Download The Pharos Winter 2011 Edition - Alpha Omega Alpha
Download The Pharos Winter 2011 Edition - Alpha Omega Alpha
Download The Pharos Winter 2011 Edition - Alpha Omega Alpha
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
���������������������������������������������<br />
� ����������� �<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> 2008 3
�Αξιος ��ωφελε�ιν το�υς ��αλγο�υντας<br />
����������������������<br />
�����������<br />
��������������������������������������������������������������������������������������������������������������<br />
������������������������������������������������������������������������������<br />
����������������������������������������������<br />
�������������������������������������������������������������������������������������������������������������������<br />
����������������������������������<br />
�����������������������������������������������������������������������������������������<br />
�������������������������������������������������������������������������������������������������������������������<br />
��������������������������������������������������������������������������������������������������������������������<br />
���������������������������������������������������������������������������������������������������������������������<br />
� �������������������������������������������������������������������������������������������������������������������<br />
������������������������������������������<br />
������������������������<br />
��������������������������������������������������������������������������������������������������������������<br />
��������������������������������������������������������������������������������������������������������������������������<br />
�<br />
������������������������<br />
���������������������������������������������������������������������������������������������������<br />
�<br />
���������������������<br />
���������������������������������������<br />
����������������������������������<br />
��������������������������������������������<br />
� �����������<br />
Officers and Directors at Large<br />
�����������������������<br />
���������<br />
������������������<br />
���������������������<br />
��������������<br />
�������������������<br />
�����������������������<br />
�������������������<br />
�������������������<br />
��������������������<br />
��������������������<br />
�������������������<br />
������������������������<br />
�����������������������<br />
����������������<br />
��������������������<br />
�������������������<br />
�����������������<br />
����������������<br />
��������������������<br />
���������������<br />
Medical Organization Director<br />
��������������������<br />
������������������������������<br />
Councilor Directors<br />
������������������������<br />
�<br />
����������������������������������<br />
�����������������<br />
���������������������������������<br />
����������������<br />
�<br />
��������������������������������<br />
Coordinator, Residency Initiatives<br />
�������������������<br />
�������������������<br />
Student Directors<br />
�������������<br />
��������������������������������<br />
�����������������������<br />
����������������������������<br />
����������������<br />
�������������������������������<br />
������<br />
���������������������<br />
��������������������<br />
������������������<br />
����������������������<br />
������������������������������<br />
����������������������������<br />
�������������������������<br />
�������������������<br />
��������������������������������<br />
�����������������������<br />
Editorial Board<br />
�������������������������<br />
������������������<br />
���������������������<br />
�����������������������<br />
�����������������������<br />
���������������<br />
�������������������<br />
���������������������<br />
�������������������<br />
������������������<br />
��������������������<br />
������������������������<br />
�������������������<br />
�������������������������<br />
����������������������<br />
�������������������<br />
����������������<br />
������������������<br />
�����������������<br />
�����������������<br />
���������������������<br />
������������������<br />
����������������<br />
�����������������<br />
�������������������<br />
���������������������<br />
�����������������������<br />
�����������������������<br />
����������������������<br />
�����������������<br />
�������������<br />
������������������������<br />
��������������������<br />
��������������������<br />
�������������������<br />
����������������<br />
��������������������<br />
���������������������<br />
�������������<br />
�������������������������<br />
������������������<br />
������������������<br />
�������������������<br />
�����������������������<br />
������������������<br />
�����������������������<br />
�������������������<br />
������������������<br />
�������������������<br />
���������������������<br />
�������������������������<br />
�������������������<br />
������������������������<br />
���������������������<br />
�����������������������<br />
�����������������<br />
��������������<br />
����������������������<br />
��������������������<br />
������������������<br />
������������������<br />
������������������<br />
������������������<br />
�������������������<br />
��������������������<br />
������������������������<br />
���������������������<br />
���������������������<br />
��������������������������<br />
����������������������<br />
��������������������<br />
��������������������������<br />
������<br />
��������������������<br />
��������������������������<br />
��������������<br />
��������������������<br />
������������������<br />
���������������<br />
�����������������������<br />
���<br />
������<br />
������<br />
��������������������<br />
���������������<br />
��������������������<br />
���������������������<br />
�<br />
���������������<br />
�<br />
�������������<br />
�������������������<br />
���������������<br />
�����������������<br />
����������������������������<br />
��������������<br />
��������������������
Editorial<br />
<strong>The</strong> song goes on<br />
Robert Atnip, MD<br />
<strong>The</strong> author (AΩA, University of Alabama, 1976)<br />
is a member of the board of directors of <strong>Alpha</strong><br />
<strong>Omega</strong> <strong>Alpha</strong>.<br />
am an academic vascular surgeon, a senior fac-<br />
I ulty member at a University Hospital, a mentor<br />
of medical students and residents, and a teacher<br />
of professionalism. My own lessons in professionalism<br />
came while in medical school, but<br />
not in any classroom or book. I don’t recall the<br />
word even being spoken during those four years<br />
(1974–78). No doubt some of those who modeled<br />
it for me were physicians, but in retrospect, the<br />
most influential person was no doctor, but a musician.<br />
That music has the power to pervade the human experience<br />
may be a mystery, but it is no secret. Music is as universal<br />
as the human senses, and as vital. As a form of human<br />
expression, music is at the same time both elemental and<br />
transcendent. It is one of humanity’s finest gifts to itself, a<br />
gift that to our lament cannot be as readily celebrated in <strong>The</strong><br />
<strong>Pharos</strong> as the visual and literary arts. Music is not for speaking<br />
or writing. Music is ineffable emotion, a sequence of nameless<br />
swells and surges that defy the bounds of speech. Our voices<br />
are put to much better use making music than describing it<br />
and, in like manner, professionalism is much less a creed to<br />
be discerned and codified than it is a craft to be realized and<br />
enacted. <strong>The</strong>rein lies the basis for choral music to instruct me<br />
in the finer points of professionalism.<br />
Nowadays, professionalism is a paramount concern to the<br />
health care world, but it was not always so. “Professionalism”<br />
was irrelevant to academia prior to 1965. My search for “professionalism”<br />
as a key word in OLD_OVID (1947–65) returned<br />
only the red-lettered retort, “Unable to match with any subject<br />
heading.” In the fifteen years that followed, “professionalism”<br />
made its debut with 180 appearances, the majority in nursing<br />
journals or, oddly enough, in the dentistry literature. But only<br />
in the last thirty years has “professionalism” gained enough<br />
traction to merit the eight subject headings to which it now<br />
maps in OVID, the thousands of publications devoted to<br />
probing its obliquities, or the several awards and grants now<br />
bestowed in its name by prestigious societies such as ours.<br />
This logarithmic progression is extraordinary for a concept<br />
that acquired its name as long ago as the fourteenth<br />
century. Toward the end of the so-called Dark Ages, the word<br />
“profess” appeared among religious orders with the meaning<br />
“to take a vow,” or “to declare [a belief] publicly.” This definition<br />
and related word forms served adequately, perhaps even<br />
admirably, throughout all subsequent ages of history and into<br />
modern times. Only in the post-Modern era has the simplicity<br />
and sparse eloquence of these phrases come to be viewed as<br />
inadequate for today’s professionals. But I think what may be<br />
lacking is not the words, but the . . . music!<br />
And so in the mid-1970s, modern professionalism’s “early<br />
years,” I came upon my unwitting mentor-to-be while in medical<br />
school in Birmingham, Alabama. Having enjoyed music<br />
and singing as a youth, and wanting some activity<br />
beyond the confines of studying anatomy<br />
and physiology, I met JWS, the organist and<br />
choirmaster at a local church. <strong>The</strong> meeting<br />
was happenstance, but serendipity has never<br />
worked any better magic than this. I joined and<br />
sang in his choir, as much an amateur singer as<br />
I was a fledgling doctor. But the experience was<br />
profound, a turning point for me, and a revelation<br />
of new worlds. For the next three years this<br />
choir became as important to me as my medical<br />
education. Under the direction of JWS, or more<br />
properly, under his spell, I learned what it is to<br />
“profess” choral music: to blend many voices into one sound,<br />
the music built on every voice, but ever greater than any one<br />
alone; to tune each voice and phrase toward perfection; to purify<br />
many harmonies into one great and coherent beauty. <strong>The</strong><br />
sounds and the music were exquisite, many of them recorded<br />
at that time, and still inspiring to me more than thirty years<br />
later. To listen to them is to understand the fruits of professionalism<br />
and, moreover, to discern therein a startling similarity<br />
to what we seek to do in the individual and corporate acts<br />
of medical practice.<br />
This connection of music to medicine may seem obscure to<br />
some, and self-evident to others. But I contend that the truths<br />
learned in the making of music are the same truths that we<br />
who profess medicine must teach our students, and re-affirm<br />
for ourselves: competence, discipline, determination, focus,<br />
artistry, the seeking of common goals, the drive to excel, the<br />
ability to lead and to follow, and one perhaps not as obvious:<br />
aesthetics—the presence of beauty and inner harmony in what<br />
we do. I do not equate humanism with professionalism, but<br />
they have much in common. <strong>The</strong>y are separate yet inseparable,<br />
linked by a common need for each to nourish the other. I was<br />
most fortunate at a remarkable and formative time of my life to<br />
be in a milieu suffused with an abundance of each. To those who<br />
cleared this path for me, I owe an inexpressible debt. <strong>The</strong>y knew<br />
that professionalism has not only a body, but a soul.<br />
It was never my destiny to become a professional musician,<br />
but I am delighted to be a musical professional. Music may not<br />
have made me a better medical scientist, but it has made me a<br />
better physician. Vita brevis, ars longa. To the extent that we<br />
are true to our identity as healers, then we must—in concert<br />
with advances in science and technology—remain centered on<br />
the collective humanity of patient and physician, which in all<br />
its forms is our common bond.<br />
JWS retired in 1998, and died in 2007 of Parkinson’s<br />
disease. He and Ted Harris were much alike. <strong>The</strong>y were extraordinary<br />
persons who led others to perform beyond expectations,<br />
and showed all those around them that exceptional<br />
effort yields uncommon rewards. <strong>The</strong>se two men were called<br />
into different professions, but each understood precisely what<br />
it meant to “take a vow.” and to “declare publicly.” It is to the<br />
betterment of humankind that each lived, and thus our own<br />
joyful duty to ensure that their song goes on.<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 1
������<br />
����������<br />
������������<br />
�������� ��������������<br />
1 Editorial<br />
<strong>The</strong> song goes on<br />
Robert Atnip, MD<br />
35<br />
42<br />
46<br />
Health policy<br />
Our health care system is not<br />
broken—it’s obsolete!<br />
Jordan J. Cohen, MD<br />
<strong>The</strong> physician at the<br />
movies<br />
Peter E. Dans, MD<br />
Wall Street: Money Never<br />
Sleeps<br />
Conviction<br />
Reviews and reflections<br />
<strong>The</strong> Checklist Manifesto: How to<br />
Get Things Right<br />
Reviewed by David A. Bennahum,<br />
MD<br />
<strong>The</strong> Jump Artist<br />
Reviewed by Jeffrey L. Ponsky,<br />
MD<br />
Henry Kaplan and the Story of<br />
Hodgkin’s Disease<br />
Reviewed by William M. Rogoway,<br />
MD<br />
<strong>The</strong> National Institutes of Health:<br />
1991–2008<br />
Reviewed by Jack Coulehan, MD<br />
51 Letters<br />
AΩA NEWS<br />
38 2010 <strong>Alpha</strong> <strong>Omega</strong><br />
<strong>Alpha</strong> Robert J. Glaser<br />
Distinguished Teacher<br />
Awards<br />
52<br />
DEPARTMENTS<br />
National and chapter news<br />
Instructions for <strong>Pharos</strong> Authors<br />
Leaders in American Medicine<br />
������<br />
ARTICLES<br />
Visionary art?<br />
Shamans, Charles Bonnet, and the cave<br />
paintings<br />
Henry N. Claman, MD<br />
�<br />
Going first<br />
Susie Morris, MD, MA<br />
��<br />
<strong>The</strong> monsters of medicine<br />
Political violence and the physician<br />
Amanda J. Redig, MD, PhD<br />
��<br />
�������
�������<br />
Breaking bad news<br />
What poetry has to say about it<br />
Dean Gianakos, MD<br />
From rabbits to the<br />
League of Nations<br />
Early standardization of the insulin unit<br />
�������<br />
��<br />
Barry Fields, MD<br />
��<br />
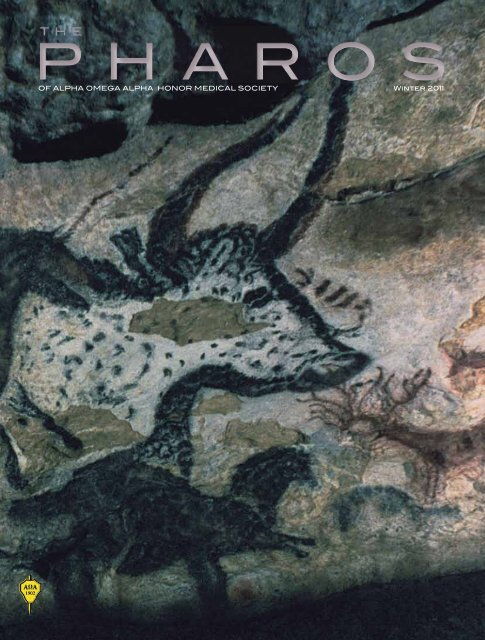
On the cover<br />
�����������������������<br />
See page 4<br />
���������� ������<br />
�������<br />
���������������������������������������������<br />
� ����������� �<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> 2008 3<br />
11 Room K461<br />
Mary Krane Derr<br />
15 Musings on an Attic<br />
Tetradrach<br />
Alvin J. Cummins, MD<br />
23 Sestina on Limb-<br />
Lengthening Surgery<br />
Jenna Le<br />
27 Heartache<br />
John Allan, MD<br />
34 <strong>The</strong> Defendant<br />
H. Harvey Gass, MD<br />
36 Memento Mori<br />
Michael R. Milano, MD<br />
37<br />
40<br />
POETRY<br />
Reading a Review<br />
H. J. Van Peenen, MD<br />
Winning Poems of the<br />
2010 Write a Poem for<br />
This Photo Contest<br />
Benevolent Instructions<br />
David R. Downs, MD<br />
Commencement<br />
David F. Dozier, Jr., MD<br />
Adolescent Choices<br />
H. J. Van Peenen, MD<br />
XX Ageless<br />
Thomas Atwater<br />
INSIDE<br />
BACK<br />
COVER
Visionary art?<br />
Shamans, Charles Bonnet, and the cave paintings<br />
Henry N. Claman, MD<br />
<strong>The</strong> author (AΩA, University of Colorado, 1979) is<br />
Distinguished Professor of Medicine and Associate Director<br />
of the Medical Humanities Program at the University of<br />
Colorado, Denver. He is a member of the editorial board of<br />
<strong>The</strong> <strong>Pharos</strong>.<br />
Paleolithic art, particularly the cave paintings of<br />
Southwestern Europe, is a source of amazement still.<br />
<strong>The</strong>se images haunt many of us, not only because of<br />
their beauty and their great age, (stretching back over 30,000<br />
years), but because they are one of the few entrées we might<br />
have into the lives of our ancestors, who are among the great<br />
masters of artistic creativity, and about whom we know very<br />
little apart from this art. <strong>The</strong> study of this art continues to<br />
expand as art historians, anthropologists, archaeologists, and<br />
natural history scientists try to unravel the mystery of what<br />
the art “means” and why it was made. <strong>The</strong>re is a wide divergence<br />
in opinions on this subject, and some experts have actually<br />
warned against further attempts to discover “the meaning”<br />
of paleolithic art. However, it is hard to abandon the quest,<br />
and this contribution attempts to call attention to another<br />
possible avenue of interpretation, relying on new neurophysiological<br />
concepts.<br />
<strong>The</strong> art was produced in profusion, and consists mainly<br />
of paintings and engravings, as well as sculpture in the round<br />
and in bas-relief. <strong>The</strong> early members of our genus and species,<br />
Homo sapiens sapiens, were hunter-gatherers. <strong>The</strong>y lived in<br />
small nomadic bands of perhaps fifty to one hundred people,<br />
in a mostly egalitarian society. <strong>The</strong>y made stone tools and had<br />
fire but made neither cloth nor pottery. Half of the art is in<br />
limestone caves and half is outside, mainly in shelters. Those<br />
in the caves are better preserved and have received the most<br />
attention.<br />
What was depicted? Many of the most prominent images<br />
are of animals, mainly large ones such as horses, bisons, bovids,<br />
lions, rhinoceri, reindeer, and so forth. Rarely seen is a<br />
small animal such as a rabbit or owl. <strong>The</strong> large animals are almost<br />
always shown in profile, in big or small images, complete<br />
or fragmentary. When I was lucky enough to be in the Great<br />
Hall of the “original” Lascaux cave (now closed to the public)<br />
I felt that I was engulfed in the midst of a huge stampede. It<br />
was an overwhelming experience of power and speed. In addition<br />
to all the animal depictions, however, there are a lesser<br />
number of human figures, or parts of humans, including positive<br />
and negative hand prints and images of (mainly female)<br />
genitalia. Intact humans are rare and almost always masked.<br />
<strong>The</strong>re is a also very large number of enigmatic forms that are<br />
Man looking at prehistoric cave painting of animals.<br />
Photo by Ralph Morse//Time Life Pictures/Getty Images.<br />
4 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 5
Visionary art?<br />
Bulls, horses, deer, Lascaux Cave, France, about 17,000 years ago.<br />
© <strong>The</strong> Bridgeman Art Library/Getty Images, Inc.<br />
difficult to describe, called abstract symbols, or designs, and<br />
so forth. <strong>The</strong>se range from simple colored dots or strokes or<br />
carved shallow cupules in the stone to complex grid-like paintings<br />
or engravings. Some of these geometric designs have been<br />
termed “tectiforms” (roof-like) although there is no evidence<br />
that there were any roofs.<br />
<strong>The</strong>se abstract forms, because of their refusal to give up<br />
their secrets, have been rather neglected by historians, at least<br />
in comparison with the more flamboyant animal images, to<br />
say nothing about the carved and decorative mostly female<br />
statuettes (misnamed “Venus” figurines). <strong>The</strong>se abstract images<br />
can give us additional clues as to the production of the<br />
art in general.<br />
Deciphering the “meanings” of paleolithic art<br />
Analyzing the art is a formidable task, and the process continues,<br />
with various schema current at one time or another. 1,2<br />
Art for art’s sake—During the period when paleolithic art<br />
was known mainly from small carved and engraved bones and<br />
antlers, the genre was regarded as aesthetic and playful. This<br />
approach has been largely abandoned.<br />
Sympathetic magic—When the great cave paintings of<br />
Altamira and Lascaux were discovered, the depiction of large<br />
hunted animals, often with spears or arrows in them, led<br />
to the concept of “hunting magic” or “sympathetic magic.”<br />
According to this model, emphasized by Sir James Frazer in<br />
<strong>The</strong> Golden Bough, hunter-gatherer people made pictures of<br />
their prey to remember yesterday’s foray or to imagine and<br />
ensure the success of tomorrow’s venture. 3 This interpretation<br />
has its advocates today.<br />
In the structuralist approach, pioneered by André Leroi-<br />
Gourhan, the images were subjected to sophisticated measuring<br />
and counting techniques that led to interpretations of the<br />
arrangement of art in symbolic terms, emphasizing quantitative<br />
correspondences and dualistic contrasts, e.g., male versus<br />
female symbols, red versus black images and horses versus<br />
bison. 4 <strong>The</strong> ultimate rationale may have been to promote fertility<br />
in both human and animal worlds, which were, of course,<br />
extremely interwoven and interdependent in hunter-gatherer<br />
societies. Many find this approach arcane.<br />
6 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
Emphasis currently centers on what has been called the<br />
mystico/religious interpretation, in which spiritual concepts<br />
are invoked and shamans are considered to be closely involved<br />
in art production and corresponding ritual activities. This approach<br />
is largely influenced by David Lewis-Williams and his<br />
studies of the rock art of the San People of South Africa. He<br />
applies this interpretation to paleolithic and neolithic art. 5,6<br />
R. Dale Guthrie dismisses this concept in favor of a natural<br />
history/evolutionary schema, placing the art in the larger context<br />
of environmental influences and linking artistic behavior<br />
to our evolutionary past. 2<br />
None of these approaches has unanimous scholarly approval.<br />
Indeed, experts are beginning to doubt that we will<br />
ever uncover “the meanings.” Yet the desire to do so is irresistible,<br />
and so let us turn to a particular image.<br />
<strong>The</strong> shaman of Lascaux<br />
This astonishing figure, discovered when the cave itself<br />
was opened in 1940, should have brought the idea of shamans<br />
to the fore right away. It is unique, being the only complete<br />
“<strong>The</strong> Shaman of Lascaux,” about 17,000 years ago. A bird-headed and -handed ithyphallic stick man in front of a wounded bison,<br />
pierced by spears, with entrails spilling out. <strong>The</strong> Shaman has a bird-head staff. © Charles and Josette Lenars/CORBIS.<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 7
Visionary art?<br />
Abstract “designs” (with perhaps a positive handprint)—a montage of items from caves in what is now France and Northern Spain, about<br />
17,000–10,000 years ago. Illustration by Jim M’Guinness.<br />
human image in the cave. It is far from the stampede of animals<br />
I mentioned above, and is placed on the wall at the bottom<br />
of an eighteen-foot “well” or “shaft”—curiously isolated<br />
and difficult to access. Considering the general profusion of<br />
animals on the walls and even the ceilings, the shaman is solitary<br />
and secluded. This stick-figure of a man, drawn poorly in<br />
outline, has a bird’s head and bird’s hands, with a bird-headed<br />
scepter at his side. He is obviously male, with a prominent<br />
erect penis (the “ithyphallic position”)—a symbol of power.<br />
He is either upright or leaning, depending on the angle of the<br />
photograph. He is next to a well-drawn bison that is looking<br />
over its shoulder at a gaping wound in his flank with his intestines<br />
falling out. <strong>The</strong>re are two spears in his side.<br />
I agree with Joseph Campbell that he is a shaman, part<br />
human, part bird. 7 Including the bison, the ensemble must<br />
be the oldest narrative visual scene in human history. Yet it<br />
is profoundly ambiguous. What is the story? What is the shaman’s<br />
role vis-à-vis the bison?—a healer?—a hunter? Is he in a<br />
trance? Is he drugged? Why is he ithyphallic?<br />
Nevertheless, he is not the only masked magic man in the<br />
caves. <strong>The</strong>re is the masked and antlered “sorcerer” man in the<br />
Trois Freres cave, and others as well.<br />
8 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
<strong>The</strong> abstract designs—providing clues?<br />
Returning to the abstract images, it is understandable<br />
that they have received less attention<br />
than those of animals and people. <strong>The</strong>y are very<br />
numerous, but are often small and have proved<br />
opaque to interpretation. Perhaps the most attentive<br />
scholar has been S. Giedion, the Swiss<br />
historian. He believed that “symbolization is the<br />
key to all paleolithic art,” 8p79 and he points out<br />
that the “great abstract symbols which have no<br />
counterpart in the world of reality” are often<br />
“hidden away in the most inaccessible parts of the<br />
caverns.” 8p241 While the meanings of female pubic<br />
triangles and vulvas as well as penile images are<br />
easy to understand in terms of fertility and procreative<br />
symbolism, this is not true of the abstract<br />
designs. What then?<br />
Lewis-Williams thinks they are hallucinations,<br />
conjured up by shamans in trances, which<br />
provided powerful spiritual experiences of the<br />
San People’s three-tiered cosmos, and which<br />
were later displayed as rock art—petrographs and<br />
petroglyphs. 5 This is a concept worth considering.<br />
<strong>The</strong> hallucination approach<br />
This is a complicated subject indeed. <strong>The</strong><br />
very long list of conditions associated with visual<br />
hallucinations includes ocular disorders, CNS<br />
disorders, toxic disturbances, psychiatric illnesses,<br />
and “normal” persons. 9 In the context of<br />
images hidden in large, dark caves, it is of interest<br />
that a number of the hallucinogenic scenarios<br />
in “normal” persons involve forms of sensory<br />
deprivations. <strong>The</strong>se include dreams, hypnagogic<br />
and hypnotic states, sleep deprivation, and simply<br />
blindfolding. To this list should now be added a<br />
relatively new syndrome.<br />
<strong>The</strong> Charles Bonnet Syndrome<br />
This condition has a curious history. 10 Bonnet,<br />
born in 1720, was a Swiss/French naturalist and<br />
philosopher. (He deserves more recognition for<br />
his experiments in wood lice, establishing the phenomenon<br />
of parthenogenesis.) In 1760 he wrote a book in which he<br />
described how his eighty-seven-year-old grandfather lost his<br />
vision to cataracts and developed hallucinations “of men, of<br />
women, of birds, of carriages, of buildings.” Interestingly, the<br />
same later happened to Bonnet himself.<br />
<strong>The</strong> situation lay fallow until 1967 when George de Morsier<br />
proposed the term Charles Bonnet Syndrome (CBS) to describe<br />
the presence of recurrent visual hallucinations generally<br />
in persons with impaired vision but without clouded<br />
sensoria. Such persons are often elderly. Since then, the<br />
syndrome has been increasingly recognized and studied. 11 It<br />
is present in perhaps ten percent of the elderly with impaired<br />
vision.<br />
<strong>The</strong> hallucinations experienced are varied and often complex,<br />
in contrast to “unformed” hallucinations such as spots<br />
and flashes of light, which are termed “phosgenes.” <strong>The</strong>y include<br />
animals, humans, geometric figures, and designs, similar<br />
to what is seen in the caves. <strong>The</strong>y are in color or black and<br />
