Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
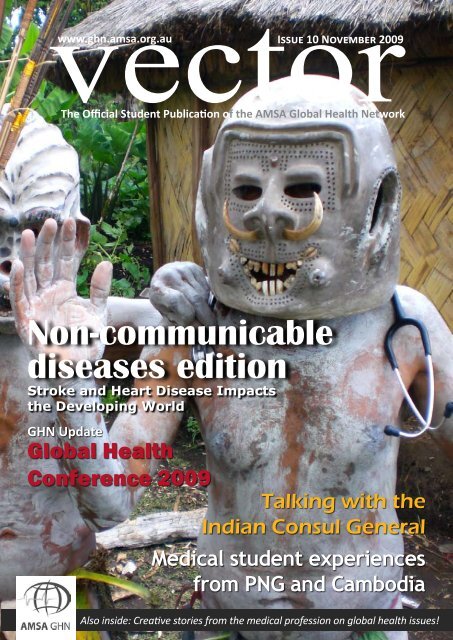
vector<br />
The Official Student Publication of the AMSA Global Health Network<br />
www.ghn.amsa.org.au<br />
<strong>Issue</strong> <strong>10</strong> November <strong>2009</strong><br />
Non-communicable<br />
diseases edition<br />
Stroke and Heart Disease Impacts<br />
the Developing World<br />
GHN Update<br />
Global Health<br />
Conference <strong>2009</strong><br />
Talking with the<br />
Indian Consul General<br />
Medical student experiences<br />
from PNG and Cambodia<br />
Also inside: Creative stories from the medical profession on global health issues!
contents<br />
issue <strong>10</strong> november <strong>2009</strong><br />
3 Editor’s Note<br />
11<br />
9<br />
4 What Lurks in the Shadows: noncommunicable<br />
disease in the<br />
developing world<br />
5 Heart Disease and Stroke Threaten<br />
Developing World<br />
6 Tipping the Scales: the ‘expansion’<br />
of the global community<br />
8 Smoking and Tobacco’s Impact<br />
on the Developing World: the<br />
worlds top health priority<br />
9 A Conversation with the Indian<br />
Consul General<br />
<strong>10</strong> The Nageri Misiion<br />
11 Mental Health Crisis in China<br />
12 Medicine and Mosquitoes: a<br />
medical student’s month in<br />
Papua New Guinea<br />
13 Stories from Cambodia<br />
14 Global Health In The News<br />
www.ghn.amsa.org.au<br />
16 13<br />
the<br />
non-communicable<br />
diseases<br />
edition<br />
2 vector november <strong>2009</strong><br />
Global Health Network Update<br />
15 Welcome to the GHN<br />
15 A Year in the GHN: Looking back<br />
and Looking Forwards<br />
16 The Global Health Conference:<br />
Challenging the world after<br />
Brisbane<br />
17 Global Health Series - University<br />
of Sydney<br />
17 Student Involvement - Helping<br />
VSAP to help others<br />
Creative Pieces<br />
18 The Boy who Jumped off the<br />
Bridge<br />
19 Noor<br />
20 at a Glance: India
editor’s<br />
note<br />
“<br />
Kruthika Narayan<br />
Vikram Joshi<br />
Rami Subhi<br />
The golden arches of McDonalds<br />
have become a ubiquitous metaphor<br />
for globalisation; previously in<br />
the economic sense, but perhaps<br />
now as a symbol of the global epidemic of<br />
‘lifestyle’ diseases. There is an inherent irony<br />
in that the very symbols of prosperity and<br />
growth have become emblems for illness, in<br />
the developed world with growing incidence<br />
of chronic non-communicable diseases<br />
(NCDs).<br />
The picture is both similar and different<br />
in the less developed world. Instead of representing<br />
the dangers of excess, the rampant<br />
increase in NCDs in less-developed countries<br />
Non-communicable diseases, with their precursors of<br />
high cholesterol, hypertension and obesity, are overwhelming<br />
the developing world much faster than the<br />
developed<br />
reflects the deficiencies of stretched health<br />
systems traditionally geared towards relief<br />
of acute illness in handling the immense<br />
burdens of chronic disease. It also highlights<br />
the effects of environmental exploitation<br />
limiting access to fresh healthy foods, and<br />
the dire struggle of the growing populations<br />
of the urban poor for whom chronic disease<br />
is yet another force perpetuating the vicious<br />
cycle of poverty.<br />
Non-communicable diseases, with their<br />
precursors of high cholesterol, hypertension<br />
and obesity, are overwhelming the developing<br />
world much faster than the developed.<br />
Added to this are high rates of smoking and<br />
the long standing struggle against chronic<br />
infections.<br />
The World Health Organisation estimates<br />
that NCDs, including cardiovascular disease,<br />
diabetes, cancer and respiratory diseases,<br />
are responsible for over half of all deaths and<br />
46% of the global disease burden.<br />
Health issues in the developing world<br />
have thus far concentrated on communicable<br />
diseases; and rightly so, since many of these<br />
are preventable and/or readily treatable. But<br />
with the rise of NCDs including HIV/AIDS, an<br />
emerging concern about the influence of climate<br />
change and the environment on health<br />
outcomes, and the appreciation<br />
of the economic<br />
implications of chronic<br />
diseases particularly when<br />
compounded with poverty<br />
and failing health systems,<br />
it is time to promote the<br />
”<br />
complexities of NCDs on the<br />
global agenda.<br />
In this issue of <strong>Vector</strong>,<br />
we consider the impact of<br />
non-communicable diseases in settings least<br />
equipped to bear the burden of mortality,<br />
morbidity and economic strain they impose.<br />
The challenges are immense. The experience<br />
of the Western World attests to the difficulty<br />
in preventing and treating chronic disease; a<br />
difficulty compounded by the resource limitations<br />
of low income countries. The multifactorial<br />
causes of NCDs require a shift in<br />
attitude, not just in local government policies<br />
but in the ethics of operation of industries,<br />
corporations and nations, and a shift in the<br />
perceptions of the global society as a whole.<br />
<strong>Vector</strong>: The Official Student Publication of the AMSA Global<br />
Health Network<br />
GHN Publicity Officer<br />
Editors<br />
Design & Layout<br />
Catherine Pendrey<br />
Kruthika Nayaran<br />
Vikram Joshi<br />
Rami Subhi<br />
Alexander Murphy<br />
Editorial enquiries: Email vectormag@gmail.com<br />
GHN enquiries: ghn.publicity@gmail.com<br />
or visit www.ghn.amsa.org.au<br />
We welcome your written submissions, letters<br />
and photos on any global health issue or topic.<br />
Please limit submissions to 500 words or less.<br />
Cover Photo: The locals in Papua New Guinea<br />
// Image by Georgia Ritchie, Medical Student,<br />
University of Sydney<br />
november <strong>2009</strong> vector3<br />
www.ghn.amsa.org.au
What lurks in the shadows:<br />
non-communicable disease in the developing world<br />
Words Fred Hersch, Medical student, University of Sydney<br />
// Image by xymonau (sxc.hu)<br />
www.ghn.amsa.org.au<br />
1.Tunstall-Pedoe H. Preventing Chronic Diseases.<br />
A Vital Investment: WHO Global Report. Geneva: World<br />
Health Organization, 2005. pp 200. CHF 30.00. ISBN 92<br />
4 1563001. Also published on http://www.who.int/chp/<br />
chronic_disease_report/en. Int J Epidemiol. 2006 Jul 19.<br />
2.AD Lopez CM, M Ezzati, DT Jamison and CJL<br />
Murray, Editors. Global burden of disease and risk factorsnext<br />
term, Oxford University Press, New York2006.<br />
3.Gaziano TA. Economic burden and the costeffectiveness<br />
of treatment of cardiovascular diseases in<br />
Africa. Heart. 2008 Feb;94(2):140-4.<br />
4.Leeder Sea. A Race Against Time: The Challenge<br />
of Cardiovascular Disease in Developing Countries (New<br />
York: Trustees of Columbia University)2004.<br />
5.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum<br />
A, Lanas F, et al. Effect of potentially modifiable risk factors<br />
associated with myocardial infarction in 52 countries<br />
(the INTERHEART study): case-control study. Lancet.<br />
2004 Sep 11-17;364(9438):937-52.<br />
6.Steyn K, Sliwa K, Hawken S, Commerford P,<br />
Onen C, Damasceno A, et al. Risk factors associated<br />
with myocardial infarction in Africa: the INTERHEART<br />
Africa study. Circulation. 2005 Dec 6;112(23):3554-61.<br />
7.Thomas A. Gaziano KSR, Fred Paccaud, Susan<br />
Horton, and Vivek Chaturvedi. 2006., editor. "Cardiovascular<br />
Disease."2006.<br />
8.Joshi R, Jan S, Wu Y, MacMahon S. Global<br />
inequalities in access to cardiovascular health care:<br />
our greatest challenge. J Am Coll Cardiol. 2008 Dec<br />
2;52(23):1817-25.<br />
9.Greenberg H, Raymond SU, Leeder SR.<br />
When we think about<br />
the global burden<br />
of disease and the<br />
plight of the poorest<br />
of the poor our minds often<br />
turn to the scourge of HIV/AIDS,<br />
malaria and tuberculosis - after<br />
all, that’s where all the attention<br />
is. Yet in the shadows lurks<br />
an uneasy truth: the rise of noncommunicable<br />
disease (NCD).<br />
Historically thought to be a disease<br />
of the “developed world”, NCD is in fact<br />
a worldwide pandemic of devastating<br />
proportions. In 2005 alone there were an<br />
estimated 35 million deaths from heart<br />
disease, stroke, cancer and other chronic<br />
diseases - approximately 50% (17.5 million)<br />
due to cardiovascular disease(1). Of<br />
these, 80% occurred in low- middle- income<br />
countries– (LMIC) twice as many<br />
deaths as from HIV, malaria and tuberculosis<br />
combined(1, 2). Cardiovascular<br />
disease (CVD), responsible for 30% of<br />
the total deaths worldwide(1)1, is the<br />
second leading cause of death in Africa,<br />
and the leading cause of death in those<br />
aged 30 or older(3). The fastest growing<br />
region for CVD is in the African region<br />
(27%) and it is estimated that over the<br />
next <strong>10</strong> years the burden from NCD will<br />
rise by 17% whilst those from communicable<br />
diseases will fall by 3% which<br />
translates to approximately 28 million<br />
deaths due to NCD over that period(1).<br />
