accessible on the LMI website at:<br />
http://www.lmi.org.uk/libraryandarchives/recentexhibi<br />
tions/thenandnowww1exhib.aspx. The library reclassification<br />
project is now complete with over 12000<br />
books barcoded. The next stage is to move the books<br />
to their new locations in subject, and not author,<br />
order. Books published between 1900 and the present<br />
day will be housed in the Library and Library Gallery.<br />
Small sub projects will be started presently. There are<br />
collections in the President’s Room and in the Archive<br />
basement ready to be classified and catalogued.<br />
The p<strong>amp</strong>hlet records in the electronic Library<br />
Management System have been checked, and<br />
corrections and many additions made. It is hoped that<br />
in due course these p<strong>amp</strong>hlets might be digitised.<br />
All LMI members should now have an LMI<br />
membership card which will facilitate access to the<br />
University of Liverpool libraries.<br />
The Library fabric has been enhanced with repainting<br />
of the Gallery, and revision of the blurbs<br />
accompanying each painting is in progress.<br />
A number of other events have taken place or are<br />
scheduled to take place in the Library this year. The<br />
annual History of Medicine Prize Evening, now a<br />
fixture in the LMI calendar, was held in November<br />
2014 and once again proved a popular and enjoyable<br />
event.<br />
Liverpool Medical Institution Historic Building Tours,<br />
run by Library staff, have proved to be immensely<br />
popular. Compared to the same period in 2014, the<br />
number of tours has increased by 500%. Tours are<br />
booked by a wide range of local organisations from<br />
U3A groups to University of Liverpool.<br />
On Friday <strong>15</strong> May, selected rooms in the building were<br />
opened for LightNight. This is Liverpool's one-night<br />
arts and culture festival taking place annually in May,<br />
www.lightnightliverpool.co.uk. There was a fabulous<br />
turnout with the rooms packed with visitors between<br />
4 and 8pm. On offer were a fruit quiz, historic<br />
instruments, and modern doctors’ training aids. Many<br />
thanks are due to Christopher Mayers from the Royal<br />
College of Physicians for his support, and training us<br />
to use the equipment.<br />
On Friday 4 September the building will open again<br />
in the evening for members of the public, on this<br />
occasion it will be for Maggie’s Culture Crawl<br />
www.maggiescentres.org/culturecrawl which will take<br />
a night-time 10k adventure around Liverpool's most<br />
fabulous sights (that’s the LMI amongst others!) and<br />
help the centre support more people with cancer in<br />
Merseyside.<br />
To continue working towards becoming an accredited<br />
museum, several items have been loaned to<br />
exhibitions in Liverpool. Amputation instruments and<br />
books circa 1865 are currently on loan to the<br />
University of Liverpool for their ‘Life and Limb’<br />
exhibition in Abercromby Square. An 18th Century<br />
microscope and several 17th Century books and<br />
p<strong>amp</strong>hlets are on loan to the University for their<br />
‘Micrographia’ exhibition, which opened on 12 May<br />
in the Victoria Gallery.<br />
In October 20<strong>15</strong> an exhibition will open in the Victoria<br />
Gallery to showcase Independent Libraries in Liverpool<br />
between 1779 and 1837. This will feature the<br />
Liverpool Medical Institution Library and the<br />
Athenaeum Library, the two oldest, still surviving,<br />
independent libraries in Liverpool. The LMI library is<br />
the oldest, but both organisations share founding<br />
members. Special items from both collections will be<br />
on display until May 2016. This will include an LMI<br />
clock, ‘The Old Doctor’ which was featured on BBC TV<br />
Antiques Roadshow on 29 March 20<strong>15</strong>.<br />
Dr Andrew Larner<br />
Honorary Librarian<br />
59
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Obituaries<br />
Dr MURIEL ANDREWS<br />
Senior Medical Officer<br />
Dr Andrews was educated<br />
at Wigan High School for<br />
Girls and qualified from<br />
Liverpool University in 1943.<br />
From the outset she pursued<br />
a career in child health,<br />
initially at the Stanley<br />
Hospital in Liverpool under<br />
Miss Nicholson, who kept<br />
strict order! Subsequently<br />
she worked at Heswall<br />
Hospital and at Booth Hall Children's Hospital in<br />
