Ileal Conduit and Continent Ileocecal Pouch for Patients Undergoing ...
Ileal Conduit and Continent Ileocecal Pouch for Patients Undergoing ...
Ileal Conduit and Continent Ileocecal Pouch for Patients Undergoing ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
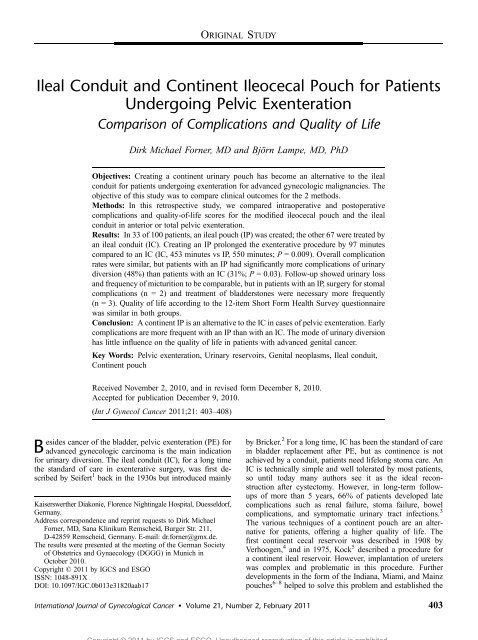
<strong>Ileal</strong> <strong>Conduit</strong> <strong>and</strong> <strong>Continent</strong> <strong>Ileocecal</strong> <strong>Pouch</strong> <strong>for</strong> <strong>Patients</strong><br />
<strong>Undergoing</strong> Pelvic Exenteration<br />
Comparison of Complications <strong>and</strong> Quality of Life<br />
Dirk Michael Forner, MD <strong>and</strong> Björn Lampe, MD, PhD<br />
Objectives: Creating a continent urinary pouch has become an alternative to the ileal<br />
conduit <strong>for</strong> patients undergoing exenteration <strong>for</strong> advanced gynecologic malignancies. The<br />
objective of this study was to compare clinical outcomes <strong>for</strong> the 2 methods.<br />
Methods: In this retrospective study, we compared intraoperative <strong>and</strong> postoperative<br />
complications <strong>and</strong> quality-of-life scores <strong>for</strong> the modified ileocecal pouch <strong>and</strong> the ileal<br />
conduit in anterior or total pelvic exenteration.<br />
Results: In 33 of 100 patients, an ileal pouch (IP) was created; the other 67 were treated by<br />
an ileal conduit (IC). Creating an IP prolonged the exenterative procedure by 97 minutes<br />
compared to an IC (IC, 453 minutes vs IP, 550 minutes; P = 0.009). Overall complication<br />
rates were similar, but patients with an IP had significantly more complications of urinary<br />
diversion (48%) than patients with an IC (31%; P = 0.03). Follow-up showed urinary loss<br />
<strong>and</strong> frequency of micturition to be comparable, but in patients with an IP, surgery <strong>for</strong> stomal<br />
complications (n = 2) <strong>and</strong> treatment of bladderstones were necessary more frequently<br />
(n = 3). Quality of life according to the 12-item Short Form Health Survey questionnaire<br />
was similar in both groups.<br />
Conclusion: A continent IP is an alternative to the IC in cases of pelvic exenteration. Early<br />
complications are more frequent with an IP than with an IC. The mode of urinary diversion<br />
has little influence on the quality of life in patients with advanced genital cancer.<br />
Key Words: Pelvic exenteration, Urinary reservoirs, Genital neoplasms, <strong>Ileal</strong> conduit,<br />
<strong>Continent</strong> pouch<br />
Received November 2, 2010, <strong>and</strong> in revised <strong>for</strong>m December 8, 2010.<br />
Accepted <strong>for</strong> publication December 9, 2010.<br />
(Int J Gynecol Cancer 2011;21: 403Y408)<br />
esides cancer of the bladder, pelvic exenteration (PE) <strong>for</strong><br />
B advanced gynecologic carcinoma is the main indication<br />
<strong>for</strong> urinary diversion. The ileal conduit (IC), <strong>for</strong> a long time<br />
the st<strong>and</strong>ard of care in exenterative surgery, was first described<br />
by Seifert 1 back in the 1930s but introduced mainly<br />
Kaiserswerther Diakonie, Florence Nightingale Hospital, Duesseldorf,<br />
Germany.<br />
Address correspondence <strong>and</strong> reprint requests to Dirk Michael<br />
Forner, MD, Sana Klinikum Remscheid, Burger Str. 211,<br />
D-42859 Remscheid, Germany. E-mail: dr.<strong>for</strong>ner@gmx.de.<br />
The results were presented at the meeting of the German Society<br />
of Obstetrics <strong>and</strong> Gynaecology (DGGG) in Munich in<br />
October 2010.<br />
Copyright * 2011 by IGCS <strong>and</strong> ESGO<br />
ISSN: 1048-891X<br />
DOI: 10.1097/IGC.0b013e31820aab17<br />
ORIGINAL STUDY<br />
by Bricker. 2 For a long time, IC has been the st<strong>and</strong>ard of care<br />
in bladder replacement after PE, but as continence is not<br />
achieved by a conduit, patients need lifelong stoma care. An<br />
IC is technically simple <strong>and</strong> well tolerated by most patients,<br />
so until today many authors see it as the ideal reconstruction<br />
after cystectomy. However, in long-term followups<br />
of more than 5 years, 66% of patients developed late<br />
complications such as renal failure, stoma failure, bowel<br />
