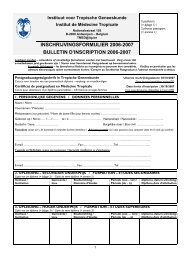
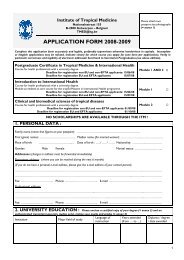
Department of - Instituut voor Tropische Geneeskunde
Department of - Instituut voor Tropische Geneeskunde
Department of - Instituut voor Tropische Geneeskunde
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Unit <strong>of</strong> Molecular Parasitology<br />
In the course <strong>of</strong> 2007, the Unit <strong>of</strong> Molecular Parasitology<br />
Unit has made considerable progress in its two main,<br />
closely related research lines on leishmaniasis, i.e.<br />
treatment failure and drug resistance, and parasite<br />
genotyping.<br />
Our studies on drug resistance were highlighted in the<br />
PhD thesis <strong>of</strong> Saskia Decuypere “Antimony treatment<br />
failure in anthroponotic visceral leishmaniasis: towards<br />
improved tools and strategies for epidemiological<br />
surveillance and disease control”, which provides<br />
a synthesis <strong>of</strong> five years work on drug resistance<br />
leishmaniasis. Saskia joined the University <strong>of</strong> Strathclyde<br />
(Pr<strong>of</strong>. G. Coombs) with a Marie-Curie scholarship, where<br />
she will pursue the biochemical characterisation <strong>of</strong> drugresistant<br />
strains for two years before continuing her<br />
postdoctoral work at the ITM. By the end <strong>of</strong> 2007, Meriem<br />
Ouakad joined the unit for postdoctoral studies on drug<br />
resistance.<br />
Our research on parasite genotyping consists <strong>of</strong> three<br />
main activities and PhD projects:<br />
• dissemination, standardisation and quality control <strong>of</strong><br />
existing typing methods<br />
• new and simple methods for species identification<br />
• the application <strong>of</strong> molecular methods to specific<br />
epidemiological questions<br />
The composition <strong>of</strong> our team, with PhD and postdoctoral<br />
fellows from Cuba, Peru, Algeria, Kenya and Nepal<br />
illustrate the success <strong>of</strong> our intercontinental networking.<br />
Among the major findings <strong>of</strong> 2007, we quote the first<br />
extensive description <strong>of</strong> the L. donovani population<br />
structure among healthy carriers in Nepal.<br />
The Euro-Mediterranean consortium “Leishmed”,<br />
which we coordinated, concluded its activities with<br />
two workshops on immunological and environmental<br />
control <strong>of</strong> leishmaniasis, both in Tunisia. A main<br />
deliverable <strong>of</strong> this project was the digital compendium<br />
on geo-referenced publications on the epidemiology<br />
<strong>of</strong> leishmaniasis in the Mediterranean, developed<br />
in close collaboration with the Leishmed partners<br />
and WHO. Another networking milestone was the<br />
“Leishrisk” conference in November 2007 in Antwerp<br />
(see highlights) which brought together 150 world class<br />
leishmaniacs.<br />
The unit pursued its contribution simplified molecular<br />
diagnosis <strong>of</strong> Leishmania and genotyping <strong>of</strong> Plasmodium<br />
by the other units in the <strong>Department</strong>.<br />
Unit <strong>of</strong> Parasite Diagnostics<br />
The Unit <strong>of</strong> Parasite Diagnostics conducts research<br />
on parasitological, serological, bioclinical and genetic<br />
markers for the diagnosis, stage determination and<br />
follow-up <strong>of</strong> trypanosomiasis (African and South-<br />
American) and leishmaniaisis. We collaborate with<br />
partners in DR Congo, Uganda, Kenya, Sudan, Malawi,<br />
Ethiopia, South Africa, Mozambique, Zambia, Burkina<br />
Faso, Venezuela, Chile and Spain, and are a partner in<br />
WHO and FIND-Diagnostics consortia aiming to develop<br />
new diagnostics for sleeping sickness.<br />
The results <strong>of</strong> the first randomised clinical trial on<br />
combination therapy for sleeping sickness were<br />
published. This pioneer study was conducted in<br />
Bwamanda (DR Congo), in collaboration with national<br />
partners and the Drugs for Neglected Diseases Initiative<br />
(DNDi). It allowed the identification <strong>of</strong> biological markers<br />
in cerebrospinal fluid (CSF) as risk factors for relapse<br />
and provided a rationale for shortening post-treatment<br />
follow-up. These results should be confirmed in a new<br />
study conducted in Mbuji-Mayi (DR Congo), where rates<br />
<strong>of</strong> treatment failure are uncommonly high. The first in<br />
vitro drug sensitivity tests on parasite strains isolated<br />
from such patients seem to reject the hypothesis that the<br />
high relapse rates are caused by parasite drug resistance.<br />
The unit is partner in the NEUROTRYP consortium, which<br />
intends to unravel the mechanisms by which African<br />
trypanosomes invade the brain. We have constructed<br />
recombinant Trypanosoma brucei strains that express<br />
Renilla luciferase enabling in vivo tracking <strong>of</strong> the parasites<br />
in mice (see highlight). Within the same project, an<br />
RESEARCH | 51