Manchester. She obtained the Diploma in Child Health<br />
in 1946 and the Diploma in Public Health in 1947. Dr<br />
Mary Sheridan, a pioneer of child development, was a<br />
great source of inspiration.<br />
Subsequently Muriel became a school medical officer<br />
in Liverpool. She grew to know families very well and<br />
helped many to overcome the difficulties of adjusting<br />
to fathers and sons returning from the war. There<br />
were many health and social problems to deal with. If<br />
parents failed to bring their children to appointments,<br />
Muriel and her team of nurses would go out and find<br />
them!<br />
During her time as Senior Clinical Medical Officer,<br />
Muriel became a founder member of the Faculty of<br />
Community Medicine in 1972. She worked with Dr<br />
Pinkerton and Dr Leveson, continuing to pursue her<br />
interest in child development.<br />
Fulwood Court, where she was cared for to the end<br />
with great affection and devotion. She passed away on<br />
19th November 2014.<br />
Muriel Andrews, MB ChB Liverpool 1943, DCH England<br />
1946, DPH Manchester 1947, Residential Medical<br />
Officer, Monsall Hospital Manchester, House Officer,<br />
Surgery, Stanley Hospital, Liverpool.<br />
Dr Ruth Hussey<br />
Dr ELEANOR MAUD HAMILTON (nee PEARSON)<br />
Research Fellow, University of Liverpool<br />
and<br />
Mr CHARLES JOHN KENNETH HAMILTON (Died: 1980)<br />
Consultant Gynaecologist<br />
Eleanor & John on their engagement<br />
She retired in 1979 and became a school governor, a<br />
member of the Committee for the Blind, and an<br />
(honorary) member of the Association for Retired<br />
Head Teachers! She also continued to support the<br />
Medical Women's Federation, Liverpool Medical<br />
Institution, the Soroptimists and the British Federation<br />
of University Women. She became a skilled<br />
embroiderer, and pursued her interests in walking and<br />
natural history.<br />
Muriel was closely involved in family life and derived<br />
much pleasure in retirement from her role as a greataunt,<br />
keeping her skills in developmental assessment<br />
well-honed on the next generation.<br />
Her final years were clouded by increasing physical and<br />
mental frailty and were spent in residential care at<br />
At the home they had designed and built<br />
On December 19th 1938, Amy Buller Warden of<br />
University Hall Liverpool wrote to Eleanor:<br />
“You already know what great gifts I feel you have to<br />
bring to your job and your home……..”<br />
On July 26th 1916, Eleanor was born to William and<br />
60
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Norah Pearson. WWI raged. Her grandparents Moss<br />
lost a son in battle so Eleanor’s arrival was a great<br />
comfort. By her own admission Eleanor had undivided<br />
attention. She repaid this privilege throughout her<br />
life. Eleanor was proud of her descent from William<br />
Moss, the Loughborough contractor who built the<br />
Adelphi Hotel and the entrance to the Mersey Tunnel.<br />
As an infant, her grandmother, Mayor of<br />
Loughborough, introduced her to the responsibility of<br />
duty towards others. Later in life she worked tirelessly<br />
for others - The Medical Benevolent Society, The<br />
Marriage Guidance Council, Abbeyfield and as a<br />
Magistrate on the Liverpool Bench. She sponsored a<br />
child in Calcutta.<br />
As a child Eleanor weekly boarded at the Herbert<br />
Strutt School in Belper. She left aged 16 with a place to<br />
study Medicine at Liverpool University. As Miss Butler’s<br />
protégée, Eleanor dined at High Table where she<br />
conversed with Jung, Adler, Henry Lunn and many<br />
others, helping her explore ideas and listen to others.<br />
She qualified in 1938 as a doctor and became a lecturer<br />
in histology. When she met John Hamilton, he was a<br />
well qualified young doctor. Colleagues noted that<br />
something was going on when he lent his precious<br />
Lagonda to an attractive young student named<br />
Eleanor. Soon their engagement was a Leicester<br />
Mercury banner headline reading ‘Lough’bro Student<br />
Medical Romance’. The couple married on 2nd<br />
September 1939.<br />
Next day WWII began and they spent their honeymoon<br />
in the Palace Hotel Buxton filling sandbags. John<br />
Hamilton was 1 of 3 gynaecologists and obstetricians<br />
covering Merseyside.<br />
His nightly call-outs to burning buildings on the dock<br />
road left Eleanor holding their babies and putting her<br />