white, and are often brilliant and clear, contrasting with the<br />
poor “regular” vision of the subjects. <strong>The</strong>y frequently fade or<br />
disappear as sight deteriorates further. <strong>The</strong> commonest cause<br />
of CBS in our society is age-related macular degeneration,<br />
but it has been reported in the young and also in association<br />
with pathological changes from the eye to the visual cortex.<br />
To diagnose CBS, there should be no evidence of delirium,<br />
dementia, psychosis, or intoxication. <strong>The</strong> visions are not felt<br />
to originate in the eye itself. 11<br />
It is well-known that hallucinations with a normal sensorium<br />
may be provoked or aggravated by a number of factors<br />
including sensory deprivation, the hypnagogic state, physical<br />
or auditory stimuli, extreme pain, etc. 9 <strong>The</strong> same is true of<br />
CBS.<br />
<strong>The</strong> pathophysiology of CBS—the release<br />
phenomenon<br />
<strong>The</strong> idea that hallucinations may be caused by “irritative”<br />
foci in the brain derives by analogy from John Hughlings<br />
Jackson’s analysis of focal epilepsy. This explanation for hallucinations<br />
has generally given way more recently to the<br />
work of David Cogan 12 (who also refers to Louis J. West 13 )<br />
that suggests that hallucinations of various types are instead<br />
“release phenomena.” Interestingly, this concept also derives<br />
from Hughlings Jackson, who developed the general concept<br />
that higher functional layers of the CNS normally inhibit<br />
lower layers. When, however, the higher layers are themselves<br />
impaired, normally suppressed activities of the lower layers<br />
are released. (Consider the spasticity of the pithed frog or<br />
alcohol-induced misbehavior.) In the visual system, normal afferent<br />
stimuli dampen or block the spontaneous “endovision”<br />
activities. But when, in some people, blindness “deafferents”<br />
the visual pathways, the spontaneous endovisual activities take<br />
over, leading to hallucinations. In fact, fMRI studies support<br />
this concept. 14<br />
Hallucination manifestations<br />
Many studies of hallucination point out similarities in the<br />
images that are seemingly independent of the cause and the<br />
culture involved. Heinrich Klüver, with an extensive experience<br />
primarily associated with mescal studies, wrote of three<br />
stages of evolving hallucinations 15 :<br />
Type I—“Form constants,” namely geometric abstract designs<br />
described as gratings, lattices, fretwork; also tunnels,<br />
alleys, vessels; and spirals.<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 9
Visionary art?<br />
Type II—Familiar objects such as people, faces, animals,<br />
landscapes.<br />
Type III—Fabulous landscapes and monstrous forms.<br />
Hallucinations in paleolithic art?<br />
<strong>The</strong> above outline of selected aspects of paleolithic imagery<br />
suggests that the abstract designs may not in fact be symbols.<br />
In fact, it was never clear what they might have symbolized.<br />
Instead they may be graphic representations of visual hallucinations—the<br />
“form constants” of Klüver’s Stage I.<br />
<strong>The</strong>re are a number of circumstances that support this<br />
hypothesis, circumstances that reinforce each other:<br />
1. Many of the paintings and engravings are made in very<br />
deep caves, where the darkness (and difficulty of access) is<br />
daunting. <strong>The</strong>ir very locations, even if dimly illuminated by<br />
the uncertain flickerings of oil lamps and flambeaux, would<br />
have been situations of considerable sensory deprivation.<br />
2. Any degree of partial visual impairment—from disease,<br />
CBS, trauma, etc.—would only heighten the deprivation.<br />
3. <strong>The</strong> possible (if not probable) use of psychedelic substances<br />
in trances or ceremonies would further the tendency<br />
to hallucinate. (What indeed was going on with the shaman<br />
of Lascaux?)<br />
4. <strong>The</strong> role of dreaming in gaining access to mental imagery<br />
should not be discounted.<br />
Conclusion<br />
Does the “hallucination approach” to the abstract designs<br />
give us any insight into the most intriguing problem of<br />
paleolithic art—the “meaning(s)” of the animal portrayals?<br />
Certainly, in a hunt-oriented culture dependent on animal<br />
protein for sustenance and perhaps also on animal skins for<br />
protection and disguise, it is not surprising to see those images.<br />
But it is not so simple. We are not seeing the mere paleolithic<br />
dinner menu, as many of the animal species portrayed<br />
were too dangerous to hunt and were, to judge from bony<br />
remains, not eaten. Nonetheless, the images of these animals<br />
demonstrate power, when one considers their numbers, their<br />
sizes, their detailed and imaginative depictions, their often<br />
secluded locations, and their artistic skill. <strong>The</strong> purposes were<br />
probably multiple, including messages such as “come here<br />
and nourish us” as well as “stay away—you’re dangerous” (the<br />
apotropaic or “warding off evil” strategy).<br />
<strong>The</strong> shaman of Lascaux confronting the wounded bison<br />
(risking being wounded himself in the process) would seem<br />
to provide a conceptual and possibly material link between<br />
the human/animal world and the realm of the spirits. It would<br />
be he who, via his trances (however induced), experienced<br />
that spiritual world and then “returned” to inspire the artists,<br />
perhaps including himself. In this context, these extraordinary<br />
portraits would reflect not only actual animals but thoughts,<br />
wishes, memories, or dreams or Type II Klüver hallucinations<br />
of them as well.<br />
E. H. Gombrich, the outstanding art historian, remarked<br />
that “the further back we go in history . . . the less sharp is<br />
the distinction between images and real things; in primitive<br />
societies, the thing and its image were simply two different . . .<br />
manifestations of the same energy or spirit.” 16p155<br />
Perhaps these artists perceived no differences at all!<br />
References<br />
1. Bahn PG, Vertut J. Journey Through the Ice Age. Berkeley<br />
(CA): University of California Press; 1997.<br />
2. Guthrie RD. <strong>The</strong> Nature of Paleolithic Art. Chicago: University<br />
of Chicago Press; 2005.<br />
3. Frazer JG. <strong>The</strong> Golden Bough: <strong>The</strong> Roots of Religion and<br />
Folklore. New York: Avenel Books; 1981.<br />
4. Leroi-Gourhan A. <strong>The</strong> Dawn of European Art: An Introduction<br />
to Palaeolithic Cave Painting. Cambridge: Cambridge University<br />
Press; 1982.<br />
5. Lewis-Williams D. <strong>The</strong> Mind in the Cave: Consciousness and<br />
the Origins of Art. London: Thames and Hudson; 2002.<br />
6. Clottes J, Lewis-Williams D. <strong>The</strong> Shamans of Prehistory:<br />
Trance and Magic in the Painted Caves. New York: Harry N.<br />
Abrams; 1998.<br />
7. Campbell J. <strong>The</strong> Masks of God: Primitive Mythology. New<br />
York: Penguin Books; 1976: 300–302.<br />
8. Giedion S. <strong>The</strong> Eternal Present: A Contribution on Constancy<br />
and Change. New York: Bollingen Foundation; 1962.<br />
9. Cummings JL, Mega MS. Chapter 13: Hallucinations. In:<br />
Cummings JL, Mega MS. Neuropsychiatry and Behavioral Neuroscience.<br />
Oxford: Oxford University Press; 2003: 187–99.<br />
10. Hedges TR Jr. Charles Bonnet, his life, and his syndrome.<br />
Surv Ophthalmol 2007; 52: 111–14.<br />
11. Menon GJ, Rahman I, Menon SJ, et al. Complex visual hallucinations<br />
in the visually impaired: <strong>The</strong> Charles Bonnet Syndrome.<br />
Surv Ophthalmol 2003; 48: 58–72.<br />
12. Cogan DG. Visual hallucinations as release phenomena. Albrecht<br />
v Graefes Arch klin exp Ophthal 1973; 188: 139–50.<br />
13. West LJ. Chapter 9: A Clinical and <strong>The</strong>oretical Overview of<br />
Hallucinatory Phenomena. In: Siegel RK, West LJ, editors. Hallucinations:<br />
Behavior, Experience, and <strong>The</strong>ory. New York: John Wiley &<br />
Sons; 1975: 287–311.<br />
14. ffytche DH, Howard RJ, Brammer MJ, et al. <strong>The</strong> anatomy<br />
of conscious vision: an fMRI study of visual hallucinations. Nature<br />
Neurosci 1988; 1: 738–42.<br />
15. Klüver H. Mescal and Mechanisms of Hallucinations. Chicago:<br />
University of Chicago Press; 1966.<br />
16. Sontag S. On Photography. New York: Farrar, Straus and<br />
Giroux; 1977.<br />
<strong>The</strong> author’s address is:<br />
Allergy/Immunology B164 RC2<br />
12700 E. 19th Avenue, Room 10100<br />
Aurora, Colorado 80045<br />
E-mail: henry.claman@ucdenver.edu<br />
10 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
R O O M<br />
For Adrian Felix Carroll<br />
Tiny blue open-backed gown<br />
that never quite ties back up.<br />
Tiny blood pressure cuff,<br />
thermometer cuff.<br />
Tiny vital signs.<br />
Tiny primary color-coded IVs,<br />
tiny calibrated pumpings<br />
of opiate, anxiolytic, total<br />
parenteral nutrition with adjusted<br />
lipids to avert liver failure.<br />
Tiny blood transfusion.<br />
Tiny ostomy bag.<br />
Tiny liquid rolling crescents<br />
of bluegreen wake-eye. Tiny<br />
flickering visits with.<br />
Tiny answers<br />
from hall-snagged docs.<br />
So what is there here<br />
to miniaturize away<br />
this innards-clawing, hemorrhagic<br />
fever of grief?<br />
Mary Krane Derr<br />
Mary Krane Derr is a poet, writer, musician,<br />
chronic disease patient, and fourth-generation<br />
South Side Chicagoan. Her address is: 6105 South<br />
Woodlawn #3S. Chicago, Illinois 60637. E-mail:<br />
marykderr@aol.com.<br />
Illustration by Jim M’Guinness<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 11
���������<br />
Susie Morris, MD, MA<br />
<strong>The</strong> author is a resident in Psychiatry<br />
at the University of Southern<br />
California. This essay won honorable<br />
mention in the 2010 <strong>Alpha</strong> <strong>Omega</strong><br />
<strong>Alpha</strong> Helen H. Glaser Student Essay<br />
Competition.<br />
She has it so easy.<br />
I guess this shouldn’t be the<br />
first thing that comes to mind<br />
when I look at her. It’s about 12:30 in<br />
the afternoon. She is supine, dare I say<br />
resting? I feel uncomfortable calling<br />
her comfortable because I wonder if<br />
she’s already dead. I wonder if she died<br />
yesterday after she stopped speaking to<br />
us. I peel her eyelids back, and they are<br />
dilated. But she is propped here nonetheless,<br />
her heart still beating faintly<br />
through layers of fat under my stethoscope.<br />
At this point, it’s a stupid ritual.<br />
Her brother and niece are here looking<br />
on.<br />
“Kat went home for a shower,” her<br />
brother tells me. “Dr. Li talked her into<br />
it this morning. He needed to remind<br />
her it was okay to take care of herself.”<br />
Kat is Jenn’s partner. I can’t tell you<br />
how many lesbians I’ve known who<br />
went by Kat or Jenn. As her brother<br />
says her name, I wonder if she was a<br />
Katie or Kathy growing up and then<br />
switched to Kat later in life because it<br />
meshed better with her butch identity.<br />
I met the two of them four days ago.<br />
I found them, Jenn and Kat, sitting in<br />
this hospital room with a broad view<br />
of the city. Kat was perched anxiously<br />
on the fold-out couch, and Jenn was<br />
reclined confidently in the armchair<br />
next to her hospital bed, fully clothed in<br />
a short-sleeved button down and denim<br />
shorts. Both women had short unmistakably<br />
gay hair—the same haircut I<br />
once attempted during college when I<br />
was trying on my own identity. I was<br />
immediately drawn to them because<br />
something about them reminded me<br />
of home.<br />
Jenn told me that she’d been having<br />
hip pain, deep in her left side. She<br />
pointed to the region, and Kat watched<br />
her with cat-like eyes as if to make sure<br />
she described it in its full detail. Jenn<br />
starts a sentence with a slow, casual<br />
voice, one of those just-because-I-can<br />
smiles on her face. Kat finishes those<br />
sentences sharply with full medical detail,<br />
leaning forward into my face closer<br />
and closer each time.<br />
“I guess it started on like Friday, I<br />
think,” Jenn says, kind of looking out at<br />
the cityscape through the window.<br />
“Yes, it was Friday,” Kat states with<br />
some urgency.<br />
No fevers, no bowel symptoms, urinary<br />
symptoms, nothing. Just the pain.<br />
“And Kat says she saw a lymph node<br />
or something. That right, hon?”<br />
“Yes, she has a swollen inguinal<br />
lymph node. I first felt it on Friday, too,<br />
when she was in the shower.” Kat’s face<br />
is wrinkled now, with worry. Her eyes<br />
are dry but red and irritated. She uses<br />
the word “inguinal” to warn me that she<br />
too is medical.<br />
Jenn and Kat are nurses, home health<br />
nurses. This is actually how they met.<br />
“She was the leader of our team,”<br />
Kat tells me later with fresh pride as if<br />
it were yesterday, when in reality, Jenn’s<br />
illness has prevented her from working<br />
for months now.<br />
I think about this: the two of them<br />
making house visits together, surrounded<br />
by the death and sickness<br />
that provided the backdrop for their<br />
romance. Kat was smiling during the<br />
retelling, and her face was transparent<br />
with the old thrill of seducing her<br />
former boss. This was twelve years ago<br />
now. Four years ago, Jenn became suspiciously<br />
swollen. She was diagnosed with<br />
ovarian cancer. <strong>The</strong> intervening years<br />
are notable now for one large reductive<br />
surgery, the loss of Jenn’s uterus,<br />
ovaries, and omentum, and half a dozen<br />
chemotherapy trials. I pulled up her latest<br />
PET scan, and stable mets glowed<br />
back at me, a reminder that the chemotherapy<br />
had only delayed the inevitable<br />
for now. Luckily, she had remained<br />
physically quite strong and was looking<br />
forward to starting a new chemo regimen<br />
next week.<br />
It was Kat who kept her so fit. She<br />
administered meticulous, gentle care<br />
round the clock, but the past six months<br />
had proven increasingly difficult as Jenn<br />
suffered from intractable abdominal<br />
pain and several admissions for small<br />
bowel obstructions. Kat knew the landscape<br />
of Jenn’s body better than Jenn<br />
ever had. This is what one would expect<br />
of lovers of twelve years, except Kat’s<br />
knowledge was borne of something different.<br />
Kat’s eyes now combed the body<br />
of her life partner seeking suspicious<br />
changes, marks that portended the future,<br />
rather than pleasured in the right<br />
12 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
now. <strong>The</strong> numbers in her last CBC, her<br />
last bowel movement, its consistency,<br />
the color and volume of her urine. It was<br />
terror that prompted her daily searches<br />
and created, for them, a new connection<br />
between their bodies, a novel sort<br />
of lovemaking.<br />
It reminded me of years earlier when<br />
I totaled my car. My partner’s mother<br />
had sent us on our way that rainy morning.<br />
We called her later that day from<br />
the interstate, my car in pieces, to tell<br />
her what happened. She told me later<br />
that every time one of her girls left<br />
home, she always imagined the worst,<br />
thinking that if she thought of it first,<br />
it would never happen. That day, it<br />
seemed her pre-emptive imaginings<br />
had betrayed her. I wonder if Kat’s<br />
relentless surveying and bargaining<br />
came out of the same hope.<br />
“It was here-ish,” Kat said, her<br />
fingers plunged into Jenn’s groin,<br />
her gray pubic hair exposed while<br />
my resident and I stood by. Jenn<br />
was half listening, half aware of the<br />
low buzz of All My Children coming<br />
from the flat screen. “For some reason,<br />
I guess I can’t feel it now,” she said, bewildered<br />
and frustrated.<br />
“I never felt anything,” Jenn laughed.<br />
Kat scowled at the floor, seemingly pondering<br />
how her own fingers had somehow<br />
deceived her.<br />
I couldn’t feel anything either.<br />
Neither could my resident. At Kat’s urging<br />
though, in addition to increasing<br />
Jenn’s pain meds, we agreed to get some<br />
lab work and an abdominal CT.<br />
Kat and Jenn had spent the past<br />
two years or so preparing for the final<br />
moments. On the palliative service, I’d<br />
found this was actually kind of rare.<br />
Most people would delay and delay,<br />
throwing radioactivity and chemicals<br />
at tumors that laughed at their efforts,<br />
growing into organs and bone, hiding<br />
from x-rays and stealing moms away<br />
from babies, babies away from moms,<br />
lovers from lovers. Kat and Jenn, in addition<br />
to pursuing aggressive curative<br />
therapies, sought comfort in psychotherapy<br />
where they spoke freely about<br />
what was to come, what Jenn wanted it<br />
to look like, when and under what circumstances<br />
she wanted to stop.<br />
“Well, I’ve had four years since I was<br />
diagnosed.” Jenn is very frank with her<br />
words. “You know, I’d love four more.<br />
Shit, I’d like forty more, but we’re prepared<br />
either way.” I believed that Jenn<br />
was. Kat was another story. Kat’s movements<br />
were like Jenn’s words, decisive<br />
and exact. Wiping sweat from Jenn’s<br />
forehead, combing her hair from her<br />
face, positioning her arms about her<br />
body. However, sometimes I caught her,<br />
in between stoic statements, staring<br />
down at the floor like someone does<br />
whose eyes just flooded, waiting for the<br />
water to resorb, and then looking back<br />
up into the conversation.<br />
We really thought her pain sounded<br />
like a pulled muscle or something.<br />
Something really mild. She was pooping<br />
and peeing and without other systemic<br />
signs of something going wrong.<br />
Perhaps her pain was just related to<br />
her being almost sixty and overweight.<br />
Perhaps it had nothing to do with her<br />
cancer at all. It appeared to be a false<br />
alarm, and I figured we’d have her back<br />
home in no time. As I talked out my differential<br />
with the two of them, Kat nodded<br />
with some degree of relief, albeit<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 13
Going first<br />
About the author<br />
I was born and raised<br />
in rural Utah. I attended<br />
Smith College and graduated<br />
with a degree in<br />
philosophy in 2004. I<br />
am a recent graduate<br />
of Northwestern<br />
University Feinberg School of<br />
Medicine where I earned my<br />
MD and my Masters in Medical<br />
Humanities and Bioethics. I am<br />
starting my residency in psychiatry<br />
this year at the University of<br />
Southern California. I hope to pursue<br />
a career in geriatric psychiatry.<br />
guarded. She accepted my explanation<br />
but called the family anyway.<br />
Jenn reminded me again: “Kat is my<br />
power of attorney.”<br />
“Yes, of course.” I was relieved they’d<br />
done the paperwork, aware of all the<br />
hospital horror stories that had befallen<br />
other gay couples, thinking also that<br />
it was premature to be worrying who<br />
would make decisions for her if she<br />
couldn’t do so herself. She looked just as<br />
healthy as I did.<br />
Radiology paged my attending the<br />
following afternoon. I pulled up Jenn’s<br />
CT. She had an abscess in her back muscle,<br />
on the left, just where her pain had<br />
originated. It was large enough for a med<br />
student to see it, meaning it was pretty<br />
damn big. It was a pillowed pocket of<br />
air and fluid, indicating either active<br />
bacteria or a fistula between her bowel<br />
and back or both. Either way, the recommendation<br />
was to stick a drain in it. I<br />
remember being surprised although not<br />
alarmed. We’d stick a central line in her<br />
neck and send her home with IV antibiotics<br />
and a drain coming out of her side.<br />
She continued to appear very well—<br />
moving around her room, her pain<br />
under better control. I was shocked<br />
to see an elevated white count on her<br />
CBC. She didn’t look sick! I scheduled<br />
her with interventional radiology the<br />
following afternoon. <strong>The</strong> drain was<br />
placed without incident. That evening,<br />
I dropped by her room to say hello.<br />
She and Kat had visitors: Jenn’s sisters,<br />
brother, and niece. Jenn seemed jovial.<br />
Kat appeared more at ease than before.<br />
She even smiled when I told her goodnight.<br />
“See you tomorrow,” Jenn said. Her<br />
sister hugged me. “See you tomorrow,<br />
girlfriend,” she said.<br />
Before heading to her room the next<br />
morning, I pulled her vitals up on the<br />
computer. Her heart rate was up, all<br />
night, into the hundreds. Her most recent<br />
blood pressure read 90/60: alarmingly<br />
low. Topped with a fever of 102<br />
degrees. All signs pointed to sepsis. I<br />
could feel my own heart bump around<br />
in my chest. I could feel my fingertips<br />
and groin get numb with the anxiety of<br />
heavy failure. How could I have not seen<br />
this coming?<br />
I waited for my attending before I<br />
went to the room. I was afraid of the<br />
picture that the vitals had painted for<br />
me, and I knew that if I actually looked<br />
at her, that would only make it real. I<br />
wasn’t ready to hit that on my own.<br />
“It appears that Jenn is septic,” my<br />
attending explained to the family. <strong>The</strong>y<br />
didn’t know sepsis from a septic tank,<br />
none of them medical. But the connection<br />
between the two seemingly related<br />
entities conjured a fitting image of severity.<br />
I could see that. Kat knew best<br />
though, herself a nurse. <strong>The</strong> word softened<br />
her voice and cut deep lines in her<br />
weary face. She looked ruddy, almost<br />
hungover with sadness this morning.<br />
She knew it all along. She had been<br />
guarded, accepting our explanations and<br />
speculations throughout the admission.<br />
Carefully optimistic, but knew to call<br />
the family anyway.<br />
Looking at Jenn: she knew too. It<br />
wasn’t the pain that brought her in, I<br />
decided, looking back at it from where<br />
I was in time now. <strong>The</strong> pain had been a<br />
sign, and she knew.<br />
We asked the regular questions.<br />
“What’s your understanding of what’s<br />
going on, Jenn?” That’s my attending’s<br />
gentle voice, priming them for the<br />
events looming on the horizon.<br />
“Well, it looks like I may die.” Her<br />
frankness was killing me. I had to swallow<br />
hard and look away from her. Kat<br />
took her hand and moved to sit on her<br />
bed. She couldn’t get close enough to<br />
her. I remember feeling that way as a<br />
child, small spooning my mom in my<br />
parent’s bed at night, thinking that if I<br />
could just get closer and closer, I would<br />
be invincible. This is how Kat looked<br />
at Jenn now—like if she could just get<br />
close enough, maybe she could keep her,<br />
get away from the bad-news voices, and<br />
be invincible.<br />
Jenn was weak, intermittently trailing<br />
off, but lucid when she needed to<br />
be. In between cracking jokes about<br />
the doom in the room, she made her<br />
intentions very clear, careful always to<br />
speak in the first person, plural. Now,<br />
she was speaking for Kat, too. Jenn may<br />
have been dying, but it seemed Kat was<br />
surrendering. She asked us to stop the<br />
antibiotics.<br />
“I’m at peace, you know,” she huffed,<br />
showing her exhaustion. “Everyone is<br />
here. Kat’s here.”<br />
“She keeps twitching,” Kat said,<br />
watching Jenn’s legs worm around under<br />
the sheets.<br />
“Oh, that doesn’t bother me,” Jenn<br />
said.<br />
We ignored Jenn and started something<br />
to stop the twitching. Our focus<br />
had shifted from treating Jenn to protecting<br />
Kat. If Kat didn’t want to see<br />
twitching, then we would make it so.<br />
That was the one thing we could do for<br />
her. It made me feel a little more useful<br />
in my attempts to make up for the colossal<br />
failure I’d suffered against the natural<br />
forces that were claiming Jenn.<br />
Jenn didn’t really speak again after<br />
that. She fell into a kind of trance,<br />
sometimes restless. At those times, we<br />
gave her morphine, and she was quieted<br />
again. Her breathing was rough.<br />
We patched her with scopolamine and<br />
fentanyl.<br />
14 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
Kat claimed that she and the family<br />
were working shifts. This was a lie. <strong>The</strong><br />
family wandered in and out through<br />
the day. Kat went nowhere, sitting on<br />
the bed, feeling Jenn’s skin, placing ice<br />
packs, requesting acetaminophen suppositories<br />
to bring down Jenn’s fever.<br />
My resident told her this morning<br />
to go home for a while, get a shower, a<br />
change of clothes. Eat something. “Don’t<br />
feel guilty,” he’d told her. And she left.<br />
During her absence, I thought I’d<br />
take a break, too. Jenn was clinging to<br />
the status quo. I thought she’d make it<br />
through the weekend. I went to the cafeteria<br />
to get a soda. My pager went off<br />
about that time.<br />
Jenn’s brother and niece were sitting<br />
next to the bed. <strong>The</strong> television was off,<br />
the sun beat down on the window. It<br />
made me think it was warm outside<br />
when really, it was just a cool 60 degrees<br />
with some incidental sunlight here and<br />
there. Jenn’s face was grey, her hands<br />
still warm. I placed my stethoscope<br />
over her chest and watched the clock.<br />
<strong>The</strong> silence in her chest was eerie. <strong>The</strong><br />
Owl, symbol of Athens, reverse of<br />
a silver tetradrachm from Athens. © Corbis.<br />
sixty seconds were long and made me<br />
very aware of the pain in my back from<br />
bending over. Kat hadn’t made it back<br />
yet, but she had just called. It was one<br />
o’clock.<br />
“Is she gone?” She asked Jenn’s niece<br />
without being prompted.<br />
“She’s in heaven now,” her niece<br />
whispered as we performed our rituals.<br />
Maybe it brought her some comfort to<br />
say that.<br />
I Googled her name until her obituary<br />
was finally posted. It took the family<br />
over a week to put her in the ground.<br />
Until that time, I knew that Kat must<br />
have been surrounded by Jenn’s family<br />
coming in and out, strangers sending<br />
things like flowers and meat trays. I<br />
decided I would give her a call a couple<br />
days after the funeral. I know from<br />
my own experience that that’s when<br />
the mourning will start—when the<br />
crowds quiet down, and Kat is left to<br />
pick through Jenn’s closet, sleep in the<br />
sheets that smell like her, throw out<br />
the pill bottles that litter her cabinets,<br />
dispose of the relics that documented<br />
the presence of her and the life they’d<br />
built together. She’d be stuck wondering<br />
if she should dispose of everything that<br />
made the longing burn fresh or worry<br />
about whether it would make her forget<br />
something sacred about them. An old<br />
shirt, a matchbook, a used pencil, a half<br />
eaten sandwich. She’d want to reach out<br />
to someone to help her decide what to<br />
keep and realize that her habit for years<br />
now was to reach for Jenn.<br />
“I just wanted you to know that your<br />
relationship is really inspiring.” This was<br />
a couple hours before Jenn’s death when<br />
I found Kat in the room by herself. She<br />
cried. I think it was something that had<br />
built up for a while, and now she just<br />
couldn’t control it.<br />
“Twelve years is just not enough,” she<br />
said, sniffing and shaking her sore, red<br />
face, “but, you know, fifty wouldn’t have<br />
been enough.”<br />
<strong>The</strong> author’s address is:<br />
4249 West Sarah Street<br />
Burbank, California 91505<br />
