Stricture Management - Cook Medical
Stricture Management - Cook Medical
Stricture Management - Cook Medical
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
The Channel<br />
A COOK NEWS PUBLICATION ISSUE 2, 2009<br />
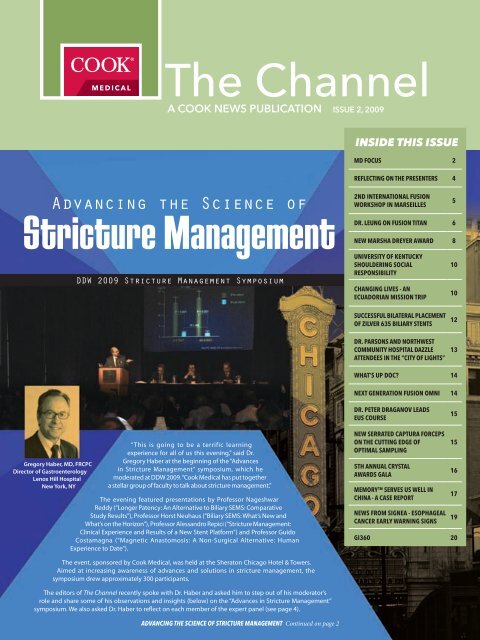
Advancing the Science of<br />
<strong>Stricture</strong> <strong>Management</strong><br />
Gregory Haber, MD, FRCPC<br />
Director of Gastroenterology<br />
Lenox Hill Hospital<br />
New York, NY<br />
DDW 2009 <strong>Stricture</strong> <strong>Management</strong> Symposium<br />
“This is going to be a terrific learning<br />
experience for all of us this evening,” said Dr.<br />
Gregory Haber at the beginning of the “Advances<br />
in <strong>Stricture</strong> <strong>Management</strong>” symposium, which he<br />
moderated at DDW 2009. “<strong>Cook</strong> <strong>Medical</strong> has put together<br />
a stellar group of faculty to talk about stricture management.”<br />
The evening featured presentations by Professor Nageshwar<br />
Reddy (“Longer Patency: An Alternative to Biliary SEMS: Comparative<br />
Study Results”), Professor Horst Neuhaus (“Biliary SEMS: What’s New and<br />
What’s on the Horizon”), Professor Alessandro Repici (“<strong>Stricture</strong> <strong>Management</strong>:<br />
Clinical Experience and Results of a New Stent Platform”) and Professor Guido<br />
Costamagna (“Magnetic Anastomosis: A Non-Surgical Alternative: Human<br />
Experience to Date”).<br />
The event, sponsored by <strong>Cook</strong> <strong>Medical</strong>, was held at the Sheraton Chicago Hotel & Towers.<br />
Aimed at increasing awareness of advances and solutions in stricture management, the<br />
symposium drew approximately 300 participants.<br />
The editors of The Channel recently spoke with Dr. Haber and asked him to step out of his moderator’s<br />
role and share some of his observations and insights (below) on the “Advances in <strong>Stricture</strong> <strong>Management</strong>”<br />
symposium. We also asked Dr. Haber to reflect on each member of the expert panel (see page 4).<br />
ADVANCING THE SCIENCE OF STRICTURE MANAGEMENT Continued on page 2<br />
INSIDE THIS ISSUE<br />
MD FOCUS 2<br />
REFLECTING ON THE PRESENTERS 4<br />
2ND INTERNATIONAL FUSION<br />
WORKSHOP IN MARSEILLES<br />
DR. LEUNG ON FUSION TITAN 6<br />
NEW MARSHA DREYER AWARD 8<br />
UNIVERSITY OF KENTUCKY<br />
SHOULDERING SOCIAL<br />
RESPONSIBILITY<br />
CHANGING LIVES - AN<br />
ECUADORIAN MISSION TRIP<br />
SUCCESSFUL BILATERAL PLACEMENT<br />
OF ZILVER 635 BILIARY STENTS<br />
DR. PARSONS AND NORTHWEST<br />
COMMUNITY HOSPITAL DAZZLE<br />
ATTENDEES IN THE “CITY OF LIGHTS”<br />
5<br />
10<br />
10<br />
12<br />
13<br />
WHAT’S UP DOC? 14<br />
NEXT GENERATION FUSION OMNI 14<br />
DR. PETER DRAGANOV LEADS<br />
EUS COURSE<br />
NEW SERRATED CAPTURA FORCEPS<br />
ON THE CUTTING EDGE OF<br />
OPTIMAL SAMPLING<br />
5TH ANNUAL CRYSTAL<br />
AWARDS GALA<br />
MEMORY SERVES US WELL IN<br />
CHINA - A CASE REPORT<br />
NEWS FROM SIGNEA - ESOPHAGEAL<br />
CANCER EARLY WARNING SIGNS<br />
15<br />
15<br />
16<br />
17<br />
19<br />
GI360 20
Gregory Haber, MD, FRCPC<br />
Director of Gastroenterology<br />
Center for Advanced<br />
Therapeutic Endoscopy<br />
Lenox Hill Hospital<br />
New York, NY<br />
Dr. Gregory Haber graduated with a<br />
degree in Medicine from the University<br />
of Toronto and completed his specialty<br />
training in Internal Medicine in 1975 and<br />
Gastroenterology in 1978. His first position<br />
after training was as a researcher at the<br />
University of Bristol where he studied bile<br />
acid metabolism, having received a <strong>Medical</strong><br />
Research Council of Canada grant for this<br />
endeavor. Two years later he returned to the<br />
University of Toronto, as a faculty member in<br />
the Division of Gastroenterology.<br />
He served on the staff of The Wellesley<br />
Hospital and St. Michael’s Hospital, University<br />
of Toronto, for 25 years, and is currently the<br />
Director, Division of Gastroenterology<br />
and Director of the Center for Advanced<br />
Therapeutic Endosocpy at Lenox Hill<br />
Hospital in New York.<br />
One of the world’s foremost experts on<br />
the treatment of digestive diseases and a<br />
prolific researcher, he has published over<br />
50 peer-reviewed articles, and numerous<br />
abstracts. His research has been funded<br />
by numerous peer-reviewed agencies, and<br />
the pharmaceutical and medical device<br />
industries. Dr. Haber has spoken as invited<br />
faculty at over 200 scientific meetings. He<br />
was an associate editor of Gastrointestinal<br />
Endoscopy, as well as a member of the<br />
board of Endoscopy and Techniques in<br />
Gastrointestinal Endoscopy.<br />
2<br />
www.cookmedical.com<br />
Q: What attracted you to the idea of moderating the<br />
“<strong>Stricture</strong> <strong>Management</strong>” symposium?<br />
Dr. Haber: My personal interest is based on a lifelong clinical career, growing up with selfexpanding<br />
metal stents in transition from plastic stents. It has been interesting to observe<br />
the evolution of stent technology and the engineering that has gone into perfecting them.<br />
The symposium helped put into perspective the use of SEMS in terms of mature, thoughtful<br />
practices. These are all matters of great interest to me.<br />
Q: Take off your<br />
moderator hat and<br />
become an audience<br />
member, and tell us<br />
your impressions.<br />
Dr. Haber: The event was very<br />
well designed and executed.<br />
<strong>Cook</strong> <strong>Medical</strong> brought together<br />
some of the finest teachers<br />
in the world. We could not<br />
have had a more impactful<br />
group of guys presenting at a<br />
symposium. Their presentations<br />
bridged new areas of investigations and how these impact on new avenues of therapeutics.<br />
The speakers are innovators and practitioners, incorporating the newer, novel therapies<br />
into clinical practice. It was fascinating to see the clinical outcomes that were associated<br />
with these new and enhanced stricture management solutions and the clinical scenarios<br />
that were addressed. These were put into perspective with the established therapies and<br />
how they are most appropriately applied to complex problems.<br />
Everyone was very positive and the event garnered high compliments for <strong>Cook</strong> <strong>Medical</strong>.<br />
Q: What would you say were the most<br />
important takeaways from the symposium?<br />
Dr. Haber: This symposium vividly illustrated that we currently have an enormous range of<br />
available technologies to help us solve the clinical problems and challenges we face. While<br />
new developments have made endoscopic therapeutic intervention easier and easier and<br />
more widely applicable and available, more solutions are needed. One of the challenges<br />
discussed was choosing which option is most appropriate at a particular point of time as<br />
the disease manifests in the patient.<br />
I think everyone at the symposium picked up some practical points as to how to use new<br />
and enhanced techniques and methods in their practice.<br />
Q: Regarding plastic vs. metal stenting*: What factors,<br />
aside from clinical outcomes, are making the choice<br />
between plastic and metal stents challenging?<br />
Dr. Haber: I think the major ongoing challenge in the “plastic versus metal” debate is trying<br />
to create validated predictors of survival rates that will help the endoscopist choose the<br />
therapy most appropriate for that length of survival.<br />
Another major determinant in deciding whether one uses plastic or metal stents is clearly<br />
the economic factor. In third-world countries and countries with diminishing resources,<br />
the economic factor plays a much more important role.<br />
*Plastic stents are used to drain obstructed biliary ducts. Metal stents are used in the palliation of malignant<br />
neoplasms in the biliary tree.