own brilliant career on hold. The introduction of the<br />
electron microscope also made a return to her subject<br />
very difficult.<br />
John and Eleanor’s great joint creation was a modern<br />
house overlooking the sea in Blundellsands designed<br />
by the award winning architect Jo Parker. It featured<br />
in Ideal Home magazine and was THE ideal home in<br />
which to enjoy their nine grandchildren.<br />
As a teenager, Eleanor looped the loop in a friend’s<br />
Tiger Moth. She won two Henry Lunn bursaries, one to<br />
the Farne Islands, the second an Hellenic Cruise where<br />
she mixed with the best scholars of the age and saw<br />
the classical sites. This academic travel established her<br />
habit of research and travel diaries. Travel with John<br />
when he was an external examiner took her to many<br />
other universities. Family holidays were educational<br />
and fun. As pioneers with the Caravan Club they<br />
explored castles, houses and landscapes with their four<br />
children. In her widowhood Eleanor travelled with her<br />
great friend Freda Adams on interfaith group visits to<br />
China, India, The Holy Land and Iona. To the end she<br />
thanked the surgeon Robin Downie for his skills and<br />
facilitating – in her own words “30 years’ travel<br />
without a bag”.<br />
Her passion for all things Liverpool, which she shared<br />
with her children and grandchildren, ranged from<br />
music at the Phil to football at Anfield. Her ashes are<br />
to be buried next to John in the family grave in<br />
Liverpool.<br />
Eleanor Hamilton, MB ChB Liverpool 1939, MRCS<br />
England, LRCP London 1939, Holt Research Fellow,<br />
University of Liverpool 1939-40.<br />
Charles John Kenneth Hamilton. Qualified MRCS, LRCP<br />
1930, B Chir Cambridge 1931, MB 1933, FRCS Ed 1934,<br />
MRCOG 1937, FRCOG 1948. Gynaecological Surgeon,<br />
Walton Hospital. Senior Consultant Surgeon Liverpool<br />
Maternity Hospital and Women’s Hospital. Clinical<br />
Lecturer in Obstetrics and Gynaecology, University of<br />
Liverpool. Life Member LMI 1975. Died 1980.<br />
Dr JOE LAVELLE<br />
General Practitioner<br />
Elspeth Hamilton<br />
Dr Joseph Owen Lavelle<br />
("Joe") was born in Liverpool<br />
in 1931 and educated at St<br />
Francis Xavier's College. He<br />
represented the college at<br />
football and excelled<br />
academically, his academic<br />
prowess culminating in the<br />
award of a place at Oxford<br />
University to read English.<br />
However, he had already<br />
decided upon a career in medicine and declined the<br />
place at Oxford in favor of a place at Liverpool Medical<br />
School, which he entered as a first year student in<br />
1951. Throughout his undergraduate years he was a<br />
keen supporter of Medical Students Society, his loyalty<br />
being rewarded by his election to the post of treasurer<br />
in 1955.<br />
61
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Following graduation in 1957, Joe did his house jobs<br />
at Broadgreen Hospital where he met a ward sister,<br />
Cecily Ryan, who later became his wife. On completing<br />
his pre-registration year, he was conscripted into the<br />
RAMC in the rank of captain and spent the next two<br />
years at Catterick Garrison, despite a request for a<br />
posting overseas.<br />
After leaving the army, he undertook training for<br />
general practice before joining a family practice in<br />
Upton, Wirral in 1963. There he stayed until 1968 when<br />
he went into partnership with Margaret Baron in<br />
Rutherford Road, Liverpool 18, where he remained in<br />
practice until his retirement in 1991, by which time Dr<br />
Peter Griffiths and Dr Barbara Gaze had joined him. In<br />
addition to his family practice, Joe was, for many years,<br />
medical officer for Liverpool University. An Honorary<br />
Life Member of Liverpool Medical Institution, he was<br />
also a stalwart member of the Innominate Club.<br />
Gifted with great clinical skills and deeply<br />
compassionate, he was admired and greatly respected<br />
by colleagues and patients alike, many of whom<br />
attended his funeral service at Bishop Eton Church,<br />
Liverpool, in April 20<strong>15</strong>.<br />
Joe's greatest interests, apart from his family and<br />
medicine, were music, literature, sport and travel - in<br />
particular, being conversant in German and French,<br />
European travel - which he greatly enjoyed with Cecily<br />
and with Sheila, his second wife. His main sporting<br />
interests included Everton Football Club, and Woolton<br />
Golf Club, of which he was a past president and past<br />
captain, scoring a hole-in-one during his captaincy.<br />
Predeceased by Cecily and by his daughter, Emma, Joe<br />
Lavelle is survived by Sheila, his sons, Martin and Peter,<br />
his stepsons, Jefferson and Jonathan and by his five<br />
grandchildren.<br />
Joseph Owen Lavelle. Born 9th November 1931.<br />
Qualified MB ChB Liverpool 1957. General Practitioner,<br />
Liverpool. Died 7th April 20<strong>15</strong>.<br />
Jim Burns<br />
Dr CHARLES STEWART McKENDRICK<br />
Consultant Physician<br />
Charles Stewart McKendrick<br />
was born in Warkworth,<br />
Northumbria, on 21st October<br />
1919. His father was a banker<br />
and his mother a milliner; he<br />
was the first of the family,<br />
after education at the Quaker<br />
Bootham School in York, to<br />
study medicine.<br />
His pre-clinical training was undertaken at St. John’s<br />
College, Cambridge and, bucking the custom for<br />
undertaking clinical training in London, he completed<br />
his training and graduation in medicine in Liverpool,<br />
in 1941. His activities at Cambridge were not confined<br />
to the academic; outraged at the permission given for<br />
a lecture at his College by Sir Oswald Mosley of the<br />
British Union of Fascists, he mustered the rugby team<br />
to bounce Mosley’s Rolls Royce into the River Cam, an<br />
endeavor apparently demanding all of their combined<br />
strength.<br />
Shortly after completing his house jobs, he enlisted in<br />
the Royal Army Medical Corps, and was later intimately<br />
involved with major battlefield surgery on the beaches<br />
of the D-Day landings in 1944, given a scalpel and an<br />
operating tent next to the senior surgeon, and ordered<br />
to get on with it. He was subsequently with the 11th<br />
Armored Division during the relief of the Bergen-<br />
Belsen concentration c<strong>amp</strong> on <strong>15</strong>th April 1945.<br />
He forever found the horror of finding 60,000<br />
emaciated prisoners in desperate need of medical<br />
attention difficult to describe. Attaining the rank of<br />
Major during the war, he later remained in the<br />
Territorial Army, retiring from the reserve force as<br />
Lieutenant-Colonel.<br />
Dr McKendrick became Consultant Cardiologist to the<br />
then Regional Cardiac Centre at Sefton General<br />
Hospital, and later, the father of modern cardiology in<br />
the City. With the realisation, in the 1960s, that the<br />
outcomes and survival of patients with acute<br />
myocardial infarction was improved by managing their<br />
care in specialised facilities staffed by specifically<br />
trained and skilled staff, he set up one of the first<br />
purpose-designed coronary care units in England.<br />
Allied to this development, the introduction in 1960 of<br />
coronary angiography by Mason Sones at the<br />
62
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Cleveland Clinic led to the establishment of cardiac<br />
catheter laboratories in the UK. Under Charles<br />
McKendrick’s foresight and leadership, Liverpool was<br />
again in the vanguard of specialised cardiac<br />
investigation, a development taken forward to the<br />
highest standards of the day by Norman Coulshed, Ellis<br />
Epstein and, later, Sandy Harley.<br />
His third key innovation was the introduction and<br />
development of the cardiac pacemaker service, initially<br />
with the cardiothoracic surgeon Ken Waddington and<br />
general surgeon Wing Turner, evolving into an almost<br />
exclusively cardiology based service from 1976 with the<br />
appointment of Richard Charles as his Senior Registrar.<br />
Again, it was Charles McKendrick’s leadership in<br />
establishing a secure and appropriately growing<br />
budget for implantable cardiac devices which catalysed<br />
the growth of this service in Liverpool into one of the<br />
largest implanting centres in Europe under Richard<br />
Charles, who succeeded him on his retirement from<br />
clinical practice in 1981.<br />
Despite his great strength of character and leadership,<br />
he also fell prey to human frailty, descending into a<br />
period of destructive alcoholism in the 1970s, an<br />
experience which he never sought to conceal. Indeed,<br />
his eventual complete recovery and return to full<br />
clinical duties under the care and support of Alcoholics<br />
Anonymous in many ways defined the rest of his life.<br />
He was completely committed to the 12-step<br />
