Management of acute exacerbation of ASTHMA in children
Management of acute exacerbation of ASTHMA in children
Management of acute exacerbation of ASTHMA in children
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
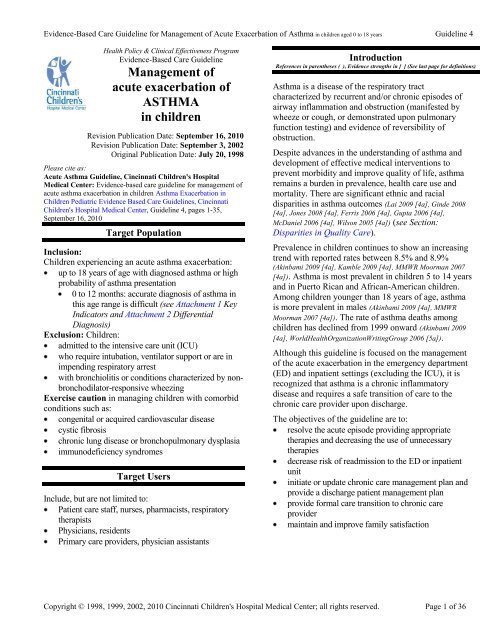
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Health Policy & Cl<strong>in</strong>ical Effectiveness Program<br />
Evidence-Based Care Guidel<strong>in</strong>e<br />
<strong>Management</strong> <strong>of</strong><br />
<strong>acute</strong> <strong>exacerbation</strong> <strong>of</strong><br />
<strong>ASTHMA</strong><br />
<strong>in</strong> <strong>children</strong><br />
Revision Publication Date: September 16, 2010<br />
Revision Publication Date: September 3, 2002<br />
Orig<strong>in</strong>al Publication Date: July 20, 1998<br />
Please cite as:<br />
Acute Asthma Guidel<strong>in</strong>e, C<strong>in</strong>c<strong>in</strong>nati Children's Hospital<br />
Medical Center: Evidence-based care guidel<strong>in</strong>e for management <strong>of</strong><br />
<strong>acute</strong> asthma <strong>exacerbation</strong> <strong>in</strong> <strong>children</strong> Asthma Exacerbation <strong>in</strong><br />
Children Pediatric Evidence Based Care Guidel<strong>in</strong>es, C<strong>in</strong>c<strong>in</strong>nati<br />
Children's Hospital Medical Center, Guidel<strong>in</strong>e 4, pages 1-35,<br />
September 16, 2010<br />
Target Population<br />
Inclusion:<br />
Children experienc<strong>in</strong>g an <strong>acute</strong> asthma <strong>exacerbation</strong>:<br />
up to 18 years <strong>of</strong> age with diagnosed asthma or high<br />
probability <strong>of</strong> asthma presentation<br />
0 to 12 months: accurate diagnosis <strong>of</strong> asthma <strong>in</strong><br />
this age range is difficult (see Attachment 1 Key<br />
Indicators and Attachment 2 Differential<br />
Diagnosis)<br />
Exclusion: Children:<br />
admitted to the <strong>in</strong>tensive care unit (ICU)<br />
who require <strong>in</strong>tubation, ventilator support or are <strong>in</strong><br />
impend<strong>in</strong>g respiratory arrest<br />
with bronchiolitis or conditions characterized by non-<br />
bronchodilator-responsive wheez<strong>in</strong>g<br />
Exercise caution <strong>in</strong> manag<strong>in</strong>g <strong>children</strong> with comorbid<br />
conditions such as:<br />
congenital or acquired cardiovascular disease<br />
cystic fibrosis<br />
chronic lung disease or bronchopulmonary dysplasia<br />
immunodeficiency syndromes<br />
Target Users<br />
Include, but are not limited to:<br />
Patient care staff, nurses, pharmacists, respiratory<br />
therapists<br />
Physicians, residents<br />
Primary care providers, physician assistants<br />
9BIntroduction<br />
10BReferences<br />
<strong>in</strong> parentheses ( ), Evidence strengths <strong>in</strong> [ ] (See last page for def<strong>in</strong>itions)<br />
Asthma is a disease <strong>of</strong> the respiratory tract<br />
characterized by recurrent and/or chronic episodes <strong>of</strong><br />
airway <strong>in</strong>flammation and obstruction (manifested by<br />
wheeze or cough, or demonstrated upon pulmonary<br />
function test<strong>in</strong>g) and evidence <strong>of</strong> reversibility <strong>of</strong><br />
obstruction.<br />
Despite advances <strong>in</strong> the understand<strong>in</strong>g <strong>of</strong> asthma and<br />
development <strong>of</strong> effective medical <strong>in</strong>terventions to<br />
prevent morbidity and improve quality <strong>of</strong> life, asthma<br />
rema<strong>in</strong>s a burden <strong>in</strong> prevalence, health care use and<br />
mortality. There are significant ethnic and racial<br />
disparities <strong>in</strong> asthma outcomes (Lai 2009 [4a], G<strong>in</strong>de 2008<br />
[4a], Jones 2008 [4a], Ferris 2006 [4a], Gupta 2006 [4a],<br />
McDaniel 2006 [4a], Wilson 2005 [4a]) (see Section:<br />
Disparities <strong>in</strong> Quality Care).<br />
Prevalence <strong>in</strong> <strong>children</strong> cont<strong>in</strong>ues to show an <strong>in</strong>creas<strong>in</strong>g<br />
trend with reported rates between 8.5% and 8.9%<br />
(Ak<strong>in</strong>bami 2009 [4a], Kamble 2009 [4a], MMWR Moorman 2007<br />
[4a]). Asthma is most prevalent <strong>in</strong> <strong>children</strong> 5 to 14 years<br />
and <strong>in</strong> Puerto Rican and African-American <strong>children</strong>.<br />
Among <strong>children</strong> younger than 18 years <strong>of</strong> age, asthma<br />
is more prevalent <strong>in</strong> males (Ak<strong>in</strong>bami 2009 [4a], MMWR<br />
Moorman 2007 [4a]). The rate <strong>of</strong> asthma deaths among<br />
<strong>children</strong> has decl<strong>in</strong>ed from 1999 onward (Ak<strong>in</strong>bami 2009<br />
[4a], WorldHealthOrganizationWrit<strong>in</strong>gGroup 2006 [5a]).<br />
Although this guidel<strong>in</strong>e is focused on the management<br />
<strong>of</strong> the <strong>acute</strong> <strong>exacerbation</strong> <strong>in</strong> the emergency department<br />
(ED) and <strong>in</strong>patient sett<strong>in</strong>gs (exclud<strong>in</strong>g the ICU), it is<br />
recognized that asthma is a chronic <strong>in</strong>flammatory<br />
disease and requires a safe transition <strong>of</strong> care to the<br />
chronic care provider upon discharge.<br />
The objectives <strong>of</strong> the guidel<strong>in</strong>e are to:<br />
resolve the <strong>acute</strong> episode provid<strong>in</strong>g appropriate<br />
therapies and decreas<strong>in</strong>g the use <strong>of</strong> unnecessary<br />
therapies<br />
decrease risk <strong>of</strong> readmission to the ED or <strong>in</strong>patient<br />
unit<br />
<strong>in</strong>itiate or update chronic care management plan and<br />
provide a discharge patient management plan<br />
provide formal care transition to chronic care<br />
provider<br />
ma<strong>in</strong>ta<strong>in</strong> and improve family satisfaction<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 1 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Guidel<strong>in</strong>e Recommendations<br />
Emergency Department <strong>Management</strong><br />
Initial History and Physical<br />
1. It is recommended that before and as therapy is<br />
<strong>in</strong>itiated, a brief, focused history and physical<br />
exam<strong>in</strong>ation is obta<strong>in</strong>ed, <strong>in</strong>clud<strong>in</strong>g: (LocalConsensus [5],<br />
NAEPP 2007 [5a])<br />
time <strong>of</strong> onset <strong>of</strong> current <strong>exacerbation</strong><br />
current medications and allergies<br />
recent frequent use <strong>of</strong> beta2-agonists<br />
risk factors for severe, uncontrolled disease (e.g.<br />
ED visits, admissions to the hospital and ICU,<br />
and prior <strong>in</strong>tubations)<br />
exposure to asthma triggers<br />
use <strong>of</strong> peak flow with home management<br />
respiratory score.<br />
Note 1: Indications <strong>of</strong> more severe <strong>exacerbation</strong><br />
<strong>in</strong>clude <strong>in</strong>creased anxiety, decreased level <strong>of</strong><br />
consciousness, breathlessness, diffuse wheez<strong>in</strong>g<br />
or absence <strong>of</strong> air movement, <strong>in</strong>creased<br />
respiratory rate, and accessory muscle use or<br />
suprasternal retractions (see Attachment 3<br />
Formal Evaluation <strong>of</strong> Severity <strong>in</strong> the ED,<br />
Attachment 4 ED <strong>Management</strong> <strong>of</strong> Asthma<br />
Exacerbation Algorithm and Recommendation<br />
#13 for severe asthma with respiratory distress).<br />
Note 2: Perform a more detailed history and<br />
physical assessment only after therapy has begun<br />
(NAEPP 2007 [5a], Camargo 2009 [5b]).<br />
Note 3: Patient and parental reports <strong>of</strong><br />
medication use, peak flow values and/or<br />
environmental irritant/allergen exposure <strong>of</strong>ten<br />
present a more favorable description <strong>of</strong> their<br />
disease management than is actual (Dell 2007 [2a],<br />
Kamps 2001 [2b], Bender 2000 [3b], Rich 2000 [3b],<br />
Dozier 2006 [4a], Halterman 2003 [4a], NAEPP 2007<br />
[5a]).<br />
2. It is recommended that repeat assessments <strong>of</strong><br />
response to therapy be conducted, <strong>in</strong>clud<strong>in</strong>g cl<strong>in</strong>ical<br />
exam<strong>in</strong>ation, asthma score, pulse oximetry, and lung<br />
function. In <strong>children</strong> with <strong>exacerbation</strong>, no s<strong>in</strong>gle<br />
assessment tool appears to be best for assess<strong>in</strong>g<br />
severity, treatment monitor<strong>in</strong>g, or predict<strong>in</strong>g<br />
admission; therefore, use <strong>of</strong> one tool may not be<br />
reliable (Sole 1999 [2a], Ribeiro de Andrade 2007 [3a], Keahey<br />
2002 [3a], LocalConsensus [5], SIGN 2008 [5a], NAEPP 2007<br />
[5a]).<br />
3. It is recommended that forced expiratory volume <strong>in</strong> 1<br />
second (FEV1) or peak flow monitor<strong>in</strong>g be attempted<br />
<strong>in</strong> <strong>children</strong> over 5 years with mild to moderate<br />
<strong>exacerbation</strong>s and who currently perform peak flow<br />
with home management (NAEPP 2007 [5a], Camargo 2009<br />
[5b]).<br />
Note: Pulmonary function measurements,<br />
although <strong>of</strong>ten difficult to obta<strong>in</strong> <strong>in</strong> <strong>children</strong>, are<br />
useful <strong>in</strong> assess<strong>in</strong>g the severity <strong>of</strong> an asthma<br />
<strong>exacerbation</strong> (Gorelick 2004 [3a]). If able to obta<strong>in</strong>,<br />
and measurement is < 40% <strong>of</strong> predicted (or<br />
personal best), consider adjunct therapies or<br />
admission (NAEPP 2007 [5a]).<br />
Initial Treatment<br />
Oxygen<br />
4. It is recommended that supplemental oxygen be<br />
started and monitored when the oxygen saturation is<br />
consistently less than 91% and to wean oxygen when<br />
saturation is higher than 94% (Geelhoed 1994 [3a], SIGN<br />
2008 [5a], NAEPP 2007 [5a]).<br />
Short-act<strong>in</strong>g <strong>in</strong>haled beta2-agonists<br />
5. It is recommended that racemic albuterol, an <strong>in</strong>haled<br />
short-act<strong>in</strong>g beta2-agonist (SABA) be adm<strong>in</strong>istered as<br />
the drug <strong>of</strong> choice for rapid reversal <strong>of</strong> airflow<br />
obstruction (NAEPP 2007 [5a], Camargo 2009 [5b]).<br />
Modify therapy based on the early cl<strong>in</strong>ical response<br />
to treatments (SIGN 2008 [5a], NAEPP 2007 [5a], Camargo<br />
2009 [5b]) (see Table 1 Aerosolized Therapies –drugs<br />
and dosage recommendations).<br />
Note: Albuterol treatments given every 10 to 20<br />
m<strong>in</strong>utes for a total <strong>of</strong> 3 doses can be given safely<br />
as <strong>in</strong>itial therapy (LocalConsensus [5], SIGN 2008 [5a],<br />
NAEPP 2007 [5a]).<br />
6. It is recommended that levalbuterol not be rout<strong>in</strong>ely<br />
used <strong>in</strong> the treatment <strong>of</strong> <strong>acute</strong> <strong>exacerbation</strong><br />
(LocalConsensus [5]).<br />
Confusion exists regard<strong>in</strong>g the selection <strong>of</strong> albuterol<br />
versus levalbuterol <strong>in</strong> the treatment <strong>of</strong> <strong>acute</strong> asthma.<br />
Although levalbuterol may prove more efficacious<br />
for some <strong>in</strong>dividuals, there is currently no data on<br />
how to identify these patients (Jalba 2008 [1b]). The<br />
follow<strong>in</strong>g <strong>in</strong>formation may assist <strong>in</strong> the decision to<br />
choose:<br />
Note 1: Efficacy<br />
Levalbuterol has demonstrated comparable<br />
efficacy to albuterol for treatment <strong>of</strong> <strong>acute</strong><br />
<strong>exacerbation</strong>s <strong>in</strong> the ED and <strong>in</strong>patient sett<strong>in</strong>gs<br />
(Gupta 2007 [1b], Ralston 2005 [2a], Carl 2003 [2a],<br />
Andrews 2009 [2b], Hardasmalani 2005 [2b], Qureshi 2005<br />
[3a]). A large double-bl<strong>in</strong>d prospective trial<br />
demonstrated a 10% reduction <strong>in</strong> hospital<br />
admissions with the use <strong>of</strong> levalbuterol (Carl 2003<br />
[2a]) and a retrospective review <strong>of</strong> consecutive<br />
cases demonstrated a 4.5% reduction (Schreck 2005<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 2 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
[4a]). The numbers needed to treat (NNT) with<br />
levalbuterol to prevent one hospital admission <strong>in</strong><br />
theses studies equals 11 and 10 respectively (Carl<br />
2003 [2a], Schreck 2005 [4a]).<br />
Note: 2: Side effect reduction<br />
Difference <strong>in</strong> the reduction <strong>of</strong> adverse events<br />
such as tachycardia, tremor, or <strong>in</strong>crease <strong>in</strong> blood<br />
pressure has not been demonstrated when<br />
equivalent doses <strong>of</strong> levalbuterol and albuterol<br />
have been studied (Andrews 2009 [2b]).<br />
The use <strong>of</strong> racemic albuterol with MDI has been<br />
shown to result <strong>in</strong> lower pulse rates when<br />
compared to nebulizer (Cates 2006 [1a], Mathew 2008<br />
[1b ], Deerojanawong 2005 [2b], SIGN 2008 [5a]). This<br />
may be an important consideration for <strong>children</strong> at<br />
risk for tachycardia <strong>in</strong>clud<strong>in</strong>g <strong>children</strong> with<br />
congenital heart disease or known arrhythmias<br />
(LocalConsensus [5]).<br />
Note 3: Cost<br />
Given that there appears to be no safety<br />
advantage to the use <strong>of</strong> levalbuterol, and the<br />
ability to identify patients who have a differential<br />
treatment response, the greatly <strong>in</strong>creased cost <strong>of</strong><br />
the drug would argue aga<strong>in</strong>st its use <strong>in</strong> the<br />
general population. Discussion <strong>of</strong> the safety and<br />
cost factors with parents may assist <strong>in</strong> the<br />
selection process (LocalConsensus [5]).<br />
Inhalation Delivery Device Selection<br />
Devices used for the delivery <strong>of</strong> bronchodilators and<br />
<strong>in</strong>haled corticosteroids can be equally efficacious.<br />
7. It is recommended that when select<strong>in</strong>g an <strong>in</strong>halation<br />
delivery device that consideration be given to the<br />
follow<strong>in</strong>g: (Dolovich 2005 [1a], Scarfone 2002 [3b])<br />
device/drug availability<br />
patient ability to use the selected device<br />
correctly<br />
device use with multiple medications<br />
cost and reimbursement<br />
drug adm<strong>in</strong>istration time<br />
convenience <strong>in</strong> both outpatient and <strong>in</strong>patient<br />
sett<strong>in</strong>gs<br />
physician and patient preference.<br />
Note 1: In <strong>children</strong> and adolescents with <strong>acute</strong><br />
asthma <strong>exacerbation</strong>, no significant difference<br />
exists for important cl<strong>in</strong>ical responses such as<br />
time to recovery <strong>of</strong> asthma symptoms, repeat<br />
visits, or hospital admissions when medications<br />
are delivered via MDI with Valved Hold<strong>in</strong>g<br />
Chamber (VHC) or nebulizer (Mathew 2008 [1b ],<br />
Delgado 2003 [2a], Jamalvi 2006 [3a], Benito-Fernandez<br />
2004 [3a], Yilmaz 2009 [4a]). With<strong>in</strong> this guidel<strong>in</strong>e, a<br />
spacer is def<strong>in</strong>ed as a VHC or ―delivery‖ device<br />
that has a one-way valve <strong>in</strong>side that prevents the<br />
medic<strong>in</strong>e from escap<strong>in</strong>g once you have pressed<br />
down on the MDI canister (LocalConsensus [5]).<br />
Spacers improve the cl<strong>in</strong>ical effect <strong>of</strong> <strong>in</strong>haled<br />
medications, especially <strong>in</strong> patients unable to use<br />
an MDI properly (Lavor<strong>in</strong>i 2009 [5b]). The use <strong>of</strong><br />
large volume spacers has been recommended for<br />
any <strong>in</strong>haled asthma drug <strong>in</strong> young <strong>children</strong>, and<br />
as a means <strong>of</strong> reduc<strong>in</strong>g systemic bioavailability<br />
<strong>of</strong> <strong>in</strong>haled corticosteroids <strong>in</strong> adults and <strong>children</strong><br />
alike (Newman 2004 [5a]). One study has<br />
demonstrated the percent difference <strong>of</strong> drug<br />
deposition <strong>in</strong>to the lung as 4.9% to 10.9% with<br />
spacer use compared to no spacer. This<br />
represents a range <strong>of</strong> approximately 52% to 87%<br />
<strong>in</strong>crease <strong>in</strong> drug deposition (Vidgren 1987 [4b]).<br />
Note 2: MDIs have been shown to shorten time<br />
to discharge from the ED, to improve pulmonary<br />
function measures, and to result <strong>in</strong> lower pulse<br />
rates when compared to nebulizer (Cates 2006 [1a],<br />
Castro-Rodriguez 2004 [1a], Mathew 2008 [1b ],<br />
Deerojanawong 2005 [2b], Boyd 2005 [3a],<br />
LocalConsensus [5], SIGN 2008 [5a]).<br />
Note 3: The <strong>in</strong>halation route for SABA<br />
adm<strong>in</strong>istration is considered optimal.<br />
Subcutaneous SABAs (ep<strong>in</strong>ephr<strong>in</strong>e, terbutal<strong>in</strong>e)<br />
provide no proven advantage over <strong>in</strong>haled<br />
medication (NAEPP 2007 [5a]). Intravenous SABAs<br />
have not been shown to improve pulmonary<br />
physiology or outcomes compared to <strong>in</strong>haled<br />
routes (Travers 2001 [1a], NAEPP 2007 [5a]).<br />
Inhaled ipratropium bromide<br />
8. It is recommended that <strong>in</strong>haled ipratropium be added<br />
to SABA and corticosteroid therapies for <strong>children</strong><br />
present<strong>in</strong>g with moderate or severe <strong>acute</strong><br />
<strong>exacerbation</strong>s or when the FEV1 is < 50% <strong>of</strong><br />
predicted (Plotnick 2009 [1a], Rodrigo 2005 [1a], Dotson 2009<br />
[1b], LocalConsensus [5], SIGN 2008 [5a], NAEPP 2007 [5a],<br />
Hayday 2002 [5a]) (see Table 1 Aerosolized Therapies -<br />
drugs and dosage recommendations).<br />
Note 1 : Add<strong>in</strong>g multiple doses (up to 3 doses)<br />
<strong>of</strong> antichol<strong>in</strong>ergics to SABAs appears safe,<br />
improves lung function and avoids hospital<br />
admission <strong>in</strong> 1 <strong>of</strong> 12 school-aged <strong>children</strong> with<br />
severe <strong>exacerbation</strong> (number needed to treat<br />
[NNT] = 12) (Plotnick 2009 [1a]).<br />
Note 2: Although ipratropium has been shown to<br />
be efficacious <strong>in</strong> prevent<strong>in</strong>g hospitalizations for<br />
<strong>children</strong> with <strong>exacerbation</strong>s where FEV1 is
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Table 1: Aerosolized Therapies - Drugs and Dosage Recommendations<br />
Aerosolized Therapies<br />
Medication<br />
(formulation)<br />
Child Dose* Adolescent Dose Notes<br />
Inhaled Short-Act<strong>in</strong>g Beta2-Agonists (SABA)<br />
Albuterol<br />
Nebulizer solution<br />
(2.5 mg/3mL,<br />
5 mg/mL)<br />
MDI<br />
(90 mcg/puff)<br />
Levalbuterol<br />
(R-albuterol)<br />
Nebulizer solution<br />
(0.31mg/3 mL,<br />
0.63 mg/3 mL,<br />
1.25 mg/0.5mL,<br />
1.25 mg/3 mL)<br />
2.5 to 5 mg every 20 m<strong>in</strong>utes for<br />
3 doses, then 2.5 to 5 mg every<br />
1 to 4 hours as needed<br />
0.5 mg/kg/hour by cont<strong>in</strong>uous<br />
nebulization<br />
< 30 kg: 2.5 mg<br />
≥ 30 kg: 5 mg<br />
6 puffs (range: 4 to 8 puffs)<br />
every 20 m<strong>in</strong>utes for 3 doses,<br />
then every 1 to 4 hours as needed<br />
0.075 mg/kg (m<strong>in</strong>imum dose<br />
1.25 mg) every 20 m<strong>in</strong>utes for 3<br />
doses, then 0.075 to 0.15 mg/kg<br />
(not to exceed 2.5 mg) every 1 to<br />
4 hours as needed<br />
2.5 to 5 mg every 20<br />
m<strong>in</strong>utes for 3 doses,<br />
then 2.5 to 10 mg<br />
every 1 to 4 hours as<br />
needed,<br />
or 10 to 15 mg/hour<br />
cont<strong>in</strong>uously<br />
6 puffs (range: 4 to 8 puffs)<br />
every 20 m<strong>in</strong>utes up to 4<br />
hours, then every 1 to 4<br />
hours as needed<br />
1.25 to 2.5 mg every 20<br />
m<strong>in</strong>utes for 3 doses, then<br />
1.25 to 5 mg every 1 to 4<br />
hours as needed<br />
MDI See albuterol MDI dose above. See albuterol MDI dose<br />
(45 mcg/puff) Above.<br />
Antichol<strong>in</strong>ergics <strong>in</strong> comb<strong>in</strong>ation with Short-Act<strong>in</strong>g Beta2-Agonist (SABA)<br />
Ipratropium<br />
bromide<br />
Nebulizer<br />
solution<br />
(500 mcg/2.5mL)<br />
MDI<br />
(18 mcg/puff)<br />
Ipratropium<br />
bromide with<br />
albuterol<br />
Nebulizer<br />
solution<br />
(Each 3 mL vial<br />
conta<strong>in</strong>s 0.5 mg<br />
ipratropium<br />
bromide and 2.5<br />
mg albuterol)<br />
500 mcg with first 3 doses <strong>of</strong><br />
albuterol, (250 mcg may be used<br />
where available)<br />
not to exceed 1500 mcg <strong>in</strong> the<br />
first hour <strong>of</strong> treatment<br />
4 to 8 puffs every 20 m<strong>in</strong>utes as<br />
needed up to 3 hours<br />
1.5 mL every 20 m<strong>in</strong>utes for 3<br />
doses<br />
500 mcg with first 3 doses<br />
<strong>of</strong> albuterol, not to exceed<br />
1500 mcg <strong>in</strong> the first hour<br />
<strong>of</strong> treatment<br />
8 puffs every 20 m<strong>in</strong>utes as<br />
needed up to 3 hours<br />
3 mL every 20 m<strong>in</strong>utes for<br />
3 doses<br />
For optimal delivery, dilute aerosols to<br />
m<strong>in</strong>imum <strong>of</strong> 3 mL at gas flow <strong>of</strong> 6 to 8<br />
L/m<strong>in</strong>. Use large volume nebulizers for<br />
cont<strong>in</strong>uous adm<strong>in</strong>istration. May mix<br />
with ipratropium nebulizer solution.<br />
In mild to moderate <strong>exacerbation</strong>s,<br />
MDI plus VHC (see recommendation<br />
7) is as effective as nebulized therapy<br />
with appropriate adm<strong>in</strong>istration<br />
technique. Add mask <strong>in</strong> <strong>children</strong><br />
unable to manage an MDI device.<br />
See Recommendation 6 <strong>of</strong> this<br />
guidel<strong>in</strong>e regard<strong>in</strong>g levalbuterol.<br />
Not necessary as first l<strong>in</strong>e therapy <strong>in</strong><br />
<strong>children</strong> with mild <strong>exacerbation</strong>s.<br />
Add to SABA therapy for <strong>children</strong><br />
with moderate and severe<br />
<strong>exacerbation</strong>s.<br />
