Heartbeat April 2020
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
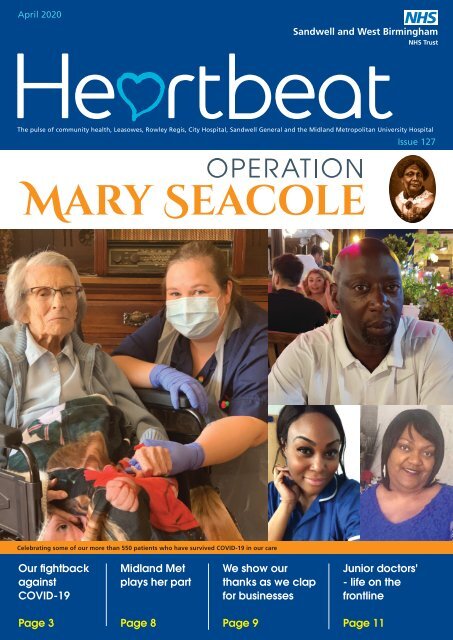
<strong>April</strong> <strong>2020</strong><br />
Sandwell and West Birmingham<br />
NHS Trust<br />
The pulse of community health, Leasowes, Rowley Regis, City Hospital, Sandwell General and the Midland Metropolitan University Hospital<br />
Issue 127<br />
Pages 4-6<br />
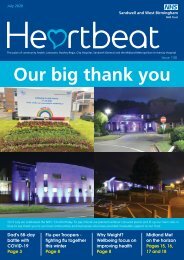
Celebrating some of our more than 550 patients who have survived COVID-19 in our care<br />
Our fightback<br />
against<br />
COVID-19<br />
Midland Met<br />
plays her part<br />
We show our<br />
thanks as we clap<br />
for businesses<br />
Junior doctors'<br />
- life on the<br />
frontline<br />
Page 3<br />
Page 8<br />
Page 9<br />
Page 11
Welcome to your <strong>April</strong> edition<br />
of <strong>Heartbeat</strong>.<br />
This month we bring you<br />
everything you need to know<br />
about COVID-19 from around our<br />
Trust. We also celebrate some of<br />
our survivors' inspirational stories.<br />
You’ll see a few photos shared in<br />
this edition with colleagues sitting<br />
or standing close to each other.<br />
Please note these were taken prior<br />
to <strong>2020</strong> BC (before coronavirus)<br />
Enjoy!<br />
HELLO<br />
Contact us<br />
Communications Team<br />
Ext 5303<br />
swbh.comms@nhs.net<br />
Communications Department<br />
Ground Floor, Trinity House<br />
Sandwell Hospital<br />
Published by<br />
Communications Team<br />
Sandwell and West Birmingham<br />
Hospitals NHS Trust<br />
Designed by<br />
Medical Illustration,<br />
Graphics Team<br />
Sandwell and West Birmingham<br />
Hospitals NHS Trust<br />
FROM THE CHAIR<br />
Leadership during the<br />
Pandemic<br />
I am sure that the impact of the<br />
COVID-19 will be a long term part of<br />
the culture of our workplace in the<br />
years ahead. The support the Trust are<br />
committing to provide to mental health<br />
organisation-wide will be with us for<br />
the long term, and I have asked Lesley<br />
Writtle, our new non-executive director,<br />
and ex-chief executive of the Black<br />
Country Partnership NHS Foundation<br />
Trust to advise us on the effectiveness<br />
of that offer as we look to make sure<br />
that you have the help you need next<br />
year and this one. Richard Burnell’s<br />
short videos have been in our bulletins<br />
and are worth coming back to and<br />
reflecting on.<br />
Simon Stevens has indicated that we are<br />
moving towards the restoration of services<br />
alongside COVID-19. We have reserved<br />
some facilities, notably the Birmingham<br />
Treatment Centre, with that in mind, and I<br />
know that Liam and Toby, alongside Paula<br />
and David, are working to put into place<br />
our restoration plans in May.<br />
Both local authorities have mobilised on<br />
a major scale to support us, but especially<br />
to supporting the most vulnerable in our<br />
communities. Yvonne Davies, as leader of<br />
Sandwell Council, has ensured that food<br />
provision is distributed across the borough.<br />
Meanwhile, you will know that Paulette<br />
Hamilton, Chair of Birmingham Health and<br />
Wellbeing Board, has led calls for action<br />
on the deaths of black and minority ethnic<br />
care staff, as well as patients. The Trust<br />
associates itself with both campaigns, and<br />
we have played our part in each.<br />
role to play as an independent overseer<br />
of the forward focus - looking at the risks<br />
and implications beyond the initial surge<br />
plans, the ongoing wellbeing of staff,<br />
the disruption of services for non-COVID<br />
diseases and conditions. Importantly, that<br />
includes how we capitalise on some of the<br />
gains which will be realised on the rapid<br />
changes our teams have been making and<br />
the quality improvement as a result. The<br />
Board is also clear that COVID-19 staffing<br />
changes are temporary and revised staffing<br />
ratios are not with us for the longer term.<br />
Thank you to all of you who have been in<br />
touch to let me know how things feel for<br />
you on the ground. It is appreciated. And<br />
thank you to every colleague who is part<br />
of our continued outstanding response<br />
to this health crisis. The character of our<br />
Trust shines through in our response. I<br />
was delighted to see the Clap For Business<br />
activities a fortnight ago, as we look to<br />
the long term economic response of the<br />
country. With the approval of our car park<br />
applications, we can now go forward for<br />
our plans to release land for development,<br />
support better housing locally, and invest in<br />
creating wealth for the long term. Our 2025<br />
ambitions are alive and well – but they play<br />
second fiddle to the kindness of our work<br />
to support everyone effected by this awful<br />
virus.<br />
Richard Samuda, Trust Chairman<br />
Submit an idea<br />
If you’d like to submit an idea<br />
for an article, contact the<br />
communications team<br />
Ext 5303<br />
swbh.comms@nhs.net<br />
Stay updated<br />
We send out a Communications<br />
Bulletin via email every day and you<br />
can now read <strong>Heartbeat</strong> articles<br />
throughout the month on Connect.<br />
Don't forget you can follow us on:<br />
From talking to partners, and to chairs of<br />
neighbouring organisations, I am clear how<br />
impressive our Trust's response has been<br />
- whether it be our transparent and open<br />
communication with you, how we have<br />
handled the provision of PPE, the support<br />
we have provided to partner organisations<br />
or our pre-emptive actions in key areas such<br />
as testing. We need to keep going, even<br />
though I know it is painful and hard, as<br />
these challenges will be with us through the<br />
second surge and deep into the summer.<br />
Ensuring appropriate governance of the<br />
organisation is as important now as ever<br />
and we have continued our Board and<br />
non-executive-led committee meetings<br />
virtually, accepting that the Trust’s response<br />
to COVID-19 is the key feature of those<br />
meetings. The Board has an important<br />
Chairman, Richard Samuda
Surging forward – our fight back<br />
against COVID-19<br />
Day to day life as we knew it has<br />
changed immeasurably across our Trust<br />
in the last few weeks. We have all<br />
pulled together and accommodated a<br />
lot of change to help fight back against<br />
the spread of COVID-19. Undoubtedly,<br />
this pandemic has brought with it<br />
stresses and strains, but our Trust has<br />
risen courageously to the challenge and<br />
together we are making progress.<br />
To ensure we were able to manage the<br />
surge of cases we have set up a series of<br />
new arrangements including:<br />
• Creating hot (red) and cold (blue)<br />
streams for COVID positive or<br />
suspected patients and patients with<br />
no COVID symptoms<br />
• Creating additional capacity for<br />
COVID patients at City and Sandwell<br />
Hospitals<br />
• Creating additional intensive care unit<br />
(ICU) capacity and expanding our<br />
non-invasive ventilation capacity<br />
• Stopping elective surgery and moving<br />
our cancer services off-site<br />
• Moving to telephone and virtual<br />
consultations and only keeping<br />
clinically urgent outpatient<br />
appointments and essential<br />
diagnostics<br />
• Moving 150 nurses into critical care<br />
and 100 nurses into base wards.<br />
Wards have changed from blue to red to<br />
accommodate the increase in COVID-19+<br />
patients. This, in turn has meant we<br />
have needed extra nursing staff on our<br />
wards and trained to work in critical<br />
care. Other training has followed with<br />
colleagues working on our wards and in our<br />
emergency departments.<br />
The opening of the Nightingale Hospital in<br />
Birmingham sees our region expanding its<br />
capacity as a whole to deal with up to an<br />
additional 4,000 patients in a worst-case<br />
scenario. We are actively playing our part<br />
and 20 of our nurses have been seconded<br />
to work at the hospital currently.<br />
For our part, Operation Mary Seacole is<br />
how we have chosen to refer to our efforts<br />
COVID-19<br />
to tackle this pandemic. An exemplary<br />
nurse, Mary was voted the greatest ever<br />
Black Briton in 2004. Many of you are<br />
experiencing this pandemic first hand,<br />
acting selflessly as Mary once did to look<br />
after the unwell.<br />
Given the scale of our operation, we<br />
have chosen Mary as our figurehead in<br />
fighting this pandemic. As a Trust, we<br />
celebrate that many of our colleagues<br />
come from different traditions, faiths,<br />
and communities. It is what makes us<br />
stronger and, more united in our fight<br />
against COVID-19, an illness that is<br />
disproportionately affecting some<br />
local people.<br />
Thank you for all you have done.<br />
We will keep moving forward, and<br />
together we will see this through.<br />
We hosted our first blue brigade event with colleagues being trained to support our portering teams<br />
3
106-year-old Connie bounces back<br />
after beating virus<br />
COVID-19 SURVIVORS<br />
Meet 106-year-old Connie Titchen.<br />
She is believed to be Britain’s oldest<br />
patient to overcome coronavirus, cared<br />
for by colleagues at City Hospital. The<br />
great grandmother of eight battled<br />
the virus for just less than three weeks<br />
and was given a clean bill of health by<br />
medics earlier this month.<br />
Connie, who was born in 1913, has<br />
lived through two World Wars. She<br />
was admitted to City Hospital in mid-<br />
March with suspected pneumonia and<br />
was diagnosed with coronavirus soon<br />
afterwards. Connie said: “I feel very lucky<br />
that I have fought off this virus. I can’t wait<br />
to see my family.”<br />
Connie’s granddaughter, Alex Jones, said<br />
her Nan bounces back from anything.<br />
“She has had an active life. She loved to<br />
dance, cycle and play golf. She has always<br />
cooked for herself too, although she likes a<br />
cheeky McDonalds now and then. I haven’t<br />
told her they are closed. I think the secret<br />
of her old age is that she is physically<br />
active and very independent. She had<br />
a hip operation in December and within<br />
30 days she was walking again. She is<br />
Connie Titchen with Sister, Kelly Smith<br />
amazing, and I know all the family can’t<br />
wait to see her.”<br />
Alex added: “The care she has received at<br />
the hospital has been brilliant and I can’t<br />
fault it. During her stay, I was kept updated<br />
constantly by the nurses looking after her<br />
and that made me happy. I want to thank<br />
the staff for all they have done for her<br />
during her stay.”<br />
Sister, Kelly Smith, who looked after Connie<br />
added: “It’s been fantastic to see Connie<br />
recover. She is amazing, and we did our<br />
best to nurse her back to health. We were<br />
pleased when she was given the all-clear. It’s<br />
nice to see patients leave our ward having<br />
beaten this virus.”<br />
Morine on the road to recovery<br />
following coronavirus scare<br />
A care manager from a Halesowen<br />
based housing association is urging<br />
everyone to take the coronavirus<br />
seriously.<br />
Morine Burrell-Banton is on the road to<br />
recovery at home after being discharged<br />
from hospital on 7 <strong>April</strong>. “As most<br />
people would be, I was initially scared<br />
about contracting the virus but all the<br />
nurses and doctors were fantastic in<br />
helping me get better,” said Morine.<br />
Morine was admitted to City Hospital<br />
site on 4 <strong>April</strong> after experiencing<br />
a higher temperature than normal<br />
and a persistent cough. She initially<br />
self-isolated, but after her symptoms<br />
gradually got worse and her health<br />
started to deteriorate further, she was<br />
admitted to hospital where she spent<br />
three days in our care.<br />
She said: “All the staff were great and<br />
very attentive to everything I needed even<br />
though they were busy with lots of other<br />
patients as well as me. I believe this is one<br />
of the main reasons for helping me stay<br />
positive but more importantly, it aided my<br />
recovery to better health.”<br />
Since her discharge, hour by hour, day by<br />
day, Morine is slowly getting back to 100<br />
per cent, however, she is pleading with<br />
the public to follow the social distancing<br />
guidance and only go out for essential<br />
journeys.<br />
“It’s disappointing that there are still some<br />
people choosing to ignore the advice from<br />
the government. Coronavirus is no joke<br />
and something we should all take very<br />
seriously. Though the majority of people<br />
are eventually getting better, unfortunately,<br />
some people are still dying which is why<br />
everyone must follow the guidance. The<br />
virus doesn’t discriminate.”<br />
Morine is currently resting at home with her<br />
family and hopes to return to work once<br />
the lockdown restrictions have been lifted.<br />
Morine is now recovering at home<br />
4
COVID-19 positive nurse urges people<br />
to seek hospital help for disease<br />
Charlene Nelson, who works as a bank<br />
nurse at Sandwell Hospital<br />
COVID-19 SURVIVORS<br />
Dad of one reveals how he beat<br />
coronavirus<br />
A dad of one who battled coronavirus<br />
from his intensive care bed revealed<br />
how thinking positively helped him<br />
recover. Anthony Morrison, aged 55,<br />
spent a week in City Hospital where he<br />
was ventilated after being diagnosed<br />
with the disease.<br />
“Many people think that having coronavirus<br />
is a death sentence, but that isn’t the case,”<br />
said Anthony. “I was in a bad way, but I<br />
pulled through, and people out there need<br />
to know that just because you have the<br />
illness does not mean you are going to pass<br />
away. I have a friend who has had it and<br />
she has also recovered.”<br />
Anthony first experienced symptoms on<br />
his way home from work. A couple of days<br />
later he began suffering headaches and<br />
had a high temperature. His wife called<br />
paramedics and initially, he was told to take<br />
paracetamol, but his symptoms didn’t ease<br />
and he collapsed.<br />
“The paramedics rushed me to hospital<br />
and once I was there it was confirmed I<br />
Colleague Charlene Nelson who<br />
battled coronavirus has urged people<br />
to seek medical help sooner if they<br />
feel they are deteriorating. The nurse,<br />
who is currently recovering at her<br />
home, was able to fight off the<br />
disease after spending just under a<br />
week in the hospital.<br />
Charlene, who works as a bank nurse at<br />
Sandwell Hospital, said she started suffering<br />
shortness of breath on 12 <strong>April</strong>. “I just<br />
couldn’t breathe. I called for an ambulance,<br />
and it all felt like a big blur. I got into A&E<br />
and I was put into isolation because of<br />
my symptoms."<br />
Charlene was taken to Sandwell Hospital<br />
and said: “If I hadn’t dialled 999, who<br />
knows what sort of condition I would be in<br />
now. The care I received was brilliant, and<br />
colleagues are doing everything they can<br />
to help patients. I am so much better than<br />
I was a week ago. I’m just glad that I got<br />
treatment when I did.”<br />
She added: “I was treated with antibiotics<br />
and tested for coronavirus. Because of<br />
my kidney condition, I was transferred to<br />
another hospital for further treatment. My<br />
results for COVID-19 came back positive. I<br />
had coronavirus,” he recalled. “My oxygen<br />
levels were really low and I was in intensive<br />
care. I knew I had to fight this disease, and I<br />
practised deep breathing techniques. I knew<br />
that I couldn’t let it beat me. It was difficult,<br />
but I knew I had to remain positive. I think<br />
that is a key factor with this illness.<br />
“Also, hearing from my relatives picked<br />
me up and when I received two handmade<br />
cards from my grandnieces that picked me<br />
up. Their messages touched my heart. I<br />
knew I had to get out of the hospital and<br />
see them again. There were small things too<br />
that I tried to do whilst I was in the hospital.<br />
I would set myself goals - every day I made<br />
sure I was able to do something that would<br />
help me in my recovery.<br />
Anthony thanked our staff for the way he<br />
was looked after. “The care I received was<br />
brilliant, right from the domestics to the<br />
doctors, everyone looked after me well.”<br />
Having now returned home, Anthony is<br />
resting until he is fit to return to work. His<br />
message to people out there is simple.<br />
was in a bad way for the first two<br />
days, and I was very scared. I soon<br />
started responding to the treatment<br />
and began improving.”<br />
“I think there may be people out there<br />
who think they don’t need to go to the<br />
hospital or believe that their situation<br />
will worsen if they do go. However, my<br />