programme, central to which is the continuous support<br />
of other alcoholics, eventually becoming the national<br />
chairman of AA, whilst remaining faithful to his local<br />
group in Toxteth. He was instrumental in setting up<br />
the Sick Doctors’ Trust, of which he became a Patron.<br />
In 1950 he married Olive Bell, a Paediatrician, and they<br />
were both strong and generous supporters in time and<br />
money to many charities; indeed, in later years he had<br />
to be restrained from donating to every good cause<br />
which came to his door.<br />
In retirement, whilst continuing active support of his<br />
favored charities, he relaxed with his great love of<br />
painting, initially in sketching and water colours, but<br />
later becoming a master of oil painting. He and his<br />
wife, Olive, his muse and indefatigable support<br />
throughout his life, were unfailingly hospitable and<br />
joyful company to all visitors. He is survived by their<br />
four children, Jenny, Posy, Jamie and Helen.<br />
Charles McKenrick, MA, MD (Cambridge & Liverpool).<br />
JP: Consultant Physician (Cardiology) Mossley Hill<br />
Hospital. Consultant Physician Sefton General Hospital,<br />
Liverpool. Died in Liverpool aged 94.<br />
Richard Charles<br />
Helen McKendrick<br />
MR HUW OWEN THOMAS<br />
Consultant Orthopedic Surgeon<br />
Huw Owen Thomas was born<br />
in 1941 in North Wales. He<br />
was an only child, born into a<br />
medical family spanning four<br />
generations. He had wanted<br />
to become a vet, but as his A<br />
level results were not<br />
sufficiently good, he found<br />
himself studying medicine<br />
instead, qualifying at the<br />
Welsh National School of<br />
Medicine in Cardiff in 1966. After house jobs in Cardiff<br />
and Rhyl, Huw returned to Liverpool where he had<br />
been brought up.<br />
His father Goronwy Thomas (President of the LMI<br />
1969) was a Consultant Orthopedic Surgeon at the<br />
David Lewis Northern Hospital.<br />
Huw shared his name with Hugh Owen Thomas, the<br />
Anglesey bonesetter and inventor of the Thomas<br />
splint, although Huw was proud to have the Welsh<br />
(and he would say the correct) spelling. He<br />
contributed some memorabilia of Hugh Owen Thomas<br />
to the LMI library, which he and his father had<br />
collected. Taking up the mantle of both his namesake<br />
and his father, Huw trained in orthopedic surgery in<br />
Liverpool, Gobowen and also at Wrightington Hospital<br />
under Professor Sir John Charnley.<br />
He had a very close and harmonious relationship with<br />
his father, working at one time as a registrar on his<br />
father’s firm, to the awe of many of his contemporary<br />
trainees. Whilst undergoing postgraduate training, he<br />
was proud to serve as a Captain in the RAMC.<br />
Huw was appointed as a Consultant Orthopedic<br />
Surgeon in Wirral, and prided himself on being a<br />
general orthopedic surgeon in an era when super<br />
specialisation was becoming the norm. He left the NHS<br />
at the age of 56 in 1997, thereafter concentrating on<br />
his medico-legal practice and tribunal work, retiring in<br />
2007.<br />
Huw’s hobbies were many. He enjoyed art,<br />
architecture, steam railways, fishing and shooting. His<br />
greatest love was classical music, about which his<br />
63
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
knowledge was encyclopedic. It amazed many that he<br />
could hear a few bars of a piano piece on the radio and<br />
would have no trouble in correctly identifying the<br />
pianist. As a student in Cardiff, Huw thought nothing<br />
of driving from Cardiff to Liverpool in his Austin Seven,<br />
to attend a concert given by the Royal Liverpool<br />
Philharmonic Orchestra, only to drive back to Cardiff<br />
the same night. Indeed he had a passion for all things<br />
beautiful, be it in music, art or buildings, and honored<br />
and admired those who could produce such wonderful<br />
works. Huw was not a pub or club man, but was<br />
happiest spending his time with his family, to which he<br />
was devoted. Sadly his last years were dogged by<br />
several health problems, which he bore with great<br />
fortitude. He leaves his wife Judith, also a doctor, two<br />
sons and a granddaughter.<br />
Huw Owen Thomas. Born Holywell, North Wales 11th<br />
May 1941. Qualified Cardiff 1966, FRCS Edinburgh<br />
1971 , FRCS England 1972, MChOrth Liverpool 1973.<br />
Consultant Orthopedic Surgeon Victoria Central<br />
Hospital (later Wirral University Hospital NHS Trust).<br />