The consequences of this are profound<br />
and far-reaching. Consider this:<br />
In contrast to our experience of NCD<br />
Cardiovascular disease and global health: threat and<br />
opportunity. Health Aff (Millwood). 2005 Jan-Jun;Suppl<br />
Web Exclusives:W-5-31-W-5-41.<br />
<strong>10</strong>.Gaziano TA. Reducing the growing burden of<br />
cardiovascular disease in the developing world. Health<br />
Aff (Millwood). 2007 Jan-Feb;26(1):13-24.<br />
11.Beaglehole R, Ebrahim S, Reddy S, Voute J,<br />
Leeder S. Prevention of chronic diseases: a call to action.<br />
Lancet. 2007 Dec 22;370(9605):2152-7.<br />
12.Lim SS, Gaziano TA, Gakidou E, Reddy KS,<br />
Farzadfar F, Lozano R, et al. Prevention of cardiovascular<br />
disease in high-risk individuals in low-income<br />
and middle-income countries: health effects and costs.<br />
Lancet. 2007 Dec 15;370(9604):2054-62.<br />
13.Gaziano TA, Galea G, Reddy KS. Scaling up interventions<br />
for chronic disease prevention: the evidence.<br />
Lancet. 2007 Dec 8;370(9603):1939-46.<br />
14.Beaglehole R, Epping-Jordan J, Patel V, Chopra<br />
M, Ebrahim S, Kidd M, et al. Improving the prevention<br />
and management of chronic disease in low-income and<br />
middle-income countries: a priority for primary health<br />
care. Lancet. 2008 Sep 13;372(9642):940-9.<br />
15.Asaria P, Chisholm D, Mathers C, Ezzati M,<br />
Beaglehole R. Chronic disease prevention: health<br />
effects and financial costs of strategies to reduce salt<br />
intake and control tobacco use. Lancet. 2007 Dec<br />
15;370(9604):2044-53.<br />
16.Gaziano TA, Opie LH, Weinstein MC. Cardiovascular<br />
disease prevention with a multidrug regimen in the<br />
developing world: a cost-effectiveness analysis. Lancet.<br />
2006 Aug 19;368(9536):679-86.<br />
being a disease of old age, in LMIC, it<br />
is often men and women in their most<br />
productive years (40‘s and 50‘s) who<br />
are most affected(4). On a personal level<br />
this is a tragedy for a family struggling<br />
for survival. At a societal level this<br />
lost productivity further compounds<br />
the challenges of economic growth.<br />
Inattention, rather than complexity<br />
contributes to the lack of action to date.<br />
A common set of known risk factors:<br />
hypertension, elevated lipids, smoking,<br />
obesity, sedentary lifestyles, and diabetes<br />
accounts for about 80% of clinical<br />
cardiovascular disease in every region of<br />
the world(5, 6). As developing countries,<br />
particularly those in sub-Saharan Africa<br />
move to the next stage of the epidemiological<br />
transition greater numbers<br />
of people are being exposed to diseaseproducing<br />
risk factors (2, 4, 7-11).<br />
The challenges are vast yet not<br />
insurmountable. We know from our<br />
experience that prevention works and<br />
there is a growing literature pointing<br />
to opportunities for scaling up low<br />
cost interventions. Tobacco control<br />
measures and dietary interventions can<br />
lead to small but significant changes in<br />
large groups of people(12-15). Health<br />
systems in LMIC traditionally oriented<br />
towards communicable disease<br />
will require re-orienting to address the<br />
chronic nature of NCD(1, 8, 12-14, 16).<br />
As we struggle towards goals such<br />
as “health for all” it would be nice to<br />
think that we can address the challenges<br />
of disease in a linear fashion - communicable<br />
then non-communicable.<br />
The inconvenient truth in all of this is<br />
that health, like life, is more complex<br />
than that. It is time that we lift the<br />
spotlight off to reveal the true picture of<br />
the global burden of disease and direct<br />
our efforts at addressing the health<br />
needs of communities as a whole. <br />
4 vector november <strong>2009</strong>
Heart disease and stroke<br />
threaten developing world<br />
Words Stephen R. Leeder and Angela Beaton<br />
Stephen Leeder is a Professor of<br />
Public Health and Community Medicine<br />
at the University of Sydney and Director<br />
of the Menzies Centre for Health Policy.<br />
He has a long history of involvement<br />
in public health research, educational<br />
development and policy. His research<br />
interests as a clinical epidemiologist<br />
have been mainly asthma and cardiovascular<br />
disease. His interest in public<br />
health was stimulated by spending 1968<br />
in the highlands of Papua New Guinea.<br />
Dr Angela Beaton is a Research Officer at<br />
the Menzies Centre for Health Policy.<br />
Heart attack and stroke,<br />
thought to be typically<br />
western diseases, are<br />
fast becoming major<br />
threats in developing countries.<br />
Four times as many deaths in<br />
mothers occur in most developing<br />
countries than do childbirth and<br />
HIV/AIDS: HIV/AIDS causes<br />
three million deaths a year; stroke<br />
and heart attack cause 17 million.<br />
Yet heart disease and stroke have<br />
attracted virtually no interest from<br />
international agencies committed<br />
to improving global health.<br />
It is time for that to change.<br />
Developing economies are seeing the<br />
kind of devastation to their workforces<br />
that Western countries experienced 50<br />
years ago. Troubling as these patterns<br />
are, they are but the first rumbles of the<br />
storm. The worldwide shift of working<br />
people from rural to city living has<br />
paralleled rising levels of prosperity and<br />
with it, greater consumption of food. A<br />
worldwide epidemic of obesity, even<br />
where under-nutrition persists in poorer<br />
quarters, presages high levels of diabetes,<br />
heart disease and stroke ahead.<br />
Fortunately, we can prevent and treat<br />
much heart disease and stroke. Treatment<br />
of raised blood pressure and blood<br />
lipids with drugs radically reduces risk<br />
and smokers who quit halve their risk<br />
of heart disease and stroke within two<br />
years. The World Health Organization<br />
has shown commendable leadership<br />
in relation to global tobacco control<br />
and now has its sights set on nutrition<br />
and exercise. Governments can assist<br />
by taxing tobacco and promoting good<br />
lifestyle habits, ensuring that all citizens<br />
have easy access to clinics, and plan<br />
healthier cities. Poor urban environments<br />
exacerbate physical and mental<br />
illnesses, now a major burden of global<br />
illness, at the expense of the economies<br />
of developing countries and our planet.<br />
To wait until heart disease and stroke<br />
decimate workforces before we take the<br />
global epidemic of heart disease and<br />
stroke seriously, would be both a health<br />
and economic tragedy. Heart disease and<br />
stroke are already propelling families<br />
into poverty in developing countries<br />
as young breadwinners and mothers<br />
die. Many developing countries have<br />
yet to create programs to control these<br />
diseases through long-term changes in<br />
macroeconomic policies, and by providing<br />
effective clinical care. Prevention<br />
programs must be locally sustainable<br />
for an indefinite future, and so developing<br />
countries should be encouraged to<br />
take the first step themselves, now.<br />
There is a responsibility for Australian<br />
medical students in advocating for<br />
action. Medical professionals have an<br />
important role in educating the public<br />
and lobbying governments to take up the<br />
challenge. Countries need the encouragement<br />
that stronger vocal advocacy for<br />
change can provide, to prod governments<br />
and donors into action, and international<br />
aid agencies should add to their agendas<br />
efforts to work with developing countries<br />
to contain these urgent and heavy threats<br />
to global health, national prosperity<br />
and family life in the developing world.<br />
Commitment from the highest levels of<br />
government in these countries is essential<br />
for comprehensive heart disease and<br />
stroke prevention. It will be important to<br />
graduate medical practitioners that have<br />
the capacity to deal with the consequences<br />
of an increased burden of chronic<br />
illness and an ageing population, and to<br />
assist communities to help themselves.<br />
november <strong>2009</strong> vector5<br />
www.ghn.amsa.org.au
tipping the scales<br />
the ‘expansion’ of the global community<br />
Words Rhea Pserickis, Medical student, University of Tasmania<br />
www.ghn.amsa.org.au<br />
I<br />
looked up from the desk and<br />
watched as my next patient<br />
walked in through the door.<br />
She was a middle-aged<br />
obese woman and beads of sweat<br />
had formed along her forehead<br />
in spite of the cooler weather. It<br />
took her a while to shuffle in, navigate<br />
the chair and find a comfortable<br />
sitting position. I noticed her<br />
heavy breathing. This patient was<br />
presenting with back and knee<br />
pain and had come in hoping for<br />
some analgesia. As I continued the<br />
consult, I pondered how to broach<br />
the fact that her weight was<br />
probably contributing to, if not<br />
directly causing, her pain. Just<br />
another obese patient with more<br />
chronic disease. Right? Well, not<br />
quite. The disparity is that this<br />
patient wasn’t in Australia nor<br />
was she a white Caucasian. I had<br />
in fact been working at a mobile<br />
clinic in remote Western Kenya,<br />
and this was a native Kenyan;<br />
more alarming, she was not the<br />
first or last obese Kenyan I came<br />
across during my time in Africa.<br />
Once considered a problem only<br />
in wealthy countries, the number of<br />
overweight and obese individuals has<br />
escalated in low and middle income<br />
countries. As risk factors for cardiovascular<br />
disease, type 2 diabetes, stroke<br />
and other chronic diseases, the rising<br />
prevalence of overweight and obesity in<br />
less developed countries is a hallmark of<br />
the now increasingly recognised ‘global<br />
society’ (1). Furthermore, the morbidity<br />
and mortality associated with these<br />
chronic diseases are significantly higher<br />
6 vector november <strong>2009</strong>
Right: Influences on the energy equation in<br />
developing countries (3). Below and facing<br />
page: One can appreciate the irony in all this<br />
when you see both the malnourished and<br />
obese side by side in a Gambian hospital (2).<br />
in less developed countries due to lack of<br />
education and understanding, as well as<br />
the age-old problem of resource insufficiency.<br />
In sub-Saharan Africa case-specific<br />
mortality rates for diabetes are more<br />
than <strong>10</strong> times higher than in the UK (2).<br />
The WHO indicates that globally,<br />
greater than 75 percent of women over<br />
the age of 30 are now overweight (1).<br />
Estimates are similar for men. In the<br />
Pacific islands of Nauru and Tonga nine<br />
out of every <strong>10</strong> adults are overweight<br />
(1). Obesity is even spreading rapidly<br />
through many an African countryside,<br />
along with its bevy of chronic disease<br />
burden which is both devastating and<br />
costly (2). Indeed, the existence of<br />
obesity and malnourishment within the<br />
one community presents an unintelligible<br />
paradox (see figure 1) (3).<br />
The increase in obesity in developing<br />
nations is due to ‘a global shift<br />
in diet towards increased energy, fat,<br />
salt and sugar intake, and a trend<br />
towards decreased physical activity<br />
due to the sedentary nature of<br />
modern work and transportation, and<br />
increasing urbanisation.’ (1) The developing<br />
world is now more than ever a<br />
target of many food companies and less<br />
developed countries present the largest<br />
growth markets for soft drink producers<br />
(4). Even where the Global Financial<br />
Crisis has tainted the US and European<br />
markets, consumption of soft drinks<br />
has increased in countries as diverse as<br />
Mexico, Egypt and China, encouraged<br />
by aggressive marketing campaigns,<br />
often aimed at children and youth (4).<br />
It is estimated that by 2015, 1.5<br />
billion individuals globally will be<br />
overweight (1). At this point, non-communicable<br />
diseases associated with the<br />
overweight and obese will surpass malnutrition<br />
as the leading cause of death in<br />
low-income communities (5). The contribution<br />
of chronic disease on the health<br />
status of the global community may paint<br />
a bleak picture, but it is our responsibility<br />
to take action to combat it. And where<br />
obesity is such a paradox to concurrent<br />
poverty, malnutrition, environmental<br />
instability and development, this responsibility<br />
becomes even more urgent. <br />
1.Anon. The World Health Organization warns of<br />
the rising threat of heart disease and stroke as overweight<br />
and obesity rapidly increase. (Media release).<br />
Geneva: September 22 2005. Article retrieved online<br />
on September 17 <strong>2009</strong> from, http://www.who.int/<br />
mediacentre/news/releases/2005/pr44/en/<br />
2.Prentice A and Webb F. Obesity admist poverty.<br />
Int J Epidemiology. 2006; 35:24-30<br />
3.Witkowski TH. Food Marketing and obesity<br />
in developing countries: analysis, ethics and public<br />
policy. J Macromarketing. 2007; 27(2):126-137<br />
4.Anon. Soft drinks and obesity: global threats<br />
to diet and health. (online article). Retrieved online<br />
on September 17 <strong>2009</strong> from, http://www.dumpsoda.<br />
org/health.pdf<br />
5.Tanumihardjo SA, Anderson C, Kaufer-Horwitz<br />
M, Bode L, Emenaker NJ, Haqq AM, Satia JA, Silver<br />
HJ and Stadler DD. Poverty, obesity and malnutrition:<br />
an international perspective recognising the paradox.<br />
J Amer Dietetic Assoc. 2007; <strong>10</strong>7(11):1966-1972<br />
november <strong>2009</strong> vector7<br />
www.ghn.amsa.org.au
Smoking and Tobacco’s Impact on the<br />
Developing World: The World’s Top Health Priority<br />
Words Cam Hollows, Medical student, University of Sydney<br />
“In the 20th century, the tobacco epidemic killed <strong>10</strong>0 million people worldwide…<br />
during the 21st century, it could kill One Billion.”<br />
“Reversing this entirely preventable epidemic must now rank as a top priority for<br />
public health and for political leaders in every country of the world.”<br />
Dr Margaret Chan, WHO Director-General (1)<br />
www.ghn.amsa.org.au<br />
// Image by Vivekchugh (sxc.hu)<br />
1. Organization WH. WHO Report on the Global<br />
Tobacco Epidemic, 2008: the MPOWER package.<br />
Geneva: World Health Organization2008 Contract No.:<br />
ISBN 9789241596282.<br />
2. The Global Fund to Fight AIDS TaM. The Global<br />
Fund to Fight AIDS, Tuberculosis and Malaria: Annual<br />
Report 2008. Vernier, Switzerland: The Global Fund to<br />
Fight AIDS, Tuberculosis and Malaria2008 2008 Contract<br />
No.: 92-9224-163-X (ISBN).<br />
3. UNAIDS. UNAIDS Report on the global AIDS<br />
epidemic: 2008. Geneva, Switzerland: UNAIDS2008<br />
August 2008 Contract No.: 978 92 9 173711 6.<br />
4. Organization WH. WHO Report <strong>2009</strong>: Global<br />
Tuberculosis Control Epidemiology,<br />
Strategy, Financing. Geneva, Switzerland: World<br />
Health Organization<strong>2009</strong> Contract No.: 978 92 4 156380<br />
2.<br />
5. Organization WH. WHO 2008 World Malaria<br />
Report. Geneva, Switzerland: World Health Organization2008<br />
Contract No.: 978 92 4 156369 7.<br />
6. Nations TU. The Millennium Development Goals<br />
Report 2208. New York, USA: United Nations2008<br />
August 2008 Contract No.: 978921<strong>10</strong>11739.<br />
7. Chapman S. Public Health Advocacy and<br />
Tobacco Control: Making Smoking History. Oxord:<br />
Blackwell Books; 2007.<br />
These statements are on<br />
the opening page of the<br />
World Health Organization<br />
Report on the<br />
Global Tobacco Epidemic, 2008.<br />
Tobacco use is recognized as<br />
harmful throughout the medical<br />
profession. The links of smoking<br />
with increased incidence of<br />
cardio-vascular disease, peripheral<br />
vascular disease, respiratory<br />
diseases, many cancers, as well as<br />
effects on reproductive health (to<br />
name but a few) have also been<br />
clearly established. Recently, new<br />
data have made clear just how<br />
harmful smoking is in a global<br />
epidemiological sense and the<br />
disproportionate impact it has on<br />
health in developing countries.<br />
Tobacco use currently kills around<br />
5.4 million people every year. To put<br />
this in perspective, in 2005 HIV/AIDS,<br />
TB & Malaria (the diseases targeted<br />
in Millennium Development Goal 6)<br />
killed approximately 4.2 million together<br />
(2-6). Whilst I am aware of the dangers<br />
of impetus splitting, and I would<br />
not for a second want to detract from<br />
the importance of programs combating<br />
these diseases (particularly having had<br />
falciparum malaria myself!), the huge<br />
impact of tobacco related disease cannot<br />
be ignored. It is estimated that smoking<br />
related deaths will rise to as much<br />
as 8 million every year by 2030. These<br />
mortality data are of course not the full<br />
picture and as medical students our own<br />
clinical experience should allow us to extrapolate<br />
the burden of associate morbidities.<br />
We should also pause for thought<br />
as to the resource demands imposed by<br />
smoking in already stretched systems.<br />
Whilst the individual circumstance<br />
is often tragic and coupled with physiological<br />
and psychological addiction,<br />
the reality is that diseases occurring<br />
due to tobacco use are entirely preventable.<br />
Tobacco is the only product on<br />
the planet which if used according to<br />
the manufacturer’s instructions kills<br />
half of the people who use it (7).<br />
The unfortunate reality for those<br />
of us working in global health is that<br />
over 80% of smoking related deaths<br />
are occurring in the developing world<br />
(1). But the burden goes further than<br />
the morbidity, mortality and economic<br />
impact. For the poor, money spent on<br />
tobacco means money not spent on<br />
basic necessities such as food, shelter,<br />
education and health care. In one study<br />
in Bangladesh low-income families<br />
were spending as much as ten times on<br />
tobacco as they were on their children’s<br />
education (1). Given our awareness of<br />
the importance of education in health<br />