Q: Given the current economic pressures in the U.S.,<br />
do you think that physicians will be asked more<br />
and more to justify their choices?<br />
Dr. Haber: Everyone has to become more tuned in and sensitized to the economic<br />
impact of therapeutic choices. That’s why it is very helpful at a symposium like this<br />
for the endoscopist to be able to get a sense of what stricture management<br />
choice is most appropriate and not just place the same stent into every<br />
patient, regardless of cost or need. I think the symposium also showed<br />
that in spite of the advances in SEMS, there is still an important role<br />
for plastic stenting. In certain countries, due to limited resources<br />
and inability to supply metal stents, not only is plastic stenting<br />
appropriate in certain patients but it may be the only choice.<br />
Q: What opportunities to solve<br />
clinical problems do you see with<br />
the 6 French Zilver?<br />
Dr. Haber: The deployment system of the 6 French<br />
Zilver is definitely a quantum leap forward. It changes<br />
the whole playing field for bilateral multiple stenting<br />
with its ability to place two or more metal stents in the<br />
bifurcation or for hilar obstruction. The key is its ability to<br />
place stents simultaneously and to ensure the stents are<br />
side-by-side, especially at the distal ends. That’s definitely<br />
a huge step forward. That will change practices in terms of<br />
hilar stenting. We will see more and more of those procedures<br />
going forward.<br />
Q: What do you feel are the big opportunities to<br />
solve clinical problems with the Fusion Marathon*?<br />
In your opinion, do you think further study<br />
results will be needed to gage the potential<br />
of that device?<br />
Dr. Haber: The results of the nonrandom trial looked very good.<br />
But I think a prospective randomized controlled multicenter trial<br />
in North America will go a long way toward making it a standard<br />
of care as opposed to an attractive option. There’s no question<br />
that such a study would be a big boon in jumpstarting<br />
widespread use. I think that even without a trial, it is likely to<br />
be implemented but at a slower pace as practitioners<br />
garner experience at individual sites.<br />
Q: Do you have any other thoughts on the<br />
symposium you would like to share?<br />
Dr. Haber: I thought the event was one of the best-run evening symposia that I’ve been<br />
involved with. The venue was excellent and the atmosphere was relaxed. It was a great<br />
format for our expert panel to share their expertise with the audience.<br />
*The Fusion Marathon stent is intended for endoscopic placement of a preloaded biliary stent to drain obstructed<br />
biliary ducts and reduce duodenal content reflux.<br />
The Channel<br />
www.cookmedical.com<br />
3
4 www.cookmedical.com<br />
Reflecting on the Presenters<br />
of “Advances in <strong>Stricture</strong> <strong>Management</strong>”<br />
Moderator Dr. Gregory Haber recently shared his<br />
thoughts on each of the expert symposium presenters<br />
Nageshwar D. Reddy, MD<br />
Director of the Asian Institute of Gastroenterology<br />
Professor, Owasis <strong>Medical</strong> College<br />
Hyderabad, India<br />
“Professor Reddy is one of the most experienced pancreatobiliary endoscopists in the world. Because<br />
of the demographics of India, where he works, he treats a very large population of specific types<br />
of disease, especially chronic pancreatic stone disease, as well as unusual biliary tract problems<br />
related to various parasitic worms, etc. In India the impact of economic restraints is a daily reality<br />
necessitating the best use of technology within a fiscal perspective. It’s been very interesting to<br />
see where he is going with that. At the symposium, it was great to hear from somebody who has<br />
so much clinical experience reflect on his past and look into the future.”<br />
Prof. Horst Neuhaus, MD<br />
Evangelisches Krankenhaus<br />
Medizinische Klinik<br />
Dusseldorf, Germany<br />
“Professor Neuhaus, one of the leading German endoscopists, has gained an international reputation<br />
by traveling to virtually every continent every few months, tracking new developments and new<br />
applications. He has his finger on the pulse of endoscopy as it is practiced around the world. He is<br />
able to not only introduce the new technologies but he is also able to put them into an international<br />
perspective. With his ability to create a stimulating and productive learning environment, Professor<br />
Neuhaus has made a major impact internationally as a teacher of endoscopy. Several years ago, he<br />
began a live endoscopy course in Düsseldorf and, from its humble beginnings of perhaps a couple<br />
of hundred attendees, it has developed a wide following, attracting some 1200 to 1500 attendees<br />
annually. It’s now one of the largest courses, outside of national society meetings, in the world.<br />
So, to have an experienced teacher and practitioner such as Horst share his experiences added<br />
enormously to the talent at the table.”<br />
Alessandro Repici, MD<br />
Director, Department of Digestive Endoscopy<br />
Istituto Clinico Humanitas<br />
Milano, Italy<br />
“I know Dr. Repici very well, going back to early in his career when he spent time with us at the<br />
Wellesley Therapeutic Endoscopy Group in Toronto when I was there. He returned to Italy, where he<br />
was obviously a rising star, emerging as one of the most dynamic, enthusiastic, energetic figures in<br />
Italian therapeutic endoscopy. He has clearly established himself one of the leaders in translational<br />
research, introducing new stent technologies into clinical practices. He has tremendous experience<br />
in enteral stenting in the esophagus, duodenum and colon. He engenders enthusiasm each time he<br />
embarks on clinical trials and enjoys taking on the challenges of new stent design and technology.”<br />
Prof. Guido Costamagna, MD, FACG<br />
Director Digestive Endoscopy Unit<br />
Agostino Gemelli University Polyclinic<br />
Professor of Surgery, Catholic University of the Sacred Heart<br />
Rome, Italy<br />
“There are a handful of leading endoscopists in Europe whom we see around the world at all the major<br />
meetings and Guido is one of them. He came from the Brussels school, trained with Michel Cremer<br />
and went back to Rome and became the preeminent therapeutic endoscopist there. He is known as<br />
a tenacious investigator, directing innovative clinical trials and evaluating new technologies. He is<br />
constantly pushing the envelope in an effort to expand endoscopic therapeutic avenues. Although<br />
he is recognized as a giant in therapeutic endoscopy, he is humble and approachable, a great and<br />
empathetic teacher who understands the challenges that even first-year endoscopists face.”