Died 4th January 20<strong>15</strong>.<br />
Judith Thomas<br />
Dr CHRISTOPHER MICHAEL WRAGG<br />
General Practitioner & Emergency Medical Doctor<br />
When we stepped from the<br />
packed chapel to the flower<br />
display after Chris Wragg’s<br />
funeral, the crematorium rang<br />
to the sound of laughter, as<br />
we swapped anecdotes about<br />
this iconic Yorkshireman.<br />
He had spent half his career in A&E – first in<br />
Merseyside, then in Scunthorpe – and undoubtedly the<br />
A&E stories were the best. Singing ‘The Laughing<br />
Policeman’ over the tannoy during the Toxteth riots;<br />
poling himself down a corridor on a trolley, singing<br />
‘Just One Cornetto’; and taking advantage of an empty<br />
waiting room, (it was a long time ago), to sit and<br />
pretend to be a patient, then storm out, inviting the<br />
new arrivals to follow. He even once took a timewaster<br />
out to the ‘Accident & Emergency’ sign on the<br />
door, and then said, “Have you had an accident?” ...<br />
“No...” “Are you an emergency?” ... “No...” “Well naff<br />
off!” Utterly unacceptable behaviour, of course, even<br />
by those days’ standards, but this gentle, kind and<br />
generous joker still felt strongly the heritage of an<br />
uncompromising Yorkshire Methodist upbringing.<br />
At Medical School in the the early seventies, his<br />
singing, impromptu performances and comic acting<br />
were legendary. He was the only man in Whiston<br />
Hospital’s history to take a tuba on the ward round as<br />
a houseman. Despite being the life and soul of every<br />
party (usually coming in fancy dress or one of his many<br />
Victorian outfits), he never drank alcohol. Indeed, he<br />
was probably the only Liverpool Medic rugby player<br />
who did not like it. But he did like rugby. He was the<br />
‘hard man’ of the Medics team, (although not always<br />
able to carry out the role effectively, as he would still<br />
be getting up from the collapse of one scrum, when<br />
another was being whistled for).<br />
He went on to become a passionate rugby league<br />
supporter, even playing the odd game for Huyton RLFC<br />
– one of several teams for which he served as club<br />
doctor (on many occasions, it should be noted, his<br />
name appeared on the Huyton team list, even though<br />
he was in the dug-out with the sponge. The club then<br />
used one of their many ‘Chris Wragg’ ringers to try<br />
desperately, at least once in a season, to win a game).<br />
Later, in his eight years as doctor at Scunthorpe United<br />
FC, these wily tricks had become just a folk memory in<br />
Rugby League.<br />
He was potty about history, especially medical and<br />
military history, and began to collect paraphernalia<br />
and memorabilia even as a student. Want to borrow a<br />
top hat? Medals? Just about anything Victorian?<br />
Ancient text books? An apothecary’s wax seal? Pictures<br />
or photos of old scenes? Whatever – Wraggy was your<br />
man. By the time of his death last month from liver<br />
cancer, (ironically), he was a member of sixteen<br />
learned medical history societies, and had filled not<br />
just every room in his house and garage, but a spare<br />
couple of garages and a full sea-going container with<br />
his E-bay purchases.<br />
In the early eighties, he settled in Kirton-in-Lindsey,<br />
initially as a GP and subsequently working in<br />
Scunthorpe A&E. He bore his diabetes, blindness, and<br />
final illness with his unique mix of joviality, spirituality<br />
and resignation. I suppose that I should finish by saying<br />
that he will be sorely missed, and of course, by those<br />
closest to him he will. But for many, both in the<br />
profession and outside, the memory of Wraggy will<br />
live on in joy – even as we hope he is now doing.<br />
Christopher Michael Wragg, DTM&H 1976, DRCOG,<br />
DCH. Died 20th September 2014.<br />
Lawrence Wood<br />
64
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Members Joined Since Last Transactions<br />
Badescu, I C<br />
Barker, T<br />
Crowley, T S<br />
Fraser, M<br />
Heseltine, J<br />
Kasbekar, S<br />
Patterson, J (reinstated)<br />
Rai, J<br />
Affiliates Joined Since Last Transactions<br />
Curtis-Summers, S<br />
Drury, K<br />
Offices of Distinction, Awards/Honours<br />
Dr Elizabeth Margaret Embray Poskitt<br />
Dr Elizabeth Poskitt, member of the LMI since 1977, helped to found the Association for the Study of Obesity,<br />
spent some time in Africa and was a Lib Dem Councillor.<br />