condition improved. I would also like to<br />
strongly urge people to stay indoors to<br />
protect those who are most vulnerable in<br />
our society.”<br />
Charlene said she doesn’t know how<br />
she contracted the disease as she had<br />
been wearing the correct PPE during her<br />
time working at the hospital and had<br />
not been treating COVID-19 patients.<br />
“It could have been from handling post<br />
or when I was food shopping. I suppose<br />
we’ll never know where I got it from,<br />
which just shows how cautious we need<br />
to be.”<br />
Get well soon, Charlene.<br />
“I really would say to people to stay<br />
positive. You can fight this disease, and I<br />
am an example of that.”<br />
Anthony Morrison beat coronavirus<br />
5
Brave doctor puts the NHS first in<br />
our battle to beat COVID-19<br />
COVID-19<br />
As we find ourselves amid a global<br />
pandemic it is stories of selflessness<br />
and sacrifice that are bringing hope<br />
to many people at this difficult time.<br />
Now more than ever, our nation has<br />
shown just how much it appreciates<br />
the work we are all doing to protect<br />
lives whilst battling this unknown<br />
and dangerous virus.<br />
Our healthcare system is a melting pot<br />
of talented people, all specialists in their<br />
areas, with some people choosing to join<br />
the NHS from outside of the UK. One<br />
such person is Dr Gerald Rajakulenthiran<br />
Santhiyapillai, a young doctor who<br />
became part of our Trust just six months<br />
ago from Sri Lanka.<br />
Having moved to the UK with his family,<br />
Dr Santhiyapillai has quickly become a<br />
well-regarded member of the cardiology<br />
team. He joined our organisation<br />
through the Medical Trainee Initiative<br />
(MTI) via the Royal College of Physicians in<br />
London. This national scheme allows junior<br />
doctors to work and train in the UK for<br />
up to 24 months before returning to their<br />
home countries. For the NHS, it means we<br />
get to work with and train up some of the<br />
most talented, young, international medical<br />
graduates.<br />
As the COVID-19 crisis began to unfold,<br />
the Sri Lankan government contacted<br />
doctors that were part of the MTI and made<br />
provisions for them to return home. Upon<br />
being contacted, Dr Santhiyapillai arranged<br />
to send his family home but decided to stay<br />
in the UK to help us battle the outbreak.<br />
Speaking exclusively to <strong>Heartbeat</strong>, he said:<br />
‘My wife and I decided that my family<br />
should return home to Sri Lanka where they<br />
could be surrounded by our family. I chose<br />
to stay here in the UK because I have taken<br />
the Hippocratic Oath. I have a duty of care<br />
towards my patients; I will not leave or<br />
resign at this time of crisis.’<br />
Understandably this altruistic act has<br />
not gone unnoticed. Dr Fairoz B Abdul,<br />
Consultant Interventional Cardiologist,<br />
commented: ‘Our department is incredibly<br />
touched by this act of selfless commitment.<br />
It has raised the morale of the team, made<br />
us stronger, more resilient and even more<br />
dedicated to beating COVID-19.<br />
He added: ‘Other registrars have since<br />
put themselves forward for the COVID-19<br />
rota without hesitation, knowing only too<br />
well the risks they face to their health. Dr<br />
Santhiyapillai has inspired our team and,<br />
we feel there is a strengthened sense of<br />
commitment despite the adverse situation<br />
we find ourselves in.’<br />
Chetan Varma, Consultant Cardiologist and<br />
Group Director, Medicine and Emergency<br />
Care added: ‘Dr Santhiyapillai is a<br />
hardworking, intelligent and efficient doctor<br />
who has adapted very quickly to working<br />
within the NHS. His kindness, generosity<br />
and dedication to our Trust is nothing<br />
short of inspiring. Like so many other key<br />
workers, he continues to come into work in<br />
these uncertain times and puts the lives of<br />
patients’ first. I would like to thank him and<br />
the rest of the team for their dedication.’<br />
Dr Gerald Rajakulenthiran Santhiyapillai pictured with his family<br />
6
Nice two metres, two metres nice:<br />
The importance of social distancing<br />
COVID-19<br />
to your role. If not, speak to<br />
your manager to clarify if you<br />
can do so.<br />
• Use telephone or online services<br />
to contact your GP or other<br />
essential services.<br />
Midwives socially distancing outside St James Medical Centre<br />
It may sound simple; wash your hands<br />
more often and for 20 seconds or longer.<br />
How many of us in reality though do<br />
that regularly throughout the day?<br />
There may be a temptation to give your<br />
hands a quick wash after the 10th time<br />
or perhaps squeeze past someone in the<br />
supermarket, but with COVID-19 cases<br />
increasing, we must observe the social<br />
distancing guidelines set out for us by<br />
the government.<br />
Done properly social distancing is in<br />
place to help reduce the transmission<br />
of COVID-19. Across the UK we are<br />
being asked to:<br />
• Avoid contact with someone who<br />
is displaying symptoms of<br />
COVID-19.These symptoms include<br />
high temperature and/or a new<br />
and continuous cough.<br />
• Avoid non-essential use of<br />
public transport.<br />
• Maintain a distance of two metres<br />
from those around you when in<br />
public places.<br />
• Work from home, where possible.<br />
This is something you should have<br />
already had a conversation about<br />
with your manager if this applies<br />
Following these guidelines is<br />
particularly important if you:<br />
• Are over 70<br />
• Have an underlying health<br />
condition<br />
• Or are pregnant.<br />
Other ways you can help prevent the<br />
spread of infection include:<br />
• Washing your hands more often.<br />
Alternatively, use a sanitiser<br />
throughout the day, when you<br />
blow your nose, sneeze, cough or<br />
eat or handle food. Clinical<br />
colleagues, in particular, are<br />
reminded of the five moments of<br />
handwashing.<br />
• Avoid touching your eyes, nose,<br />
and mouth with unwashed hands<br />
• Cover your cough or sneeze with<br />
a tissue, then throw the tissue in<br />
a bin and wash your hands<br />
• Clean and disinfect frequently<br />
touched objects and surfaces in<br />
the home.<br />
People across the UK have received letters<br />
from the Prime Minister asking them to<br />
stay home, protect the NHS and save lives.<br />
Five moments of<br />
handwashing<br />
1. Before touching<br />
a patient<br />
2. Before clean/aseptic<br />
procedures<br />
3. After body fluid<br />
exposure/risk<br />
4. After touching<br />
a patient<br />
5. After touching patient<br />
surroundings.<br />
7
Midland Met plays her part to lead<br />
coronavirus testing<br />
COVID-19<br />
Our new University Hospital<br />
proposed to have the busiest<br />
A&E in Europe and scheduled for<br />
completion in 2022 has become<br />
the testing bed of the Midlands for<br />
coronavirus.<br />
The Midland Metropolitan University<br />
Hospital has officially opened up to our<br />
community colleagues as well as primary<br />
care, social care and other public sector<br />
workers across the region to get tested<br />
for COVID-19.<br />
Our Midland Met testing site has<br />
become Birmingham’s second mass<br />
testing centre and will help boost tests<br />
numbers within the local area. One of<br />
the key factors in making this decision<br />
was having studied countries such as<br />
South Korea and Italy, the Trust was<br />
convinced that both colleague and<br />
community testing targeted and well<br />
delivered, is important in trying to<br />
control the pandemic.<br />
Appointment slots will be allocated<br />
and our ambition is to test hundreds<br />
of people a week. We hope that by<br />
testing more of our local community, we<br />
will enable key workers to continue to<br />
do the essential work they need to do<br />
Midland Met has become a testing bed of the Midlands for coronavirus<br />
whilst keeping themselves and others free of<br />
the virus.<br />
Toby Lewis, Chief Executive, believes increased<br />
testing will help the fight against coronavirus.<br />
He said: “Our Trust has been one of the<br />
biggest testing NHS bodies over the last three<br />
weeks and we are thrilled to be launching<br />
this service for transport workers, GPs, refuge<br />
workers, social workers and emergency<br />
service staff. Midland Met is more than a<br />
hospital.”<br />
He added: “We will continue to test across<br />
our Sandwell and City sites, but with the help<br />
of friends at Balfour Beatty we can increase<br />
testing massively. This will be crucial in<br />
not only reducing the first surge but also<br />
better managing the second curve in later<br />
months.”<br />
If you believe you have symptoms<br />
of COVID-19 and need testing,<br />
please call 0121 507 2664 and<br />
choose option 5. If you are selfisolating<br />
because of a family<br />
member they too can be tested<br />
by contacting the same number<br />
including children.<br />
8
Over 300 colleagues benefit from hotel<br />
accommodation to protect themselves an<br />
Top quality hotel rooms are still available<br />
if you feel you need to move into one.<br />
Please consider this seriously if you are<br />
recognising that for the next little while<br />
the best answer for you, your work, and<br />
your loved ones is separation.<br />
As part of our plan to manage the pandemic,<br />
we need to have the right workforce at work<br />
and keep absence of all types below 30 per<br />
cent.<br />
Hotels we are currently using include:<br />
• Mercure Hotel, West Bromwich<br />
• Holiday Inn Express, St Chads,<br />
Birmingham<br />
• Holiday Inn Express, Oldbury<br />
• Serviced City Apartments Ltd.<br />
Any patient-facing colleagues including ward<br />
service officers and porters can have access<br />
to our reserved rooms to enable you to be<br />
away from a household with someone who<br />
has symptoms. We strongly recommend<br />
that patient-facing colleagues take up this<br />
provision so that you can continue providing<br />
your vital service to our patients.<br />
Mark Whitehouse, Head of Patient Access<br />
& Planned Care, told us: “The main perk of<br />
staying in the hotel is reducing the risk of<br />
taking anything back to the family on a daily<br />
basis. I would encourage staff to book a room<br />
if they are at all worried about transporting<br />
the flu from work to home. The rooms at The<br />
Mercure are big and for your one hour exercise<br />
the hotel is located right next to Sandwell<br />
Valley Park.”<br />
Staying in a hotel may increase the risk of<br />
passing the virus between colleagues working<br />
in different environments. National guidance is<br />
that where possible:<br />
• Minimise time in communal areas of the<br />
hotel including receptions and corridors<br />
to reduce risk of infection to colleagues.<br />
• Where possible, to limit to one or two<br />
people at a time in lifts where possible,<br />
or to use the stairs if appropriate.<br />
• Ideally eat in your room. If meals are<br />
provided within the hotel, please try to<br />
sit at tables at least two metres apart<br />
from other residents in any bar or<br />
restaurant.<br />
We will be working with the hotels and<br />
providing guidance so they are aware of this<br />
and are working to support you.<br />
COVID-19<br />
To book your room email<br />
swbh.hotel-booking@nhs.net<br />
We still have hotel rooms available. Please<br />
take advantage of them if you want and<br />
are able to.<br />
We clap for businesses that have<br />
supported our Trust<br />
Earlier this month, we unveiled “thank<br />
you” banners recognising businesses in<br />
the area which have come to the aid of<br />
our organisation during the pandemic.<br />
The signs were revealed at City Hospital<br />
where colleagues gathered on 15 <strong>April</strong>,<br />
to clap for businesses.<br />
Despite many companies feeling the strain<br />
of lockdown, they have helped to ensure<br />
supplies of consumables, equipment and<br />
food are still being provided. As a sign<br />
of our continued thanks, our Trust will<br />
continue to add names of other companies<br />
to the signs over the coming weeks. This<br />
includes firms building special equipment<br />
on the organisation’s behalf.<br />
Toby Lewis, Chief Executive, said: “At the<br />
time when our NHS has most needed it,<br />
local businesses have come forward to<br />
offer us help, even when they have been<br />
struggling with the impact of lockdown.<br />
Just as people come out every week to clap<br />
for our carers, today we want to show our<br />
appreciation for the fantastic support we<br />
have had from suppliers that enables us to<br />
care for patients and colleagues throughout<br />
this pandemic.”<br />
Paul Faulkner, CEO of Greater Birmingham<br />
Chambers of Commerce, said: “This is a<br />
lovely display of thanks to all the many<br />
businesses who have stepped forward at<br />
this time to provide support for the patients<br />
and staff at the Trust. Of course, we all<br />
think that it is the staff working throughout<br />
Colleagues come together to clap for businesses<br />
the NHS, and in other critical care roles,<br />
who are the true heroes. This gesture helps<br />
to highlight how business is also a force for<br />
good and demonstrates the way people<br />
across our society and communities are<br />
pulling together at this difficult time.”<br />
9
Virtual is now a reality across our<br />
workplace<br />
COVID-19<br />
The COVID-19 pandemic has<br />
drastically changed the way we all<br />
work with teams constantly looking<br />
at different approaches to meet the<br />
daily challenges presented by the<br />
pandemic.<br />
One thing we have all embraced during<br />
this pandemic is the use of technology<br />
with WebEx meetings and events<br />
becoming the norm. Part of this digital<br />
‘revolution’ has also seen clinics being<br />
done digitally using an online tool called<br />
Visionable.<br />
Mark Whitehouse, Head of Patient<br />
Access & Planned Care, told <strong>Heartbeat</strong><br />
that our clinicians have been using<br />
Visionable to see their patients virtually<br />
for a number of weeks now with some<br />
great feedback.<br />
“Patients have really embraced the<br />
technology and have welcomed not<br />
having to travel to hospital for routine<br />
follow up appointments whilst also<br />
saving on taxi fares, parking fees and<br />
having to book time off from work,”<br />
said Mark.<br />
“Clinicians have also been pleased with<br />
the way Visionable works, it is secure<br />
and allows them to assess patients and<br />
call them in for a face to face if they feel<br />
that is necessary for their treatment.”<br />
Mark added: “We are only scratching<br />
the surface in terms of what the<br />
technology can do. It is possible for<br />
instance for clinicians to share x-ray<br />
results with the patient, inviting other<br />
clinicians into the consultation for<br />
second opinions and other members of<br />
the team like physios or even interpreters<br />
Taking part in a Webex virtual ward round - Jaron Kooner, Patient Access Team Leader (holding the<br />
IPAD) with Lisa Anderson, Stroke Alert Nurse and Dr Iqbal, Stroke Consultant<br />
all through virtual technology. We are liaising<br />
with colleagues to see what else they would<br />
like to do within Visionable and we will work<br />
with the supplier to ensure we are using the<br />
technology to its maximum potential.”<br />
Visionable/WebEx is also about to change the<br />
way we do ward rounds. Earlier this month<br />
Respiratory Consultant, Arvind Rajasekaran<br />
conducted a trial of a virtual ward round using<br />
Webex on Newton 3 and was positive about<br />
the outcome.<br />
He told us: “Initial feedback was very<br />
encouraging. The audio and video was very<br />
clear and patients (aged up to 70) involved in<br />
the trial were very positive too.<br />
“Although older patients (80 and above)<br />
did appear to struggle with interface, often<br />
searching for the consultant and speaking out<br />
of sync. Our recommendation is that we avoid<br />
using the technology when the ward is very<br />
busy (with bleep monitors in the back ground)<br />
as it degrades the consultation experience for<br />
both the patient and the clinician.”<br />
Arvind did not get the opportunity to test<br />
scenarios that require a sensitive conversation<br />
such as DNACPR but suggested the virtual<br />
ward would be ideal for routine ward rounds<br />
and checks on patients following a normal<br />
face to face contact.<br />
He said: “It would be great for the<br />
afternoon huddle with a quick check on a<br />
patient or two especially if the clinician is on<br />
a different site and to facilitate decisions on<br />
patient transfer. Visionable/Webex may also<br />
be suitable for weekend ward rounds where<br />
discharges can be facilitated following<br />