and sustainable development, and the<br />
prevalence of extreme poverty, this sort<br />
of study should chill us to the very core.<br />
In Australia, tobacco control is a<br />
public health success story. That our<br />
rates of smoking are so low and rates of<br />
tobacco related disease are dropping is<br />
to be lauded (7). Most other countries<br />
in the world are much worse off than<br />
we are in terms of what they can spend<br />
on tobacco control. Whether we are<br />
interested in it or not, the problems of<br />
tobacco related illness cannot be ignored;<br />
the numbers and impacts are simply too<br />
large. So where and when we can, we<br />
must remember to add tobacco control to<br />
our list of priorities as we try to address<br />
the challenges of equitable and sustainable<br />
health in the developing world. <br />
8 vector november <strong>2009</strong>
Many of you<br />
may recognise<br />
the<br />
painting as<br />
Van Gogh’s Wheatfields<br />
with Crows. Each of you<br />
will be struck by some aspect<br />
of the painting and form your<br />
own impression of it. What if you<br />
were then told that this was Van<br />
Gogh’s last painting before his<br />
suicide? Given this key piece of<br />
information, do your perceptions<br />
then change? The flying birds<br />
perhaps, are crows, harbingers<br />
of death; the chaotic landscape a<br />
reflection of his inner turmoil. In<br />
reality, Wheatfields<br />
is not<br />
Van Gogh’s<br />
last painting.<br />
Does this fact<br />
once again<br />
completely alter<br />
the perceptions<br />
proceeding<br />
from the<br />
previous one?<br />
This was the<br />
eloquent example<br />
with which<br />
the Consul-<br />
General of India,<br />
Sydney, Mr<br />
Amit Dasgupta,<br />
commenced his<br />
talk to medical<br />
students at the University of Sydney. As<br />
part of the Global Health Stream, the<br />
Medical Faculty’s international health<br />
curriculum, we had the valuable opportunity<br />
of speaking with the Consul-General<br />
on Thursday 17 September about health<br />
issues in India. Prior to his appointment<br />
in Sydney, Mr Dasgupta has held various<br />
diplomatic positions across the world,<br />
from Cairo to Kathmandu. His wide<br />
experience is reflected in the numerous<br />
books he has edited and written in both<br />
fiction and non-fiction. Caught up as<br />
we are in the world of medical facts, the<br />
Consul-General’s talk was an important<br />
eye-opener into the more philosophical<br />
issues surrounding health policy.<br />
a conversation with the<br />
Indian Consul General<br />
Words Kruthika Narayan, Medical student, University of Sydney<br />
Van Gogh’s Wheatfields was a<br />
poignant illustration of how essential<br />
pieces of information shape the way<br />
we perceive a situation and how these<br />
perceptions may not always be correct.<br />
As the Consul-General emphasised, this<br />
is particularly important in addressing<br />
the various issues of international health.<br />
It highlights that a health model which<br />
works in one developing country situation,<br />
may not necessarily be transplanted<br />
with equal effectiveness to another. In<br />
India, as the Consul-General explained,<br />
the diversity in language, culture and<br />
customs within states, let alone between<br />
them, makes the implementation of<br />
health policy a complex issue, requiring<br />
a different approach in each region.<br />
The burgeoning of chronic disease<br />
in India highlights the importance of<br />
targeted health intervention programs.<br />
According to <strong>2009</strong> WHO statistics,<br />
the age–standardised mortality rate for<br />
cardiovascular disease is 382/<strong>10</strong>0 000<br />
and studies suggest that chronic diseases,<br />
particularly cardiovascular, are<br />
fast becoming the main cause of mortality<br />
in urban and rural populations. Not<br />
to mention diabetes, the prevalence<br />
of which was estimated to be greater<br />
than 31 million in 2005 and growing.<br />
The Consul-General spoke of some of<br />
the health interventions implemented by<br />
the Government to counter this increase<br />
in chronic illness. Recognising that a<br />
centralised approach to health policy<br />
would be less effective, one strategy<br />
has been to empower village councils or<br />
‘Panchayats’, funded by, but not accountable<br />
to, the Government. Composed<br />
of local villagers and an elected leader,<br />
these Panchayats have a better picture of<br />
the cultural and social characteristics of<br />
a region, and are in a position to know<br />
what policies would be most suitable.<br />
Another includes the health education<br />
programs, run by the Central<br />
Health Education Bureau, focusing on<br />
the education of women and children<br />
and taking into account the differences<br />
in beliefs between regions.<br />
These two strategies mentioned by<br />
Mr Dasgupta reiterate that approach<br />
is the key message. Health interventions<br />
need to be tailored and not run<br />
as an identical franchise from state<br />
to state, or as the Consul General put<br />
it, ‘McDonalised’. It comes back to<br />
how we interpret the picture of chronic<br />
disease in India, or in any country;<br />
ensuring the individual characteristics<br />
of that particular picture are what<br />
shape our perceptions and actions. <br />
november <strong>2009</strong> vector9<br />
www.ghn.amsa.org.au
www.ghn.amsa.org.au<br />
The Nageri Mission<br />
Words Jennifer Prince, MS Gen Surgery trainee, CMCH Vellore<br />
Having been in Christian<br />
Medical College<br />
(CMC), a tertiary<br />
hospital throughout<br />
my training, I entered with a<br />
sinking feeling into the Church of<br />
South India (CSI) hospital Nageri,<br />
located on the Andhra Pradesh-<br />
Tamilnadu border in South India.<br />
This was a part of a rural<br />
service obligation. In contrast to<br />
CMC's state-of-the art facilities,<br />
the Nageri hospital was a single<br />
storied building with a minimum<br />
of amenities.. The hospital was<br />
located <strong>10</strong>0km from Chennai, the<br />
capital city of the state of Tamilnadu<br />
and 70km from Tirupati, one<br />
of the large pilgrimage centres of<br />
the neighbouring state of Andhra<br />
Pradesh. It was a cultural potpourri<br />
of the two states yet, development<br />
came slowly to this region.<br />
The hospital itself was conceived<br />
by Dr Fanny Gibbens, a missionary<br />
doctor, and begun in the front yard of<br />
her house. She was in a land of strangers<br />
with just the will to serve the sick.<br />
I find it hard to imagine the depth of<br />
commitment that step would have asked<br />
of her. A new building sprung up as<br />
the workload increased and in a few<br />
years, the hospital reached the zenith of<br />
its development, with long queues of<br />
outpatients stretching into the night and<br />
inpatients awaiting their turn for admission<br />
on the floor between the cots.<br />
But with Dr Gibbens' death the<br />
hospital joined the ranks of Mission<br />
Hospitals started by committed individuals<br />
but struggling to remain open.<br />
The reasons were many- lack of doctors,<br />
paramedical staff, equipment and<br />
a committed leadership. And here<br />
I was, fresh from Internship, full of<br />
hopes, and plans and apprehension.<br />
There was a small medical staff<br />
at the hospital, including the Medical<br />
Superintendent, a Paediatrician, an<br />
auxiliary nurse midwife in charge of<br />
obstetrics and a senior from medical<br />
school. We catered to a patient profile<br />
that varied from those who could not<br />
afford a 5 day course of Amoxycillin for<br />
their children, to affluent businessmen<br />
presenting for follow up between their<br />
regular reviews in private city hospitals.<br />
As the days passed into months, the<br />
other doctors left Nageri and my senior<br />
and I were left to care for the hospital.<br />
As a primary evaluation centre,<br />
the spectrum of cases was wide, from<br />
respiratory infections and viruses to the<br />
common emergencies of traffic accidents<br />
and poisonings. Organophosphorous pesticides<br />
were readily available to the farming<br />
community of Nageri and were the<br />
poison of choice for suicidal attempts.<br />
As we did not have access to monitoring<br />
equipment like an ECG monitor or<br />
a pulse oximeter, or to a ventilator, the<br />
patients were given a gastric lavage and<br />
atropine. If there was any suggestion<br />
of respiratory compromise, the patient<br />
would be intubated and taken<br />
“<br />
by relatives<br />
to the nearest city. What<br />
can I say? It was far from<br />
the ideal in my head;<br />
some made it and some<br />
did not. But occasionally,<br />
we were rewarded<br />
in the form of a patient<br />
who returned for follow up after being<br />
on a ventilator for almost a fortnight.<br />
We did have a functional Operating<br />
Theatre. However, in the absence of<br />
an Anaesthetist, most of the surgeries<br />
we performed were those that could be<br />
done under spinal or local anaesthesia.<br />
On some days, the city hospitals<br />
would oblige us with the services of an<br />
