Pathology of the Peripheral Neuroblastic Tumors - LabMedicine
Pathology of the Peripheral Neuroblastic Tumors - LabMedicine
Pathology of the Peripheral Neuroblastic Tumors - LabMedicine
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Review<br />
Received 3.31.06 | Revisions Received 5.4.06 | Accepted 5.9.06<br />
<strong>Pathology</strong> <strong>of</strong> <strong>the</strong> <strong>Peripheral</strong> <strong>Neuroblastic</strong> <strong>Tumors</strong><br />
Hiroyuki Shimada, MD, PhD, 1 Atsuko Nakagawa, MD, PhD 2<br />
( 1 Department <strong>of</strong> <strong>Pathology</strong> and Laboratory Medicine, Childrens Hospital Los Angeles and University <strong>of</strong> Sou<strong>the</strong>rn California Kech School<br />
<strong>of</strong> Medicine, Los Angeles, CA, 2 Division <strong>of</strong> <strong>Pathology</strong>, Department <strong>of</strong> Clinical Laboratory Medicine, National Center for Child Health<br />
and Development, Tokyo, Japan)<br />
DOI: 10.1309/0506C1BM8GBVV224<br />
Abstract<br />
<strong>Peripheral</strong> neuroblastic tumors (pNTs;<br />
neuroblastoma, ganglioneuroblastoma,<br />
ganglioneuroma) in infants and children, once<br />
called as “enigmatic,” are now considered as<br />
<strong>Peripheral</strong> neuroblastic tumors (pNTs including neuroblastoma,<br />
ganglioneuroblastoma, and ganglioneuroma) comprise<br />
one <strong>of</strong> <strong>the</strong> most common groups <strong>of</strong> neoplastic disease in infants<br />
and children. 1 They are derived from immature sympa<strong>the</strong>tic<br />
neuroblasts and diagnosed in <strong>the</strong> primary sites related to <strong>the</strong> embryonic<br />
distribution <strong>of</strong> neural crest cells, such as adrenal medulla<br />
and structures <strong>of</strong> <strong>the</strong> sympa<strong>the</strong>tic nervous system in <strong>the</strong> thorax,<br />
abdomen, and pelvic cavity. These tumors are well known to<br />
show unique and <strong>of</strong>ten unpredictable clinical behaviors. Recent<br />
advances in basic, translational, and clinical research lead us to<br />
believe that <strong>the</strong> pNTs are heterogeneous and composed <strong>of</strong> biologically<br />
different, favorable and unfavorable, tumors. 2,3 The<br />
biologically favorable tumors have a potential <strong>of</strong> involution/<br />
spontaneous regression or tumor maturation with or without<br />
chemo<strong>the</strong>rapy/irradiation <strong>the</strong>rapy. In contrast, <strong>the</strong> biologically<br />
unfavorable tumors progress aggressively and <strong>of</strong>ten bring a fatal<br />
outcome to <strong>the</strong> patients despite intensive treatment. It is also<br />
speculated that differences between <strong>the</strong> biologically favorable<br />
and unfavorable tumors could be determined during <strong>the</strong> early<br />
stage <strong>of</strong> <strong>the</strong> neoplastic process by molecular/genetic properties <strong>of</strong><br />
<strong>the</strong> individual cases. 2,3<br />
<strong>Peripheral</strong> neuroblastic tumors are so unique that those<br />
factors useful in <strong>the</strong> routine practice <strong>of</strong> surgical pathology, such<br />
as positive surgical margins, tumor necrosis, vascular invasion,<br />
and even hematogenous/lymphatic spread, are not necessarily<br />
significant indicators <strong>of</strong> aggressive tumor progression and a<br />
poor clinical outcome <strong>of</strong> <strong>the</strong> patients. Biologic properties are<br />
<strong>of</strong>ten more important and critical than those conventional<br />
prognostic factors for predicting clinical behavior <strong>of</strong> <strong>the</strong> tumor<br />
in individual cases. The Children’s Oncology Group (COG)<br />
Neuroblastoma Biology Study has been utilizing front-end<br />
prognostic factors for patient stratification and protocol assignment<br />
<strong>of</strong> this disease. Those prognostic factors include patient’s<br />
age at diagnosis, clinical stage 4 (see Table 1), histopathology,<br />