French Society of Digestive Endoscopy<br />
President Hosts<br />
International<br />
Fusion Workshop<br />
in Marseilles<br />
Gastroenterologists from Slovakia and Croatia journeyed to the southeastern French La Timone<br />
Hospital in Marseilles to learn new endoscopic techniques and hone their skills.<br />
Led by Professor René Laugier – director of gastroenterology, digestive endoscopy and therapeutic<br />
endoscopy at the hospital – the visiting physicians benefited from two days of presentations<br />
and hands-on procedures involving short wire exchange, stenting and endotherapy of chronic<br />
pancreatitis, pancreatic cancer and biliary diseases.<br />
Professor Laugier, a specialist in biliopancreatic diseases and therapeutic endoscopy, currently serves<br />
as President of the French Society of Digestive Endoscopy. At the 1000-bed La Timone Hospital, he<br />
is head of the department of gastroenterology (including endoscopy department) and sees more<br />
than 40 patients per week for consultation and averages two days of diagnostic and therapeutic<br />
endoscopy per week.<br />
Prior to the workshop, Professor Laugier set some ambitious goals, including: demonstrating the<br />
most recent endoscopic procedures, presenting and discussing the latest endoscopic equipment,<br />
examining the advantages and disadvantages of short wire guides and suggesting ways<br />
to reduce bacterial risk in ERCP, as well as reducing the risk of pancreatitis.<br />
A Wide Range of Endoscopic Topics<br />
Professor Laugier offered participants a wide variety of endoscopic topics. “On Thursday<br />
we covered every kind of digestive endoscopy procedure,” he said. “We also presented<br />
a range of <strong>Cook</strong> endoscopic products, with emphasis on material based on Fusion. This<br />
was followed by more than three hours of videos illustrating all therapeutic endoscopy<br />
techniques as well as hands-on training for developing good technique.”<br />
Topics that Professor Laugier covered included: chronic pancreatitis (pancreatic duct<br />
and main bile duct stenosis, stone destruction and extraction), biliary stenting in<br />
pancreatic cancer, double stenting for hilum strictures, digestive cystostomies and<br />
digestive metal stenting.<br />
On Friday the group was in the operating room from 8 a.m. to 4 p.m. for live cases. “All participants<br />
worked in the endoscopic room, along with nurses, who did great work using Fusion products. We<br />
presented each case, discussed the indications, explained the endotherapy, and commented on<br />
every aspect. This segment involved examining and treating patients with varying pancreatobiliary<br />
or digestive tract illnesses.”<br />
The feedback Professor Laugier received was overwhelmingly positive. “The physicians were highly<br />
pleased and proud to be chosen to attend,” said Professor Laugier. “They heard many technical aspects<br />
and were keen for this kind of education. They learned important details on many aspects, particularly<br />
on how we perform examinations. There were many compliments for the opportunity to participate.”<br />
For the next international workshop, Professor Laugier plans to duplicate the two-day format. “All<br />
feedback indicates this was an appropriate format and length,” he concluded.<br />
The Channel<br />
www.cookmedical.com<br />
5
Joseph Leung, MD, FRCP,<br />
FACP, FACG, FASGE<br />
Mr. and Mrs. C.W. Law Professor of<br />
Medicine, University of California,<br />
Davis School of Medicine, Chief<br />
of Gastroenterology, VA Northern<br />
California Health Care System<br />
Brian Lim, MD, MCR<br />
Gastroenterology<br />
Kaiser Permanente Riverside<br />
<strong>Medical</strong> Center<br />
(Former gastroenterology<br />
fellow at UC Davis<br />
<strong>Medical</strong> Center)<br />
6 www.cookmedical.com<br />
pening<br />
p<br />
Balloon dilation of a bile duct stricture facilitates access into the biliary system or beyond the<br />
obstruction for removal of bile duct stones or placement of a biliary stent to provide drainage.<br />
Because of the larger balloon diameter, they are more effective compared to the more rigid<br />
(but much smaller) graded dilation catheters.<br />
Technique of balloon dilation<br />
An overview of<br />
balloon dilation in<br />
the management<br />
of biliary disease<br />
Dilation balloons or biliary balloon dilatation catheters (as some refer to) come<br />
in different sizes and in general, range from 4 to 10 mm in diameter and 2<br />
to 4 cm in length, e.g. Hurricane (Boston Scientific, Natick, MA) or Fusion<br />
Titan Biliary Dilation Balloon (<strong>Cook</strong> Endoscopy, Winston Salem, NC). They<br />
are mostly made of nylon or polyethylene terephthalate (PET) and are<br />
minimally-compliant balloons. It is recommended to use a regular .035”<br />
wire guide to provide rigidity for effective dilation. The balloon is inserted<br />
over a pre-positioned wire guide placed within the bile duct or across<br />
the bile duct stricture. The two ends of the balloon are indicated by<br />
radiopaque ring markers to help positioning of the balloon across<br />
the stricture (usually with the stricture located at the midpoint of the<br />
balloon for effective dilation). Inflation of the balloon is performed<br />
using a pressure insufflator by injecting diluted contrast to fill the<br />
balloon. The appearance of initial waist formation on the balloon<br />
denotes the level of the obstruction. The balloon is inflated slowly to the<br />
recommended pressure (per manufacturer) and the obliteration of the<br />
waist indicates effective dilation of the stricture/papilla. Depending on<br />
individual physicians, the balloon is kept inflated for between 15 seconds<br />
to a minute to allow proper stretching of the stricture.<br />
Recent improvement to balloon design<br />
The earlier balloons (e.g., Quantum Balloon Dilators) were designed with only<br />
one proximal side-hole (or inflation port) that connects to the balloon, which<br />
allows inflation and deflation of the balloon. However, the limitation to the flow of<br />
contrast (especially for normal or dense contrast) with a single side-hole meant that<br />
the balloon is inflated from the proximal end which often predisposes the balloon to<br />
migration (especially in case with a tight biliary stricture). Proper positioning of the balloon<br />
is maintained sometimes by pulling or pushing on the balloon catheter, especially during early<br />
balloon inflation, to resist its migration. Furthermore, the single side-hole limits return (free flow) of<br />
contrast, making deflation of the balloon more difficult. This happens more often when the partially
Figure 1<br />
Balloon dilation after endoscopic<br />
sphincterotomy to facilitate removal<br />
of CBD stones through a distal bile<br />
duct sricture.<br />
deflated balloon is pulled back into the scope channel, further restricting the return<br />
flow of contrast. A partially deflated balloon makes it more difficult to be withdrawn<br />
into the scope channel and increases the difficulty with wire guide exchange.<br />
Although the use of more diluted contrast is helpful, there are still limitations in rapid<br />
inflation and deflation of the balloon related to a single side-hole.<br />
The new Fusion Titan Biliary Dilation Balloons (<strong>Cook</strong> Endoscopy, Winston Salem, NC)<br />
have an improved design, which incorporates two sets of side-holes at either end of the<br />
balloon. This design allows efficient insufflation and deflation of the balloon and minimizes<br />
the risk of balloon migration because both sides of the balloon can be inflated, holding it in<br />
position like a “dog-bone appearance,” especially in the case of a tight stricture. Furthermore, the<br />
balloon can be efficiently and completely deflated, making withdrawal of the balloon and subsequent<br />
wire guide exchange more easily without losing the wire position.<br />
Application in bile duct stricture<br />
management and stone extraction<br />
Endoscopic sphincterotomy (ES) is an established treatment for the removal of common bile duct<br />
stones. Removal of stones proximal to a relative distal bile duct narrowing can be challenging. In<br />
order to facilitate stone removal, the bile duct obstruction is dilated before balloon sweep. Although<br />
transient post-dilation bleeding has been reported, surprisingly the incidence of post-dilation<br />
pancreatitis from prolonged balloon dilation has not increased significantly. This however, may be<br />
related to the use of prophylactic pancreatic stenting in some cases to prevent post-ERCP pancreatitis.<br />
Patients with intrahepatic stones pose a challenge to endoscopic removal, and effective dilation<br />
of the associated stricture is necessary to facilitate stone removal. Indeed, the persistence of waist<br />
formation on the balloon despite full insufflation would signify difficulties in removing the stone(s)<br />
without resorting to lithotripsy. The Fusion Titan Balloon, which resists migration during insufflation,<br />
is more effective in dilating the intrahepatic stricture.<br />
Application in bile duct strictures<br />
In the management of patients with malignant biliary obstruction or benign post-operative bile duct<br />
strictures such as post liver transplantation, balloon dilation facilitates the placement of biliary stents<br />
for drainage. In the case of post-surgical changes, we recommend initial stenting for drainage only<br />
without any balloon dilation until the injury or stricture is set. We usually wait three months before<br />
contemplating balloon dilation of the stricture. Insertion of multiple biliary stents is technically<br />
difficult although, when successful, provides more effective drainage as well as splinting for the<br />
stricture. In choosing the right size balloon, it is important to assess the diameter of the normal<br />
part of the bile duct (usually the distal CBD below the level of the obstruction). Excess balloon size<br />
poses a risk of perforation from overzealous balloon dilation. The placement of multiple stents can<br />
be facilitated using the Fusion OASIS system (<strong>Cook</strong> Endoscopy, Winston Salem, NC), which allows<br />
intraductal exchange of the wire guide above the obstruction thus maintaining access across the bile<br />