Anaesthetist for more complex cases.<br />
As I mentioned earlier, we had a<br />
section of patients who were from an<br />
affluent background. They often presented<br />
with chronic illnesses such as<br />
Diabetes Mellitus, Hypertension and<br />
Obesity. In fact, infected trophic ulcers<br />
constituted one of the most common<br />
as well as dreaded complications of<br />
poorly controlled Diabetes Mellitus<br />
resulting in amputations and numerous<br />
visits for wound care. The patients were<br />
provided advice on lifestyle modification<br />
and were offered the services of<br />
the visiting Physician and an Ophthalmologist<br />
whenever possible.<br />
My favourite part was the weekly<br />
outreach clinic in a selected village<br />
around the hospital, aided by a Non-<br />
Government Organisation. There was<br />
a social worker who supervised four<br />
female workers, each of whom collected<br />
the Health Statistics from areas<br />
around the hospital. Regular Medical and<br />
Ophthalmology camps were a unique<br />
feature of this programme, as well as<br />
health education and preventive medicine.<br />
We worked towards understanding<br />
their beliefs and perceptions on health as<br />
well as addressing some superstitions.<br />
Notable examples of these included<br />
the avoidance of food or water during<br />
diarrhoea or that a febrile illness with<br />
rash was due to divine visitation. These<br />
clinics provided the ideal perspective<br />
of a patient's illness, allowing us to see<br />
firsthand his or her usual environment,<br />
lifestyle and beliefs. I will treasure the<br />
friendships that I have with many of the<br />
families through these interactions.<br />
What did I learn from my experience?<br />
That what mattered most was<br />
that you did the best you could with<br />
the situation rather than looking at the<br />
What can I say? It was far<br />
from the ideal in my head;<br />
some made it and some did not.<br />
”<br />
flaws. I learnt not to take resources for<br />
granted: indeed the hardest problems<br />
were the lack of resources and expertise.<br />
Gloves and sutures were hard to come<br />
by and are to be used carefully. In the<br />
absence of a senior doctor, I learnt to do<br />
what I could in a given situation, often<br />
performing surgical procedures with an<br />
open book for my guide. It did add to<br />
my self confidence and I learnt to rely<br />
on myself in the absence of supervision.<br />
It was also a lesson in administration.<br />
I hope to go back to Nageri after<br />
my General Surgery training. We have<br />
a new administrative team, operations<br />
are being scheduled on a regular basis<br />
and things are indeed looking up. The<br />
Nageri hospital was started with the<br />
vision of service to the ailing. What<br />
this requires is consistent work, vision<br />
and money. Sometimes I question<br />
if one person will be able to make a<br />
difference. But the reality is that there<br />
is often only one person and he/she is<br />
the one who makes the difference. <br />
<strong>10</strong> vector november <strong>2009</strong>
Mental Health Crisis<br />
in China<br />
Words Ron Cheung<br />
Medical student<br />
University of Sydney<br />
// Image by Ringoc2 (sxc.hu)<br />
Mental health is<br />
a substantially<br />
underestimated<br />
problem in China.<br />
In a four province study, 63 000<br />
people were screened in random<br />
urban and rural sites. A trained<br />
psychiatric nurse screened-out<br />
those at high risk of mental illness,<br />
or those with a pre-existing<br />
diagnosis of a severe mental<br />
illness. Those at moderate to low<br />
risk were administered a Chinese<br />
version of the Structured<br />
Clinical Interview for (DSM)-IV<br />
axis I disorders by a psychiatrist.<br />
Importantly, clinicians who<br />
spoke the local dialect and were<br />
familiar with local expressions<br />
and culture were selected, so<br />
they could adapt questions in<br />
order for patients to understand.<br />
Seventeen percent (17%) of the<br />
population had a form of mental illness<br />
(this is 173 million people!). Eleven<br />
percent (11%) of men had issues with<br />
alcohol abuse: an increasing problem<br />
that has thus far not received attention.<br />
Of those with mental illness, 25% were<br />
so severely disabled by it that they<br />
were unable to work. Among all those<br />
with mental illness, only 5% have ever<br />
seen any mental health professional.<br />
Unfortunately, China’s health care<br />
system is plagued by systematic issues.<br />
There are no mental health services in<br />
rural areas. There is a stigma towards<br />
mental illness and even though people<br />
realize they have it, they refuse to seek<br />
treatment. There is a lack of knowledge<br />
- 60% of people interviewed had never<br />
heard of the word depression, even<br />
though they had full blown symptoms.<br />
In China, GP’s do not offer mental<br />
health services, only large psychiatric<br />
wards in large hospitals do<br />
so. It is not seen as part of a GP’s<br />
duties to address mental health.<br />
Closing the gap in mental illness<br />
and services in China is challenging.<br />
The culture of medicine will need to<br />
be changed: barriers will need to be<br />
overcome, medical school curriculums<br />
redeveloped, effective reimbursement<br />
patterns in hospitals introduced, and<br />
the makeup of the health care workforce<br />
that includes a consideration<br />
of the mental health agenda. <br />
november <strong>2009</strong> vector11<br />
www.ghn.amsa.org.au
I<br />
was fortunate enough to spend a month of my Christmas<br />
holidays in Papua New Guinea (PNG). The people of PNG have<br />
the lowest health status in the Pacific region. Despite this, life<br />
in PNG is full and the people embrace it with all their might.<br />
I was welcomed with huge smiles and all around kindness. I was<br />
often invited back into people’s homes to meet their families and<br />
be shown their village life.<br />
MEDICINE<br />
and<br />
MOSQUITOES<br />
a medical student’s<br />
month in papua new<br />
guinea<br />
www.ghn.amsa.org.au<br />
One particular day in the town of<br />
Goroka, I was invited to a Christmas<br />
party by the surgical team. For Christmas<br />
the staff often prepare a ‘mumu’, a<br />
traditional way of cooking in PNG where<br />
a whole pig or goat is killed, wrapped in<br />
banana leaves and cooked in the ground<br />
with hot rocks. For this Christmas party<br />
they had decided that they would prepare<br />
a pig for the mumu. So they brought the<br />
pig to the hospital, where it waited on the<br />
first floor balcony until they could kill it<br />
and prepare the mumu. The pig, however,<br />
had other ideas and was last seen<br />
running frantically around the hospital<br />
grounds followed closely by the entire<br />
theatre staff, leaving an empty theatre<br />
and a rather bewildered looking surgeon.<br />
I was later informed that pigs are highly<br />
valued in PNG and are a symbol of<br />
wealth and social standing. In fact they<br />
12 vector november <strong>2009</strong><br />
are so important that women will often<br />
breastfeed the piglets when they are born.<br />
Now after they had caught the pig<br />
and it was prepared for the mumu I sat<br />
down with the theatre staff and surgical<br />
team to enjoy the feast. However, this<br />
was not for long as the surgical resident<br />
and myself were called to emergency to<br />
assess a patient. Having been in PNG for<br />
over 3 weeks I was not easily shocked<br />
by anything I saw, but this still did shock<br />
me! On entering the ED I was directed<br />
to a young man sitting on the edge of a<br />
bed with three arrows protruding from<br />
his body. He had been shot four times<br />
in total; the first arrow was in the ninth<br />
intercostal space on the left, the second<br />
entered the superficial tissue on his right<br />
flank, the third was embedded in his<br />
groin and the fourth he had removed<br />
himself from his right triceps. Despite<br />
Words and Photos<br />
Georgia Ritchie<br />
Medical student<br />
University of Sydney<br />
the wounds, he sat perfectly still and<br />
appeared not to be in any pain. Despite<br />
much effort the radiographer at the hospital<br />
could not be contacted that evening<br />
so the young man had to wait until morning<br />
for his X-rays and surgery to remove<br />
the arrows. This meant he had to sleep<br />
on his front with three arrows protruding<br />
form his body! When he eventually went<br />
to surgery, it was found that the arrow<br />
entering the chest had passed through the<br />
spleen, the duodenum and the transverse<br />
colon. After 7 hours of surgery, the arrow<br />
was removed, the spleen saved and the<br />
puncture wounds to the bowls closed and<br />
he was sent to the ward for recovery.<br />
I have a story about each day I<br />
spent in PNG. Whether it is about the<br />
amazing people I met or the interesting<br />
medical cases I saw, I was constantly<br />
in awe of the country. Although<br />
at times a hard place to comprehend,<br />
I feel that I understood by the end<br />
of my trip and fell in love with the<br />
PNG, its culture and the people.
