may edition file
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
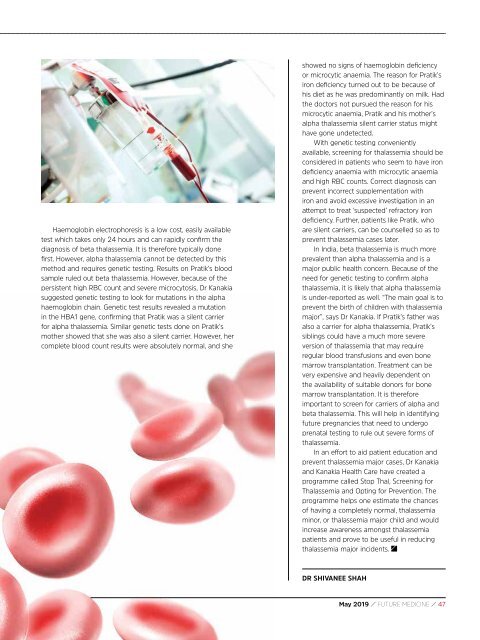
Haemoglobin electrophoresis is a low cost, easily available<br />
test which takes only 24 hours and can rapidly confirm the<br />
diagnosis of beta thalassemia. It is therefore typically done<br />
first. However, alpha thalassemia cannot be detected by this<br />
method and requires genetic testing. Results on Pratik’s blood<br />
sample ruled out beta thalassemia. However, because of the<br />
persistent high RBC count and severe microcytosis, Dr Kanakia<br />
suggested genetic testing to look for mutations in the alpha<br />
haemoglobin chain. Genetic test results revealed a mutation<br />
in the HBA1 gene, confirming that Pratik was a silent carrier<br />
for alpha thalassemia. Similar genetic tests done on Pratik’s<br />
mother showed that she was also a silent carrier. However, her<br />
complete blood count results were absolutely normal, and she<br />
showed no signs of haemoglobin deficiency<br />
or microcytic anaemia. The reason for Pratik’s<br />
iron deficiency turned out to be because of<br />
his diet as he was predominantly on milk. Had<br />
the doctors not pursued the reason for his<br />
microcytic anaemia, Pratik and his mother’s<br />
alpha thalassemia silent carrier status might<br />
have gone undetected.<br />
With genetic testing conveniently<br />
available, screening for thalassemia should be<br />
considered in patients who seem to have iron<br />
deficiency anaemia with microcytic anaemia<br />
and high RBC counts. Correct diagnosis can<br />
prevent incorrect supplementation with<br />
iron and avoid excessive investigation in an<br />
attempt to treat ‘suspected’ refractory iron<br />
deficiency. Further, patients like Pratik, who<br />
are silent carriers, can be counselled so as to<br />
prevent thalassemia cases later.<br />
In India, beta thalassemia is much more<br />
prevalent than alpha thalassemia and is a<br />
major public health concern. Because of the<br />
need for genetic testing to confirm alpha<br />
thalassemia, it is likely that alpha thalassemia<br />
is under-reported as well. “The main goal is to<br />
prevent the birth of children with thalassemia<br />
major”, says Dr Kanakia. If Pratik’s father was<br />
also a carrier for alpha thalassemia, Pratik’s<br />
siblings could have a much more severe<br />
version of thalassemia that <strong>may</strong> require<br />
regular blood transfusions and even bone<br />
marrow transplantation. Treatment can be<br />
very expensive and heavily dependent on<br />
the availability of suitable donors for bone<br />
marrow transplantation. It is therefore<br />
important to screen for carriers of alpha and<br />
beta thalassemia. This will help in identifying<br />
future pregnancies that need to undergo<br />
prenatal testing to rule out severe forms of<br />
thalassemia.<br />
In an effort to aid patient education and<br />
prevent thalassemia major cases, Dr Kanakia<br />
and Kanakia Health Care have created a<br />
programme called Stop Thal, Screening for<br />
Thalassemia and Opting for Prevention. The<br />
programme helps one estimate the chances<br />
of having a completely normal, thalassemia<br />
minor, or thalassemia major child and would<br />
increase awareness amongst thalassemia<br />
patients and prove to be useful in reducing<br />
thalassemia major incidents.<br />
DR SHIVANEE SHAH<br />
May 2019 / FUTURE MEDICINE / 47