duct stricture after initial stent deployment. This allows subsequent double or triple stent placement<br />
without having to recannulate or renegotiate the stricture.<br />
The Channel<br />
a<br />
b<br />
c<br />
d<br />
Figure 2a - b<br />
Multiple biliary<br />
stenting using<br />
the Fusion OASIS<br />
after balloon<br />
dilation of CHD<br />
stricture.<br />
Figure 3<br />
a. Balloon with simulated stricture (O-ring).<br />
Note radiopaque ring markers (large arrows)<br />
on either end of the balloon and side-holes<br />
(small arrows).<br />
b. Partial filling of the balloon. Note that the<br />
proximal half of the balloon is filling first<br />
but the distal portion also fills, keeping the<br />
balloon (waist formation) in a stable position<br />
in relation to the stricture.<br />
c. Complete obliteration of the waist.<br />
d. Rapid collapse of the balloon on either side<br />
of the stricture upon deflation.<br />
www.cookmedical.com<br />
7
Fig A<br />
Fig B<br />
A 75-year-old patient<br />
presents with 10 days<br />
of painless jaundice and<br />
itching. On abdominal<br />
examination the patient has<br />
a fluctuant mass palpable<br />
below the right costal<br />
margin in the midclavicular<br />
line. The resident who<br />
examines him describes<br />
Dr John Baillie<br />
the “mass” as feeling like<br />
a “rubber ball” that he can “bounce” under<br />
his fingers, but he can’t get above it. He<br />
suggests a diagnosis, which is supported by<br />
an abdominal CT scan (Figs A and B).<br />
What structure is the resident<br />
feeling on abdominal palpation?<br />
What abnormalities are<br />
present on the CT scan?<br />
What diagnosis did the resident<br />
suggest to explain (unify) all the<br />
findings? Whose “sign” is present?<br />
What endoscopic intervention<br />
will help this patient?<br />
To confirm your diagnosis, click on<br />
newsletter button on endoscopy homepage<br />
of www.cookmedical.com <br />
We are looking for more submissions and<br />
welcome your participation. If you want to<br />
submit an image with a written case history<br />
and clinical explanation, please contact Kevin<br />
Chmura at kevin.chmura@cookmedical.com.<br />
8 www.cookmedical.com<br />
<strong>Cook</strong> <strong>Medical</strong> and ASGE Announce New<br />
AWARD<br />
At the 2009 Crystal Awards Dinner in Chicago, <strong>Cook</strong> <strong>Medical</strong> Endoscopy division<br />
President Bill Gibbons and the ASGE announced the newly established Marsha<br />
Dreyer Award. The award will pay travel expenses for up to three international trainee<br />
members’ (up to $4,500) to attend Digestive Disease Week® beginning in 2010.<br />
Introducing the award, Gibbons said,<br />
“For more than three decades, Marsha worked alongside some<br />
of the leading gastroenterologists in the world. And, fortunately for us,<br />
Marsha was driven to share that knowledge with all who were willing to<br />
learn from her through her passionate commitment to continuing education<br />
opportunities for GI professionals around the globe. So, in a fitting tribute to<br />
Marsha, today we are proud to announce that her commitment and<br />
her passion will live on with the Marsha Dreyer Award.”<br />
ASGE’s International Committee will review the applications and make<br />
recommendations to the ASGE Governing Board, which will make the final selections.<br />
Priority will be given to applicants who would otherwise not be able to attend DDW.<br />
To be eligible for the Marsha Dreyer Award, applicants must:<br />
1. Be a current ASGE international trainee member<br />
within five years of completing training.<br />
2. Be first or submitting author of a DDW 2010<br />
abstract. Case reports are not eligible.<br />
In order for abstracts to be considered for the award, the <strong>Cook</strong> <strong>Medical</strong> Marsha Dreyer<br />
Award checkbox must be marked on the DDW abstract submission application.<br />
There will be three awards selected from approved DDW 2010 abstracts. The<br />
abstracts must be submitted by Tuesday, December 1, 2009 to DDW (visit www.ddw.<br />
org regarding abstract submissions). Late submissions will not be considered. For<br />
additional information please contact Holly Becker, Manager of International Member<br />
Relations, American Society for Gastrointestinal Endoscopy, 1520 Kensington Road,<br />
Suite 202, Oak Brook, IL 60523; phone: 630-570-5631; fax 630-573-0691; or email<br />
hbecker@asge.org.
Expand your procedural possibilities.<br />
When facing challenging biliary stenting procedures, sometimes you have to<br />
think small. With the market’s smallest introducer and coil-reinforced<br />
construction, the new Zilver 635 opens up your procedural possibilities. For<br />
instance, the Zilver 635 is the only introducer in the world that allows you to<br />
simultaneously place and align two metal stents at the bifurcation. By combining<br />
the latest in access capability and the proven benefits of Zilver, the 635 is sure<br />
to advance the field of biliary stenting.<br />
Contact your <strong>Cook</strong> <strong>Medical</strong> representative or visit www.cookmedical.com for<br />
more information about the Zilver 635 Biliary Self-Expanding Stent.<br />
<strong>Cook</strong> <strong>Medical</strong> – Delivering the clinical advantage.<br />
AORTIC<br />
INTERVENTION<br />
CARDIOLOGY<br />
CRITICAL<br />
CARE<br />
ENDOSCOPY<br />
INTERVENTIONAL<br />
RADIOLOGY<br />
PERIPHERAL<br />
INTERVENTION<br />
Warning: The safety and effectiveness of<br />
this device for use in the vascular system<br />
has not been established.<br />
SURGERY UROLOGY<br />
WOMEN’S<br />
HEALTH<br />
© COOK 2009<br />
Image Courtesy of Dr. Terruzzi Vittorio & Dr. Radaelli Franco, Ospedale Valduce Como, Italy
University of<br />
Kentucky<br />
Shouldering<br />
Social<br />
Responsibility<br />
For more than a decade, medical teams from Kentucky have served<br />
health needs in Ecuador. Shoulder to Shoulder Ecuador (STSE) was<br />
established by Dr. Tom Young, professor of pediatrics, UK College<br />
of Medicine, along with Lexington, KY community partners. STSE is<br />
based in Kentucky and works in partnership with Hombro a Hombro<br />
Ecuador in Santo Domingo to improve the health and lives of children<br />
and their families.<br />
Over the years, the university has established strong relationships in<br />
Quito and Santo Domingo. Through a series of community meetings<br />
in Santo Domingo, community leaders identified Carlos Ruiz Burneo<br />
(population 20,000) as an area of extreme poverty in dire need of<br />
access to medical care.<br />
April 2007 marked the opening of Centro Medico Hombro a Hombro<br />
in Carlos Ruiz Burneo. Physicians, nurses, a dentist and support staff<br />
operate the primary care center there. Since the opening, the center<br />
has treated more than 3,000 new patients. Services include:<br />
Primary medical care Public health programs<br />
School health Feeding programs for<br />
programs infants and mothers<br />
Gastroenterology services Dental services<br />
Cancer screenings<br />
Tom Young, MD,<br />
Professor of Pediatrics,<br />
UK College of Medicine<br />
Also at the University of Kentucky, <strong>Medical</strong> Mission Ecuador – led by<br />
Dr. Henry Vasconez, professor of surgery and chief of plastic surgery,<br />
UK College of Medicine – has provided medical and surgical services<br />
to Ambato, Ecuador for many years. For example, during the past five<br />
years, UK’s Department of Pediatrics led pediatric teams to Ecuador<br />
with faculty, residents and students. UK has a formal relationship<br />
with the PUCE <strong>Medical</strong> School in Quito for the exchange of faculty<br />
and students.<br />
Partners and supporters of STSE and MME include the University<br />
of Kentucky (UK), Cathedral of Christ the King, UK International<br />
Federation of <strong>Medical</strong> Students Association (IFMSA), UK STSE Student<br />
Association, Josephson Foundation, Kiwanis Club of Lexington,<br />
UK Newman Center, Kroger, LexAir, Inc., Jubileo Foundation, and<br />
community volunteers. In Ecuador, the Kiwanis Club of Santo<br />
Domingo and FASCA (a Catholic social service agency) are partners.<br />
10 www.cookmedical.com<br />
and<br />
perspectives<br />
An Ecuadorian mission trip<br />
Nicholas J. Nickl, MD,<br />
Professor of Medicine,<br />
University of Kentucky HealthCare<br />
“Should you have an opportunity to serve<br />
humanity this way,” says gastroenterologist<br />
Nicholas J. Nickl, “take it! The experience will<br />
change the lives of the people you treat. And<br />
it will change your life.”<br />
The experience that Dr. Nickl – Professor<br />
of Medicine at the University of Kentucky<br />
HealthCare – is referring to is the medical<br />
mission he took to an impoverished area of<br />
Ecuador in August 2008.<br />
Dr. Nickl – along with endoscopist Luis<br />
R, Pena, MD, and endoscopic nurse Betsy<br />
Matthews, RN, both also from the university’s<br />
GI division – joined a team of other healthcare<br />
professionals and traveled to Santo Domingo,<br />
a city three hours west of Ecuador’s capital<br />
Quito. Healthcare services provided by the<br />
group included family practice, pediatrics,<br />
dental, nursing and gastroenterology.<br />
The group worked at an indigent barrio<br />
clinic founded and run jointly by Shoulder<br />
to Shoulder Ecuador, the University of<br />
Kentucky and the Roman Catholic<br />
diocese of Santo Domingo. (See sidebar:<br />
“University of Kentucky: Shouldering Social<br />
Responsibility”). Dr. Nickl also lent a hand<br />
at Gustavo Dominguez Hospital, where he<br />
treated the digestive health needs of 21<br />
patients. “During this mission, I saw patients<br />
with gastritis, several cases of H pylori<br />
infection and some serious reflux diseases.<br />
All patients had some significant digestive<br />
healthcare needs.”<br />
Providing “the best<br />
healthcare available”<br />
Dr. Nickl is especially proud that the team<br />
was able to care so well for people who had<br />
so little. “It felt good to provide the best<br />
healthcare available. We made no quality<br />
compromises and used the same state-ofthe-art<br />
equipment and procedures we have<br />
in the U.S. In fact, it was as good as any place<br />
in the world.”