She has been elected Mayor of Woodstock, Oxfordshire, at the age of 75.<br />
Mr Roy Farquharson<br />
Mr Roy Farquharson is now Chair elect (20<strong>15</strong>-2017) of the European Society of Human Reproduction and<br />
Embryology.<br />
65
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Liverpool Medical Institution<br />
Consolidated Statement of Financial Activities and Balance Sheet<br />
for the Year Ended 31st December 2014<br />
SMC regrets to announce that due to the retirement of the Finance Officer, Mr Jim Penwill, in the final quarter<br />
of last year due to illness, the final accounts for 2014 have not yet been audited and approved, and could not<br />
therefore be presented for adoption by the membership at the AGM in April 20<strong>15</strong>.<br />
Members can however rest assured that the situation is in hand. Succession plans are well in place, and Mrs<br />
Karen Alsop has been appointed by SMC as Finance Manager, in addition to her current project work for the LMI.<br />
The accounts will be completed over the summer well in advance of the regulators’ submission deadlines.<br />
Members present at the AGM in April agreed that the meeting be adjourned and re-convened in October 20<strong>15</strong><br />
to complete the presentation of accounts to the membership. We hope you can join us all then. The date of the<br />
resumed AGM will be announced on the LMI’s programme, included with this publication.<br />
We wish to thank Mr Penwill for his hard work, professionalism, honesty and integrity as Finance Officer during<br />
the past 11 years, and offer congratulations on a job well done and a retirement well deserved.<br />
A Ellis<br />
Hon Treasurer<br />
66
Presidents of the Liverpool Medical Institution<br />
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
1840-65 J Dawson 1956 B McFarland<br />
1866 J Vose 1957 M E Thomas<br />
1867 J McNaught 1958 A M Reid MC TD<br />
1870 E R Bickersteth 1959 E N Chamberlain<br />
1872 J Cameron 1960 P Hawe TD<br />
1874 W McShane 1961 P H Whitaker<br />
1876 J M Turnbull 1962 R W Brookfield<br />
1878 A T H Waters 1963 I Forshall<br />
1880 R Harrison 1964 A W Downie FRS<br />
1882 T S Walker 1965 J C Ross<br />
1884 R Gee 1966 T N A Jeffcoate (Kt)<br />
1886 J B Nevins 1967 J W Cheetham OBE<br />
1888 W Carter 1968 R R Edwards<br />
1890 W M Banks (Kt) 1969 G Thomas<br />
1892 T R Glynn 1970 C A Clarke KBE FRS<br />
1894 C Puzey 1971 A S Kerr<br />
1896 R Caton 1972 J D Hay<br />
1898 W M C<strong>amp</strong>bell 1973 T Seager<br />
1900 E A Browne 1974 T C Gray CBE<br />
1902 R Parker 1975 I Leveson<br />
1904 J Barr (Kt) 1976 J A Shepherd VRD<br />
1906 F T Paul 1977 D C Watson MC<br />
1908 T H Bickerton 1978 C M Ogilvie<br />
1910 T R Bradshaw 1979 J H Smellie<br />
1912 R Jones (Bt, 1926) 1980 E W Parry<br />
1914 E W Hope 1981 J H E Carmichael<br />
1916 C J MacAlister TD 1982 E Rees<br />
1918 W T Thomas 1983 N O K Gibbon<br />
1920 J E Gemmell 1984 D N Menzies<br />
1922 J H Abram 1985 R B McConnell TD<br />
1924 G P Newbolt CBE (d 9th March) 1986 P M Stell<br />
1924 R C Dun 1987 I K Brown (d 28.3.88)<br />
1926 J C M Given 1987 P M Stell (from 20.4.88)<br />
1928 J Hay 1988 R Shields (Kt)<br />
1930 K W Monsarrat TD 1989 P M E Drury<br />
1931 W Blair-Bell 1990 A T Carty<br />
1932 R E Kelly CB (Kt, 1939) 1991 C C Evans<br />
1933 H R Hurter 1992 W M Mackean RD<br />
1934 J M Bligh 1993 H Carty<br />
1935 C O Stallybrass 1994 M C L’E Orme<br />
1936 G C E Simpson OBE TD 1995 A Zsigmond<br />
1937 R E Kelly CB (Kt, 1939) 1996 R E Cudmore<br />
1938 E G Bark 1997 R A Sells<br />
1939 W Johnson MC 1998 S Evans<br />
1940 A L Robinson 1999 R Walker<br />
1941 O H Williams 2000 K Parsons<br />
1942 R G Wills 2001 J Earis<br />
1943 E I Spriggs KCVO 2002 C A Hart<br />
1944 R S Taylor 2003 J M Rhodes<br />
1945 R Kennon MC 2004 A C Swift<br />
1946 G F R Smith TD 2005 P M A Calverley<br />
1947 H Wallace-Jones 2006 R G Farquharson<br />
1948 T P McMurray CBE 2007 P D O Davies<br />
1949 C Wells CBE 2008 G V Gill<br />
1950 D Johnston 2009 W Taylor<br />
1951 R Coope 2010 P Dangerfield<br />
1952 N B Capon 2011 I Gilmore (Kt)<br />
1953 J B Oldham VRD QHS CBE 2012 R E Franks<br />
1954 H Cohen CH (Kt, Baron 1956) 2013 L de Cossart CBE<br />
1955 R J Minnitt 2014 M S McCormick<br />
67
LMI Transactions and Report 2014 - 20<strong>15</strong><br />
Charitable Donations<br />
GIFT AID<br />
This is the most popular form of tax-efficient giving. Where a donation is made under this scheme the LMI can<br />