complications, <strong>and</strong> symptomatic urinary tract infections. 3<br />
The various techniques of a continent pouch are an alternative<br />
<strong>for</strong> patients, offering a higher quality of life. The<br />
first continent cecal reservoir was described in 1908 by<br />
Verhoogen, 4 <strong>and</strong> in 1975, Kock 5 described a procedure <strong>for</strong><br />
a continent ileal reservoir. However, implantation of ureters<br />
was complex <strong>and</strong> problematic in this procedure. Further<br />
developments in the <strong>for</strong>m of the Indiana, Miami, <strong>and</strong> Mainz<br />
pouches 6Y8 helped to solve this problem <strong>and</strong> established the<br />
International Journal of Gynecological Cancer & Volume 21, Number 2, February 2011 403<br />
Copyright © 2011 by IGCS <strong>and</strong> ESGO. Unauthorized reproduction of this article is prohibited.
Forner <strong>and</strong> Lampe International Journal of Gynecological Cancer & Volume 21, Number 2, February 2011<br />
continent bladder replacement in the 1990s. Both the Miami<br />
<strong>and</strong> Mainz pouches use the ileocecal segment, creating a<br />
reservoir by detubulizing it <strong>and</strong> diverting the urine via an<br />
ileal segment or the appendix. Since then, several other<br />
techniques using various ileal or colonic segments have been<br />
developed, but still the ileal conduit is more widely used in<br />
cancer surgery than its continent alternatives.<br />
Farnham 9 did not find any significant differences in<br />
the frequency of surgical complications <strong>for</strong> the various<br />
methods of urinary diversion. He concluded that as long as<br />
there are no contraindications against one method or the<br />
other, the appropriate procedure should be chosen individually<br />
according to the underlying disease, quality of life,<br />
<strong>and</strong> patient’s personal preference.<br />
In this study, we compared intraoperative <strong>and</strong> postoperative<br />
complications <strong>and</strong> quality-of-life scores of the modified<br />
ileocecal pouch <strong>and</strong> the ileal conduit as described by<br />
Wallace 10 in anterior or total PEs.<br />
MATERIALS AND METHODS<br />
<strong>Patients</strong> who had undergone exenterative surgery in our<br />
department between July 2000 <strong>and</strong> June 2010 were identified,<br />
their records were reviewed, <strong>and</strong> data were analyzed retrospectively.<br />
Compilation <strong>and</strong> analysis of data were done by the<br />
statistics program BiAS <strong>for</strong> Windows (Software, Version 9.2,<br />
University of Frankfurt/ Main, Germany) using the Mann-<br />
Whitney test <strong>for</strong> data without normal distribution <strong>and</strong> the<br />
Fisher-Yates exact test with mid-P methods. The confidence<br />
level was P = 0.05.<br />
To evaluate the quality of life, the patients were<br />
asked to fill in the Short Form-12 Health Survey Questionnaire<br />
(SF-12). 11 The SF-12 questionnaire uses 12 items to<br />
describe a summary scale <strong>for</strong> quality of life. In addition, a<br />
mental <strong>and</strong> physical summary scale is reported. The regression<br />
weightings used <strong>for</strong> scoring the SF-12 come from a<br />
general population. 11<br />
Technique of Creating the <strong>Ileocecal</strong> <strong>Pouch</strong><br />
<strong>Continent</strong> ileocecal pouches were created using the<br />
modified technique according to Hünlich <strong>and</strong> Egger. 12 An<br />
ileocecal segment consisting of approximately 20 cm of<br />
ileum <strong>and</strong> 15 cm of cecum was dissected <strong>and</strong> isolated.<br />
Continuity was reestablished by side-to-side anastomosis.<br />
The ileal <strong>and</strong> cecal parts of the isolated segment were then<br />
joined side by side down to the Bauhins valve by a linear titan<br />
stapler, thus detubulizing the segment by cutting the circular<br />
musculature. The resulting pouch was approximately the<br />
size of a fist. To be able to use the appendix as a neourethra,<br />
its tip was cut off <strong>and</strong> widened with Hegars dilators to 5-mm<br />
diameter. A urinary catheter (Charrière 14) was placed in the<br />
neourethra. The appendix-urethra was then lead out through<br />