previously agreed plans.<br />
“Having the option of virtual ward rounds<br />
is great for colleagues although I do not<br />
anticipate that this will replace of face to<br />
face ward rounds. For the virtual ward<br />
round to work well, the junior doctor and<br />
the consultant need to ensure they study<br />
each case independently to avoid the risk of<br />
overlooking information and thus making<br />
the process safer.<br />
“The human to human non-verbal<br />
interaction that happens on a team ward<br />
round is removed and the effect of this<br />
is unclear. The environmental impact<br />
and sustainability agenda will have to be<br />
captured so involving our sustainability team<br />
would be a good idea. However, overall the<br />
virtual ward round is a positive experience.”<br />
How the virtual ward round works<br />
1. All patients are prepped by junior<br />
doctor and a summary entered on<br />
the clinical summary section of<br />
clinical workflow.<br />
2. Consultant and junior doctor agree a<br />
start time and the order of the ward<br />
round starting bay 1 bed1 etc.<br />
3. Consultant looks at the first patient<br />
summary on Unity (clinical work<br />
flow), reviews vitals, bloods, drug<br />
chart, CXR etc. In COVID-19 scenario,<br />
particular emphasis on escalation<br />
plans, previous conversations with<br />
patient and family.<br />
4. Consultant dials in using video<br />
chat function.<br />
5. Junior doctor (in full PPE) picks<br />
the call.<br />
6. Consultant and junior doctor run<br />
through the clinical summary and<br />
check understanding. If a nurse is<br />
required for the consultation, the<br />
nurse is brought into bedside.<br />
7. Junior doctor takes the IPad to<br />
patient and a consultation<br />
follows. On occasions a three-way<br />
conversation with the nurse (AHP)<br />
and the patient ensues.<br />
8. Consultation finishes with the patient<br />
9. Consultant and junior doctor agree<br />
the documentation schema.<br />
10. Consultant and trainee doctor agree<br />
which patient to see next with either<br />
the same or a different junior<br />
doctor (hands over the IPad that<br />
being the case).<br />
11. Call ends.<br />
12. Junior doctor completes the<br />
documentation as WR Dr Consultant.<br />
13. Consultant checks documentation<br />
and modifies and verifies with<br />
signature.<br />
14. Consultant looks at second patient<br />
summary on Unity (step 3).<br />
For further information about<br />
Visionable or Webex contact Mark<br />
Whitehouse markwhitehouse@nhs.net<br />
or visit https://visionable.com/videos<br />
10
Junior doctors – life on the frontline<br />
Our Trust has mobilised in a way and<br />
at a pace unknown to us before and<br />
everyone has a part to play. Colleagues<br />
from administrative functions, nurses<br />
to HCAs and of course, our medical<br />
teams, have all pulled together at this<br />
challenging time.<br />
Our junior doctors are playing a particularly<br />
significant role in this pandemic. There<br />
is a mix of experience and levels of<br />
responsibility among them, with some just<br />
newly qualified to those with a decade of<br />
practical experience working in hospitals.<br />
With approximately 53,000 junior doctors<br />
practising in England alone, they make up<br />
a sizeable part of any NHS Trust, and in<br />
ours, they are crucial in our battle against<br />
COVID-19.<br />
Speaking of the positives, Alison explained<br />
how working through this pandemic has<br />
brought a sense of camaraderie to the<br />
frontline.<br />
“We have lots of junior doctors in our<br />
Trust; some of them at the beginning<br />
of their training, whilst others like me<br />
have several years’ experience. I am very<br />
overwhelmed and impressed by how we<br />
have come together, sharing best practice,<br />
looking after each other and learning how<br />
to tackle this pandemic. I feel particularly<br />
supported by the consultants – having that<br />
senior presence has been essential. Nurses,<br />
doctors, HCAs and ward services - we've all<br />
become closer as a team.”<br />
Dr Sarah Faloon, CT2 Stroke Medicine,<br />
echoed these sentiments. She told us:<br />
“Working as a junior doctor during a<br />
global pandemic is not something I would<br />
have ever expected. I am amazed by how<br />
well everyone has pulled together and<br />
the willingness to volunteer into new and<br />
unfamiliar roles. Some of us have new<br />
responsibilities, for instance, myself and<br />
other core medical trainees have moved<br />
onto the medical registrar rota. Whilst<br />
initially daunting we have been so well<br />
supported by the consultants, other junior<br />
doctors and nursing staff.<br />
“Morale and teamwork have been fantastic.<br />
Managing sick patients is what we are<br />
trained to do; however, the increased<br />
amount of end of life care and breaking bad<br />
news, especially when we have to do this<br />
COVID-19<br />
over the telephone can be psychologically<br />
and emotionally demanding. The Trust and<br />
wellbeing team have looked after us by<br />
providing opportunities for debriefing and<br />
with their wellbeing campaign. I have been<br />
extremely moved by the public support, and<br />
I am very proud to work for the NHS as a<br />
medic here.”<br />
Professor Jawad Khan, Director of Medical<br />
Education, told us how incredibly proud<br />
he is of our junior medical colleagues.<br />
Speaking to <strong>Heartbeat</strong>, he said: “I would<br />
like to draw particular attention to the<br />
resolve, determination and bravery of our<br />
junior medical staff in facing adversity<br />
at a time which has been physically and<br />
emotionally draining. The physical demands<br />
on us as doctors are substantial. Working,<br />
whilst wearing PPE, adds considerable effort<br />
in terms of caring for patients.<br />
“The junior doctors have been pivotal in<br />
our efforts to address the surge in clinical<br />
demand. They are at the very forefront of<br />
our efforts, showing great flexibility when<br />
redeployed into new clinical environments,<br />
adapting to new roles and rotas. They have<br />
matured quickly, adjusted and remained<br />
steadfast to maintaining the highest<br />
standard of patient care. Their conduct<br />
has been exemplary. Their compassion and<br />
dedication cannot be overstated.”<br />
Dr Alison Eastaugh<br />
We caught up with Alison Eastaugh,<br />
Geriatric and Chief Medical Registrar, to<br />
find out what life on the frontline has been<br />
like for her. She told us: “I think at first<br />
anticipation and anxiety were common<br />
feelings among myself and my colleagues.<br />
There was a sense of the unknown, we<br />
weren’t sure how many patients we would<br />
see or how unwell they might be. Many of<br />
my colleagues were also being moved to<br />
other areas to provide support where they<br />
were most needed.”<br />
Working through this pandemic has<br />
brought with it some unfamiliar challenges.<br />
“Wearing personal protection equipment<br />
(PPE) all day can be very uncomfortable. It<br />
also makes communication with colleagues<br />
and patients difficult. Breaking bad news to<br />
families on the telephone is also emotionally<br />
challenging.”<br />
Some of our junior doctors at their induction in 2019 before the outbreak of COVID-19<br />
11
welearn to recognise excellence<br />
COVID-19<br />
<strong>April</strong>’s Quality Improvement Half<br />
Day (QIHD) saw the launch of<br />
welearn from excellence across our<br />
workplace.<br />
welearn from excellence provides<br />
a platform for you to recognise<br />
colleagues for their everyday brilliance.<br />
The Trust, and the whole NHS, is<br />
currently responding on a scale and at<br />
a pace never before known due to the<br />
impact of the COVID-19 pandemic.<br />
welearn from excellence will capture<br />
the learning and appreciate the amazing<br />
work that our colleagues are delivering<br />
today and every day.<br />
Positive reporting is quick and<br />
easy…<br />
Simply visit Connect and click on the<br />
welearn from excellence logo on the<br />
homepage. You will just need to answer<br />
three quick questions:<br />
• Tell us about a colleague or team<br />
whose excellence you would like<br />
to positively report<br />
• What can we learn?<br />
• Optional: How did it feel to be<br />
involved?<br />
<strong>Heartbeat</strong> caught up with Claire Hubbard,<br />
Deputy Director of Governance: Knowledge<br />
and Learning who told us more.<br />
“Although the portal has only been live for a<br />
few weeks we are delighted with the number<br />
of positive reports we have received so far.<br />
“It is clear that even though everyone is<br />
working under extreme pressure we are all still<br />
taking the time to recognise the good work<br />
that is taking place around us.<br />
“All excellence received via the portal will be<br />
positively acknowledged so that colleagues<br />
receive recognition and we can share<br />
the appreciation and learning across our<br />
workplace.”<br />
QIHD goes digital<br />
<strong>April</strong> also saw the first time that QIHD was<br />
an all-digital affair with many teams logging<br />
in via WebEx.<br />
“QIHD via WebEx has been very well<br />
received,” added Claire. “Many colleagues<br />
have commented on how they saved time<br />
as they didn’t have to travel cross-site and<br />
they were still able to see each other via<br />
WebEx!<br />
“It was good to see 422 colleagues across<br />
30 teams connect online to share learning.<br />
We will certainly support teams to continue<br />
to communicate digitally even when we do<br />
go back to business as usual.”<br />
For more information on welearn<br />
from excellence please email<br />
swbh.welearnlfe@nhs.net<br />
New volunteer role launched at<br />
the Trust<br />
With the outbreak of coronavirus<br />
across the world, our volunteer<br />
service has seized this opportunity<br />
to offer a helping hand.<br />
Our hospital sites may have gone into<br />
lockdown in recent weeks, but that<br />
hasn’t stopped us in wanting to be<br />
caring and kind and more importantly,<br />
ensure our patients are still our number<br />
one priority.<br />
With visiting restricted due to the<br />
outbreak of COVID-19, our volunteer<br />
service decided they wanted to turn this<br />
negative into a positive by launching<br />
a new role for the service - a <strong>2020</strong><br />
response volunteer.<br />
“The role of a <strong>2020</strong> response volunteer<br />
is to assist the organisation during the<br />
coronavirus pandemic,” said Patricia<br />
Hunt, Volunteer Service Manager.<br />
“All our response volunteers will be<br />
flexible and able to take on a variety of<br />
Kay is ready and rearing to support the frontline<br />
in her new response volunteer role<br />
duties from distributing information leaflets,<br />
posters to helping us with the many donations<br />
from the community and wayfinding. The<br />
role is designed to help support our frontline<br />
colleague whilst they care for our patients.”<br />
Kamal (Kay) Deep has taken up this new<br />
volunteer opportunity and is thriving in her<br />
new role. She told us: “It always feels good<br />
to be able to give back to people in my<br />
local area and help others, especially during<br />
such difficult times. If by me wayfinding or<br />
carrying out any of my other duties helps<br />
our patients and key workers, then it is a<br />
job I am proud to be doing.”<br />
Liza Gill, Volunteer Service Manager<br />
believes the response volunteers will make a<br />
significant difference across all our sites. She<br />
said: "Our response volunteers encapsulate<br />
our strapline of ‘giving time to care’ and will<br />
most definitely have a positive impact across<br />
the whole Trust.<br />
“Since the national call out from the NHS<br />
encouraging volunteers to help the most<br />
vulnerable, we have had a massive influx of<br />
potential volunteers wanting to offer their<br />
time to help us.”<br />
You can contact our volunteer service<br />
on 0121 507 4855 or email<br />
swbh.volunteer@nhs.net<br />
12
Rainbow brigades provide a<br />
kaleidoscope of vital assistance<br />
If you were to mention rainbows at<br />
present you might end up having<br />
a conversation about some of the<br />
many wonderful drawings, paintings<br />
and other pieces of art visible in the<br />
windows of homes across the region.<br />
However, rainbows are also connected<br />
to the newly created COVID-19 brigades.<br />
Back on 3 <strong>April</strong>, our organisation asked<br />
volunteers to join our brigades. Three days<br />
later following the release of updated<br />
working from home guidance, colleagues<br />
were asked to consider whether their role<br />
was needed full time during the next ten<br />
weeks of the pandemic. Of those not<br />
needed full time, volunteers were then<br />
sought to take up temporary redeployment<br />
into key support functions.<br />
Our brigades are split into the<br />
following areas:<br />
Red – clinical administration<br />
This includes, along with purple,<br />
colleagues shielding and working from<br />
home.*<br />
This brigade supports ward teams and<br />
emergency care services with clinical<br />
administration duties. This also involves<br />
keeping in touch with patients whose<br />
care has been delayed or deferred by the<br />
focus on COVID-19.<br />
Yellow – PPE wardens<br />
This brigade has two key roles. Firstly,<br />
making sure that everyone has the right<br />
PPE and wears it as required. Secondly, this<br />
brigade will be supporting areas as runners<br />
to ensure that teams stay in PPE in their<br />
affected departments.<br />
Green – Cleaning<br />
This focuses on cleaning communal areas,<br />
door handles and other risk touchpoints.<br />
Most of the work will not be in clinical<br />
areas.<br />
Blue – Portering and transport<br />
Colleagues work within portering<br />
supporting the existing experienced teams.<br />
Some individuals might also be involved in<br />
driving duties.<br />
Purple – Specialist projects<br />
This involves an evolving series of pieces<br />
of work including projects on wellbeing,<br />
isolation and the recovery programme.<br />
Keep an eye out for more information within<br />
the regular daily bulletins and on Connect. If,<br />
with the ongoing changing of circumstances,<br />
your time now allows to volunteer you<br />
can get in touch with the brigade team via<br />
volunteerbrigade.swbh@nhs.net.<br />
COVID-19<br />
We’ll also be featuring some of the<br />
great work you are all doing across<br />
our workplace in upcoming editions of<br />
<strong>Heartbeat</strong>. If you’d like to feature, please<br />
email swbh.comms@nhs.net.<br />
Sonia Arnett and Brinderjit Rai from the<br />
Improvement Team have joined the Green<br />
Brigade<br />
* Remember if you are either<br />
shielding or working from home you<br />
must be registered on the Trust’s<br />
database. Failure to register will be<br />
regarded as absence without leave<br />
unless you are formally isolating or<br />
otherwise off sick.<br />
Nightingale Hospital opens its doors<br />
A number of colleagues have been<br />
drafted in to help at the new NHS<br />
Nightingale Hospital based at<br />
Birmingham’s National Exhibition Centre<br />
(NEC), which will be used if the local NHS<br />
hospitals need additional capacity to<br />
treat patients as a result of the pandemic.<br />
The unit, which is currently set up to house<br />
500 beds, was officially opened by Prince<br />
William in mid-<strong>April</strong> and is fully equipped to<br />
support patients with COVID-19 who may<br />
no longer need intensive hospital care. The<br />
facility will have the ability to scale up quickly<br />
to 4,000 beds if needed.<br />
NHS Nightingale Hospital Birmingham has<br />
been built to provide extra capacity if needed<br />
to local services dealing with the increased<br />
number of patients during the peak of<br />
coronavirus.<br />
It is led by University Hospitals Birmingham<br />
NHS Foundation Trust (UHB) and has a<br />
workforce of doctors, nurses, therapists and<br />
support staff who will ensure that all patients<br />
receive the highest possible standards of care.<br />
The NHS Nightingale Hospitals – currently also<br />
in London, Manchester, Harrogate and Bristol<br />
- are part of a nationwide effort to respond to<br />
the greatest global health emergency in more<br />
than a century. These measures mean that<br />
capacity still exists in hospitals to deal with<br />
coronavirus, with the Nightingales standing<br />
ready if local services need them.<br />
The main purpose of the Nightingale<br />
Birmingham will be to ease pressure on other<br />
hospitals in the area. By looking after general<br />
medical COVID-19 patients, it will allow<br />
existing hospitals and their expert clinical<br />
teams to focus on those who need intensive<br />
care.<br />
Dr David Rosser, Chief Executive, UHB, said:<br />