Stories from<br />
Cambodia<br />
Behind these smiles are stories of great<br />
sadness and tragedy<br />
Words and Photos Nilru Vitharana<br />
Medical student, University of Sydney<br />
During my summer<br />
holidays last year, I<br />
spent a few weeks<br />
volunteering at an<br />
orphanage and medical clinic in<br />
rural Cambodia in a town called<br />
Neak Leung on the banks of the<br />
Mekong River. Cambodia has<br />
some of the worst health statistics<br />
in the world – 1 in 7 children<br />
will die before the age of 5.<br />
The charity I visited was called<br />
Damnok Toek, which means ‘a drop<br />
of water’ in Khmer. Ironic, given<br />
that the area is surrounded by flooded<br />
rice paddy fields, and the houses<br />
are built up on stilts to avoid the<br />
floodwaters during rainy season.<br />
Damnok Toek houses 60 orphans,<br />
provides schooling for a further 150<br />
children and has a social work program<br />
and medical clinic. As you can see<br />
from the photos, the children here are<br />
all smiles, but behind these smiles are<br />
stories of great sadness and tragedy.<br />
Some of the children in the permanent<br />
centre had been sold into child<br />
prostitution and child labour in Thailand’s<br />
notorious Pattaya district before<br />
they were rescued, some are AIDS<br />
orphans, some are mentally or physically<br />
handicapped and thus abandoned<br />
by their families who cannot afford<br />
to take care of them, and others were<br />
the victims of domestic violence.<br />
The medical clinic here provides a<br />
vital service for the rural poor. The government<br />
healthcare system is expensive<br />
($20 US for a consultation) and underresourced.<br />
The poor,<br />
many of whom earn<br />
less than $1 a day,<br />
simply cannot afford<br />
it. In contrast, the<br />
medical clinic costs<br />
12 cents (including<br />
medication). People<br />
would travel several<br />
hours to receive affordable<br />
medical care.<br />
I also spent much<br />
of my time doing<br />
social work in the<br />
community. One day we went to followup<br />
a child who hadn’t been turning up<br />
to school, which surprised us because he<br />
loved going to school and hadn’t missed<br />
a day. When we arrived at his home we<br />
discovered that his older brother had died<br />
of AIDS, and now he had to stay at home<br />
to take care of his younger brother. Stories<br />
like his are a prime example of the<br />
“cycle of poverty” – now he is likely to<br />
miss out on the opportunity of education.<br />
Living with a local family, I was<br />
able to immerse myself in the language<br />
and culture of the Khmer<br />
people. Having fallen in love with the<br />
people of Cambodia, I will be returning<br />
this year to Damnok Toek. <br />
november <strong>2009</strong> vector13<br />
www.ghn.amsa.org.au
global health<br />
in the news<br />
Copenhagen Climate Change<br />
Summit will be held in December<br />
<strong>2009</strong>. For the health impacts<br />
of climate change, refer<br />
to the editorial published by the<br />
Lancet and BMJ and University<br />
College London in September<br />
<strong>2009</strong>.<br />
http://en.cop15.dk<br />
World Diabetes Day<br />
14th November <strong>2009</strong><br />
WHO estimates that more than 180 million people worldwide have diabetes,<br />
according to 2005 figures. This number is likely to more than double by<br />
2030 without intervention. Almost 80% of diabetes deaths occur in low and<br />
middle-income countries.<br />
www.worlddiabetesday.org<br />
HIV vaccine?<br />
A trial of a vaccine to prevent infection<br />
by HIV involving 16,000 participants<br />
in Thailand this year has shown modest<br />
results with 26% reduction in rates of<br />
infection compared to placebo controls.<br />
Refer to the October 20th <strong>2009</strong> issue of<br />
the New England Journal of Medicine.<br />
PNG’s Liquid Nitrogen Gas<br />
(LNG) Project will officially open<br />
in 20<strong>10</strong>, is expected to double the<br />
country’s GDP, and will have a profound<br />
impact on trade and health<br />
in the Pacific region. Refer to a<br />
series by Jo Chandler of The Age<br />
published September this year.<br />
www.ghn.amsa.org.au<br />
Indonesia’s official death toll stands<br />
at 650, with a 672 people missing, following<br />
the devastation of the recent<br />
earthquake. Damage to roads, disruption<br />
to electrical power and sources of clean<br />
water could make the situation much<br />
worse in the coming weeks.<br />
There is similar concern in Samoa<br />
about the spread of infectious diseases,<br />
such as causes of acute watery diarrhoea,<br />
typhoid fever and dengue fever<br />
following the Tsunami.<br />
2nd November <strong>2009</strong> commemorates renewed efforts to promote pneumonia<br />
on the global health agenda by 2011. Wear blue jeans on the 2nd of November<br />
(signifying the 2 million deaths of children every year due to pneumonia) and support<br />
this cause.<br />
www.worldpneumoniaday.org<br />
14 vector november <strong>2009</strong>
global health network<br />
update<br />
Welcome to the GHN<br />
A Year in the GHN:<br />
Looking back and<br />
looking forwards<br />
Trung Nghia Ton<br />
WakeUp! GHN Officer, University of Newcastle<br />
AMSA GHN Chair <strong>2009</strong> - 20<strong>10</strong><br />
Tamara Vu<br />
AMSA GHN Chair<br />
2008-09<br />
A very warm<br />
welcome to you all on<br />
behalf of the AMSA<br />
Global Health Network<br />
Committee! This issue<br />
of <strong>Vector</strong> marks the start of yet another<br />
Global Health Calendar year (kicked off by<br />
a truly rousing Global Health Conference in<br />
Brisbane).<br />
We look forward to adding to the<br />
monumental efforts of the GHN Committee<br />
of 08/09 who have worked tirelessly to bring<br />
together students from all over the country<br />
to collaborate in common interests in global<br />
health awareness and action. This culminated<br />
in the very first GHN National project, the<br />
Red Party concept, which raised national<br />
funds and awareness for HIV/AIDS, and was<br />
a huge success. This is a tangible example of<br />
how our efforts at a local level can be part<br />
of a global impact. Additionally, The GHN<br />
began its first national advocacy movements,<br />
further highlighting the GHN’s increasing<br />
ability to inform, represent and advocate for<br />
medical students in matters of global health.<br />
I would like to extend heartfelt congratulations<br />
and thanks to the outgoing<br />
GHN Committee for their successes this last<br />
12 months. It is without a doubt that their<br />
efforts have made a real and tangible difference,<br />
and has set up a national framework<br />
for us to continue to grow and mature as an<br />
organisation. Their efforts continue to reflect<br />
on the new committee as they mentor us<br />
through a very steep learning curve.<br />
With much enthusiasm, the newly<br />
elected GHN committee for 09/<strong>10</strong> are getting<br />
right onto the task. Realising this year’s GHN<br />
National project, the South East Asian Libraries<br />
Project, will be a challenging undertaking<br />
but with the experience and motivation of<br />
each global health group (GHG) we hope to<br />
exploit the growing momentum and make<br />
a longstanding impact by helping our fellow<br />
medicos in the developing world (watch this<br />
space!). We also hope to strengthen our<br />
collective voices and to bring truly pressing<br />
global health advocacy issues to the fore in<br />
our chosen active advocacy campaigns, especially<br />
in regards to the crucial Millennium<br />
Development Goals, and the treatment of<br />
refugees and asylum seekers.<br />
The GHN remains an avenue for medical<br />
students to bring ideas, issues and action to<br />
a national level, but it is vitally important for<br />
us all to look at developing our own Global<br />
Health Groups (GHG) and individual initiatives<br />
– there are so many opportunities available<br />
to bring grass roots ideas and projects to<br />
fruition and collaborate on a local, regional<br />
and national level.<br />
I invite you all to become active members<br />
of your local GHG as they grow into dynamic<br />
student organisations. It is incredibly exciting<br />
to see the initiatives of GHGs around the<br />
country in 09/<strong>10</strong> and I look forward to working<br />
with an exceptional and motivated GHN<br />
Committee and witness medical students<br />
making a real difference in our global community.<br />
As the outgoing<br />
Chair of the Global<br />
Health Network (GHN),<br />
I am delighted to<br />
report on our successful<br />
year of global health group development<br />
and support; our wildly successful National<br />
Project, the Red Party, which raised over<br />
$88 022 for HIV/AIDS support and research;<br />
and our advocacy working party, which<br />
developed the Millennium Development<br />
Goals policy that in February became<br />
AMSA’s first-ever global health-based policy<br />
document.<br />
It’s been a great year for medical<br />
students in global health, with new and<br />
exciting work happening in global health<br />
groups, in the GHN, at GHC09, and at AMSA<br />
level. It has been my privilege to serve as<br />
GHN Chair during the last twelve months.<br />
Along with the other outgoing GHN Representatives<br />
and officers, I am delighted to be<br />
handing over the reigns to a new committee,<br />
as I know Trung and his team will be<br />
dedicated and enthusiastic in promoting<br />
and supporting global health activities<br />
around Australia. And, looking back on the<br />
various global health events of the past<br />
year, I look forward to seeing what the next<br />
twelve months will bring.<br />
november <strong>2009</strong> vector15<br />
www.ghn.amsa.org.au
The Global Health Conference:<br />
Challenging the world after Brisbane<br />
Meg Scott Deputy Convenor GHC <strong>2009</strong><br />
www.ghn.amsa.org.au<br />
As I think back over the 4 days of the<br />
Global Health Conference <strong>2009</strong> (GHC),<br />
certain events and lessons I learned remind<br />
me to do more with my life and challenge my<br />
world!<br />
Our biggest achievement, the event we<br />
put the most blood, sweat and tears into<br />
was challenge day. The <strong>10</strong> station, half-day<br />
workshop challenged the delegates to work<br />
through various situations one might come<br />
up against in an overseas medical aid situation.<br />
Delegates planned a refugee camp and<br />
were marked on the appropriateness of their<br />
toilet selection, as well as deciding how many<br />
farms they would have. Groups got to try<br />
talking their way into a prisoner of war camp<br />
past cheeky guards, and the guards were<br />
also marked on their ability to stick to their<br />
guns. The triage station allowed the clinical<br />