The people that he met and treated have<br />
left a lasting impression on Dr. Nickl. “They<br />
were so sweet, friendly and grateful for the<br />
healthcare. I recall one patient who was so<br />
excited to see a North American GI professor<br />
that he walked to the clinic in his Sunday<br />
best clothing. Suddenly, these heretofore<br />
faceless people became familiar faces. They<br />
are wonderful people who love their children.<br />
They were no longer just stereotyped images<br />
we had of South Americans. The people we<br />
met were open to North Americans. They do<br />
not think of us as heartless.”<br />
International politics were not a concern<br />
for the mission team. “Ecuador is a stable<br />
democracy,” says Dr. Nickl. “They use the U.S.<br />
dollar as their currency.”<br />
More trips to Ecuador to come<br />
This was the second trip to Ecuador for Dr.<br />
Nickl. In July 2007, he was part of a churchsponsored<br />
Habitat for Humanity group.<br />
At that time, the Centro Medico Hombro<br />
a Hombro in Carlos Ruiz Burneo was just<br />
getting started and Nickl and his medical<br />
colleagues treated many of its first patients.<br />
“That 2007 trip and last year’s trip have given<br />
me new perspectives on all the privileges we<br />
have in our country,” says Dr. Nickl. “We cannot<br />
ignore these people and their needs.” Dr. Nickl<br />
plans to return to Ecuador this summer (2009)<br />
and he is planning an eight-month sabbatical<br />
there in 2010.<br />
“It is all about helping people.”<br />
The August 2008 mission to Ecuador was<br />
sponsored primarily by the University of<br />
Kentucky <strong>Medical</strong> Center as well as other<br />
charities, including the Roman Catholic<br />
Cathedral of Christ the King church in<br />
Lexington. Each member of the team paid<br />
his or her own way and used vacation time<br />
to make the trip. Shoulder to Shoulder<br />
Ecuador is an independent group consisting<br />
of members of the University of Kentucky<br />
medical community, which provides<br />
administrative and fundraising assistance to<br />
support the Hombro a Hombro Clinic.<br />
Healthcare<br />
Ecuador<br />
in<br />
Total population: 13,200,000<br />
The Channel<br />
Life expectancy at birth (years): Men 70, Women 76<br />
Probability of dying before age five: (per 1,000 live births) 24<br />
Total expenditure on health per capita: $297<br />
Total expenditure on health as a % of gross<br />
domestic product: 5.4%<br />
Top ten causes of death, all ages:<br />
Ischemic heart disease Cerebrovascular disease<br />
Diabetes mellitus Lower respiratory infections<br />
Hypertensive heart disease Tuberculosis<br />
Parinatal conditions Violence<br />
Stomach cancer Nephritis and nephrosis<br />
Source: World Health Organization, 2006<br />
www.cookmedical.com<br />
11
12 www.cookmedical.com<br />
case report<br />
Successful<br />
of<br />
Zilver 635 Biliary<br />
Self-Expanding Stents<br />
Terruzzi Vittorio, M.D. and<br />
Radaelli Franco, M.D.<br />
Ospedale Valduce di Como, Italy<br />
A 70-year-old patient with a six month history of cholangiocarcinoma with hilar<br />
involvement (Klatskin tumor class IIIb, according to Bismuth classification) was<br />
admitted to our department for acute cholangitis. The patient had previously<br />
been treated with chemotherapy and radiotherapy for breast cancer in<br />
2005; past medical history was otherwise unremarkable.<br />
Six months before, the patient came to our attention for jaundice and<br />
fever. A diagnosis of Klatskin tumor was made by imaging (helical CT<br />
and NMR). ERCP was subsequently performed for brushing (which<br />
confirmed the diagnosis of cholangiocarcinoma) and biliary stenting.<br />
After biliary sphincterotomy, 8.5 FR, 12 cm plastic stent (Cotton-<br />
Huibregtse, <strong>Cook</strong>) and 10 FR, 9 cm plastic stent were positioned<br />
(OASIS-<strong>Cook</strong>) in the left and right branch, respectively, and good<br />
drainage of the biliary tree was achieved. An explorative laparoscopy<br />
was subsequently made to evaluate the possibility of resectability, but<br />
the patient was considered unfit for surgery due to a nodal involvement.<br />
The patient was jaundiced and febrile when admitted the second time. A<br />
blood culture resulted positive for E. Coli and abdominal ultrasound showed<br />
a diffuse dilation of the intrahepatic biliary tree. An ERCP was urgently planned<br />
for changing the previously placed biliary stents and positioning two metal stents<br />
(ZILBS-635-10-8) in the right and left branches. For this purpose, a large channel (4.2<br />
mm) duodenoscope was used.<br />
After removing both the plastic stents, a Tracer Metro® wire guide (METII-35-480) and a Fusion®<br />
LoopTip wire guide (FS-LT-35-480) were placed through a Glo-Tip II® ERCP catheter (GT-2-T-RB) in<br />
the right and left branches, respectively. Over the wire guides, the metal stents were positioned<br />
across the hilar stenosis. The stent catheters were lubricated with silicon spray, and insertion of the<br />
two stents through the scope was very easy. No problem occurred during cannulation of the papilla.<br />
Once the correct position of both stents across the stenosis was confirmed by fluoroscopy, we started<br />
to partially deploy the left stent for about 15-20 mm, and immediately after we did the same with<br />
the right one. Both systems were then fully deployed simultaneously and both delivery systems were<br />
removed at the same time. The distal end of the right stent was seen out from the papilla. Immediately<br />
after stent deployment, dark bile and pus flowed out the papilla and a complete drainage of contrast<br />
medium from the biliary tree was achieved.<br />
The patient was discharged two days after the procedure. At the 30-day follow-up visit, the patient was doing well,<br />
and total bilirubin was 2.3 g/dL.