“The extraordinary effort in creating the<br />
Nightingale Hospital in Birmingham is a total<br />
team effort. Without this collective purpose,<br />
we would not have been able to make the<br />
staggering preparations to deliver this facility.<br />
“The progress made on this site in just a<br />
few days, to turn it from a vast warehouse<br />
into an operational patient facility is quite<br />
unbelievable. It’s yet another example of the<br />
NHS pulling out all the stops alongside our<br />
military, ambulance, contractor and NEC<br />
partners to make this happen.”<br />
West Midlands Ambulance Service Chief<br />
Executive, Anthony Marsh, said: “West<br />
Midlands Ambulance Service stands ready to<br />
support our colleagues in the acute sector<br />
and transfer patients from hospitals around<br />
the region to the new Nightingale Hospital as<br />
required. Our crews will also be on hand to<br />
take people home or onto other care facilities<br />
once they have recovered sufficiently.”<br />
CEO of the NEC Group, Paul Thandi, said: “It<br />
is our honour as a company and workforce<br />
to step forward to help our country’s fight<br />
against the life-threatening virus COVID-19.<br />
“All teams involved have worked seamlessly<br />
alongside our brilliant NHS and the Ministry of<br />
Defence to deliver this facility, and we stand<br />
ready to continue playing our part in the<br />
NHS’s fight to save the lives of our families,<br />
friends and fellow citizens.”<br />
13
PPE: Staying safe<br />
at work<br />
COVID-19<br />
Personal Protective Equipment,<br />
otherwise known as PPE has become<br />
one of the key talking points during<br />
the COVID-19 pandemic. As we<br />
learn more about how the virus is<br />
transmitted the PPE requirements<br />
have changed. This may have<br />
caused some confusion and anxiety<br />
amongst colleagues. It is important<br />
that colleagues understand the<br />
correct use of PPE to keep ourselves,<br />
patients and colleagues safe.<br />
From FFP3 to N95 masks, gowns to gloves,<br />
the assortment of protective equipment<br />
has steadily morphed as we have learnt<br />
lessons from countries that have battled<br />
COVID-19 before us, and changed the way<br />
we work to protect ourselves, colleagues<br />
and patients.<br />
Throughout this pandemic, from the initial<br />
preparation phase to where we are now,<br />
one thing has stood the test of time - that<br />
being the need to protect colleagues as an<br />
utmost priority. From supporting face mask fit<br />
testing across the organisation, where almost<br />
5,000 colleagues now know exactly which<br />
masks to use to be able to safely care for<br />
patients with COVID-19, to ensuring that as a<br />
Trust we’re able to adapt our practices to be<br />
one step ahead of COVID-19.<br />
To find out more about the work being done<br />
to protect colleagues and patients, <strong>Heartbeat</strong><br />
caught up with Infection Control Lead Nurse,<br />
Julie Booth. She said: “We know we need<br />
to protect colleagues to be able to continue<br />
caring for our patients safely, so it’s important<br />
we have the right support in place. We have<br />
been working hard to ensure that we’re able<br />
to reinforce not only our practices but our<br />
provisions to protect staff.<br />
“Colleagues will no doubt have seen all of the<br />
posters that have been put up highlighting<br />
the red and blue areas as well as top to toe<br />
guidance on PPE. We now also have stations<br />
on the entrances to every ward area with<br />
clear guidance and supplies of PPE and we’re<br />
working with colleagues in supplies to ensure<br />
that we’re able to keep colleagues protected<br />
should there be any further changes to the<br />
guidance.”<br />
Colleagues must remember to wash their<br />
hands, this is the most important thing<br />
that everyone must do regularly alongside<br />
ensuring that they are wearing the correct<br />
PPE appropriate to the right environment and<br />
patient contact. Remember that not everyone<br />
in a given ward or department will wear<br />
the same; there are differences due to the<br />
procedures that each person carries out that<br />
dictate the level of PPE.<br />
For further information on PPE, contact<br />
the infection control team or keep up to<br />
date via the daily bulletin and Connect.<br />
R&D: Leading the way to innovations<br />
in COVID-19<br />
The strong research and development<br />
culture at our Trust has once again come<br />
to the forefront as out R&D team has<br />
stepped forward and stepped up our<br />
involvement in a range of research trials<br />
looking in to COVID-19.<br />
With innovation and ideas flowing from<br />
clinicians across the world, all with the aim<br />
of tackling COVID-19 and stopping it in its<br />
tracks, research trials have stepped up pace<br />
and nowhere more evident is that than our<br />
own Trust where to date, we have already<br />
managed to recruit over 63 patients in to a<br />
range of studies.<br />
To find out more about the work of R&D in<br />
COVID-19, <strong>Heartbeat</strong> caught up with Gina<br />
Dutton, Head of Research and Development,<br />
she said, “Our Trust is proud of its long track<br />
record of excellence in clinical research and<br />
we’re keen to use all of our knowledge and<br />
ability to develop more effective ways of<br />
looking after our patients. COVID-19 has<br />
undoubtedly had a significant impact on<br />
both patients and healthcare professionals<br />
and it’s an ideal opportunity to support<br />
research in to innovations in treatment and<br />
care of COVID-19 patients.<br />
“The portfolio of COVID-19 studies is<br />
increasing rapidly and I am proud to say<br />
A patient being examined with the new<br />
Bioptigen handheld device<br />
that we have already opened or have in<br />
set up six of the most important COVID-19<br />
clinical trials and observational studies,<br />
completing local governance checks and set<br />
up processes in record time. Key to this has<br />
been our close working relationship with the<br />
trials pharmacy team. This has been a whole<br />
Trust effort with all colleagues in various<br />
medical specialties pulling together to ensure<br />
that patients are offered these studies during<br />
their hospital stay.”<br />
Shortly after it was announced that the<br />
prestigious RECOVERY trial had nationally<br />
recruited its 5000th participant, the Trust<br />
recruited its 50th. This study is looking<br />
at a range of drug treatment options for<br />
patients who are admitted to hospital with<br />
COVID-19. It is a rapidly changing study<br />
The infection control team are supporting<br />
colleagues to stay safe<br />
so that it can assess a range of treatments<br />
quickly. The current medications in the study<br />
include Lopinavir-Ritonavir, a commonly used<br />
HIV drug, Low-dose Dexamethasone - a<br />
type of steroid, which is used in a range of<br />
conditions typically to reduce inflammation,<br />
Hydroxychloroquine (anti-malarial drug),<br />
Azithromycin (antibiotic) and Tocilizumab (an<br />
anti-inflammatory treatment).<br />
Two other treatment trials are for patients<br />
who are more poorly; REMAP-CAP is a drug<br />
trial using similar treatments to RECOVERY<br />
and RECOVERY RS: Respiratory Support<br />
is looking at different types of breathing<br />
support, continuous positive airway pressure<br />
(CPAP) and High flow nasal oxygen (HFNO).<br />
A fourth treatment trial, PRINCIPLE, is in set<br />
up with our GP colleagues in Your Health<br />
Partnership.<br />
Two other studies are collecting data and<br />
samples to improve the understanding of<br />
genetics of COVID-19 and how it impacts on<br />
patients.<br />
As this is such a rapidly changing portfolio,<br />
R&D has created a special Connect page so<br />
that Trust staff can be kept informed of our<br />
current COVID research. https://connect2.<br />
swbh.nhs.uk/research-and-development/<br />
covid-19-clinical-research/<br />
14
Caring for relatives during COVID-19<br />
By Paula Gardner, Chief Nurse<br />
Paula Gardner, Chief Nurse<br />
COVID-19 has changed the world as<br />
we know it in many ways, but one of<br />
the most significant ways that I see<br />
the impact, as a nurse, is the sheer<br />
challenge of relatives not being able<br />
to spend time with their loved ones<br />
who are in hospital. This goes against<br />
everything we nurses are used to and<br />
are comfortable with and has often<br />
left us stepping in more to provide that<br />
social contact and empathy that their<br />
relatives would normally bring.<br />
Our patients remain at the forefront and at<br />
times, when we don’t see them, it can be<br />
easy to forget about the importance of regular<br />
communication with relatives. This is why we<br />
introduced our purple point telephone service<br />
two years ago – to allow visitors and patients<br />
to get on the spot help when they need it.<br />
It is certainly even more difficult to speak to<br />
relatives during the pandemic as they are not<br />
popping in as they used to. But it is precisely<br />
at this time that we need to consider more<br />
than ever how we talk to relatives about the<br />
care that the patient is receiving. We must<br />
all put ourselves in the shoes of those people<br />
whose anxiety must be heightened by the<br />
inability to visit and see how their friend or<br />
family member is getting on. I know, from<br />
speaking to relatives after their loved one has<br />
sadly passed away, just how traumatic the<br />
experience has been for them and how sad<br />
they are for not being able to spend as much<br />
time together as they wanted.<br />
Our wards have tablets and phones to help<br />
people stay in touch. Yes, it might feel like it<br />
takes time to help people use these, but this<br />
time is essential in enabling patients to see<br />
their family and the absent family member to<br />
feel some closeness with their relative. This is<br />
COVID-19<br />
just as important as the hands on care<br />
we provide to every patient.<br />
Colleagues supporting patients in the<br />
community have the same struggles<br />
– whereas home visits still take place,<br />
some are replaced with a telephone call<br />
to check in and often the relative can<br />
feel excluded from this.<br />
There are some great examples across<br />
the Trust of good, planned conversations<br />
with relatives. The critical care team have<br />
put together some excellent information<br />
for relatives that clearly sets out how<br />
they will communicate with them and<br />
gives them information on how to<br />
make contact virtually with patients.<br />
One of the key lessons we must learn<br />
throughout this pandemic is that careful,<br />
consistent communication with relatives<br />
is just as important as the care we give<br />
to our patients.<br />
Understanding more about COVID-19<br />
By Professor David Carruthers, Medical Director<br />
Professor David Carruthers, Medical Director<br />
Since we first heard about this new virus<br />
the world has been trying to understand<br />
more about it….Who is most affected?<br />
How is it transmitted? Can you be<br />
immune to it? Why do some people<br />
have a mild illness and other cases<br />
end in a tragic outcome? What clinical<br />
interventions do patients respond to?<br />
At our Trust, we are no exception to this<br />
hunger for information to understand<br />
COVID-19 so that we might best protect and<br />
treat patients who catch the virus.<br />
We began seeing patients in our acute<br />
hospitals with potential coronavirus<br />
symptoms in February, but on testing, the<br />
initial query cases were negative. Our first<br />
confirmed case was at City Hospital on 12<br />
March. We now have information on every<br />
patient who has been treated by us with a<br />
positive test result, every patient who has sadly<br />
died with COVID-19 and all those who we<br />
have seen and tested, whose test result came<br />
back clear.<br />
We are undertaking our own data analysis on<br />
acute admissions to the Trust, contributing to<br />
national research projects (clinical, therapeutic<br />
and genetic) as well as detailed reviews of<br />
mortality data.<br />
This information feeds into wider regional and<br />
national data analysis but even within our own<br />
Trust we can start to see patterns emerging<br />
– although it is important not to jump to<br />
conclusions. It is very evident that underlying<br />
health conditions contribute to the risk of more<br />
severe disease.<br />
Age is a definite risk factor with 47 per cent<br />
of all COVID+ patients who have died in our<br />
hospitals being over 85 years old. Men seem<br />
to be affected more than women. Of the<br />
patients we have seen with COVID-19, 58 per<br />
cent have hypertension and 39 per cent have<br />
diabetes. This is higher for the patients who<br />
have died. We have also seen a difference over<br />
time since the start of the positive cases at our<br />
Trust. More of the patients who died were at<br />
City Hospital in March but this has changed<br />
in <strong>April</strong>, indicating the dynamic changing<br />
nature of the epidemic. When we have looked<br />
at ethnicity, there doesn’t appear to be a<br />
disproportionate impact on patients from<br />
different ethnic backgrounds at Sandwell<br />
Hospital, whereas in March, 39 per cent<br />
of the deaths of patients with COVID-19<br />
at City Hospital were in black patients,<br />
but only 19 per cent in <strong>April</strong> which is line<br />
with the wider Birmingham population.<br />
This could indicate a geographical cluster<br />
in March in western Birmingham at the<br />
start of the outbreak.<br />
We continue to collect and analyse this<br />
information as well as review deaths<br />
in our care whether covid-related or<br />
not. I am really pleased that our Trust is<br />
participating in several research studies<br />
on this virus as you can see elsewhere in<br />
<strong>Heartbeat</strong>.<br />
The clinical care of patients in hospitals<br />
is also being reviewed carefully. The early<br />
provision of oxygen therapy, proning<br />
of patients (patients are placed on their<br />
front and the bed is tilted to relieve<br />
pressure on the lungs) and increased<br />
use of NIV/CPAP seems to be having a<br />
positive impact on some patients. We<br />
continue to share learning with other<br />
NHS organisations and see what has<br />
worked well in other parts of the world,<br />
modifying our approach to patient care as<br />
we learn more. Many thanks to all of you<br />
involved in patient care that makes rapid<br />
changes in our approach to management<br />
of COVID-19 possible.<br />
15
It may be work b<br />
With COVID-19 changing so many of the<br />
things we all took for granted we’ve all had<br />
to adapt the way we do things, not least the<br />
way we work. Luckily at our Trust, we have<br />
the flexibility to allow some colleagues to<br />
work remotely at home.<br />
Cyndi E Corlis<br />
Organisational Development & Learning<br />
Q How have you adjusted to<br />
working from home?<br />
A Much better than I expected, very<br />
well actually.<br />
Q Can you tell us some of the<br />
benefits of working from home?<br />
A I get to finish a cup of coffee<br />
(or two). I have more time to focus<br />
on tasks and time to think without<br />
rushing.<br />
Q What do you miss about<br />
going into work?<br />
A I miss the interactions I have with<br />
others, the journey, or just the<br />
change of scenery.<br />
Q What’s your top tip for<br />
working from home?<br />
A Routine – Implement the same<br />
start and finish times as if you are<br />
still working on site. Have a<br />
designated office area if you can<br />
and get dressed!<br />
Gemma Botfield<br />
Specialist Community Public Health Nurse<br />
Q How are you finding working<br />
from home?<br />
A I am on week five of working from<br />
home and feel like I’ve adapted to<br />
it well. My manager and colleagues<br />
are all very supportive; we’ve even set<br />
up a WhatsApp group. This helps us<br />
all check in with each other<br />
throughout the day.<br />
Q What has been the biggest<br />
change for you?<br />
A I miss the contact with children<br />
and young people, however, we have<br />
still been able to complete video calls<br />
whilst at home. I also miss going into<br />
schools and having contact with other<br />
professionals. The same goes for my<br />
work colleagues. We have our daily<br />
catch ups which we use to complete<br />
weekly cluster meetings.<br />
Q Can you share some of the<br />
benefits of working from home?<br />
A I’ve not been stuck in traffic every<br />
day. I also feel that communication<br />
with other agencies has been easier<br />
and faster.<br />
Q What’s your top tip for working<br />
from home?<br />
A Ensure you set up a workspace with<br />
all the correct equipment, a private<br />
area is essential for taking and making<br />
calls. Taking regular screen breaks is a<br />
must too.