MYCN oncogene status, and DNA index. By combination <strong>of</strong><br />
<strong>the</strong>se factors, 3 risk groups: low, intermediate, and high are<br />
distinguished among <strong>the</strong> pNT cases (Table 2). 5<br />
biologically heterogeneous. The unique<br />
clinical/biological behaviors: such as,<br />
involution, spontaneous regression, tumor<br />
maturation, and aggressive progression, are<br />
closely related to <strong>the</strong> molecular/genetic<br />
properties <strong>of</strong> <strong>the</strong> tumors <strong>of</strong> individual cases. In<br />
this article, we describe prognostic significance<br />
and biological relevance <strong>of</strong> <strong>the</strong> International<br />
Neuroblastoma <strong>Pathology</strong> Classification (INPC).<br />
Since pNTs <strong>of</strong>fer one <strong>of</strong> <strong>the</strong> best models for analysis/evaluation<br />
<strong>of</strong> histologic features as phenotypical manifestation <strong>of</strong><br />
multiple factors including age and various molecular/genetic<br />
properties <strong>of</strong> <strong>the</strong> tumors, <strong>the</strong> international committee <strong>of</strong> pathologists<br />
established a histopathology classification [<strong>the</strong> International<br />
Neuroblastoma <strong>Pathology</strong> Classification (INPC)] in<br />
1999 6,7 and partly modified it in 2003. 8 In this article, we first<br />
describe a definition <strong>of</strong> pNTs and <strong>the</strong>n apply this histopathology<br />
classification to 6 representative cases for illustrating prognostic<br />
significance and biological relevance <strong>of</strong> <strong>the</strong> INPC system.<br />
Discussion focuses on <strong>the</strong> close relationship between histologic<br />
features and molecular/genomic alterations <strong>of</strong> (1) MYCN amplification,<br />
an established marker indicating aggressive tumor<br />
progression, 9,10 (2) DNA index separating near-triploid tumors<br />
with a better prognosis from near-diploid tumors with a poor<br />
prognosis, 11 and (3) trkA (a high-affinity nerve growth factor<br />
receptor) expression reported to have anti-oncogenic effects 12,13<br />
in pNTs.<br />
Definition<br />
The name peripheral neuroblastic tumors (pNTs) indicates<br />
that <strong>the</strong> tumors in this group are composed <strong>of</strong> <strong>the</strong> neoplastic cells<br />
with a neuronal phenotype <strong>of</strong> neuronal (neural crest) cellular origin.<br />
<strong>Peripheral</strong> neuroblastic tumors should be clearly distinguished<br />
from those having neuronal phenotype but <strong>of</strong> unknown (presumably<br />
non-neuronal) cellular origin. For example, pPNET (peripheral<br />
primitive neuroectodermal tumor), known to have a limited<br />
neuronal differentiation, does not seem to have a proven neuronal<br />
cellular origin. These 2 tumor entities, pNTs and pPNET, also<br />
have distinct molecular properties: pNTs are <strong>of</strong>ten associated with<br />
deletion <strong>of</strong> chromosome 1p and MYCN amplification, 2,3 whereas<br />
pPNET has unique chromosomal translocation fusing EWS/ETS. 14<br />
Fur<strong>the</strong>rmore, transfection <strong>of</strong> EWS/ETS fusion genes into NIH<br />
3T3 fibroblasts is reported to induce epi<strong>the</strong>lial and neuroectodermal<br />
differentiation <strong>of</strong> pPNET-phenotype. 15,16<br />
684 LABMEDICINE � Volume 37 Number 11 � November 2006 labmedicine.com
Table 1_International Neuroblastoma Staging System (INSS)<br />
Stage Definition<br />
1 Localized tumor confined to <strong>the</strong> area <strong>of</strong> origin. Complete gross resection with or without microscopic residual disease; identifiable ipsilateral and<br />
contralateral lymph node negative for tumor. Adherent lymph nodes in direct continuity with and removed with <strong>the</strong> tumor may be positive for <strong>the</strong> tumor.<br />