The Channel<br />
Dr. Parsons and Northwest Community Hospital dazzle attendees in the<br />
Interventional Interventional Endoscopy Endoscopy Course Course For For GI GI Nurses Nurses and and Technicians Technicians<br />
Dr. Willis G. Parsons and Northwest Community Hospital (Arlington Heights, IL) held their annual<br />
Interventional Endoscopy Course at the Flamingo in Las Vegas, Nevada. The recent event, traditionally<br />
well attended, grew even larger this year: Approximately 200 participants representing 22 states<br />
were treated to several days of interesting lectures, working dry labs and the wonders of the Las<br />
Vegas strip at night.<br />
The annual event featured presentations by Dr. Parsons, Center for Advanced Therapeutic Endoscopy,<br />
Director of Gastroenterology Center at Northwest Community Hospital; Dr. Todd Baron, Professor<br />
of Medicine, Division of Gastroenterology & Hepatology at the Mayo Clinic College of Medicine,<br />
Rochester. Also, presenting were Kathy Lamont, RN, BS, MBA, Director of the Gastroenterology<br />
Center at Northwest Community Hospital and Colleen Himan, RN, MSN, APN, Center for Advanced<br />
Therapeutic Endoscopy. Dry-lab participants received very specialized instruction by faculty from<br />
Northwest Community GI Center and representatives from <strong>Cook</strong> <strong>Medical</strong>, Olympus America, Barrx<br />
<strong>Medical</strong> and Bracco Diagnostics.<br />
On the first day, following early registration, there was a “welcome” reception in which everyone had<br />
time to mingle and become acquainted. This was especially great since participants came from all<br />
over the country and enjoyed sharing stories and making new friendships.<br />
The opening lecture featured Colleen Himan, RN, MSN, APN, addressing “Anatomy and Physiology<br />
of the Biliary/Pancreatic Systems.” She included clinical scenarios along with slides that showed<br />
various anatomical models and terminology that assisted everyone from the experienced nurse and<br />
technician to those just beginning to perform ERCPs. Dr. Parsons consistently engaged the crowd<br />
with his lecture on “ERCP: Biliary Tract Disease” by showing biliary access; biliary sphincterotomy;<br />
stone and stricture management; and how to avoid, recognize and manage complications. During<br />
his lecture the exuberant crowd received various prizes for correctly answering questions regarding<br />
materials covered during the presentation. Afterwards, Dr. Baron’s presentation on “ERCP: Pancreatic<br />
Disease” described various types of pancreatic interventions, while defining fluid collections and<br />
just how and when to intervene. We looked at pancreatitis, pseudocysts and ductal abnormalities<br />
followed by audience questions.<br />
The morning session concluded with interactive dry labs in which participants were able to view and<br />
work with various types of products in a skills-building environment. The group broke out into four<br />
stations that rotated through wire guides (exchanges, biliary access), sphincterotomy, mechanical<br />
lithotripsy (stone management) and stenting. These stations gave key insight into the techniques,<br />
preparation and the do’s and don’ts of ERCP product assistance.<br />
The afternoon session began with Dr. Baron discussing “Enteral Stenting.” He defined indications for<br />
enteral self-expanding stents and described products currently available on the market. He then<br />
demonstrated cases of esophageal, duodenal and colonic SEMS, which lead to group discussion<br />
and questions. Dr. Parsons followed with “Ablation Therapy of Barrett’s Esophagus.” This presentation<br />
discussed disease progression, treatment goals and most common treatment options and concluded<br />
with ablation techniques. Once again the audience was treated to the much-anticipated question<br />
and answer period where participants gained rewards for correct responses. Day One concluded<br />
with Kathy Lamont’s presentation, “Building an Interventional GI Team.” Everyone learned what an<br />
interventional team actually is plus the benefits and the potential downfalls of a select team and<br />
how to avoid them. The training, skill sets, stats and potential Med-Surgical cost per case were also<br />
discussed followed by questions.<br />
Sunday began with a nice breakfast gathering leading into exciting lectures covering EUS/EMR, a<br />
GI bleeding update and a challenging and fun ERCP Flouro Quiz, all given by a very humorous Dr.<br />
Parsons. There was additional time spent in the dry lab with vendors and nurses, covering various<br />
products and procedural techniques. This was the conclusion of a well spent weekend and everyone<br />
left the “City that never sleeps” with a great deal of knowledge and anticipation of returning next<br />
year for this annual program, which will be held at Caesar's Palace in Las Vegas, February 26-28, 2010.<br />
Willis G. Parsons, MD<br />
Director of Gastroenterology<br />
Center for Advanced<br />
Therapeutic Endoscopy<br />
Northwest Community<br />
Hospital<br />
Arlington Heights, IL<br />
Back row (L to R) - Isidro Buenrrostro, GI<br />
Tech; Colleen Shanahan, RN; Kim Scalzitti,<br />
RN; Geraldine De La O, Tech; Alla Pol, Tech;<br />
Laura Mich, RN and Jennifer McLenna, RN.<br />
Front row (L to R) - Diane VanOverbake, RN;<br />
Danilo Samson, GI Tech and Allison<br />
Thielmann, RN<br />
www.cookmedical.com<br />
13
N E X T G E N E R A T I O N<br />
14 www.cookmedical.com<br />
featuring a<br />
design on FS-OMNI and FS-OMNI-35<br />
<strong>Cook</strong> Endoscopy’s Fusion ERCP product line is advancing ERCP through ongoing product<br />
development with the goal of helping to achieve successful patient outcomes. The next<br />
generation Fusion OMNI features the latest in evolutionary clear catheter technology,<br />
while maintaining the important benefits of our initial sphincterotome design.<br />
From a clinician’s perspective, you now have optimal wire guide visibility throughout<br />
the entire length of the device. As an added benefit, there is a significant reduction in<br />
the amount of force required to initially break through our solid channel design, as<br />
well as having the ability to perform a more efficient exchange by pulling the device<br />
at any angle.<br />
Other notable key features of the Fusion OMNI include the new<br />
look of access with the smooth, round shape of our exclusive<br />
DomeTip design. The Fusion OMNI is the only device on the<br />
market that maintains the choice of your clinical preference as<br />
to whether you choose physician wire guide control or use the<br />
Fusion OMNI in a traditional long wire manner by utilizing our<br />
fully-functional traditional wire guide lumen. Also, if you prefer<br />
to use smaller wire guide diameters, the Fusion OMNI has the<br />
capability of using any wire guide diameter ranging from 035”<br />
to .018” – including the one-of-a-kind Fusion LoopTip – without<br />
having to switch to another device.<br />
The Fusion OMNI streamlines the ERCP process, meeting all of<br />
your clinical needs with one device.<br />
<strong>Cook</strong>’s Endoscopy Fusion ERCP product line – advancing ERCP<br />
and delivering solutions for successful patient outcomes.
Dr. Peter V. Draganov<br />
Course leader<br />
Dr. Peter V. Draganov<br />
Associate Professor<br />
University of Florida<br />
College of Medicine<br />
Gainesville, FL<br />
Course participants<br />
Dr. M. Rodwan Hiba, MD<br />
Spring Hill Regional Hospital<br />
Brooksville Regional Hospital<br />
Brooksville, FL<br />
Dr. Yasser Saloum, MD<br />
Tampa General Hospital<br />
University of South Florida Surgery<br />
and Endoscopy Center<br />
Tampa, FL<br />
Dr. Ahmed Shobassy, MD<br />
Halifax <strong>Medical</strong> Center<br />
Advanced Gastroenterology<br />
Center<br />
Port Orange, FL<br />
Course learning objectives<br />
Upon conclusion of this program,<br />
participants should be able to:<br />
• Identify the unique features of<br />
dedicated echoendoscopes and<br />
catheter probes.<br />
• Identify normal EUS anatomy.<br />
• Establish the T, N and M stage<br />
for luminal tumors and<br />
pancreatic cancer.<br />
• Differentiate the various types of<br />
cystic pancreatic tumors.<br />
• Identify the utility of EUS for<br />
evaluating patients with chronic<br />
pancreatitis.<br />
• Differentiate the various<br />
subepithelial mass lesions.<br />
Leads<br />
EUS Course<br />
at the University of Florida<br />
A recent EUS course at the University of Florida<br />
allowed participating gastroenterologists to<br />
gain knowledge and hands-on experience in<br />
a comprehensive multidisciplinary review of<br />
endoscopic ultrasound. The course leader, nationally<br />
renowned expert Dr. Peter Draganov, discussed the<br />
impact and role of EUS in the participants’ practices.<br />
The EUS devices used to instruct the participants<br />
included <strong>Cook</strong>’s EchoTip® Ultra and Quick-Core®<br />
ultrasound needles as well as the EchoBrush<br />
sampling brush.<br />
Draganov supervised live case demonstrations,<br />
using the opportunity to encourage lively exchanges<br />
between he and the course participants. He<br />
emphasized technical aspects of performing EUS<br />
and demonstrated the use of standard equipment<br />
as well new devices. During each of the cases, he<br />
instructed the clinicians on navigating difficult<br />
anatomy and identifying important anatomical<br />
landmarks. Each case was discussed and clinical<br />
recommendations made before, during and after<br />
the procedures.<br />
The “in-the-room” instruction enhanced the overall<br />
educational experience. At the end of the day, all the<br />
participating clinician were very pleased and came<br />
away with a greater knowledge of EUS products and<br />
better prepared to accurately diagnose and treat<br />
their EUS patients.<br />
The Channel<br />
NEW<br />
The<br />
cutting edge of<br />
optimal sampling<br />
Captura® Disposable Biopsy<br />
Forceps now available in serrated<br />
edged cups.<br />
<strong>Cook</strong> <strong>Medical</strong>’s Captura Forceps – now<br />
available with serrated cups – has been<br />
specifically designed to help you acquire<br />
the best possible tissue sample. And,<br />
because the jaws remain closed without<br />
constant handle pressure, you can be<br />
confident that acquired tissue remains<br />
in the cups when extracting the sample.<br />
For controlled passage through the<br />
endoscope, the coated sheath delivers<br />
variable suppleness and rigidity. <strong>Cook</strong><br />
forceps: Get on the cutting edge.<br />
COLD<br />
Shaft<br />
Order Number Description Length<br />
DBF-2.4S-230 2.4mm Serrated 230cm<br />
DBF-2.4S-230SP 2.4mm Serrated<br />
with Spike<br />
230cm<br />
DBF-2.4S-160 2.4mm Serrated 160cm<br />
DBF-2.4S-160SP<br />
HOT<br />
2.4mm Serrated<br />
with Spike<br />
160cm<br />