Current formulation (HFA) is safe for<br />
persons with peanut allergy.<br />
May mix ipratropium bromide <strong>in</strong> same<br />
nebulizer with albuterol.<br />
Ipratropium is not necessary as first<br />
l<strong>in</strong>e therapy <strong>in</strong> <strong>children</strong> with mild<br />
<strong>exacerbation</strong>s.<br />
Add ipratropium to SABA therapy for<br />
<strong>children</strong> with moderate and severe<br />
<strong>exacerbation</strong>s. Once the child is<br />
hospitalized, further use <strong>of</strong> ipratropium<br />
has not been shown to provide<br />
significant benefit.<br />
*Children < 12 years <strong>of</strong> age<br />
Abbreviations: HFA = hydr<strong>of</strong>luoroalkane propellant; kg = kilogram; L/m<strong>in</strong> = liter per m<strong>in</strong>ute; mcg = microgram; MDI = metered dose <strong>in</strong>haler;<br />
mg = milligram; mL = milliliter; SABA = short-act<strong>in</strong>g beta 2-agonist; VHC = valved hold<strong>in</strong>g chamber<br />
Adapted from the National Heart Blood and Lung Institute, National Education and Prevention Program<br />
Expert Panel Report 3: Diagnosis and <strong>Management</strong> <strong>of</strong> Asthma, 2007 (LocalConsensus [5], NAEPP 2007 [5a], Taketomo [5a]).<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 4 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Table 2: Corticosteroids - Drugs and Dosage Recommendations<br />
Systemic Corticosteroids<br />
Medication Dosage Notes<br />
Prednisone<br />
Prednisolone<br />
Methylprednisolone<br />
(sodium succ<strong>in</strong>ate)<br />
1 mg/kg once daily<br />
(maximum 60 mg/day)<br />
for a total <strong>of</strong> 5 days<br />
Dexamethasone Oral:<br />
0.6 mg/kg once daily<br />
(max 16 mg/dose)<br />
for 1 to 2 days (Qureshi 2001 [2a])<br />
Dosages <strong>in</strong> excess <strong>of</strong> 1mg/kg <strong>of</strong> prednisone or<br />
prednisolone have been associated with adverse<br />
behavioral effects <strong>in</strong> <strong>children</strong>, whereas 1mg/kg<br />
provides equivalent pulmonary benefit with<br />
decreased adverse effects (Kayani 2002 [2b]).<br />
Intramuscular (dexamethasone sodium<br />
phosphate):<br />
0.6 mg/kg s<strong>in</strong>gle dose<br />
(max 15 mg) (Gordon 2007 [2a])<br />
No advantage has been found for higher dose corticosteroids <strong>in</strong> severe asthma <strong>exacerbation</strong>s.<br />
There is no advantage for <strong>in</strong>travenous adm<strong>in</strong>istration over oral therapy, provided gastro<strong>in</strong>test<strong>in</strong>al function is <strong>in</strong>tact.<br />
Therapy follow<strong>in</strong>g a hospitalization or ED visit is typically 5 days, but may last from 3 to 10 days. Studies <strong>in</strong>dicate there is<br />
no need to taper the systemic corticosteroid dose when given up to 10 days.<br />
Any previous IV doses may be considered as part <strong>of</strong> the total steroid dose.<br />
Abbreviations: ED = emergency department; IV = <strong>in</strong>travenous; kg = kilogram; max = maximum; mg = milligram<br />
Adapted from the National Heart Blood and Lung Institute, National Education and Prevention Program<br />
Expert Panel Report 3: Diagnosis and <strong>Management</strong> <strong>of</strong> Asthma, 2007 (Chang 2008 [2a], LocalConsensus [5], SIGN 2008 [5a], NAEPP 2007 [5a],<br />
Taketomo [5a]).<br />
Corticosteroids<br />
9. It is recommended that oral corticosteroids be<br />
adm<strong>in</strong>istered to patients who do not respond<br />
completely to <strong>in</strong>itial <strong>in</strong>haled SABAs (Edmonds 2009<br />
[1a], NAEPP 2007 [5a], Camargo 2009 [5b]) (see Table 2<br />
drugs and dosage recommendations).<br />
Note 1: Corticosteroids speed the resolution <strong>of</strong><br />
airflow obstruction, reduce the rate <strong>of</strong> relapse,<br />
and may reduce hospitalizations, especially if<br />
adm<strong>in</strong>istered with<strong>in</strong> one hour <strong>of</strong> presentation to<br />
the ED (Rowe 2009a [1a], Edmonds 2009 [1a]).<br />
Note 2: Oral prednisone has effects equivalent to<br />
those <strong>of</strong> <strong>in</strong>travenous methylprednisolone<br />
<strong>in</strong>clud<strong>in</strong>g tolerance by <strong>children</strong> (Rowe 2009a [1a],<br />
SIGN 2008 [5a], NAEPP 2007 [5a], Camargo 2009 [5b]).<br />
Note 3: For treatment <strong>of</strong> <strong>acute</strong> <strong>exacerbation</strong>,<br />
<strong>in</strong>sufficient evidence exists for <strong>in</strong>haled<br />
corticosteroid therapy alone or as an additive<br />
benefit when used with systemic corticosteroids<br />
(Edmonds 2009 [1a], Schuh 2006 [2b], Nakanishi 2003<br />
[2b], NAEPP 2007 [5a], Camargo 2009 [5b]).<br />
Note 4: If the patient is on rout<strong>in</strong>e <strong>in</strong>haled<br />
steroids for chronic control it is not necessary to<br />
stop their use dur<strong>in</strong>g <strong>exacerbation</strong>. The <strong>in</strong>haled<br />
corticosteroids can be started at anytime<br />
regardless <strong>of</strong> oral dos<strong>in</strong>g for the <strong>exacerbation</strong><br />
(LocalConsensus [5], SIGN 2008 [5a], NAEPP 2007 [5a]).<br />
Note 5: It is recognized that many <strong>children</strong> will<br />
have problems with treatment adherence due to<br />
an oral aversion to medic<strong>in</strong>e, especially bittertast<strong>in</strong>g<br />
corticosteroid preparations. In such cases,<br />
alternatives such as <strong>in</strong>tramuscularly adm<strong>in</strong>istered<br />
dexamethasone, oral dexamethasone, and orally<br />
adm<strong>in</strong>istered <strong>in</strong>travenous versions <strong>of</strong><br />
corticosteroids have been proven efficacious<br />
(Rowe 2009a [1a], Smith 2009 [1a], Gordon 2007 [2a],<br />
Altamimi 2006 [2a], Qureshi 2001 [2a], Greenberg 2008<br />
[2b], Huang 2007 [2b], Gries 2000 [2b]).<br />
Adjunctive Therapies<br />
Magnesium Sulfate<br />
10. It is recommended <strong>in</strong> <strong>children</strong> with moderate to<br />
severe <strong>exacerbation</strong>s who are m<strong>in</strong>imally responsive<br />
or unresponsive to <strong>in</strong>itial treatment (SABA, oral<br />
corticosteroids, and ipratropium), that <strong>in</strong>travenous<br />
magnesium sulfate be adm<strong>in</strong>istered (Rowe 2009b [1a],<br />
Mohammed 2007 [1a], Ciarallo 2000 [2b], SIGN 2008 [5a])<br />
(see Table 3 Adjunctive Therapies - drugs and<br />
dosage recommendations).<br />
Note 1: In patients with <strong>acute</strong> <strong>exacerbation</strong> who<br />
have been maximized on standard therapy,<br />
<strong>in</strong>travenous magnesium sulfate has been shown<br />
to reduce hospitalizations and to improve lung<br />
function without significant side effects. Possible<br />
side effects to be aware <strong>of</strong> <strong>in</strong>clude hypotension,<br />
hypotonia, or abnormal reflexes when given<br />
doses above that recommended for asthma (Rowe<br />
2009b [1a], Mohammed 2007 [1a], Alter 2000 [1a]).<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 5 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Note 2: There is <strong>in</strong>sufficient evidence regard<strong>in</strong>g<br />
the use <strong>of</strong> nebulized magnesium sulfate <strong>in</strong> <strong>acute</strong><br />
<strong>exacerbation</strong> (Blitz 2009 [1b]).<br />
Ep<strong>in</strong>ephr<strong>in</strong>e and Terbutal<strong>in</strong>e<br />
11. It is recommended for patients who are m<strong>in</strong>imally<br />
responsive or respond<strong>in</strong>g poorly to SABA /<br />
ipratropium / systemic corticosteroid/magnesium<br />
sulfate therapies, or who are unable to tolerate<br />
aerosol treatments, that parenteral ep<strong>in</strong>ephr<strong>in</strong>e or<br />
terbutal<strong>in</strong>e be considered (NAEPP 2007 [5a]) see Table<br />
3 Adjunctive Therapies - drugs and dosage<br />
recommendations).<br />
Heliox<br />
12. There is <strong>in</strong>sufficient evidence and lack <strong>of</strong> consensus<br />
regard<strong>in</strong>g the effectiveness <strong>of</strong> heliox <strong>in</strong> <strong>acute</strong><br />
<strong>exacerbation</strong> <strong>of</strong> asthma to make a recommendation<br />
for its rout<strong>in</strong>e use (Rivera 2006 [2b], SIGN 2008 [5a]).<br />
Note: Heliox-driven albuterol nebulization may<br />
be considered for patients who have life-<br />
threaten<strong>in</strong>g <strong>exacerbation</strong> or who rema<strong>in</strong> <strong>in</strong> severe<br />
<strong>exacerbation</strong> after <strong>in</strong>tensive conventional<br />
adjunctive therapy (Rodrigo 2006 [1a], Kim 2005 [2b],<br />
NAEPP 2007 [5a]). In one small study,<br />
improvement <strong>in</strong> respiratory score and shorter ED<br />
length <strong>of</strong> stay were seen when heliox was<br />
adm<strong>in</strong>istered <strong>in</strong> moderate and severe<br />
<strong>exacerbation</strong> (Kim 2005 [2b]).<br />
Severe Asthma with Respiratory Distress and<br />
Normal Mental Status<br />
13. It is recommended that multiple therapies as<br />
described below be started simultaneously while<br />
either a consult from the Pediatric Intensive Care is<br />
requested or transport to a higher level <strong>of</strong> care is<br />
arranged (LocalConsensus [5]) (see Table 3 Adjunctive<br />
Therapies- drugs and dosage recommendations)<br />
Adm<strong>in</strong>ister:<br />
cont<strong>in</strong>uous albuterol<br />
ipratropium bromide, up to 3 doses<br />
systemic coticosteroids<br />
(dexamethasone IM or<br />
methylprednisolone IV)<br />
ep<strong>in</strong>ephr<strong>in</strong>e IM<br />
magnesium Sulfate IV<br />
consider terbutal<strong>in</strong>e IV bolus, and <strong>in</strong>fusion.<br />
Table 3: Adjunctive Therapies - Drugs and Dosage Recommendations<br />
Medication Child (< 12 years <strong>of</strong> age) Adolescent Notes<br />
Magnesium Bolus: 50 mg/kg/dose (25 to 100 mg/kg/dose; There is <strong>in</strong>sufficient evidence regard<strong>in</strong>g the benefit<br />
Sulfate<br />
max 2 gms)<br />
from cont<strong>in</strong>uous <strong>in</strong>fusion <strong>of</strong> Magnesium Sulfate<br />
Intravenous (IV) Adm<strong>in</strong>ister over 20 m<strong>in</strong>utes<br />
(Mohammed 2007 [1a]).<br />
Systemic (<strong>in</strong>jected) Beta2-Agonists<br />
Ep<strong>in</strong>ephr<strong>in</strong>e<br />
Intramuscular (IM)<br />
1:1,000<br />
(1 mg/mL)<br />
Terbutal<strong>in</strong>e<br />
Intravenous (IV) or<br />
Subcutaneous (SQ)<br />
(1 mg/mL)<br />
0.01 mg/kg<br />
(max 0.3 to 0.5 mg)<br />
every 20 m<strong>in</strong>utes<br />
for 3 doses<br />
0.01 mg/kg bolus<br />
(max 0.4 mg )<br />
Over 10 m<strong>in</strong>utes<br />
0.01 mg/kg<br />
(max 0.25 mg)<br />
May repeat every 15<br />
m<strong>in</strong>utes for 3 doses<br />
0.3 to 0.5 mg<br />
every 20 m<strong>in</strong>utes<br />
for 3 doses<br />
0.01 mg/kg bolus<br />
(max 0.75 mg)<br />
Over 10 m<strong>in</strong>utes<br />
0.01 mg/kg<br />
(max 0.25 mg)<br />
May repeat every 15<br />
m<strong>in</strong>utes for 3 doses<br />
One small study demonstrated more rapid absorption<br />
and higher plasma levels <strong>of</strong> ep<strong>in</strong>ephr<strong>in</strong>e when<br />
adm<strong>in</strong>istered <strong>in</strong>tramuscularly <strong>in</strong>to the thigh compared<br />
to subcutaneously or <strong>in</strong>tramuscularly <strong>in</strong>to the arm (up<br />
to 4 times faster)(Simons 1998 [2b]).<br />
Start<strong>in</strong>g cont<strong>in</strong>uous <strong>in</strong>fusion dose <strong>in</strong> the ED or PICU<br />
sett<strong>in</strong>gs: 1 mcg/kg/m<strong>in</strong>ute<br />
Abbreviations: ED = emergency department; gms = grams; kg = kilogram; max = maximum; mcg = microgram; mg = milligram;<br />
mL = milliliter; PICU = pediatric <strong>in</strong>tensive care unit<br />
Adapted from the National Heart Blood and Lung Institute, National Education and Prevention Program<br />
Expert Panel Report 3: Diagnosis and <strong>Management</strong> <strong>of</strong> Asthma, 2007 (LocalConsensus [5], NAEPP 2007 [5a], Taketomo [5a]).<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 6 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Tim<strong>in</strong>g <strong>of</strong> Disposition from the Emergency<br />
Department<br />
The response to <strong>in</strong>itial treatment <strong>in</strong> the ED after a period<br />
<strong>of</strong> observation is a better predictor <strong>of</strong> the need for<br />
hospitalization than is the severity <strong>of</strong> an <strong>exacerbation</strong><br />
(NAEPP 2007 [5a]).<br />
14. It is recommended that the current severity <strong>of</strong> the<br />
<strong>exacerbation</strong> be <strong>in</strong> the ―mild‖ range when evaluat<strong>in</strong>g<br />
a child for discharge from ED or hospital<br />
(LocalConsensus [5]) (see Attachment 3 Formal<br />
Evaluation <strong>of</strong> Severity <strong>in</strong> the ED, Attachment 4 ED<br />
<strong>Management</strong> <strong>of</strong> Asthma Exacerbation Algorithm) .<br />
Note 1: In the ED, if <strong>in</strong>itial severity is moderate<br />
or severe, then the severity assessment 1 hour<br />
after treatment is better than <strong>in</strong>itial severity<br />
assessment for determ<strong>in</strong><strong>in</strong>g the need for hospital<br />
admission as well as for predict<strong>in</strong>g the need for<br />
ICU <strong>in</strong> patients <strong>in</strong>itially assessed as severe (Kelly<br />
2004 [3a], LocalConsensus [5]).<br />
Note 2: In <strong>acute</strong> childhood asthma, a repeat pulse<br />
oximetry <strong>of</strong> < 92 to 94 % at 1 hour after treatment<br />
better predicts need for hospitalization than the<br />
<strong>in</strong>itial pulse oximetry (Kelly 2004 [3a], Wright 1997<br />
[3b], LocalConsensus [5]).<br />
Inpatient <strong>Management</strong><br />
General Therapy<br />
15. It is recommended, with the exception <strong>of</strong> the use <strong>of</strong><br />
antichol<strong>in</strong>ergics such as ipratropium, that usual<br />
<strong>in</strong>patient hospital management be viewed as a<br />
cont<strong>in</strong>uation <strong>of</strong> any therapies <strong>in</strong>itiated <strong>in</strong> the ED<br />
<strong>in</strong>clud<strong>in</strong>g: (NAEPP 2007 [5a])<br />
aerosolized bronchodilators<br />
oxygen<br />
corticosteroids<br />
<strong>in</strong>itiation and cont<strong>in</strong>uation <strong>of</strong> controller (anti<strong>in</strong>flammatory)<br />
agents<br />
cont<strong>in</strong>ued assessment<br />
<strong>in</strong>termittent assessment <strong>of</strong> oxygen saturation<br />
FEV1 or peak expiratory flow (PEF) on<br />
admission, 15 to 20 m<strong>in</strong>utes after bronchodilator<br />
therapy dur<strong>in</strong>g <strong>acute</strong> phase and daily until<br />
discharge (<strong>in</strong> <strong>children</strong> > 5 years <strong>of</strong> age if able to<br />
perform).<br />
Failure to Progress<br />
16. It is recommended that the follow<strong>in</strong>g care be<br />
<strong>in</strong>itiated for patients who fail to progress after 12<br />
hours <strong>of</strong> care: (LocalConsensus [5])<br />
notify treat<strong>in</strong>g healthcare provider <strong>of</strong> any child<br />
that has not progressed after 12 hours <strong>of</strong> care<br />
assessment:<br />
physical exam<strong>in</strong>ation and respiratory score<br />
explore reason/s for failure to progress (e.g.<br />
poor SABA responder, pneumonia or other<br />
diagnosis, suboptimal steroid dose or<br />
suboptimal frequency <strong>of</strong> adm<strong>in</strong>istration)<br />
escalate plan based on assessment f<strong>in</strong>d<strong>in</strong>gs<br />
treatment considerations, as <strong>in</strong>dicated:<br />
albuterol treatments every 10 to 20 m<strong>in</strong>utes<br />
for 3 doses or cont<strong>in</strong>uous albuterol<br />
adm<strong>in</strong>istered over 30 m<strong>in</strong>utes, and reassess<br />
chest x-ray<br />
adm<strong>in</strong>ister or re-adm<strong>in</strong>ister IV steroid if<br />
greater than or equal to 12 hours s<strong>in</strong>ce last<br />
dose (oral or IM if cannot acquire IV<br />
access)<br />
venous or capillary blood gas<br />
if status is improved after treatment escalation,<br />
then reassess hourly<br />
if status is not improved, discuss potential for<br />
transfer to PICU or higher level <strong>of</strong> care<br />
consider subspecialty consult.<br />
Decompensation<br />
17. It is recommended that the follow<strong>in</strong>g care be<br />
<strong>in</strong>itiated for the patient whose condition is assessed<br />
as decompensat<strong>in</strong>g from a prior stabilized state: (this<br />
is not for the patient <strong>in</strong> an obvious medical<br />
emergency for whom a medical code needs to be<br />
<strong>in</strong>itiated): (LocalConsensus [5])<br />
albuterol treatments every 10 to 20 m<strong>in</strong>utes for a<br />
total <strong>of</strong> 3 doses or cont<strong>in</strong>uous albuterol over 30<br />
m<strong>in</strong>utes, and reassess<br />
<strong>in</strong>itiate the Medical Response Team (MRT) or the<br />
team responsible for immediate assessment <strong>of</strong> a<br />
child with a change <strong>in</strong> condition<br />
notify treat<strong>in</strong>g healthcare provider that child is<br />
decompensat<strong>in</strong>g<br />
assess for treatment escalation options:<br />
consider other adjunctive medications<br />
- ep<strong>in</strong>ephr<strong>in</strong>e IM<br />
- ipratropium unless previously given<br />
- magnesium sulfate unless previously given<br />
adm<strong>in</strong>ister or readm<strong>in</strong>ister steroid if <strong>in</strong>dicated<br />
(oral, IM, or IV if available)<br />
<strong>in</strong>sert IV<br />
portable chest x-ray<br />
prohibit eat<strong>in</strong>g or dr<strong>in</strong>k<strong>in</strong>g (NPO)<br />
consider capillary or venous blood gas<br />
consider subspecialty consult<br />
reassess after treatment escalation<br />
if improved, resume hourly assessment<br />
if not improved, transfer to PICU or higher<br />
level <strong>of</strong> care.<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 7 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Consistency <strong>of</strong> Care<br />
18. It is recommended that available protocols such as<br />
cl<strong>in</strong>ical pathways or protocols be used, direct<strong>in</strong>g<br />
consistent provision <strong>of</strong> care for patients present<strong>in</strong>g<br />
with an <strong>acute</strong> asthma <strong>exacerbation</strong> (SIGN 2008 [5a],<br />
NAEPP 2007 [5a]). At C<strong>in</strong>c<strong>in</strong>nati Children’s Hospital<br />
Medical Center, such protocol usage <strong>in</strong>cludes:<br />
Asthma Cl<strong>in</strong>ical Order set<br />
Aerosol and Oxygen Protocol.<br />
Note: Use <strong>of</strong> a cl<strong>in</strong>ical pathway or designated<br />
care providers for <strong>in</strong>patient management has<br />
been shown to decrease length <strong>of</strong> stay, use <strong>of</strong><br />
SABA therapy, nurs<strong>in</strong>g and laboratory costs,<br />
and to improve quality <strong>of</strong> care with no <strong>in</strong>crease<br />
<strong>in</strong> readmission rates (Johnson 2000 [2a], McDowell<br />
1998 [2a], Norton 2007 [4a], Wazeka 2001 [4a],<br />
Ebb<strong>in</strong>ghaus 2003 [4b], Kelly 2000 [4b]).<br />
Complementary and Alternative Medic<strong>in</strong>e<br />
19. It is recommended that the cl<strong>in</strong>ician ask<br />
patients/parents about all medications and treatments<br />
they are us<strong>in</strong>g for asthma (LocalConsensus [5], NAEPP<br />
2007 [5a]).<br />
Note 1: A high level <strong>of</strong> use <strong>of</strong> complementary<br />
and alternative medic<strong>in</strong>e (CAM) has been<br />
reported <strong>in</strong> several studies: 45% <strong>of</strong> care providers<br />
reported us<strong>in</strong>g herbal products with their <strong>children</strong><br />
(Lanski 2003 [3a]), 63% <strong>of</strong> adolescents reported the<br />
use <strong>of</strong> complementary medic<strong>in</strong>e when surveyed<br />
(Reznik 2002 [3a]), and a review <strong>of</strong> literature <strong>of</strong><br />
CAM use <strong>in</strong> asthma found the level ranged from<br />
33% to 89% <strong>in</strong> studies <strong>of</strong> <strong>children</strong> and adolescents<br />
(Mark 2007 [1b]). Currently there is <strong>in</strong>sufficient<br />
evidence to support or refute the use <strong>of</strong> CAM<br />
therapies (Altunc 2007 [1a], Hondras 2005 [1a], Mark<br />
2007 [1b]).<br />
Note 2: Patients who use herbal treatments may<br />
need caution regard<strong>in</strong>g the potential for harmful<br />
<strong>in</strong>gredients <strong>in</strong> herbal treatments and <strong>in</strong>teractions<br />
with asthma medications (Lanski 2003 [3a], NAEPP<br />
2007 [5a]).<br />
20. It is recommended that acupuncture not be used for<br />
the treatment <strong>of</strong> asthma. No evidence <strong>of</strong> an effect <strong>of</strong><br />
acupuncture <strong>in</strong> reduc<strong>in</strong>g asthma symptoms has been<br />
demonstrated (McCarney 2009 [1a], Mart<strong>in</strong> 2002 [1a],<br />
NAEPP 2007 [5a]).<br />
ED or Inpatient <strong>Management</strong><br />
Screen<strong>in</strong>g<br />
21. It is recommended that systematic screen<strong>in</strong>g be<br />
conducted us<strong>in</strong>g a broad assessment tool, such as<br />
Child Asthma Risk Assessment Tool (CARAT) for<br />
identification <strong>of</strong> risks <strong>in</strong>clud<strong>in</strong>g medical,<br />
environmental, adherence, f<strong>in</strong>ancial, psychosocial or<br />
health literacy (LocalConsensus [5]). The CARAT may<br />
be accessed via the follow<strong>in</strong>g URL:<br />
http://carat.asthmarisk.org<br />
Consultations<br />
22. It is recommended that the need for consultations be<br />
considered at the time <strong>of</strong> presentation or as early as<br />
possible <strong>in</strong> the <strong>acute</strong> course (LocalConsensus [5]).<br />
Medical consultation: Usual <strong>in</strong>dications for medical<br />
consultation (usually, a fellowship-tra<strong>in</strong>ed allergist or<br />
pulmonologist; occasionally, other physicians who<br />
have expertise <strong>in</strong> asthma management, developed<br />
through additional tra<strong>in</strong><strong>in</strong>g and experience) <strong>in</strong><br />