ut not as we know it!<br />
Kajal Sondhi<br />
Volunteer Service<br />
Q How have you adjusted to<br />
working from home?<br />
A It has been a big change, it took a<br />
few weeks to adjust but it has not<br />
been impossible.<br />
Q What has been the biggest<br />
change?<br />
A The biggest change for me has<br />
been not seeing as many people as<br />
I usually would.<br />
Q What do you miss about coming<br />
into work?<br />
A I miss the little things, such as<br />
talking face to face with colleagues,<br />
meeting new people and doing<br />
different things every day.<br />
Q What’s your top tip for working<br />
from home?<br />
A It is important to keep a routine. It<br />
took me a while to get into one, but<br />
I am glad that I set one for myself. It’s<br />
important to find a good working<br />
space, and it helps to get into an<br />
exercise routine too.<br />
Here are our top tips to help you establish<br />
an efficient home working regime:<br />
Get dressed<br />
This may sound like an obvious<br />
tip but it makes a big difference<br />
to how you face your day.<br />
Making the effort to get ready<br />
will help you to focus on the<br />
day ahead.<br />
Work your usual hours<br />
Keeping to a routine will help you to maintain a sense<br />
of normality in these unusual times. Don’t be tempted<br />
to have late nights – getting enough sleep will help<br />
you to feel rested and ready to take on whatever your<br />
working day has in store for you. If you’ve saved a<br />
considerable amount of time on your commute to<br />
and from work you could use this time to invest in<br />
something you enjoy like reading or taking part in an<br />
online exercise class.<br />
Talk to your colleagues<br />
We all have lots of ways to communicate - WhatsApp,<br />
Skype, Webex, the list is endless. The truth is whilst<br />
these tools are fantastic for helping us stay in touch;<br />
it’s nice to hear from someone. Make time to check in<br />
with your colleagues at home, a quick five-minute chat<br />
may not only cheer up someone’s day but help to boost<br />
productivity and save you sending countless emails. It’s<br />
good to talk!<br />
Take a break<br />
You may find getting your main<br />
tasks done in the morning a little<br />
easier, or perhaps you think better<br />
in the afternoon. Whatever works<br />
for you remember to take a break<br />
– enjoy a cuppa or you could set<br />
up a work playlist to help you<br />
power through. If you are lucky enough to have some<br />
outside space you could have lunch in the garden.
CORPORATE AND GENERAL<br />
NEWS<br />
Shout out has been a regular feature<br />
in <strong>Heartbeat</strong> and it is fantastic to see<br />
colleagues regularly taking the time<br />
to give positive feedback to each<br />
other.<br />
We regularly receive positive feedback<br />
from our patients too, and this month<br />
we wanted to share some of those<br />
heart-warming messages which have<br />
been sent via our website and social<br />
media platforms.<br />
To – Jooby Thomas on the Respiratory Hub<br />
For being really supportive in making plans<br />
for increasing our nurse staffing numbers<br />
in line with additional capacity.<br />
From – Beth Hughes<br />
To – Lesley Dowie<br />
For taking amazing care of all the labour<br />
ward staff and rustling up a cooked<br />
dinner for the night shift team! Very much<br />
appreciated!<br />
From – Howard Stringer<br />
To – All staff on the 6 PCCT Community<br />
Wards<br />
Thank you for continually seeking<br />
opportunities to go the extra mile, from<br />
putting on afternoon tea parties to<br />
supporting each other which often involves<br />
travelling from City to Rowley or vice versa<br />
- we appreciate it.<br />
From – Justine Irish<br />
To – Nursing staff on Priory 2<br />
A big thank you to the wonderful nursing<br />
staff on Priory 2 for cleaning the ward<br />
in between looking after the patients so<br />
it takes some of the pressure off Ward<br />
Services. It is highly commendable that we<br />
are all pulling together during this trying<br />
time. Well done!<br />
From – Shila Patel<br />
To – Domestics/ward services<br />
A huge shout out to our fabulous SWBH<br />
domestics /ward services officers at City and<br />
Sandwell. Our amazing domestic services<br />
teams are on the front line against virus<br />
spread right now and they are doing an<br />
amazing job. Amidst all the uncertainty<br />
that inevitably results during an outbreak<br />
of a virus, they keep calm and carry on.<br />
Huge respect and thanks.<br />
From – Mark Lee<br />
To – Kevin Johnson - Portering team<br />
Went above and beyond to help AMAA<br />
staff move to medical infusions suite.<br />
Not only stayed past his shift time but<br />
supported the moving process, was very<br />
helpful and was a great support.<br />
From – Natalie Binfield<br />
To – Amy Dawes<br />
She looked after my nan/mum on Surgical<br />
Day Case Unit when she thought she<br />
was going to have her op. Amy kept us<br />
informed of the situation; she was lovely,<br />
kind and helpful.<br />
From – Rachel Humphreys<br />
To – Stacey Caffrey<br />
A big thank you to our fabulous new<br />
starter link nurse for being amazingly<br />
supportive and available for all the<br />
newbies on AMU.<br />
From – Fiona Boddy<br />
To – Sherry Craig<br />
Just to say thank you Sherry and all the<br />
Lyndon 3 crazy team. You're a fantastic lot<br />
to work with because of your team work<br />
ethic and support for each other. You make<br />
me look forward to being at work with my<br />
second family. Thank you all.<br />
From – Barbara Boparai<br />
To – Medical Infusion<br />
For packing up their ward and moving to<br />
Rowley Regis in 4 hours.<br />
From – Mercia Buddle<br />
To – Vanessa Neimke<br />
Thank you Vanessa for all your support<br />
with revising the New-born Blood Spot<br />
screening process which has been disrupted<br />
considerably by COVID-19. Your can-do<br />
attitude and proactive approach have<br />
helped a huge amount.<br />
From – Becky Fox<br />
To – Julie McFarlane<br />
Thank you for your wonderful work that<br />
you do in the antenatal clinic at Sandwell.<br />
Especially this week where you have been<br />
on your own doing all the bloods and<br />
covering the front desk in what have been<br />
very difficult circumstances. You are very<br />
much appreciated.<br />
From – Louise Bates<br />
To – Ashley Pedersen-Gosling<br />
Thank you Ashley for being so proactive<br />
and offering support to other areas of<br />
Maternity. Much appreciated, especially in<br />
the face of current challenges.<br />
From – Becky Fox<br />
To – Pharmacy Stores and Distribution<br />
Team<br />
Helen Whiles, Sue Jones, Hugh Brown<br />
and the pharmacy stores team. Thank you<br />
for your hard work in responding to the<br />
stock changes required to support ward<br />
reconfigurations.<br />
From – Emma Archer<br />
To – Emma Shaw<br />
Emma has dealt with major changes to the<br />
ward amazingly well over the weekend.<br />
All of the Lyndon 2 team are very proud<br />
of you.<br />
From – Sarah Phillips<br />
18
Year of the Nurse and Midwife<br />
Each month we profile some of our wonderful nurses as part of our<br />
<strong>2020</strong> year of the nurse and midwife celebrations.<br />
Read on to find out about the career pathway of Matron for Primary Care<br />
Community and Therapies, Natalie Whitton.<br />
As you may be aware, this year<br />
marks International Year of the<br />
Nurse and Midwife, a campaign by<br />
the World Health Organisation in<br />
honour of the 200th birthday of<br />
Florence Nightingale.<br />
Nurses and midwives play a vital role in<br />
providing health services in our workplace.<br />
They devote their lives to caring for<br />
mothers and children; giving lifesaving<br />
immunisations and health advice; looking<br />
after older people and generally meeting<br />
everyday essential health needs. They<br />
are often the first and only point of care<br />
in their communities. Throughout the<br />
year we will be highlighting some of our<br />
nurses, HCAs and midwives who are<br />
making a difference to our patients.<br />
For <strong>April</strong>, we feature Matron for Primary<br />
Care Community and Therapies, Natalie<br />
Whitton.<br />
Natalie was inspired to be a nurse by her<br />
aunt. She told us: “I started my career as<br />
a student nurse back in 2004 at the Trust.<br />
At that time I had two young children and<br />
was juggling this alongside my studying<br />
which wasn’t easy, but I was determined<br />
to achieve my goal.”<br />
Just 16 months after qualifying, Natalie<br />
was promoted to a ward sister. Natalie<br />
briefly spent time away from the Trust,<br />
before being persuaded by her peers to<br />
Natalie Whitton<br />
Matron for Primary Care, Community and Therapies.<br />
Then and now. Natalie at the start of her career and pictured more recently as Matron for<br />
Primary Care, Community and Therapies<br />
apply for a senior sister post in primary<br />
care, communities and therapies.<br />
“I wasn’t sure about returning to the Trust<br />
at first as I thought many things would<br />
have changed and I may find it difficult to<br />
adapt. However, after a few conversations<br />
with some of my old colleagues, I knew it<br />
was an opportunity I didn’t want to miss<br />
out on so I applied.” She was successful<br />
in getting the role and returned to us in<br />
January 2017.<br />
After an impressive 18 months, she was<br />
successful in obtaining a matron post.<br />
Natalie went on to win New Leader of the<br />
Year at the 2018 Star Awards. She believes<br />
this is one of her greatest achievements at<br />
the Trust and is grateful to all those who<br />
recognised her hard work as a leader.<br />
She said: “To be recognised by staff as<br />
being a person who has demonstrated<br />
outstanding ability, talent and leadership<br />
whilst showing great promise for the<br />
future is a wonderful feeling. I was truly<br />
thankful to all those who nominated me<br />
for this award.”<br />
Natalie continues to show what a fantastic<br />
nurse she is. Most recently she played a<br />
pivotal role in organising a tea party on<br />
D47 which brought together colleagues,<br />
patients and their families and, more<br />
importantly, encouraged patients to get<br />
out of their beds more often and use the<br />
communal areas in the ward.<br />
19
Ramadan during COVID-19<br />
CORPORATE AND GENERAL<br />
NEWS<br />
This year Ramadan began on 23 <strong>April</strong><br />
and for many, it will be a different<br />
experience as places of religious<br />
worship of all denominations are<br />
closed across the UK. Ramadan is<br />
a time of spiritual reflection, selfimprovement,<br />
and heightened<br />
devotion and worship. Muslims are<br />
expected to put more effort into<br />
following the teachings of Islam<br />
and perhaps with the events of<br />
<strong>2020</strong> so far it will play an even more<br />
important part in the lives of many<br />
people.<br />
Typically, Ramadan lasts for 29-30 days<br />
and ends with the celebration of Eid-<br />
Ul-Fitr. Many Muslims will fast each day<br />
from sunrise to sunset. This includes not<br />
eating food, drinking liquids or smoking.<br />
It is common to have one meal known<br />
as the suhoor just before sunrise and<br />
an evening meal known as Iftar after<br />
sunset.<br />
It’s also a time for charitable activity,<br />
some people may make donations, and<br />
others may participate in events. This<br />
year there is lots of activity going on in<br />
and around our Trust which colleagues<br />
may wish to participate in.<br />
Ramadan is a time of spiritual reflection<br />
Respecting the important role of Ramadan is<br />
something we support at our Trust. This year<br />
we will be doing things a little differently.<br />
Some of the key changes include:<br />
• Prayer facilities will be available in ‘hot<br />
areas’ to enable colleagues to pray<br />
without leaving the area<br />
• Prayer mats will be available in local<br />
prayer areas with disposable covers<br />
• Colleagues will be offered night shifts<br />
• Food will be made available to break<br />
fast at the correct time.<br />
Fasting is a central part of Ramadan. It is,<br />
however, important to highlight that some<br />
people and indeed patients we may see might<br />
be exempt from fasting. These people include:<br />
• All those who are unable to fast due to<br />
illness (physical or mental) or being frail<br />
• Pregnant and menstruating women<br />
• Lactating women who have<br />
concerns about their own, or their<br />
child’s health.<br />
It’s also worth noting that some medical<br />
procedures do not break fasting. These may<br />
include things such as:<br />
• Injections (Intravenous, intramuscular,<br />
intracardiac, intraosseous, intradermal<br />
and subcutaneous)<br />
• Taking bloods (thumb prick or<br />
intravenous)<br />
• Eye or ear drops (unless the tympanic<br />
membrane is perforated)<br />
• Urethral infusion, transdermal patch<br />
(i.e. nicotine patches), concentrate<br />
oxygen, epidural analgesia and<br />
haemodialysis.<br />
Dr Parijat De, Consultant in Diabetes and<br />
Endocrinology commented: “Exemptions<br />
exist for people with serious medical<br />
conditions, including many with diabetes,<br />
but a large number will participate, often<br />
against medical advice. With the correct<br />
advice and support from health care<br />
practitioners and local guidelines, many<br />
people with type 2 diabetes and other<br />
medical conditions may be able to fast<br />
safely during Ramadan.”<br />
Our latest Ramadan guidance is on<br />
Connect.<br />
Keeping SWB safe and secure<br />
On 23 March <strong>2020</strong>, Prime Minister,<br />
Boris Johnson announced that the<br />
UK was going into lockdown. With<br />
COVID-19 accelerating rapidly across<br />
the UK this move was made to<br />
protect the NHS and to help save<br />
lives.<br />
As a Trust, this meant we had to act<br />
decisively to place all of our sites into<br />
full lockdown to ensure patient and<br />
colleague security was not compromised.<br />
We caught up with Anil Bhogal, Security<br />
Manager who told us more.<br />
“We worked with our security teams to<br />
lockdown all three of our hospitals. Our<br />
security personnel made it their priority<br />
priority to ensure there was a security<br />
presence onsite across those sites. We<br />
also inducted ten agency security staff<br />
to assist with strengthening our security<br />
presence.<br />
Our hospital lockdown has meant our<br />
security team had to change the way<br />
Members of the security team who work to keep our sites secure<br />
they do things and fast. Anil told us: “It<br />
was a huge challenge to have everything<br />
completed within a limited timeframe. We<br />
had to complete a building risk assessment<br />
of each site and ensure that all the doors<br />
were repaired in time to support the physical<br />
security of a lockdown. This also meant we<br />
had to prepare our staffing rota three months<br />
in advance, plus ensure we had substantive<br />
and bank staff in place to support our plans at<br />
this busy time.<br />
He added: “We have restricted access<br />
to all visitors coming on to our sites and<br />
challenge everyone about why they<br />
need to enter one of our sites, including<br />
colleagues. This has helped to reduce the<br />
risk of COVID-19 spreading by decreasing<br />
the number of people entering our sites.<br />
Everyone has been very understanding - it<br />
has been a huge team effort and we’re<br />
thankful to everyone who has helped us<br />
achieve a safe and effective lockdown.”<br />
20
Celebrating our<br />
stars of the week<br />
Star of the Week<br />
Edward Fogden<br />
Gastroenterology Consultant<br />
example was brought up for good practice<br />
and will be used as an example of this.”<br />
Well done Edward!<br />
Star of the Week<br />
Anil Bhogal<br />
Security Manager<br />
Star of the Week<br />
Kulbinder Sidhu<br />
HCA<br />
Congratulations are in order for a<br />