E-mail: susielisa@gmail.com<br />
Musings on an Attic Tetradrachm<br />
What hands are these that stamped wide-eyed<br />
Owls on rounds of Laurian silver,<br />
And whose knives are those who carved<br />
Humanity on blocks of solid stone?<br />
What artist’s brush has painted antic<br />
Nymphs on urns of reddened clay,<br />
And whose minds are they who plumbed<br />
So deep within the human soul?<br />
Whose book is this which tells such tales of<br />
Bloody death on ancient Trojan shores,<br />
What princely youth has led his men<br />
To trample vast miles of Asian soil?<br />
And which men with their lines and angles<br />
First measured the circumference of the Earth?<br />
Now seek ye out the Olympian gods,<br />
And as the Delphic Sybil nods,<br />
Athena’s owl will tell you Who<br />
Alvin J. Cummins, MD<br />
Dr. Cummins (AΩA, Johns Hopkins University, 1944) is retired as professor of Medicine at the<br />
University of Tennesseee Center for the Health Sciences in Memphis. His address is: 13114 Brooks<br />
Landing Place, Carmel, Indiana 46033. E-mail: nero6@aol.com.<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 15
��������<br />
Victim testifies at the Nuremberg Trials. <strong>The</strong> Doctors Trial<br />
considered the fate of twenty-three German physicians who<br />
either participated in the Nazi program to euthanize persons<br />
or who conducted experiments on concentration camp prisoners<br />
without their consent. Sixteen of the doctors charged<br />
were found guilty. Seven were executed.<br />
16 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong><br />
© dpa/dpa/Corbis
����<br />
Political violence and the physician<br />
Amanda J. Redig, MD, PhD<br />
<strong>The</strong> author (AΩA, Northwestern University, 2010) is a<br />
resident in the Department of Medicine at Brigham and<br />
Women’s Hospital in Boston. This essay won second prize<br />
in the 2010 Helen H. Glaser Student Essay Competition.<br />
Human health in the early days of a new millennium<br />
stands at the crossroads of a paradox: thanks to a vast<br />
increase in knowledge and technology, we are more<br />
effective than ever before in both the saving and the taking of<br />
lives. Indeed, the twentieth century is characterized by two<br />
incongruous realities. On the one hand, we have the hope and<br />
optimism generated by groundbreaking strides against the suffering<br />
caused by disease. Yet coupled to such progress is the<br />
dark legacy of genocide, war, and political violence on a scale<br />
previously unimaginable. What makes reconciling these two<br />
competing visions so difficult for the medical profession is the<br />
fact that physicians have been instrumental in advancing not<br />
only the achievements but also the atrocities.<br />
Decades after their deaths, physicians such as Jonas Salk<br />
or Alexander Fleming remain household names because of<br />
the effect their work has had on the advancement of medicine’s<br />
ability to heal. In contrast, there are also physicians<br />
whose names have become synonymous with the very worst<br />
of humanity, such as the “Angel of Death,” Dr. Josef Mengele.<br />
Fortunately, there are far more famous than infamous physicians,<br />
but no matter how much the medical profession may<br />
wish to think otherwise, the physician who chooses to embrace<br />
death over life is not an anomaly.<br />
<strong>The</strong> list of physicians who have participated in and furthered<br />
political violence is extensive. Nazi physicians directed<br />
the mass murder of the weak, the ill, and the disabled in 1930s<br />
Germany, as well as the horrific medical experiments of Nazi<br />
World War II concentration camps. Japan’s World War II<br />
Project 731, led by Dr. Shiro<br />
Ishii, killed thousands of POWs<br />
and Chinese and Soviet citizens<br />
in experiments on germ warfare<br />
and vivisection. Among other<br />
historic firsts, including leadership<br />
of the first organization<br />
to use hijacked airliners as a<br />
political tool, Palestinian pediatrician<br />
George Habash was also<br />
responsible for orchestrating a<br />
rocket attack on a bus full of<br />
children in which nine passen-<br />
Major Nidal Hasan<br />
HO/Reuters/Corbis<br />
gers died. Out of the violence that turned neighbor against<br />
neighbor in the former Yugoslavia, psychiatrist Radovan<br />
Karadzic is currently standing trial in the Hague for his role<br />
in the massacre of Bosnian Muslims at Srebenica and the<br />
Siege of Sarajevo. Al-Qaeda counts numerous physicians as<br />
operatives, from number two Ayman al-Zawahiri to the individuals<br />
responsible for the failed suicide bombing at Glasgow<br />
International Airport in 2007. Most recently, Fort Hood<br />
psychiatrist Major Nidal Hasan was responsible for the worst<br />
attack of terrorism on a domestic U.S. military installation in<br />
American history.<br />
Clearly, incongruity aside, physicians are not exempt from<br />
participation in the most chilling of crimes against humanity.<br />
Despite the repugnance with which most physicians view<br />
such actions on the part of their colleagues, the fact remains<br />
that politically-motivated violence perpetrated by physicians<br />
happens far too often, across all lines of politics, religion,<br />
and ethnicity. <strong>The</strong> questions to be asked are thus far more<br />
complex than whether or not a profession built on the best of<br />
intentions can exist side by side with great evil. Instead, the<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 17
<strong>The</strong> monsters of medicine<br />
medical profession must face far more nuanced questions that<br />
are much more difficult to answer. Why do some physicians<br />
act as if some lives have no value? What do their actions mean<br />
for those choosing instead to live by primum non nocere? It<br />
is too simplistic to dismiss the Mengeles and al-Zawahiris<br />
among us as either terrorists or sociopaths. <strong>The</strong> medical profession<br />
needs to go through the potentially painful process<br />
of looking inward to recognize both its unique strengths and<br />
weaknesses. After all, we remember the names of medicine’s<br />
most infamous members not because of their heinous deeds<br />
but rather because such actions were carried out by doctors.<br />
Consequently, we must look more closely at the roots of terrorism<br />
and state-led violence to understand both the physicians<br />
who embrace them, as well as those who do not.*<br />
Internal pressure: surely they must be mad<br />
<strong>The</strong> first explanation often used to make sense of physician<br />
violence is mental illness. <strong>The</strong> gulf that divides what a physician<br />
is supposed to do and what some physicians have done is<br />
so vast that it is not surprising we question the sanity of those<br />
we cannot understand. <strong>The</strong> sociopathy defense provides society—and<br />
especially the medical community—with a mental<br />
escape from the possibility that a sane individual, someone<br />
who could be any of us, would willingly engage in such horrors.<br />
At a superficial level, this initial impression seems accurate<br />
as a way of explaining aspects of both barbarism that<br />
defies words and actions that are so contradictory they cannot<br />
be reconciled. <strong>The</strong> Holocaust and the campaign in the Pacific<br />
are among the most extensively analyzed and referenced topics<br />
in the historical literature,<br />
yet the details of the medical<br />
torture that took thousands of<br />
lives still remain in the shadows.<br />
<strong>The</strong> thought of physicians<br />
removing organs or limbs from<br />
live patients without anesthesia,<br />
spinning people in centrifuges<br />
until they died, or using prisoners<br />
tied to posts to test the efficacy<br />
of flame-throwing devices<br />
stand apart as too horrific to<br />
contemplate. And what could be<br />
more contradictory than an individual<br />
who chooses a career as a<br />
physician and then participates<br />
Dr. Josef Mengele<br />
© Bettmann/CORBIS<br />
in political violence? Several of<br />
the physicians implicated in the<br />
* In this paper “terrorism” refers to Paul Wilkinson’s definition of<br />
“violence or the threat of violence,” here used primarily in reference<br />
to non-state actors. 1 “State-led violence” is used for similar actions,<br />
specifically war crimes and genocide, orchestrated by state actors.<br />
<strong>The</strong> word “violence” is used exclusively to refer to actions that have<br />
an underlying political nature, regardless of the organizational level<br />
at which such goals are pursued.<br />
Glasgow International Airport suicide<br />
bombing plot were not only<br />
practicing medicine at the time<br />
but were also living among the<br />
very people they were attempting<br />
to destroy. <strong>The</strong> duality of treating<br />
one’s neighbors by day and plotting<br />
to blow them up at night makes no<br />
sense. Even though Major Nidal<br />
Hasan’s trial has not yet begun, it<br />
is assumed that he will use an insanity<br />
defense because his actions<br />
are so at odds with his professional<br />
career. <strong>The</strong> DSM-IV definition of<br />
antisocial personality disorder—<br />
the preferred way of referencing<br />
the sociopath of common usage—<br />
Dr. Ayman al-Zawahiri<br />
AFP/Getty Images<br />
includes at its core a lack of regard for the rights of others. 2<br />
In this sense, at least, the actions of such infamous physicians<br />
seem to fit.<br />
Yet, a closer examination of the actions of these physicians<br />
makes it clear that mental illness does not explain their atrocities.<br />
<strong>The</strong> DSM definition of antisocial personality disorder<br />
is far more complex than the superficial understanding of a<br />
person who does the unthinkable; it also includes several essential<br />
criteria, starting with a pervasive pattern of disregard<br />
for and violation of the rights of others occurring since the age<br />
of fifteen. 2 Patients with this disorder must also meet three (or<br />
more) of the following:<br />
1. failure to conform to social norms with respect to lawful<br />
behaviors as indicated by repeatedly performing acts that<br />
are grounds for arrest<br />
2. deceitfulness, as indicated by repeated lying, use of<br />
aliases, or conning others for personal profit or pleasure<br />
3. irritability and aggressiveness, as indicated by repeated<br />
physical fights or assaults<br />
4. reckless disregard for safety of self or others<br />
5. consistent irresponsibility, as indicated by repeated<br />
failure to sustain consistent work behavior or honor financial<br />
obligations<br />
6. lack of remorse, as indicated by being indifferent<br />
to or rationalizing having hurt, mistreated, or stolen from<br />
another. 2<br />
This more nuanced pattern does not entirely fit any of the<br />
physicians whose crimes the profession would like to forget.<br />
<strong>The</strong> very act of choosing a career in medicine and completing<br />
medical school makes psychopathology at a level that<br />
encompasses mass murder untenable. Medicine is a profession<br />
entered as an adult with extensive emphasis on social norms<br />
and regulated, responsible behavior, and for which consistency<br />
in meeting numerous obligations is essential. While it<br />
is clear that something is grievously wrong with physicians<br />
like Mengele and his ilk, attributing even the most despotic<br />
18 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
Dr. Karl Brandt at the Nuremberg trial.<br />
© dpa/Corbis<br />
of actions solely to psychiatric disease misses an essential, if<br />
unsettling, element of the dark side of physician behavior: they<br />
were once just like us.<br />
Nazi physician Karl Brandt was the director of the T-4<br />
euthanasia program that murdered thousands of Germans<br />
before it became the inspiration for the gas chambers of the<br />
death camps. At his trial at Nuremberg, Brandt said this:<br />
Would you believe that it was a pleasure to me to receive<br />
the order to start euthanasia? For fifteen years I had<br />
laboured at the sick-bed and every patient was to me like a<br />
brother, every sick child I worried about as if it had been my<br />
own. . . . With the deepest devotion I have tortured myself<br />
again and again, but no philosophy or other wisdom helped<br />
here. <strong>The</strong>re was the decree and on it there was my name. 3<br />
Before his execution by hanging, Brandt offered himself as<br />
the subject for medical experimentation. 3 His offer was rejected,<br />
but both his words and actions speak to the guilt and<br />
conflicted emotions of an individual who is clearly tormented,<br />
yet hardly insane. A trial with similar charges is set to start<br />
in March 2010, as Radovan Karadzic will have to answer for<br />
his role in orchestrating the slaughter of Bosnia’s Muslims.<br />
Karadzic has thus far refused to cooperate in his own defense,<br />
but the details of his evasion from capture for over a decade<br />
speak volumes. After he was apprehended, a New York Times<br />
profile sought out those who knew Karadzic as New Age<br />
healer Dragan Dabic. 4 Although most acknowledged the eccentricity<br />
of their new neighbor, no one made the connection<br />
between the bearded alternative medicine guru and the man<br />
once known as the Beast of Bosnia.<br />
When daylight came, Goran Kojic, the Healthy Life<br />
editor, wanted to talk one more time. He seemed the most<br />
troubled by the unresolvable contradictions of his recent<br />
life. Was the pose of gentle spiritualist a complete fake and a<br />
cover for a soul darkly outed as hideous, violent and bestial?<br />
Or was there some truth to Dabic’s character?<br />
“<strong>The</strong>re are two options,” said Kojic, cautiously, hesitantly,<br />
as if he were speaking for a nation. “Either we are all a bunch<br />
About the author<br />
I studied biochemistry and creative<br />
writing at the University of Arizona before<br />
enrolling in the medical scientist training<br />
program at Northwestern University.<br />
While in Chicago, I completed my PhD<br />
in cancer biology and graduated with the<br />
Feinberg School of Medicine Class of 2010. I am currently<br />
a resident in Internal Medicine at the Brigham<br />
and Women’s Hospital in Boston and plan to pursue a<br />
career as an oncologist. Interests include translational<br />
research but also medical humanities/narrative and<br />
health/science policy. I have been an online contributor<br />
to the Virginia Quarterly Review and have had medical<br />
narratives featured in the Journal of the American<br />
Medical Association and Health Affairs.<br />
of fools and madmen who believed<br />
in the existence of a nonexistent<br />
man.” Or, he said, there<br />
is the possibility of redemption. 4<br />
Those with personal knowledge of<br />
both Karadzic himself and the carnage<br />
he caused are unable to separate<br />
the threads of his identity. We<br />
do not have similar commentary<br />
from those who personally knew<br />
physician-suicide bombers, but<br />
these individuals did not live the<br />
life of the criminally insane. <strong>The</strong>y<br />
worked as physicians; some had<br />
families. Clearly, physicians who<br />
participate in political violence<br />
Dr. Radovan Karadzic<br />
© dpa/Corbis<br />
share the undeniable trait of humanity gone horribly awry, but<br />
this truth provides neither a final answer nor an excuse for the<br />
medical profession to settle for such an oversimplification.<br />
External pressure: the genuine grievance theory<br />
Another common explanation rationalizing physician<br />
atrocities on behalf of state or non-state actors is terrorism.<br />
Recasting the actions of certain physicians as rank-and-file<br />
terrorists can mask the need to probe the healer/destroyer<br />
dichotomy. Physician. Terrorist. What more need be said?<br />
Even though physicians spearheaded the establishment of<br />
many of the most violent terrorist groups in the Middle East<br />
in the 1960s and ’70s, their paradoxical role is rarely examined.<br />
Physician George Habash graduated from the American<br />
University of Beirut before he started the Popular Front for<br />
the Liberation of Palestine. 5 His political colleague and former<br />
medical school classmate, Dr. Wadih Haddid, 5 is the mastermind<br />
behind the hijacking of commercial airliners even before<br />
the horrors of September 11, 2001. Islamic Jihad was founded<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 19
<strong>The</strong> monsters of medicine<br />
Dr. George Habash<br />
© Bettmann/CORBIS<br />
Dr. Ikuo Hayashi<br />
AFP/Getty Images<br />
Dr. Wadih Haddid<br />
© Bettmann/CORBIS<br />
by yet another physician,<br />
Dr. Fathi Shiqaqi. 6 <strong>The</strong> Aum<br />
Shinrikyo sarin nerve gas attack<br />
on the Tokyo subway<br />
that made headlines around<br />
the globe probably would<br />
not have succeeded without<br />
the involvement of Dr. Ikuo<br />
Hayashi, a one-time rising<br />
star at the Japanese Ministry<br />
of Science and Technology. 7<br />
Even with the series of al-<br />
Qaeda-associated bombings<br />
perpetrated by physicians<br />
over the last five years from<br />
Glasgow in 2007 to Jordan<br />
in 2009, nearly all analyses of the attacks’ significance focus<br />
on the development and re-structuring of al-Qaeda tactics,<br />
not the startling (or so one would think) observation that<br />
physicians are so openly participating. <strong>The</strong> evidence is clear<br />
that the physician-terrorist is far from a unique construct, yet<br />
rather than explore this puzzling reality, in a leap of circular<br />
reasoning, the existence of such a duality has itself become a<br />
substitute explanation for it.<br />
Unfortunately, this approach also draws the medical community<br />
into acknowledging elements of the genuine grievance<br />
theory in an attempt to understand the unthinkable. While<br />
this perspective represents an important first step in any rootcause<br />
analysis, it may also legitimize terrorist acts. During a<br />
time in which the Palestinian cause was inextricably linked<br />
to violence targeting civilians, Yasser Arafat stood before the<br />
United Nations General Assembly and stated: “<strong>The</strong> difference<br />
between the revolutionary and the terrorist lies in the reason<br />
for which each fights. For whoever stands by a just cause . . .<br />
cannot possibly be called terrorist.” 8 His words are shocking,<br />
but they are also an uncanny echo of Menachem Begin, who<br />
wrote twenty years before: “the ideal is the important thing,<br />
not the man.” 9<br />
It is this seeming connection of the almost universally<br />
accepted ideal of freedom with terrorism that has led to the<br />
maxim: “Terrorism appears whenever people have genuine,<br />
legitimate grievances. Remove the grievances and terror will<br />
cease. Like all good lies, this statement cloaks itself in an<br />
almost-convincing mantle of truth. Indeed, an analysis of the<br />
personal lives of so-called physician-terrorists reveals more<br />
than one connection to some of the most turbulent events of<br />
recent history. George Habash and Wadih Haddid were young<br />
medical students when their families lost everything to the<br />
fledgling Israeli Army of 1948. 5 <strong>The</strong> desperation and suffering<br />
endured by generations of Palestinians living without hope or<br />
a future is a powerful stimulus for many elements of organized<br />
terror, both past and present. <strong>The</strong> same struggle for national<br />
independence can be seen at the root of the conflicts involving<br />
Algeria and the FLN, or Ireland and the IRA. Although not as<br />
direct a correlation, al-Qaeda propaganda uses the suffering of<br />
Muslim civilians in the Middle East as a powerful recruiting<br />
tool for many who have not themselves lived through the horrors,<br />
including physicians.<br />
But despite an accurate recognition of the value of justice<br />
and the unfortunate historical reality of injustice, the arguments<br />
forming the genuine grievance theory are based on a logic that<br />
is both unsound and a precept the medical profession should<br />
never accept as an explanation for the troubling existence of the<br />
physician-terrorist. Those who turn to terror undermine their<br />
own cause by denying the meaning and universality of the very<br />
principles to which they appeal. Even the most cherished ideals<br />
of freedom and self-determination cannot be used to legitimize<br />
a cause that only applies them in one direction. This is part of<br />
what makes the individual who wields a stethoscope in one hand<br />
and a bomb in the other so difficult to comprehend. Medicine<br />
as a profession is based on helping all those in need, a principle<br />
��������������������������������<br />
�����<br />
������������������������������������<br />
—Yasser Arafat<br />
������������������������<br />
�<br />
������������<br />
—Menachem Begin<br />
enshrined in one form or another in medical oaths spanning<br />
both geography and time. <strong>The</strong> Hippocratic Oath and its injunction<br />
to “first do no harm” is most familiar to the Western world,<br />
20 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
ut this concept is a universal one, paralleling the evolution of<br />
the physician as an individual with a unique and honored calling.<br />
<strong>The</strong> Charaka Samhita is an ancient Sanskrit text dating to<br />
the third century BCE which states, “Day and night, however<br />
thou mayest be engaged, thou shalt endeavor for the relief of<br />
patients with all thy heart and soul.” 10 What is thus so troubling<br />
for the medical profession is that one of its members could fully<br />
accept the responsibility of the physician but only as applied<br />
to a few select persons. Whatever the supposed grievance, the<br />
terrorist attempts to hide behind moral relativism even while<br />
claiming a monopoly on moral superiority, as in Yasser Arafat’s<br />
reference to Abu Nidal as “a real terrorist” after Nidal’s nearsuccessful<br />
assassination attempt against the PLO leader. 11 <strong>The</strong><br />
hypocrisy of any attempt to cling to a moral code one has shown<br />
no compunction in violating underscores the vital role that ethics<br />
plays in any analysis of terrorism, especially that perpetrated<br />
by physicians.<br />
And this is the second point the medical profession must<br />
acknowledge as we attempt to first understand and then prevent<br />
the actions of those who claim our calling but reject our<br />
creed. <strong>The</strong> justification used by physicians who take life to advance<br />
political goals—whether acting on behalf of the state or<br />
non-state actors—is unmistakably a moral decision that must<br />
be recognized as such before it can ever be rejected. Both religious<br />
and secular terrorists, as well as those acting on behalf<br />
of the state in cases of genocide, provide moral justification for<br />
their actions in a way that clearly rejects the universal value<br />
of individual human life that is at the heart of medicine. <strong>The</strong><br />
writings of Carlos Marighella have been translated into over<br />
a dozen languages and discovered in more than one hundred<br />
terrorist safe houses throughout the world; his Minimanual<br />
of the Urban Guerrilla states, “the urban guerrilla’s arms are<br />
inferior to the enemy’s, but from a moral point of view, the<br />
urban guerrilla has an undeniable superiority.” 12 <strong>The</strong> most<br />
important significance of this work for such a broad range of<br />
organizations lies in the conclusions that equate the legitimacy<br />
of a cause with the methods used to achieve it. This codified<br />
morality for the actions of a terrorist is one in which human<br />
life is not respected. His words horrify, yet it should not be<br />
surprising that upon learning his bomb destroyed German<br />
instead of Israeli tourists, the bombmaker responded, “Infidels<br />
are all the same.” 13 <strong>The</strong> difficulties in establishing a working<br />
definition of terrorism and even the use of the word as a<br />
descriptive label imply a moral judgment that can be used to<br />
wage a war of semantics against unwanted political behavior.<br />
But despite legitimate definitional challenges, the conscious<br />
choice to take life in defiance of the profession that stands<br />
for saving it is a moral decision framed by a rejection of the<br />
fundamental worth of the individual. It is only in recognizing<br />
this fact that the medical community can ask the difficult<br />
questions about itself that must be the first steps towards any<br />
attempt to combat such actions by physicians.<br />
Moving forward<br />
Reframing the infamous physicians as one who chooses to<br />
devalue human life—regardless of confounding psychiatric<br />
or political factors—raises two compelling questions for the<br />
medical profession with implications at the practical level.<br />
First, is there something about medical training that can<br />
lead to some physicians rejecting the value of human life?<br />
While the overarching values of the medical profession say<br />
absolutely not, a closer analysis of the day-to-day process of<br />
becoming a physician and practicing medicine suggests otherwise.<br />
From the very beginning of medical school, the training<br />
process demands would-be physicians put aside some of<br />
their most basic human instincts. As human beings, we draw<br />
away from death, from blood, from suffering, yet medical<br />
training demands that we embrace and sometimes even cause<br />
all of the above. What starts in the cadaver lab extends to the<br />
surgical theater, the chemotherapy clinic, and the radiation<br />
suite. <strong>The</strong> goal of practicing medicine is to support life, but<br />
in the process of doing so, physicians nonetheless act in a way<br />
that in any other setting would be unthinkable: we take knives<br />
to flesh, administer the deadliest of toxins, direct radiation to<br />
permanent harm. In other settings, each of these activities<br />
has been the basis for charges of crimes against humanity. In<br />
many settings, transplant surgery or experimental protocols<br />
among them, physicians can take on the role that throughout<br />
history has traditionally been granted only to God: determining<br />
who lives and who dies. <strong>The</strong> regulation of clinical trials<br />
and human experimentation has undergone dramatic development<br />
throughout the last decades, but even with the deep<br />
scrutiny of today’s IRB committees the role of directly experimenting<br />
on human subjects is an established part of modern<br />
medicine. No amount of preclinical development and testing<br />
can take away the fact that the goal of Phase I clinical trials is<br />
to identify toxicities in a human population.<br />
Clearly, most physicians complete their medical training<br />
without following the twisted path of one who uses it to<br />
destroy rather than heal. Yet the fact remains that a career in<br />
medicine forces one to confront questions of life, death, suffering,<br />
and healing at a level of intimacy that no other profession<br />
can match. Ironically, it is spiritual leaders who likely come the<br />
closest, and the relationship between organized religion and<br />
political violence needs no further elaboration here. In the setting<br />
of medical training, then, both the events of the past and<br />
the developments of today suggest that physicians—like those<br />
from any background of deep ideological convictions—may be<br />
vulnerable to radicalizing influences not in spite of their training<br />
but perhaps because of it. While this is a sobering reality<br />
to consider, it is also one that offers the promise of change.<br />
Medical training has undergone a remarkable transformation<br />
over the last decades, with an emphasis on ethics and professionalism<br />