childhood asthma <strong>in</strong>clude: (LocalConsensus [5], NAEPP<br />
2007 [5a])<br />
the diagnosis <strong>of</strong> asthma is <strong>in</strong> question<br />
current life-threaten<strong>in</strong>g or severe asthma<br />
<strong>exacerbation</strong> possibly requir<strong>in</strong>g MRT (medical<br />
response team)<br />
poor-responder or requir<strong>in</strong>g escalation <strong>in</strong> rout<strong>in</strong>e<br />
care or unexpla<strong>in</strong>ed deterioration<br />
repeated life-threaten<strong>in</strong>g hospital admissions,<br />
history <strong>of</strong> <strong>in</strong>tensive care admission, frequent ED<br />
visits for asthma<br />
patient has required more than two bursts <strong>of</strong> oral<br />
corticosteroids <strong>in</strong> the past 12 months<br />
any <strong>exacerbation</strong> requir<strong>in</strong>g hospitalization <strong>in</strong> the<br />
last 12 months<br />
evaluation for addition or discont<strong>in</strong>uation <strong>of</strong><br />
LABA therapy<br />
conditions complicat<strong>in</strong>g asthma or its diagnosis<br />
(e.g. s<strong>in</strong>usitis, nasal polyps, aspergillosis, severe<br />
rh<strong>in</strong>itis, vocal cord dysfunction, gastroesophageal<br />
reflux, and chronic obstructive pulmonary<br />
disease)<br />
need for extensive education and guidance on<br />
allergen avoidance, problems with adherence to<br />
therapy and poor control, or complications <strong>of</strong><br />
therapy.<br />
Mental Health consultation: Patients who have<br />
significant psychiatric, psychosocial, or family<br />
problems that <strong>in</strong>terfere with their asthma therapy may<br />
need referral to an appropriate mental health<br />
pr<strong>of</strong>essional for counsel<strong>in</strong>g or treatment.<br />
Social Service Consultation: Indications for<br />
consider<strong>in</strong>g social service consultation <strong>in</strong>clude:<br />
family's social or f<strong>in</strong>ancial difficulties might be<br />
impediments to adherence with the treatments and<br />
medical follow-up<br />
family resources are compromised or uncerta<strong>in</strong><br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 8 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Interpreter Services Consultation: Indication for<br />
consider<strong>in</strong>g services:<br />
family <strong>in</strong> need <strong>of</strong> language <strong>in</strong>terpretation<br />
Pharmacist Consultation: Indications for<br />
consider<strong>in</strong>g pharmacist consultation (where<br />
available) <strong>in</strong>clude review <strong>of</strong> the medication regimen<br />
<strong>of</strong> a patient admitted for asthma <strong>exacerbation</strong><br />
Note: Medication regimen evaluation may<br />
<strong>in</strong>clude: screen<strong>in</strong>g for adverse drug reactions,<br />
screen<strong>in</strong>g for drug <strong>in</strong>teractions, ensur<strong>in</strong>g<br />
appropriate medication use and dos<strong>in</strong>g,<br />
appropriate route <strong>of</strong> adm<strong>in</strong>istration, appropriate<br />
dos<strong>in</strong>g <strong>in</strong>tervals and/or comparison <strong>of</strong> the<br />
medication reconciliation record with the<br />
current medication orders (Sanghera 2006 [1a],<br />
Kaushal 2008 [3a]).<br />
Therapies Generally NOT Recommended<br />
23. It is recommended that theophyll<strong>in</strong>e or<br />
am<strong>in</strong>ophyll<strong>in</strong>e not be adm<strong>in</strong>istered rout<strong>in</strong>ely <strong>in</strong> the<br />
ED or hospitalized patient because they do not appear<br />
to provide additional benefit to optimal SABA therapy<br />
(D'Avila 2008 [2b]) and may <strong>in</strong>crease frequency <strong>of</strong><br />
adverse effects <strong>in</strong> <strong>acute</strong> <strong>exacerbation</strong> (Mitra 2009 [1a],<br />
SIGN 2008 [5a], NAEPP 2007 [5a]).<br />
Note 3: Patients us<strong>in</strong>g theophyll<strong>in</strong>e as<br />
outpatients may cont<strong>in</strong>ue on their usual doses <strong>in</strong><br />
the hospital; obta<strong>in</strong><strong>in</strong>g a therapeutic level while<br />
the child is hospitalized may be considered,<br />
because illness can affect serum levels.<br />
Additionally, a pharmacist consult may be<br />
useful for review <strong>of</strong> drug <strong>in</strong>teractions (NAEPP<br />
2007 [5a]).<br />
24. It is recommended that antibiotics not be used<br />
rout<strong>in</strong>ely for <strong>acute</strong> asthma <strong>exacerbation</strong>s <strong>in</strong> the<br />
absence <strong>of</strong> an identified bacterial focus (Graham 2009<br />
[1a], SIGN 2008 [5a], NAEPP 2007 [5a], Blasi 2007 [5b]).<br />
25. It is recommended that aggressive rehydration not<br />
be used rout<strong>in</strong>ely for <strong>acute</strong> asthma <strong>exacerbation</strong> <strong>in</strong><br />
the absence <strong>of</strong> cl<strong>in</strong>ical dehydration (NAEPP 2007 [5a]).<br />
26. It is recommended that chest physiotherapy (CPT),<br />
<strong>in</strong>centive spirometry, and mucolytics not be used<br />
rout<strong>in</strong>ely for <strong>acute</strong> asthma <strong>exacerbation</strong>s as they can<br />
trigger bronchospasm or worsen cough or air flow<br />
obstruction dur<strong>in</strong>g an <strong>acute</strong> asthma attack (NAEPP<br />
2007 [5a]).<br />
27. It is recommended that anxiolytic and hypnotic<br />
drugs not be used rout<strong>in</strong>ely for <strong>acute</strong> asthma<br />
<strong>exacerbation</strong>s outside <strong>of</strong> an <strong>in</strong>tensive care sett<strong>in</strong>g, as<br />
they may cause respiratory depression (NAEPP 2007<br />
[5a]).<br />
28. It is recommended that oral albuterol not be used<br />
for <strong>acute</strong> <strong>exacerbation</strong> (LocalConsensus [5]).<br />
Therapy Cautions/Considerations<br />
29. It is recommended that for therapies outl<strong>in</strong>ed <strong>in</strong> this<br />
section, caution and consideration be used <strong>in</strong><br />
treatment selections (LocalConsensus [5]).<br />
Ibupr<strong>of</strong>en: In <strong>children</strong> without known Aspir<strong>in</strong> Induced<br />
Asthma (AIA), ibupr<strong>of</strong>en may be a better choice than<br />
acetam<strong>in</strong>ophen for the treatment <strong>of</strong> fever/pa<strong>in</strong> <strong>in</strong> <strong>children</strong><br />
present<strong>in</strong>g with <strong>acute</strong> asthma <strong>exacerbation</strong>s.<br />
Acetam<strong>in</strong>ophen has been associated with an <strong>in</strong>creased risk<br />
<strong>of</strong> wheez<strong>in</strong>g (Kanabar 2007 [1a], Karimi 2006 [4a]).<br />
In <strong>children</strong> with known AIA, it is prudent to counsel<br />
parents regard<strong>in</strong>g the potential for cross-sensitivities to<br />
non-steroidal anti-<strong>in</strong>flammatory drugs (NSAIDs) (Debley<br />
2005 [1a]). This patient population demonstrates less crosssensitivity<br />
to acetam<strong>in</strong>ophen.<br />
Cross-Sensitivities: (Jenk<strong>in</strong>s 2004 [1a])<br />
ibupr<strong>of</strong>en < 400mg 98%<br />
naproxen < 100mg 100%<br />
dicl<strong>of</strong>enac < 40mg 93%<br />
acetam<strong>in</strong>ophen > 500mg 7%<br />
Long-Act<strong>in</strong>g Beta2-Agonists<br />
Epidemiological evidence suggests a l<strong>in</strong>k between longact<strong>in</strong>g<br />
beta2-agonists (LABAs) and <strong>in</strong>creases <strong>in</strong> asthma<br />
mortality. Concern rema<strong>in</strong>s that symptomatic benefit<br />
from treatment with LABAs might lead to<br />
underestimation <strong>of</strong> <strong>acute</strong> attack severity and long-term<br />
use could lead to tolerance to their bronchodilator<br />
effects (Cates 2009b [1a], Cates 2009a [1a]). In addition,<br />
recent analyses by the Food and Drug Adm<strong>in</strong>istration<br />
(FDA) and others concluded that use <strong>of</strong> LABAs is<br />
associated with an <strong>in</strong>creased risk <strong>of</strong> severe worsen<strong>in</strong>g <strong>of</strong><br />
asthma symptoms, lead<strong>in</strong>g to hospitalization <strong>in</strong> both<br />
<strong>children</strong> and adults and death <strong>in</strong> some patients with<br />
asthma (Salpeter 2010 [1a], Walters 2007 [1a], Salpeter 2006<br />
[1a], FDA 2010 [5]). The FDA is requir<strong>in</strong>g further studies<br />
for safety evaluation and has concluded that although<br />
these medic<strong>in</strong>es play an important role <strong>in</strong> help<strong>in</strong>g some<br />
patients control asthma symptoms, their use be limited<br />
to patients whose asthma cannot be controlled with<br />
<strong>in</strong>haled corticosteroids alone (FDA 2010 [5]). There is no<br />
good evidence as to which subpopulation would benefit<br />
or be harmed with use <strong>of</strong> a LABA. One recent study,<br />
evaluat<strong>in</strong>g step-up therapy <strong>in</strong> <strong>children</strong>, concluded that<br />
response to LABA was more likely to provide a better<br />
response compared to ICS or leukotriene-receptor<br />
antagonist (LTRA). However many <strong>children</strong> had a best<br />
response to ICS or LTRA step-up, highlight<strong>in</strong>g the need<br />
to regularly monitor and appropriately adjust each<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 9 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
child’s asthma therapy with<strong>in</strong> this level <strong>of</strong> care before<br />
further step-up (Lemanske 2010 [2a]).<br />
Until further studies are concluded, it is suggested<br />
that all patients treated with LABA be <strong>in</strong>dividually<br />
evaluated to ensure that this is the best option for<br />
asthma control (Cates 2009b [1a], Cates 2009a [1a]).<br />
Such evaluation may best be performed <strong>in</strong><br />
conjunction with an Asthma Specialist<br />
(LocalConsensus [5]) (see Recommendation #35 for<br />
evaluation <strong>of</strong> LABA use).<br />
Disparities <strong>in</strong> quality <strong>of</strong> care: When treat<strong>in</strong>g <strong>children</strong><br />
with asthma, it is important to consider the<br />
socioeconomic factors that might lead to avoidable<br />
hospitalizations and premature mortality (Cope 2008 [4a],<br />
Gupta 2006 [4a]). Special consideration <strong>of</strong> the follow<strong>in</strong>g<br />
conditions assists <strong>in</strong> the provision <strong>of</strong> patient-centered,<br />
equitable care:<br />
Medicaid-covered, m<strong>in</strong>ority <strong>children</strong> have worse<br />
asthma status (parental report) and are less likely to<br />
be us<strong>in</strong>g preventive, anti-<strong>in</strong>flammatory agents than<br />
white <strong>children</strong> (Ferris 2006 [4a], Lieu 2002 [4a]).<br />
Children un<strong>in</strong>sured or on Medicaid have ranked<br />
significantly lower on seven quality measures<br />
<strong>in</strong>clud<strong>in</strong>g ED utilization, prescriptions from the ED,<br />
and access to and use <strong>of</strong> a primary care provider<br />
(Lara 2003 [2a], Knudson 2009 [4a], Wilson 2005 [4a], Ferris<br />
2001 [4a]).<br />
Black <strong>children</strong> demonstrate more likelihood to have<br />
asthma and to experience ED visits for asthma,<br />
compared with otherwise comparable white <strong>children</strong><br />
(Flores 2005 [3a], Jones 2008 [4a]).<br />
The effect <strong>of</strong> comorbid conditions and mental illness<br />
<strong>in</strong> mothers <strong>of</strong> asthmatic <strong>children</strong> has recently been<br />
shown to impact asthma control and health services<br />
utilization related to asthma (Coughlan 2001 [1a],<br />
Bartlett 2001 [3a], Belamarich 2000 [3a], Rodriguez 2002<br />
[4a], Shalowitz 2001 [4a], NAEPP 2007 [5a]) (see<br />
Recommendation #22, Consultations, Social<br />
Services).<br />
Discharge/Transition Preparation<br />
Although this guidel<strong>in</strong>e is focused on the <strong>acute</strong><br />
management <strong>of</strong> asthma <strong>exacerbation</strong>s, it is recognized<br />
that asthma is a chronic disease. Discharge plann<strong>in</strong>g is<br />
<strong>in</strong>tended to assist the transition from the <strong>acute</strong><br />
<strong>exacerbation</strong> to chronic management, identify<strong>in</strong>g factors<br />
with<strong>in</strong> the chronic action plan that may need adjust<strong>in</strong>g to<br />
prevent future <strong>exacerbation</strong>s and improve long-term<br />
patient outcomes. The transition plan is expected to<br />
enhance the likelihood that the family, and ultimately<br />
the child, will become skilled <strong>in</strong> self-management <strong>of</strong> this<br />
chronic condition. Early plann<strong>in</strong>g is important to assure<br />
that problems with details associated with follow-up<br />
have been resolved prior to discharge.<br />
Recommendations for comprehensive management <strong>of</strong><br />
chronic asthma can be found <strong>in</strong> the most recent update<br />
<strong>of</strong> the national asthma guidel<strong>in</strong>e (NAEPP 2007 [5a]).<br />
30. It is recommended that plann<strong>in</strong>g for discharge beg<strong>in</strong><br />
when the child first presents to the ED or hospital<br />
unit (LocalConsensus [5]).<br />
31. It is recommended that prior to discharge the patient<br />
undergo Severity Classification <strong>of</strong> chronic asthma (see<br />
Attachment 5 Severity Classification). This will<br />
support a patient-centered approach to therapy (NAEPP<br />
2007 [5a]). Also, Severity Classification may be useful<br />
to the primary care provider <strong>in</strong> identify<strong>in</strong>g <strong>children</strong><br />
with special health care needs and facilitat<strong>in</strong>g care<br />
coord<strong>in</strong>ation (LocalConsensus [5]).<br />
32. It is recommended that case or care management by<br />
tra<strong>in</strong>ed health pr<strong>of</strong>essionals be considered for<br />
patients who have poorly controlled asthma and have<br />
recurrent visits to the ED or hospital. Caremanagement<br />
processes are tools to improve the<br />
efficiency and quality <strong>of</strong> primary care delivery, self<br />
management, and have demonstrated a reduction <strong>in</strong><br />
ED visits (Schulte 2004 [1b], Levy 2006 [2a], Walders 2006<br />
[2a], Griffiths 2004 [2a], Portnoy 2006 [4a], Rosen 2006 [4a],<br />
Spiegel 2006 [4a], Wood 2006 [4a], Allcock 2009 [4b], CMSA<br />
2010 [5]).<br />
33. It is recommended, before the patient is discharged<br />
from the ED or <strong>in</strong>patient unit, that education be<br />
provided that is tailored to the identified needs,<br />
beliefs, and learn<strong>in</strong>g styles <strong>of</strong> the patient and family<br />
and addresses identified patient-desired outcomes<br />
(Zorc 2005 [2a], LocalConsensus [5], Mansour 2009 [5a], SIGN<br />
2008 [5a], NAEPP 2007 [5a]).<br />
Note 1: When usual care for asthma was<br />
compared to more <strong>in</strong>tensive educational programs<br />
(provided <strong>in</strong> either the ED, hospital, home or<br />
cl<strong>in</strong>ic), reduction <strong>in</strong> subsequent ED visits and<br />
hospital admissions occurred <strong>in</strong> those receiv<strong>in</strong>g<br />
<strong>in</strong>tensive education (Boyd 2009 [1a], Wolf 2008 [1a],<br />
Karnick 2007 [2a], Brown 2006 [2a], Ng 2006 [2a],<br />
Sockrider 2006 [2a]). The most effective type,<br />
duration or <strong>in</strong>tensity <strong>of</strong> education has not been<br />
determ<strong>in</strong>ed (Boyd 2009 [1a], C<strong>of</strong>fman 2008 [1a], Wolf<br />
2008 [1a], Zorc 2009 [2a]). Patient-centered, specific<br />
education efforts may be more effective than<br />
general or poorly targeted <strong>in</strong>terventions (Can<strong>in</strong>o<br />
2008 [2a], Forbis 2002 [2b], NAEPP 2007 [5a]).<br />
Note 2: Asthma education plans have been<br />
successfully implemented <strong>in</strong> busy EDs (Boychuk<br />
2006 [3a], NAEPP 2007 [5a]).<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 10 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Components <strong>of</strong> education programs have not been<br />
comparatively studied; however, programs that have<br />
demonstrated improvement have <strong>in</strong>cluded the follow<strong>in</strong>g<br />
components: (Boyd 2009 [1a], C<strong>of</strong>fman 2008 [1a], Wolf 2008 [1a])<br />
etiology, prognosis, and risk factors emphasiz<strong>in</strong>g<br />
chronicity <strong>of</strong> condition<br />
medication purpose, and when and how to use<br />
medications (Smith 2008 [4a])<br />
provision or updat<strong>in</strong>g <strong>of</strong> written asthma plan<br />
Note: Parental attitudes toward and knowledge <strong>of</strong><br />
asthma (pathophysiology, medications, action<br />
plans, and environmental triggers) <strong>in</strong>fluenced<br />
adherence to prescribed asthma medications and<br />
action plans <strong>in</strong> several studies (Jones 2002 [2a],<br />
Douglas 2002 [2b], NAEPP 2007 [5a]).<br />
identification <strong>of</strong> environmental triggers for prevention<br />
<strong>of</strong> <strong>acute</strong> <strong>exacerbation</strong>s (Lanphear 2001b [4a], Lanphear<br />
2001a [4a]) (see Attachment 6 How to Control what<br />
Makes Your Asthma Worse)<br />
Note: Multifaceted allergen education and control<br />
<strong>in</strong>terventions delivered <strong>in</strong> the home sett<strong>in</strong>g have<br />
been shown to be effective <strong>in</strong> reduc<strong>in</strong>g exposures<br />
to cockroach, rodent, and dust-mite allergens and<br />
associated asthma morbidity (Arshad 2007 [2a],<br />
Morgan 2004 [2a], Schonberger 2004 [2a], Chan-Yeung 2002<br />
[2a], Custovic 2001 [2a], F<strong>in</strong>n 2000 [3a], NAEPP 2007 [5a]).<br />
demonstration <strong>of</strong> correct use <strong>of</strong> <strong>in</strong>haler / spacer (Hussa<strong>in</strong>-<br />
Rizvi 2009 [2b]) (see Attachment 7 MDI Use)<br />
demonstration <strong>of</strong> peak flow technique if send<strong>in</strong>g home<br />
with peak flow meter – (for patients with moderate or<br />
severe persistent asthma or a history <strong>of</strong> severe<br />
<strong>exacerbation</strong>s, or patients who are poor perceivers <strong>of</strong><br />
airflow obstruction) (see Attachment 8 Peak Flow Use)<br />
Note: Peak flow measurement can be a useful<br />
addition for severity assessment <strong>of</strong> an asthma<br />
<strong>exacerbation</strong> and is most useful <strong>in</strong> patients with<br />
moderate to severe persistent asthma (McMullen 2002<br />
[2a], Yoos 2002 [2a]). It can be used <strong>in</strong> short-term<br />
monitor<strong>in</strong>g, <strong>acute</strong> <strong>exacerbation</strong>s, and daily chronic<br />
monitor<strong>in</strong>g (Goldberg 2001 [4a], Brand 1999 [4a], NAEPP<br />
2007 [5a]).<br />
home management <strong>of</strong> <strong>exacerbation</strong> or relapse<br />
<strong>in</strong>clud<strong>in</strong>g evaluation <strong>of</strong> early cl<strong>in</strong>ical signs and<br />
symptoms <strong>of</strong> airway <strong>in</strong>flammation<br />
Note: Beg<strong>in</strong>n<strong>in</strong>g treatment at home may avoid<br />
treatment delays, prevent <strong>exacerbation</strong>s from<br />
becom<strong>in</strong>g severe, and also adds to patients’ sense<br />
<strong>of</strong> control over their asthma. The degree <strong>of</strong> care<br />
provided <strong>in</strong> the home depends on the patients’ (or<br />
parents’) abilities and experience and on the<br />
availability <strong>of</strong> emergency care (NAEPP 2007 [5a]).<br />
Accurate evaluation <strong>of</strong> symptom severity by<br />
parents and <strong>children</strong> will assist to avoid delays<br />
<strong>in</strong> care and <strong>in</strong>appropriate home management<br />
(Garbutt 2009 [2a]).<br />
importance and purpose <strong>of</strong> follow-up appo<strong>in</strong>tment –<br />
explore action plan, evaluate patient goal atta<strong>in</strong>ment,<br />
identify barriers to meet<strong>in</strong>g activity goals, identify<br />
potential treatment adjustments to help meet goals and<br />
prevent future <strong>exacerbation</strong>s (Zorc 2005 [2a], Zorc 2003<br />
[2a], Flores 2005 [3a]):<br />
• schedule before discharge for hospitalized<br />
patient 1 to 5 days after discharge<br />
• contact primary care provider before discharge<br />
from ED<br />
importance <strong>of</strong> cont<strong>in</strong>ual and consistent care <strong>in</strong><br />
outpatient sett<strong>in</strong>g, partner<strong>in</strong>g with primary care<br />
provider to tailor <strong>in</strong>terventions toward the child’s<br />
goals for activity<br />
provision <strong>of</strong> Asthma Specialists resource <strong>in</strong>formation<br />
if <strong>in</strong>dicated.<br />
34. It is recommended that SABAs be used at home on an<br />
as-needed basis after recovery from an <strong>acute</strong> asthma<br />
<strong>exacerbation</strong> (Walters 2002 [1a], NAEPP 2007 [5a]). If<br />
patient’s need is greater than 6 puffs every 3 to 4<br />
hours by 24 to 48 hours after discharge provide family<br />
with <strong>in</strong>struction to seek medical care (LocalConsensus<br />
[5]).<br />
35. It is recommended that if a LABA was <strong>in</strong> use before<br />
admission, it be suspended dur<strong>in</strong>g hospitalization for<br />
<strong>exacerbation</strong> and the patient be evaluated for<br />
cont<strong>in</strong>uation <strong>of</strong> therapy after discharge: (LocalConsensus<br />
[5], SIGN 2008 [5a]).<br />
Note 1: There is no evidence that cont<strong>in</strong>u<strong>in</strong>g a<br />
LABA dur<strong>in</strong>g <strong>exacerbation</strong> is beneficial and<br />
concern rema<strong>in</strong>s regard<strong>in</strong>g harm with its<br />
cont<strong>in</strong>ued use.<br />
Note 2: The beneficial effects <strong>of</strong> LABA <strong>in</strong><br />
comb<strong>in</strong>ation therapy for the patients who require<br />
more therapy than low-dose ICS alone to control<br />
asthma need to be weighed aga<strong>in</strong>st the potential<br />
<strong>in</strong>creased risk <strong>of</strong> severe <strong>exacerbation</strong>s, associated<br />
with the daily use <strong>of</strong> LABAs <strong>in</strong> some patients<br />
(Cates 2009b [1a], Cates 2009a [1a], Nelson 2006 [2a],<br />
NAEPP 2007 [5a]).<br />
Consider consultation with an Asthma Specialist<br />
for questions regard<strong>in</strong>g cont<strong>in</strong>uation <strong>of</strong> LABA<br />
follow<strong>in</strong>g hospital discharge (LocalConsensus [5]).<br />
Note 3: In February <strong>of</strong> 2010 the FDA announced<br />
new safety controls for LABAs as follows:<br />
―LABAs are contra<strong>in</strong>dicated without the use<br />
<strong>of</strong> an asthma controller medication such as<br />
<strong>in</strong>haled corticosteroid, and should not be<br />
used alone‖ (FDA 2010 [5], NAEPP 2007 [5a]).<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 11 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
―LABAs ought to only be used long-term <strong>in</strong><br />
patients whose asthma cannot be adequately<br />
controlled on other asthma controller<br />
medications‖ (FDA 2010 [5]).<br />
―LABAs ought to only be used for the<br />
shortest duration <strong>of</strong> time required to achieve<br />
control <strong>of</strong> asthma symptoms and<br />
discont<strong>in</strong>ued, if possible, once asthma<br />
control is achieved‖ (FDA 2010 [5]).<br />
Note 4: Of the adjunctive therapies available,<br />
LABAs are the preferred therapy to comb<strong>in</strong>e with<br />
ICS <strong>in</strong> youths ≥ 12 years <strong>of</strong> age and adults (NAEPP<br />
2007 [5a]).<br />
Note 5: For patients ≥ 5 years <strong>of</strong> age who have<br />
moderate persistent asthma or asthma<br />
<strong>in</strong>adequately controlled on low-dose ICS, the<br />
option to <strong>in</strong>crease the ICS dose may be given<br />
equal weight to the option <strong>of</strong> add<strong>in</strong>g LABA<br />
(NAEPP 2007 [5a]). A recent study suggests that<br />
patients are most likely to have a differential<br />
response to the addition <strong>of</strong> LABA to low dose<br />
ICS compared to <strong>in</strong>creas<strong>in</strong>g ICS or add<strong>in</strong>g a<br />
leukotriene receptor antagonist. However, the<br />
safety <strong>of</strong> long term use <strong>of</strong> LABA rema<strong>in</strong>s<br />
uncerta<strong>in</strong> (Lemanske 2010 [2a]).<br />
Note 6: For patients ≥ 5 years <strong>of</strong> age who have<br />
severe persistent asthma or asthma <strong>in</strong>adequately<br />
controlled, the comb<strong>in</strong>ation <strong>of</strong> LABA and ICS is<br />
the preferred therapy (NAEPP 2007 [5a]).<br />
Note 7: For patients < 4 years <strong>of</strong> age, there is<br />
<strong>in</strong>sufficient evidence for use <strong>of</strong> a LABA. These<br />
drugs are not labeled for use <strong>in</strong> this age group.<br />
Consider consultation with an Asthma Specialist<br />
for questions regard<strong>in</strong>g this subset <strong>of</strong> asthma<br />
patients before add<strong>in</strong>g LABA therapy<br />
(LocalConsensus [5], NAEPP 2007 [5a]).<br />
36. It is recommended that patients already on ICS<br />
cont<strong>in</strong>ue ICS therapy after discharge from ED or<br />
<strong>in</strong>patient sett<strong>in</strong>g. Consider <strong>in</strong>itiat<strong>in</strong>g ICS for patients<br />
with persistent asthma if not already receiv<strong>in</strong>g (SIGN<br />
2008 [5a], NAEPP 2007 [5a]).<br />
Note: Initiat<strong>in</strong>g ICS at discharge for patients not<br />
already on ICS has demonstrated a decreased risk<br />
<strong>of</strong> subsequent ED visits for patients with persistent<br />
asthma (S<strong>in</strong> 2002 [4a], NAEPP 2007 [5a]).<br />
37. It is recommended, when possible, that long term<br />
controller medications and medic<strong>in</strong>es to complete<br />
<strong>exacerbation</strong> therapy are provided to the patient prior<br />
to discharge (Qureshi 2001 [2a], Cooper 2001 [4a]).<br />
Note: Prescriptions are not always filled after<br />
discharge (Qureshi 2001 [2a], Cooper 2001 [4a]).<br />
Outcomes demonstrated from prescriptions not<br />
filled have been an <strong>in</strong>crease <strong>in</strong> missed school and<br />
work days (Qureshi 2001 [2a]). It is also believed<br />
that provid<strong>in</strong>g medic<strong>in</strong>es will result <strong>in</strong> decrease<br />
readmission rates (LocalConsensus [5], NAEPP 2007<br />
[5a]).<br />
38. It is recommended that patients have a written plan<br />
that reflects adjustments necessary due to the current<br />
<strong>exacerbation</strong> and <strong>in</strong>cludes a stepwise approach<br />
coord<strong>in</strong>at<strong>in</strong>g with the child’s plan for chronic<br />
management (Zemek 2008 [1a], Bhogal 2006 [1a], NAEPP<br />
2007 [5a]) (see Attachment 9, Stepwise <strong>Management</strong>).<br />
39. It is recommended that every attempt be made to<br />
schedule the follow-up appo<strong>in</strong>tment before the<br />
child is discharged from the facility. When this is<br />
not possible, attempt to notify the primary care<br />
provider <strong>of</strong> the current <strong>exacerbation</strong> event (Zorc 2005<br />
[2a], Zorc 2003 [2a], LocalConsensus [5], NAEPP 2007<br />
[5a]).<br />
Note: A significant number <strong>of</strong> patients from the<br />
C<strong>in</strong>c<strong>in</strong>nati population consider the ED their<br />
regular source <strong>of</strong> care, and a commonly held<br />
health belief is that the ED is the appropriate place<br />
to seek care for a breath<strong>in</strong>g problem (Mansour 2000<br />
[2b]). Hav<strong>in</strong>g fewer general practice contacts <strong>in</strong><br />
the previous year has been <strong>in</strong>dependently<br />
associated with an <strong>in</strong>creased risk <strong>of</strong> fatal asthma,<br />
<strong>in</strong>creas<strong>in</strong>g the importance <strong>of</strong> the follow-up visit<br />
either with the primary care provider or asthma<br />
specialist (LocalConsensus [5], NAEPP 2007 [5a]).<br />
Discharge read<strong>in</strong>ess<br />
Ongo<strong>in</strong>g assessment will provide the needed <strong>in</strong>formation<br />
<strong>of</strong> the patient progression to determ<strong>in</strong>e the read<strong>in</strong>ess for<br />
discharge. Discharge read<strong>in</strong>ess usually <strong>in</strong>cludes the<br />
follow<strong>in</strong>g:<br />
child stable on therapies that can be adm<strong>in</strong>istered at<br />
home<br />
home environment is able to safely fulfill discharge<br />
plan<br />
sufficient knowledge <strong>of</strong> asthma to manage care at<br />
home or seek help if symptoms worsen<br />
arrangements for any special medications or<br />
equipment required for home therapies are complete<br />
transition plan based on admission screen<strong>in</strong>g is<br />
complete and reflects the patients cont<strong>in</strong>uum <strong>of</strong> care<br />
needs<br />
follow-up care is arranged, coord<strong>in</strong>at<strong>in</strong>g with<br />
primary care provider or asthma specialist if<br />
<strong>in</strong>dicated, and providers agree with plans.<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 12 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Future Research Agenda<br />
Cl<strong>in</strong>ical questions <strong>of</strong> potential <strong>in</strong>terest to CCHMC<br />
<strong>in</strong>vestigators related to the population <strong>of</strong> <strong>children</strong> 12<br />
months to 18 years <strong>of</strong> age with <strong>acute</strong> asthma:<br />
1. Does the discont<strong>in</strong>uation <strong>of</strong> LABA upon<br />
<strong>exacerbation</strong> compared to cont<strong>in</strong>uation <strong>of</strong> LABA:<br />
decrease the length <strong>of</strong> <strong>exacerbation</strong>?<br />
decrease the number <strong>of</strong> treatment failures (e.g.<br />
decompensation, admission)?<br />
2. Does the use <strong>of</strong> same dose Levalbuterol compared<br />
to Albuterol:<br />
decrease admissions?<br />
decrease costs?<br />
decrease cardiac adverse events (e.g.<br />
tachycardia, arrhythmia)?<br />
3. Does the use <strong>of</strong> a respiratory score compared to no<br />
score:<br />
decrease length <strong>of</strong> stay?<br />
CCHMC Guidel<strong>in</strong>e Implementation Tools<br />
Any available implementation tools are available onl<strong>in</strong>e<br />
and may be distributed by any organization for the<br />
global purpose <strong>of</strong> improv<strong>in</strong>g child health outcomes.<br />
Website address:<br />
http://www.c<strong>in</strong>c<strong>in</strong>nati<strong>children</strong>s.org/svc/alpha/h/health-policy/evbased/default.htm<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 13 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
KEY INDICATORS FOR CONSIDERING A DIAGNOSIS OF <strong>ASTHMA</strong><br />
Consider a diagnosis <strong>of</strong> asthma and perform<strong>in</strong>g spirometry if any <strong>of</strong> these <strong>in</strong>dicators is present.*<br />
These <strong>in</strong>dicators are not diagnostic by themselves, but the presence <strong>of</strong> multiple key <strong>in</strong>dicators<br />
<strong>in</strong>creases the probability <strong>of</strong> a diagnosis <strong>of</strong> asthma. Spirometry is needed to establish a diagnosis <strong>of</strong><br />
asthma.<br />
Wheez<strong>in</strong>g—high-pitched whistl<strong>in</strong>g sounds when breath<strong>in</strong>g out—especially <strong>in</strong> <strong>children</strong>. (Lack<br />
<strong>of</strong> wheez<strong>in</strong>g and a normal chest exam<strong>in</strong>ation do not exclude asthma.)<br />
History <strong>of</strong> any <strong>of</strong> the follow<strong>in</strong>g:<br />
Cough, worse particularly at night<br />
Recurrent wheeze<br />
Recurrent difficulty <strong>in</strong> breath<strong>in</strong>g<br />
Recurrent chest tightness<br />
Symptoms occur or worsen <strong>in</strong> the presence <strong>of</strong>:<br />
Exercise<br />
Viral <strong>in</strong>fection<br />
Animals with fur or hair<br />
House-dust mites (<strong>in</strong> mattresses, pillows, upholstered furniture, carpets)<br />
Mold<br />
Smoke (tobacco, wood)<br />
Pollen<br />
Changes <strong>in</strong> weather<br />
Strong emotional expression (laugh<strong>in</strong>g or cry<strong>in</strong>g hard)<br />
Airborne chemicals or dusts<br />
Menstrual cycles<br />
Symptoms occur or worsen at night, awaken<strong>in</strong>g the patient.<br />
Attachment 1<br />
*Eczema, hay fever or a family history <strong>of</strong> asthma or atopic diseases are <strong>of</strong>ten associated with asthma, but<br />
they are not key <strong>in</strong>dicators.<br />
(NAEPP 2007 [5a])<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 14 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
DIFFERENTIAL DIAGNOSTIC POSSIBILITIES FOR <strong>ASTHMA</strong><br />
Infants and Children<br />
Upper airway diseases<br />
Allergic rh<strong>in</strong>itis and s<strong>in</strong>usitis<br />
Adults<br />
Obstructions <strong>in</strong>volv<strong>in</strong>g large airways<br />
Foreign body <strong>in</strong> trachea or bronchus<br />
Vocal cord dysfunction<br />
Vascular r<strong>in</strong>gs or laryngeal webs<br />
Laryngotracheomalacia, tracheal stenosis, or bronchostenosis<br />
Enlarged lymph nodes or tumor<br />
Obstructions <strong>in</strong>volv<strong>in</strong>g small airways<br />
Viral bronchiolitis or obliterative bronchiolitis<br />
Cystic fibrosis<br />
Bronchopulmonary dysplasia<br />
Heart disease<br />
Attachment 2<br />
Other causes<br />
Diagnosed recurrent cough not due to asthma<br />
Aspiration from swallow<strong>in</strong>g mechanism dysfunction or gastroesophageal reflux<br />
COPD (e.g., chronic bronchitis or emphysema)<br />
Congestive heart failure<br />
Pulmonary embolism<br />
Mechanical obstruction <strong>of</strong> the airways (benign and malignant tumors)<br />
Pulmonary <strong>in</strong>filtration with eos<strong>in</strong>ophilia<br />
Cough secondary to drugs (e.g., angiotens<strong>in</strong>-convert<strong>in</strong>g enzyme (ACE) <strong>in</strong>hibitors)<br />
Vocal cord dysfunction<br />
(NAEPP 2007 [5a])<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 15 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Attachment 3<br />
Formal Evaluation <strong>of</strong> Asthma Exacerbation Severity <strong>in</strong> ED or Urgent Care Sett<strong>in</strong>g<br />
Mild Moderate<br />
Symptoms<br />
Severe Subset: Respiratory<br />
Arrest Imm<strong>in</strong>ent<br />
Breathlessness While walk<strong>in</strong>g<br />
Can lie down<br />
While at rest (<strong>in</strong>fant:<br />
s<strong>of</strong>ter, shorter cry,<br />
difficulty feed<strong>in</strong>g)<br />
Prefers sitt<strong>in</strong>g<br />
While at rest (<strong>in</strong>fant:<br />
stops feed<strong>in</strong>g)<br />
Sits upright<br />
While at rest<br />
Talks <strong>in</strong> Sentences Phrases Words Cannot talk<br />
Alertness Normal or may be<br />
agitated<br />
Usually agitated<br />
Signs<br />
Usually agitated Drowsy or confused<br />
Respiratory rate Normal or <strong>in</strong>creased Increased Increased, <strong>of</strong>ten<br />
>30/m<strong>in</strong>ute<br />
Normal or decreased<br />
Guide to rates <strong>of</strong> breath<strong>in</strong>g <strong>in</strong> awake <strong>children</strong>:<br />
Age Normal Rate<br />
< 2 months < 60/m<strong>in</strong>ute<br />
2 to 12 months < 50/m<strong>in</strong>ute<br />
1 to 5 years < 40/m<strong>in</strong>ute<br />
6 to 8 years < 30/m<strong>in</strong>ute<br />
Use <strong>of</strong> accessory muscles; Usually not Commonly Usually Paradoxical<br />
suprasternal retractions;<br />
thoracoabdom<strong>in</strong>al<br />
nasal flar<strong>in</strong>g; abdom<strong>in</strong>al<br />
breath<strong>in</strong>g<br />
movement<br />
Wheeze Moderate, <strong>of</strong>ten only Loud; throughout Loud, throughout M<strong>in</strong>imal or absent<br />
end expiratory exhalation<br />
<strong>in</strong>spiration and<br />
exhalation or may be<br />
absent<br />
Pulse/m<strong>in</strong>ute (at <strong>in</strong>itial<br />
presentation)<br />
< 100 100 to 120 > 120 Bradycardia<br />
Pulsus paradoxus Absent 25 mmHg (adult)<br />
20 to 40 mmHg (child)<br />
respiratory muscle fatigue<br />
Functional Assessment<br />
PEF (peak expiratory > 70% Approx. 40 to 69% or < 40% < 25%<br />
flow)<br />
Response to treatment<br />
Note: PEF test<strong>in</strong>g may not<br />
Percent predicted or<br />
lasts < 2 hours<br />
be needed <strong>in</strong> very severe<br />
percent personal best<br />
attacks<br />
PaO2 (arterial oxygen Normal (test not > 60 mmHg (test not < 60 mmHg: possible<br />
pressure, on room air)<br />
and/or<br />
usually necessary) usually necessary) cyanosis<br />
PCO2 (partial pressure <strong>of</strong> < 42 mmHg (test not < 42 mmHg (test not > 42 mmHg: possible<br />
carbon dioxide)<br />
usually necessary) usually necessary) respiratory failure<br />
SaO2 (oxygen saturation)<br />
(on room air)<br />
> 95% 90 to 95% < 90%<br />
at sea level Hypercapnia (hypoventilation) develops more easily <strong>in</strong> young <strong>children</strong> than<br />
<strong>in</strong> adolescents and adults.<br />
The presence <strong>of</strong> several parameters, but not necessarily all, <strong>in</strong>dicates the general classification <strong>of</strong> the <strong>exacerbation</strong><br />
Many <strong>of</strong> these parameters have not been systematically studied, especially as they correlate with each other and thus serve only as<br />
general guides<br />
Adapted from the National Heart Blood and Lung Institute, National Education and Prevention Program<br />
Expert Panel Report 3: Diagnosis and <strong>Management</strong> <strong>of</strong> Asthma, 2007 (LocalConsensus [5], NAEPP 2007 [5a]).<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 16 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Emergency Department <strong>Management</strong> <strong>of</strong> Asthma Exacerbations – Algorithm Attachment 4<br />
Initial Assessment: Brief History, physical exam<strong>in</strong>ation (auscultation, use <strong>of</strong> accessory muscles, heart rate, respiratory rate, pulse<br />
oximetry), PEF or FEV 1 (if performed), or Asthma score, oxygen saturation, and other tests as <strong>in</strong>dicated<br />
Mild: see Attachment 3 for<br />
details <strong>of</strong> signs and<br />
symptoms:<br />
Speaks <strong>in</strong> sentences<br />
Wheeze mild to moderate<br />
(end expiratory)<br />
Mild<br />
Oxygen to achieve SaO 2 > 90%<br />
Inhaled SABA by nebulizer or MDI<br />
with valved hold<strong>in</strong>g chamber, up to 3<br />
doses <strong>in</strong> 1 st hour<br />
Oral systemic corticosteroids if no<br />
response or if patient recently took oral<br />
systemic corticosteroids<br />
Moderate Exacerbation<br />
Asthma Score, PEF or FEV 1 (40 to 69%<br />
predicted/personal best)<br />
Inhaled SABA every 60 m<strong>in</strong>utes<br />
Oral systemic corticosteroids<br />
Cont<strong>in</strong>ue treatment 1 to 3 hours,<br />
provided there is improvement; make<br />
admit decision <strong>in</strong> < 4 hours<br />
Good Response<br />
Asthma Score, PEF or FEV 1<br />
(> 70%)<br />
Response susta<strong>in</strong>ed at least 60<br />
m<strong>in</strong>utes after last treatment<br />
No distress<br />
Physical exam: normal<br />
Moderate: see Attachment 3<br />
for details <strong>of</strong> signs and<br />
symptoms:<br />
Speaks <strong>in</strong> words<br />
Wheeze loud (throughout<br />
exhalation)<br />
Repeat Assessment: Symptoms, physical exam<strong>in</strong>ation, Asthma Score or PEF, FEV 1 (if performed), oxygen saturation, other tests as<br />
<strong>in</strong>dicated<br />
Discharge Home<br />
Cont<strong>in</strong>ue treatment with <strong>in</strong>haled SABAs.<br />
Cont<strong>in</strong>ue course <strong>of</strong> oral systemic<br />
corticosteroid.<br />
Cont<strong>in</strong>ue on ICS. For those not on long-term<br />
control therapy, consider <strong>in</strong>itiation <strong>of</strong> an ICS.<br />
Patient education (e.g., review medications<br />
<strong>in</strong>clud<strong>in</strong>g <strong>in</strong>haler technique; review/<strong>in</strong>itiate<br />
action plan; recommend close medical followup<br />
and, whenever possible, environmental<br />
control measures).<br />
Before discharge, schedule follow-up<br />
appo<strong>in</strong>tment with PCP and /or asthma<br />
specialist <strong>in</strong> 1-5 days.<br />
If unable to schedule from ED, notify PCP <strong>of</strong><br />
status<br />
Moderate / Severe<br />
Oxygen to achieve SaO 2 > 90%<br />
High-dose <strong>in</strong>haled SABA by nebulizer or<br />
MDI with valved hold<strong>in</strong>g chamber, every<br />
10 to 20 m<strong>in</strong>utes or cont<strong>in</strong>uously for 1<br />
hour PLUS ipratropium<br />
Oral systemic corticosteroids<br />
Incomplete Response<br />
Unchang<strong>in</strong>g Asthma Score,<br />
PEF or FEV 1 (40 – 69%)<br />
Symptoms persist<br />
Decide patient’s disposition<br />
Severe: see Attachment 3 for<br />
details <strong>of</strong> signs and symptoms:<br />
Speaks <strong>in</strong> phrases<br />
Wheeze loud (throughout<br />
<strong>in</strong>halation or exhalation) or<br />
absent<br />
Severe Exacerbation<br />
Asthma Score, PEF or FEV 1 (
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Severity Classification<br />
(NAEPP 2007 [5a])<br />
Attachment 5<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 18 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Severity Classification (cont<strong>in</strong>ued)<br />
(NAEPP 2007 [5a])<br />
Attachment 5<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 19 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
How to Use Your Metered-Dose Inhaler<br />
Attachment 7<br />
Us<strong>in</strong>g an <strong>in</strong>haler seems simple, but most people do not use it the right way. When an <strong>in</strong>haler is used the wrong<br />
way, less medic<strong>in</strong>e gets to the lungs. Use <strong>of</strong> a hold<strong>in</strong>g chamber/spacer <strong>in</strong>creases reliability <strong>of</strong> drug effectiveness,<br />
especially when <strong>in</strong>halers are not used correctly.<br />
For the next few days, read these steps aloud as you do them or ask someone to read them to you. Ask your<br />
primary care provider to check how well you/your child are us<strong>in</strong>g the <strong>in</strong>haler.<br />
Use the <strong>in</strong>haler <strong>in</strong> the way pictured below.<br />
Steps for us<strong>in</strong>g your <strong>in</strong>haler:<br />
Gett<strong>in</strong>g ready 1. Take <strong>of</strong>f the cap, shake the <strong>in</strong>haler and attach spacer<br />
2. Breathe out all the way.<br />
3. Hold the <strong>in</strong>haler the way <strong>in</strong>structed by your primary care provider (see picture).<br />
4. Press down on the <strong>in</strong>haler, with<strong>in</strong> 5 seconds, beg<strong>in</strong> to breathe <strong>in</strong> slowly through your<br />
mouth.<br />
5. Keep breath<strong>in</strong>g <strong>in</strong> slowly, as deeply as possible.<br />
6. Hold your breath and count to 10 slowly, if possible.<br />
7. Remove the <strong>in</strong>haler and breathe out through pursed lips (like blow<strong>in</strong>g out a candle)<br />
8. For <strong>in</strong>haled quick-relief medic<strong>in</strong>e (beta2-agonists), wait about 1 m<strong>in</strong>ute between puffs.<br />
There is no need to wait between puffs for other medic<strong>in</strong>es.<br />
Clean your <strong>in</strong>haler as needed, and know when to replace your <strong>in</strong>haler. For <strong>in</strong>structions, read the package <strong>in</strong>sert or<br />
talk to your primary care provider or pharmacist. It is important to refill your prescription before the medic<strong>in</strong>e<br />
runs out or the <strong>in</strong>haler expires to ensure medic<strong>in</strong>e is available when needed.<br />
Adapted from the National Heart Blood and Lung Institute, National Education and Prevention Program<br />
Expert Panel Report 3: Diagnosis and <strong>Management</strong> <strong>of</strong> Asthma, 2007 (Roller 2007 [4a], LocalConsensus [5], NAEPP 2007 [5a]).<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 22 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Peak Flow Use<br />
(NAEPP 2007 [5a])<br />
Attachment 8<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 23 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Peak Flow Use (cont<strong>in</strong>ued)<br />
(NAEPP 2007 [5a])<br />