years delegates to shine, using their ability<br />
to interpret vital signs to save many a paper<br />
doll life. We made nutritional food packs, delivered<br />
babies (and placentas) in emergency<br />
situations, learned about the difficulties in<br />
communicating with non-English speaking<br />
patients, allocated sparse resources to those<br />
who needed it the most, and perhaps most<br />
importantly, enjoyed the Brisbane sunshine!<br />
The inspiring opening plenary from Dr.<br />
Sujit taught me a couple of things. One, if<br />
you want to add prestige to a product, print<br />
the label in English; if the people can’t read<br />
it, they’ll want it more. Two, having nothing<br />
is no excuse; start where you are and<br />
the financial support will come. There is no<br />
reason why one person can’t start making<br />
a difference in the community. Personally,<br />
I was amazed at how easy Dr. Sujit made it<br />
all sound! Starting at a farm, negotiating the<br />
use of a barn for a clinic, to shortly thereafter<br />
running numerous hospitals and schools! He<br />
definitely challenged my idea that one needs<br />
money to make a difference.<br />
Tania Major continued the unintended<br />
theme to get out there and start doing, with<br />
her challenging Australians’ attitudes towards<br />
the Indigenous population. She spoke of her<br />
work increasing awareness of Indigenous<br />
issues, which she has been doing for the<br />
majority of her life. She reminded us that<br />
whether Indigenous or non-Indigenous, we<br />
are all Australian, and we must look after<br />
our own. We all know of the 17 year age<br />
gap between the two populations, and the<br />
barriers towards proper healthcare for those<br />
in remote communities are not new. Tania<br />
showed us that grassroots action is vital in<br />
making a change. As Tania so eloquently<br />
stated, “just fucking do it!”<br />
Carolyn Hardy showed us what has been<br />
done so far in combating HIV/AIDS, and we<br />
are sadly nowhere near meeting the Millennium<br />
Development Goal. Again we were<br />
shown how to challenge the problems in<br />
bringing healthcare to those who need it,<br />
and how to overcome these obstacles. Carolyn<br />
spoke of the potential for conducting HIV<br />
tests remotely via mobile phone and picture<br />
texts! With unbelievable solutions like this<br />
in the works, I was reminded to look outside<br />
the box for solutions to decade-old problems.<br />
Dr. Nick Coatsworth gave me wanderlust<br />
recounting his missions with MSF to such<br />
places as Darfur and the Sudan. He also<br />
spoke of getting in there and working at a<br />
grassroots level and somehow managed to<br />
make immunising hundreds of children a day<br />
for 4 weeks straight sound exciting! He’s definitely<br />
an inspiration for all medical students,<br />
showing us that it is possible to have a life,<br />
train in a specialty and work overseas all at<br />
once.<br />
Gabi Hollows, on behalf of the Fred<br />
Hollows Foundation (FHF), taught us that<br />
enthusiasm is enough; that having passion<br />
for a cause will make things happen. She<br />
also reminded us of the need for medical<br />
aid in Australia. Sure, while the FHF now<br />
have clinics and factories all over the world,<br />
Fred Hollows’ work started in rural/remote<br />
Australia, and Gabi reminded us we cannot<br />
overlook our own country. Also, what struck<br />
me from the Fred Hollows story was that one<br />
persons’ passion and hard work can continue<br />
indefinitely.<br />
After all that energy spent learning<br />
and inspiring, I wouldn’t have<br />
thought anyone had enough energy<br />
for a party, but boy, was I wrong!<br />
Perhaps the memory burned into my<br />
mind the most was the monkey dancing<br />
with the genie, or was it seeing 2<br />
sumo wrestlers trying to get onto a<br />
bus? Check out the pictures on our<br />
website to decide for yourself…<br />
Thank you everyone for coming<br />
to Brisbane, for participating so fully<br />
in the program (both day and night!),<br />
and for challenging yourself and your<br />
peers to do more and be more. I look<br />
forward to seeing you in Hobart for<br />
GHC 20<strong>10</strong> and hearing about how you<br />
have challenged your world this year.<br />
Left: The GHC is a ‘hands-on’ event.<br />
Far left and above left: Dr Sujit inspires<br />
the audience to make a difference. Images:<br />
www.amsa.org.au/ghc09<br />
16 vector november <strong>2009</strong>
Student Involvement<br />
Helping VSAP to help others<br />
What is VSAP?<br />
The Victorian Students’ Aid Program<br />
(VSAP) is a student initiative run by medical<br />
students at the University of Melbourne,<br />
which delivers much needed equipment and<br />
health resources to disadvantaged communities<br />
globally.<br />
Our vision is that all doctors worldwide<br />
will have essential medical supplies and<br />
equipment to treat their patients.<br />
Recently, VSAP has elected to broaden its<br />
scope and fulfil the role of being the University<br />
of Melbourne’s global health group. This<br />
financial year we will be taking on additional<br />
projects as well as expanding into the areas<br />
of education and advocacy.<br />
Check out our website for more information<br />
on: our Teddy Bear Hospital community<br />
project, our Global Health Short Course being<br />
held in collaboration with the Nossal Institute<br />
for Global Health, and our Red Party fundraising<br />
event that raises money for HIV/AIDS<br />
research and awareness. One of our main,<br />
ongoing projects is the Wishlist Project.<br />
What is the Wishlist Project?<br />
The Wishlist Project aims to contribute<br />
to global health equity by sending<br />
targeted aid to hospitals in<br />
poorly resourced areas via medical<br />
students completing their elective<br />
placements there.<br />
To ensure that we are supplying<br />
appropriate and effective<br />
equipment, the hospitals are asked<br />
to compile a ‘wishlist’ of the supplies<br />
and equipment that they require.<br />
VSAP works with hospitals and medical<br />
suppliers in Australia to fulfil these wishlists<br />
and these donations are delivered with the<br />
medical student when they leave for their<br />
elective placement.<br />
Since its inception in 2005, VSAP has<br />
delivered over $30000 worth of equipment<br />
and monetary donations to countries as<br />
diverse as Guatemala, Tanzania, East Timor<br />
and Vietnam.<br />
How can you be involved?<br />
Student involvement – Helping VSAP to help<br />
others<br />
We are always looking for travelling<br />
students who can deliver donated supplies to<br />
areas where health care professionals are in<br />
need of medical supplies. We are also looking<br />
for students to get involved in our various<br />
projects. Please contact us by email.<br />
Equipment and financial contributions for<br />
Wishlists<br />
VSAP relies on the generosity of sponsors<br />
to obtain equipment to send to underresourced<br />
communities. In the past, health<br />
institutions have been the main contributors<br />
of equipment particularly when they reorganise,<br />
close down, have excess supplies,<br />
or upgrade.<br />
VSAP is also responsible for the logistics<br />
of delivering donated supplies to destination<br />
hospitals. Assistance with airfreight,<br />
packaging, and transport would also be very<br />
welcome.<br />
We are always looking for sponsors of<br />
medical equipment and supplies. If you<br />
would like to donate, please contact us by<br />
email.<br />
Contact us<br />
General enquiries:<br />
vsap.aid@gmail.com<br />
Sponsorship enquiries:<br />
vsap.sponsorship@gmail.com<br />
For more information, visit http://www.<br />
vsap.org.au<br />
Right: Sanka Amadoru delivering<br />
supplies to Kibosho Hospital, Tanzania.<br />
Far right: Alexandra Bryson<br />
using a donated anaesthetic machine,<br />
Papua New Guinea<br />
Global Health Lecture Series - The University of Sydney<br />
Nilru Vitharana, Acting Chair, USyd GlobalHOME [Global Health Group]<br />
After attending the Global Health Conference, students from<br />
globalHOME (Sydney University’s global health group) were inspired<br />
to educate their fellow students about global health by developing<br />
a lecture series to improve the global health awareness and skills of<br />
medical students.<br />
The 8-part lecture series will be delivered by leading experts<br />
in the field, from doctors, public health personnel, and NGOs. The<br />
topics to be covered include: aid and poverty, healthcare in conflict<br />
settings, emergency response to natural disasters, tropical infectious<br />
diseases, climate change and its impact on health, malnutrition and<br />
indigenous health. This series will equip students with the necessary<br />
clinical and public health skills to understand global health issues<br />
that they may encounter whilst on elective or in their future careers.<br />
The lecture series will feature case studies, scenarios, interactive<br />
discussion and is designed to appeal to students from across all<br />
years of the medical program. The lectures will be held on Tuesday<br />
evenings in March and May. Students from other universities are<br />
most welcome to attend. Please sign up to our Yahoo Group (http://<br />
groups.yahoo.com/group/globalhome/) to join our mailing list and<br />
keep up to date with details of our lecture series.<br />
november <strong>2009</strong> vector17<br />
www.ghn.amsa.org.au
creative<br />
pieces<br />
www.ghn.amsa.org.au<br />
“It was in the news. He<br />
jumped off the bridge last<br />
qweek. He died.” My old<br />
school friend told me in<br />
tears on the phone. The sunlight<br />
is so bright. I sit, feeling a little<br />
nauseous. In that country, it is<br />
the coldest time of the year. Did<br />
he drown or freeze to death?<br />
“Does anyone know why he killed<br />
himself?” We used to go to the same<br />
primary school. We were in the same<br />
class although he was 3 years older<br />
than the rest of the class. Kids used to<br />
laugh at him, because his legs looked<br />
funny. He had poliomyelitis. He would<br />
never catch anyone after being teased. It<br />
would only cause more laughs. And he<br />
walked in the most awkward way, too.<br />
“They said he was a psycho, he went<br />
to see a shrink a few times.” The last<br />
time I heard about him was last year.<br />
He published an article on a famous<br />
magazine, named “A sad river”. I can<br />
just remember the words he used in<br />
that book. That unbearable sense of<br />
sorrow floods my heart even now.<br />
“Was he depressed?” He never really<br />
spoke to anyone. I supposed we were<br />
all immature and didn’t want to hang<br />
out with a kid who couldn’t play with<br />
us. He dropped out of school after high<br />
school. It was simply too far away. His<br />
parents couldn’t afford anything after<br />