consultant who has been praised far<br />
and wide for the amazing care and<br />
support he has been providing patients<br />
in the BTC.<br />
Edward Fogden, Gastroenterology<br />
Consultant was nominated for the Star of<br />
the Week award by Dr Eoin Dore, ACCS<br />
CT2 anaesthetics.<br />
Nominating Edward for the award, Eoin<br />
said: “He is an example of excellence<br />
in dealing with trainees and his use/<br />
encouragement of the exception reporting<br />
system when trainees/junior doctors have<br />
to stay late to cover clinical issues. Despite<br />
his very busy schedule, his ward rounds are<br />
known for being excellent for teaching. His<br />
Star of the Week<br />
Neil Davies<br />
Community Transport Driver<br />
Congratulations are in order for a<br />
community transport driver who has<br />
been described as ‘incredibly helpful’<br />
by colleagues.<br />
Neil Davies is a community transport driver<br />
who has been working at our Trust for<br />
over 15 years in a range of roles and most<br />
recently has been turning his hand to<br />
transport.<br />
Congratulations are in order for Anil<br />
Bhogal, Security Manager who is our<br />
most recent Star of the week award.<br />
Anil has worked hard to transform the<br />
security team growing the team significantly<br />
in a very short period of time to be able<br />
to respond appropriately to the difficult<br />
situations that COVID-19 has presented.<br />
Working alongside his front-line colleagues<br />
Anil has taken the lead in shaping the face<br />
of security to be friendly and supportive as<br />
well as firm and assertive to protect both<br />
colleagues and patients.<br />
Nominating Neil for the award, Interim<br />
Clinical Directorate Lead for iBeds wrote,<br />
“Neil is consistently an asset to our PCCT<br />
team, frequently assisting with a number<br />
of last minute requests for transport of<br />
patients, equipment and other essential<br />
supporting roles.<br />
On Wednesday he worked exceptionally<br />
hard to facilitate the transfer of patients at<br />
extremely short notice from Leasowes to<br />
different locations in our area, taking some<br />
to new ward locations at Rowley and at<br />
City sites, as well as taking some patients<br />
to their own homes.<br />
He worked tirelessly with the team,<br />
transporting nine patients from the unit,<br />
releasing vital capacity for our Patient<br />
Transport Service. He worked with positivity<br />
and enthusiasm throughout and without<br />
him we wouldn’t have successfully<br />
completed the move within the day. He<br />
reassured anxious patients and helped to<br />
keep the whole team positive.”<br />
Thank you Neil, your hard work is highly<br />
valued by us all!<br />
Congratulations are in order for a HCA<br />
who has been praised far and wide<br />
for the amazing care and support<br />
she has been providing patients and<br />
colleagues.<br />
Kulbinder Sidhu, Healthcare Assistant on<br />
the Respiratory Hub at City Hospital was<br />
nominated for the Star of the Week award<br />
by not just one colleague but by five in<br />
total, all of whom felt that her personable<br />
attitude, hard work and determination to<br />
do the best for her patients and colleagues<br />
made her a worthy nominee for the weekly<br />
award.<br />
Nominating Kulbinder for the award, Sister<br />
Alice Sibanda wrote, “Kully has been a<br />
God send since the move from Sandwell to<br />
the new respiratory hub! She has kept the<br />
ward tidy, managed stock, worked really<br />
hard and managed all the new HCAs we<br />
have had, helping to orientate them to the<br />
ward. She has worked tirelessly including<br />
coming in on bank to make sure the ward<br />
is running smoothly. We can’t thank her<br />
enough for her hard work and dedication<br />
to the ward.”<br />
Sharing her experience of working with<br />
Kulbinder, Staff Nurse Alice Winter wrote,<br />
“I have recently started on the Respiratory<br />
Hub at City Hospital and Kulbinder has<br />
been invaluable. She has been there<br />
to show me where everything is, made<br />
me feel welcome and supported me in<br />
delivering patient care. She has made<br />
my first few weeks as a newly qualified<br />
much easier and she should know how<br />
appreciated she is!”<br />
Well done Kulbinder!<br />
If you have someone in your team<br />
that has gone above and beyond<br />
the call of duty, put them forward<br />
as a Star of the Week by logging a<br />
nomination on Connect.<br />
21
Multi-storey car parks granted<br />
approval<br />
CORPORATE AND GENERAL<br />
NEWS<br />
Our organisation has been given<br />
the green light to build multi-storey<br />
car parks at City and Sandwell<br />
Hospitals which will improve access<br />
for colleagues, patients and visitors.<br />
Permission was granted by Sandwell<br />
Council for a 400-space facility, whilst<br />
Birmingham City Council gave the goahead<br />
for a 550-space car park at our<br />
City site.<br />
The move will improve parking by creating<br />
the new facilities. Sandwell Hospital is<br />
undergoing some significant changes over<br />
the coming years with work underway for<br />
a £6 million health development which<br />
will house Carters Green Medical Centre<br />
and Lyndon Health Centre. The existing<br />
provision of car parking space will be<br />
constructed to meet the parking demands of<br />
the site.<br />
City Hospital is due to be redeveloped over<br />
the coming years to incorporate new housing<br />
and commercial space. It will also continue<br />
to provide health services at the Birmingham<br />
Treatment Centre, the Birmingham and Midland<br />
Eye Centre and the Sheldon Block.<br />
The Trust is working with car park operator,<br />
Q-Park using its estates development partner<br />
Prime to develop the plans for the new car<br />
parks. Residents, councillors and hospital<br />
staff were invited to hear about the proposals<br />
during engagement events held in October<br />
2019. The views, ideas and concerns fed into<br />
the planning application.<br />
James Pollitt, Associate Director of Strategic<br />
Development from the Trust, said: “We're<br />
delighted to have received planning<br />
permission, which will address a longstanding<br />
concern for our dedicated workforce. Our<br />
schemes will include electric charge vehicle<br />
provision and will help us to tackle parking on<br />
neighbouring streets. The Trust continues to<br />
invest in supporting other modes of travel as<br />
part of our net zero commitment.”<br />
Ewan Forsyth, Prime’s Development Director,<br />
said: “These consents allow us to take the<br />
first steps towards delivering much-needed<br />
infrastructure for the Trust to help achieve its<br />
strategic vision and deliver affordable, highquality<br />
facilities that improve the patient,<br />
visitor and staff experience.”<br />
Sandwell site map showing where our new multistorey car park will be built<br />
<strong>2020</strong> - International Year of the Nurse and Midwife<br />
May <strong>2020</strong> - National Walking Month<br />
4 May Deaf Awareness Week<br />
4 May Maternal Mental Health<br />
Awareness Week<br />
5 May International Day of the<br />
Midwife<br />
7 May Public Trust Board 9am -1pm<br />
(Webex)<br />
8 May Bank Holiday<br />
11 May Dementia Action Awareness<br />
Week<br />
12 May International Nurses Day<br />
18 May Mental Health Awareness Week<br />
25 May Bank Holiday<br />
26 May Clinical Leadership Executive<br />
2pm-5pm (Webex)<br />
27 May - TeamTalk 1pm (Webex)<br />
22
Medicine administration –<br />
supporting safe and effective care<br />
CORPORATE AND GENERAL<br />
NEWS<br />
Colleagues must scan barcodes on medicines and wristbands<br />
Medicine administration – the art of<br />
giving the right dosage of the right<br />
medication to the right patient at<br />
the right time. While this sounds like<br />
its fraught with danger, it’s actually<br />
quite a safe process - if you follow the<br />
approved workflow.<br />
One of the key features of Unity is<br />
clinical safety, and in no other role is<br />
this most evident than it is in medicine<br />
administration. With the operational<br />
pressures of busy wards, the constant<br />
demands on nursing staff, a safe process to<br />
administer medication was one of the first<br />
elements established in Unity.<br />
A simple scan of a barcode on a patient’s<br />
wristband is all that is needed to pull up a<br />
list of medication to administer, followed<br />
by scanning the barcode on the medication<br />
before it is administered. This means there<br />
are two automated system checks to make<br />
sure that mistakes don't happen.<br />
To find out more about the duty of care<br />
when dispensing drugs, <strong>Heartbeat</strong> caught<br />
up with Chief Pharmacist, Puneet Sharma.<br />
He said, “Barcode scanning of patients’<br />
wristbands and medication is mandatory<br />
for all staff when administering medication.<br />
Bypassing the scan to save time puts lives at<br />
risk and could prove fatal.<br />
“Occasionally it is necessary to bypass a<br />
scan, whether it’s a faulty scanner or an<br />
unreadable wristband, however these<br />
should be few and far between. And<br />
in these few cases, the bypass must be<br />
documented.”<br />
Following feedback from our nursing<br />
colleagues, changes have been made to<br />
the medication administration wizard<br />
in Unity about how not being able to<br />
barcode scan a patient’s wristband, or<br />
not barcode scanning the medication<br />
is now recorded. With the new dropdown<br />
recording, we can track which<br />
particular medication has not scanned<br />
(and if there is a barcode issue resolve<br />
this quickly), or if the medication has<br />
not scanned for a valid reason. This is<br />
then recorded against individual Unity<br />
logins, so ward managers can see if<br />
there are particular members of the<br />
team that need further support through<br />
reports.<br />
Should you have any queries or<br />
difficulties using barcode scanning,<br />
please speak to the Unity Super User in<br />
the first instance. If further information<br />
is needed, please email the EPMA team<br />
via swbh.PharmEPMABuild@nhs.net<br />
BMEC still keen to see you right<br />
SURGICAL SERVICES<br />
It is an unfortunate necessity of the<br />
COVID-19 pandemic that with such<br />
dramatic changes to how we treat<br />
patients in our care, services and how<br />
we, as an organisation, operate them<br />
have in some instances changed.<br />
Be that in the way we offer them, the<br />
location of treatment, the availability of<br />
the service (in terms of opening hours), a<br />
reduction in capacity and in a handful of<br />
cases they’ve been temporarily closed due to<br />
the redistribution of personnel throughout<br />
the hospital.<br />
One vital department that is still going<br />
strong is the Birmingham Midland Eye<br />
BMEC<br />
Centre (BMEC). They’re very keen to get the<br />
message out about their continued availability,<br />
especially with people’s eyesight at stake. BMEC’s<br />
emergency care department is still open and<br />
seeing any patients that have an urgent need for<br />
treatment.<br />
Hilary Lemboye, Group Director of<br />
Operations, said: "When it comes to eye<br />
sight it’s something that often can’t wait –<br />
and people shouldn’t. It’s vital that patients<br />
know that they can still come to BMEC and<br />
take advantage of our services. We want to<br />
get that message out and let people know<br />
that if they have an enquiry they can always<br />
contact our central phone line.”<br />
The advice given by the ophthalmology<br />
team is that any contact lens wearer who is<br />
experiencing eye pain, redness and reduced<br />
vision that doesn’t settle or gets worse over<br />
24 hours must attend eye casualty. If you<br />
are concerned about either eye related pain<br />
or loss of vision, don’t wait, either contact<br />
either our regions local urgent eyecare<br />
services, or alternately call our emergency<br />
and urgent care teams on 0121 507 4440<br />
where you will be given advice by one of our<br />
skilled ophthalmic nurse, or clinicians.<br />
23
Strength of teams praised at Rowley<br />
Regis and Leasowes<br />
PRIMARY CARE, COMMUNITIES<br />
AND THERAPIES<br />
“A unique time with some<br />
exceptional and sometimes<br />
unsettling challenges” was the way<br />
one colleague explained to <strong>Heartbeat</strong><br />
how COVID-19 had affected the lives<br />
of staff and patients at two of its<br />
facilities.<br />
With COVID-19 hitting hardest amongst<br />
the elderly and those with pre-existing<br />
health conditions, March and <strong>April</strong><br />
proved to be an ongoing battle for both<br />
the staff at Rowley Regis Hospital and the<br />
Leasowes End of Life Care Centre, each<br />
of which deals predominantly with elderly<br />
and frail patients.<br />
For colleagues at Rowley Regis, there<br />
has been not just the battle against<br />
coronavirus but an even bigger concern,<br />
if possible, to keep matters contained.<br />
There was a fear that the virus could<br />
travel rapidly through its patient base<br />
with deadly consequences if were not<br />
for the constant vigilance of doctors and<br />
nurses.<br />
One colleague told us: “As with all<br />
members of the Trust we’ve been going<br />
to great lengths, aided by the guidance<br />
put out by teams, such as infection<br />
control, to do all we can to help with this<br />
fight. For the Rowley teams, it’s a war not<br />
just for victory over COVID-19, but it’s a<br />
war for peace. Peace for all our patients<br />
whether blue or red. I’m so proud of all<br />
the teams at Rowley right now, they’re<br />
working so hard.”<br />
It’s a sense of pride that is echoed across<br />
the way at Leasowes. As readers can no<br />
doubt imagine, it has been a particularly tough<br />
time for colleagues at the centre, as the effects<br />
of the virus have accelerated the number of<br />
deaths seen. But whilst they had, ‘taken more<br />
than just one gut punch’ over the last couple<br />
of months, the team is still standing together.<br />
<strong>Heartbeat</strong> spoke to Palliative Care Team Leader,<br />
Sue Law and asked her to lay out just some of<br />
the challenges her team have faced.<br />
“Leasowes opened to 20 end of life patients on<br />
19 March, but within hours the palliative care<br />
team had identified an additional nine patients<br />
for transfer to Leasowes,” explains Sue. “This is<br />
a complex task as the palliative care team had<br />
to liaise with the ward teams, the patient, the<br />
family, transport and of course Leasowes itself<br />
to ensure it all flows easily for these patients.<br />
The Palliative Care Hub checks daily for patients<br />
from the wards or home who need to use a<br />
bed at Leasowes and then support the patients<br />
and families at this difficult time.”<br />
“Put simply, the workforce at Leasowes across<br />
the board have been brilliant. Working hard<br />
so that all patients and their families are well<br />
cared for at this most trying time. An example<br />
of the change in circumstances is that one of<br />
our specialist palliative care nurses changed<br />
her role to give a daily presence at Leasowes.<br />
This was necessary to not only prescribe and<br />
support families but offer to colleagues the<br />
support they needed in dealing with the<br />
ongoing situation and offer additional training<br />
on palliative concerns. At night the palliative<br />
urgent response team have supported the<br />
Leasowes team with symptom control and care<br />
after death when regretfully necessary.”<br />
Teams also worked together to ensure that vital<br />
equipment such as syringe drivers and oxygen<br />
concentrators have been readily available as<br />
demand increased, exacerbated by the nature<br />
of the virus. The palliative care consultants<br />
are also supporting the GPs and nurses<br />
with symptom control and issuing death<br />
certificates.<br />
Among the teams also namechecked for<br />
their hard work were the pharmacy team<br />