in medical education as never before. We already<br />
have the tools to strengthen our commitment to respecting<br />
the humanity and dignity of all who cross our path—the challenge<br />
now before us is how best to utilize them. Just as an individual<br />
physician makes the choice about where her deepest<br />
allegiance lies, so too can the medical profession.<br />
This, in turn, raises a related point that can be all the more<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 21
<strong>The</strong> monsters of medicine<br />
difficult to recognize for its subtlety. Any discussion of political<br />
violence, war crimes, and terrorism must emphasize the deep<br />
ideological fervor of participants that permits participation in<br />
atrocities. But convictions of even the most deeply-held principles<br />
are in themselves neutral entities; only in their application<br />
do we truly see what an individual has chosen to reject or<br />
embrace. For every physician who joins the medical profession<br />
with a deep faith in a given principle only to emerge a monster,<br />
there are far more who use their values to shape a commitment<br />
to medicine into something of profound inspiration. Most telling<br />
of all, the potential for making positive rather than negative<br />
contributions can be seen in medical organizations that cut<br />
across the spectrum of religious and secular beliefs. <strong>The</strong> stated<br />
mission of Physicians for Human Rights is to “[mobilize] health<br />
professionals to advance health, dignity, and justice.” 14 For the<br />
strength of this commitment and its real-world application,<br />
the organization shared the 1997 Nobel Peace Prize. Two years<br />
later, Doctors without Borders, an organization “based on the<br />
humanitarian principles of medical ethics and impartiality”<br />
was recognized with this same award. 15 Furthermore, deep<br />
spiritual convictions do not automatically translate to fundamentalist<br />
hate. In this context, consider the example of the mission<br />
statements of the Islamic Medical Association of North<br />
America (IMANA) and the Christian Medical and Dental<br />
Association (CMDA). Both acknowledge the fundamental role<br />
of the Islamic or Christian faith, respectively, in the lives of<br />
their members. Both incorporate spiritual beliefs that are only<br />
accepted by members of their distinct faiths. Yet it is the deep<br />
and abiding respect for life on spiritual grounds in conjunction<br />
with a professional calling to medicine that also brings both<br />
organizations to a conclusion utterly repudiating the actions of<br />
those who claim a spiritual heritage to legitimize acts of great<br />
evil. <strong>The</strong> IMANA mission statement concludes with this verse<br />
from the Qur’an: “If anyone has killed one person (except in<br />
lieu of murder or mischief on earth) it is as if he has killed the<br />
whole of mankind, and if he has saved one life it is as if he saved<br />
the whole of mankind.” 16 <strong>The</strong> CMDA mission statement indicates<br />
that the organization exists to equip Christian physicians<br />
to, “pursue professional competence and Christ-like compassion<br />
in their daily work.” 17 <strong>The</strong> inspiration for such compassion<br />
is this injunction from the gospel of Mathew: “You shall love<br />
your neighbor as yourself.” 18<br />
It is these words—and others like them—that represent the<br />
true challenge facing the medical profession as we continue<br />
to struggle with the paradox of physicians who both heal and<br />
destroy. As a profession, we must understand our heritage and<br />
walk the very fine line of respecting the personal differences<br />
among us while refusing to compromise on the moral integrity<br />
on which medicine is based. We must challenge ourselves to<br />
treat all equally. We must recognize that principle always has<br />
a place in argument even while acknowledging that principles<br />
themselves can be hijacked and used to justify heinous acts of<br />
violence. In short, we must be physicians, first and always, but<br />
we must also be physicians who live in the real world and never<br />
lose sight of any opportunity—from improving medical education<br />
to supporting humanitarian medical aid—to emphasize<br />
the uncompromising foundation of respect for humanity on<br />
which our profession is built. This approach will not remove<br />
every threat to the integrity of the physician posed by political<br />
violence, but it does provide a place to start from the only<br />
perspective that matters: one life at a time.<br />
References<br />
1. Wilkinson P. Terrorism and the Liberal State. Second edition.<br />
New York: New York University Press; 1986.<br />
2. American Psychiatric Association. DSM-IV-TR Diagnostic<br />
Criteria for Antisocial Personality Disorder (301.y). In: Diagnostic<br />
and Statistical Manual of Mental Disorders. Fourth edition. Washington<br />
(DC): American Psychiatric Association; 1994.<br />
3. Spartacus Educational web site. Karl Brandt. www.spartacus.<br />
schoolnet.co.uk/GERbrandtK.htm.<br />
4. Hitt J. Radovan Karadzic’s new-age adventure. New<br />
York Times 2009 Jul 22. www.nytimes.com/2009/07/26/<br />
magazine/26karadzic-t.html.<br />
5. Habash G, Soueid M. Interview: Taking stock: An interview<br />
with George Habash. J Palestinian Stud 1998; 28: 86–101.<br />
6. Greenberg J. Islamic group vows revenge for slaying<br />
of its leader. New York Times 1995 Oct 30: A9. www.nytimes.<br />
com/1995/10/30/world/islamic-group-vows-revenge-for-slaying-ofits-leaders.html.<br />
7. Murakami H. Underground: <strong>The</strong> Tokyo Gas Attack and the<br />
Japanese Psyche. New York: Vintage; 2001.<br />
8. Richardson L. What Terrorists Want: Understanding the<br />
Enemy, Containing the Threat. New York: Random House; 2007.<br />
9. Laqueur W, editor. <strong>The</strong> Terrorism Reader: A Historical Anthology.<br />
New York: New American Library; 1978.<br />
10. Menon LA, Haberman HF. <strong>The</strong> medical students’ oath of<br />
ancient India. Med Hist 1970; 14: 295–99.<br />
11. Harmon C. Terrorism Today. London: Frank Cass; 2000: 191.<br />
12. Marighella C. Minimanual of the urban guerrilla. New World<br />
Liberation Front; 1970.<br />
13. Hoffman B. Inside Terrorism. New York: Columbia University<br />
Press; 1998: 168.<br />
14. Physicians for Human Rights web site. About PHR. physiciansforhumanrights.org/about/.<br />
15. Doctors Without Borders web site. About Us—History and<br />
Principles. www.doctorswithoutborders.org/aboutus/.<br />
16. Islamic Medical Association of North America web site. Mission<br />
and Vision. www.imana.org/index.php?option=com_content&v<br />
iew=article&id=196&Itemid=65.<br />
17. Christian Medical and Dental Association web site. Mission<br />
& Beliefs. www.cmda.org/WCM/CMDA/Navigation/About/MissionsBeliefs/Missions_Beliefs.aspx.<br />
18. <strong>The</strong> Holy Bible Containing the Old and New Testaments<br />
New King James Version. Nashville (TN): Thomas Nelson Publishers;<br />
1982: 873.<br />
<strong>The</strong> author’s e-mail is: aredig@partners.org<br />
22 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
Sestina on Limb-Lengthening<br />
Surgery<br />
John’s father was a famous novelist,<br />
his mom a musical sensation. In short,<br />
John was born with two silver spoons in mouth.<br />
A bright boy, he sailed through Harvard, then<br />
demonstrated<br />
valor in the Horn of Africa. A great<br />
career in politics awaited; the only<br />
obstacle was John’s stature: he was only<br />
five-foot-two, puny as a sapling that lists<br />
whichever way the wind blows. For a great<br />
price, John secured the services of a shortspoken<br />
but skilled cosmetic surgeon, who operated<br />
on John’s bones to make him taller, so his mouth<br />
could speechify from a loftier place. <strong>The</strong> mouth<br />
of conventional wisdom says that only<br />
females are vain, preening in front of crenellated<br />
mirror frames, making lengthy shopping lists<br />
of perfumes, lipsticks, skirts, and shorts;<br />
but masculine vanity is no less great.<br />
My friend Millie, whose voice is apt to grate,<br />
but who has pretty eyes and a sweet mouth,<br />
helped me see why this is the long-and-short<br />
of the matter. She tells me that she only<br />
dates boys who are at least five-foot-ten, lest<br />
their offspring’s height be too modest, too understated.<br />
Where prejudices of this kind are indurated,<br />
it’s no surprise that male vanity is great.<br />
<strong>The</strong> man I date, the man who tops the list<br />
of men in my life, with his honest mouth<br />
says that his brothers tower over him only<br />
because he is a twin: he has been short<br />
ever since he, together with his short<br />
sister, inhabited their mom’s trabeculated<br />
womb. He regrets his shortness, saying, “If only<br />
I were taller . . . ,” while the fire in the grate<br />
backlights the beauty of his face; his mouth,<br />
nose, eyes all vie for which is loveliest<br />
to me. My stammering mouth replies at last,<br />
“My patient, John, could have been great if only<br />
a complicated surgery hadn’t cut his life short.”<br />
Jenna Le<br />
Ms. Le is a member of the Class of 2010 at the Columbia University<br />
College of Physicians and Surgeons. This poem won first prize in the 2010<br />
<strong>Pharos</strong> Poetry Competition. Ms. Le’s e-mail address is: jenna.le@gmail.com.<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 23
Dean Gianakos, MD<br />
B������������<br />
What poetry has to say about it<br />
<strong>The</strong> author is the associate director of the Lynchburg Family<br />
Medicine Residency in Lynchburg, Virginia, and a member<br />
of the editorial board of <strong>The</strong> <strong>Pharos</strong>.<br />
Breaking bad news to patients is difficult. Even experienced<br />
physicians struggle to do it competently. Until<br />
recently, it’s a skill that has received little attention<br />
in medical schools, residencies, and fellowship training programs.<br />
1 <strong>The</strong>re is scant evidence on how to do it well. 2,3 Most<br />
articles on the subject refer to certain steps that may be helpful:<br />
create a comfortable setting for patients and families; find<br />
out what patients know about their condition; ask them how<br />
much they desire to know; deliver the news in a clear, concise<br />
fashion; show empathy; be prepared to respond to various<br />
reactions to the news—sadness, denial, anger, or guilt; and,<br />
finally, summarize and outline a plan for the patient. 3–5<br />
Experience, frequent practice, coaching from mentors,<br />
and reviewing the medical literature are traditional ways to<br />
improve one’s ability to deliver bad news. I believe reading<br />
poetry is another way: reading poems with care and empathy<br />
fosters an appreciation of the importance of language, feelings,<br />
and nuance in communication and relationships. Raymond<br />
Carver’s poem, “What <strong>The</strong> Doctor Said,” offers insights into<br />
patient-physician relationships not found in other forms of<br />
instruction. In this poem, Carver shows how difficult, frightening,<br />
and awkward (for the patient and physician) delivering<br />
and receiving bad news can be:<br />
He said it doesn’t look good<br />
he said it looks bad in fact real bad<br />
he said I counted thirty-two of them on one lung before<br />
I quit counting them<br />
I said I’m glad I wouldn’t want to know<br />
about any more being there than that<br />
he said are you a religious man do you kneel down<br />
in forest groves and let yourself ask for help<br />
when you come to a waterfall<br />
mist blowing against your face and arms<br />
do you stop and ask for understanding at those moments<br />
I said not yet but I intend to start today<br />
he said I’m real sorry he said<br />
I wish I had some other kind of news to give you<br />
I said Amen and he said something else<br />
I didn’t catch and not knowing what else to do<br />
and not wanting him to have to repeat it<br />
and me to have to fully digest it<br />
I just looked at him<br />
for a minute and he looked back it was then<br />
I jumped up and shook hands with this man who’d just given<br />
me<br />
something no one else on earth had ever given me<br />
I may have even thanked him habit being so strong 6<br />
<strong>The</strong> doctor in the poem botches it—badly. 7 In his first<br />
attempt to deliver the news, he tries a detached, scientific approach:<br />
he counts. Not only does he count the nodules; he reports<br />
the number to the patient—the number before he stops<br />
counting. Ten, twenty, or thirty-two nodules—what clinical<br />
difference does it make? <strong>The</strong>n he resorts to quasi-religious,<br />
poetic imagery: “do you kneel down in forest groves and let<br />
yourself ask for help when you come to a waterfall, mist blowing<br />
against your face and arms.” I’m fine with asking patients<br />
if they are religious, but does anyone want this question after<br />
being told they have more than “thirty-two of them on one<br />
lung”?<br />
24 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
<strong>The</strong> truth is, most of us blunder from time to time, no<br />
matter how experienced we are in communicating serious<br />
news. We come prepared with the words that soothe—“this<br />
must be very difficult for you; I cannot imagine how you must<br />
feel”—only to utter stupid, insensitive things. And sometimes<br />
the patient saves us from ourselves. He feels the doctor’s discomfort<br />
in breaking the news, and works to ease the doctor’s<br />
pain, jumping up and even thanking him!<br />
Every time I read this poem, I feel uncomfortable. I squirm<br />
as the anxious physician who cannot find the right words<br />
Illustrations by Erica Aitken<br />
to communicate in an honest, sensitive way. I squirm as the<br />
patient who suffers through not only the news about a devastating<br />
diagnosis, but also the nonsense coming from the<br />
physician’s mouth. What could the physician in Carver’s poem<br />
have done differently? What can any of us do when we realize<br />
the conversation is going badly? After his first verbal blunder,<br />
maybe the physician should have said something like: “I’m not<br />
saying this very well; let me start over.” Maybe he should have<br />
started the conversation with “I wish I had some other kind<br />
of news to give you,” and then quietly waited for the patient’s<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 25
Breaking bad news<br />
response after delivering the diagnosis. Things might have<br />
gone differently. Perhaps not. At many points in the dialogue,<br />
I simply want the physician to stop talking. And maybe that is<br />
one of the major lessons of the poem.<br />
Dr. John Stone’s poem “Talking to the Family” delivers<br />
other insights:<br />
My white coat waits in the corner<br />
like a father.<br />
I will wear it to meet the sister<br />
in her white shoes and organza dress<br />
in the live of winter,<br />
the milkless husband<br />
holding the baby.<br />
I will tell them.<br />
<strong>The</strong>y will put it together<br />
and take it apart.<br />
<strong>The</strong>ir voices will buzz.<br />
<strong>The</strong> cut ends of their nerves<br />
will curl.<br />
I will take off the coat,<br />
drive home,<br />
and replace the light bulb in the hall. 8<br />
<strong>The</strong> physician’s fear of doing his duty is palpable. Like a boy<br />
who dreads telling his father about an accident or other bad<br />
news, but knows he must, the physician reluctantly puts on<br />
his white coat of authority to inform the family of the patient’s<br />
death. As Kathryn Montgomery beautifully puts it,<br />
the secret of the poem, the reason its speaker is not the<br />
heartless bastard a first-year student every now and then<br />
will argue he must be, is that, except for the first line, it is<br />
written in the future tense. . . . <strong>The</strong> dreadful telling has not<br />
happened yet. <strong>The</strong> speaker is still elsewhere, off stage, in his<br />
office perhaps, and the dread—along with the acceptance of<br />
a physician’s duty—is his. 9<br />
Despite the tragedy, life goes on. <strong>The</strong> physician cannot<br />
dwell on the moment—he has other patients to see, and other<br />
patients to console. He also has other things to do. Doctoring<br />
is only one of his roles. <strong>The</strong> doctor slips on his white coat at<br />
work, and slips it off when his professional duty is done. He<br />
goes home and, like the rest of us, must perform mundane<br />
tasks such as changing light bulbs.<br />
<strong>The</strong> simple, mechanical task takes his mind off the terrible<br />
news. Changing the light bulb is an important step toward<br />
focusing on the present, renewing his energy, and healing<br />
his own pain. <strong>The</strong> light goes out in one life, but the doctor<br />
is climbing the ladder again, making physical and emotional<br />
adjustments so that he can bring new life and light to others.<br />
Life goes on.<br />
Physicians need to be intellectually and emotionally prepared<br />
to deliver bad news. Patients and families may have<br />
many questions about treatment and prognosis. <strong>The</strong>y may<br />
react to the news in a variety of ways, including sadness, anger,<br />
or shock. And physicians themselves will have their own<br />
reactions to the telling of the news. But preparation for these<br />
things is not sufficient. Once they are in the middle of a conversation,<br />
physicians must be flexible, creative, and self-aware,<br />
ready if necessary to change the direction of the dialogue, offer<br />
a tissue, or simply be quiet. Like Stone’s poem, what’s left<br />
unsaid often has more power than what is said: Stone does not<br />
explicitly tell us about the husband’s grief—he uses a remarkable<br />
image, “the milkless husband holding the baby,” to convey<br />
the impending grief and loss.<br />
Reading the poems above is no substitute for preparation,<br />
practice, and clinical experience. Nevertheless, I believe<br />
physicians who read these poems with attention and empathy<br />
will enhance their understanding of language, feelings, and<br />
the communication of bad news. <strong>The</strong> poems also remind us<br />
how unpredictable these conversations can be, no matter how<br />
frequently we rehearse for them. Finally, we should not be surprised<br />
by our dread and reluctance to do our duty and deliver<br />
the message: a milkless husband is hard to bear.<br />
References<br />
1. Hebert HD, Butera JN, Castillo J, Mega AE. Are we training<br />
fellows adequately in delivering bad news to patients? A survey of<br />
hematology/oncology program directors. J Palliat Med 2009; 12:<br />
1119–24.<br />
2. Walsh RA, Girgis A, Sanson-Fisher RW. Breaking bad news.<br />
2: What evidence is available to guide clinicians? Behav Med 1998;<br />
24: 61–72.<br />
3. Barclay JS, Blackhall LJ, Tulsky JA. Communication strategies<br />
and cultural issues in the delivery of bad news. J Palliat Med 2007;<br />
10: 958–77.<br />
4. Back A, Arnold R, Tulsky J. Mastering Communication with<br />
Seriously Ill Patients: Balancing Honesty with Empathy and Hope.<br />
Cambridge: Cambridge University Press; 2009.<br />
5. Ptacek JT, Eberhardt, TL. Breaking bad news: A review of the<br />
literature. JAMA 1996; 276: 496–502.<br />
6. Carver R. All Of Us: <strong>The</strong> Collected Poems. New York: Vintage<br />
Books; 2000: 289.<br />
7. Gianakos D. What the Doctor Said: Commentary. Acad Med<br />
2008; 83: 420–21.<br />
8. Stone J. Music From Apartment 8. Baton Rouge (LA): Louisiana<br />
State University Press; 2004: 51.<br />
9. Montgomery K. A setback: In memory of John Stone, 1936–<br />
2008. Lit Med 2008 Fall; 27: 119–23.<br />
<strong>The</strong> author’s address is:<br />
Lynchburg Family Medicine Residency<br />
2323 Memorial Avenue, #10<br />
Lynchburg, Virginia 24501<br />
E-mail: deangianakos@yahoo.com<br />
26 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
���������<br />
A heart aches<br />
Like the earth when it quakes<br />
A void left where ground once lay<br />
Impossible to heal<br />
A scar fills the space<br />
With memories that once were real<br />
John Allan, MD<br />
Dr. Allan (AΩA, Saint Louis University, 2009)<br />
is a PGY-2 in Internal Medicine at New York-<br />
Presbyterian Hospital Weill-Cornell Medical Center.<br />
His address is: 445 East 68th Street, Apartment 8G,<br />
New York, New York 10065. E-mail: allanj@slu.edu.<br />
Illustration by Jim M’Guinness<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 27
�����<br />
�������<br />
�������<br />
�������<br />
Early standardization of the insulin unit<br />
Barry Fields, MD<br />
28 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
<strong>The</strong> author is chief resident in<br />
Internal Medicine at the Yale<br />
Primary Care Residency Program.<br />
From its advent in September<br />
2006 until its removal from the<br />
market in October 2007, inhaled<br />
insulin for diabetes mellitus<br />
represented the first effective alternative<br />
to subcutaneous injections in<br />
more than eighty years. Aside from<br />
its administration modality, Exubera<br />
(Insulin Human [rDNA origin]) also<br />
transformed dosage labeling from<br />
the traditional insulin “unit” into<br />
milligrams. While this conversion<br />
may have appeared novel, it actually<br />
harked back to a time early in insulin<br />
therapy’s history. Indeed, defining insulin<br />
quantity in terms of milligrams<br />
sits at the heart of post-World War I<br />
efforts to ensure the new product’s<br />
safety and reliability. <strong>The</strong>se early attempts<br />
at its international standardization<br />
laid the foundation on which<br />
insulin dosage is still based today.<br />
Frederick Grant Banting.<br />
Courtesy of the National Library of Medicine.<br />
Producing an insulin extract<br />
In the autumn of 1920, Canadian<br />
surgeon Frederick Grant Banting<br />
scribbled,<br />
Diabetus<br />
Ligate pancreatic ducts of<br />
dog. Keep dogs alive till acini<br />
degenerate leaving Islets.<br />
Try to isolate the internal secretion<br />
of these to relieve glycosurea<br />
[sugar in the urine]. 1p50<br />
In this short note, Banting<br />
outlined how he would<br />
find the quintessentialtreatment<br />
for a disease he could not even spell.<br />
Over the next year, Banting worked<br />
in the University of Toronto physiology<br />
laboratory of Professor J. J. R.<br />
Macleod. With the help of graduate<br />
students Charles Best and Clark<br />
Noble, he purified his first insulin extract<br />
from the degenerating pancreases<br />
of canine subjects and showed it<br />
could transiently reduce the animals’<br />
blood sugar.<br />
Banting presented his findings to<br />
the American Physiological Society<br />
conference in December 1921. Among<br />
attendees expressing interest in extract<br />
production was George H. A.<br />
Clowes, research director for the Eli<br />
Lilly Pharmaceutical Company of<br />
Indianapolis. Though his offer was<br />
initially turned down, it caused the<br />
researchers to patent their process<br />
to maintain their control over the<br />
integrity of the extract’s manufacture<br />
and purification. <strong>The</strong> University of<br />
Toronto’s Board of Governors subsequently<br />
licensed the process to Lilly’s<br />
laboratories. 1 American production<br />
supplemented the relatively meager<br />
yields at Toronto’s own Connaught<br />
Antitoxin Laboratories, supplying<br />
a burgeoning international market<br />
with insulin therapy.<br />
To oversee insulin’s future licensing<br />
and distribution, the Board<br />
of Governors organized Toronto’s<br />
Insulin Committee (IC) in 1922. One<br />
of its first actions was to offer patent<br />
rights to the British Medical Research<br />
Council (MRC), thus giving Europe<br />
its first access to insulin. <strong>The</strong> MRC<br />
sent Dr. Henry H. Dale, a department<br />
director at their National<br />
Institute for Medical Research, to<br />
Toronto. Dale quickly recognized the<br />
promise of insulin and suggested the<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 29
From rabbits to the League of Nations<br />
MRC accept control of the British patent.<br />
At the same time, he and his traveling<br />
companion, biochemist Harold W.<br />
Dudley, expressed serious reservations<br />
regarding the IC’s earliest definition of<br />
the insulin unit. Dale wrote:<br />
<strong>The</strong> Toronto definition of a “unit”<br />
of the specific insulin activity, was<br />
the dose required, with intravenous<br />
injection, to throw 3 out of 5 rabbits<br />
into hypoglycaemic convulsions! I<br />
had made it no secret, from the first,<br />
. . . that I regarded such a definition<br />
as having so little claim to accuracy,<br />
as to be practically almost useless,<br />
and eventually misleading. 2p445<br />
Clowes from Lilly later echoed these<br />
misgivings when developing a reliable<br />
insulin unit became a matter of international<br />
concern.<br />
A rabbit-based unit<br />
Dale’s observation came months after<br />
the first insulin unit was defined.<br />
During the spring of 1922, Macleod,<br />
James B. Collip, Banting, and Best began<br />
calibrating insulin by its effects on animals.<br />
Using two-kilogram rabbits, they<br />
determined that hypoglycemic convusions<br />
usually appeared as the animals’<br />
blood sugar component fell below 0.045<br />
percent. This observation served as a<br />
threshold on which to base the first<br />
“physiologic unit” or “rabbit unit” of insulin,<br />
about one cc. <strong>The</strong> authors wrote:<br />
As a tentative basis for the physiological<br />
assay of insulin we consider<br />
as one unit the number of<br />
cubic centimeters which causes the<br />
blood sugar of normal rabbits to fall<br />
to 0.045 per cent within 4 hours.<br />
This dose is decidedly active in lowering<br />
the blood sugar in diabetic<br />
patients. 3p175<br />
<strong>The</strong>ir report also compared the effects<br />
of infused insulin solution on a<br />
two-kilogram normal rabbit with an<br />
eleven-kilogram depancreatized dog.<br />
<strong>The</strong> authors noted that, after taking<br />
into account the animals’ weight and<br />
dosage disparities, the dog still showed a<br />
much more dramatic reduction in blood<br />
sugar levels after having received only<br />
one third the dose that the rabbit had<br />
received. 3 <strong>The</strong> unit’s value would change<br />
later that year to reflect this observation.<br />
<strong>The</strong>se early attempts to define an<br />
insulin unit coincided with the first<br />
diabetic human patients being treated<br />
with the pancreatic extract. Fifteenyear-old<br />
Elizabeth Hughes, the diabetic<br />
daughter of New York governor<br />
and future Chief Justice Charles Evans<br />
Hughes, began her injections in mid-<br />
August. Just one cc twice daily effectively<br />
cleared the sugar from her urine.<br />
However, by October her dosage had<br />
risen to five cc twice daily. In a letter to<br />
her mother, Hughes wrote:<br />
Courtesy of the National Library of Medicine.<br />
30 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
Charles H. Best.<br />
Courtesy of the National Library of Medicine.<br />
We only have a two cc. syringe you<br />
know and so Blanche [her nurse]<br />
fills that and gives it to me and then<br />
unscrews it from the needle which<br />
is left sticking in to me (I feel like a<br />
pincushion) fills it again, and gives<br />
me that (am left a pincushion once<br />
more), and then have the fifth cc.<br />
It really is quite a process, and altogether<br />
takes about twenty minutes<br />
for the whole performance. 1p155<br />
<strong>The</strong>re is no indication that Elizabeth<br />
Hughes’s diabetes had worsened, nor<br />
that her sensitivity to insulin had decreased.<br />
Since she remained in Toronto<br />
for the first months of treatment, it is<br />
almost certain she received her insulin<br />