Attachment 8<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 24 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Stepwise Approach<strong>in</strong>g to Manag<strong>in</strong>g Asthma <strong>in</strong> Children 0 to 4 years <strong>of</strong> age<br />
Attachment 9<br />
(NAEPP 2007 [5a])<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 25 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Stepwise Approach<strong>in</strong>g to Manag<strong>in</strong>g Asthma <strong>in</strong> Children 5 to 11 years <strong>of</strong> age<br />
Attachment 9<br />
(NAEPP 2007 [5a])<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 26 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Members <strong>of</strong> Asthma Team 2010<br />
Community Physicians<br />
Scott Callahan, MD, Co-Chair (General Pediatrics)<br />
William DeBuys, MD (General Pediatrics)<br />
CCHMC Physicians<br />
Carolyn Kercsmar, MD, Co-Chair (Allergy and Pulmonary<br />
Medic<strong>in</strong>e)<br />
Jeffrey Simmons, MD, Methodologist (General Pediatrics)<br />
*Michele Lierl, MD (Allergy and Pulmonary Medic<strong>in</strong>e)<br />
Craig Gosd<strong>in</strong>, MD (General Pediatrics)<br />
Laurie Johnson, MD (Emergency Medic<strong>in</strong>e)<br />
Sue Poynter, MD (Critical Care Medic<strong>in</strong>e)<br />
Rajit Basu, MD (Critical Care Medic<strong>in</strong>e)<br />
Residents<br />
Angela Statile, MD (Chief Resident)<br />
Corr<strong>in</strong>e Bria, MD (Chief Resident)<br />
Nurs<strong>in</strong>g<br />
Sue Wieser, RN<br />
Lisa Crosby, RN<br />
Pharmacy<br />
Bradley McCrory, PharmD<br />
Michelle Caruso, PharmD, BCPS<br />
Respiratory Therapy<br />
Edward Conway, RRT (Certified Asthma Educator)<br />
Lisa Devoto, RN, RT, CPN (Certified Asthma Educator)<br />
Rachel Keller, RRT, RPFT (Certified Asthma Educator)<br />
James M. Anderson Center (AC) - Support<br />
*Eloise Clark, MPH, MBA (Lead Program Adm<strong>in</strong>istrator)<br />
*Wendy Gerhardt, MSN, RN-BC (Program Adm<strong>in</strong>istrator)<br />
Danette Stanko-Lopp, MA, MPH (Epidemiologist)<br />
Karen Vonderhaar, RN, MSN (Program Adm<strong>in</strong>istrator)<br />
Ad hoc Advisors<br />
Lorie Ferenzi, (Allergy and Pulmonary Medic<strong>in</strong>e)<br />
*Richard Ruddy, MD (Director, Emergency Medic<strong>in</strong>e)<br />
*Amal Assa'ad, MD (Allergy)<br />
Karen McDowell, MD (Pulmonary Medic<strong>in</strong>e)<br />
Christopher J Cates, Division <strong>of</strong> Population Hlth Sci and Educ, St.<br />
George’s, U <strong>of</strong> London, UK<br />
Annie L<strong>in</strong>tzenich, MD, Gen Peds, Med U <strong>of</strong> SC<br />
Ronald J Teufel II, MD, MSCR, Pediatrics/Internal Medic<strong>in</strong>e, Gen<br />
Peds Hospital Section, Med U <strong>of</strong> SC<br />
*Member <strong>of</strong> 2002 Development Team<br />
Development Process<br />
The process by which this guidel<strong>in</strong>e was developed is documented <strong>in</strong><br />
the Guidel<strong>in</strong>e Development Process Manual; relevant development<br />
materials are kept electronically. The recommendations conta<strong>in</strong>ed <strong>in</strong><br />
this guidel<strong>in</strong>e were formulated by an <strong>in</strong>terdiscipl<strong>in</strong>ary work<strong>in</strong>g group<br />
which performed systematic search and critical appraisal <strong>of</strong> the<br />
literature, us<strong>in</strong>g the Table <strong>of</strong> Evidence Levels described follow<strong>in</strong>g the<br />
references, and exam<strong>in</strong>ed current local cl<strong>in</strong>ical practices.<br />
To select evidence for critical appraisal for this guidel<strong>in</strong>e, the<br />
Medl<strong>in</strong>e, EmBase and the Cochrane databases were searched for<br />
dates <strong>of</strong> January, 2002 to November, 2009 to generate an unref<strong>in</strong>ed,<br />
―comb<strong>in</strong>ed evidence‖ database us<strong>in</strong>g a search strategy focused on<br />
answer<strong>in</strong>g cl<strong>in</strong>ical questions relevant to <strong>acute</strong> <strong>exacerbation</strong> <strong>of</strong><br />
asthma and employ<strong>in</strong>g a comb<strong>in</strong>ation <strong>of</strong> Boolean search<strong>in</strong>g on<br />
human-<strong>in</strong>dexed thesaurus terms (MeSH head<strong>in</strong>gs us<strong>in</strong>g an OVID<br />
Medl<strong>in</strong>e <strong>in</strong>terface) and ―natural language‖ search<strong>in</strong>g on words <strong>in</strong><br />
the title, abstract, and <strong>in</strong>dex<strong>in</strong>g terms. The citations were reduced<br />
by: elim<strong>in</strong>at<strong>in</strong>g duplicates, review articles, non-English articles,<br />
and adult articles. The result<strong>in</strong>g abstracts were reviewed by a<br />
methodologist to elim<strong>in</strong>ate low quality and irrelevant citations.<br />
Dur<strong>in</strong>g the course <strong>of</strong> the guidel<strong>in</strong>e development, additional cl<strong>in</strong>ical<br />
questions were generated and subjected to the search process, and<br />
some relevant review articles were identified. September, 2002 was<br />
the last date for which literature was reviewed for the previous<br />
version <strong>of</strong> this guidel<strong>in</strong>e. The details <strong>of</strong> that review strategy are<br />
documented and ma<strong>in</strong>ta<strong>in</strong>ed <strong>in</strong> an asthma literature b<strong>in</strong>der.<br />
However, all previous citations were reviewed for appropriateness<br />
to this revision. Any new literature encountered for this October,<br />
2010 version was reviewed by two or more team members and then<br />
discussed as a team.<br />
Experience with the implementation <strong>of</strong> earlier publications <strong>of</strong> this<br />
guidel<strong>in</strong>e has provided learn<strong>in</strong>gs which have been <strong>in</strong>corporated <strong>in</strong>to<br />
this revision.<br />
Once the guidel<strong>in</strong>e has been <strong>in</strong> place for five years, a team<br />
reconvenes to explore the cont<strong>in</strong>ued validity <strong>of</strong> the guidel<strong>in</strong>e. This<br />
phase can be <strong>in</strong>itiated at any po<strong>in</strong>t that evidence <strong>in</strong>dicates a critical<br />
change is needed.<br />
The guidel<strong>in</strong>e was externally appraised by three reviewers us<strong>in</strong>g the<br />
AGREE <strong>in</strong>strument and the results by doma<strong>in</strong> are:<br />
• Scope and Purpose 100%<br />
• Stakeholder Involvement 86%<br />
• Rigor <strong>of</strong> Development 92%<br />
• Clarity and Presentation 97%<br />
• Applicability 74%<br />
• Editorial Independence 72%<br />
Recommendations have been formulated by a consensus process<br />
directed by best evidence, patient and family preference and<br />
cl<strong>in</strong>ical expertise. Dur<strong>in</strong>g formulation <strong>of</strong> these recommendations,<br />
the team members have rema<strong>in</strong>ed cognizant <strong>of</strong> controversies and<br />
disagreements over the management <strong>of</strong> these patients. They have<br />
tried to resolve controversial issues by consensus where possible<br />
and, when not possible, to <strong>of</strong>fer optional approaches to care <strong>in</strong> the<br />
form <strong>of</strong> <strong>in</strong>formation that <strong>in</strong>cludes best support<strong>in</strong>g evidence <strong>of</strong><br />
efficacy for alternative choices.<br />
The guidel<strong>in</strong>e has been reviewed and approved by cl<strong>in</strong>ical experts<br />
not <strong>in</strong>volved <strong>in</strong> the development process, distributed to senior<br />
management, and other parties as appropriate to their <strong>in</strong>tended<br />
purposes.<br />
The guidel<strong>in</strong>e was developed without external fund<strong>in</strong>g. All Team<br />
Members and AC Support staff listed, have declared whether they<br />
have any conflict <strong>of</strong> <strong>in</strong>terest and none were identified.<br />
Copies <strong>of</strong> this Evidence-based Care Guidel<strong>in</strong>e (EBCG) and any<br />
available implementation tools are available onl<strong>in</strong>e and may be<br />
distributed by any organization for the global purpose <strong>of</strong> improv<strong>in</strong>g<br />
child health outcomes. Website address:<br />
http://www.c<strong>in</strong>c<strong>in</strong>nati<strong>children</strong>s.org/svc/alpha/h/health-policy/evbased/default.htm<br />
Examples <strong>of</strong> approved uses <strong>of</strong> the EBCG <strong>in</strong>clude the follow<strong>in</strong>g:<br />
• copies may be provided to anyone <strong>in</strong>volved <strong>in</strong> the organization’s<br />
process for develop<strong>in</strong>g and implement<strong>in</strong>g evidence-based care<br />
guidel<strong>in</strong>es;<br />
• hyperl<strong>in</strong>ks to the CCHMC website may be placed on the<br />
organization’s website;<br />
• the EBCG may be adopted or adapted for use with<strong>in</strong> the<br />
organization, provided that CCHMC receives appropriate<br />
attribution on all written or electronic documents; and<br />
• copies may be provided to patients and the cl<strong>in</strong>icians who manage<br />
their care.<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 27 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Notification <strong>of</strong> CCHMC at HPCEInfo@cchmc.org for any EBCG, or<br />
its companion documents, adopted, adapted, implemented or<br />
hyperl<strong>in</strong>ked by the organization is appreciated.<br />
NOTE: These recommendations result from review <strong>of</strong><br />
literature and practices current at the time <strong>of</strong> their<br />
formulations. This guidel<strong>in</strong>e does not preclude us<strong>in</strong>g care<br />
modalities proven efficacious <strong>in</strong> studies published subsequent to<br />
the current revision <strong>of</strong> this document. This document is not<br />
<strong>in</strong>tended to impose standards <strong>of</strong> care prevent<strong>in</strong>g selective<br />
variances from the recommendations to meet the specific and<br />
unique requirements <strong>of</strong> <strong>in</strong>dividual patients. Adherence to this<br />
guidel<strong>in</strong>e is voluntary. The cl<strong>in</strong>ician <strong>in</strong> light <strong>of</strong> the <strong>in</strong>dividual<br />
circumstances presented by the patient must make the ultimate<br />
judgment regard<strong>in</strong>g the priority <strong>of</strong> any specific procedure.<br />
For more <strong>in</strong>formation about this guidel<strong>in</strong>e, its support<strong>in</strong>g<br />
evidences and the guidel<strong>in</strong>e development process, contact the AC<br />
<strong>of</strong>fice at: 513-636-2501 or HPCEInfo@cchmc.org .<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 28 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
References<br />
Note: When us<strong>in</strong>g the electronic version <strong>of</strong> this document, �<br />
<strong>in</strong>dicates a hyperl<strong>in</strong>k to the PubMed abstract. A hyperl<strong>in</strong>k<br />
follow<strong>in</strong>g this symbol goes to the article PDF when the user is<br />
with<strong>in</strong> the CCHMC network<br />
1. Ak<strong>in</strong>bami, L. J.; Moorman, J. E.; Garbe, P. L.; and<br />
Sondik, E. J.: Status <strong>of</strong> childhood asthma <strong>in</strong> the United<br />
States, 1980-2007. Pediatrics, 123 Suppl 3: S131-45,<br />
2009, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd =Retrieve&db=PubMed&dopt=Citation&list_uids=19221156 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaA k<strong>in</strong>bami2009.pdf.<br />
2. Allcock, D.: Us<strong>in</strong>g a community respiratory service to reduce<br />
<strong>children</strong>'s hospital admissions. Nurs<strong>in</strong>g Times, 105(4):<br />
22-3, 2009, [4b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19263772 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaAllcock2009.pdf.<br />
3. Altamimi, S.; Robertson, G.; Jastaniah, W.; Davey, A.;<br />
Dehghani, N.; Chen, R.; Leung, K.; and Colbourne,<br />
M.: S<strong>in</strong>gle-dose oral dexamethasone <strong>in</strong> the emergency<br />
management <strong>of</strong> <strong>children</strong> with <strong>exacerbation</strong>s <strong>of</strong> mild to<br />
moderate asthma. Pediatric Emergency Care, 22(12):<br />
786-93, 2006, [2a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE =fulltext&A N=17198210&D =medl � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_A sthma/AsthmaAltam<strong>in</strong>i2006.PDF.<br />
4. Alter, H. J.; Koepsell, T. D.; and Hilty, W. M.: Intravenous<br />
magnesium as an adjuvant <strong>in</strong> <strong>acute</strong> bronchospasm: a<br />
meta-analysis. Annals <strong>of</strong> Emergency Medic<strong>in</strong>e, 36(3):<br />
191-7, 2000, [1a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEW S=N&PAG E=fulltext&AN=10969219&D=med4 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaAlter2000.pdf.<br />
5. Altunc, U.; Pittler, M. H.; and Ernst, E.: Homeopathy for<br />
childhood and adolescence ailments: systematic review<br />
<strong>of</strong> randomized cl<strong>in</strong>ical trials. Mayo Cl<strong>in</strong>ic Proceed<strong>in</strong>gs,<br />
82(1): 69-75, 2007, [1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Cita tion&list_uids=17285788 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaAltunc2007.pdf.<br />
6. Andrews, T.; McG<strong>in</strong>tee, E.; Mittal, M. K.; Tyler, L.;<br />
Chew, A.; Zhang, X.; Pawlowski, N.; and Zorc, J. J.:<br />
High-dose cont<strong>in</strong>uous nebulized levalbuterol for pediatric<br />
status asthmaticus: a randomized trial. Journal <strong>of</strong><br />
Pediatrics, 155(2): 205-10.e1, 2009, [2b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19464028 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaAndrews2009.PDF.<br />
7. Arshad, S. H.; Bateman, B.; Sadeghnejad, A.; Gant, C.;<br />
and Matthews, S. M.: Prevention <strong>of</strong> allergic disease<br />
dur<strong>in</strong>g childhood by allergen avoidance: the Isle <strong>of</strong> Wight<br />
prevention study. Journal <strong>of</strong> Allergy & Cl<strong>in</strong>ical<br />
Immunology, 119(2): 307-13, 2007, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17291851 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaArshad2007.pdf.<br />
8. Bartlett, S. J., Kolodner, Kenneth, Butz, Arlene M,<br />
Eggeston Peyton, Malveaux, Floyd J, Rand, Cynthia<br />
S: Maternal Depressive Symptoms and Emergency<br />
Department Use Among Innere-city Children with<br />
Asthma Archives <strong>of</strong> Pediatrics & Adolescent Medic<strong>in</strong>e,<br />
155: 347-353, 2001, [3a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11231800 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_A sthma/AsthmaBartlett2001.pdf.<br />
9. Belamarich: Do Obeses Inner-City Children with Asthma<br />
have more Symptoms than Nonobese Children with<br />
Asthma? Pediatrics, 106(6): 1436-1441, 2000, [3a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=11099600 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaBelamarich2000.pdf.<br />
10. Bender, B.; Wamboldt, F. S.; O'Connor, S. L.; Rand, C.;<br />
Szefler, S.; Milgrom, H.; and Wamboldt, M. Z.:<br />
Measurement <strong>of</strong> <strong>children</strong>'s asthma medication adherence<br />
by self report, mother report, canister weight, and Doser<br />
CT. Annals <strong>of</strong> Allergy, Asthma, & Immunology, 85(5):<br />
416-21, 2000, [3b] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE =fulltext&A N=11101187&D =med4 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaBender2000.pdf.<br />
11. Benito-Fernandez, J.; Gonzalez-Balenciaga, M.; Capape-<br />
Zache, S.; Vazquez-Ronco, M. A.; and M<strong>in</strong>tegi-Raso,<br />
S.: Salbutamol via metered-dose <strong>in</strong>haler with spacer<br />
versus nebulization for <strong>acute</strong> treatment <strong>of</strong> pediatric<br />
asthma <strong>in</strong> the emergency department. Pediatric<br />
Emergency Care, 20(10): 656-9, 2004, [3a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15454738<br />
� http://groups/p2/EBC_Files/Ar<br />
ticles_Cited_<strong>in</strong>_Asthma/AsthmaBenito- Fernandez2004.pdf.<br />
12. Bhogal, S.; Zemek, R.; and Ducharme, F. M.: Written<br />
action plans for asthma <strong>in</strong> <strong>children</strong>. Cochrane Database<br />
<strong>of</strong> Systematic Reviews, 3: CD005306, 2006, [1a]<br />
http://www.ncbi.nlm.n ih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=16856090 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaBhogal2006.pdf.<br />
13. Blasi, F., and Johnston, S. L.: The role <strong>of</strong> antibiotics <strong>in</strong><br />
asthma. International Journal <strong>of</strong> Antimicrobial Agents,<br />
29(5): 485-93, 2007, [5b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P<br />
ubMed&dopt=Citation&list_uids=17353114 � http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaBlasi2007.pdf.<br />
14. Blitz, M.; Blitz, S.; Beasely, R.; D<strong>in</strong>er, B.; Hughes, R.;<br />
Knopp, J. A.; and Rowe, B. H.: Inhaled magnesium<br />
sulfate <strong>in</strong> the treatment <strong>of</strong> <strong>acute</strong> asthma. Cochrane<br />
Database <strong>of</strong> Systematic Reviews, (4), 2009, [1b]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=15846687 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaBlitz2009.pdf.<br />
15. Boychuk, R. B. et al.: Change <strong>in</strong> approach and delivery <strong>of</strong><br />
medical care <strong>in</strong> <strong>children</strong> with asthma: results from a<br />
multicenter emergency department educational asthma<br />
management program. Pediatrics, 117(4 Pt 2): S145-51,<br />
2006, [3a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16777830 � http://groups/ce/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma_ED/AsthmaBoychuk2006.pdf.<br />
16. Boyd, M.; Lasserson, T. J.; McKean, M. C.; Gibson, P. G.;<br />
Ducharme, F. M.; and Haby, M.: Interventions for<br />
educat<strong>in</strong>g <strong>children</strong> who are at risk <strong>of</strong> asthma-related<br />
emergency department attendance.[update <strong>of</strong> Cochrane<br />
Database Syst Rev. 2001;(1):CD001290; PMID:<br />
11279713]. Cochrane Database <strong>of</strong> Systematic Reviews,<br />
(2): CD001290, 2009, [1a] http://www.ncbi.nlm<br />
.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19370563 � http://groups/ce/EBC_Files/Ar<br />
ticles_Cited_<strong>in</strong>_Asthma_ED/AsthmaBoyd2009.pdf.<br />
17. Boyd, R., and Stuart, P.: Pressurised metered dose <strong>in</strong>halers<br />
with spacers versus nebulisers for beta-agonist delivery <strong>in</strong><br />
<strong>acute</strong> asthma <strong>in</strong> <strong>children</strong> <strong>in</strong> the emergency department.<br />
Emergency Medic<strong>in</strong>e Journal, 22(9): 641-2, 2005, [3a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=16113185 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaBoyd2005.pdf.<br />
18. Brand, P., Duiverman, EJ, Waalkens, HJ, vanEssen-<br />
Zandvliet, EEM, Kerrbijn, KF, & the Dutch CNSLD<br />
Study Group: Peak flow variation <strong>in</strong> childhood asthma:<br />
correlation with symptoms, airways obstruction, and<br />
hyperresponsiveness dur<strong>in</strong>g long term treatment with<br />
<strong>in</strong>haled corticosteroids. Thorax, 54: 103-107, 1999, [4a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retr ieve&db=P ubMed&dopt=Citation&list_uids=10325912 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaBrand1999.pdf.<br />
19. Brown, M. D.; Reeves, M. J.; Meyerson, K.; and<br />
Korzeniewski, S. J.: Randomized trial <strong>of</strong> a<br />
comprehensive asthma education program after an<br />
emergency department visit.[see comment]. Annals <strong>of</strong><br />
Allergy, Asthma, & Immunology, 97(1): 44-51, 2006,<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 29 <strong>of</strong> 36<br />
[2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16892780<br />
http://groups/ce/E<br />
�<br />
20. Camargo, C. A., Jr.; Rachelefsky, G.; and Schatz, M.:<br />
Manag<strong>in</strong>g asthma <strong>exacerbation</strong>s <strong>in</strong> the emergency<br />
department: summary <strong>of</strong> the National Asthma Education<br />
and Prevention Program Expert Panel Report 3 guidel<strong>in</strong>es<br />
for the management <strong>of</strong> asthma <strong>exacerbation</strong>s. Journal <strong>of</strong><br />
Emergency Medic<strong>in</strong>e, 37(2 Suppl): S6-S17, 2009, [5b]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=19683665 � http://groups/p2/EBC_Files/Articles_Cited_<br />
<strong>in</strong>_Asthma/AsthmaCamargo2009.pdf.<br />
BC_Files/Articles_Cited_<strong>in</strong>_A sthma_ED/AsthmaBrown2006.pdf.<br />
21. Can<strong>in</strong>o, G.; Vila, D.; Normand, S.-L. T.; Acosta-Perez, E.;<br />
Ramirez, R.; Garcia, P.; and Rand, C.: Reduc<strong>in</strong>g<br />
asthma health disparities <strong>in</strong> poor Puerto Rican <strong>children</strong>:<br />
the effectiveness <strong>of</strong> a culturally tailored family<br />
<strong>in</strong>tervention. Journal <strong>of</strong> Allergy & Cl<strong>in</strong>ical Immunology,<br />
121(3): 665-70, 2008, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18061648 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_A sthma/AsthmaCan<strong>in</strong>o2008.pdf.<br />
22. Carl, J. C.; Myers, T. R.; Kirchner, H. L.; and Kercsmar,<br />
C. M.: Comparison <strong>of</strong> racemic albuterol and levalbuterol<br />
for treatment <strong>of</strong> <strong>acute</strong> asthma. Journal <strong>of</strong> Pediatrics,<br />
143(6): 731-6, 2003, [2a] http://ovidsp.ovid.com /ovidweb.cgi?T=JS&NEWS=N&PAGE =fullte xt&AN=14657817&D=med4 � http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaCarl2003.pdf.<br />
23. Castro-Rodriguez, J. A., and Rodrigo, G. J.: beta-agonists<br />
through metered-dose <strong>in</strong>haler with valved hold<strong>in</strong>g<br />
chamber versus nebulizer for <strong>acute</strong> <strong>exacerbation</strong> <strong>of</strong><br />
wheez<strong>in</strong>g or asthma <strong>in</strong> <strong>children</strong> under 5 years <strong>of</strong> age: a<br />
systematic review with meta-analysis. Journal <strong>of</strong><br />
Pediatrics, 145(2): 172-7, 2004, [1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=15289762 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaCastro-Rodr iquez2004.pdf.