for their medicine delivery and the transport<br />
team for their helpfulness in providing a<br />
‘vital, essential and invaluable’ link to the<br />
facility. Praise was also heaped on the GPs<br />
from Your Health Partnership, who recently<br />
joined our Trust, for being steadfast in their<br />
support.<br />
The challenges faced by colleagues,<br />
particularly in regards to mental health,<br />
are far from unnoticed. The Trust has<br />
regularly shared the range of health and<br />
wellbeing support that is available to<br />
colleagues as part of the daily COVID-19<br />
bulletin. Services having been extended<br />
to help us all deal with the impact of the<br />
pandemic on our mental wellbeing. You<br />
can find examples of that help and advice<br />
here – some is specific to our Trust and<br />
other support listed is for all NHS workers.<br />
• Meet up with someone for a<br />
virtual coffee. Email<br />
swbh.letsgettalking.nhs.net<br />
• Do you need to talk to someone?<br />
Book a free confidential<br />
appointment with an accredited<br />
counsellor by calling 3306.<br />
• Individual resilience coaching can help.<br />
Email Richard.burnell@nhs.net to<br />
see if this is for you. You can also<br />
review the suite of wellbeing films<br />
and podcasts in our dedicated online<br />
library.<br />
One size does not fit all so speak up if<br />
there is something you need that is<br />
not currently available. You can email<br />
lawrencekelly@nhs.net - we want to<br />
hear from you.<br />
Chairman, Richard Samuda pictured in 2019 with colleagues from Leasowes<br />
24
Helping SWB put our best foot<br />
forward during COVID-19<br />
As many of you will know, podiatrists<br />
are healthcare professionals who have<br />
been trained to diagnose and treat<br />
abnormal conditions of the feet and<br />
lower limbs. They also prevent and<br />
correct deformity, keep people mobile<br />
and active, relieve pain and treat<br />
infections.<br />
With COVID-19 gripping the nation,<br />
colleagues at our Trust have had to change<br />
the way they do things to benefit both<br />
patients and our organisation. We caught<br />
up with Thomas Calderbank, Clinical Lead<br />
Podiatrist who told us more.<br />
“We have completely reconfigured our<br />
service. We are now only completing faceto-face<br />
care for our most vulnerable or<br />
urgent patients and supporting all of our<br />
other patients by telephone. This has seen<br />
an 80 per cent reduction in our normal<br />
face-to-face activity. That, in turn, is helping<br />
to protect the public by complying with<br />
government social isolation advice.<br />
“The other positive to come from this<br />
change is that our team have more time<br />
available to assist other areas. We currently<br />
have seven clinicians supporting the<br />
mortuary team, four clinicians supporting<br />
the swabbing team and two clinicians<br />
completing FIT testing. As well as this, we<br />
are also providing administrative support to<br />
the phlebotomy service where required.”<br />
Thomas Calderbank, Clinical Lead Podiatrist<br />
Thomas has been coordinating the team’s<br />
response to the pandemic and told us just<br />
how in awe he is of their willingness to<br />
take on new roles and challenges. “Some<br />
of the roles that our team have undertaken<br />
are far removed from their normal positions<br />
in foot health. One of our clinicians, Sarah<br />
Underhill, is currently working across four<br />
different services. This is in addition to her<br />
day job where she works as an advanced<br />
PRIMARY CARE, COMMUNITIES<br />
AND THERAPIES<br />
prescribing podiatrist working with<br />
our most at-risk patients. Sarah has<br />
been taking bloods on hot wards with<br />
the phlebotomy team, completing FIT<br />
testing and working in the mortuary. She<br />
is an absolute trooper, and she is just<br />
one of many people stepping outside<br />
of their usual roles to help us all fight<br />
COVID-19.”<br />
Another area where the team has got<br />
involved is in the community contact<br />
centre. Thomas explained: “The<br />
community contact centre at Sandwell<br />
keeps our department running. They<br />
cover all administrative aspects leaving<br />
our clinicians to focus on patient care. To<br />
free up the contact centre team who are<br />
now busy supporting other areas, our<br />
clinical team have almost entirely taken<br />
over the administrative side. This has<br />
been a real eye-opener to the amount<br />
of work the contact centre does on our<br />
behalf.”<br />
He added: “All in all, it has been a<br />
massive team effort. I’m proud of how<br />
everyone has chipped in and supported<br />
each other. We truly are all in this<br />
together.”<br />
Members of our podiatry team that have given their full support to keeping our Trust running smoothly during COVID-19 (photo taken before<br />
introduction of social distancing)<br />
25
World Autism Awareness<br />
Week <strong>2020</strong><br />
PRIMARY CARE, COMMUNITIES<br />
AND THERAPIES<br />
World Autism Awareness Week<br />
took place from 30 March – 5 <strong>April</strong><br />
this year. The week had one clear<br />
focus and that was to help raise<br />
awareness and acceptance for<br />
those who live with autism. To help<br />
find out how we support children<br />
within our Trust, we caught up with<br />
Meridith Durham, Children's Senior<br />
Occupational Therapist, and Natalie<br />
Pountney, Children's Senior Speech<br />
and Language Therapist.<br />
Meredith and Natalie work as part of<br />
Children’s Therapies and their role is to<br />
support children with autistic spectrum<br />
disorders (ASD) and their families and<br />
education providers to develop their<br />
communication, learning and wellbeing.<br />
Speech and language therapists and<br />
occupational therapists work closely with<br />
colleagues in both health and education<br />
in the diagnosis of ASD.<br />
Natalie explained ‘For nursery children,<br />
speech and language therapists<br />
support families to improve their child’s<br />
communication and wellbeing at home.<br />
For example, by setting up symbols to<br />
Children’s Therapies support children with<br />
autistic spectrum disorders (ASD), their<br />
families and education providers to develop<br />
their communication, learning and wellbeing.<br />
help children communicate and helping<br />
parents understand how to play with<br />
children to help their language development.<br />
For school-age children, schools can access<br />
training and drop-ins to help set up social<br />
skills groups, language activities and<br />
communication systems. For children who<br />
need symbols to help them to communicate,<br />
we work closely with schools and families.<br />
It’s very much a team effort’.<br />
Part of the occupational therapy service is<br />
to provide sensory education and advice to<br />
parents. Meridith told us: ‘Presentations,<br />
activities and discussion groups offer<br />
parents the opportunity to learn about<br />
sensory processing. The aim is to support<br />
them in understanding their child's sensory<br />
needs and develop strategies to help<br />
their child organise their sensory system.<br />
Due to COVID-19, the sensory education<br />
presentations and resources will be made<br />
available online. Please contact Children's<br />
Therapies on 0121 612 2345 if you would<br />
like more information’.<br />
As we all adapt to the evolving COVID-19<br />
situation it is important to establish routines<br />
that work for you and your family. This is<br />
especially important if you or someone you<br />
live with has autism as it provides order in<br />
what might otherwise feel like a world of<br />
chaos, and can make engaging in daily life<br />
much easier.<br />
We've outlined some top tips to help you<br />
develop a routine that works for you:<br />
• Support your autistic family member to<br />
understand the changes;<br />
• Put in structure, support and new<br />
routines to manage anxiety;<br />
• Focus on activities and learning to<br />
keep things positive.<br />
If you’d like to keep up to date<br />
with Children’s Therapies you can<br />
follow them on social media. Visit<br />
@SandwellSPOT on Twitter and<br />
SWBH_ChildrensTherapies on Facebook<br />
for all the latest news.<br />
26
It’s time to talk about the menopause<br />
Vicki Fox delivers the seminar on menopause<br />
Seminars are taking place to help<br />
women working within our Trust who<br />
are going through the menopause.<br />
The sessions cover reasons it happens,<br />
hormones, as well as signs and symptoms.<br />
Run by Vicki Fox, Care Services Manager<br />
from The Kaleidoscope Plus Group, the<br />
seminars also share statistics, the impact of the<br />
menopause, how it affects our stress levels,<br />
what we can do, self-care, and workplace<br />
adjustments.<br />
The Kaleidoscope Plus Group developed<br />
a course as it became clear that working<br />
women were struggling to understand their<br />
symptoms. Vicki said: “The sessions are open<br />
to anyone, including managers supporting<br />
those experiencing the menopause and those<br />
going through it themselves. We want to<br />
normalise women’s experiences and give them<br />
the tools to make the transition as comfortable<br />
as possible.”<br />
Symptoms of the menopause include hot<br />
flushes, a feeling of nowhere to escape<br />
WOMEN AND CHILD HEALTH<br />
to, brain fog, lack of concentration,<br />
confusion, embarrassment, selfconsciousness<br />
and many more.<br />
Speaking to <strong>Heartbeat</strong>, Vicki said, “The<br />
more sessions that are held, the more we<br />
discover. These seminars will give women<br />
the tools to help themselves; they’ll learn<br />
how to build their resilience and what<br />
treatments are available. We also look<br />
at what reasonable adjustments can be<br />
requested in the workplace.”<br />
To find out more contact the<br />
occupational health team on<br />
extension 3306, option 4.<br />
Maternity teams up with Baggies and<br />
the Villa to provide clinics for women<br />
Our maternity department has teamed<br />
up with the Baggies and the Villa to<br />
set up temporary clinics at the football<br />
clubs. The facilities are for women<br />
undergoing antenatal and postnatal<br />
care and have been set up at the West<br />
Bromwich Albion and Aston Villa<br />
grounds.<br />
Helen Hurst, Director of Midwifery, said:<br />
“We wanted to provide an alternative space<br />
for women who are having antenatal and<br />
postnatal care. Women are slightly anxious<br />
about coming to the hospital in the current<br />
climate so we wanted to find a safe space<br />
away from the hospital.<br />
“It will be for women who are 24 weeks<br />
onwards, and there will be postnatal clinics<br />
for those who have been discharged. It will<br />
be as safe as the services that are currently<br />
provided by our midwives within the<br />
community and in GP clinics. Should the<br />
need arise, we will be able to call on the<br />
ambulance service.”<br />
Albion Chief Executive, Mark Jenkins, said:<br />
“We are more than happy to open our<br />
doors to enable this vital service to be safely<br />
conducted. It is another example of how<br />
the club can help within our community<br />
during the pandemic, something we are<br />
determined to continue to do. We like to<br />
think you are never too young to join the<br />
Albion family.”<br />
Guy Rippon, Head of Foundation and<br />
Community Partnerships at Aston Villa,<br />
Some of our nursing colleagues pictured at West Bromwich and Aston Villa FC<br />
said: “We are delighted to be able to help<br />
out our local NHS hospitals by opening up<br />
Villa Park as a temporary maternity clinic.<br />
During these uncertain times, our famous<br />
home will provide a safe environment for<br />
local expectant mothers and their midwives<br />
and nurses to be able to carry out their vital<br />
work.”<br />
Three clinics will run at the Baggies<br />
Monday to Friday, between 9am and<br />
5pm in the East Stand.<br />
Five clinics will run at the Villa from<br />
Monday to Friday, between 9am and<br />
5pm in the North Stand.<br />
27
Putting patients first during<br />
COVID-19<br />
IMAGING<br />
Radiology have been doing A-OK as they<br />
work remotely and adapt their services<br />
during the COVID-19 pandemic.<br />
COVID-19 has undoubtedly changed<br />
the way we do things across our Trust.<br />
What it has shown us over the past<br />
few weeks is just how resilient we<br />
are. One of the most positive things<br />
to come out of this pandemic so far is<br />
our ability to adapt and keep pushing<br />
forward to deliver the best patient<br />
outcomes.<br />
Our radiology team are just one of many<br />
to have changed the way they do things.<br />
One of the main adjustments has seen<br />
colleagues working from home. Previously<br />
some members of the team had taken<br />
advantage of working flexibly at home;<br />
however, it has now become the norm for<br />
many of our radiologists.<br />
We caught up with Fiona Rotherham,<br />
Deputy Group Director of Operations,<br />
Imaging, who told us more. “A number of<br />
our radiologists have been reporting from<br />
home before the outbreak of COVID-19.<br />
However, with the current pandemic,<br />
many more are now routinely working<br />
remotely. This has been facilitated by<br />
the IT/PACS team who have helped us<br />
The fracture clinic gets plastered for<br />
a good cause!<br />
Orthopaedic Practitioners, Stephanie<br />
Craig and Steven Hackett-Cann have<br />
recently led a project at City fracture<br />
clinic to create a children’s corner in<br />
the plaster room. As anyone who’s<br />
ever broken a bone or had a fracture<br />
will know the thought of getting<br />
yourself put back together is a<br />
daunting prospect.<br />
The colourful play area was created to<br />
make children’s experiences within the<br />
clinic more welcoming. Equipped with<br />
everything from a portable DVD player<br />
to watch films on, to books, bubbles and<br />
colouring in posters, the area has been<br />
designed to ensure our young patients are<br />
entertained. It also means that children<br />
are distracted from thinking about the<br />
procedures they are about to undergo.<br />
Pleased with how the transformation has<br />
gone, Stephanie said: “We felt collectively<br />
as a team that we could make our area<br />
more inviting for children. Steven and I<br />
have taken the lead on this project, but it<br />
has been a team effort. We couldn’t have<br />
made this happen without the support of<br />
our colleagues. We have enjoyed working<br />
on a project that we know makes a real<br />
difference to the children we look after.”<br />
The revamped children’s area<br />
Steven added: “It’s a pleasure to see<br />
our young patients enjoying the area.<br />
It’s turned out just as planned and, we<br />
couldn’t be happier with the results. It<br />
brings a smile to your face knowing that<br />
you’ve done something that makes a<br />
hospital visit that bit more pleasurable.”<br />
Denise Gnosill, Sister in the fracture clinic,<br />
told <strong>Heartbeat</strong>: “Stephanie and Steven<br />
have worked incredibly hard to create<br />
an area that children find friendly and<br />
with the provision of specialist reporting<br />
equipment.<br />
“Our radiologists can review images taken<br />
at all of our sites and report them at<br />
home, in addition to also vetting requests<br />
and providing an off-site advisory service.<br />
Being able to work in this way has meant<br />
that any radiologists required to isolate or<br />
shield at home during this pandemic can<br />
continue to support Imaging which we are<br />
thankful for.<br />
Sarah Yusuf, Group Director, Imaging<br />
added: “I am proud of the way the team<br />
have adjusted over the last few weeks. As<br />
well as working remotely, something new<br />
we are doing is providing a consultant-led<br />
on-call service due to the redeployment<br />
of our junior doctors’. The team adapted<br />
to this new working pattern within a<br />