reclaim income tax at the basic rate (currently 20%) from HMRC i.e. LMI can reclaim a refund amounting to 25%<br />
of the basic donation. If the donor pays income tax at a higher rate than 20% the donor can reclaim, from the<br />
HMRC, the difference between their marginal rate of tax (40% or higher) and the basic rate when they or their<br />
accountant prepares their annual return.<br />
Individuals are required to complete a Gift Aid Declaration Form, copies of which are available from the LMI<br />
Administration Department.<br />
There is a strictly enforced scale of benefits that the LMI can give to donors without impairing the LMI’s right to<br />
the benefits of the Gift Aid legislation or its charitable status. Subscriptions and charges for attending social or<br />
technical meetings are subject to this scale (e.g. 2.5% of a gift up to £100). However these payments may be<br />
deductible under the individual’s personal tax regime.<br />
GIFT AID SMALL DONATIONS SCHEME<br />
This scheme was set up in 2013 to enable eligible charities to make a claim under the Gift Aid scheme in respect<br />
of small cash donations of £20 or less from an individual without the donor completing any formal<br />
documentation. An ex<strong>amp</strong>le would be a bucket or similar passed round a group of partygoers to make cash<br />
donations towards a charity. We enquired whether we could implement such a scheme at the LMI by adding a<br />
percentage to the bill for refreshments, however this was refused. It must be a voluntary cash donation, cheques<br />
and credit card contributions are now allowed, of £20 or less collected at the function concerned or by the charity<br />
concerned.<br />
The scheme has possibilities as the LMI entertains many non-paying guests over the year who might be willing<br />
to make a contribution to the LMI towards their evening’s entertainment. It is allowed to give a lapel sticker or<br />
similar to acknowledge the gift.<br />
Companies are not required to deduct tax from their charitable payments, the full amount of the payment is<br />
deducted from the profits of the company in calculating the corporation tax payable.<br />
LIFETIME NON-CASH GIFTS<br />
This includes FTSE shares and securities including AIM shares, units in unit trusts, shares in OEIC companies and<br />
interests in offshore funds. Relief is also available for gifts of UK lands and buildings. In general the amount of<br />
the relief, by deduction from income for tax purposes, is the market value of the gifted assets (i.e. the net benefit<br />
received by the LMI). However certain restrictions were made to this scheme from 2009 so professional advice<br />
should be sought prior to implementing such a scheme.<br />
LEGACIES<br />
Gifts to qualifying charities (i.e. one recognised as such by HMRC which includes the LMI) either outright or to<br />
be held on trust for charitable purposes are exempt from IHT. From April 2012, if 10% or more of the net value<br />
of a person’s estate is left to a qualifying charity the tax due may be paid at a reduced rate of 36% (as opposed<br />
to 40%). The net value of an estate is the sum of all the assets after deducting any debts, liabilities, relief,<br />
exemptions and the IHT nil rate band. The application of this reduced rate depends on the asset components in<br />
the estate and the circulation is best left to a qualified adviser.<br />
For more information, please contact Karen Alsop, Finance Officer.<br />
68
LMI Conference<br />
Centre<br />
An exceptional venue at exceptional value<br />
The LMI offers a relaxed and professional setting for<br />
meetings, away/training days, formal/informal dinner parties and<br />
receptions.<br />
• Magnificent Grade II* Listed venue<br />
• Centrally located in the Hope Street quarter and<br />
University precinct, opposite the Metropolitan Cathedral<br />
• Dedicated conference team to meet your needs<br />
• Lecture Theatre seating up to 120<br />
• Three seminar rooms seating 30-40<br />
• Meeting room seating 8<br />
• Videoconference facilities and audio visual equipment<br />
available in Lecture Theatre and Seminar Rooms<br />
• Dining Room seats 30 – extends to 90<br />
• Event catering for 120<br />
• Licensed bar<br />
• Exhibition and display areas<br />
• Fully accessible<br />
• Free WiFi throughout the building<br />
Please contact LMI Conference Office on<br />
0<strong>15</strong>1 709 9125 ext 2 or email admin@lmi.org.uk<br />
A Meetings Industry Accredited venue