Shaft<br />
Order Number Description Length<br />
HDBF-2.4S-230 2.4mm Serrated 230cm<br />
www.cookmedical.com<br />
15
16 www.cookmedical.com<br />
<strong>Cook</strong> <strong>Medical</strong><br />
Endoscopy<br />
division<br />
President<br />
Bill Gibbons<br />
presents award<br />
to Sun-Young<br />
Lee, MD,<br />
Daniel Von<br />
Renteln, MD and<br />
Andres Sanchez<br />
Yague, MD.<br />
HONORS IMPORTANT CONTRIBUTORS TO ENDOSCOPY<br />
The American Society for Gastrointestinal Endoscopy (ASGE) honored important contributions to<br />
the field of endoscopy during the fifth annual ASGE Crystal Awards on May 31 as part of Digestive<br />
Disease Week (DDW). The always popular and elegant awards banquet was hosted by ASGE and<br />
the ASGE Foundation at the historic Navy Pier on the Chicago lakefront. During the gala, the newly<br />
established Marsha Dreyer Award, sponsored by <strong>Cook</strong> <strong>Medical</strong>, was introduced by <strong>Cook</strong> <strong>Medical</strong><br />
Endoscopy division President Bill Gibbons. (See page 8)<br />
Highlighting achievement and dedication, the ASGE Crystal Awards symbolize the finest in leadership,<br />
research and scientific pursuit. The event recognized the 2009 award and grant recipients who have<br />
shared their expertise to advance and strengthen the field of gastrointestinal endoscopy and the<br />
ASGE. Newly designated ASGE Fellows were recognized at this event. Proceeds from the event will<br />
benefit the ASGE Foundation in support of GI endoscopy-related research, physician education and<br />
training, and public outreach initiatives.<br />
The Crystal Awards Dinner featured live music, dinner and presentations to honorees by ASGE<br />
President, John L. Petrini, MD, FASGE, ASGE Foundation Chair, Francis Tedesco, MD, FASGE, various<br />
ASGE leaders and Master of Ceremonies, ASGE Past President and Foundation Trustee, David Carr-<br />
Locke, MD, FASGE.<br />
Crystal Awards recipients include:<br />
Christopher J. Gostout, MD, FASGE, Mayo Clinic, Rochester, MN, winner of the Rudolf V. Schindler<br />
Award, which is ASGE’s highest honor. This award is given to a member whose accomplishments in<br />
endoscopic research, teaching and/or service to ASGE exemplifies the standards and traditions of<br />
Rudolf V. Schindler, MD, founder of the American Gastroscopic Club, the forerunner of ASGE.<br />
George Triadafilopoulos, MD, DSc, FASGE, Stanford University School of Medicine, Stanford, CA,<br />
winner of the Distinguished Service Award, which is granted to an individual who has made long-term<br />
contributions to GI endoscopy in the areas of equipment research and development, as well as an<br />
individual who has been a strong supporter of the educational and research mission of the society.<br />
Anthony N. Kalloo, MD, FASGE, Johns Hopkins Hospital, Baltimore, MD, winner of the Distinguished<br />
Educator Award, which recognizes physicians who substantially contribute to the education of<br />
fellows through endoscopy seminars, participation in national postgraduate courses and published<br />
scholarly reviews or educational materials, including videos.<br />
D. Nageshwar Reddy, MD, Asian Institute of Gastroenterology, Hyderabad, India, winner of the Master<br />
Endoscopist Award, which recognizes physicians who spend the majority of their time in patient<br />
care and are recognized regionally or nationally for their expertise and longitudinal contributions<br />
to the practice of gastrointestinal endoscopy.<br />
Ma Somsouk, MD, MAS, University of California, San Francisco, CA, winner of the <strong>Cook</strong> <strong>Medical</strong><br />
Career Development Award for the project: Defective adaptive immune response and colorectal<br />
neoplasia in HIV infected individuals.<br />
Sun-Young Lee, MD, Konkuk University School of Medicine, Seoul, Republic of Korea, Daniel Von<br />
Renteln, MD, Klinikum Ludwigsburg, Ludwigsburg, Germany, and Andres Sanchez Yague, MD,<br />
Hospital Costa del Sol, Marbella, Spain, each won a <strong>Cook</strong> <strong>Medical</strong> Don Wilson Award, which provides<br />
advanced fellows or junior faculty with the opportunity to train outside of their home country<br />
with a premier GI endoscopist or group to advance their training. The awards are named to honor<br />
Don Wilson, founder of Wilson <strong>Cook</strong> <strong>Medical</strong>, who was a strong advocate and supporter of<br />
international education and training in GI endoscopy. The awards are underwritten by a grant from<br />
<strong>Cook</strong> <strong>Medical</strong>.<br />
<strong>Cook</strong> <strong>Medical</strong> congratulates all the 2009 Crystal Award winners. For a complete listing of the winners,<br />
contact ASGE at info@asge.org. The next Crystal Awards Dinner will take place during DDW in May<br />
2010 in New Orleans.
Memory <br />
serves us well<br />
in China<br />
A CASE REPORT<br />
Since our ERCP practice started in 1984, we have gradually built<br />
up an accumulation of experience and understanding along with<br />
a consistent increase in annual procedure numbers. At the same<br />
time, we feel strongly that procedural success rates and safety have<br />
a close correlation with the enhancement of design and quality of<br />
endoscopes as well as accessories. The Memory Basket, 7 FR Hard<br />
Wire (MWB), produced by <strong>Cook</strong> <strong>Medical</strong>, is one of our favorites<br />
among a range of extraction device options.<br />
While the CBD stone is a major indication of ERCP, extraction of<br />
stones plays an ultimate and essential role during the procedure<br />
after a sphincterotomy. Common extraction baskets usually handle<br />
well the removal of a single or a few small stones. However, most of<br />
our patients in China often show the presence of common bile duct<br />
dilation with a filling defect and piling of numerous stones or biliary<br />
sludge. Moreover, some patients even have a mass of intrahepatic<br />
stones. In such cases, it is usually difficult for a common basket to<br />
expand and pass across the stones. Instead, the extended basket<br />
can become distorted or bent and fail to capture the stones. For<br />
instance, the wire of one competitive basket may be too floppy<br />
to fully expand, while that of a second competitor’s basket is too<br />
rigid, with a sharp tip that is likely to injure the bile duct. By using<br />
the Memory Basket with spiral wires, we can rotate the handle to<br />
drive the distal end spirally forward. In addition, it is observed that<br />
sometimes the basket goes across the stones even more easily if<br />
we extend only 1/2 or 1/3 of the basket out of the sheath. Thanks<br />
to its wire, which has sufficient strength and good shape retention,<br />
the basket has an extra forward force and extraordinary expansion<br />
The First People’s<br />
Hospital of<br />
Hangzhou, Zhejiang<br />
- One of the most<br />
important ERCP<br />
training centers in<br />
China, completing<br />
over 1,500 ERCP<br />
cases annually.<br />
The Channel<br />
Prof. Zhang Xiao<br />
Director of Endoscopy<br />
Digestive Department of the<br />
First People’s Hospital of Hangzhou, Zhejiang<br />
www.cookmedical.com<br />
17
Figure 1<br />
T-tube cholangiography reveals<br />
image characteristics as a convex<br />
cup edge in lower part of CBD, and<br />
contrast medium fails to flow into<br />
enteric cavity.<br />
Figure 2<br />
After dislodging the stone, the<br />
papilla was dilated and the stone<br />
was successfully extracted.<br />
18 www.cookmedical.com<br />
capability to easily trap stones with less likelihood<br />
of injury to the dissected papilla and inner wall<br />
of the bile duct when extended. The distal end<br />
of the basket has a short, straight and rigid<br />
segment, which together with adjustments<br />
in endoscope orientation, aids in selectively<br />
entering bilateral intrahepatic bile ducts as<br />
needed. The Memory Basket dimensions are<br />
3×6 cm and 2×4 cm, with the former being more<br />
frequently used in our experience.<br />
Case Report<br />
A 75-year-old patient underwent surgery in May 2009<br />
at a local hospital due to acute obstructive suppurative<br />
cholangitis (AOSC). Choledochotomy was performed to<br />
remove stones and a T-tube was deployed for drainage. Prior<br />
to post-operative extubation, routine T-tube cholangiography<br />
was performed and revealed incarceration of a residual stone with a<br />
diameter of about 1 cm in the lower part of common bile duct, showing<br />
image characteristics as a convex cup edge. Contrast medium failed to flow into<br />
the enteric cavity. After two failed attempts of stone removal by choledochoscope, the<br />
patient was referred to our hospital. Repeated T-tube cholangiography demonstrated the<br />
same signs as before. (See Fig. 1)<br />
Routine ERCP was performed with a successful standard cannulation. However, repeated<br />
pushing forward of the wire guide against the stone resulted in the tip of the wire guide<br />
returning to the papillary opening. After sphincterotomy, we tried again to dislodge the<br />
stone by using an ERCP catheter with a preloaded wire guide, but again failed to push the<br />
stone up the duct. Though one of the competitive baskets has a rigid outer sheath with<br />
good pushability, its sharp tip makes us reluctant to use it when considering the risk of bile<br />
duct perforation. Initially, we used a second competitor’s basket, first holding it out against<br />
the stone, and then extending the basket out of the sheath. However, the basket wires bent<br />
back without dislodging the stone. After we changed to a Memory Basket (MWB-3x6), the<br />
stone was successfully pushed upward to the middle segment of the dilated common bile<br />
duct when we extended the basket wires abruptly. After dilation of the papillary opening to<br />
one cm, the stone was successfully extracted by the basket. (See Fig. 2)<br />
This case features a post-operative residual stone with incarceration. Two following attempts<br />
at stone removal by choledochoscope might have pushed the stone to a narrow lower<br />
segment of the CBD, resulting in an even tighter incarceration and more difficulties in lifting<br />
and freeing the stone during subsequent ERCP. An initial attempt at stone dislodgement with<br />
a competitor’s basket was unsuccessful, with the basket simply bending back when being<br />
extended against the stone. This may have been due to the baskets thin wire multifilament<br />
composition and the low pushability of its soft sheath. However, benefiting from the great<br />
catheter pushability and atraumatic blunt tip design of the Memory Basket, we eventually<br />
succeeded in extracting the stone. During the essential attempt of pushing the stone up<br />
the duct, the monofilament spiral wire was able to drive the incarcerated stone ahead once<br />
it had loosened slightly.