from the same source, Connaught<br />
Antitoxin Laboratories. A lack of consistency<br />
in production protocol and<br />
continued efforts to increase their yield<br />
resulted in wide fluctuation<br />
in the final product’s<br />
activity. <strong>The</strong>refore, while<br />
Canadian researchers held<br />
the definition of an insulin<br />
unit constant in terms of<br />
its clinical effects on rabbits,<br />
the actual dosage fluctuated<br />
greatly. 1<br />
An ever-evolving unit<br />
Late in 1922, additional<br />
criticism of the definition<br />
of the insulin unit emerged<br />
from giants in American<br />
diabetology such as Dr.<br />
Frederik Madison Allen<br />
and Dr. Elliot P. Joslin.<br />
<strong>The</strong>se physicians and their<br />
colleagues disliked the<br />
“physiologic unit” of insulin<br />
because its relative<br />
strength in humans forced<br />
some patients to receive<br />
fractions of a unit, creating<br />
confusion among patients<br />
and nurses alike. 4 Clowes<br />
at Lilly brought their<br />
concerns to the IC. On<br />
December 30, 1922, they<br />
announced:<br />
<strong>The</strong> Toronto Committee conferred<br />
with Drs Clowes, Allen and Joslin as<br />
to the adoption of a unit for Insulin<br />
required to lower the blood sugar<br />
and the following conclusions were<br />
arrived at:<br />
1) <strong>The</strong> unit adopted for Insulin<br />
shall be approximately one-fifth that<br />
of the original Toronto unit, which<br />
is the amount of Insulin required to<br />
lower the blood sugar of a 2 kg fed<br />
rabbit 0.045 per cent within four<br />
hours, and cause symptoms. 4<br />
This new unit was to be called the “clinical<br />
unit” of insulin as opposed to the<br />
original “physiological,” “Toronto,” or<br />
“rabbit” unit. In this manner, the IC<br />
had adjusted its calibration of insulin to<br />
accommodate the needs of clinicians,<br />
as represented by Lilly. Further col-<br />
laborations between the pharmaceutical<br />
company and the IC would not proceed<br />
as smoothly.<br />
As with Elizabeth Hughes’s insulin<br />
supply, clinicians in 1923 complained of<br />
potency discrepancies among batches<br />
supposedly of the same clinical strength.<br />
California physician W. D. Sansum and<br />
his research team provided unique insight<br />
into the unit’s evanescence. During<br />
early 1923, they helped establish the<br />
“sugar-metabolizing power” of a given<br />
lot of insulin—the amount of sugar metabolized<br />
by each insulin unit. <strong>The</strong>y<br />
showed Lilly’s insulin to have 1.25 grams<br />
of sugar metabolizing power per unit. 5<br />
Unfortunately, clinicians and their patients<br />
remained vulnerable to continued<br />
unit modifications elsewhere.<br />
Beginning in May, the researchers<br />
noted that previously well-controlled<br />
diabetic patients had sugar reappearing<br />
in their urine. <strong>The</strong> new insulin<br />
units’ sugar metabolizing power had<br />
decreased by approximately one third<br />
compared to one month previously. <strong>The</strong><br />
authors state:<br />
We then learned that the unit had<br />
been redefined as being one-third<br />
of the amount required to lower<br />
the blood sugar below 0.045% and<br />
cause convulsions in a two-kilogram<br />
rabbit which had been previously<br />
starved for twenty-four hours. This<br />
redefinition was based on the belief,<br />
supported by experimental evidence,<br />
that it requires four times as<br />
much insulin to cause a convulsion<br />
in a two kilogram rabbit as in a<br />
one kilogram rabbit. In using onethird<br />
instead of one-fourth the convulsion<br />
[dose] in the two kilogram<br />
rabbits, these workers believed that<br />
they were increasing the value of<br />
the unit. 5<br />
<strong>The</strong>ir comments allude to discrepancies<br />
in rabbit size between Lilly’s laboratories<br />
and those of the IC. While Toronto<br />
had been using two-kilogram fed rabbits<br />
in its tests of potency, Lilly had<br />
been using one-kilogram fasting rabbits.<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 31
From rabbits to the League of Nations<br />
To complicate matters further, Clowes<br />
never applied the IC’s new definition of<br />
the clinical unit to his product. Instead<br />
of dividing the physiologic unit by five<br />
per their directive, Clowes divided it<br />
by four and added twenty-five percent<br />
to account for product deterioration.<br />
He cited discrepancies in experimental<br />
results between Lilly and the IC and the<br />
tendencies of clinicians to desire a more<br />
potent unit to rationalize his decision. 4<br />
With an increasingly reliable extract<br />
provided by the IC and Lilly, attention<br />
could shift toward improving its international<br />
standardization.<br />
A weight-based standardization<br />
scheme<br />
A standardized drug is one that is<br />
always produced at equal potency in all<br />
manufactured lots. An international effort<br />
to standardize emerging treatments<br />
had been underway for decades before<br />
insulin was developed. Without knowing<br />
the chemical composition of these<br />
new biologic extracts, tests to determine<br />
potencies were relative; the substance’s<br />
effect on one group of animals (or “biological<br />
system”) would be compared to<br />
its effects on another reference or “standard”<br />
system. This procedure, however,<br />
assumed that the substance being tested<br />
and the animals in each test group were<br />
identical, an untenable assumption. 6,7<br />
As Lilly’s rabbits had demonstrated,<br />
standardization based solely on a reference<br />
biological system was fraught with<br />
dangerous inaccuracy.<br />
In 1897, German physician Paul<br />
Ehrlich described attempts at medical<br />
standardization based on activity<br />
of a certain weight of active ingredient.<br />
His task had been to ensure uniform<br />
potency of the newly-developed<br />
diphtheria antitoxin; due to the instability<br />
of the diphtheria toxin, he was<br />
consistently unsuccessful. Recognizing<br />
the fallibility of the biological system,<br />
he devised a standardization scheme<br />
based on weight of dried antitoxin. His<br />
institute in Germany kept samples of<br />
the sterile, dried product in vacuum at<br />
low temperature. Units of antisera were<br />
defined in terms of the weight of this<br />
standard. Laboratories and production<br />
plants around the world could periodically<br />
obtain samples and compare them<br />
to their new product to ensure the potency<br />
of its unit matched the standard<br />
in Germany.<br />
<strong>The</strong> MRC’s Henry Dale studied<br />
Ehrlich’s principles during a period in<br />
which he became increasingly frustrated<br />
with the international community’s attempt<br />
to standardize many medical<br />
breakthroughs. Efforts to institute unit<br />
standards consisted mostly of debates<br />
concerning the merits of one biological<br />
method over another. 8 With Dale’s<br />
encouragement, the League of Nations<br />
Health Committee sponsored a 1923<br />
Edinburgh Conference to discuss new<br />
methods of international standardization.<br />
In the months before the conference,<br />
Dale directed Dudley to prepare a<br />
solid form of insulin, resulting in insulin<br />
hydrochloride, a dried powder standard<br />
that companies and laboratories could<br />
compare their product against.<br />
<strong>The</strong> League of Nations weighs in<br />
When the International Congress<br />
met at Edinburgh in 1923, champions<br />
of biological systems proposed extending<br />
rodent hypoglycemia methods to<br />
international acceptance. Dale objected,<br />
citing the many drawbacks of such systems.<br />
He wrote:<br />
the definition, for permanent adoption<br />
and international transmission,<br />
of any unit of biological activity in<br />
terms of the reaction of a proportion<br />
of test animals, was inadmissible;<br />
and that the only safe basis for the<br />
definition of a unit of insulin, or of<br />
any other potent remedy, would be<br />
in terms of a precise weight of a<br />
standard, stable sample of the remedy<br />
in question, in the form of a<br />
completely dried powder. 2p448<br />
After displaying a vial containing the<br />
insulin hydrocholoride Dudley had developed,<br />
Dale proposed that interested<br />
parties work to correlate amounts of the<br />
powder with what they believed to be<br />
the experimental activity of one insulin<br />
unit. He also suggested they ask the<br />
League of Nations for another conference<br />
in two years, at which investigators<br />
taking part in the trials could present<br />
their findings.<br />
Reorganization within the League of<br />
Nations helped make that future conference<br />
a viable reality. In 1924, the League<br />
of Nations Health Committee became<br />
its Health Organization, one of several<br />
“technical agencies” that functioned<br />
semi-autonomously within the League. 9<br />
Its president, Thorvald Madsen, placed<br />
biological standardization near the top<br />
of his priority list for world health initiatives.<br />
7 <strong>The</strong>se developments within the<br />
League, combined with ever-increasing<br />
numbers of new biological compounds,<br />
set the groundwork for a Second<br />
International Conference on Biological<br />
Standards at Geneva in 1925.<br />
In the interim, five institutions, including<br />
Connaught Laboratories and<br />
Lilly, contributed samples of their insulin<br />
product to a growing pool of extract<br />
at the MRC. Under Dale and Dudley’s<br />
supervision, the preparations were combined<br />
and then converted to a single<br />
batch of powdered insulin hydrochloride.<br />
<strong>The</strong> product was divided into 100mg<br />
ampules, dried, sealed, and sent to<br />
laboratories in England, Canada, and<br />
the United States. Those independent<br />
labs could determine the value of “solid”<br />
insulin in terms of their own units at<br />
the time. <strong>The</strong>ir results were remarkably<br />
consistent, showing each milligram of<br />
powder to have a value of 8.4 to 8.8<br />
units. To avoid fractional units, the IC<br />
declared that the solid insulin standard<br />
contained 8 units per milligram. 10<br />
<strong>The</strong> Second International Conference<br />
met in late August and early September<br />
of 1925. Chaired by Henry Dale, it considered<br />
the standardization of several<br />
biological products, with insulin receiving<br />
particular attention. <strong>The</strong>ir unanimous<br />
recommendation read:<br />
That the dry preparation of insulin<br />
hydrochloride, prepared by<br />
the Medical Research Council of<br />
Great Britain at the request of the<br />
Edinburgh Conference, should be<br />
32 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
accepted as the international standard<br />
preparation of insulin. That 1<br />
milligram of this standard contains<br />
8 units of insulin (or 1 unit = 0.125<br />
milligrams), as provisionally defined<br />
by the Insulin Committee of the<br />
University of Toronto. 8p61<br />
<strong>The</strong> League of Nations’ Permanent<br />
Commission on Biological Standards<br />
subsequently adopted this recommendation.<br />
In doing so, the insulin unit<br />
was transformed from being defined by<br />
rodent convulsions to one determined<br />
by comparison to an internationally<br />
recognized standard preparation, in<br />
milligrams.<br />
Over the next decade, decreases<br />
in the use of the standard preparation<br />
method and further advances<br />
in insulin purification led world authorities<br />
to seek a new standard insulin<br />
unit. 10 In 1935, the League of<br />
Nations Permanent Commission on<br />
Biological Standardisation “accepted<br />
the new standard for international<br />
use and redefined the unit of insulin<br />
as the specific insulin activity of one<br />
twenty-second (1/22) of a milligramme<br />
of the new standard.” 11p486 A Third and<br />
Fourth International Standard would<br />
be elucidated under the World Health<br />
Organization, United Nations’ equivalent<br />
to the League of Nations Health<br />
Organization. Remarkably similar to the<br />
1935 standard, the Fourth International<br />
Standard defines biologically extracted<br />
insulin as 24.0 insulin units per milligram.<br />
10<br />
<strong>The</strong>refore, more than eighty years<br />
after a unit-milligram equivalency was<br />
first created to ensure international insulin<br />
standardization, this concept was<br />
resurrected to simplify inhaled insulin<br />
dosing and administration in a new<br />
form. Tables on Pfizer’s Exubera web<br />
site and in print aided clinicians and<br />
their patients in making this contemporary<br />
unit-to-milligram conversion<br />
(Pfizer’s web page for Exubera has been<br />
removed; a web page with similar information<br />
is referenced). 12 In doing so,<br />
they also brought to mind a historical<br />
definition—that of the insulin unit itself.<br />
Henry H. Dale.<br />
Courtesy of the National Library of Medicine. F. Netter, compliments Armour Laboratory, Chicago.<br />
Acknowledgment<br />
I thank my faculty advisors Stephanie<br />
Brown-Clark, MD, PhD, and Michael Green,<br />
MD, MSc, for their thoughtful comments,<br />
guidance, and support in preparation of this<br />
manuscript.<br />
References<br />
1. Bliss M. <strong>The</strong> Discovery of Insulin.<br />
Chicago: <strong>The</strong> University of Chicago Press;<br />
1982.<br />
2. Murnaghan JH, Talalay P. H. H.<br />
Dale’s account of the standardization of<br />
insulin. Bull Hist Med 1992; 66: 440–50.<br />
3. Banting FG, Best CH, Collip JB, et<br />
al. <strong>The</strong> effect of pancreatic extract (insulin)<br />
on normal rabbits. Am J Physiol 1922; 62:<br />
162–76.<br />
4. Sinding C. Making the unit of insulin:<br />
Standards, clinical work, and industry,<br />
1920–1925. Bull Hist Med 2002; 76: 231–70.<br />
5. Sansum WD, Blatherwick NR, Smith<br />
FH, et al. <strong>The</strong> treatment of diabetes with<br />
insulin. J Metab Res 1923; 3: 641–65.<br />
6. Miles AA. Biological standards and<br />
the measurement of therapeutic activity. Br<br />
Med Bull 1951; 7: 283–91.<br />
7. Cockburn WC. <strong>The</strong> international<br />
contribution to the standarization of biological<br />
substances. I. Biological standards<br />
and the League of Nations 1921–1946. Bio-<br />
logicals 1991; 19: 161–69.<br />
8. Knaffl-Lenz E, League of Nations<br />
Health Organisation Permanent Commission<br />
on Standardization of Sera, Serological<br />
Reactions and Biological Products.<br />
Memoranda on Cardiac Drugs, Thyroid<br />
Preparations, Ergot Preparations, Filix<br />
Mas, Suprarenal Preparations, Vitamins,<br />
Pituitary, Salvarsan, Oil of Chenopodium,<br />
Insulin. III. Health. 1928 III. 10. Geneva:<br />
Publications of the League of Nations; 1928.<br />
9. Aufricht H. Guide to League of Nations<br />
Publications: A Bibliographical Survey<br />
of the Work of the League, 1920–1947. New<br />
York: Columbia University Press; 1951.<br />
10. Lacey AH. <strong>The</strong> unit of insulin. Diabetes<br />
1967; 16: 198–200.<br />
11. Best CH, Dale HH. I. Insulin. 1. <strong>The</strong><br />
new international insulin standard and the<br />
re-definition of the existing unit in terms<br />
therof. League of Nations Q Bull Health Org<br />
1936; 5: 584–658.<br />
12. Exubera (Insulin Human [rDNA origin])<br />
Drug Information: Uses, Side Effect,<br />
Drug Interactions and Warnings at RxList.<br />
http://www.rxlist.com/exubera-drug.htm.<br />
<strong>The</strong> author’s address is:<br />
5221 Town Walk Drive<br />
Hamden, Connecticut 06518<br />
E-mail: barry.fields@yale.edu<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 33
� ������������<br />
<strong>The</strong>re in a royal box<br />
ordinary folks still as rocks<br />
posed as in a portrait<br />
decide another’s fate<br />
watching evidence passing by<br />
like shooting stars in the sky.<br />
At recess the courtroom a deserted camp.<br />
In one corner the flag hangs limp<br />
like a runner out of breath.<br />
<strong>The</strong> defendant alone, the last on earth.<br />
<strong>The</strong> clock points its moving finger<br />
distanced from slander and anger.<br />
Worry directs every thought<br />
about what legal tacks have wrought<br />
that may dissolve dreams to dust<br />
threatening future with rust.<br />
<strong>The</strong> decision, at last, is made<br />
by citizens returning in parade.<br />
His honor enters in his black gown.<br />
Suspense suppresses every sound.<br />
All wait for words cast in cement<br />
that will terminate this event.<br />
“No cause,” the verdict of the jury.<br />
Behold the plaintiff’s fury.<br />
From the defendant relief effervescent bubbles<br />
from a bottle of troubles.<br />
H. Harvey Gass, MD<br />
Dr. Gass (AΩA, University of Michigan, 1941) is retired from practice as a clinical<br />
professor of Neurosurgery at Wayne State Medical School. His address is: 6155 East<br />
Longview Drive, East Lansing, Michigan 48823. E-mail: sgass@msu.edu.<br />
Illustration by Jim M’Guinness<br />
34 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
Health policy<br />
Our health care system is not broken—<br />
it’s obsolete!<br />
Jordan J. Cohen, MD<br />
<strong>The</strong> author (AΩA, Tufts University, 1978) is professor<br />
of Medicine and Public Health at George Washington<br />
University and president emeritus of the Association of<br />
American Colleges.<br />
We often hear that our health care system is “broken.”<br />
Indeed, it’s become a pat refrain among<br />
policymakers and the media. But thinking the<br />
system is “broken” implies that it can be “fixed”—patched<br />
up to make it work like it used to. That’s what would-be<br />
health care reformers seem to think when they tinker with<br />
“fixes” like expanding insurance coverage with mandates and<br />
subsidies, guaranteeing insurance despite pre-conditions,<br />
crafting pay-for-performance incentives to change provider<br />
behavior, and expanding use of electronic medical records.<br />
All of these “fixes” would undoubtedly be helpful and should<br />
be implemented without delay. But unfortunately, even in the<br />
aggregate, these and other attempts to tinker with the current<br />
system cannot get at the fundamental problems we have to<br />
solve and, hence, are a far cry from true health care reform.<br />
Why? Because our health care system is not “broken.”<br />
Rather, it’s outmoded. It’s archaic. It’s a legacy system that is<br />
simply incapable —inherently incapable—of meeting today’s<br />
health care needs, no matter how much we tinker with it.<br />
Imagine trying to fix a Model T Ford so that it could fly. You<br />
could put in a more powerful engine, take off the fenders,<br />
strap on wings, and put on a pair of aviator goggles. But you<br />
still couldn’t get the darned thing off the ground!<br />
<strong>The</strong> hand-me-down system we’ve inherited is just like that<br />
old car, the product of a bygone era that was well designed for<br />
yesteryear but is no longer serviceable. Yesteryear was when<br />
the health care system needed to deal primarily with acute,<br />
often self-limited illness and injury; when medical technologies<br />
were much more limited in scope and much less complex;<br />
when we thought “the world’s best health care system”<br />
delivered uniformly high-quality care to everyone; and when<br />
the overall cost of health care was still in the single digits as a<br />
percentage of GDP.<br />
In times like those, our country could get along quite well<br />
with autonomous doctors working solo or in small groups.<br />
And we rather liked having our doctors in total control,<br />
with all other health care professionals playing supporting<br />
roles. We could tolerate independent hospitals<br />
competing with one another for patients. We had<br />
a fee-for-service payment system that was well<br />
designed to deal with isolated episodes of<br />
illness and discrete encounters with individual<br />
providers. And paper-based<br />
medical records kept separately by<br />
each of our providers worked<br />
well enough.<br />
Today, we face an entirely different set of realities, realities<br />
that our legacy system was never designed for, and can never<br />
be retrofitted to deal with satisfactorily. Chief among them are<br />
rising costs, an increasing burden of chronic, unrelenting disease<br />
and disability, way too many medical errors, inexplicable<br />
variations in the way medicine is practiced across the country,<br />
profound lapses in quality, and wide disparities in health and<br />
health care even among those with adequate insurance.<br />
<strong>The</strong> fragmented, uncoordinated, fee-for-service conglomeration<br />
we have inherited cannot hope to cope effectively with<br />
these twenty-first-century challenges.<br />
If policymakers would shift their mental model from “broken,<br />
let’s fix it” to “obsolete, let’s redesign it,” I doubt there<br />
would be much disagreement about the features a new system<br />
should have. We’d want “units of accountability” big enough<br />
to be held responsible for delivering comprehensive, high-<br />
quality, cost-effective care to large groups of people. <strong>The</strong>se<br />
units of accountability would be required to develop systematic<br />
approaches to weeding out waste, to coordinating the care<br />
of the chronically ill, to avoiding redundant tests, to guaranteeing<br />
that preventive strategies were broadly implemented,<br />
and to fully utilizing the skills of all health care workers in<br />
high-performing teams.<br />
Moving from our dysfunctional, fragmented legacy system<br />
to an integrated, accountable system will not be easy and will<br />
not happen quickly. <strong>The</strong> barriers to achieving the fundamental<br />
transformation required are enormous. An entirely different<br />
financing scheme will be needed to release the system from<br />
the paralyzing constraints of our current fee-for-service arrangement,<br />
and a new cultural paradigm among providers will<br />
be needed to foster collaboration, teamwork, accountability,<br />
quality improvement, and patient safety. Even before clearing<br />
those barriers, however, a way must be found to overcome the<br />
resistance from entrenched stakeholders who are profiting<br />
handsomely from the current system and who have powerful<br />
political allies.<br />
But the risk of trying to preserve an obsolete system is<br />
simply too great to let these obstacles stand in the way of<br />
needed reforms. Fortunately, a window of opportunity has<br />
opened up. Buried in the myriad “fixes” included in the Patient<br />
Protection and Affordable Care Act is a call for CMS to promote<br />
demonstration projects to implement and evaluate innovative<br />
approaches to organizing and delivering health care.<br />
Such demonstrations could allow for the creation, on a large<br />
scale, of what Stephen Shortell and Lawrence Casalino have<br />
called accountable care systems, systems that are “capable of<br />
implementing organized processes for improving the quality<br />
and controlling the costs of care, and of being held accountable<br />
for the results.” 1 Being “accountable” would entail both<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 35
Our health care system is not broken—it’s obsolete!<br />
demonstrating appropriate clinical outcomes and taking on<br />
significant financial risk. It’s hard to imagine how these expectations<br />
could be met in the absence of a fully integrated system<br />
of providers in which doctors, nurses, hospitals, public health<br />
professionals, nursing homes, pharmacists, home health<br />
agencies, etc. join forces to manage cost-effectively the care of<br />
individuals and to deal systematically with the known health<br />
needs of a region or population.<br />
As possible points of departure for developing such<br />
truly accountable care systems, Shortell and Casalino suggest<br />
several current organizational arrangements including<br />
multispecialty group practices, hospital staff organizations,<br />
physician-hospital organizations, independent practice organizations,<br />
and health plan-provider organizations or networks.<br />
I’m concerned that none of these existing organizational arrangements<br />
is likely to be sufficiently scalable to meet the real<br />
challenges. What has more potential of doing so, in my view,<br />
are well-organized academic health centers.<br />
Indeed, many academic health centers are uniquely poised<br />
to develop the kind of integrated health care systems that we<br />
need. Many already have organized faculty practice plans, a<br />
network of affiliated hospitals, community physician referral<br />
bases, a relatively robust IT infrastructure, a tradition of innovation,<br />
loyal patients, and the trust and respect of their communities.<br />
Modern information technologies could be used to<br />
stitch together the network of hospitals, doctors, home health<br />
agencies, pharmacies, and other community resources needed<br />
both to provide for the health and health care needs of a large<br />
population and to monitor the system’s fiscal performance<br />
and to identify opportunities for improvement. Given their<br />
existing capabilities—and their avowed mission to serve the<br />
public interest—academic health centers, either individually<br />
or preferably in partnership with others, should lead the way<br />
toward solving what is arguably the most urgent health problem<br />
facing our county.<br />
However we do it, if we want our health care system to fly<br />
in the twenty-first century, we’ve got to stop trying to repair<br />
a hodgepodge arrangement that is hopelessly antiquated and<br />
get on with the hard work of replacing it with a real system<br />
that can actually do the job. Now that Congress has provided<br />
CMS with substantial resources to fund more appropriate<br />
ways to structure and finance health care services, I believe<br />
academic health centers—as engines of innovation—should<br />
seize the opportunity to demonstrate what true health care<br />
reform might look like.<br />
References<br />
1. Shortell SM, Casalino LP. Health care reform requires accountable<br />
care systems. JAMA 2008; 300: 95–7.<br />
Memento Mori<br />
<strong>The</strong> first one caught me by surprise.<br />
I was doing my initial thoracentesis,<br />
a task less daunting than the word implies.<br />
A cheerful woman gasped from fluid in her chest,<br />
a pleural effusion caused by rampant cancer.<br />
<strong>The</strong>re was no effusiveness in the somber needle<br />
I guided carefully through her chest wall.<br />
“I’m going to die now,” she calmly said,<br />
and, with nothing further, laid back dead.<br />
It was the moment doctors dread;<br />
full frontal with the enemy ahead<br />
And I midwife to the highest drama.<br />
This was no time for contemplation.<br />
Coding, CPR, intracardiac adrenaline;<br />
we were quick and forceful, but for naught.<br />
Relatives were notified, and in intense detail<br />
we probed each second, searching for a clue or cause.<br />
None came, and nothing from a later autopsy.<br />
We had no solution, no solace, and no one to blame.<br />
While preachers celebrate the rising soul,<br />
and mystics sense transfiguration, and<br />
loved ones clasp one another, casting<br />
hope against the loneliness of death,<br />
we found no answer in her body,<br />
no meaning in the metaphysics,<br />
and nothing in ourselves to talk about.<br />
Michael R. Milano, MD<br />
<strong>The</strong> author’s address is:<br />
1177 22nd Street, NW<br />
Jim M’Guinness<br />
Washington, DC 20037<br />
E-mail: msdjjc@gwumc.edu<br />
Dr. Milano (AΩA, Albany Medical College, 1964) is a psychiatrist living<br />
36 and practicing in Teaneck, New Jersey. <strong>The</strong> His <strong>Pharos</strong>/<strong>Winter</strong> e-mail address is: milanovino- <strong>2011</strong><br />
nos@aol.com.