A grossly resected midline tumor without ipsilateral (with: stage 2A) or contralateral (with: stage 2B) lymph node involvement is considered stage 1<br />
2A Unilateral with incomplete gross resection; identifiable ipsilateral and contralateral lymph node negative for tumor<br />
2B Unilateral with complete or incomplete gross resection; with ipsilateral lymph node positive for tumor; identifiable contralateral lymph node negative for tumor<br />
3 Tumor infiltrating across midline with or without regional lymph node involvement; or unilateral tumor with contralateral lymph node involvement or midline<br />
tumor with bilateral lymph node involvement<br />
4 Dissemination <strong>of</strong> tumor to distant lymph nodes, bone marrow, liver, or o<strong>the</strong>r organs except as defined as stage 4S<br />
4S Localized primary tumor as defined for stage 1 or 2 with dissemination limited to liver, skin, and bone marrow (
Review<br />
<strong>of</strong> neuroblastic differentiation and MKI to <strong>the</strong> nodular (neuroblastomatous)<br />
component.<br />
Case Presentation<br />
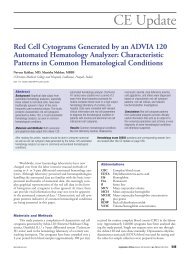
Case 1: A 4-month-old female with a clinical stage 4S disease<br />
<strong>of</strong> <strong>the</strong> adrenal primary and liver involvement.<br />
Microscopic sections from <strong>the</strong> adrenal tumor and liver<br />
biopsy sample showed <strong>the</strong> same appearance <strong>of</strong> neuroblastoma<br />
(Schwannian stroma-poor), poorly differentiated subtype with a<br />
low mitosis-karyorrhexis index (MKI) (Image 1A). Because <strong>of</strong><br />
<strong>the</strong> age <strong>of</strong> <strong>the</strong> patient at diagnosis, <strong>the</strong> case was classified into a<br />
favorable histology group (Table 2). The tumor sample had nonamplified<br />
MYCN and high trkAI/II (high-affinity nerve growth<br />
factor receptor, a receptor tyrosine kinase that binds nerve<br />
growth factor) expression, and <strong>the</strong> DNA index, as determined<br />
by flow cytometry, was 1.25. According to <strong>the</strong> COG risk-grouping<br />
scheme, <strong>the</strong> patient was placed in <strong>the</strong> low-risk protocol<br />
(Table 1). The tumor regressed spontaneously, and she is alive<br />
and well 4 years after diagnosis.<br />
Comment: This was an example <strong>of</strong> spontaneous regression<br />
<strong>of</strong> a widely spread disease. Favorable histology, non-amplified<br />
MYCN, and a hyperdiploid DNA pattern all supported that <strong>the</strong><br />
tumor <strong>of</strong> this case was biologically favorable. A high level <strong>of</strong><br />
trkAI/II expression also suggested a potential <strong>of</strong> ei<strong>the</strong>r maturation<br />
or apoptosis (see description in Discussion) <strong>of</strong> <strong>the</strong> neuroblastic<br />
cells. 12,13 Stage 4S (S=special) is defined as a disease<br />
condition in patients
<strong>of</strong> neuroblastic cells expressing lower level <strong>of</strong> trkAI/II, and do<br />
not seem to have a potential <strong>of</strong> age-appropriate maturation.<br />
Case 5: A 5-year and 2-month-old male with a clinical<br />
stage 1 tumor located in <strong>the</strong> pelvis.<br />
Microscopic sections from <strong>the</strong> completely resected tumor<br />
showed <strong>the</strong> appearance <strong>of</strong> ganglioneuroblastoma, intermixed<br />
A B<br />
C D<br />
E F<br />
Review<br />
(Schwannian stroma-rich) (Image 1E). The case was classified<br />
into a favorable histology group. The tumor sample had nonamplified<br />
MYCN and a diploid pattern <strong>of</strong> DNA content. Level<br />
<strong>of</strong> trkAI/II expression was not tested. He was a low-risk patient<br />
(Table 2), and is now alive and well 10 years after <strong>the</strong> surgery<br />
without chemo<strong>the</strong>rapy/irradiation <strong>the</strong>rapy.<br />
labmedicine.com November 2006 � Volume 37 Number 11 � LABMEDICINE 687
Review<br />
Comment: More than 50% <strong>of</strong> tumor tissue in this case was<br />