week and what it means is that there<br />
is consultant cover every night and at<br />
weekends to vet and report emergency<br />
and inpatient plain film and CT requests.<br />
We know this is a particularly stressful<br />
time for our patients, so we are doing all<br />
we can to ensure things run as smoothly<br />
as possible for them.”<br />
where they can relax. These changes mean<br />
that they have something to divert their<br />
attention. It also makes the experience<br />
of visiting the hospital less scary and<br />
overwhelming.”<br />
The transformation of the children’s corner<br />
has been so successful that Sandwell<br />
Hospital is in the process of creating their<br />
very own child-friendly area.<br />
Well done to Stephanie, Steve and the<br />
team at City fracture clinic.<br />
28
Our local community has shown their appreciation for the NHS by proudly displaying posters<br />
in their windows. Thank you for all that you are doing to keep us all safe and healthy.<br />
29
Letters, of less than 200 words please, can be sent to the Communications Department,<br />
Trust Headquarters, Sandwell Hospital or by email to swb–tr.SWBH–GM–<strong>Heartbeat</strong>@nhs.net<br />
YOUR RIGHT TO BE HEARD<br />
Wind tunnel outside Anne<br />
Gibson for shuttle bus<br />
Dear <strong>Heartbeat</strong>,<br />
Are there plans to create a wind/weather<br />
break for those waiting for the shuttle<br />
under the portico at the Anne Gibson<br />
pickup spot maybe along the lines of the<br />
shelter provided at Sandwell?<br />
Before Anne Gibson was closed you<br />
could, if you arrived slightly early for the<br />
shuttle and the weather was inclement,<br />
go through the doors and shelter whilst<br />
waiting; now you are standing exposed<br />
to the elements.<br />
I appreciate that if you are able to time<br />
your arrival to just before the shuttle<br />
leaves it would be less of an issue but,<br />
sometimes you are not able to do that<br />
and what if the shuttle was running<br />
behind schedule?<br />
Regards,<br />
Anon<br />
Thanks for your letter and I’m sorry<br />
that you are suffering from being<br />
cold while you wait for the shuttle<br />
bus. Hopefully you are able to at<br />
least shelter from the rain under the<br />
portico. We may be relocating the<br />
bus stop in the future as the Anne<br />
Gibson rooms have been taken out<br />
of use, so we will consider something<br />
that provides more shelter before<br />
the winter.<br />
Best wishes,<br />
Rachel Barlow, Director of System<br />
Transformation<br />
Annual leave – what will be<br />
happening coming March<br />
2021!?<br />
Dear <strong>Heartbeat</strong>,<br />
I’m sure I’m not the only one, but during<br />
the COVID-19 pandemic everyone at the<br />
Trust (both clinical and non- clinical staff)<br />
have been working really hard. However,<br />
when we are hopefully through the thick<br />
of it what will happen with annual leave?<br />
Will a lot the staff be forced to take the<br />
majority of their leave before March 2021<br />
meaning there will be reduced staffing<br />
numbers or will we be allowed to carry over<br />
limited days depending on our individual<br />
circumstances? Will the Trust pay us back<br />
the leave we don’t take perhaps? If we<br />
could have clarification on this matter that<br />
would be great.<br />
Anon<br />
Dear colleague,<br />
We very much want people to take<br />
annual leave and in most parts of the<br />
Trust currently it is not workload that is<br />
leading to leave stand-down. Instead it<br />
is individuals feeling that a lock-down<br />
fortnight at home was not the vacation<br />
they had in mind. There are exceptions<br />
to that where colleagues have very<br />
decently foregone leave for service<br />
need. We will revisit the possibility<br />
of us buying out leave for individuals<br />
(not en masse) in July and August. You<br />
rightly worry about a bulk of leave<br />
taken together later in the year. We are<br />
working on leave guidance but expect<br />
to treat leave as a two year matter<br />
across <strong>April</strong> <strong>2020</strong> to March 2022 because<br />
of Covid-19, notwithstanding leave<br />
constraints that the move into Midland<br />
Met in early summer 2022 may impose!<br />
Kind regards,<br />
Frieza Mahmood, Deputy Director –<br />
People and Organisation Development<br />
COVID+ offices should be closed<br />
Dear <strong>Heartbeat</strong>,<br />
As a matter of deep concern we wish<br />
to bring to your attention that a contact<br />
centre within the Hallam building at<br />
Sandwell General Hospital continues to<br />
operate fully staffed and in situ when we<br />
believe members of its staff have been<br />
positively identified as having COVID-19.<br />
If COVID-19 has been positively identified<br />
within this office surely it should be realised<br />
that there is a high likelihood that other<br />
members of staff have been infected and<br />
are therefore infectious (even amongst<br />
those that may not show symptoms).<br />
So why is this office still open? Remember<br />
these are office staff not frontline medical<br />
staff (who have taken an oath of duty and<br />
care and the risks that go with the job)…<br />
In order to contain this situation and avoid<br />
and further occurrences and the possible<br />
consequences that go with it, we hope you<br />
will give this your urgent attention.<br />
Kind regards<br />
Anon<br />
Dear colleague,<br />
I am really sorry that you feel you have<br />
to raise this concern anonymously<br />
and would hope that you would have<br />
approached the management team for<br />
this unit directly, or raised it with me or<br />
others in such a way that I can actually<br />
help you. Social distancing is important<br />
in all workplaces and managers and<br />
staff have been asked to ensure that<br />
you take local responsibility for that.<br />
It is not sensible to suggest that if one<br />
person in a team has tested positive for<br />
COVID-19 that we can be confident it<br />
was conveyed at work, nor that that<br />
should lead us to extreme measures in<br />
terms of workplace colleagues’ welfare.<br />
The whole point about testing is that<br />
it should be matched with tracing, and<br />
a sensitive, non-stigmatising approach<br />
to those who could have come into<br />
contact with one of us with COVID-19.<br />
It will be incredibly important in coming<br />
weeks that we approach this as one<br />
organisation. Of course you are right<br />
that we are looking at home working<br />
and how it is extended and you should<br />
consult the bulletin for details of our<br />
updated guidance in early May. What<br />
all of us can do, working at home or on<br />
site, to take responsibility for our own<br />
social distancing, challenging others’,<br />
and, of course for hand washing over<br />
and over and over again.<br />
Toby Lewis, Chief Executive<br />
30
Toby writes about… the future‘s bright,<br />
the future’s orange<br />
TobyLewis_SWBH<br />
TOBY’S LAST WORD<br />
I know the headline for this article is<br />
an old technology strapline, which felt<br />
appropriate as the NHS moves through<br />
a year where doing stuff via WebEx or<br />
Visionable has suddenly become almost<br />
second nature. This though is not an<br />
article all about the virus.<br />
While we work and worry, the<br />
construction of the Midland<br />
Metropolitan University Hospital<br />
continues. Almost 200 people are<br />
working on the project currently, and<br />
that will rise nearer to 900 towards the<br />
end of the year. The Board has asked<br />
for assurance on their safety and social<br />
distancing, just as Balfour’s has. Of<br />
course, the real challenge is how supply<br />
chains are managed in a lockdown, or<br />
lockdown-lite, situation. But the real<br />
economy demands that we press on.<br />
Our Victorian wards and 1970s bays<br />
are the backdrop to what we are doing<br />
now. They really bring home to me<br />
what good design could do to help us<br />
work and to help outcomes. Over 300<br />
single rooms will give us the chance<br />
to isolate and manage outbreaks that<br />
currently we struggle sometimes to<br />
do. A modern design for critical care<br />
with some expansion space as well.<br />
Adjacencies that do not require so<br />
much lift movement, be it blue or red.<br />
Imaging sat right next to ED.<br />
Anyway, I am not writing this article<br />
just to show you light at the end of the<br />
tunnel. Instead to make sure that we<br />
are all, and I know many are, thinking<br />
now about the service design we<br />
need for 2022. The clinical model for<br />
Midland Met starts in primary care.<br />
How we best support people in their<br />
own home, how we ‘case-find’ people<br />
who may be deteriorating. What can<br />
we can do remotely to ensure best<br />
management of high blood pressure, or<br />
the best support to our care homes, and<br />
in local schools? All the things that have<br />
been the focus of our attention in recent<br />
weeks and in our strategy for several<br />
years. The NHS ‘restoration and recovery’<br />
story needs to be with this in mind.<br />
Midland Met in 2032, or 2027, will<br />
only be right-sized if we succeed. We<br />
have to cut admission numbers over<br />
the decade where our population ages<br />
and grows, and make sure that stays in<br />
the nine floors of the hospital are only<br />
during an acute phase of care. What<br />
the design does give us is a caring<br />
environment that helps to put kindness<br />
more easily into how we work, with<br />
privacy, bathrooms designed for those on<br />
crutches and in wheelchairs, and kitchens<br />
and ‘normal life’ in the centre of how we<br />
rehabilitate people. That compassion has<br />
always been important. It feels urgent<br />
now.<br />
Remember, we have a 3D virtual reality<br />
vision of the new hospital available in<br />
our libraries. We are asking teams now to<br />
be thinking about how you might work<br />
in 700 days’ time. The acute rotas we<br />
have created to cope with COVID-19 may<br />
not be the ones we need then, but<br />
our pre-COVID rotas certainly are<br />
not either. By the end of <strong>2020</strong> we<br />
intend to lockdown (in a different<br />
sense) the clinical model that we<br />
will work with – so that 2021 can<br />
be spent simulating how to work<br />
that way before the move. Rachel<br />
Barlow, Jayne Dunn and the team<br />
are working to prepare material and<br />
ideas and to engage and involve<br />
you in how that will work. The<br />
robots are arriving shortly to support<br />
distribution (not that our PPE hubs<br />
have not been fantastic). As those<br />
references imply we want to make<br />
it easier in MMUH for clinicians<br />
to focus on patient care, with a<br />
user-focused model of supply of<br />
medicines, kit and wellbeing that<br />
maximises your time to look after<br />
yourself and your patients.<br />
The spirit of just-try and experiment<br />
that has sat around our response<br />
to the pandemic has been at times<br />
inspiring. That does not mean that<br />
no plan for the new hospital is<br />
required. Rather that we ought to<br />
have confidence in our ability to<br />
innovate and change, to calibrate<br />
risk, and to work differently and<br />
smarter. We must carry the emphasis<br />
on wellbeing and peer support into<br />
that endeavour, and to make sure<br />
that the weariness of the year ahead<br />
does not mean 2022 comes upon<br />
us too fast. I am sure we can do<br />
that. It will be a massive effort. But<br />
worthwhile in so many ways as we<br />
aim to make the site the very best<br />
of what only the NHS can do. We<br />
might even clap when we open.<br />
31
A pop-up lifeline<br />
YOUR TRUST CHARITY<br />
@SWBHCharity To donate<br />
to the Your Trust Charity text<br />
“SWBH16 £5” to 70070<br />
As the effects of the coronavirus have<br />
continued to be felt up and down the<br />
country, what was the normalcy of<br />
life has been fundamentally altered.<br />
Things that we once took for granted<br />
are now tasks that have to be planned,<br />
sometimes meticulously planned.<br />
With longer hours and the uncertainty<br />
of what the day will bring, even going<br />
shopping has become a logistical<br />
hurdle for numerous colleagues<br />
around our organisation.<br />
As part of the ongoing efforts around<br />
all our sites to try to make things a bit<br />
more manageable, a new pop-up shop<br />
for colleagues has opened in Sandwell<br />
Hospital’s learning and development room.<br />
Its creation, masterminded by Your Trust<br />
Charity, was achieved through the help<br />
and generosity of both colleagues and<br />
the community. Now open Mondays,<br />
Wednesdays and Fridays, Sandwell workers<br />
can, once a week, take a quick browse<br />
of the shelves and stock up on essentials<br />
such as bread, pasta, toiletries, fruit, veg<br />
and even cleaning products. There’s also<br />
the odd treat as well for those in need of a<br />
sweet treat.<br />
Fundraising Manager, Amanda Winwood<br />
is the driving force behind efforts for Your<br />
Trust Charity, she told <strong>Heartbeat</strong>: “We<br />
have been extremely lucky to be able to<br />
procure a wide array of products for the<br />
store thanks to access to warehouses<br />
and contacting wholesalers. Some of<br />
it we are selling, other items such as<br />
water cartons, the fruit and vegetables and<br />
cleaning products are given as freebies to<br />
each shopper to help things along. The latter<br />
was only made possible from NewG420 Ltd<br />
which works out to about £25,000 in soap,<br />
disinfectant and other cleaning products.”<br />
If you are based at City Hospital, there is a<br />
service also available at Nisa Local, Crabtree<br />
Road a 5 min walk from the hospital. The<br />
shop has opened up to give colleagues early<br />
access from 7am-8am and 7pm-8pm. Ensure<br />
you have your ID badge with you to allow<br />
you in. Rav Garcha, the store manager, is<br />
also organising an option to order via their<br />
Facebook page (click and collect) where they<br />
will bring your shopping out to the car. The<br />
click and collect is in the very early stages but<br />
hope that it will benefit you.<br />
Other organisations that have helped include<br />
Bristnall Hall Academy, which provided<br />
sandwiches, crisps and drinks, enough for 10<br />
days’ worth of packed lunches. Prestige Suite<br />
has been cooking chilled meals that have<br />
been delivered to City, Sandwell and Rowley<br />
Regis hospitals daily along with fresh fruit.<br />
In total over £50,000 in donations have<br />
been accrued, be it cash, stock or through<br />
other donation methods such as Your Trust<br />
Charity’s Amazon Wish List which has seen<br />
members of the public support doctors and<br />
nurses though much needed donations of<br />
hand cream, sanitiser and other personal<br />
hygiene products.<br />
“We all felt this was needed. We saw the<br />
public over buying essential goods causing<br />
a shortage. Front line staff, who are putting<br />
their lives at risk, were unable to have the<br />
daily essentials we all need and deserve,”<br />
explains Jay from NewG420 on his company’s<br />
gesture. “We are fortunate enough to have<br />
these supplies available, and this is the time<br />
we need to give back to the community and<br />
fight back against this pandemic. Our faith<br />
teaches us to earn our living and share what<br />
we have, and that’s what we are doing along<br />
with our friends.”<br />
It's been a busy month for Your Trust Charity<br />
supporting our colleagues and the local<br />
community. A big thank you to everyone that<br />
has donated goods and their time.<br />
<strong>April</strong> <strong>2020</strong> staff lottery results<br />
1st £192.50<br />
Madhane Glenn<br />
2nd £115.50<br />
Jane Burton<br />
3rd £77<br />
Catherine Heron<br />
Don’t forget that Your Trust Charity lottery costs just £1 a month and anyone<br />
who works for the Trust can join. Payment is deducted from your wages each<br />
month. To take part email amanda.winwood@nhs.net.