Susan Wu, MD, FAAP, Editor - American Academy of Pediatrics
Susan Wu, MD, FAAP, Editor - American Academy of Pediatrics
Susan Wu, MD, FAAP, Editor - American Academy of Pediatrics
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
In Conclusion<br />
The inpatient management <strong>of</strong> patients<br />
with eating disorders can be challenging,<br />
both medically and socially. However,<br />
the medical risks <strong>of</strong> these illnesses are<br />
real, and lifetime mortality rates are<br />
remarkably high. Inpatient physicians<br />
can find solace in the fact that most<br />
eating disorder patients, especially those<br />
who are adolescents or young adults,<br />
recover when they receive a combination<br />
<strong>of</strong> appropriate nutritional therapy and<br />
aggressive psychosocial support.<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
REFERENCES<br />
1. www.nationaleatingdisorders.org<br />
2. Robergeau et al., Hopitalization <strong>of</strong> Children<br />
and Adolescents for Eating Disorders<br />
in the State <strong>of</strong> New York, Journal <strong>of</strong><br />
Adolescent Health 39, p. 806-810, 2006.<br />
3. Katzman, D., Medical Complications<br />
in Adolescents with Anorexia Nervosa:<br />
A Review <strong>of</strong> the Literature, Int J<br />
Eat Disord 37, S52-59, 2005.<br />
4. AAP Policy Statement on Identifying and<br />
Treating Eating Disorders, Committee<br />
on Adolescence, January 2003.<br />
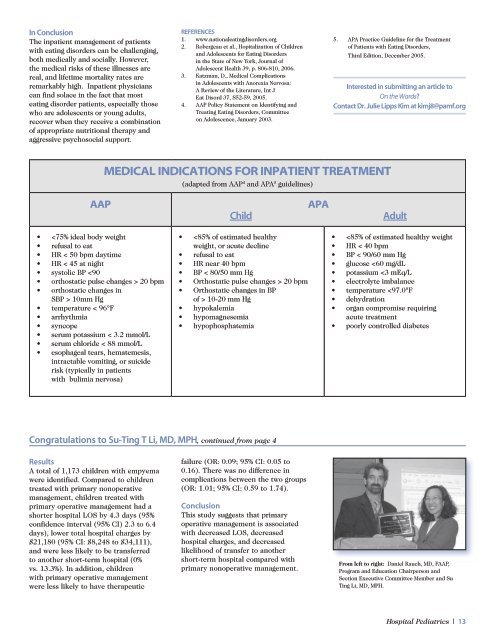
MEDICAL INDICATIONS FOR INPATIENT TREATMENT<br />
(adapted from AAP 4 and APA 5 guidelines)<br />
5.<br />
APA Practice Guideline for the Treatment<br />
<strong>of</strong> Patients with Eating Disorders,<br />
Third Edition, December 2005.<br />
Interested in submitting an article to<br />
On the Wards?<br />
Contact Dr. Julie Lipps Kim at kimj8@pamf.org<br />
AAP APA<br />
Child Adult<br />
10mm Hg<br />
temperature < 96°F<br />
arrhythmia<br />
syncope<br />
serum potassium < 3.2 mmol/L<br />
serum chloride < 88 mmol/L<br />
esophageal tears, hematemesis,<br />
intractable vomiting, or suicide<br />
risk (typically in patients<br />
with bulimia nervosa)<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
20 bpm<br />
Orthostatic changes in BP<br />
<strong>of</strong> > 10-20 mm Hg<br />
hypokalemia<br />
hypomagnesemia<br />
hypophosphatemia<br />
Congratulations to Su-Ting T Li, <strong>MD</strong>, MPH, continued from page 4<br />
Results<br />
A total <strong>of</strong> 1,173 children with empyema<br />
were identified. Compared to children<br />
treated with primary nonoperative<br />
management, children treated with<br />
primary operative management had a<br />
shorter hospital LOS by 4.3 days (95%<br />
confidence interval (95% CI) 2.3 to 6.4<br />
days), lower total hospital charges by<br />
$21,180 (95% CI: $8,248 to $34,111),<br />
and were less likely to be transferred<br />
to another short-term hospital (0%<br />
vs. 13.3%). In addition, children<br />
with primary operative management<br />
were less likely to have therapeutic<br />
failure (OR: 0.09; 95% CI: 0.05 to<br />
0.16). There was no difference in<br />
complications between the two groups<br />
(OR: 1.01; 95% CI: 0.59 to 1.74).<br />
Conclusion<br />
This study suggests that primary<br />
operative management is associated<br />
with decreased LOS, decreased<br />
hospital charges, and decreased<br />
likelihood <strong>of</strong> transfer to another<br />
short-term hospital compared with<br />
primary nonoperative management.<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />