Coding and Billing for Outpatient Rehab Made Easy
Coding and Billing for Outpatient Rehab Made Easy
Coding and Billing for Outpatient Rehab Made Easy
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
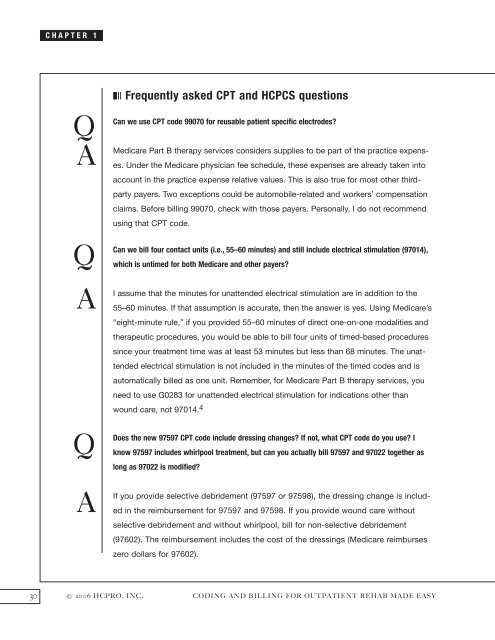
CHAPTER 1<br />
Q A<br />
Q<br />
A<br />
Q<br />
A<br />
❚❘❘ Frequently asked CPT <strong>and</strong> HCPCS questions<br />
Can we use CPT code 99070 <strong>for</strong> reusable patient specific electrodes?<br />
Medicare Part B therapy services considers supplies to be part of the practice expenses.<br />
Under the Medicare physician fee schedule, these expenses are already taken into<br />
account in the practice expense relative values. This is also true <strong>for</strong> most other thirdparty<br />
payers. Two exceptions could be automobile-related <strong>and</strong> workers’ compensation<br />
claims. Be<strong>for</strong>e billing 99070, check with those payers. Personally, I do not recommend<br />
using that CPT code.<br />
Can we bill four contact units (i.e., 55–60 minutes) <strong>and</strong> still include electrical stimulation (97014),<br />
which is untimed <strong>for</strong> both Medicare <strong>and</strong> other payers?<br />
I assume that the minutes <strong>for</strong> unattended electrical stimulation are in addition to the<br />
55–60 minutes. If that assumption is accurate, then the answer is yes. Using Medicare’s<br />
“eight-minute rule,” if you provided 55–60 minutes of direct one-on-one modalities <strong>and</strong><br />
therapeutic procedures, you would be able to bill four units of timed-based procedures<br />
since your treatment time was at least 53 minutes but less than 68 minutes. The unattended<br />
electrical stimulation is not included in the minutes of the timed codes <strong>and</strong> is<br />
automatically billed as one unit. Remember, <strong>for</strong> Medicare Part B therapy services, you<br />
need to use G0283 <strong>for</strong> unattended electrical stimulation <strong>for</strong> indications other than<br />
wound care, not 97014. 4<br />
Does the new 97597 CPT code include dressing changes? If not, what CPT code do you use? I<br />
know 97597 includes whirlpool treatment, but can you actually bill 97597 <strong>and</strong> 97022 together as<br />
long as 97022 is modified?<br />
If you provide selective debridement (97597 or 97598), the dressing change is included<br />
in the reimbursement <strong>for</strong> 97597 <strong>and</strong> 97598. If you provide wound care without<br />
selective debridement <strong>and</strong> without whirlpool, bill <strong>for</strong> non-selective debridement<br />
(97602). The reimbursement includes the cost of the dressings (Medicare reimburses<br />
zero dollars <strong>for</strong> 97602).<br />
30 © 2006 HCPRO, INC. CODING AND BILLING FOR OUTPATIENT REHAB MADE EASY