composed <strong>of</strong> Schwannian stroma. Microscopic nests <strong>of</strong> neuroblasts,<br />
differentiating neuroblasts, and maturing ganglion cells in a<br />
background <strong>of</strong> neuropil were clearly recognizable, but well<br />
blended in <strong>the</strong> surrounding Schwannian stromal tissue. This is a<br />
transitional form to ganglioneuroma, [ie, fully mature form <strong>of</strong><br />
pNTS where <strong>the</strong> tumor tissue is predominantly composed <strong>of</strong><br />
Schwannian stroma (Schwannian stroma-dominant) with individually<br />
scattered ganglion cells]. Both ganglioneuroblastoma,<br />
intermixed and ganglioneuroma, are commonly diagnosed in<br />
older children and young adults, and always associated with an<br />
excellent prognosis <strong>of</strong> <strong>the</strong> patients. They do not have MYCN<br />
amplification, and flow cytometry test on those tumors usually<br />
detect a diploid pattern <strong>of</strong> Schwannian stromal cells ra<strong>the</strong>r than<br />
a hyperdiploid (near-triploid) pattern <strong>of</strong> biologically favorable<br />
neuroblastic/ganglion cells.<br />
Case 6: A 1-year and 11-month-old female with a clinical<br />
stage 2a disease <strong>of</strong> <strong>the</strong> mediastinal primary.<br />
The tumor was composed <strong>of</strong> 2 different components: one<br />
component was solid and tan-yellow, and <strong>the</strong> o<strong>the</strong>r was hemorrhagic<br />
and fragile. The former component showed an appearance<br />
<strong>of</strong> ganglioneuroblastoma, intermixed (Image 1F, left side).<br />
The latter was neuroblastoma, poorly differentiated subtype with<br />
a low MKI (Image 1F, right side). This tumor was placed into a<br />
category <strong>of</strong> ganglioneuroblastoma, nodular (composite,<br />
Schwannian stroma-rich/stroma-dominant, and stroma-poor).<br />
Because <strong>of</strong> <strong>the</strong> histologic features <strong>of</strong> <strong>the</strong> neuroblastoma component<br />
and <strong>the</strong> age <strong>of</strong> <strong>the</strong> patient at diagnosis, <strong>the</strong> case was classified<br />
into an unfavorable subset (unfavorable histology) <strong>of</strong><br />
ganglioneuroblastoma, nodular. 8 The tumor sample had nonamplified<br />
MYCN and <strong>the</strong> DNA index <strong>of</strong> 1. Level <strong>of</strong> trkAI/II<br />
expression was not tested. This is a low-risk case according to <strong>the</strong><br />
COG scheme. However, she died <strong>of</strong> progressive disease with<br />
bone metastasis 2 years after <strong>the</strong> diagnosis.<br />
Comment: This was an example <strong>of</strong> composite tumor having<br />
2 different clones. Based on our experience, prognosis <strong>of</strong> <strong>the</strong><br />
patients with <strong>the</strong> composite tumor like this one is determined by<br />
<strong>the</strong> behavior <strong>of</strong> neuroblastomatous component. The same criteria<br />
<strong>of</strong> age-appropriate evaluation <strong>of</strong> histologic features as used in<br />
Table 3_International Neuroblastoma <strong>Pathology</strong> Classification<br />
<strong>the</strong> FH and UH distinction for neuroblastoma tumors are applied<br />
to <strong>the</strong> neuroblastomatous component to distinguish favorable<br />
and unfavorable subset in this tumor category. 8<br />
Discussion<br />
The International Neuroblastoma <strong>Pathology</strong> Classification<br />
(INCP) significantly distinguishes 2 prognostic groups (Table<br />
3), (ie, favorable histology group and unfavorable histology<br />
group). 6-8 As for <strong>the</strong> tumors in <strong>the</strong> categories <strong>of</strong> neuroblastoma<br />
(Schwannian stroma-poor) and ganglioneuroblastoma, nodular<br />
(composite, Schwannian stroma-dominant/stroma-rich and<br />
stroma-poor), <strong>the</strong> INPC employs an age-linked evaluation system<br />
on histologic features (grade <strong>of</strong> neuroblastic differentiation<br />
and MKI) for determining 2 prognostic groups. <strong>Tumors</strong> in <strong>the</strong><br />
categories <strong>of</strong> ganglioneuroblastoma, intermixed, and ganglioneuroma<br />
are always classified into <strong>the</strong> favorable histology group.<br />
As illustrated above Cases 1, 2, 5 were <strong>the</strong> examples <strong>of</strong> <strong>the</strong><br />
favorable histology group and all <strong>the</strong> patients are alive and well.<br />
In contrast, Cases 3, 4, 6 were classified into an unfavorable histology<br />
group, and <strong>the</strong> patients died <strong>of</strong><strong>the</strong> disease.<br />
The following is a summary <strong>of</strong> clinically as well as biologically<br />
important relationships between histologic features and<br />
molecular/genomic alterations in pNTs.<br />
(1) It is well known that patients with amplified MYCN<br />
tumor have a very poor clinical outcome. 9,10 The MYCN amplification<br />
followed by excessive MYCN protein expression with subsequent<br />
myc-max heterodimer formation in <strong>the</strong> neuroblastoma<br />
cells24 is considered to be a powerful driving force for preventing<br />
cellular differentiation and increasing mitotic and karyorrhectic<br />
activities. Accordingly, MYCN amplified tumor typically shows<br />
an appearance <strong>of</strong> neuroblastoma (Schwannian stroma-poor) <strong>of</strong><br />
ei<strong>the</strong>r undifferentiated or poorly differentiated subtype with a high<br />
MKI. 21,22<br />
Favorable histology tumors are almost always MYCN nonamplified.<br />
Among <strong>the</strong> UH tumors, about 40% are MYCN amplified<br />
with an extremely poor clinical outcome <strong>of</strong> <strong>the</strong> patients,<br />
and 60% are MYCN non-amplified also with a poor prognosis<br />
<strong>of</strong> <strong>the</strong> patients.<br />
Category Favorable Histology Unfavorable Histology<br />
Neuroblastoma Grade <strong>of</strong> Differentiation MKI Grade <strong>of</strong> Differentiation MKI<br />
(Schwannian stroma-poor)<br />
Age
(2) Patients with tumors having near-diploid DNA contents<br />
have a significantly worse prognosis than those having neartriploid<br />
DNA contents. 11 The near-diploid tumors tend to have<br />
structural aberrations, such as MYCN amplification and 1p<br />
deletion, more frequently than <strong>the</strong> near-triploid tumors. It is<br />
noted that <strong>the</strong> neuroblastic cells in <strong>the</strong> favorable histology group<br />
are usually near-triploid, and Schwannian stromal cells are always<br />
diploid. It is also noted that favorable histology tumors can<br />
promote Schwannian stromal development, and come up to <strong>the</strong><br />
advanced maturational stages <strong>of</strong> ganglioneuroblastoma, intermixed<br />
(Schwannian stroma-rich), and ganglioneuroma<br />
(Schwannian stroma-dominant). Because <strong>of</strong> <strong>the</strong> difference <strong>of</strong><br />
ploidy patterns, we assume that Schwannian stromal cells<br />
(diploid) and neuroblastic cells (near-triploid) do not have a<br />
common cellular origin, and <strong>the</strong> stromal cells are recruited by<br />
<strong>the</strong> neuroblastic tumor cells. 18,19<br />
(3) TrkA (high-affinity nerve growth factor receptor),<br />
mapped to chromosome 1q21-q22 and organized into 17 exons,<br />
has 2 splice variants, trkAI (lacking mini-exon 9 in <strong>the</strong> extracellular<br />
domain) and trkAII. It is reported that patients with tumors<br />
expressing higher levels <strong>of</strong> trkAI/II have a significantly<br />
better prognosis than those expressing lower levels <strong>of</strong> trkAI/II. 13<br />
It is also reported that NGF(Nerve Growth Factor)/trkA(I/II)/<br />
Ras/MAPK signaling pathway is anti-oncogenic causing cellular<br />
differentiation, growth arrest, apoptosis, and anti-angiogenesis. 12<br />
However, our recent analysis shows that <strong>the</strong> levels <strong>of</strong> trkA expression<br />
did not add any additional prognostic information significantly<br />