the navel, <strong>and</strong> its mucosa was fixed to the skin. Both ureters<br />
were implanted antirefluxively in the cecal wall <strong>and</strong> stented<br />
<strong>for</strong> 14 days.<br />
In all patients, a drain was placed in the pouch of<br />
Douglas. Serum electrolytes including chloride <strong>and</strong> phosphate<br />
were checked regularly during the hospital stay. All<br />
patients were trained by a specialized stoma nurse in the care<br />
of their ileal conduit or in self-catheterization of their ileal<br />
pouch, respectively.<br />
RESULTS<br />
A total of 100 patients were identified who had undergone<br />
anterior or total exenterative procedures with bladder<br />
reconstruction between July 2000 <strong>and</strong> June 2010. The median<br />
age of the patients was 56 years (range, 35Y81 years), postoperative<br />
hospital stay was <strong>for</strong> a median of 34 days (range,<br />
10Y147 days). On average, 4 units of packed red blood<br />
cells (0Y20 units) <strong>and</strong> 2 units (0Y6 units) of fresh frozen<br />
plasma were required. Median operating time was 490 minutes<br />
(range, 237Y724 minutes). None of the patients died<br />
intraoperatively or within the first 100 days after surgery.<br />
Total exenteration was per<strong>for</strong>med in 59 patients, <strong>and</strong><br />
anterior exenteration was per<strong>for</strong>med in 35 patients. Six<br />
patients with advanced ovarian cancer had a complete exenteration<br />
according to Bristow III. 13 For 41 of 49 patients with<br />
supralevatoric total exenteration, a deep rectal anastomosis<br />
was created simultaneously, including a protective colostomy<br />
in 25 cases.<br />
Fifty-four patients had cervical cancer, 11 had endometrial<br />
cancer, 20 had vulval cancer, <strong>and</strong> 6 had vaginal<br />
cancer. Six patients presented with an advanced ovarian<br />
malignancy, <strong>and</strong> 3 patients presented with other malignancies<br />
in the pelvis. Fifty-four patients had a relapse, whereas<br />
35 patients had undergone previous radiotherapy.<br />
In 33 patients, an ileal pouch (IP) was created; the<br />
other 67 patients were treated with an ileal conduit (IC), the<br />
latter group being slightly older (IP, 52 years vs IC, 63 years;<br />
P = 0.02). Creating an IP prolonged the procedure by<br />
97 minutes compared to creating an IC (IC, 453 minutes vs<br />
IP, 550 minutes; P = 0.009). In anterior exenteration, the<br />
difference was 59 minutes (P = 0.01); in total PE, the difference<br />
was 108 minutes. However, in total PE, rectal anastomoses,<br />
which add to prolonging the procedure, were<br />
significantly more frequent (IC, 20/37 [55%]; IP: 21/22<br />
[95%]; P G 0.001). The 2 groups did not differ in the length of<br />
postoperative intensive care or in the need <strong>for</strong> units of packed<br />
red blood cells or fresh frozen plasma (Table 1).<br />
Postoperative recovery was free of complications <strong>for</strong> 31<br />
patients with IC (46%) <strong>and</strong> <strong>for</strong> 9 patients with IP (27%). In 22<br />
patients with IC (33%) <strong>and</strong> in 12 patients with IP (36%),<br />
minor complications occurred, which were treated conservatively.<br />
Surgical treatment of complications was necessary<br />
in 14 patients with IC (21%) <strong>and</strong> 12 patients with IP (36%,<br />
not significant; Table 2).<br />
Overall, complications of urinary diversion were significantly<br />
more frequent in patients with IC (21 patients<br />
[31%]) than in patients with IP (16 patients [48%]; P = 0.03).<br />
The frequency of the different types of complications was<br />
similar in both groups <strong>and</strong> did not change over the years<br />
(Table 3). Complications of urinary diversion requiring surgical<br />
treatment occurred in 7 patients with IC (10%). Those<br />
consisted of 4 leaks of the ureteroileal anastomosis, one<br />
necrosis of the ureter <strong>and</strong> 2 leaks of the intestinal anastomosis.<br />
In the early stage, no complication of the stoma<br />
was seen. One patient with IC had an acute anterenal failure<br />
requiring transient hemodialysis. No other patient of either<br />
404 * 2011 IGCS <strong>and</strong> ESGO<br />
Copyright © 2011 by IGCS <strong>and</strong> ESGO. Unauthorized reproduction of this article is prohibited.
International Journal of Gynecological Cancer & Volume 21, Number 2, February 2011 <strong>Ileal</strong> <strong>Conduit</strong> <strong>and</strong> <strong>Ileocecal</strong> <strong>Pouch</strong><br />
TABLE 1. Characteristics of patients with <strong>Ileal</strong> conduit or ileocecal pouch <strong>and</strong> significant differences according to<br />
Mann-Whitney or Fisher-Yates exact test<br />
<strong>Ileal</strong> <strong>Conduit</strong> <strong>Ileocecal</strong> <strong>Pouch</strong><br />
Median Range Median Range P*<br />
Age, yrs 63 35Y81 52 35Y74 0.02<br />
Duration of procedure, min 453 237Y724 550 308Y653 0.009<br />
Days in hospital 32 10Y147 38 16Y117 0.02<br />
Days on intensive care 3 1Y40 4 1Y13 0.32<br />
Packed red blood cells, 500 cc 4 0Y20 4.5 4Y10 1.00<br />
Fresh frozen plasma, 500 cc 2 0Y6 2 0Y60.96 Quality-of-life score 56 38Y92 81 38Y92 0.10<br />
n=67 % n=33 % P†<br />
Preceding radiotherapy 24 35.8 11 33.3 0.82<br />
Recurrence 39 58.2 14 42.4 0.17<br />
Total Exenteration 37 55.2 22 66.7 0.24<br />
Rectal anastomosis 20 55 21 95 0.001<br />
Rectal anastomosis was more frequently needed in patients with ileal pouch.<br />
*Mann-Whitney test.<br />
†Fisher-Yates exact test.<br />
group showed a rise in creatinine, <strong>and</strong> there was no case of<br />
hypochloremic acidosis. Six patients with IP (18%) needed<br />
surgical intervention owing to complications of urinary<br />
diversion: In 4 patients, there was a leak at the pouch or at<br />
the implantation of the ureter; 2 patients had complications<br />
of the appendix stoma, requiring trans<strong>for</strong>mation into a wet<br />
stoma. There were no leaks at the ileo-ascendostomies. Of<br />
the 31 patients with IP without resurgery <strong>for</strong> stoma complications,<br />
29 (94%) were continent <strong>and</strong> able to empty their<br />
IP by self-catheterization at discharge from hospital.<br />
Overall, 35 patients had prior irradiation, 24 of which<br />
were treated with an IC <strong>and</strong> 11 with an IP. In the IC group, of<br />
TABLE 2. Morbidity <strong>and</strong> mortality according to the classification of postexenterative complications<br />
Category No. <strong>Patients</strong> Complications No. <strong>Patients</strong> Affected*<br />
Without complications 40<br />
Minor complications<br />
without surgical intervention<br />
Major complication requiring<br />
surgical intervention<br />
*Several complications possible in same patient.<br />
34 Urinary tract infection 10<br />
Urinary tract obstruction 7<br />
Seroma/Lymphocele 8<br />
Fever 938 h 6<br />
Failure of wound healing 5<br />
Nerve lesion 2<br />
Pleural effusion requiring drainage 1<br />
Thrombosis 1<br />
Ileus 1<br />
Retracted colostomy 1<br />
26 Leak of intestinal anastomosis 8<br />
Leak of ureteric anastomosis 9<br />
Intraperitoneal abscess 2<br />
Complete wound dehiscence 2<br />
Bleeding after disseminated intravascular coagulation 2<br />
Colostomic tear-out 1<br />
* 2011 IGCS <strong>and</strong> ESGO 405<br />
Copyright © 2011 by IGCS <strong>and</strong> ESGO. Unauthorized reproduction of this article is prohibited.
Forner <strong>and</strong> Lampe International Journal of Gynecological Cancer & Volume 21, Number 2, February 2011<br />
TABLE 3. Urinary diversionYrelated early complications of <strong>Ileal</strong> conduit <strong>and</strong> <strong>Ileocecal</strong> pouch show no significant<br />
differences in Fisher-Yates exact test<br />
<strong>Ileal</strong> <strong>Conduit</strong> <strong>Ileocecal</strong> <strong>Pouch</strong><br />
n = 67 % n = 33 % P*<br />
Renal failure 1 1.4 0 0 0.67<br />
Urinary tract infection 9 13.4 5 15.1 0.51<br />
Urinary tract obstruction 3 4.4 4 12.1 0.16<br />
Leak of ureter anastomosis 4 6.0 4 12.1 0.24<br />
Ureter necrosis 1 1.4 0 0 0.67<br />
Stomal complication 0 0 2 6.1 0.11<br />
Leak of ileal anastomosis 2 3.0 0 0 0.44<br />
Several complications are possible in same patient.<br />
*Fisher-Yates exact test.<br />
the 5 patients that had a leakage, one had had prior irradiation.<br />
In the IP group, 2 of 4 patients with a leakage had prior<br />
irradiation. A correlated cause could not be determined. The<br />
incidence of complications was neither correlated to negative<br />
or positive margins nor to lymph node status.<br />
Regarding complications other than urinary diversion,<br />
3 patients in each group needed revision surgery <strong>for</strong> failure of<br />
wound healing or complete wound dehiscence. Leaks of the<br />
colonic anastomosis occurred in 5 patients with IC <strong>and</strong> 3<br />
patients with IP (nonsignificant). No patient had an ileus.<br />
Postoperative hospital stay was longer <strong>for</strong> patients with IP<br />
than <strong>for</strong> patients with IC (38 vs 32 days, P = 0.02).<br />
Of 100 patients, 97 were followed up <strong>for</strong> a median of<br />
37 months. Thirty-seven patients are still alive (34 of them<br />
free of disease). Twenty-two of these patients have an IC, <strong>and</strong><br />
15 have an IP. Two patients with IC (9%) <strong>and</strong> one patient with<br />
IP (7%) experience an involuntary loss of urine. Seventy-five<br />
percent <strong>and</strong> 78% of the patients, respectively, need to empty<br />
their stomal bag or IP no more than twice per night, the others<br />
more frequently. In both groups, 2 patients needed resurgery<br />
<strong>for</strong> stomal complications. Bladder stones were only seen in 3<br />
patients with IP. <strong>Patients</strong> with IP needed treatment <strong>for</strong> urinary<br />
tract infection (33%) significantly more frequently than<br />
patients with IC (4%, P = 0.02). Quality of life was tested<br />
with the SF-12 questionnaire, <strong>and</strong> results were not statistically<br />
different between the groups (Table 4). Both groups had<br />
the same frequency of colonic anastomoses <strong>and</strong> colostomies,<br />
hence not biasing the quality-of-life score results.<br />
DISCUSSION<br />
In this study, we present the ileocecal pouch as modified<br />
by Hünlich <strong>and</strong> Egger 12 <strong>and</strong> compare its intraoperative<br />
<strong>and</strong> early postoperative data with the ileal conduit in the<br />
setting of an exenteration. The IP requires a considerably<br />
higher surgical ef<strong>for</strong>t, with an anterior exenteration taking an<br />
average of 97 minutes longer. Also, the overall rate of complications<br />
related to urinary diversion is higher <strong>for</strong> the IP (IC,<br />
21/67 [31%] vs IP, 16/33 [48%]; P = 0.10). The rate of<br />
complications requiring surgical intervention, however, is not<br />
significantly different (10% vs 18%).<br />
Similar rates were reported <strong>for</strong> other types of urinary<br />
diversion. Of 396 patients with a Mainz I pouch <strong>and</strong> appendix-stoma,<br />
93 patients (23.5%) needed surgical intervention<br />
<strong>for</strong> complications of the stoma. 14 Twelve of 77 patients<br />
(15.8%) supplied with a Miami pouch needed another intervention,<br />
4 of them <strong>for</strong> stoma complications (5.1%). 15 Two of<br />
our patients (6%) with IP needed intervention <strong>for</strong> stoma<br />
complications; in another 2 patients (6%), problems of<br />
catheterization could be treated conservatively.<br />
In another study on the Mainz pouch, the frequency of<br />
stomal failure was 11%, <strong>and</strong> the frequency of stomal stenosis<br />
TABLE 4. Quality of life as measured by SF-12 questionnaire <strong>for</strong> patients treated by ileal conduit <strong>and</strong> ileocecal<br />
pouch shows no significant difference between the 2 groups<br />
<strong>Ileal</strong> <strong>Conduit</strong> <strong>Ileocecal</strong> <strong>Pouch</strong><br />
Mean SD Mean SD P*<br />
Quality-of-life score 60 22.0 71 14.6 0.18<br />
Physical component summary score 48 10.5 43 11.0 0.38<br />
Mental component summary score<br />
*Mann-Whitney test.<br />
49 10.8 45 13.7 0.46<br />
406 * 2011 IGCS <strong>and</strong> ESGO<br />
Copyright © 2011 by IGCS <strong>and</strong> ESGO. Unauthorized reproduction of this article is prohibited.
International Journal of Gynecological Cancer & Volume 21, Number 2, February 2011 <strong>Ileal</strong> <strong>Conduit</strong> <strong>and</strong> <strong>Ileocecal</strong> <strong>Pouch</strong><br />
13%. 16 Stomal complications occurred in 22.1% of the<br />
patients with the Miami pouch 15 <strong>and</strong> in 14.7% of patients<br />
with Rome pouches. 17<br />
We did not find a significant difference in the leakage<br />
rate between IC <strong>and</strong> IP: In 4 patients with IP (12%) <strong>and</strong><br />
4 patients with IC (6%), repeat intervention was required <strong>for</strong><br />
leaks of the pouch or of the implantation site of the ureter.<br />
Goldberg, 18 too, did not find any significant difference in the<br />
rate of ureteric anastomosal leak between IC <strong>and</strong> a continent<br />
pouch (14% vs 13%). For the Miami pouch, Mirhashemi 19<br />
found these complications in 6.5% of patients (5/77),<br />
Penalver 20 reports a rate of 12.1% (8/66). Chang 21 describes<br />
fistulae of the Miami pouch in 4 of 21 patients (19.0%). With<br />
1 in 40 patients (2.5%), Ramirez 22 saw a lower rate of<br />
leakages. For the Rome pouch, a similar rate of 5.7% (2/35)<br />
was reported. 23<br />
Whereas studies on the conduits of the ileum or colon<br />
report a permanent loss of renal function in 12% 24 <strong>and</strong> 17%<br />
of patients, 25 respectively, this has not been seen in continent<br />
urinary diversions. 15 In our own group of patients, no postrenal<br />
complications occurred, which is in line with the findings<br />
of Goldberg. 18 However, an 81-year-old patient with<br />
an IC developed a transient anterenal failure early after<br />
operation.<br />
Wilkin et al 26 report that complications are more frequent<br />
in patients with antecedent radiotherapy. In our group,<br />
35 of 100 patients had been previously irradiated. We did<br />
not find a correlation with early complications. Whereas in<br />
the study by Panici et al, 17 the proportion of previously<br />
irradiated patients was similar (15/35 [42.8%]), Ramirez 19<br />
had 98% <strong>and</strong> Angioli had 92%. 15 The reason <strong>for</strong> these discrepancies<br />
is mainly that in Germany, exenteration is seen<br />
as a treatment option besides radiotherapy <strong>for</strong> primary cervical<br />
cancer, whereas in the US, this is not the case. 27<br />
In our study, we found no difference in the qualityof-life<br />
scores <strong>for</strong> patients with a continent ileal pouch<br />
compared with those with a wet ileal conduit stoma. In the<br />
course of the past decades, several studies on the quality of<br />
life after cystectomy came up with various results: Many of<br />
these studies were limited by small patient numbers <strong>and</strong><br />
heterogeneous treatment groups with respect to age or<br />
comorbidities. 28Y30 Most have shown that the overall quality<br />
of life after cystectomy remains satisfactory <strong>for</strong> most<br />
patients. The current body of published literature is insufficient<br />
to conclude that one <strong>for</strong>m of urinary diversion is<br />
superior to another based on quality-of-life outcomes. 31<br />
Quality-of-life might be improved by orthotopic bladder<br />
replacement in selected cases. 32<br />
CONCLUSION<br />
The continent urinary pouch is an alternative to the<br />
wet ileal conduit in patients in need of a bladder replacement<br />
due to PE. Owing to the higher surgical complexity of the<br />
procedure, early complications are more frequent with the<br />
urinary pouch than with an ileal conduit. Conservative<br />
management is sufficient <strong>for</strong> most of the complications.<br />
The rate of complications requiring repeat intervention is<br />
acceptable but higher than with an IC. Furthermore, our study<br />
did not confirm the increase in the quality of life postulated<br />
<strong>for</strong> all <strong>for</strong>ms of continent urinary diversion.<br />
REFERENCES<br />
1. Seiffert L. The intestinal siphon-bladder. Arch Klin Chir.<br />
1935;183:569.<br />
2. Bricker EM. Bladder substitution after pelvic exenteration.<br />
Surg Clin North Am. 1950;30:1511Y1521.<br />
3. Madersbacher S, Schmidt J, Eberle JM, et al. Long-term<br />
outcome of ileal conduit diversion. JUrol. 2003;169:985.<br />
4. Verhoogen J. Neostomie uretero-caecale: <strong>for</strong>mation d’une<br />
novelle poche vesicale et d’un nouvel uretre. Ass France d’Urol.<br />
1908;12:362.<br />
5. Kock NG, Nilson AE, Nilson LO, et al. Urinary diversion via<br />
continent ileal reservoir. Clinical result in 12 patients. JUrol.<br />
1982;128:469.<br />
6. Rowl<strong>and</strong> RG, Mitchell ME, Bihrle R, et al. Indiana continent<br />
urinary reservoir. JUrol. 1987;137:1136Y1139.<br />
7. Penalver MA, Bejany DE, Averette HE, et al. <strong>Continent</strong><br />
urinary diversion in gynecologic oncology. Gynecol Oncol.<br />
1989;34:274Y288.<br />
8. Thuroff JW, Alken P, Engelmann U, et al. The Mainz<br />
pouch (mixed augmentation ileum ’n zecum) <strong>for</strong> bladder<br />
augmentation <strong>and</strong> continent urinary diversion. Eur Urol.<br />
1985;11:152Y160.<br />
9. Farnham SB, Cookson MS. Surgical complications of urinary<br />
diversion. World J Urol. 2004;22:157Y167.<br />
10. Wallce DM. Uretric diversion using a conduit: a simplified<br />
technique. Br J Urol. 1966;38:522Y527.<br />
11. Ware J, Kosinski M, Keller SD. A 12-Item Short-Form<br />
Health Survey: construction of scales <strong>and</strong> preliminary tests<br />
of reliability <strong>and</strong> validity. Med Care. 1996;34:220Y233.<br />
12. Hünlich T, Egger H. [Longtime experience with Uropouch].<br />
Coloproctology. 1996;18:43Y47.<br />
13. Birstow RE, Lagasse LD. Cytoreductive surgery: pelvis. In:<br />
Bristow RE, Karlan BE. Surgery <strong>for</strong> Ovarian Cancer:<br />
Principles <strong>and</strong> Practice. Ox<strong>for</strong>dshire, UK: Taylor & Francis;<br />
2005:135Y144.<br />
14. Wiesner C, Bonfig R, Stein R, et al. <strong>Continent</strong> cutaneous<br />
urinary diversion: long-term follow-up of more than 800 patients<br />
with ileocecal reservoirs. World J Urol. 2006;24:315Y318.<br />
15. Angioli R, Estape R, Cantuaria G, et al. Urinary complications<br />
of Miami pouch: trend of conservative management. Am J<br />
Obstet Gynecol. 1998;179:343Y348.<br />
16. Lampel A, Fisch M, Stein R, et al. <strong>Continent</strong> diversion with<br />
the Mainz pouch. World J Urol. 1996;14:85Y91.<br />
17. Panici PB, Angioli R, Plotti F, et al. <strong>Continent</strong> ileocolonic<br />
urinary diversion (Rome pouch) <strong>for</strong> gynecologic malignancies:<br />
technique <strong>and</strong> feasibility. Gynecol Oncol. 2007;107:194Y199.<br />
18. Goldberg GL, Sukumvanich P, Einstein MH, et al. Total<br />
pelvic exenteration: the Albert Einstein College of Medicine/<br />
Montefiore Medical Center Experience (1987 to 2003).<br />
Gynecol Oncol. 2006;101:261Y268.<br />
19. Mirhashemi R, Lamrbou N, Hus N, et al. The gastrointestinal<br />
complications of the Miami <strong>Pouch</strong>: a review of 77 cases.<br />
Gynecol Oncol. 2004;92:220Y224.<br />
20. Penalver MA, Angioli R, Mirhashemi R, et al. Management of<br />
early <strong>and</strong> late complications of ileocolonic continent urinary<br />
reservoir (Miami pouch). Gynecol Oncol. 1998;69:185Y191.<br />
21. Chang HK, Lo KY, Chiang HS. Complications of urinary<br />
diversion after pelvic exenteration <strong>for</strong> gynecological malignancy.<br />
Int Urogynecol J Pelvic Floor Dysfunct. 2000;11:358Y360.<br />
* 2011 IGCS <strong>and</strong> ESGO 407<br />
Copyright © 2011 by IGCS <strong>and</strong> ESGO. Unauthorized reproduction of this article is prohibited.
Forner <strong>and</strong> Lampe International Journal of Gynecological Cancer & Volume 21, Number 2, February 2011<br />
22. Ramirez PT, Modesitt SC, Morris M, et al. Functional<br />
outcomes <strong>and</strong> complications of continent urinary diversions<br />
in patients with gynecologic malignancies. Gynecol Oncol.<br />
2002;85:285Y291.<br />
23. Angioli R, Zullo MA, Plotti F, et al. Urologic function <strong>and</strong><br />
urodynamic evaluation of urinary diversion (Rome pouch)<br />
over time in gynecologic cancers patients. Gynecol Oncol.<br />
2007;107:200Y204.<br />
24. Segreti EM, Morris M, Levenback C, et al. Transverse colon<br />
urinary diversion in gynecologic oncology. Gynecol Oncol.<br />
1996;63:66Y70.<br />
25. Hancock KC, Copel<strong>and</strong> LJ, Gershenson DM, et al. Urinary<br />
conduits in gynecologic oncology. Obstet Gynecol.<br />
1986;67:680Y684.<br />
26. Wilkin M, Horwitz G, Seetharam A, et al. Long-term<br />
complications associated with the Indiana pouch urinary<br />
diversion in patients with recurrent gynecologic cancers after<br />
high-dose radiation. Urol Oncol. 2005;23:12Y15.<br />
27. Marnitz S, Dowdy S, Lanowska M, et al. Exenterations 60 years<br />
after first description. Int J Gynecol Cancer. 2009;19:974Y977.<br />
28. Skinner EC. Quality of life with reconstruction. Semin Urol<br />
Oncol. 2001;19:56Y58.<br />
29. Gerharz EW, Mansson A, Hunt S, et al. Quality of life after<br />
cystectomy <strong>and</strong> urinary diversion: an evidence based analysis.<br />
JUrol. 2005;174:1729Y1736.<br />
30. Autorino R, Quarto G, Di Lorenzo G, et al. Health related<br />
quality of life after radical cystectomy: comparison of ileal<br />
conduit to continent orthotopic neobladder. Eur J Surg Oncol.<br />
2009;35:858Y864.<br />
31. Porter MP, Penson DF. Health related quality of life after<br />
radical cystectomy <strong>and</strong> urinary diversion <strong>for</strong> bladder cancer:<br />
a systematic review <strong>and</strong> critical analysis of the literature.<br />
JUrol. 2005;173:1318Y1322.<br />
32. Chiva LM, Lapuente F, Nunez C, et al. <strong>Ileal</strong> orthotopic<br />
neobladder after pelvic exenteration <strong>for</strong> cervical cancer.<br />
Gynecol Oncol. 2009;113:47Y51.<br />
408 * 2011 IGCS <strong>and</strong> ESGO<br />
Copyright © 2011 by IGCS <strong>and</strong> ESGO. Unauthorized reproduction of this article is prohibited.