Reading a Review<br />
M. Esteller. Molecular Origins of Cancer: Epigenetics in Cancer.<br />
N Engl J Med 2008; 358: 1148.<br />
I have learned from this reading that I will die<br />
not by the agency of great gods of sea and sky,<br />
or of the lesser ones, the sprites of groves and wells,<br />
nor even by will of the many-breasted mother,<br />
Earth herself.<br />
I must kneel instead to bits of my own cells,<br />
those invisible smalls within, where methyls delve,<br />
and shortened ribbons of RNA<br />
plug phosphates to genes and capriciously play<br />
with my molecules making them epigenetic.<br />
This change in belief runs through me like a panic attack.<br />
Worship my genes? <strong>The</strong>y are far too small<br />
for that. I am used to gods who are huge, and call<br />
on lightning’s power, or sometimes explode a sun<br />
over a cave in Palestine.<br />
Water from rock, pillars of fire define<br />
my life and beliefs. How can I live with the notion<br />
that these new gods of cancer, incapable of emotion,<br />
not even of guilt, have no concept of<br />
a high God’s mercy and unearthly love?<br />
Must I plead to my own, these bits of cell débris,<br />
even as they settle down to murder me?<br />
H. J. Van Peenen, MD<br />
Dr. Van Peenen is retired from medical practice. His address is: 74 W. 29th<br />
Avenue, Apartment 1103, Eugene, Oregon 97405. E-mail: lkvanp@comcast.net.<br />
Illustration by Jim M’Guinness<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 37
2010 <strong>Alpha</strong><br />
<strong>Omega</strong> <strong>Alpha</strong><br />
Robert J. Glaser<br />
Distinguished<br />
Teacher Awards<br />
Each year since 1988, <strong>Alpha</strong><br />
<strong>Omega</strong> <strong>Alpha</strong>, in cooperation<br />
with the Association of American<br />
Medical Colleges, presents four AΩA<br />
Distinguished Teacher Awards to<br />
faculty members in American medical<br />
schools. Two awards are for ac-<br />
Gary L. Dunnington, MD (Clinical)<br />
J. Roland Folse Professor and Chair of<br />
Surgery, Southern Illinois University<br />
School of Medicine<br />
Dr. Dunnington (AΩA, University<br />
of Southern California, 1994) joined<br />
Southern Illinois University School of<br />
Medicine in 1979 as professor in the<br />
Department of Surgery. Since then, he<br />
has been director of the General Surgery<br />
Residency Program and professor and<br />
chair of the Department of Surgery. He<br />
was named the J. Roland Folse Professor<br />
and Chair of Surgery in 2009.<br />
Dr. J. Kevin Dorsey, dean of the<br />
complishments in teaching the basic<br />
sciences and two are for inspired<br />
teaching in the clinical sciences.<br />
In 1997, AΩA named the award to<br />
honor its retiring executive secretary<br />
Robert J. Glaser, MD. Nominations<br />
for the award are submitted to the<br />
AAMC each spring by the deans of<br />
medical schools.<br />
Nominations were reviewed by a<br />
committee chosen by AΩA and the<br />
AAMC. This year’s committee members<br />
were: Ronald Arky, MD; David<br />
A. Asch, MD, MBA; J. John Cohen,<br />
MD, PhD; Molly Cooke, MD; Eugene<br />
C. Corbett, MD, FACP; Linda S.<br />
Costanza, PhD; Arthur F. Dailey II,<br />
PhD; Erika Goldstein, MD; Aviad<br />
Distinguished teachers Gary L. Dunnington, MD; Duane E. Haines, PhD; John W. Pelley,<br />
PhD; and James R. Stallworth, MD. Deborah E. Powell, MD, immediate past chair of<br />
the AAMC board of directors and Associate Vice President for New Models of Medical<br />
Education is on the left. On the right are Richard L. Byyny, MD, Executive Director of <strong>Alpha</strong><br />
<strong>Omega</strong> <strong>Alpha</strong>, and Darrell G. Kirch, MD, President and CEO of the AAMC.<br />
Photo credit: Richard Greenhouse Photography, Inc. Courtesy of the AAMC.<br />
SIU School of Medicine, writes: “Dr.<br />
Dunnington is a passionate advocate<br />
and practitioner of excellence in medical<br />
education. He has received nineteen<br />
teaching awards at three institutions,<br />
including the Outstanding Teacher of<br />
the Year award at SIU in 2010. With<br />
several colleagues, he developed and<br />
refined an academic incentive system<br />
that has been in use at SIU for more<br />
than ten years. Dr. Dunnington’s influence<br />
spreads far beyond the walls of<br />
SIU, however. He was one of the thought<br />
leaders involved in the ACGME’s Task<br />
Haramati, PhD; Bruce M. Koeppen,<br />
MD, PhD; Jeanette Norden, PhD;<br />
Paul L. Rogers, MD; James L.<br />
Sebastian, MD; Gabriel Virella, MD,<br />
PhD.<br />
Winners of the award receive<br />
$10,000, their schools receive<br />
$2,500, and active AΩA chapters<br />
at those schools receive $1,000.<br />
Schools nominating candidates for<br />
the award receive a plaque with the<br />
name of the nominee.<br />
Brief summaries of the accomplishments<br />
in medical education of<br />
the 2010 award recipients follow.<br />
Richard L. Byyny, MD<br />
Executive Director<br />
Force charged with developing the six<br />
competencies toward which all residencies<br />
in the United States now train. He<br />
and four other surgeons were founding<br />
members of the American College of<br />
Surgeon’s Surgeons as Educators course.<br />
He facilitated the development of a “surgery<br />
readiness” elective for senior medical<br />
students, which is among the highest<br />
rated electives in the school and has<br />
inspired other SIU clinical departments<br />
to create similar electives. <strong>The</strong> report of<br />
the program in the medical literature has<br />
spawned numerous clones. A comprehensive<br />
system for evaluating operating<br />
room performance was selected by the<br />
American Board of Surgery as a template<br />
for a national system for rating operative<br />
performance. It will be required for all<br />
applicants for board certification.”<br />
Dr. Dunnington says of teaching, “You<br />
have to teach from the learner’s agenda,<br />
not from scripts. A truly great teacher<br />
says, ‘What can I help you learn today?’ ”<br />
Duane E. Haines, PhD (Basic)<br />
Professor and Chairman, Department<br />
of Anatomy, University of Mississippi<br />
Medical Center School of Medicine<br />
Dr. Haines received his PhD in<br />
Anatomy-Physical Anthropology at<br />
Michigan State University. He joined<br />
the University of Mississippi in 1985<br />
as a professor of Anatomy. He has received<br />
the A. J. Ladman AAA/Wiley<br />
Exemplary Service Award and the Henry<br />
Gray/Elsevier Distinguished Educator<br />
Award from the American Association<br />
of Anatomists, and the Silver Hammer<br />
Award as Teacher of the Year from<br />
38 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
the Department of Neurology at the<br />
University of Mississippi Medical Center.<br />
Dr. LouAnn Woodward, dean of the<br />
University of Mississippi Medical Center<br />
School of Medicine writes of Dr. Haines:<br />
“Dr. Haines embodies the definition of<br />
“doctor” from the Latin “to teach.” He<br />
has consistently gone the extra mile to<br />
provide an excellent quality education<br />
program with a focus on clinically relevant<br />
information.<br />
“Dr. Haines is well recognized for his<br />
atlas of the human brain, Neuroanatomy:<br />
An Atlas of Structures, Sections, and<br />
Systems, now in its eighth edition. He<br />
is also the editor and co-author of<br />
Fundamental Neuroscience for Basic and<br />
Clinical Applications, currently in its<br />
third edition.<br />
“At every medical center where he<br />
has held a faculty position, Dr. Haines<br />
has been extensively involved in teaching<br />
programs of his department. His many<br />
teaching awards span both undergraduate<br />
and graduate education.<br />
“Dr. Haines is a model educator and<br />
true scholar with a great heart for students.”<br />
John W. Pelley, PhD (Basic)<br />
Associate Professor of Cell Biology<br />
and Biochemistry, Texas Tech Health<br />
Sciences Center School of Medicine<br />
Dr. Pelley received his PhD in Zoology<br />
from the University of North Carolina.<br />
He joined TTUHSC in 1972 as assistant<br />
professor in Biochemistry.<br />
Dr. Pelley has received the President’s<br />
Excellence in Teaching Award twice<br />
at TTUHSC. He has also received the<br />
School of Nursing Dean’s award for<br />
teaching pathophysiology. He has received<br />
the SGEA Medical Education<br />
Scholarship Award for the Outstanding<br />
Presentation and the Award for Merit<br />
for Applications in Healthcare Education<br />
by the International Associate for<br />
Psychological Type.<br />
Dr. Steven L. Berk, dean of the<br />
School of Medicine, writes: “Dr. Pelley<br />
has achieved significant recognition for<br />
his teaching contributions both within<br />
and outside of the TTUHSC School of<br />
Medicine due to his use of innovations in<br />
the classroom such as concept mapping,<br />
question analysis and ‘prefrontal pauses.’<br />
<strong>The</strong>se teaching strategies are designed<br />
to develop the student’s ability to learn<br />
as well as to improve delivery of content.<br />
He has authored a popular USMLE Step<br />
1 review book, now in its third edition,<br />
and a course companion biochemistry<br />
book that is part of an integrated series<br />
(second edition in preparation).<br />
“Dr. Pelley’s teaching extends well<br />
beyond biochemistry. He has developed<br />
an expertise in learning theory and strategies<br />
in medical education. He developed<br />
his metacognitive approach to learning<br />
during his ten-year tenure as associate<br />
dean for Academic Affairs, which he<br />
documented in the book SuccessTypes in<br />
Medical Education, freely available at the<br />
SuccessTypes Medical Education Page<br />
(www.ttuhsc.edu/som/success/default.<br />
htm). Dr. Pelley is an active member<br />
of the international medical education<br />
listserve, DR-ED, the Southern Group<br />
on Educational Affairs, International<br />
Association of Medical Science<br />
Educators, and Team Based Learning<br />
Collaborative.”<br />
James R. Stallworth, MD (Clinical)<br />
Associate Professor, Department<br />
of Pediatrics, University of South<br />
Carolina School of Medicine<br />
Dr. Stallworth (AΩA, University<br />
of South Carolina, 1987) joined the<br />
University of South Carolina in 1979<br />
as an instructor in Pediatrics. He is<br />
currently associate professor in the<br />
Department of Pediatrics, Vice Chair<br />
for Education and Faculty Development,<br />
the M-III Pediatrics Clerkship Director,<br />
and Director of Student Recruitment.<br />
Dr. Richard A. Hoppmann, dean of the<br />
School of Medicine, writes: “<strong>The</strong>re is<br />
only a short list of names on the outstanding<br />
teachers list at the University<br />
of South Carolina School of Medicine.<br />
<strong>The</strong> name of Dr. James Stallworth is at<br />
the top of that list. A faculty member for<br />
over thirty years, he has become a legend<br />
among students, faculty, and alumni.<br />
Dr. Stallworth’s involvement in undergraduate<br />
education spans all four years<br />
of medical school, but he is best known<br />
for his role as M-III Pediatrics Clerkship<br />
Director, a position that he has held for<br />
twenty-seven years. <strong>The</strong> reason he remains<br />
clerkship director has nothing to<br />
do with lack of ambition, but everything<br />
to do with his passion for medical education<br />
and his desire to see every student<br />
reach their full potential and succeed as<br />
a physician. Over the years he has garnered<br />
tremendous respect from students<br />
for his straightforward, no-nonsense approach<br />
to pediatric clinical education,<br />
and for the high ethical and professional<br />
standards that he sets for himself and for<br />
students.<br />
“It is because of Dr. Stallworth that<br />
many of our students over the years have<br />
chosen to train as pediatricians. Former<br />
students would tell you about his caring<br />
and concern for his patients. <strong>The</strong>y would<br />
also tell that Dr. Stallworth could be<br />
quite intimidating, but he never let any<br />
of them give any less than their best for<br />
their patients and themselves.”<br />
Distinguished teacher nominees<br />
Patricia Lipford Abbitt, MD, University of<br />
Florida College of Medicine<br />
Ezra Amsterdam, MD, University of California,<br />
Davis, School of Medicine<br />
Charles L. Bardes, MD, Weill Cornell Medical<br />
College<br />
John B. Bass, Jr., MD, University of South<br />
Alabama School of Medicine<br />
David M. Clive, MD, University of<br />
Massachusetts Medical School<br />
Joseph C. Fantone, MD, University of Michigan<br />
Medical School<br />
Mark Christian Flemmer, MD, Eastern Virginia<br />
Barbara Freeman, PhD, Case Western Reserve<br />
University School of Medicine<br />
Joshua I. Goldhaber, MD, David Geffen School<br />
of Medicine at UCLA<br />
Stephen B. Greenberg, MD, MACP, Baylor<br />
College of Medicine<br />
Richard Gunderman, MD, PhD, MPH, Indiana<br />
University School of Medicine<br />
Jesse B. Hall, MD, University of Chicago<br />
Pritzker School of Medicine<br />
Thomas Karl Hoskison, MD, University of<br />
Oklahoma College of Medicine<br />
David C. Kaufman, MD, FCCM, University of<br />
Rochester<br />
James P. Keating, MD, Washington University<br />
in St. Louis School of Medicine<br />
Gary L. Kolesari, MD, PhD, Medical College of<br />
Wisconsin<br />
Susan Lehmann, MD, Johns Hopkins University<br />
School of Medicine<br />
Ruth Levine, MD, University of Texas Medical<br />
Branch at Galveston<br />
Fred A. Lopez, MD, LSU Health Sciences<br />
Center School at of Medicine at New Orleans<br />
Salvatore Mangione, MD, Jefferson Medical<br />
College of Thomas Jefferson University<br />
Kathryn Montgomery, PhD, Northwestern<br />
University, <strong>The</strong> Feinberg School of Medicine<br />
David Muller, MD, Mount Sinai School of<br />
Medicine of New York University<br />
Dennis H. Novack, MD, Drexel University<br />
College of Medicine<br />
Mark T. O’Connell, MD, University of Miami<br />
Miller School of Medicine<br />
Noor A. Pirzada, MD, <strong>The</strong> University of Toledo<br />
College of Medicine<br />
Mark L. Savicakas, PhD, Northeastern Ohio<br />
University Colleges of Medicine and Pharmacy<br />
Maria C. Savoia, MD, University of California,<br />
San Diego, School of Medicine<br />
John S. Sergent, MD, Vanderbilt University<br />
School of Medicine<br />
Paul Shanley, MD, State University of New<br />
York Upstate Medical University College of<br />
Medicine<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 39
<strong>The</strong> Write a Poem for This Photo Contest was the brainchild of<br />
Ted Harris, who loved the intersection of images and imagery.<br />
<strong>The</strong> charming photograph illustrating the poems was taken<br />
by Dr. Anthony Shaw (AΩA, University of Virginia, 1980) of<br />
Pasadena, California.<br />
<strong>The</strong> winning poems in this year’s contest are:<br />
First prize: “Benevolent Instructions” by David R. Downs, MD.<br />
Second prize: “Commencement” by David F. Dozier, Jr., MD.<br />
Third prize: “Adolescent Choices” by H. J. Van Peenen, MD.<br />
Benevolent Instructions<br />
If I’ve told you once, I’ve told you twice<br />
It’s this way, Junior, to the ice.<br />
David R. Downs, MD<br />
Dr. Downs was elected to AΩA at the University of<br />
Wisconsin in 1957. His address is: 411 West Merrimac Street,<br />
Dodgeville, WI 53533-1409. E-mail: dbdowns@mhtc.net.<br />
40 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong><br />
W
����������������<br />
�<br />
�����������������<br />
�<br />
������������������<br />
Commencement<br />
I see him with his friend,<br />
Describing sights he’s just discovered.<br />
I feel a father’s pride<br />
As he revels in his furry youth.<br />
This is no time to tell him<br />
Of the Orca, or the sea’s<br />
Potential rage and power.<br />
I’ll keep my distance,<br />
Keep him safe by nudge<br />
And praising, and let him feel<br />
<strong>The</strong> buoyant joy of entering the water.<br />
Soon enough he’ll grow and hunt for food,<br />
And huddle with the family<br />
When the winter blizzards blast us.<br />
For now, he rules his world,<br />
But I’ll be watching.<br />
David F. Dozier, Jr., MD<br />
Dr. Dozier received his MD from Stanford University<br />
in 1961. His address is 5168 Mississippi Bar Drive,<br />
Orangevale, California 95662. E-mail: david_dozier@<br />
sbcglobal.net.<br />
Adolescent Choices<br />
Two friends are making up their minds.<br />
To stay or go? How compromise if<br />
Right wants out and Left wants stay?<br />
Which one of them for both decides?<br />
“That way,” Right points a furry wing,<br />
but Left is skeptical. He thinks<br />
Right too impulsive, immature,<br />
and leaving home so soon unwise.<br />
<strong>The</strong> next frame of the film will show<br />
them parting. Left will turn away,<br />
the good son going back to mother.<br />
(She’s at the photo’s edge, her head<br />
embroidered yellow, white, and red.)<br />
And Right the tempter, Right the other,<br />
will waddle to the right to seek<br />
whatever comes from being born<br />
with an impulsive stubborn streak.<br />
<strong>The</strong>se two age mates, once hatched together,<br />
once childhood friends and now half-grown,<br />
part frostily to grow alone<br />
into a harsh maturity.<br />
One to warm eggs on frozen feet.<br />
One be eaten by a seal.<br />
H. J. Van Peenen, MD<br />
Dr. Van Peenen’s address is 74 W. 29th Avenue,<br />
Apartment 1103, Eugene, Oregon 97405. E-mail:<br />
lkvanp@comcast.net.<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 41
<strong>The</strong> physician at the movies<br />
Peter E. Dans, MD<br />
Wall Street: Money Never Sleeps<br />
Starring Michel Douglas, Shia La Beouf, Josh Brolin, Carey<br />
Mulligan, Eli Wallach.<br />
Directed by Oliver Stone. Rated PG-13. Running time 133<br />
minutes.<br />
It’s hard to believe that the original Wall Street was released<br />
twenty-three years ago. Like <strong>The</strong> Godfather, it has achieved<br />
iconic status with its memorable Oscar-winning performance<br />
by Michael Douglas as Gordon Gekko and its signature line<br />
“Greed is good.” Gekko accumulates billions by wedding his<br />
belief that “information is the most valuable commodity” with<br />
a philosophy based on the writings of the sixth-century-BC<br />
Chinese warlord Sun Tzu. As Gekko tells his protégé Bud<br />
Fox (Charlie Sheen), “I don’t just throw darts at a board. Read<br />
Sun Tzu’s <strong>The</strong> Art of War. Every battle is won before it is ever<br />
fought.” To Gekko, the game is “not about the money; it’s<br />
about the game between people.” In short, it’s about winning,<br />
or in the words of a popular phrase of the time, “the one<br />
who dies with the most toys wins.”<br />
Not surprisingly, the sales of <strong>The</strong> Art of War,<br />
which is still used in war colleges, skyrocketed after<br />
the film as Gekko wannabes tried to absorb<br />
some of its lessons. In the original movie,<br />
Shia La Beouf in Wall Street: Money Never Sleeps.<br />
20th Century-Fox/Photofest<br />
Gekko is brought down by Fox who, after he is caught doing<br />
insider trading, saves his hide by wearing a wire to incriminate<br />
Gekko. Before being sent to prison, Gekko sequesters $100<br />
million in a Swiss account in his children’s names.<br />
<strong>The</strong> sequel begins in October 2001 at Sing Sing, where<br />
Gekko is released after having served his eight-year sentence<br />
for insider trading and securities fraud. He reclaims his possessions,<br />
including an out-of-date cell phone and, when no<br />
one is there to meet him, he takes a cab back to “the city.” <strong>The</strong><br />
scene shifts to 2008 with two Gen Xers in bed as the morning<br />
news comes on the television. <strong>The</strong> woman is Gekko’s estranged<br />
daughter Winnie, who angrily shuts off the TV upon<br />
hearing that Gekko is back in the limelight promoting his<br />
book Is Greed Good? Winnie used to visit her father regularly<br />
in prison until her brother died of a drug overdose that she<br />
blamed on her father. As seeming recompense for Gordon’s<br />
sins, she has become a blogger for an anti-corporate website,<br />
Frozen Truth. Her live-in boyfriend, Jake Moore (Shia La<br />
Beouf), insists that she ought to hear about him, but she wants<br />
none of it. Jake, it turns out, is an up-and-coming Wall Street<br />
trader whose “saving grace” is his championing of alternative<br />
energy technology to save the planet. He is employed by the<br />
firm Keller/Zabel (KZI), headed by a one-time powerful figure<br />
Louis Zabel (Frank Langella), to whom Jake is devoted. Zabel<br />
42 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
dodges Jake’s questions about rumors that KZI is on the brink<br />
of insolvency, saying, “Are we going under? That’s the wrong<br />
question. Who isn’t?” He ends the conversation by giving Jake<br />
a $1.45 million bonus, telling him to enjoy it. Jake uses part<br />
of it to buy Winnie an engagement ring (although he knows<br />
she’s against marriage) and to go out partying. He decides to<br />
plow the rest into KZI despite a friend’s warning that the firm,<br />
having kept subprime mortgage toxic debt off its books, is in<br />
danger of collapse.<br />
Enter Bretton James (Josh Brolin), the CEO of Churchill<br />
Schwartz, a fictional firm meant to represent a combination<br />
of Goldman Sachs and J.P. Morgan. By refusing to support a<br />
bailout for KZI, he engineers its destruction as a payback for<br />
Zabel’s not bailing out Churchill Schwartz eight years before<br />
under similar circumstances. <strong>The</strong>re are ominous meetings of<br />
the Federal Reserve Commission in New York as Zabel unsuccessfully<br />
tries to trade on old loyalties and friendships by<br />
pleading his case before the group that holds his fate in their<br />
hands. <strong>The</strong>re are a couple of great scenes on the Upper West<br />
Side in Central Park and the subway, involving a distraught<br />
Zabel and Jake.<br />
Re-enter Gekko as he goes on the lecture circuit to Fordham<br />
Business School to publicize his book. He tells the students<br />
that “money is a bitch that never sleeps and she is jealous.” He<br />
reiterates his old axiom that greed is good, but too much is<br />
not, and that greed is legal. He notes that forty percent of the<br />
nation’s profits come from financial services, not production<br />
of goods, principally involving what he calls “banks on steroids.”<br />
Jake goes up to him after the lecture and tells him that<br />
he is engaged to Winnie. <strong>The</strong>y ride the subway together and<br />
forge a quid pro quo arrangement in which Gekko helps Jake<br />
unravel the steps leading to the destruction of KZI in return<br />
for trying to reconcile him with his daughter. This grafting<br />
of a love affair, such as it is, onto the picture’s main theme of<br />
the convoluted machinations of the Wall Street traders never<br />
really works. It seems like an attempt to reach a younger audience<br />
while showing that Gekko has some humanity (although<br />
not much). He is not averse to duping his daughter and Jake<br />
to get back his $100 million, which he promptly turns into $1<br />
billion, showing that he hasn’t lost his old touch.<br />
<strong>The</strong> film is filled with what might be called “inside baseball,”<br />
with references to the cutthroat side of the financial<br />
world with its own arcane language of credit default swaps,<br />
hedge funds, derivatives, bundling subprime mortgages, and<br />
toxic debt. At the time, these terms were totally unfamiliar to<br />
the majority of the public whose retirement funding depended<br />
on their effects on the markets. <strong>The</strong>y were also ignored by the<br />
numerous public watchdogs at the Federal Reserve, the relevant<br />
Congressional committees, and the SEC until the crisis<br />
exploded into public consciousness in 2008. <strong>The</strong>re are also<br />
the references to banks being “too big to fail” and their being<br />
given bailouts in which they are awarded 100 cents on the<br />
dollar while investors are short-changed. This illustrates the<br />
concept of “moral hazard”—someone takes your money and<br />
acts differently when insulated from risks than he would if he<br />
were fully responsible for losses. <strong>The</strong> comment in the film is<br />
that it is “unethical but not illegal.”<br />
Though long, the film held my interest throughout. What<br />
is particularly good about it is the acting, first by Douglas<br />
who looks as old, tired, and sick as he is in real life. Look for<br />
another Best Actor Oscar, possibly posthumously. Next is the<br />
outstanding supporting cast. Frank Langella is great as an old<br />
Lion being eaten alive by the unscrupulous young shark played<br />
by Josh Brolin. Eli Wallach is also great as Jules Steinhardt, another<br />
old Lion, who looks half-dead but is still in control, just<br />
as he was in <strong>The</strong> Godfather until he got bumped off by that<br />
cannoli. As he drops his little pearls, he emits a little whistle,<br />
one of the best touches in the film that I have to believe he improvised.<br />
Susan Sarandon is less effective as Jake’s mother, who<br />
is forever cadging money from her son for failed real estate<br />
schemes. Also look for Oliver Stone, who pulled a Hitchcock<br />
by appearing in both films as a trader. <strong>The</strong>re are many shots<br />
of New York’s buildings and a little taste of sex, drugs, and<br />
materialistic excess as the young lions get outrageous bonuses.<br />