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
24. Cates, C. J.; Crilly, J. A.; and Rowe, B. H.: Hold<strong>in</strong>g<br />
chambers (spacers) versus nebulisers for beta-agonist<br />
treatment <strong>of</strong> <strong>acute</strong> asthma.[update <strong>of</strong> Cochrane Database<br />
Syst Rev. 2003;(3):CD000052; PMID: 12917881].<br />
Cochrane Database <strong>of</strong> Systematic Reviews, (2):<br />
CD000052, 2006, [1a] http://www.ncbi.nlm<br />
.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16625527 � http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_A sthma/AsthmaCates2006.pdf.<br />
25. Cates, C. J.; Lasserson, T. J.; and Jaeschke, R.: Regular<br />
treatment with formoterol and <strong>in</strong>haled steroids for<br />
chronic asthma: serious adverse events. Cochrane<br />
Database <strong>of</strong> Systematic Reviews, (2): CD006924, 2009a,<br />
[1a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEW S=N&PAG E=fulltext&AN=19370661&D=medl � http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_A sthma/AsthmaCates2009a.pdf.<br />
26. Cates, C. J.; Lasserson, T. J.; and Jaeschke, R.: Regular<br />
treatment with salmeterol and <strong>in</strong>haled steroids for chronic<br />
asthma: serious adverse events. Cochrane Database <strong>of</strong><br />
Systematic Reviews, (3): CD006922, 2009b, [1a]<br />
http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE =fulltext&AN=19588410&D=medl � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaCates2009b.pdf.<br />
27. Chan-Yeung, M., Ferguson, Alexander, Dimich-Ward,<br />
Helen, Watson, Wade, Manfreda, Jure, Becker, Allan:<br />
Effectiveness <strong>of</strong> and compliance to <strong>in</strong>tervention measures<br />
<strong>in</strong> reduc<strong>in</strong>g house dust and cat allergen levels Anals <strong>of</strong><br />
Allergy and Immunology 88: 52-58, 2002, [2a] �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaChan-Yeng2002.pdf.<br />
28. Chang, A. B.; Clark, R.; Sloots, T. P.; Stone, D. G.; Petsky,<br />
H. L.; Thearle, D.; Champion, A. A.; Wheeler, C.;<br />
and Acworth, J. P.: A 5- versus 3-day course <strong>of</strong> oral<br />
corticosteroids for <strong>children</strong> with asthma <strong>exacerbation</strong>s<br />
who are not hospitalised: a randomised controlled trial.<br />
Medical Journal <strong>of</strong> Australia, 189(6): 306-10, 2008, [2a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=18803532 � http://groups/ce/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma_ED/AsthmaChang2008.pdf.<br />
29. Ciarallo, L.; Brousseau, D.; and Re<strong>in</strong>ert, S.: Higher-dose<br />
<strong>in</strong>travenous magnesium therapy for <strong>children</strong> with<br />
moderate to severe <strong>acute</strong> asthma. Archives <strong>of</strong> Pediatrics<br />
& Adolescent Medic<strong>in</strong>e, 154(10): 979-83, 2000, [2b]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=11030848 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaCiarallo2000.PDF.<br />
30. CMSA: Case <strong>Management</strong> Society <strong>of</strong> America<br />
http://www.cmsa.org/, 2010, [5] �.<br />
31. C<strong>of</strong>fman, J. M.; Cabana, M. D.; Halp<strong>in</strong>, H. A.; and Yel<strong>in</strong>,<br />
E. H.: Effects <strong>of</strong> asthma education on <strong>children</strong>'s use <strong>of</strong><br />
<strong>acute</strong> care services: a meta-analysis. Pediatrics, 121(3):<br />
575-86, 2008, [1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18310208 � http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaC<strong>of</strong>fman2008.pdf.<br />
32. Cooper, W. O., Hickson, Gerald B: Corticsteroid<br />
Prescription Fill<strong>in</strong>g for Children Covered by Medicaid<br />
Follow<strong>in</strong>g an Emergency Department Visit or a<br />
Hospitalization for Asthma Archives <strong>of</strong> Pediatric<br />
Adolescent Medic<strong>in</strong>e, 155: 1111-1115, 2001, [4a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=11576005 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaCooper2001.pdf.<br />
33. Cope, S. F.; Ungar, W. J.; and Glazier, R. H.:<br />
Socioeconomic factors and asthma control <strong>in</strong> <strong>children</strong>.<br />
Pediatric Pulmonology, 43(8): 745-52, 2008, [4a]<br />
http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE =fulltext&AN=18615669&D=medl � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaCope2008.PDF.<br />
34. Coughlan, J., Gibson, PG, Henry RL Medical Treatment for<br />
reflux oesophaitis doesnot consistently improve asthma<br />
control: a systematic review. Thorax, 56: 198-204, 2001,<br />
[1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11182012<br />
http://groups/p2/E<br />
�<br />
35. Custovic, A., Simpson, Bridget M, SImpson, Angela,<br />
Kissen, Patricia, Woodcock, Ashley: Effect <strong>of</strong><br />
Environmental Manipulation <strong>in</strong> Pregnancy and early Life<br />
on Respiratory Symptoms, and Atopy Dur<strong>in</strong>g First Year<br />
<strong>of</strong> Life: a Randomized Trial. Lancet, 358: 188-193, 2001,<br />
[2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11476835<br />
http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaCoughlan2001.pdf.<br />
�<br />
36. D'Avila, R. S.; Piva, J. P.; Marostica, P. J. C.; and<br />
Amantea, S. L.: Early adm<strong>in</strong>istration <strong>of</strong> two <strong>in</strong>travenous<br />
bolus <strong>of</strong> am<strong>in</strong>ophyll<strong>in</strong>e added to the standard treatment <strong>of</strong><br />
<strong>children</strong> with <strong>acute</strong> asthma. Respiratory Medic<strong>in</strong>e,<br />
102(1): 156-61, 2008, [2b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17869497 � http://groups/ce/E BC_Files/Articles_Cited_<strong>in</strong>_A sthma_ED/AsthmaD'Avila2008.pdf.<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaCustovic2001.pdf.<br />
37. Debley, J. S.; Carter, E. R.; Gibson, R. L.; Rosenfeld, M.;<br />
and Redd<strong>in</strong>g, G. J.: The prevalence <strong>of</strong> ibupr<strong>of</strong>ensensitive<br />
asthma <strong>in</strong> <strong>children</strong>: a randomized controlled<br />
bronchoprovocation challenge study.[see comment].<br />
Journal <strong>of</strong> Pediatrics, 147(2): 233-8, 2005, [1a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=16126056 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaDebley2005.pdf.<br />
38. Deerojanawong, J.; Manuyakorn, W.; Prapphal, N.;<br />
Harnruthakorn, C.; Sritippayawan, S.; and<br />
Samransamruajkit, R.: Randomized controlled trial <strong>of</strong><br />
salbutamol aerosol therapy via metered dose <strong>in</strong>halerspacer<br />
vs. jet nebulizer <strong>in</strong> young <strong>children</strong> with wheez<strong>in</strong>g.<br />
Pediatric Pulmonology, 39(5): 466-72, 2005, [2b]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=15786440 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaDeerojanawong2005.pdf.<br />
39. Delgado, A.; Chou, K. J.; Silver, E. J.; and Cra<strong>in</strong>, E. F.:<br />
Nebulizers vs metered-dose <strong>in</strong>halers with spacers for<br />
bronchodilator therapy to treat wheez<strong>in</strong>g <strong>in</strong> <strong>children</strong> aged<br />
2 to 24 months <strong>in</strong> a pediatric emergency department.<br />
Archives <strong>of</strong> Pediatrics & Adolescent Medic<strong>in</strong>e, 157(1):<br />
76-80, 2003, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12517199 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaDelgado2003.pdf.<br />
40. Dell, S. D.; Foty, R.; Becker, A.; Franssen, E.; and<br />
Chapman, K. R.: Parent-reported symptoms may not be<br />
adequate to def<strong>in</strong>e asthma control <strong>in</strong> <strong>children</strong>. Pediatric<br />
Pulmonology, 42(12): 1117-24, 2007, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17960807<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 30 <strong>of</strong> 36<br />
� http://groups/p2/EBC_Files/Ar<br />
ticles_Cited_<strong>in</strong>_Asthma/AsthmaDell2007.pdf.<br />
41. Dolovich, M. B. et al.: Device selection and outcomes <strong>of</strong><br />
aerosol therapy: Evidence-based guidel<strong>in</strong>es: American<br />
College <strong>of</strong> Chest Physicians/American College <strong>of</strong><br />
Asthma, Allergy, and Immunology. Chest, 127(1): 335-<br />
71, 2005, [1a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEW<br />
S=N&PAG E=fulltext&AN=15654001&D =med4 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_A<br />
sthma/AsthmaDolovich2005.pdf.<br />
42. Dotson, K. M. D.; Dallman, M. M. D.; Bowman, C. M. M.<br />
D.; and Titus, M. O. M. D.: Ipratropium Bromide for<br />
Acute Asthma Exacerbations <strong>in</strong> the Emergency Sett<strong>in</strong>g:<br />
A Literature Review <strong>of</strong> the Evidence. Pediatric<br />
Emergency Care, 25(10): 687-692, 2009, [1b] http://ovidsp.ovid.com /ovidweb.cgi?T=JS&NEWS=N&PAGE =fulltext&A N=00006565-<br />
200910000-00018&D=ovftjV NOvid TechnologiesD BJournals@Ovid � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaDotson2009.PDF.<br />
43. Douglas, J., Aroni, R, Oeman, D, Stewart, K, Sawyer, S,<br />
Thien, F: A Qualitative Study <strong>of</strong> Asction Plans for<br />
Asthma British Medical Journal, 324, 2002, [2b] �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaDouglass2002.pdf.<br />
44. Dozier, A.; Aligne, C. A.; and Schlabach, M. B.: What is<br />
asthma control? Discrepancies between parents'<br />
perceptions and <strong>of</strong>ficial def<strong>in</strong>itions. Journal <strong>of</strong> School<br />
Health, 76(6): 215-8, 2006, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16918841 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaDozier2006.pdf.<br />
45. Ebb<strong>in</strong>ghaus, S., and Bahra<strong>in</strong>wala, A. H.: Asthma<br />
management by an <strong>in</strong>patient asthma care team. Pediatric<br />
Nurs<strong>in</strong>g, 29(3): 177-83, 2003, [4b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=12836993 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaEb<strong>in</strong>ghaus2003.pdf.<br />
46. Edmonds, M.; Camargo, C. A.; Pollack, C. V.; and Rowe,<br />
B. H.: Early use <strong>of</strong> <strong>in</strong>haled corticosteroids <strong>in</strong> the<br />
emergency department treatment <strong>of</strong> <strong>acute</strong> asthma.<br />
Cochrane Database <strong>of</strong> Systematic Reviews, (4), 2009,<br />
[1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12917930<br />
http://groups/ce/E<br />
�<br />
47. FDA: New Safety Controls for Long-Act<strong>in</strong>g Beta Agonists,<br />
Medications used to Treat Asthma - News Release.<br />
www.fda.gov/drugs/DrugSafety/InformationbyDrugClass<br />
/ucm199565.htm, 2010, [5] � .<br />
48. Ferris, T. G., Cra<strong>in</strong>, Ellen F, Oken, Emily, Wang, L<strong>in</strong>da,<br />
Clark, Sunday, Camargo, Carlos A, : Insurance and<br />
Quality <strong>of</strong> Care for Children with Acutre Asthma<br />
Ambulatory Pediatrics 1(5): 267-274, 2001, [4a]<br />
BC_Files/Articles_Cited_<strong>in</strong>_A sthma_ED/AsthmaEdmonds2009.pdf.<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=11888414 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaFerris2001.pdf.
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
49. Ferris, T. G.; Kuhlthau, K.; Ausiello, J.; Perr<strong>in</strong>, J.; and<br />
Kahn, R.: Are m<strong>in</strong>ority <strong>children</strong> the last to benefit from<br />
a new technology? Technology diffusion and <strong>in</strong>haled<br />
corticosteriods for asthma. Medical Care, 44(1): 81-6,<br />
2006, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16365616 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaFerris2006.pdf.<br />
50. F<strong>in</strong>n, P. W., Boudreau, Jacques O, Hongzhen, BS,<br />
Yunsheng, Wang, Champman, MArt<strong>in</strong> D, V<strong>in</strong>cent,<br />
Carey, Burge, Harriet A, Weiss, Scott T, Perk<strong>in</strong>s,<br />
David L, Gold, Diane R: Children at Risk for Asthma:<br />
Home Allergen Levels, Lymphocyte Proliferation, and<br />
Wheeze. Journal <strong>of</strong> Allergy & Cl<strong>in</strong>ical Immunology, 105:<br />
933-942, 2000, [3a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=10808174 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaF<strong>in</strong>n2000.pdf.<br />
51. Flores, G.; Abreu, M.; Tomany-Korman, S.; and Meurer,<br />
J.: Keep<strong>in</strong>g <strong>children</strong> with asthma out <strong>of</strong> hospitals:<br />
parents' and physicians' perspectives on how pediatric<br />
asthma hospitalizations can be prevented. Pediatrics,<br />
116(4): 957-65, 2005, [3a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16199708 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_A sthma/AsthmaFlores2005.PDF.<br />
52. Forbis, S., Aligne, CA Poor Readability <strong>of</strong> Written Asthma<br />
<strong>Management</strong> Plans Found <strong>in</strong> National Guidel<strong>in</strong>es.<br />
Pediatrics, 109(4), 2002, [2b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11927725 � http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaForbis2002.pdf.<br />
53. Garbutt, J.; Highste<strong>in</strong>, G.; Nelson, K. A.; Rivera-Spoljaric,<br />
K.; and Strunk, R.: Detection and home management <strong>of</strong><br />
worsen<strong>in</strong>g asthma symptoms. Annals <strong>of</strong> Allergy, Asthma,<br />
& Immunology, 103(6): 469-73, 2009, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=20084839<br />
� http://groups/p2/EBC_Files/Ar<br />
ticles_Cited_<strong>in</strong>_Asthma/AsthmaGarbutt2009.pdf.<br />
54. Geelhoed, G. L. L., ; Le Souef, PN: Evaluation <strong>of</strong> SaO2 as a<br />
predictor <strong>of</strong> outcome <strong>in</strong> 280 <strong>children</strong> present<strong>in</strong>g with<br />
<strong>acute</strong> asthma Annals <strong>of</strong> Emergency Medic<strong>in</strong>e 23(6):<br />
1236-41, 1994, [3a] � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaGeelhood1994.pdf.<br />
55. G<strong>in</strong>de, A. A.; Esp<strong>in</strong>ola, J. A.; and Camargo, C. A., Jr.:<br />
Improved overall trends but persistent racial disparities <strong>in</strong><br />
emergency department visits for <strong>acute</strong> asthma, 1993-<br />
2005.[see comment]. Journal <strong>of</strong> Allergy & Cl<strong>in</strong>ical<br />
Immunology, 122(2): 313-8, 2008, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18538382 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaG<strong>in</strong>de2008.pdf.<br />
56. Goldberg, S., Spr<strong>in</strong>ger, C, Avital, A, GOdfrey, S, Bar-<br />
Yishay, E: Can Peak Expiratory Flow Measurmenets<br />
Estimate Small Airway Function <strong>in</strong> Asthmatic Children?<br />
. Chest, 120: 482-488, 2001, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11502647 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma.<br />
57. Gordon, S.; Tompk<strong>in</strong>s, T.; and Dayan, P. S.: Randomized<br />
trial <strong>of</strong> s<strong>in</strong>gle-dose <strong>in</strong>tramuscular dexamethasone<br />
compared with prednisolone for <strong>children</strong> with <strong>acute</strong><br />
asthma. Pediatric Emergency Care, 23(8): 521-7, 2007,<br />
[2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17726409<br />
http://groups/p2/E<br />
�<br />
58. Gorelick, M. H.; Stevens, M. W.; Schultz, T.; and<br />
Scribano, P. V.: Difficulty <strong>in</strong> obta<strong>in</strong><strong>in</strong>g peak expiratory<br />
flow measurements <strong>in</strong> <strong>children</strong> with <strong>acute</strong> asthma.<br />
Pediatric Emergency Care, 20(1): 22-6, 2004, [3a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=14716161 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaGorelick2004.pdf.<br />
59. Graham, V.; Lasserson, T. J.; and Rowe, B. H.: Antibiotics<br />
for <strong>acute</strong> asthma. Cochrane Database <strong>of</strong> Systematic<br />
Reviews, (4), 2009, [1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11687022 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaGraham2009.pdf.<br />
60. Greenberg, R. A.; Kerby, G.; and Roosevelt, G. E.: A<br />
comparison <strong>of</strong> oral dexamethasone with oral prednisone<br />
<strong>in</strong> pediatric asthma <strong>exacerbation</strong>s treated <strong>in</strong> the<br />
emergency department. Cl<strong>in</strong>ical Pediatrics, 47(8): 817-<br />
23, 2008, [2b] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEW S=N&PAG E=fulltext&D=medl&A N=18467673 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_A sthma_ED/AsthmaGreenberg2008.pdf.<br />
61. Gries, D. M.; M<strong>of</strong>fitt, D. R.; Pulos, E.; and Carter, E. R.: A<br />
s<strong>in</strong>gle dose <strong>of</strong> <strong>in</strong>tramuscularly adm<strong>in</strong>istered<br />
dexamethasone acetate is as effective as oral prednisone<br />
to treat asthma <strong>exacerbation</strong>s <strong>in</strong> young <strong>children</strong>. Journal<br />
<strong>of</strong> Pediatrics, 136(3): 298-303, 2000, [2b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation& list_uids=10700684<br />
� http://groups/p2/EBC_Files/Ar<br />
ticles_Cited_<strong>in</strong>_Asthma/AsthmaGries2007.PDF.<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaGordon2007.pdf.<br />
62. Griffiths, C. et al.: Specialist nurse <strong>in</strong>tervention to reduce<br />
unscheduled asthma care <strong>in</strong> a deprived multiethnic area:<br />
the east London randomised controlled trial for high risk<br />
asthma (ELECTRA). British Medical Journal,<br />
328(7432): 144, 2004, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=14718266 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaGriffiths2004.pdf.<br />
63. Gupta, M. K., and S<strong>in</strong>gh, M.: Evidence based review on<br />
levosalbutamol. Indian Journal <strong>of</strong> Pediatrics, 74(2): 161-<br />
7, 2007, [1b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17337829 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_A sthma/AsthmaGupta2007.PDF.<br />
64. Gupta, R. S.; Carrion-Carire, V.; and Weiss, K. B.: The<br />
widen<strong>in</strong>g black/white gap <strong>in</strong> asthma hospitalizations and<br />
mortality. Journal <strong>of</strong> Allergy & Cl<strong>in</strong>ical Immunology,<br />
117(2): 351-8, 2006, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=16461136 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaGupta;Carrion2006.pdf.<br />
65. Halterman, J. S.; McConnochie, K. M.; Conn, K. M.;<br />
Yoos, H. L.; Kaczorowski, J. M.; Holzhauer, R. J.;<br />
Allan, M.; and Szilagyi, P. G.: A potential pitfall <strong>in</strong><br />
provider assessments <strong>of</strong> the quality <strong>of</strong> asthma control.<br />
Ambulatory Pediatrics, 3(2): 102-5, 2003, [4a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=12643784 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma.<br />
66. Hardasmalani, M. D.; DeBari, V.; Bithoney, W. G.; and<br />
Gold, N.: Levalbuterol versus racemic albuterol <strong>in</strong> the<br />
treatment <strong>of</strong> <strong>acute</strong> <strong>exacerbation</strong> <strong>of</strong> asthma <strong>in</strong> <strong>children</strong>.<br />
Pediatric Emergency Care, 21(7): 415-9, 2005, [2b]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=16027572 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaHardasmalani2005.PDF.<br />
67. Hayday, K., and Stevermer, J. J.: In <strong>children</strong> hospitalized<br />
for asthma <strong>exacerbation</strong>s, does add<strong>in</strong>g ipratropium<br />
bromide to albuterol and corticosteroids improve<br />
outcome? Journal <strong>of</strong> Family Practice, 51(3): 280, 2002,<br />
[5a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEW S=N&PAG E=fulltext&AN=11978242&D=med4 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaHayday2001.PDF.<br />
68. Hondras, M. A.; L<strong>in</strong>de, K.; and Jones, A. P.: Manual<br />
therapy for asthma.[update <strong>of</strong> Cochrane Database Syst<br />
Rev. 2002;(4):CD001002; PMID: 12519548]. Cochrane<br />
Database <strong>of</strong> Systematic Reviews, (2): CD001002, 2005,<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 31 <strong>of</strong> 36<br />
[1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15846609<br />
http://groups/p2/E<br />
�<br />
69. Huang, L., Shyur, SD., Wen, DC., Chang, YC., Ma, YC.,<br />
L<strong>in</strong>, SC., Wu, WC., Wu, JY.,: Prednisolone solution for<br />
<strong>acute</strong> asthma. Acta Paediatric Taiwan, 48(5): 257-262,<br />
2007, [2b] � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_A sthma/AsthmaHuang2007.pdf.<br />
70. Hussa<strong>in</strong>-Rizvi, A.; Kunkov, S.; and Cra<strong>in</strong>, E. F.: Does<br />
parental <strong>in</strong>volvement <strong>in</strong> pediatric emergency department<br />
asthma treatment affect home management? Journal <strong>of</strong><br />
Asthma, 46(8): 792-5, 2009, [2b] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE =fulltext&A N=19863282&D =medl �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaHussa<strong>in</strong>_Rivzi2009.pdf.<br />
71. Jalba, M.-S.: Three generations <strong>of</strong> ongo<strong>in</strong>g controversies<br />
concern<strong>in</strong>g the use <strong>of</strong> short act<strong>in</strong>g beta-agonist therapy <strong>in</strong><br />
asthma: a review. Journal <strong>of</strong> Asthma, 45(1): 9-18, 2008,<br />
[1b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18259990<br />
http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaHondras2005.pdf.<br />
�<br />
72. Jamalvi, S. W.; Raza, S. J.; Naz, F.; Shamim, S.; and<br />
Jamalvi, S. M. Z.-u.-W.: <strong>Management</strong> <strong>of</strong> <strong>acute</strong> asthma<br />
<strong>in</strong> <strong>children</strong> us<strong>in</strong>g metered dose <strong>in</strong>haler and small volume<br />
nebulizer. Journal <strong>of</strong> the Pakistan Medical Association,<br />
56(12): 595-9, 2006, [3a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=17312651 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaJamalvi2006.pdf.<br />
73. Jenk<strong>in</strong>s, C.; Costello, J.; and Hodge, L.: Systematic review<br />
<strong>of</strong> prevalence <strong>of</strong> aspir<strong>in</strong> <strong>in</strong>duced asthma and its<br />
implications for cl<strong>in</strong>ical practice.[see comment]. British<br />
Medical Journal, 328(7437): 434, 2004, [1a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=14976098 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaJenk<strong>in</strong>s2004.pdf.<br />
74. Johnson, K. B.; Blaisdell, C. J.; Walker, A.; and Eggleston,<br />
P.: Effectiveness <strong>of</strong> a cl<strong>in</strong>ical pathway for <strong>in</strong>patient<br />
asthma management. Pediatrics, 106(5): 1006-12, 2000,<br />
[2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11061767<br />
http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma.<br />
�<br />
75. Jones, K. G., Bell J, Fehrenbach, C, Pearce, L, Grimley, D,<br />
McCarthy, TP, : Understand<strong>in</strong>g Patient Perceptions <strong>of</strong><br />
Asthma: Results <strong>of</strong> the Asthma Control and Expectations<br />
(ACE) Survey. Interanational Journal <strong>of</strong> Cl<strong>in</strong>ical<br />
Practice, 56(2): 89-93, 2002, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=11926712 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaJones2002.pdf.<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaJohnson2000.pdf.
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
76. Jones, R.; L<strong>in</strong>, S.; Munsie, J. P.; Radigan, M.; and Hwang,<br />
S.-A.: Racial/ethnic differences <strong>in</strong> asthma-related<br />
emergency department visits and hospitalizations among<br />
<strong>children</strong> with wheeze <strong>in</strong> Buffalo, New York. Journal <strong>of</strong><br />
Asthma, 45(10): 916-22, 2008, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19085583 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaJones2008.pdf.<br />
77. Kamble, S., and Bharmal, M.: Incremental direct<br />
expenditure <strong>of</strong> treat<strong>in</strong>g asthma <strong>in</strong> the United States.<br />
Journal <strong>of</strong> Asthma, 46(1): 73-80, 2009, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19191142<br />
� http://groups/p2/EBC_Files/Ar<br />
ticles_Cited_<strong>in</strong>_Asthma/AsthmaKamble2009.pdf.<br />
78. Kamps, A. W. A.; Roorda, R. J.; and Brand, P. L. P.: Peak<br />
flow diaries <strong>in</strong> childhood asthma are unreliable. Thorax,<br />
56(3): 180-182, 2001, [2b] http://thorax.bmj.com/cgi/content/abstract/56/3/180 � http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaKamps2001.pdf.<br />
79. Kanabar, D.: Ibupr<strong>of</strong>en and asthma <strong>in</strong> paediatric populations:<br />
cl<strong>in</strong>ical concern or cl<strong>in</strong>ical reality? Journal <strong>of</strong> the Royal<br />
Society <strong>of</strong> Medic<strong>in</strong>e, 100 Suppl 48: 15-7, 2007, [1a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=18335849 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaKanabar2007.pdf.<br />
80. Karimi, M.; Mirzaei, M.; and Ahmadieh, M. H.:<br />
Acetam<strong>in</strong>ophen use and the symptoms <strong>of</strong> asthma, allergic<br />
rh<strong>in</strong>itis and eczema <strong>in</strong> <strong>children</strong>. Iranian Journal <strong>of</strong><br />
Allergy Asthma & Immunology, 5(2): 63-7, 2006, [4a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=17237578 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaKarimi2006.pdf.<br />
81. Karnick, P.; Margellos-Anast, H.; Seals, G.; Whitman, S.;<br />
Aljadeff, G.; and Johnson, D.: The pediatric asthma<br />
<strong>in</strong>tervention: a comprehensive cost-effective approach to<br />
asthma management <strong>in</strong> a disadvantaged <strong>in</strong>ner-city<br />
community. Journal <strong>of</strong> Asthma, 44(1): 39-44, 2007, [2a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=17365203 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaKarnick2007.pdf.<br />
82. Kaushal, R.; Bates, D. W.; Abramson, E. L.; Soukup, J.<br />
R.; and Goldmann, D. A.: Unit-based cl<strong>in</strong>ical<br />
pharmacists' prevention <strong>of</strong> serious medication errors <strong>in</strong><br />
pediatric <strong>in</strong>patients. American Journal <strong>of</strong> Health-System<br />
Pharmacy, 65(13): 1254-60, 2008, [3a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE =fulltext&A N=18574016&D =medl �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaKaushal2008.pdf.<br />
83. Kayani, S., and Shannon, D. C.: Adverse Behavioral Effects<br />
<strong>of</strong> Treatment for Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong><br />
Children. Chest, 122(2): 624, 2002, [2b] http://search.ebscohost.com/log<strong>in</strong>.aspx?direct=true &db=a9h&AN=10258224&log<strong>in</strong>page =Log<strong>in</strong>.asp&site=ehost-live&scope=site<br />
� http://groups/p2/EBC_<br />
Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaKayani2002.pdf.<br />
84. Keahey, L.; Bulloch, B.; Becker, A. B.; Pollack, C. V., Jr.;<br />
Clark, S.; Camargo, C. A., Jr.; and Multicenter<br />
Asthma Research Collaboration, I.: Initial oxygen<br />
saturation as a predictor <strong>of</strong> admission <strong>in</strong> <strong>children</strong><br />
present<strong>in</strong>g to the emergency department with <strong>acute</strong><br />
asthma. Annals <strong>of</strong> Emergency Medic<strong>in</strong>e, 40(3): 300-7,<br />
2002, [3a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE<br />
=fulltext&D =med4&AN=12192354 � http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaKeaney2002pdf.pdf.<br />
85. Kelly, A.-M.; Kerr, D.; and Powell, C.: Is severity<br />
assessment after one hour <strong>of</strong> treatment better for<br />
predict<strong>in</strong>g the need for admission <strong>in</strong> <strong>acute</strong> asthma?<br />
Respiratory Medic<strong>in</strong>e, 98(8): 777-81, 2004, [3a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=15303644 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaKelly2004.pdf.<br />
86. Kelly, C. S.; Andersen, C. L.; Pestian, J. P.; Wenger, A. D.;<br />
F<strong>in</strong>ch, A. B.; Strope, G. L.; and Luckstead, E. F.:<br />
Improved outcomes for hospitalized asthmatic <strong>children</strong><br />
us<strong>in</strong>g a cl<strong>in</strong>ical pathway. Annals <strong>of</strong> Allergy, Asthma, &<br />
Immunology, 84(5): 509-16, 2000, [4b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=10831004 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaKelly2000.pdf.<br />
87. Kim, I. K.; Phrampus, E.; Venkataraman, S.; Pitetti, R.;<br />
Saville, A.; Corcoran, T.; Gracely, E.; Funt, N.; and<br />
Thompson, A.: Helium/oxygen-driven albuterol<br />
nebulization <strong>in</strong> the treatment <strong>of</strong> <strong>children</strong> with moderate to<br />
severe asthma <strong>exacerbation</strong>s: a randomized, controlled<br />
trial. Pediatrics, 116(5): 1127-33, 2005, [2b]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=16263999 �<br />
http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaKim2005.pdf.<br />
88. Knudson, A.; Casey, M.; Burlew, M.; and Davidson, G.:<br />
Disparities <strong>in</strong> pediatric asthma hospitalizations. Journal<br />
<strong>of</strong> Public Health <strong>Management</strong> & Practice, 15(3): 232-7,<br />
2009, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19363403 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaKnudson2009.pdf.<br />
89. Lai, C. K. W.; Beasley, R.; Crane, J.; Foliaki, S.; Shah, J.;<br />
Weiland, S.; International Study <strong>of</strong>, A.; and Allergies<br />
<strong>in</strong> Childhood Phase Three Study, G.: Global variation<br />
<strong>in</strong> the prevalence and severity <strong>of</strong> asthma symptoms:<br />
phase three <strong>of</strong> the International Study <strong>of</strong> Asthma and<br />
Allergies <strong>in</strong> Childhood (ISAAC).[see comment]. Thorax,<br />
64(6): 476-83, 2009, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P<br />
ubMed&dopt=Citation&list_uids=19237391 � http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaLai2009.pdf.<br />
90. Lanphear, B. P., ALigne, C. Andrew, Au<strong>in</strong>ger, Peggy,<br />
Weitzman, Michael, Byrd, Robert S: Residential<br />
Exposures Associated with Asthma <strong>in</strong> US Children.<br />
Pediatrics, 107(3): 505-511, 2001b, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11230590 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaLanphear2001b.pdf.<br />
91. Lanphear, B. P., Kahn, Robert S, Berger, Omer, Au<strong>in</strong>ger,<br />
Peggy, Bortnick, Steven M, Nahhas, Ramzi W:<br />
Contribution <strong>of</strong> Residential Exposures to Asthma <strong>in</strong> US<br />
Children and Adolescents. Pediatrics, 107(6), 2001a,<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 32 <strong>of</strong> 36<br />
[4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11389296<br />
http://groups/p2/E<br />
�<br />
92. Lanski, S. L.; Greenwald, M.; Perk<strong>in</strong>s, A.; and Simon, H.<br />
K.: Herbal therapy use <strong>in</strong> a pediatric emergency<br />
department population: expect the unexpected.<br />
Pediatrics, 111(5 Pt 1): 981-5, 2003, [3a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12728075<br />
� http://groups/ce/EBC_Files/Ar<br />
ticles_Cited_<strong>in</strong>_Asthma_ED/AsthmaLanski2003.pdf.<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaLanphear2001a.pdf.<br />
93. Lara, M.; Duan, N.; Sherbourne, C.; Halfon, N.;<br />
Leibowitz, A.; and Brook, R. H.: Children's use <strong>of</strong><br />
emergency departments for asthma: persistent barriers or<br />
<strong>acute</strong> need? Journal <strong>of</strong> Asthma, 40(3): 289-99, 2003, [2a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=12807173 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaLara2003.pdf.<br />
94. Lavor<strong>in</strong>i, F., and Fontana, G. A.: Target<strong>in</strong>g drugs to the<br />
airways: The role <strong>of</strong> spacer devices. Expert Op<strong>in</strong>ion on<br />
Drug Delivery, 6(1): 91-102, 2009, [5b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19236210 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaLavor<strong>in</strong>i2009.pdf.<br />
95. Lemanske, R. F., Jr. et al.: Step-up therapy for <strong>children</strong> with<br />
uncontrolled asthma receiv<strong>in</strong>g <strong>in</strong>haled corticosteroids.<br />
New England Journal <strong>of</strong> Medic<strong>in</strong>e, 362(11): 975-85,<br />
2010, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=20197425 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaLamanske2010.PD F.<br />
96. Levy, M.; Heffner, B.; Stewart, T.; and Beeman, G.: The<br />
efficacy <strong>of</strong> asthma case management <strong>in</strong> an urban school<br />
district <strong>in</strong> reduc<strong>in</strong>g school absences and hospitalizations<br />
for asthma. Journal <strong>of</strong> School Health, 76(6): 320-4, 2006,<br />
[2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16918863<br />
http://groups/p2/E<br />
�<br />
97. Lieu, T. A., Lozano, Paula, F<strong>in</strong>kelste<strong>in</strong>, Jonathan A, Chi,<br />
Felicia W, Jensvold, Nancy G, Capra, Angela M,<br />
Queensberry, Charles P, Selby, Joe V, Farber, Harold<br />
J: Racial/Ethnic Variation <strong>in</strong> Asthma Status and<br />
<strong>Management</strong> Practices Among Children <strong>in</strong> Managed<br />
Medicaid. Pediatrics, 109(5): 857-865, 2002, [4a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=11986447 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaLieu2002.pdf.<br />
98. LocalConsensus, [5] �.<br />
99. Mansour, M. E.: How do we support follow-up with the<br />
primary care provider after an emergency department<br />
visit for asthma?[comment]. Pediatrics, 124(4): 1206-7,<br />
2009, [5a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19770174 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaMansour2009.pdf.<br />
100. Mansour, M. E.; Lanphear, B. P.; and DeWitt, T. G.:<br />
Barriers to asthma care <strong>in</strong> urban <strong>children</strong>: parent<br />
perspectives. Pediatrics, 106(3): 512-9, 2000, [2b]<br />
http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE =fulltext&D=med4&AN=10969096 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaMansour2000.pdf.<br />
101. Mark, J. D.: Integrative medic<strong>in</strong>e and asthma. Pediatric<br />
Cl<strong>in</strong>ics <strong>of</strong> North America, 54(6): 1007-23; xii, 2007, [1b]<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaLevy2006.pdf.<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=18061788 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaMark2007.pdf.
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
102. Mart<strong>in</strong>, J.; Donaldson, A. N. A.; Villarroel, R.; Parmar, M.<br />
K. B.; Ernst, E.; and Higg<strong>in</strong>son, I. J.: Efficacy <strong>of</strong><br />
acupuncture <strong>in</strong> asthma: systematic review and metaanalysis<br />
<strong>of</strong> published data from 11 randomised controlled<br />
trials. European Respiratory Journal, 20(4): 846-52,<br />
2002, [1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12412674 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaMart<strong>in</strong>2002.pdf.<br />
103. Mathew, J. L., and S<strong>in</strong>gh, M.: Metered dose <strong>in</strong>haler with<br />
spacer <strong>in</strong> <strong>children</strong> with <strong>acute</strong> asthma. Indian Pediatrics,<br />
45(4): 295-7, 2008, [1b ] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=18451447 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaMathew2008.pdf.<br />
104. McCarney, R. W.; Br<strong>in</strong>khaus, B.; Lasserson, T. J.; and<br />
L<strong>in</strong>de, K.: Acupuncture for chronic asthma. Cochrane<br />
Database <strong>of</strong> Systematic Reviews, (1), 2009, [1a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=14973944 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaMcCarney2009.pdf.<br />
105. McDaniel, M.; Paxson, C.; and Waldfogel, J.: Racial<br />
disparities <strong>in</strong> childhood asthma <strong>in</strong> the United States:<br />
evidence from the National Health Interview Survey,<br />
1997 to 2003. Pediatrics, 117(5): e868-77, 2006, [4a]<br />
http://www.ncbi.nlm.n ih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=16651291 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaMcDaniel2006.pdf.<br />
106. McDowell, K. M.; Chatburn, R. L.; Myers, T. R.;<br />
O'Riordan, M. A.; and Kercsmar, C. M.: A costsav<strong>in</strong>g<br />
algorithm for <strong>children</strong> hospitalized for status<br />
asthmaticus. Archives <strong>of</strong> Pediatrics & Adolescent<br />
Medic<strong>in</strong>e, 152(10): 977-84, 1998, [2a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE =fulltext&D=med4&AN=9790607 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaMcDowell1998.pdf.<br />
107. McMullen, A. H.; Yoos, H. L.; and Kitzman, H.: Peak flow<br />
meters <strong>in</strong> childhood asthma: parent report <strong>of</strong> use and<br />
perceived usefulness. Journal <strong>of</strong> Pediatric Health Care,<br />
16(2): 67-72, 2002, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11904640 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaMcMullen2002.pdf.<br />
108. Mitra, A. A. D.; Bassler, D.; Watts, K.; Lasserson, T. J.;<br />
and Ducharme, F. M.: Intravenous am<strong>in</strong>ophyll<strong>in</strong>e for<br />
<strong>acute</strong> severe asthma <strong>in</strong> <strong>children</strong> over two years receiv<strong>in</strong>g<br />
<strong>in</strong>haled bronchodilators. Cochrane Database <strong>of</strong><br />
Systematic Reviews, (4), 2009, [1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15846615 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaMitra2009.pdf.<br />
109. MMWR Moorman, J. E. et al.: National surveillance for<br />
asthma--United States, 1980-2004. Morbidity &<br />
Mortality Weekly Report, Surveillance Summaries. 56(8):<br />
1-54, 2007, [4a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE =fulltext&A N=17947969&D =medl � http://groups/p2/E BC_Files/Articles_Cited_i n_Asthma/AsthmaMMWR2004.pdf.<br />
110. Mohammed, S., and Goodacre, S.: Intravenous and<br />
nebulised magnesium sulphate for <strong>acute</strong> asthma:<br />
systematic review and meta-analysis. Emergency<br />
Medic<strong>in</strong>e Journal, 24(12): 823-30, 2007, [1a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=18029512 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaMohammed2007.pdf.<br />
111. Morgan, W. J. et al.: Results <strong>of</strong> a home-based environmental<br />
<strong>in</strong>tervention among urban <strong>children</strong> with asthma. New<br />
England Journal <strong>of</strong> Medic<strong>in</strong>e, 351(11): 1068-80, 2004,<br />
[2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15356304<br />
http://groups/p2/E<br />
�<br />
112. NAEPP: Expert Panel Report 3 (EPR-3): Guidel<strong>in</strong>es for the<br />
Diagnosis and <strong>Management</strong> <strong>of</strong> Asthma-Summary Report<br />
2007.[erratum appears <strong>in</strong> J Allergy Cl<strong>in</strong> Immunol. 2008<br />
Jun;121(6):1330]. Journal <strong>of</strong> Allergy & Cl<strong>in</strong>ical<br />
Immunology, 120(5 Suppl): S94-138, 2007, [5a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=17983880 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaNAEPPExpertPanel3Exac2007.pdf.<br />
113. Nakanishi, A. K.; Klasner, A. K.; and Rub<strong>in</strong>, B. K.: A<br />
randomized controlled trial <strong>of</strong> <strong>in</strong>haled flunisolide <strong>in</strong> the<br />
management <strong>of</strong> <strong>acute</strong> asthma <strong>in</strong> <strong>children</strong>.[see comment].<br />
Chest, 124(3): 790-4, 2003, [2b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12969999 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaNakanishi2003.pdf.<br />
114. Nelson, H. S.; Weiss, S. T.; Bleecker, E. R.; Yancey, S. W.;<br />
Dor<strong>in</strong>sky, P. M.; and Group, S. S.: The Salmeterol<br />
Multicenter Asthma Research Trial: a comparison <strong>of</strong><br />
usual pharmacotherapy for asthma or usual<br />
pharmacotherapy plus salmeterol.[Erratum appears <strong>in</strong><br />
Chest. 2006 May;129(5):1393]. Chest, 129(1): 15-26,<br />
2006, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16424409 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaNelson2006.PDF.<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaMorgan2004.pdf.<br />
115. Newman, S. P.: Spacer devices for metered dose <strong>in</strong>halers.<br />
Cl<strong>in</strong>ical Pharmacok<strong>in</strong>etics, 43(6): 349-60, 2004, [5a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=15086274 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaNewman2004.pdf.<br />
116. Ng, D. K. K.; Chow, P.-Y.; Lai, W.-P.; Chan, K.-C.; And,<br />
B.-L. T.; and So, H.-Y.: Effect <strong>of</strong> a structured asthma<br />
education program on hospitalized asthmatic <strong>children</strong>: a<br />
randomized controlled study. Pediatrics International,<br />
48(2): 158-62, 2006, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=16635175 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaNG2006.pdf.<br />
117. Norton, S. P.; Pusic, M. V.; Taha, F.; Heathcote, S.; and<br />
Carleton, B. C.: Effect <strong>of</strong> a cl<strong>in</strong>ical pathway on the<br />
hospitalisation rates <strong>of</strong> <strong>children</strong> with asthma: a<br />
prospective study. Archives <strong>of</strong> Disease <strong>in</strong> Childhood,<br />
92(1): 60-6, 2007, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16905562 � http://groups/ce/E BC_Files/Artic les_Cited_<strong>in</strong>_Asthma_ED/AsthmaNorton2007.pdf.<br />
118. Plotnick, L., and Ducharme, F.: Comb<strong>in</strong>ed <strong>in</strong>haled<br />
antichol<strong>in</strong>ergics and beta2-agonists for <strong>in</strong>itial treatment<br />
<strong>of</strong> <strong>acute</strong> asthma <strong>in</strong> <strong>children</strong>. Cochrane Database <strong>of</strong><br />
Systematic Reviews, (4), 2009, [1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11034671 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaPlotnic k2009.pdf.<br />
119. Portnoy, J. M., and Jenn<strong>in</strong>gs, D.: Utilization patterns <strong>in</strong> an<br />
asthma <strong>in</strong>tervention. Annals <strong>of</strong> Allergy, Asthma, &<br />
Immunology, 97(1 Suppl 1): S25-30, 2006, [4a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=16892768 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaPortnoy2006.pdf.<br />
120. Qureshi, F.; Zaritsky, A.; and Poirier, M. P.: Comparative<br />
efficacy <strong>of</strong> oral dexamethasone versus oral prednisone <strong>in</strong><br />
<strong>acute</strong> pediatric asthma. Journal <strong>of</strong> Pediatrics, 139(1): 20-<br />
6, 2001, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11445789 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_A sthma/AsthmaQureshi2001.pdf.<br />
121. Qureshi, F.; Zaritsky, A.; Welch, C.; Meadows, T.; and<br />
Burke, B. L.: Cl<strong>in</strong>ical efficacy <strong>of</strong> racemic albuterol<br />
versus levalbuterol for the treatment <strong>of</strong> <strong>acute</strong> pediatric<br />
asthma. Annals <strong>of</strong> Emergency Medic<strong>in</strong>e, 46(1): 29-36,<br />
2005, [3a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15988423 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaQureshi2005.PD F.<br />
122. Ralston, M. E.; Euwema, M. S.; Knecht, K. R.; Ziolkowski,<br />
T. J.; Coakley, T. A.; and Cl<strong>in</strong>e, S. M.: Comparison <strong>of</strong><br />
levalbuterol and racemic albuterol comb<strong>in</strong>ed with<br />
ipratropium bromide <strong>in</strong> <strong>acute</strong> pediatric asthma: a<br />
randomized controlled trial. Journal <strong>of</strong> Emergency<br />
Medic<strong>in</strong>e, 29(1): 29-35, 2005, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=15961004 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaRalston2005.pdf.<br />
123. Reznik, M.; Ozuah, P. O.; Franco, K.; Cohen, R.; and<br />
Motlow, F.: Use <strong>of</strong> complementary therapy by<br />
adolescents with asthma. Archives <strong>of</strong> Pediatrics &<br />
Adolescent Medic<strong>in</strong>e, 156(10): 1042-4, 2002, [3a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=12361452 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaReznik2002.pdf.<br />
124. Ribeiro de Andrade, C.; Duarte, M. C.; and Camargos, P.:<br />
Correlations between pulse oximetry and peak expiratory<br />
flow <strong>in</strong> <strong>acute</strong> asthma. Brazilian Journal <strong>of</strong> Medical &<br />
Biological Research, 40(4): 485-90, 2007, [3a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=17401491 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaRibeiro.2007.pdf.<br />
125. Rich, M.; Lamola, S.; Amory, C.; and Schneider, L.:<br />
Asthma <strong>in</strong> Life Context: Video Intervention/Prevention<br />
Assessment (VIA). Pediatrics, 105(3): 469, 2000, [3b]<br />
http://search.ebscohost.com/log<strong>in</strong>.aspx?direct=true&db=a9h&A N=2870180&log<strong>in</strong>page=Log<strong>in</strong>.asp&site=ehost-live&scope =site � http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaRich2000.pdf.<br />
126. Rivera, M. L.; Kim, T. Y.; Stewart, G. M.; M<strong>in</strong>asyan, L.;<br />
and Brown, L.: Albuterol nebulized <strong>in</strong> heliox <strong>in</strong> the<br />
<strong>in</strong>itial ED treatment <strong>of</strong> pediatric asthma: a bl<strong>in</strong>ded,<br />
randomized controlled trial. American Journal <strong>of</strong><br />
Emergency Medic<strong>in</strong>e, 24(1): 38-42, 2006, [2b]<br />
http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE =fulltext&AN=16338507&D=medl � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaRivera2006.PD F.<br />
127. Rodrigo, G. J., and Castro-Rodriguez, J. A.:<br />
Antichol<strong>in</strong>ergics <strong>in</strong> the treatment <strong>of</strong> <strong>children</strong> and adults<br />
with <strong>acute</strong> asthma: a systematic review with metaanalysis.<br />
Thorax, 60(9): 740-6, 2005, [1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db =PubMed&dopt=Citation&list_uids=16055613<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 33 <strong>of</strong> 36<br />
� http://groups/p2/EBC_Files/Ar<br />
ticles_Cited_<strong>in</strong>_Asthma/AsthmaRodrigo2005.pdf.