paying for his expensive medications.<br />
“Depression. Emm… Maybe. But it<br />
is not a problem for poor people. People<br />
have enough trouble paying for food,<br />
it’s not at the top of their agenda.” It is<br />
true. Who would pay money to see a<br />
psychologist when that same money was<br />
enough for a month’s worth of food.<br />
He didn’t have a job as far as<br />
I know. So many people who had<br />
good legs were still unemployed.<br />
The boy who<br />
jumped off<br />
the bridge<br />
Words Mengying Su<br />
Medical student, University of Tasmania<br />
“Couldn’t he apply for government<br />
support?”<br />
“The government? Are you kidding?<br />
I don’t think it is rich enough<br />
to look after everyone here. The<br />
hospital wouldn’t treat anyone who<br />
can’t pay the bill up front.”<br />
// Image by OmirOnia (sxc.hu)<br />
Outside the window, children walk<br />
across the street after school. They<br />
are young, healthy and happy. Just<br />
like how we were like. I feel sorry<br />
for that boy. I wonder if it would be<br />
any different if we were young today<br />
or if he lived somewhere else. <br />
18 vector november <strong>2009</strong>
This morning, with<br />
thanks to the Australian<br />
Cricket Team, morale<br />
seems particularly high<br />
in Michael's Care Home, New<br />
Delhi. The staff<br />
and clients of the<br />
AIDS hospice<br />
and mini hospital,<br />
squash up on the<br />
old cast iron beds<br />
of the main ward<br />
and watch Australia<br />
(32 for 3)<br />
squirm live on TV.<br />
Between overs,<br />
one of the care workers disentangles<br />
himself from the jubilant add break<br />
highlights recap, and bounds up to<br />
me with a piece of paper in his hand.<br />
The paper, though of creamy, freshly<br />
minted quality, is already softening<br />
along the fold, a sign of being<br />
read and re-read many times over.<br />
We stand next to the bed of Noor, the<br />
patient who I came today to visit, and<br />
share the contents of the page. On this<br />
day of victory, its contents make me cry.<br />
Before that though, let<br />
me tell you about Noor.<br />
Noor is about 45. Tall. Muscled.<br />
My earliest memory of Noor is<br />
in the kitchen of 'Sahara', the heroin<br />
rehabilitation centre to which Michael's<br />
Care Home is attached. Long<br />
hair in a ponytail, white singlet with<br />
sweat crescents under the arms. Hoisting<br />
kilo upon kilo of rice or hovering<br />
above the perpetual dhal pot, bini (local<br />
cigarette) smoke trailing from his lips<br />
as he tossed in onions. A tomato.<br />
He ran a slick kitchen. Vital, sunnywindowed<br />
place. The sort of kitchen<br />
you feel drawn to. I remember leaning<br />
against the bench top, sipping water<br />
and listening to Phantom of The Opera<br />
on his radio in one ear and instalments<br />
from his 15 year saga with the<br />
Afghani Embassy in the other. Noor<br />
was an Albanian refugee, somehow<br />
made it through Afghanistan to India<br />
where he wound up in heroin rehab.<br />
Despite the smallness of the Sahara<br />
kitchen, Noor never shooed me away.<br />
He churned out three meals a day for<br />
all present at mealtime, the aroma of<br />
his cooking as reliable as the sun.<br />
Brown and ambiguous, we made<br />
jokes about 'The Noor Curry' then.<br />
The details of how Noor went from<br />
staff member at the men's rehab centre<br />
to patient at Michael's Care Home are<br />
foggy. It happened around Christmas<br />
time. Alcohol was involved. A fall. Brain<br />
haemorrhage. Emergency surgery.<br />
NOOR<br />
Words Cara Munro<br />
Now a piece of his skull is missing<br />
and a thick line of cable stitching<br />
closes the place where his brain was<br />
exposed. His long black hair is shorn<br />
and the jagged greying crop makes<br />
him look vulnerable as a lamb. Occasionally<br />
his eyes respond to words.<br />
The care workers have been trying<br />
to help him walk. At night he sits<br />
up and mutters a little in his first language.<br />
The rest of the time his hands<br />
are bandaged to the bed sides and he<br />
sleeps. They tell me he needs further<br />
surgery, but for now, rest and healing.<br />
Michael's Care Home first came into<br />
being in 1998 to care for those marginalised<br />
by addiction and ostracised<br />
from society by HIV. Public hospitals<br />
in Delhi, were too scared to touch them.<br />
So were their families. So, rather than<br />
let people die on the path outside the<br />
emergency departments (as was happening)<br />
Michael's Care Home was born.<br />
There still aren't many family<br />
visitors to Michael's Care Home.<br />
Blood relatives don't cook special<br />
convalescent cuisine or send cards.<br />
But a care force has been<br />
formed to look after Noor.<br />
Sporting tattoos and track marks<br />
and the signature Sahara combed hair<br />
and worn but washed clothes, they take<br />
turns at occupying the uncomfortable<br />
plastic chair at Noor's bedside, by day<br />
and night, anticipating his every need.<br />
His meals are prepared by an exclient<br />
of the rehab centre (now the<br />
hospice cook) and spoon fed to him by<br />
a team of young men (all ex-injecting<br />
drug users) who, having completed some<br />
or all of their own rehabilitation, have<br />
volunteered to be with Noor in his.<br />
Noor, with no family to speak<br />
of in India, has someone with<br />
him 24 hours a day.<br />
One of the volunteers, a handsome<br />
and talented soccer player (also, along<br />
with his brother, a refugee from Iran and<br />
witness to his own father's execution) sits<br />
with his patient by<br />
night. He speaks in<br />
Persian to Noor and<br />
translates what little<br />
anyone can offer in<br />
encouragement.<br />
Another, onetime<br />
street child,<br />
shaves Noor with<br />
gentleness that cuts<br />
directly to the heart.<br />
And still another,<br />
stands beside me<br />
this morning, bashfully holding a clean<br />
piece of paper on which his recently<br />
written letter of reference is printed.<br />
We read together slowly.<br />
'Mr. Satish, 27 years old has been<br />
working with us as a care worker from<br />
2003–present. He is diligent, committed<br />
and his performance is satisfactory in<br />
every way ... We wish him every success<br />
in future undertakings ...' It is signed<br />
by Sahara 's Director of Medicine.<br />
His hard yards in heroin rehab and<br />
then as a volunteer care worker are<br />
coming to an end and he has applied<br />
for a job in a hospital outside Michael's<br />
Care Home. He plans to continue to<br />
live at Sahara and help out where he<br />
can around the hospice, caring for<br />
people such as Noor, but build a life<br />
and a career in the world outside also.<br />
In mixed Hindi and English.<br />
'I just like to care for people.'<br />
I feel the heat of tears rising. Satish<br />
has never had a letter of reference before.<br />
His job interview is at <strong>10</strong>am tomorrow<br />
morning. No doubt he'll be<br />
sighted in a borrowed shirt and freshly<br />
pressed pants, reference in hand.<br />
The Cricket score is Australia 155<br />
for 5. A roar erupts throughout Michael's<br />
Care Home. Noor is sleeping. <br />
'The world is full of suffering, it is<br />
also full of overcoming it.' –Hellen Keller<br />
Cara is a registered Division 1 nurse<br />
who undertook the PHC Jamkhed Course<br />
with the University of Melbourne in<br />
2005. She has since lived and worked in<br />
India in the area of HIV / Aids, heroin rehabilitation<br />
and Public Health and in the<br />
process of writing about many of these<br />
experiences.<br />
november <strong>2009</strong> vector19<br />
www.ghn.amsa.org.au
at a glance<br />
india<br />
// Image by asifthebes (sxc.hu)<br />
India has had significant economic growth in the<br />
past decade from which the general health of the<br />
population has benefitted in many ways. The following<br />
summarises many of the facts regarding health in the<br />
world’s second most populous nation.<br />
Indicator<br />
Date Preceding<br />
Most Recent<br />
Date<br />
Target by 2015<br />
Proportion of population below 37% (1990) 26% (2000) 18.5%<br />
poverty line<br />
Proportion of population undernourished<br />
62% (1990) 53% (2000) 31%<br />
as whole<br />
Proportion of children undernourished<br />
54% (1990) 47% (1998) 27%<br />
Under five mortality rate (per 125 (1990) 98 (2000) 41<br />
<strong>10</strong>00 births)<br />
Maternal Mortality Rate (per 437 (1991) 407 (1998) <strong>10</strong>7<br />
<strong>10</strong>0 000 births)<br />
Deaths due to AIDS 471 (2000) 1114 (2004) Arrest the spread of HIV.<br />
The estimated adult prevalence<br />
of AIDS in 2007 was<br />
0.3%<br />
Deaths due to TB (per <strong>10</strong>0 000) 56 (1999) 33 (2003) Reverse the number of<br />
deaths due to TB<br />
Deaths due to Malaria (per <strong>10</strong>0<br />
000)<br />
Healthcare investment (proportion<br />
of GDP)<br />
0.13 (1994) 0.09 (2004) Reverse the number of<br />
deaths due to malaria<br />
Approximately<br />
3% (1990)<br />
Approximately 5%<br />
(2000)<br />
Increased economic growth<br />
is expected to reflect a<br />
greater investment in<br />
health care<br />
Healthcare Staff<br />
As of 2004, India had:<br />
• 503 900 doctors<br />
• 737 000 nurses<br />
• 350 000 chemists<br />
• 15 000 hospitals<br />
India has a three tiered healthcare<br />
system with 23 000 Primary Healthcare<br />
Centres (urban), 137 000 subcentres<br />
(semi-urban and rural) and<br />
3000 community health care centres.<br />
// Image by barunpatro (sxc.hu)<br />
www.ghn.amsa.org.au<br />
Adapted From:<br />
Government of<br />
India. (2005). Millennium<br />
Development Goals India<br />
Country Report 2005. New<br />
Delhi: India.<br />
Indian Council of<br />
Medical Research. (2005).<br />
Assessment of Burden of<br />
Non-Communicable Diseases.<br />
Ansari Nagar: India.<br />
<strong>Issue</strong><br />
Ischaemic<br />
Heart Disease<br />
Urban<br />
Weighted<br />
average prevalence<br />
/<strong>10</strong>00<br />
(+20y.o.)<br />
Rural<br />
Weighted average<br />
prevalence<br />
/<strong>10</strong>00<br />
(+20y.o.)<br />
Total Number of<br />
entire population<br />
affected<br />
64.37 25.27 18 600 984 (1998)<br />
22 367 840 (2004)<br />
Stroke 1.54 792 628 (1998)<br />
930 985 (2004)<br />
Consequences<br />
Expected to be single greatest cause<br />
of mortality in India by 2015.<br />
Total number of DALYS attributable<br />
to stroke approximately 6.37 million<br />
in 2004<br />
Diabetes 118.02 38.67 37 768 402 (2004) Rates of diabetes incidence are<br />
expected to increase significantly<br />
within the next two decades<br />
Hypertension 164.20 157.44 Total contribution of hypertension in<br />
combination with other risk factors,<br />
as it occurs, would prove worse<br />
outcomes than shown here.<br />
20 vector november <strong>2009</strong>