Oliver Stone is one of my bête noirs. His outlandish attempts<br />
to rewrite history, his admiration for Castro and Chavez, and<br />
his inane pronouncements characterizing Hitler as simply a<br />
“product of his time” and extolling the “good” side of Stalin,<br />
have discredited him in my view. Still, I must commend him<br />
for clearly being ahead of the curve with these two films.<br />
He was filming the first one in 1985 and released it in 1987,<br />
when the financial crash occurred. As for the second, he was<br />
promptly on the case of the 2008 debacle in that the film began<br />
shooting that year. He also has highlighted the fact that<br />
wealth in America was once based on the production of goods.<br />
That has changed in the computer age, when information<br />
can make or break individuals and companies and paper has<br />
replaced tangible goods as the currency of wealth. He presumably<br />
learned that lesson from his father, who was a broker at<br />
Shearson Lehman into the 1980s. Maybe he should give up<br />
making pictures and be “the canary in the coal mine” in the<br />
corner at those federal watchdog group meetings.<br />
Conviction<br />
Starring Hilary Swank, Sam Rockwell, Minnie Driver, Juliette<br />
Lewis and Peter Gallagher.<br />
Directed by Tony Goldwyn. Rated R. Running time 107 minutes.<br />
I<br />
’m conflicted about Conviction. I attended a screening with<br />
a friend and if I had driven my own car, I would have been<br />
gone after the first fifteen minutes. If I had been watching it<br />
at home, I certainly would have gonged it. Here’s why. <strong>The</strong><br />
film opens in 1980 with a long handheld camera sequence<br />
panning over a grisly, blood-soaked murder scene in Ayer,<br />
Massachusetts, where a woman named Katharina Brow had<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 43
<strong>The</strong> physician at the movies<br />
been stabbed over thirty times. This is followed by rapid<br />
clips of two children, Kenny and Betty Anne Waters, stealing<br />
from and trashing the lady’s house, getting punished by their<br />
mother who gave birth to nine children by seven fathers, and<br />
being sent to foster homes, intercut with scenes of them as<br />
adults. Kenny (Sam Rockwell) is clearly a certifiable sociopath,<br />
alternating between turning on the charm and acting out his<br />
violent temper. He is repeatedly taken into custody by policemen<br />
who profess to like him and excuse his behavior. <strong>The</strong><br />
scene that really turned me off was where he is in a bar dancing<br />
with his little child in his arms at a family celebration. A<br />
person he accidentally knocks into questions his taking such<br />
a toddler into a bar and at that time of night. Kenny slowly<br />
puts his child down and goes over and punches out the guy’s<br />
lights. <strong>The</strong>n he turns on the charm by buying everyone a drink<br />
and does a full striptease to the amusement of his family and<br />
the patrons. I found this scene hard to believe as well as to<br />
stomach.<br />
After the woman is killed, Kenny is confronted by the police<br />
and detective Nancy Taylor (Melissa Leo) while sawing<br />
wood at his home next door to the murder scene. He fights<br />
being arrested and although he has an alibi, Taylor, whom he<br />
taunts, is seemingly out to get him. Two years later during the<br />
funeral for his grandfather in a Catholic Church, the police<br />
march down the aisle and interrupt the service to haul him off<br />
to jail in handcuffs. I’ve lived in Massachusetts and that just<br />
wouldn’t happen. I realize that this is a movie where the story<br />
is fictionalized, but this whole setup is ludicrous.<br />
I hung in for the rest of the story, which was fairly predictable<br />
but did raise some interesting issues. Kenny is brought<br />
to trial; the evidence consists of his having blood type O, the<br />
same as the perpetrator, and testimony that he had indeed<br />
been the killer by two ex-girl friends, one of whom he was<br />
living with at the time and with whom he had had a child. In<br />
1983, he is sentenced to life without parole. His sister Betty<br />
Anne (Hilary Swank) is sure he is innocent and devotes her life<br />
to exonerating him. A high school dropout, she gets her GED,<br />
a bachelor’s degree, and a law degree from Roger Williams<br />
Law School. With the help of law school classmate Abra Rice<br />
(Minnie Driver) and Barry Scheck (Peter Gallagher), cofounder<br />
of the Innocence Project, she uses DNA evidence to<br />
exonerate Kenny in 2001 after eighteen years of incarceration.<br />
During this period her devoted husband leaves her because<br />
of her obsession on behalf of her brother and all the time<br />
that her studies take away from the family. Her two children<br />
receive little attention, given her time at school and work as<br />
a waitress in a bar. <strong>The</strong> children ask to live with their father,<br />
although they appear to come back to her when he remarries.<br />
It’s particularly interesting that all the publicity and reviews<br />
refer to her doing this as a “single mom,” but she certainly<br />
didn’t start out that way.<br />
<strong>The</strong> film ends when Kenny is freed and reunited with his<br />
daughter, who had been estranged from him presumably<br />
because his weekly letters were intercepted by her mother<br />
and she believed that he was the killer. <strong>The</strong> filmmakers don’t<br />
mention that Kenny died six months after his release. <strong>The</strong><br />
few write-ups that do mention his death say only that he died<br />
“tragically,” without giving the details. Actually, he died scaling<br />
a fifteen-foot fence taking a shortcut to a convenience<br />
store. He fell on his head and was later found dead. In 2009,<br />
the town of Ayer settled his estate’s civil rights suit for $3.4<br />
million.<br />
In addition to those cited earlier, there were other problems<br />
with this movie. First of all, I was puzzled by how little attention<br />
was paid to developing Taylor’s character to gain insights<br />
into her willingness to frame Kenny as well as at least one<br />
other person. <strong>The</strong> only reason posed is that it was tough being<br />
a female detective in those days. Really! Does that justify<br />
framing people? Would they have us believe that women who<br />
pioneered in those positions had to do that to gain awards?<br />
That’s an insult to them. In addition, she seemed to have suffered<br />
no consequences beyond being given a desk job.<br />
I was also struck by the lack of attention to solving the<br />
murder. <strong>The</strong> police spent two fruitless years investigating a<br />
murder that cried out for seeking someone who knew the<br />
victim and hated her with a passion. Given all the evidence<br />
at the crime scene, consisting of fingerprints, hair, and blood,<br />
they dawdled before nailing the wrong guy. <strong>The</strong>re was also<br />
no mention of using the DNA database even though it was<br />
operational years later. <strong>The</strong> emphasis was on exoneration, not<br />
solving the murder. Not only that, but the producers never<br />
met with the victim’s children to tell them of the movie, which<br />
justly troubled them, another example of how negligent they<br />
were in touching base with the principals in the case except<br />
for Betty Anne Waters.<br />
Okay, what are the redeeming features? First, the acting.<br />
Hilary Swank, who is in almost every scene, although she<br />
never seems to age, gives an earnest if unexceptional performance.<br />
Still, I predict she will earn an Oscar nomination in<br />
this year’s Erin Brockovich secular saint category. Much better<br />
is Juliette Lewis in a small role as Roseanna Perry, a reclusive<br />
alcoholic girlfriend with rotten teeth and a loopy demeanor<br />
who is persuaded by Taylor to testify that Kenny was the killer.<br />
Interestingly, Lewis never met the actual person she plays and<br />
a blogger who knew the woman said neither she nor her teeth<br />
were anything like what was portrayed in the film, although<br />
Kenny did knock out two teeth which she got replaced.<br />
Getting the story right seems to take a back seat to an Oscar<br />
nominating performance. By contrast, Sam Rockwell gives a<br />
riveting pull-out-all-the-stops performance that doesn’t sugarcoat<br />
Kenny. He should win the Academy award for Best Actor,<br />
given that the Academy loves anti-heroes, especially those that<br />
are somewhat depraved. Rockwell drew from his hardscrabble<br />
youth as a rebel in a home broken by divorce when he was<br />
five and as someone who committed petty crimes, to create<br />
a character who alternates between Dr. Jekyll and Mr. Hyde.<br />
44 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
Hilary Swank and Sam Rockwell in Conviction. Photo by Ron Batzdorf.<br />
<strong>The</strong> film also shows how misleading evidence based on<br />
blood typing was in the days before DNA testing was available.<br />
<strong>The</strong> film credits Barry Schenk and the Innocence Project<br />
he co-founded in 1992 at Cardozo School of Law of Yeshiva<br />
University in 1992 for providing the guidance that got Kenny<br />
off. <strong>The</strong>y receive thousands of requests per year and have been<br />
able to use DNA evidence, as of November 2, 2010, to exonerate<br />
261 convicted felons, some of whom had been on death<br />
row. This figure is impressive, and I couldn’t help but marvel<br />
at the fact that DNA evidence could be exculpatory but in the<br />
case of O.J. Simpson insufficient to obtain his conviction, in<br />
part because DNA testing was impugned by the defense.<br />
Finally, there is an interesting sidebar involving Martha<br />
Coakley, the attorney general of Massachusetts who lost the<br />
senatorial contest to Scott Brown in 2010. She is portrayed as<br />
a villain because she was presumably the Middlesex County<br />
District Attorney (DA) when Taylor framed Kenny, and who<br />
gave Taylor an award. She’s also shown stonewalling the performance<br />
of the DNA testing and then refusing to act on the<br />
results when the DNA evidence exonerated him. Actually,<br />
she didn’t become the Middlesex County DA until 1998.<br />
Furthermore, her office not only facilitated the testing and<br />
a second test to corroborate it but she moved to vacate the<br />
conviction three days after receiving the test results and he<br />
was freed within two weeks. After a screening, she graciously<br />
complimented Swank and ascribed the misrepresentation<br />
to the need to telescope events in movies. She cheerfully<br />
lamented that it hadn’t been a good year for her. 2 It’s hard<br />
to understand the motives of the director and screenwriter.<br />
I am not a litigious person but I would sue for defamation of<br />
character, especially since the film opened two weeks before<br />
she stood for re-election as Massachusetts Attorney General.<br />
References<br />
1. <strong>The</strong> Innocence Project—About Us: Mission Statement. www.<br />
innocenceproject.org/about/Mission-Statement.php.<br />
2. Gelzinis P. Martha Coakley: Movie’s “inaccurate” but a<br />
“delight.” news.bostonherald.com/news/columnists/view.<br />
bg?articleid=1288682.<br />
Dr. Dans (AΩA, Columbia University College of Physicians and<br />
Surgeons, 1960) is a member of <strong>The</strong> <strong>Pharos</strong>’s editorial board and<br />
has been its film critic since 1990. His address is:<br />
11 Hickory Hill Road<br />
Cockeysville, Maryland 21030<br />
E-mail: pdans@comcast.net<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 45
Reviews and reflections<br />
David A. Bennahum, MD, and Jack Coulehan, MD, Book Review Editors<br />
<strong>The</strong> Checklist Manifesto: How<br />
To Get Things Right<br />
Atul Gawande<br />
New York, Metropolitan Books, 2009<br />
Reviewed by David A. Bennahum,<br />
MD (AΩA, University of New Mexico,<br />
1984)<br />
In <strong>The</strong> Checklist Manifesto, his latest<br />
lucid and elegantly written analysis<br />
of how to improve health care, Atul<br />
Gawande addresses the idea that the<br />
simple introduction of checklists to patient<br />
care can reduce costs and save<br />
lives. In each of his books and essays<br />
Gawande has engaged the reader’s interest<br />
with stories that illustrate specific<br />
points and problems. Here he begins<br />
with a surgical case that had been<br />
recounted to him by a physician<br />
colleague about a patient who<br />
had almost exsanguinated<br />
from an abdominal stab<br />
wound so deep it had<br />
cut the aorta.<br />
<strong>The</strong>re are a thousand ways that<br />
things can go wrong when you’ve<br />
got a patient with a stab wound. But<br />
everyone involved got almost every<br />
step right—the head-to-toe examination,<br />
the careful tracking of the<br />
patient’s blood pressure and pulse<br />
and rate of breathing, the monitoring<br />
of his consciousness, the fluids<br />
run in by IV, the call to the blood<br />
bank to have blood ready, the placement<br />
of a urinary catheter to make<br />
sure his urine was running clear,<br />
everything. Except no one remembered<br />
to ask the patient or the emergency<br />
medical technicians what the<br />
weapon was.<br />
“Your mind doesn’t think of a<br />
bayonet in San Francisco,” John<br />
could only say. p3<br />
<strong>The</strong> staff knew that the patient had<br />
been stabbed, but he was comfortable<br />
and talking so no one thought to ask<br />
with what and then consider the possible<br />
consequences of a deep stab wound.<br />
In the second case, a patient undergoing<br />
surgery to remove a cancer of the<br />
stomach suddenly went into cardiac<br />
arrest. Because the patient had a low<br />
potassium before surgery the anesthesiologist<br />
had given him corrective dose of<br />
potassium. Gawande in his understated<br />
but dramatic style quotes the surgeon.<br />
I was chagrined at having missed<br />
this. An abnormal level of potassium<br />
is a classic cause of asystole.<br />
It’s mentioned in every textbook.<br />
I couldn’t believe I overlooked it.<br />
Severely low potassium levels can<br />
stop the heart, in which case a cor-<br />
rective dose of potassium is the remedy.<br />
And too much potassium can<br />
stop the heart, as well—that’s how<br />
the states execute prisoners.<br />
<strong>The</strong> senior anesthesiologist<br />
asked to see the potassium bag that<br />
had been hanging. Someone fished<br />
it out of the trash and that was when<br />
they figured it out. <strong>The</strong> anesthesiologist<br />
had used the wrong concentration<br />
of potassium, a concentration<br />
one hundred times higher than he’d<br />
intended. He had, in other words,<br />
given the patient a lethal dose of<br />
potassium. p6<br />
<strong>The</strong> patient was lucky and survived,<br />
but Gawande uses these stories to argue<br />
for a simple method to prevent such<br />
errors, a checklist. In the first chapter<br />
he writes about problems of extreme<br />
complexity and how training and practice<br />
can achieve astonishing results;<br />
but he argues that in medicine we expect<br />
miracles such as that offered by<br />
penicillin. We have lost the discipline<br />
that a methodical approach requires.<br />
More than 50 million operations are<br />
performed annually in the United States<br />
and Americans undergo an average of<br />
seven operations in a lifetime. Yet we<br />
suffer 150,000 post-surgical deaths each<br />
year. Gawande writes:<br />
Moreover, research has consistently<br />
showed that at least half our deaths<br />
and major complications are avoidable.<br />
<strong>The</strong> knowledge exists. But<br />
however supremely specialized and<br />
trained we may have become, steps<br />
are still missed. Mistakes are still<br />
made. p31<br />
46 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
To better understand this idea<br />
Gawande turns to the introduction<br />
of checklists in 1935 by the U.S. Army<br />
Aircorps when it was flight-testing the<br />
aircraft that would become the B17<br />
bomber, the famous Flying Fortress.<br />
After a number of flight failures the<br />
aeronautical engineers realized that the<br />
complexity of the modern airplane required<br />
not better test pilots but rather<br />
a simple method to prevent mistakes,<br />
the checklist. He follows this by reminding<br />
the reader of the four vital signs to<br />
which a fifth sign, pain, has recently<br />
been added and asks whether these are<br />
not checklists that guide nurses.<br />
Gawande recounts the remarkable<br />
experience of Dr. Peter Pronovost at<br />
Johns Hopkins in 2001. Provonost identified<br />
five steps that a physician must<br />
take to place a central line and then<br />
asked the nurses to observe whether<br />
every physician unfailingly followed<br />
each step. In more than a third of the<br />
patients, doctors skipped at least one.<br />
Pronovost then persuaded the hospital<br />
administration to allow the nurses to<br />
stop any physician who had skipped a<br />
step. Over the next year “the ten-day<br />
line-infection rate went from 11 percent<br />
to zero.” p38 Only two line infections<br />
occurred over the next fifteen months!<br />
Pronovost had proven that checklists<br />
raised baseline performance.<br />
Gawande then goes on to explore the<br />
use of checklists in several industries<br />
and the literature on complexity. He<br />
reports that researchers have defined<br />
three categories of problems: simple,<br />
such as baking a cake; complicated,<br />
such as sending a rocket to the moon;<br />
and complex, such as raising a child. He<br />
notes the evidence in favor of checklists<br />
for simple and complicated problems,<br />
then asks whether checklists are also<br />
helpful in situations of great complexity.<br />
To address that question he cites<br />
data from the building industry about<br />
the construction of massive skyscrapers.<br />
And there again he found checklists<br />
at every level and “an annual avoidable<br />
failure rate of less than 0.00002 percent.”<br />
p71<br />
Gawande finds that checklists “are<br />
not comprehensive how-to guides,<br />
whether for building a skyscraper or<br />
getting a plane out of trouble. <strong>The</strong>y<br />
are quick and simple tools aimed to<br />
buttress the skills of expert professionals.”<br />
p128 He writes that on January 14,<br />
2009 the World Health Organization<br />
came out with a “Safe Surgery” checklist.<br />
<strong>The</strong> very next day Captain Chesley<br />
B. Sullenberger III saved U.S. Airways<br />
Flight 1549 after a flock of Canada geese<br />
flew into and stalled his aircraft’s engines.<br />
While the cool demeanor, good<br />
judgment, and experience of the pilots<br />
and crew were crucial, no less so were<br />
the years of attention to detail and the<br />
relentless discipline of their aviation<br />
checklists.<br />
This is a marvelous and elegant<br />
book. It is an important if very simple—<br />
but not simplistic—contribution to the<br />
medical literature, as is almost everything<br />
that Gawande writes. While most<br />
of the book focuses on the application<br />
of checklists to technical practice, there<br />
is one point that I found very appealing.<br />
Gawande describes that as a surgeon<br />
introducing the checklist to his own<br />
surgical teams he now asks that they<br />
begin each operation by reintroducing<br />
themselves to each other, thereby leveling<br />
the distinctions between physicians,<br />
nurses, and technicians and creating<br />
a team of the moment for the benefit<br />
of the patient. Captain Sullenberger<br />
pointed out that he and his crew were<br />
also a team, each equally important to<br />
the final outcome. At the core of <strong>The</strong><br />
Checklist Manifesto is a plea for an ethic<br />
of relationship between individuals who<br />
work together on any project and especially<br />
for those with a commitment to<br />
excellent patient care.<br />
Dr. Bennahum is a book review editor for<br />
<strong>The</strong> <strong>Pharos</strong> and a member of its editorial<br />
board. He is emeritus professor of Internal<br />
Medicine at the University of New Mexico<br />
School of Medicine. His address is:<br />
1707 Notre Dame Drive NE<br />
Albuquerque, New Mexico 87106<br />
E-mail: dbennahum@salud.unm.edu<br />
<strong>The</strong> Jump Artist<br />
Austin Ratner<br />
New York, Bellevue Literary Press, 2009<br />
Reviewed by Jeffrey L. Ponsky,<br />
MD (AΩA, Case Western Reserve<br />
University, 1971)<br />
I n the tradition of Chekhov, Somerset<br />
Maugham, and William Carlos<br />
Williams comes another MD who writes<br />
beautiful and compelling literary fiction.<br />
Austin Ratner, a graduate of Johns<br />
Hopkins Medical School, turned to fiction<br />
as a career after receiving his MD.<br />
His debut novel, <strong>The</strong> Jump Artist is a<br />
worthy addition to the ranks of literary<br />
historical fiction.<br />
<strong>The</strong> history that forms the basis for<br />
the novel is fascinating and largely unknown.<br />
Philippe Halsman was a young<br />
Latvian Jew hiking with his father in<br />
the Tyrolean Alps when his father<br />
fell to his death while walking behind<br />
Philippe on the hiking path. In an affair<br />
dubbed in Europe “<strong>The</strong> Austrian<br />
Dreyfuss Affair,” Philippe was arrested<br />
and convicted of his father’s murder<br />
and imprisoned in an Austrian jail for<br />
two years, despite only circumstantial<br />
evidence. <strong>The</strong> young, still adolescent<br />
Halsman was thrown into a world of<br />
horror and only released by a pardon,<br />
not an exoneration, after the tireless<br />
efforts of his sister Liouba and the assistance<br />
of human rights activists all<br />
over the world, including such notables<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 47
Reviews and reflections<br />
as Albert Einstein, Thomas Mann, and<br />
Eleanor Roosevelt. After being released<br />
from prison, the young Halsman was<br />
expelled from Austria permanently and<br />
went to Paris, to try fulfill his father’s<br />
dream for him of becoming an engineer<br />
or doctor. After much struggle, Philippe<br />
became a well-known Parisian photographer,<br />
only to flee Paris as the Nazis invaded.<br />
Penniless and stateless, Philippe<br />
emigrated to the United States and rose<br />
to become one of the country’s most<br />
celebrated photographers of the 1950s<br />
and 1960s. His name may be unfamiliar,<br />
but his work we all know: the famous<br />
headshot of Albert Einstein, Marilyn<br />
Monroe in a white dress backed into a<br />
corner, Salvador Dali with the curling<br />
moustache, the Duke and Duchess of<br />
Windsor jumping in the air. Halsman<br />
had more Life magazine covers to his<br />
credit than any photographer in history.<br />
<strong>The</strong> story of <strong>The</strong> Jump Artist is<br />
compelling as an arc from despair to<br />
triumph, but it is not in the straightforward<br />
telling of the story that this strong<br />
debut novel succeeds. Rather, Ratner<br />
writes the inner life of a human being<br />
who has experienced a level of trauma<br />
beyond imagination. His vivid descriptions<br />
of prison, of helplessness, and of<br />
the unearned, but agonizingly felt, guilt<br />
of a victim and survivor are so richly<br />
imagined that the reader feels that he<br />
comes to know the interior Halsman.<br />
We feel his adolescent struggles with<br />
a father whom he loved and venerated<br />
but was irritated by, his haunting sense<br />
of loss, his shocked passivity in the face<br />
of victimization, and his self-loathing,<br />
so common in victims of trauma. As<br />
he tries to make sense of his surreal<br />
experience, he moves to art just as the<br />
surrealist movement is gaining sway in<br />
Europe, and his use of the camera begins<br />
to move him into the outside world.<br />
<strong>The</strong> camera captures the full range of<br />
human emotion, from the surreal to<br />
the playful to the beautiful. As Halsman<br />
slowly allows love and art into his life,<br />
he reclaims his life. Ratner’s use of language<br />
and his strong artistic storytelling<br />
draws the reader deep into Halsman’s<br />
world and, as the novel builds, we root<br />
for his success, hoping he will overcome<br />
the tragedy of his youth. It is not just the<br />
story that stays with you, it is Halsman<br />
the human being.<br />
As physicians we are always struggling<br />
to understand the human condition.<br />
This stunning novel does what all<br />
truly fine novels should do. It illuminates<br />
an understanding of the human<br />
condition through its moving exploration<br />
of trauma, suffering, and redemption.<br />
Dr. Ponsky is the Oliver H. Payne Professor<br />
and chairman of the Department of<br />
Surgery at Case Western Reserve University<br />
and the Surgeon-in-Chief of University<br />
Hospital at Case Medical Center in Cleveland.<br />
His address is:<br />
University Hospitals, Case Medical<br />
Center<br />
Department of Surgery<br />
11100 Euclid Avenue, LKS-5047<br />
Cleveland, Ohio 44106<br />
E-mail: jeffrey.ponsky@uhhospitals.org<br />
Henry Kaplan and the Story of<br />
Hodgkin’s Disease<br />
Charlotte De Croes Jacobs<br />
Stanford, California, Stanford University<br />
Press, 2010<br />
Reviewed by William M. Rogoway,<br />
MD<br />
<strong>The</strong> 1960s and early ’70s were times<br />
of significant change in the approach<br />
to cancer therapy in this country.<br />
As the hazards and potential benefits of<br />
radiation therapy became more widely<br />