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
128. Rodrigo, G. J.; Pollack, C. V.; Rodrigo, C.; and Rowe, B.<br />
H.: Heliox for non-<strong>in</strong>tubated <strong>acute</strong> asthma patients.<br />
Cochrane Database <strong>of</strong> Systematic Reviews, (4), 2006,<br />
[1a] � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaRodrigo2009.pdf.<br />
129. Rodriguez, M. A., W<strong>in</strong>klleby, Marilyn A, Ahn, David,<br />
Sunquist Jan, Kraemer, Helena C: Identification <strong>of</strong><br />
Population Subgroups <strong>of</strong> Children and Adolescents with<br />
High Asthma Prevalence Archives <strong>of</strong> Pediatrics &<br />
Adolescent Medic<strong>in</strong>e, 156: 269-275, 2002, [4a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=11876672 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaRodriguez2002.pdf.<br />
130. Roller, C. M.; Zhang, G.; Troedson, R. G.; Leach, C. L.;<br />
Le Souef, P. N.; and Devadason, S. G.: Spacer<br />
<strong>in</strong>halation technique and deposition <strong>of</strong> extraf<strong>in</strong>e aerosol<br />
<strong>in</strong> asthmatic <strong>children</strong>. European Respiratory Journal,<br />
29(2): 299-306, 2007, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17005581 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_A sthma/AsthmaRoller2007.pdf.<br />
131. Rosen, C. M., and Rodriguez, L.: The Inner-City Asthma<br />
Intervention asthma counselor program: a collaborative<br />
model between physician and social worker to help<br />
empower families. Annals <strong>of</strong> Allergy, Asthma, &<br />
Immunology, 97(1 Suppl 1): S16-9, 2006, [4a]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=16892766 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaRosen2006.pdf.<br />
132. Rowe, B., Spooner, C., Ducharme, F., Bretzlaff, J., Bota,<br />
G.: Early emergency department treatment <strong>of</strong> <strong>acute</strong><br />
asthma with systemic corticosteroids [Systematic<br />
Review]. Cochrane Database <strong>of</strong> Systematic Reviews, 1:<br />
1, 2009a, [1a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE =fulltext&D=coch&AN=00075320-100000000-01559 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaRower2009a.pdf.<br />
133. Rowe, B. H.; Bretzlaff, J.; Bourdon, C.; Bota, G.; Blitz, S.;<br />
and Camargo, C. A.: Magnesium sulfate for treat<strong>in</strong>g<br />
<strong>exacerbation</strong>s <strong>of</strong> <strong>acute</strong> asthma <strong>in</strong> the emergency<br />
department. Cochrane Database <strong>of</strong> Systematic Reviews,<br />
(4), 2009b, [1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=10796650 � http://groups/ce/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma_ED/AsthmaRowe2009.pdf.<br />
134. Salpeter, S. R.; Buckley, N. S.; Ormiston, T. M.; and<br />
Salpeter, E. E.: Meta-analysis: effect <strong>of</strong> long-act<strong>in</strong>g<br />
beta-agonists on severe asthma <strong>exacerbation</strong>s and<br />
asthma-related deaths. Annals <strong>of</strong> Internal Medic<strong>in</strong>e,<br />
144(12): 904-12, 2006, [1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16754916 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaSalpeter2006.pdf.<br />
135. Salpeter, S. R.; Wall, A. J.; and Buckley, N. S.: Long-act<strong>in</strong>g<br />
beta-agonists with and without <strong>in</strong>haled corticosteroids<br />
and catastrophic asthma events. American Journal <strong>of</strong><br />
Medic<strong>in</strong>e, 123(4): 322-8.e2, 2010, [1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=20176343 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaSalpeter2010.PDF.<br />
136. Sanghera, N.; Chan, P.-Y.; Khaki, Z. F.; Planner, C.; Lee,<br />
K. K. C.; Cranswick, N. E.; and Wong, I. C. K.:<br />
Interventions <strong>of</strong> hospital pharmacists <strong>in</strong> improv<strong>in</strong>g drug<br />
therapy <strong>in</strong> <strong>children</strong>: a systematic literature review. Drug<br />
Safety, 29(11): 1031-47, 2006, [1a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE=fulltext&A N=17061909&D =medl �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaSanghera2006.pdf.<br />
137. Scarfone, R. J.; Capraro, G. A.; Zorc, J. J.; and Zhao, H.:<br />
Demonstrated use <strong>of</strong> metered-dose <strong>in</strong>halers and peak<br />
flow meters by <strong>children</strong> and adolescents with <strong>acute</strong><br />
asthma <strong>exacerbation</strong>s.[see comment]. Archives <strong>of</strong><br />
Pediatrics & Adolescent Medic<strong>in</strong>e, 156(4): 378-83, 2002,<br />
[3b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11929373<br />
http://groups/p2/E<br />
�<br />
138. Schonberger, H. J. A. M.; Maas, T.; Dompel<strong>in</strong>g, E.;<br />
Knottnerus, J. A.; van Weel, C.; and van Schayck, C.<br />
P.: Compliance <strong>of</strong> asthmatic families with a primary<br />
prevention programme <strong>of</strong> asthma and effectiveness <strong>of</strong><br />
measures to reduce <strong>in</strong>halant allergens--a randomized trial.<br />
Cl<strong>in</strong>ical & Experimental Allergy, 34(7): 1024-31, 2004,<br />
[2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15248845<br />
http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaScarfone2002.pdf.<br />
�<br />
139. Schreck, D. M., and Bab<strong>in</strong>, S.: Comparison <strong>of</strong> racemic<br />
albuterol and levalbuterol <strong>in</strong> the treatment <strong>of</strong> <strong>acute</strong><br />
asthma <strong>in</strong> the ED. American Journal <strong>of</strong> Emergency<br />
Medic<strong>in</strong>e, 23(7): 842-7, 2005, [4a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE =fulltext&AN=16291438&D=med4 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaSchreck2005.PDF.<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaSchonberger2004.pdf.<br />
140. Schuh, S.; Dick, P. T.; Stephens, D.; Hartley, M.; Khaik<strong>in</strong>,<br />
S.; Rodrigues, L.; and Coates, A. L.: High-dose <strong>in</strong>haled<br />
fluticasone does not replace oral prednisolone <strong>in</strong> <strong>children</strong><br />
with mild to moderate <strong>acute</strong> asthma. Pediatrics, 118(2):<br />
644-50, 2006, [2b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16882819 � http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaSchuh2006.pdf.<br />
141. Schulte, A.; Musolf, J.; Meurer, J. R.; Cohn, J. H.; and<br />
Kelly, K. J.: Pediatric asthma case management: a<br />
review <strong>of</strong> evidence and an experimental study design.<br />
Journal <strong>of</strong> Pediatric Nurs<strong>in</strong>g, 19(4): 304-10, 2004, [1b]<br />
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=15308981 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaSchulte2004.pdf.<br />
142. Shalowitz, M. U., Berry, Carolyn A, Qu<strong>in</strong>n, Kelly A, Wolf,<br />
Raoul L: The Relationship <strong>of</strong> Life Stressores and<br />
Maternal Depression to Pediatric Asthma Morbidity <strong>in</strong> a<br />
Subspecialty Practice. Ambulatory Pediatrics, 1(4): 185-<br />
193, 2001, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&l ist_uids=11888399 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_A sthma/AsthmaShalowitz2001.pdf.<br />
143. SIGN: British Guidel<strong>in</strong>e on the <strong>Management</strong> <strong>of</strong> Asthma:<br />
Scottish Intercollegiate Guidel<strong>in</strong>es Network Thorax, 63<br />
Suppl 4: iv1-121, 2008, [5a] http://www.ncbi.nlm .nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=18463203 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaBritishThroacic2008.pdf.<br />
144. Simons, F. E.; Roberts, J. R.; Gu, X.; and Simons, K. J.:<br />
Ep<strong>in</strong>ephr<strong>in</strong>e absorption <strong>in</strong> <strong>children</strong> with a history <strong>of</strong><br />
anaphylaxis. Journal <strong>of</strong> Allergy & Cl<strong>in</strong>ical Immunology,<br />
101(1 Pt 1): 33-7, 1998, [2b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=9449498 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaSimons1998.pdf.<br />
145. S<strong>in</strong>, D. D., and Man, S. F.: Low-dose <strong>in</strong>haled corticosteroid<br />
therapy and risk <strong>of</strong> emergency department visits for<br />
asthma. Archives <strong>of</strong> Internal Medic<strong>in</strong>e., 162(14): 1591-5,<br />
2002, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12123402 � http://groups/ce/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma_ED/AsthmaS<strong>in</strong>2002.pdf.<br />
146. Smith, L. A. et al.: Modifiable risk factors for suboptimal<br />
control and controller medication underuse among<br />
<strong>children</strong> with asthma. Pediatrics, 122(4): 760-9, 2008,<br />
[4a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEW S=N&PAG E=fulltext&AN=18829799&D=medl � http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_A sthma/AsthmaSmith2008.pdf.<br />
147. Smith, M.; Iqbal, S. M. S. I.; Rowe, B. H.; and N'Diaye, T.:<br />
Corticosteroids for hospitalised <strong>children</strong> with <strong>acute</strong><br />
asthma. Cochrane Database <strong>of</strong> Systematic Reviews, (4),<br />
2009, [1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12804441 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaSmith2009.pdf.<br />
148. Sockrider, M. M.; Abramson, S.; Brooks, E.; Cav<strong>in</strong>ess, A.<br />
C.; Pilney, S.; Koerner, C.; and Macias, C. G.:<br />
Deliver<strong>in</strong>g tailored asthma family education <strong>in</strong> a pediatric<br />
emergency department sett<strong>in</strong>g: a pilot study. Pediatrics,<br />
117(4 Pt 2): S135-44, 2006, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=16777829 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma_ED/AsthmaSoc krider2006.pdf.<br />
149. Sole, D.; Komatsu, M. K.; Carvalho, K. V.; and Naspitz, C.<br />
K.: Pulse oximetry <strong>in</strong> the evaluation <strong>of</strong> the severity <strong>of</strong><br />
<strong>acute</strong> asthma and/or wheez<strong>in</strong>g <strong>in</strong> <strong>children</strong>. Journal <strong>of</strong><br />
Asthma, 36(4): 327-33, 1999, [2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=10386496 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaSole1999PulseOx.pdf.<br />
150. Spiegel, J.; Love, A. S.; Wood, P. R.; Griffith, M.; Taylor,<br />
K. R.; Williams, S. G.; and Redd, S. C.: The Inner-City<br />
Asthma Intervention: description <strong>of</strong> a community-based<br />
implementation <strong>of</strong> an evidence-based approach to asthma<br />
management. Annals <strong>of</strong> Allergy, Asthma, & Immunology,<br />
97(1 Suppl 1): S6-10, 2006, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=16892764 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaSpiegel2006.pdf.<br />
151. Taketomo, C.; Hiodd<strong>in</strong>g, J.; and Kraus, D.: Pediatric<br />
Dosage Handbook: Includ<strong>in</strong>g Neonatal Dos<strong>in</strong>g, Drug<br />
Adm<strong>in</strong>istration, & Extemporaneous Preparations, 16 Ed,<br />
[5a] �.<br />
152. Travers, A.; Jones, A. P.; Kelly, K.; Barker, S. J.;<br />
Camargo, C. A.; and Rowe, B. H.: Intravenous beta2agonists<br />
for <strong>acute</strong> asthma <strong>in</strong> the emergency department.<br />
Cochrane Database <strong>of</strong> Systematic Reviews, (2):<br />
CD002988, 2001, [1a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE=fulltext&A<br />
N=11406055&D =m ed4 � http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaTravers2001.PDF.<br />
153. Vidgren, M.; Paronen, P.; and A, K.: Effect <strong>of</strong> Extension<br />
Devices on Drug Deposition from Inhalation Aerosols.<br />
International Journal <strong>of</strong> Pharmaceutics, 39: 107-112,<br />
1987, [4b] � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_A sthma/AsthmaVidgren1981.pdf.<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 34 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
154. Walders, N.; Kercsmar, C.; Schluchter, M.; Redl<strong>in</strong>e, S.;<br />
Kirchner, H. L.; and Drotar, D.: An <strong>in</strong>terdiscipl<strong>in</strong>ary<br />
<strong>in</strong>tervention for undertreated pediatric asthma. Chest,<br />
129(2): 292-9, 2006, [2a] http://ovidsp.ovid.com /ovidweb.cgi?T=JS&NEWS=N&PAGE =fullte xt&AN=16478844&D=medl � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaWalders2006.pdf.<br />
155. Walters, E., Watlers, J Inhaled short-act<strong>in</strong>g beta2-agonists<br />
use <strong>in</strong> Asthma: Regular versus Needed Treatment<br />
Cochrane Database <strong>of</strong> Systematic Reviews, (1), 2002,<br />
[1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12804401<br />
http://groups/p2/E<br />
�<br />
156. Walters, E. H.; Gibson, P. G.; Lasserson, T. J.; and<br />
Walters, J. A. E.: Long-act<strong>in</strong>g beta2-agonists for chronic<br />
asthma <strong>in</strong> adults and <strong>children</strong> where background therapy<br />
conta<strong>in</strong>s varied or no <strong>in</strong>haled corticosteroid. Cochrane<br />
Database <strong>of</strong> Systematic Reviews, (1): CD001385, 2007,<br />
[1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17253458<br />
http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaWalters2002.PDF.<br />
�<br />
157. Wazeka, A.; Valacer, D. J.; Cooper, M.; Caplan, D. W.;<br />
and DiMaio, M.: Impact <strong>of</strong> a pediatric asthma cl<strong>in</strong>ical<br />
pathway on hospital cost and length <strong>of</strong> stay. Pediatric<br />
Pulmonology, 32(3): 211-6, 2001, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11536450 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaWazeka2001.pdf.<br />
158. Wilson, S. E.; Leonard, A.; Moomaw, C.; Schneeweiss, S.;<br />
and Eckman, M. H.: Underuse <strong>of</strong> controller medications<br />
among <strong>children</strong> with persistent asthma <strong>in</strong> the Ohio<br />
medicaid population: evolv<strong>in</strong>g differences with new<br />
medications. Ambulatory Pediatrics, 5(2): 83-9, 2005,<br />
[4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15780019<br />
http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaWalters2007.PDF.<br />
�<br />
159. Wolf, F.; Guevara, J. P.; Grum, C. M.; Clark, N. M.; and<br />
Cates, C. J.: Educational <strong>in</strong>terventions for asthma <strong>in</strong><br />
<strong>children</strong>. Cochrane Database <strong>of</strong> Systematic Reviews, (4),<br />
2008, [1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12535395 � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaWolf2008.pdf.<br />
160. Wood, P.; Tumiel-Berhalter, L.; Owen, S.; Taylor, K.; and<br />
Kattan, M.: Implementation <strong>of</strong> an asthma <strong>in</strong>tervention <strong>in</strong><br />
the <strong>in</strong>ner city. Annals <strong>of</strong> Allergy, Asthma, & Immunology,<br />
97(1 Suppl 1): S20-4, 2006, [4a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=P ubMed&dopt=Citation&list_uids=16892767 �<br />
http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaWood2006.pdf.<br />
161. WorldHealthOrganizationWrit<strong>in</strong>gGroup:<br />
Nonpharmaceutical <strong>in</strong>terventions for pandemic <strong>in</strong>fluenza,<br />
national and community measures. Emerg<strong>in</strong>g Infectious<br />
Diseases [serial on the Internet] www.cdc.gov/eid, 12(1),<br />
2006, [5a] http://www.cdc.gov/ncidod/EID/vol12no01/05-1371.htm �.<br />
162. Wright, R. S., KA.; jay, GD.; Steele, DW.; : Evaluation <strong>of</strong><br />
pre- and posttreatment pulse oximetry <strong>in</strong> <strong>acute</strong> childhood<br />
asthma. Academy <strong>of</strong> Emergency Medic<strong>in</strong>e 4(2): 114-7,<br />
1997, [3b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db =PubMed&dopt=Citation&list_uids=9043537 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaWright1997.pdf.<br />
163. Yilmaz, O.; Sogut, A.; Kose, U.; Sak<strong>in</strong>ci, O.; and Yuksel,<br />
H.: Influence <strong>of</strong> ambulatory <strong>in</strong>haled treatment with<br />
different devices on the duration <strong>of</strong> <strong>acute</strong> asthma f<strong>in</strong>d<strong>in</strong>gs<br />
<strong>in</strong> <strong>children</strong>. Journal <strong>of</strong> Asthma, 46(2): 191-3, 2009, [4a]<br />
http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE =fulltext&AN=19253129&D=medl � http://groups/p2/EBC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaYilmaz2009.pdf.<br />
164. Yoos, H. L.; Kitzman, H.; McMullen, A.; Henderson, C.;<br />
and Sidora, K.: Symptom monitor<strong>in</strong>g <strong>in</strong> childhood<br />
asthma: a randomized cl<strong>in</strong>ical trial compar<strong>in</strong>g peak<br />
expiratory flow rate with symptom monitor<strong>in</strong>g. Annals <strong>of</strong><br />
Allergy, Asthma, & Immunology, 88(3): 283-91, 2002,<br />
[2a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11926622<br />
http://groups/p2/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaWilson2005.pdf.<br />
�<br />
165. Zemek, R. L.; Bhogal, S. K.; and Ducharme, F. M.:<br />
Systematic review <strong>of</strong> randomized controlled trials<br />
exam<strong>in</strong><strong>in</strong>g written action plans <strong>in</strong> <strong>children</strong>: what is the<br />
plan? Archives <strong>of</strong> Pediatrics & Adolescent Medic<strong>in</strong>e,<br />
162(2): 157-63, 2008, [1a] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18250241 � http://groups/p2/E BC_Files/Articles_Cited_<strong>in</strong>_A sthma/AsthmaZemek2008.pdf.<br />
166. Zorc, J. J.; Chew, A.; Allen, J. L.; and Shaw, K.: Beliefs<br />
and barriers to follow-up after an emergency department<br />
asthma visit: a randomized trial. Pediatrics, 124(4):<br />
1135-42, 2009, [2a] http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEW S=N&PAG E=fulltext&D=medl&A N=19786448 � http://groups/p2/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma/AsthmaZorc2009.pdf.<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma/AsthmaYoos2002.PDF.<br />
167. Zorc, J. J.; Scarfone, R. J.; Li, Y.; Hong, T.; Harmel<strong>in</strong>, M.;<br />
Grunste<strong>in</strong>, L.; Andre, J. B.; and Randomized, t.:<br />
Scheduled follow-up after a pediatric emergency<br />
department visit for asthma: a randomized trial.<br />
Pediatrics, 111(3): 495-502, 2003, [2a] � http://groups/ce/E<br />
BC_Files/Articles_Cited_<strong>in</strong>_Asthma_ED/AsthmaZorc2003.pdf.<br />
168. Zorc, J. J.; Scarfone, R. J.; Li, Y.; Zorc, J. J.; Scarfone, R.<br />
J.; and Li, Y.: Predictors <strong>of</strong> primary care follow-up after<br />
a pediatric emergency visit for asthma. Journal <strong>of</strong><br />
Asthma, 42(7): 571-6, 2005, [2a] � http://groups/ce/EBC_Files/Ar ticles_Cited_<strong>in</strong>_Asthma_ED/AsthmaZorc2005.pdf.<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 35 <strong>of</strong> 36
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> Acute Exacerbation <strong>of</strong> Asthma <strong>in</strong> <strong>children</strong> aged 0 to 18 years Guidel<strong>in</strong>e 4<br />
Note: Full tables <strong>of</strong> evidence grad<strong>in</strong>g system available <strong>in</strong> separate document:<br />
Table <strong>of</strong> Evidence Levels <strong>of</strong> Individual Studies by Doma<strong>in</strong>, Study Design, & Quality (abbreviated table below)<br />
Grad<strong>in</strong>g a Body <strong>of</strong> Evidence to Answer a Cl<strong>in</strong>ical Question<br />
Judg<strong>in</strong>g the Strength <strong>of</strong> a Recommendation (abbreviated table below)<br />
Table <strong>of</strong> Evidence Levels (see note above)<br />
Quality level Def<strong>in</strong>ition<br />
1a† or 1b† Systematic review, meta-analysis, or meta-synthesis <strong>of</strong> multiple studies<br />
2a or 2b Best study design for doma<strong>in</strong><br />
3a or 3b Fair study design for doma<strong>in</strong><br />
4a or 4b Weak study design for doma<strong>in</strong><br />
5a or 5b Other: General review, expert op<strong>in</strong>ion, case report, consensus report, or guidel<strong>in</strong>e<br />
5 Local Consensus<br />
†a = good quality study; b = lesser quality study<br />
Table <strong>of</strong> Recommendation Strength (see note above)<br />
Strength Def<strong>in</strong>ition<br />
―Strongly recommended‖ There is consensus that benefits clearly outweigh risks and burdens<br />
(or visa-versa for negative recommendations).<br />
―Recommended‖ There is consensus that benefits are closely balanced with risks and burdens.<br />
No recommendation made There is lack <strong>of</strong> consensus to direct development <strong>of</strong> a recommendation.<br />
Dimensions: In determ<strong>in</strong><strong>in</strong>g the strength <strong>of</strong> a recommendation, the development group makes a considered judgment <strong>in</strong> a consensus<br />
process that <strong>in</strong>corporates critically appraised evidence, cl<strong>in</strong>ical experience, and other dimensions as listed below.<br />
1. Grade <strong>of</strong> the Body <strong>of</strong> Evidence (see note above)<br />
2. Safety / Harm<br />
3. Health benefit to patient (direct benefit)<br />
4. Burden to patient <strong>of</strong> adherence to recommendation (cost, hassle, discomfort, pa<strong>in</strong>, motivation, ability to adhere, time)<br />
5. Cost-effectiveness to healthcare system (balance <strong>of</strong> cost / sav<strong>in</strong>gs <strong>of</strong> resources, staff time, and supplies based on published studies or<br />
onsite analysis)<br />
6. Directness (the extent to which the body <strong>of</strong> evidence directly answers the cl<strong>in</strong>ical question [population/problem, <strong>in</strong>tervention,<br />
comparison, outcome])<br />
7. Impact on morbidity/mortality or quality <strong>of</strong> life<br />
Copyright © 1998, 1999, 2002, 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 36 <strong>of</strong> 36