to <strong>the</strong> risk model currently used by <strong>the</strong> COG<br />
Neuroblastoma Biology Study that is created by <strong>the</strong> combination<br />
<strong>of</strong> clinical stage, histopathology, and MYCN status. 25 It is<br />
also noted that neuroblastic cells having non-amplified MYCN<br />
and high levels <strong>of</strong> trkAI/II expression have a potential <strong>of</strong> agedependent<br />
differentiation after a certain in vivo latent period<br />
within a framework <strong>of</strong> <strong>the</strong> INPC system. 25<br />
Recently, Tacconelli and colleagues reported ano<strong>the</strong>r splice variant,<br />
trkAIII, and its oncogenic/tumor-promoting effect in<br />
pNTs. 26,27 This variant does not have exons 6, 7, and 9 in <strong>the</strong> extracellular<br />
domain, is NGF-unresponsive, and seems to antagonize<br />
NGF/trkA(I/II) signaling. Fur<strong>the</strong>r investigation should be required<br />
especially for clinical significance <strong>of</strong> trkAIII expression in pNTs.<br />
Summary<br />
Histopathology classification is a very useful tool for distinguishing<br />
<strong>the</strong> pNT patients who require aggressive treatment protocols<br />
from those who need no or reduced treatment modalities<br />
after biopsy/surgery. Pediatric tumors, especially pNTs, provide<br />
us with an excellent opportunity to investigate a biologically significant<br />
relationship between <strong>the</strong> genetic/molecular alterations<br />
and <strong>the</strong>ir clinical behaviors. This is one <strong>of</strong> <strong>the</strong> most exciting<br />
fields where we pathologists can play a significant role <strong>of</strong> bridging<br />
between <strong>the</strong> laboratory bench and clinical bedside. We can<br />
recognize unique morphologic features as <strong>the</strong> manifestation <strong>of</strong><br />
various genetic/molecular changes, known or still unknown,<br />
and also analyze <strong>the</strong> prognostic significance <strong>of</strong> those morphologic<br />
features for <strong>the</strong> sake <strong>of</strong> <strong>the</strong> patients. LM<br />
1. Ross JA, Severson RK, Pollock BH, et al. Childhood cancer in <strong>the</strong> United<br />
States. A geographical analysis <strong>of</strong> cases from <strong>the</strong> Pediatric Cooperative Clinical<br />
Trials groups. Cancer. 1996;77:201-207.<br />
2. Brodeur GM, Maris JM. Neuroblastoma. In: Pizzo PA, Poplack DG, editors.<br />
Principles and Practice <strong>of</strong> Pediatric Oncology (4th edition). Philadelphia:<br />
Lippincott Williams & Wilkins, 2002: 865-937.<br />
Review<br />
3. Brodeur GM. Neuroblastoma: Biological insights into a clinical enigma.<br />
Nature Rev Cancer. 2003;3:203-216.<br />
4. Brodeur GM, Pritchard J, Berthold F, et al. Revisions <strong>of</strong> <strong>the</strong> international<br />
criteria for neuroblastoma diagnosis, staging, and response to treatment. J Clin<br />
Oncol. 11:1466-1477, 1993.<br />
5. Weinstein JL, Katzenstein HM, Cohn SL. Advances in <strong>the</strong> diagnosis and<br />
treatment <strong>of</strong> neuroblastoma. Oncologist. 2003;8:278-292.<br />
6. Shimada H, Ambros IM, Dehner LP, et al. Terminology and morphologic<br />
criteria <strong>of</strong> neuroblastic tumors. Recommendations by <strong>the</strong> International<br />
Neuroblastoma <strong>Pathology</strong> Committee. Cancer. 1999;86:349-363.<br />
7. Shimada H, Ambros IM, Dehner LP, et al. The International Neuroblastoma<br />
<strong>Pathology</strong> Classification (<strong>the</strong> Shimada System). Cancer. 1999;86:364-372.<br />
8. Peuchmaur M, d’Amore ESG, Joshi VV, et al. Revision <strong>of</strong> International<br />
Neuroblastoma <strong>Pathology</strong> Classification: Confirmation <strong>of</strong> favorable and<br />
unfavorable prognostic subsets in ganglioneuroblastoma, nodular. Cancer.<br />
2003;98:2274-2281.<br />
9. Brodeur GM, Seeger RC, Schwab M, et al. Amplification <strong>of</strong> N-myc in<br />