appreciated, it became a powerful treatment<br />
tool. At the same time, drugs were<br />
developed that not only led to tumor<br />
shrinkage, but, in the case of childhood<br />
leukemia, could eradicate disease.<br />
Henry Kaplan was a towering figure in<br />
this heady time of oncologic creativity.<br />
Charlotte Jacobs traces Kaplan’s beginnings<br />
in Chicago as the older son<br />
of Russian immigrants, recounting the<br />
early death of his father and his determined<br />
mother’s struggles to keep the<br />
family afloat financially and to further<br />
her favorite child’s ambitious goals. This<br />
story is interwoven with the history of<br />
the gradual recognition of Hodgkin’s<br />
disease as an entity, from Thomas<br />
Hodgkin’s original cases to Dorothy<br />
Reed’s defining pathologic description,<br />
as well as the development of radiation<br />
therapy from a scientific curiosity to a<br />
therapeutic tool. By the time Dr. Kaplan<br />
graduated from Rush Medical College<br />
in 1941, a rudimentary understanding<br />
of the disease with which he became so<br />
identified existed and radiotherapy had<br />
been used as treatment.<br />
Dr. Jacobs outlines Henry Kaplan’s<br />
rapid professional trajectory from<br />
trainee to chairman of Radiology at<br />
Stanford Medical School at age twentynine;<br />
the remainder of the book is devoted<br />
to his diverse and impressive<br />
scientific and personal achievements.<br />
<strong>The</strong> over-riding theme is that of a brilliant<br />
physician driven to ever-more ambitious<br />
goals.<br />
Where does one begin? <strong>The</strong> Stanford<br />
linear accelerator that permitted higher<br />
energy and more targeted x-ray therapy,<br />
the willingness to deliver higher doses<br />
of radiation to wider fields in the quest<br />
for Hodgkin’s disease cure, the identification<br />
of the mouse leukemia virus and<br />
the search for a human viral etiology for<br />
malignancy, attempts to create antibodies<br />
to human tumors. Kaplan gained<br />
48 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
credit for all these, sometimes leaving<br />
the contributions other investigators<br />
played in these advances forgotten or<br />
little noted. While he played a pivotal<br />
role in the clinical development of the<br />
accelerator and aggressively pushed its<br />
use forward, other clinicians at other<br />
centers were moving in the same direction.<br />
Dose escalation and contiguous<br />
uninvolved field therapy built heavily on<br />
the work of the Canadian Vera Peters,<br />
and an understanding of the logical<br />
pattern of Hodgkin’s disease spread was<br />
very much a product of his colleague<br />
Saul Rosenberg. Kaplan never did identify<br />
the elusive human tumor virus and<br />
monoclonal antibody success was left<br />
to others.<br />
Kaplan’s lasting scientific achievement<br />
was the rigorous investigation of<br />
Hodgkin’s disease. He and his associates<br />
pioneered the randomized clinical trial,<br />
answering one question and proceeding<br />
to the next in single institution studies<br />
with the single-minded goal of curing<br />
the disease and lessening the complications<br />
of therapy.<br />
Concurrent with his science, HSK, as<br />
his associates knew him, attempted to<br />
reshape Stanford’s medical school in his<br />
image. From the time he became chairman<br />
of Radiology, he assumed a leadership<br />
role in creating a research-oriented<br />
school as the university moved its medical<br />
school campus from San Francisco<br />
to Palo Alto. He was instrumental in recruiting<br />
a sterling faculty that included<br />
three future Nobel Laureates. As his<br />
department grew, he envisioned a nationally<br />
sanctioned comprehensive cancer<br />
center, but as his dream threatened<br />
to dominate the school, close colleagues<br />
withdrew support and the center never<br />
happened. This was a devastating and<br />
embittering defeat. His struggles, sometimes<br />
very contentious, with deans and<br />
other faculty were legendary, his failures<br />
and successes are carefully chronicled.<br />
<strong>The</strong>re were forays as well in the national<br />
scientific scene and HSK played<br />
a key role in refining the 1971 National<br />
Cancer Act that paved the way for a<br />
dramatic increase in funding for cancer<br />
research and NCI independence.<br />
Throughout his career, HSK developed<br />
a few close professional and<br />
personal relationships. <strong>The</strong>se were significant<br />
scientists whose common characteristic<br />
seemed to be the same drive,<br />
ambition, and dismissiveness toward<br />
others less forceful. Perhaps most interesting<br />
is the thorough account of his<br />
evolving friendship with Dr. Vincent<br />
DeVita, who was key in developing curative<br />
combination drug therapy for<br />
Hodgkin’s disease that rivaled Stanford’s<br />
radiotherapy efforts and who ultimately<br />
became the director of the National<br />
Cancer Institute. In interviewing over<br />
one hundred of his colleagues, patients,<br />
friends, and family members, Dr. Jacobs<br />
was able to bring detail to HSK’s fascinating<br />
and multifaceted life and his<br />
impact on others. Particularly revealing<br />
are first-person recollections of confrontations<br />
with associates and friends<br />
whose views differed from his. His<br />
close, though imperfect, relationship<br />
with his children is tenderly presented.<br />
Dr. Jacobs has authored a loving account<br />
of a powerful figure. While the<br />
chronology is painstaking, I’m not sure<br />
that one comes away with a balanced<br />
picture of this giant of American medicine.<br />
As Dr. Jacobs writes toward the<br />
end of her book, “anonymity wasn’t<br />
Henry’s way. If you had the chance to<br />
reach your goal, you grabbed it.” p310 He<br />
began poor with a very visible physical<br />
deformity, a brilliant mind and a desire<br />
to achieve. He worked tirelessly and<br />
with tremendous self-assurance built<br />
a scientific career that was outstanding.<br />
While not detailed in the book, at<br />
a time when radiation oncology was a<br />
relatively new discipline, his early trainees<br />
became department chairs at half<br />
a dozen academic medical centers. He<br />
had talents and a drive beyond most,<br />
but alienated many associates and his<br />
own brother. While warm and compassionate<br />
toward patients, he could be dismissive<br />
to associates. While he was very<br />
public in much of what he did professionally,<br />
his humanitarian work was carried<br />
out with much less flourish. He was<br />
a complex and flawed man, but indeed<br />
a visionary who brought a scientific<br />
rigor to the practice of oncology and<br />
helped move Hodgkin’s disease from an<br />
untreatable malignancy to one for which<br />
cure is now the rule. Dr. Jacobs’ book is<br />
a riveting read, meticulously covering a<br />
time of dramatic creativity in American<br />
medicine while also revealing the personal<br />
infighting that took place behind<br />
the scenes.<br />
Dr. Rogoway is a member of the editorial<br />
board of <strong>The</strong> <strong>Pharos</strong> and emeritus adjunct<br />
clinical professor of Medicine at Stanford<br />
University. His address is:<br />
266 Old Spanish Trail<br />
Portola Valley, California 94028<br />
E-mail: rogoway@stanford.edu<br />
<strong>The</strong> National Institutes of<br />
Health: 1991–2008<br />
John Kastor<br />
New York, Oxford University Press,<br />
2010, 271 pages<br />
Reviewed by Jack Coulehan, MD<br />
(AΩA, University of Pittsburgh, 1969)<br />
W hen I did my internship at the<br />
Hospital of the University of<br />
Pennsylvania, John Kastor was a rising<br />
star in Penn’s Division of Cardiology.<br />
He was also one of my favorite attending<br />
physicians, partly because of excellent<br />
teaching and obvious commitment to<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 49
Reviews and reflections<br />
patients, but also because of his compassion<br />
for students and house officers. At<br />
the end of my rotation with Dr. Kastor,<br />
he invited our whole team to his home<br />
for dinner. And a splendid evening it<br />
was! I remember that dinner as an island<br />
of warmth and conviviality in the<br />
often turbulent sea of internship. Since<br />
then, Kastor has become one of the nation’s<br />
most prominent cardiologists and<br />
a leading figure in American medical<br />
education. He is the author of several<br />
important books on academic medicine,<br />
including Governance of Teaching<br />
Hospitals (2003), Specialty Care in<br />
the Era of Managed Care (2005), and<br />
Selling Teaching Hospitals and Practice<br />
Plans (2008). <strong>The</strong>se works focus, in particular,<br />
on issues of governance in large<br />
health care institutions.<br />
In his new book, <strong>The</strong> National<br />
Institutes of Health: 1991–2009, Kastor<br />
turns his attention to “the premier organization<br />
for performing and funding<br />
biomedical research in the United<br />
States.” pxi <strong>The</strong> book is primarily a description<br />
of the structure, function, mission,<br />
finances, and priorities of the NIH<br />
over nearly two decades, a period that<br />
spans the terms of three NIH directors:<br />
Bernadine Healy, Harold Varmus, and<br />
Elias Zerhouni. While the author presents<br />
plenty of “hard” historical facts,<br />
the real energy of his book arises from<br />
its human perspective: 222 interviews<br />
of present and past NIH administrators<br />
and scientists and other knowledgeable<br />
observers, conducted over a nearly<br />
two-year period. <strong>The</strong> text relies heavily—and<br />
appropriately—on quotations<br />
from these interviews, which provide<br />
the reader with a sense of living history.<br />
<strong>The</strong> NIH consists of twenty research<br />
Institutes and seven Centers, five of<br />
which serve as providers of infrastructure<br />
and support for the institutes. <strong>The</strong><br />
NIH budget in 2008 was around $29<br />
billion, eighty-five percent of which<br />
supported extramural research, i.e.,<br />
grants to universities, hospitals, and<br />
laboratories throughout the United<br />
States. Another ten percent funded the<br />
intramural research program, which<br />
employs over one thousand scientists<br />
at its Bethesda campus, as well as a<br />
large number of trainees. <strong>The</strong> final five<br />
percent of the budget was devoted to<br />
administration. <strong>The</strong> individual research<br />
Institutes range in size from the enormous<br />
National Cancer Institute (NCI,<br />
$4.8 billion budget) and National Heart,<br />
Lung and Blood Institute (NHLBI, $2.9<br />
billion) to the tiny National Institute for<br />
Nursing Research (NINR, $139 million).<br />
It requires over seventy separate administrative<br />
entities—and their acronyms—<br />
to fully characterize the structure and<br />
governance of the NIH. Fortunately, the<br />
reader need not internalize most of this<br />
alphabet soup to gain a basic understanding<br />
of the organization, although<br />
for the interested masochist Kastor provides<br />
an appendix listing every single<br />
acronym and its meaning.<br />
As an academic physician, I found<br />
some of the trends described in <strong>The</strong><br />
National Institutes of Health especially<br />
interesting. First, although I was aware<br />
that the NIH budget had grown in<br />
the 1990s, I had no idea of how much.<br />
During the six-year period 1998 through<br />
2003, its budget more than doubled<br />
from $13.6 to $27.1 billion, an average<br />
increase of about fifteen percent per<br />
year. Even more amazing was the sustained<br />
average annual eight and a half<br />
percent increase over the preceding<br />
twenty-seven years (1971–1997). On the<br />
other hand, during most of the Bush era<br />
(2003 through 2008), the NIH budget,<br />
when corrected for inflation, suffered an<br />
annual decline.<br />
Another interesting point was the<br />
historical trend of the NIH’s intramural<br />
research training program. Kastor<br />
writes of the “yellow berets,” physicians<br />
commissioned in the United States<br />
Public Health Service and assigned to<br />
the NIH in the 1950s, ’60s and ’70s,<br />
who provided the nation with a large<br />
pool of budding physician scientists. In<br />
subsequent decades, as the doctor draft<br />
ended and NIH research training became<br />
less attractive to young physicians,<br />
the size of this pool decreased, resulting<br />
in the NIH having more difficulty<br />
recruiting physician investigators for its<br />
intramural programs. However, the NIH<br />
still provides the major source of financial<br />
support for the training of physician<br />
scientists through its Medical Scientist<br />
Training Program (MSTP), which supports<br />
MD/PhD students in medical<br />
schools throughout the country.<br />
Finally, I learned for the first rime<br />
about the “Roadmap for Medical<br />
Research,” a strategic plan developed<br />
in 2002 and 2003 by then-NIH director<br />
Elias Zerhouni. Zerhouni wrote, “It was<br />
clear to me that science had changed, but<br />
the NIH had not.” p179 A “convergence of<br />
concepts and methodologies” had made<br />
many of the traditional rigid distinctions<br />
between disciplinary Institutes outdated.<br />
Zerhouni initiated a process to answer<br />
such questions as “What are today’s<br />
scientific challenges?” and “What are<br />
the roadblocks to progress?” This led<br />
to a strategic plan, which, among other<br />
things, placed new emphasis on clinical<br />
research. Zerhouni also set aside funds<br />
for Roadmap projects, a practice later<br />
endorsed by Congress when it created<br />
the “Common Fund” as a separate pool<br />
of money to support the initiation of innovative<br />
interdisciplinary projects.<br />
In <strong>The</strong> National Institutes of Health:<br />
1991–2008, John Kastor has written a<br />
clear, concise, and highly informative<br />
book that will serve as a useful entrypoint<br />
for anyone interested in gaining<br />
a basic understanding of the structure<br />
and inner workings of the NIH. As a<br />
bonus, the book also presents a human<br />
perspective on the NIH’s recent history,<br />
with fascinating insights on the process,<br />
as well as examples of the content, of<br />
NIH intramural research.<br />
Dr. Coulehan is a book review editor for<br />
<strong>The</strong> <strong>Pharos</strong> and a member of its editorial<br />
board. His address is:<br />
Center for Medical Humanities, Compassionate<br />
Care, and Bioethics<br />
HSC L3-080<br />
State University of New York at Stony<br />
Brook<br />
Stony Brook, New York 11794-8335<br />
E-mail: jcoulehan@notes.cc.sunysb.edu<br />
50 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong>
Letters to the editor<br />
���������������������������������������������� �����������<br />
Edward D. Harris, M.D.<br />
1937 — 2010<br />
����������� ����������������<br />
Poetry and Ted Harris<br />
I never met Ted Harris. Never spoke<br />
a single word to him. I only knew him<br />
as the editor of a journal I enjoyed<br />
reading. About ten years ago, I sent Dr.<br />
Harris a letter expressing my desire to<br />
serve on <strong>The</strong> <strong>Pharos</strong> editorial board.<br />
I practice and teach internal medicine<br />
in a small community in Central<br />
Virginia. Although I’ve been interested<br />
in the humanities since college, there<br />
was little in my CV to suggest I was<br />
qualified to serve. He did not grant<br />
me a position, but asked me to review<br />
submissions. I accepted. I was eager to<br />
review articles on history, philosophy,<br />
and literature.<br />
Every few months, Ted would send<br />
me a poem. I waited for essays to be<br />
sent; they never came. What did I<br />
know about poetry? Not much. As<br />
soon as a poem arrived, I analyzed the<br />
poem as best I could and immediately<br />
returned it. This went on for years. I<br />
began to study poetry, and read it<br />
every day.<br />
You know how the story<br />
ends. Ted (and Debbie<br />
Lancaster) gave me<br />
a position on the<br />
board in 2004.<br />
It’s been a wonderfully rewarding experience,<br />
and I’m forever grateful.<br />
Ted gave me something else: poetry.<br />
He also showed me how to open<br />
academic doors for others.<br />
Dean Gianakos, MD<br />
Lynchburg Family Medicine Residency<br />
Lynchburg, Virginia<br />
Vicarious respect for Ted Harris<br />
I only met Dr. Harris briefly, and<br />
that was unrelated to medicine. I barely<br />
knew him personally, yet I think I had<br />
an insight many did not. Imagine my<br />
surprise when receiving this summer’s<br />
<strong>Pharos</strong>, and immediately recognizing<br />
him on the cover. Needless to say, I was<br />
a little stunned, as this to me was so<br />
unexpected.<br />
Let me backtrack a little to the early<br />
1960s. I had recently moved with my<br />
parents to a small bedroom community<br />
on the West Shore of Harrisburg,<br />
Pennsylvania. My Latin teacher that<br />
year was a stern taskmaster, the way it<br />
used to be—and perhaps should still<br />
be. No nonsense was tolerated, and total<br />
respect was demand by Mrs. Harris.<br />
Somehow I survived. By my senior<br />
year, I had enough seniority to get a<br />
coveted paper route. By chance, she<br />
became my customer. She lived alone<br />
in a modest home that had a large, flat<br />
front yard. More on that later. I eventually<br />
graduated from Camp Hill High<br />
School, some ten years after her son<br />
had.<br />
Fast forward to my general surgery<br />
residency in 1975 at the Dartmouth<br />
Affiliated Hospitals in Hanover, New<br />
Hampshire, and White River Junction,<br />
Vermont. In those days, residents<br />
were indeed residents. We leaped at<br />
any chance to do something “normal,”<br />
and the annual medical school tennis<br />
tournament was just that excuse. My<br />
doubles partner and I were soundly<br />
defeated in the first round by none<br />
other than Ted Harris, that being my<br />
only personal encounter. Soon after<br />
that, though, he brought his mother to<br />
live in Hanover. She would often visit<br />
and go shopping with my wife, also a<br />
Camp Hill alumna. Mrs. Harris proved<br />
to be hugely independent, intelligent,<br />
and quite friendly, all surprising attributes<br />
considering my opinion as an<br />
adolescent. By the way, she informed<br />
us, her front yard had been a grass tennis<br />
court, where her son had learned<br />
the game well, permitting our paths to<br />
eventually cross.<br />
Can it be just a coincidence how<br />
all our lives are intertwined in some<br />
way? <strong>The</strong> passing of Dr. Harris abruptly<br />
engendered in me a fear of my own<br />
mortality. Yet is only DNA immortal<br />
as it passes from one generation to the<br />
next? I think not. <strong>The</strong> human lives we<br />
as physicians and teachers touch and<br />
influence daily, no matter how briefly,<br />
in some intangible way create another<br />
pathway to gain a sense of immortality,<br />
through their achievements as well. We<br />
both came from a small town, yet Ted<br />
Harris rose from humble beginnings to<br />
achieve grander things, to change the<br />
lives of many. His revitalized <strong>Pharos</strong><br />
became an extension of his personality<br />
that again influenced me later as a “senior”<br />
attending. Hopefully, it will survive<br />
his loss. <strong>The</strong> world will be a lesser<br />
place without him.<br />
Geoffrey G. Hallock, MD<br />
(AΩA, Jefferson Medical College, 1975)<br />
Allentown, Pennsylvania<br />
<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2011</strong> 51
Instructions for <strong>Pharos</strong> authors<br />
We welcome material that addresses scholarly and nontechnical<br />
topics in medicine and public health such as history,<br />
biography, health services research, ethics, education,<br />
and social issues. Poetry is welcome, as well as photograph/<br />
poetry combinations. Photography and art may also be<br />
submitted. Scholarly fiction is accepted. All submissions are<br />
subject to editorial board review. Contributors need not be<br />
members of <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong>. Papers by medical students<br />
and residents are particularly welcome.<br />
Submissions must meet the following criteria:<br />
1. Submissions may not have been published elsewhere<br />
or be under review by another journal.<br />
2. Essays should have a maximum of 15 pages (approximately<br />
5000 words), and be submitted in 12-point<br />
type, double-spaced, with one-inch margins. <strong>The</strong>y should<br />
be accompanied by a covering letter and a title page with<br />
the word count (or page count), return address, and e-mail<br />
address. Papers exceeding the page count noted will be<br />
returned to the author. References should not exceed 20<br />
unique items (see below).<br />
3. Poems or photograph/poetry combinations should be<br />
in 12-point type, with one-inch margins, with the author’s<br />
name, address, and e-mail address on the first page.<br />
4. Electronic submissions are preferred. Send them to<br />
info@alphaomegaalpha.org. Or send by mail to Richard L.<br />
Byyny, MD, Editor of <strong>The</strong> <strong>Pharos</strong>, 525 Middlefield Road,<br />
Suite 130, Menlo Park, California 94025.<br />
5. After peer review, comments on the manuscript will<br />
be sent to the author along with an editorial decision. Every<br />
attempt is made to complete preliminary reviews within six<br />
weeks.<br />
6. <strong>The</strong> editors of <strong>The</strong> <strong>Pharos</strong> will edit all manuscripts<br />
that are accepted for publication for style, usage, relevance,<br />
felicity, and grace of expression, and may provide appropriate<br />
illustrative material. Authors should not purchase illustrative<br />
material because the editors cannot guarantee that it<br />
will be used.<br />
7. In accordance with revised copyright laws, each contributor<br />
will need to sign an Author’s Agreement, which will<br />
be sent with the edited galleys. Information on copyright<br />
ownership and re- publication of articles is detailed in the<br />
Author’s Agreement.<br />
Reference information<br />
Authors are responsible for the accuracy of citations and<br />
quotations in their papers. Once a manuscript has been accepted<br />
for publication, therefore, the author will be required<br />
to provide photocopies of all direct quotations from the<br />
primary source material, indicating page numbers. (Please<br />
mark the quoted material on the photocopies with highlighter.)<br />
In addition, the editors will require photocopies of<br />
all references: the title page and copyright pages of all books<br />
cited, the first and last pages of book chapters cited, and the<br />
first and last pages of journal articles cited, as well as the<br />
Table of Contents of the particular issue of the journal in<br />
which the cited article appeared. <strong>The</strong> foregoing items will be<br />
used to verify the accuracy of the quotations in the text and<br />
the references cited, and to correct any errors or omissions.<br />
<strong>The</strong> photocopies will not be returned.<br />
References should be double-spaced, numbered consecutively<br />
in the text, and cited at the end in the following<br />
standard form:<br />
Journal: Zilm DH, Sellers EM, MacLeod SM, Degani N.<br />
Propranolol effect on tremor in alcoholic withdrawal. Ann<br />
Intern Med 1975; 83: 234–36.<br />
Book: Harris ED Jr. Rheumatoid Arthritis. Philadelphia:<br />
WB Saunders; 1997.<br />
Book chapter: Pelligrini CA . Postoperative<br />
Complications. In: Way LW, editor. Current Surgical<br />
Diagnosis and Treatment, Ninth <strong>Edition</strong>. Norwalk (CT):<br />
Appleton & Lange; 1991: pp 25–41.<br />
Each reference should be listed in the bibliography only<br />
once, with multiple uses of a single reference citing the same<br />
bibliography reference number. Examples are available at<br />
our web site: www.alphaomegaalpha.org.<br />
Citation of web sites as references is discouraged unless a<br />
site is the single source of the information in question or has<br />
official or academic credentials. Examples of such sites are<br />
official government web pages such as that of the National<br />
Institutes of Health. Encyclopedia sites such as britannica.<br />
com are not primary references.<br />
Leaders in American Medicine<br />
In 1967, as a result of a generous gift from Drs. David<br />
E. and Beatrice C. Seegal, <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong> initiated a<br />
program of one-hour videotapes featuring interviews with<br />
distinguished American physicians and medical scientists.<br />
<strong>The</strong> collection has been donated to the National Library<br />
of Medicine, which will maintain it for permanent use by<br />
scholars visiting the library. A listing of tapes available<br />
for loan from AΩA can be found on our web site: www.<br />
alphaomegaalpha.org, or by contacting Debbie Lancaster at<br />
d.lancaster@ alphaomegaalpha.org or (650) 329-0291. Those<br />
wishing to purchase copies may do so by contacting Ms.<br />
Nancy Dosch, manager, Historical Audiovisuals, History<br />
of Medicine, Building 38, Room 1E-21, 8600 Rockville Pike,<br />
Bethesda, Maryland 20891. Telephone (301) 402-8818, e-mail<br />
nancy_dosch@nlm.nih.gov.
2 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> 2008