untreated human neuroblastoma correlates with advanced disease stage.<br />
Science. 1984;224:1121-1124.<br />
10. Seeger RC, Brodeur GM, Sa<strong>the</strong>r H, et al. Association <strong>of</strong> multiple copies <strong>of</strong> <strong>the</strong><br />
N-myc oncogene with rapid progression <strong>of</strong> neuroblastomas. New Engl J Med.<br />
1985;313:1111-1116.<br />
11. Look AT, Hayes FA, Nitschke R, et al. Cellular DNA content as a predictor<br />
<strong>of</strong> response to chemo<strong>the</strong>rapy in infants with unresectable neuroblastoma.<br />
New Engl J Med. 1984;311:231-235.<br />
12. Eggert A, Ikegaki N, Liu XG, et al. TrkA signal transduction pathways in<br />
neuroblastoma. Med Pediatr Oncol. 2001;36:108-110.<br />
13. Nakagawara A, Arima-Nakagawara M, Scavarda NJ, et al. Association between<br />
high levels <strong>of</strong> expression <strong>of</strong> <strong>the</strong> TRK gene and favorable outcome in human<br />
neuroblastoma. New Engl J Med. 1993;328:847-854.<br />
14. Delattre O, Zucman J, Melot T, et al. Ewing family <strong>of</strong> tumors: A subgroup <strong>of</strong><br />
small-round-cell tumors defined by specific chimeric transcripts. N Engl J Med.<br />
1994;331:294-299.<br />
15. Teitel MA, Thompson AD, Sorensen PHB, et al. EWS/ETC fusion genes<br />
induce epi<strong>the</strong>lial and neuroectodermal differentiation in NIH3T3 fibroblasts.<br />
Lab Invest. 1999;79:1535-1543.<br />
16. Thompson AD, Teitel MA, Arvand A, Denny CT. Divergent Ewing’s sarcoma<br />
EWS/ETS fusions confer a common tumorigenic phenotype on NIH3T3 cells.<br />
Oncogene. 1999;18:5506-5513.<br />
17. Mora J, Cheung N-K, Juan G, et al. <strong>Neuroblastic</strong> and schwannian stroma cells<br />
<strong>of</strong> neuroblastoma are derived from a tumoral progenitor cell. Cancer Res.<br />
2001;61:6892-6898.<br />
18. Ambros IM, Zellner A, Roald A, et al. Role <strong>of</strong> ploidy, chromosome 1p, and<br />
Schwann cells in <strong>the</strong> maturation <strong>of</strong> neuroblastoma. N Engl J Med.<br />
1996;334:1505-1511.<br />
19. Ambros IM, Attarbaschi A, Rumpler S, et al. Neuroblastoma cells provoke<br />
Schwann cell proliferation in vitro. Med Pediatr Oncol. 2001;36:163-168.<br />
20. Tornoczky T, Kalman E, Kajtar PG, et al. Large cell neuroblastoma: A distinct<br />
phenotype with aggressive clinical behavior. New entity? Cancer.<br />
2004;100:390-397.<br />
21. Shimada H, Stram DO, Chatten J, et al. Identification <strong>of</strong> subsets <strong>of</strong><br />
neuroblastoma by combined histopathologic and N-myc analysis. J Natl<br />
Cancer Inst. 1995;19:1470-1476.<br />
22. Goto S, Umehara S, Gerbing RB, et al. Histopathology and MYCN status in<br />
peripheral neuroblastic tumors: A report from <strong>the</strong> Children’s Cancer Group.<br />
Cancer. 2001;92:2699-2708.<br />
23. Kobayashi C, Monforte-Munoz H, Gerbing RB, et al. Enlarged and prominent<br />
nucleoli may be indicative <strong>of</strong> MYCN amplification: A study <strong>of</strong> neuroblastoma<br />
(Schwannian stroma-poor), undifferentiated/poorly differentiated subtype with<br />
a high mitosis-karyorrhexis index. Cancer. 2005;103:174-180.<br />
24. Wenzel A, Cziepluch C, Hamann U, et al. The N-Myc oncoprotein is<br />
associated in vivo with <strong>the</strong> phosphoprotein Max (P20/22) in human<br />
neuroblastoma cells. EMBO J. 1991;10:3703-3712.<br />
25. Shimada H, Nakagawa A, Peters J, et al. TrkA expression in peripheral<br />
neuroblastic tumors: Prognostic significance and biological relevance. Cancer.<br />
2004;101:1873-1881.<br />
26. Tacconelli A, Farina AR, Cappabianca L, et al. TrkA alternative splicing: A<br />
regulated tumor-promoting switch in human neuroblastomas. Cancer Cell.<br />
2004;6:347-360.<br />
27. Tacconelli A, Farina AR, Cappabianca L, et al. TrkAIII. A novel hypoxiaregulated<br />
alternative TrkA splice variant <strong>of</strong> potential physiological and<br />
pathological importance. Cell Cycle. 2005;4:8-9.<br />
labmedicine.com November 2006 � Volume 37 Number 11 � LABMEDICINE 689