The Channel<br />
N E W S F R O M<br />
SIGNEA<br />
Society of International Gastroenterological Nurses and Endoscopy Associates<br />
Dr. Fazel is the Chief of Gastroenterology and <strong>Medical</strong> Director for Advanced Endoscopy at INOVA Fairfax Hospital in Fairfax, Virginia.<br />
According to the American Cancer Society<br />
(ACS), more than 16,000 new esophageal<br />
cancer cases are diagnosed each year in<br />
the U.S. Unfortunately the survival rate in<br />
these cases is only 10 percent. This alarming<br />
statistic is due largely to the fact that by the<br />
time the majority of cases are diagnosed, the<br />
cancerous tumors have grown to the point of<br />
inoperability. Raising patient awareness about<br />
potential conditions that, if left untreated, could<br />
progress into esophageal cancer, will encourage<br />
patients to seek the appropriate care through<br />
their physician.<br />
Contributing Risk Factors<br />
Many people are aware that tobacco use<br />
increases the risk of developing esophageal<br />
cancer; however, there are several other<br />
common contributing risk factors including:<br />
excessive alcohol consumption, obesity, lye<br />
ingestion and gastroesophageal reflux disease<br />
(GERD), also known as acid reflux or heartburn.<br />
A recent ACS Gallup poll revealed that 44<br />
percent of adults in the U.S. have heartburn at<br />
least once per month and that approximately<br />
30 percent of esophageal cancer cases can be<br />
linked to GERD. GERD is a condition in which<br />
acid (with some pepsin and bile) splashes up<br />
from the stomach into the esophagus. These<br />
three fluids are potentially dangerous to the<br />
sensitive esophageal tissue, as they can damage<br />
the lining of the esophagus, a condition known<br />
as esophagitis.<br />
If GERD becomes a chronic condition, it can<br />
develop into Barrett’s esophagus, a precursor<br />
to esophageal cancer. Barrett’s esophagus is a<br />
condition in which the color and composition<br />
of the cells lining the lower esophagus change<br />
due to repeated exposure to stomach acid. Only<br />
a small percentage of people with GERD develop<br />
Barrett’s esophagus, but once it is diagnosed,<br />
patients should be sure to meet with their<br />
physician regularly as they are at a greater risk<br />
of developing esophageal cancer.<br />
Symptoms of advanced GERD or the presence<br />
of Barrett’s esophagus include:<br />
Frequent heartburn. A burning-type<br />
pain in the lower part of the mid-chest,<br />
behind the breast bone, and in the<br />
mid-abdomen.<br />
Difficulty swallowing. Often, a narrowing<br />
of the esophagus (esophageal stricture)<br />
leads to trouble swallowing or dysphagia.<br />
Bleeding. A person may vomit red blood<br />
or blood that looks like coffee grounds, or<br />
your stools may be black, tarry or bloody.<br />
Weight loss and loss of appetite.<br />
According to the ACS, prevention of Barrett’s<br />
esophagus can begin with controlling GERD by<br />
making some simple lifestyle changes, such as:<br />
Losing weight. Obesity increases<br />
abdominal pressure, which can then push<br />
stomach contents up into the esophagus;<br />
Eating a diet full of fruits and vegetables,<br />
eating smaller and more frequent meals<br />
and not eating two to three hours prior<br />
to bedtime;<br />
Smoking cessation, as nicotine relaxes<br />
the esophageal sphincter and smoking<br />
also stimulates the production of<br />
stomach acid;<br />
Discontinuing the consumption<br />
of alcohol.<br />
People with severe GERD and Barrett’s<br />
esophagus often require aggressive treatment<br />
and prevention methods including medications,<br />
other nonsurgical medical procedures such as<br />
endoscopic therapies, or even laparoscopic<br />
and open surgeries. Often times, swallowing<br />
difficulty (known as dysphagia) and other<br />
symptoms can be treated if identified early.<br />
Technologies Emerging<br />
However, due to the aggressive nature of<br />
the disease, the majority of patients who<br />
have esophageal cancer are not surgical<br />
candidates. In these situations, the primary focus<br />
becomes palliative care – providing comfort<br />
measures to help maintain quality of life. This<br />
includes treating the dysphagia and restoring<br />
the patient’s ability to swallow food and<br />
drink liquids by opening the stricture within<br />
the esophagus.<br />
To open the barriers caused by tumor in-growth<br />
physicians use an esophageal metal stent. Prior<br />
to the stent placement the patient may require<br />
dilation of the stricture to allow room for the<br />
stent to be positioned, thereby expanding<br />
the lumen of the esophagus. Traditionally,<br />
the placement of the stent can be a painful<br />
process for the patient, yet new technologies<br />
are making this procedure easier on the patient<br />
and physician.<br />
New, innovative delivery systems enable<br />
accurate deployment and recapturability of the<br />
stent. This reduces the stent from moving or<br />
migrating into the stomach and thus the need<br />
for repeat procedures to replace or reposition the<br />
stent, one of the more common complications<br />
in traditional esophageal stenting.<br />
Increase Awareness<br />
Raising awareness about the primary precursors<br />
to esophageal cancer – GERD and<br />
Barrett’s esophagus – will encourage patients<br />
with these conditions to consult their physicians<br />
for the necessary screenings and treatment<br />
options. However, when palliative care becomes<br />
the primary option for patients with esophageal<br />
cancer, recent advancements in medical device<br />
technologies enable physicians to more easily<br />
implant an esophageal stent and in turn<br />
improve patients’ quality of life.<br />
www.cookmedical.com<br />
19
<strong>Cook</strong> <strong>Medical</strong> has long understood that optimal<br />
patient care is your focus, and it continues to be<br />
our focus as well. That’s why for more than twenty<br />
years we have assisted healthcare professionals<br />
in learning the latest in endoscopic GI technology<br />
and related disease information.<br />
That tradition continues as <strong>Cook</strong> <strong>Medical</strong>, in<br />
partnership with HealthStream (an accredited<br />
provider of continuing nursing education), offers<br />
three new educational activities:<br />
Updates in Esophageal Cancer with<br />
Focus on Barrett’s Esophagus<br />
Updates in Esophageal Cancer with<br />
Focus on Therapeutic Treatment Options<br />
Updates in Esophageal Cancer with<br />
Focus on Diagnosis and Palliation<br />
We are pleased to announce that the American Board<br />
of Certification for Gastroenterology Nurses (ABCGN)<br />
has reviewed these educational activities and<br />
recognized them as providing GI specific content.<br />
These activities are presented without charge by<br />
your <strong>Cook</strong> <strong>Medical</strong> district manager. Educational<br />
activity descriptions, objectives and the related<br />
accreditation information can be found at http://<br />
www.cookendoscopy.com/educationalpages/<br />
edprograms.html.<br />
Contact your <strong>Cook</strong> representative for more<br />
information or to arrange a presentation<br />
opportunity.<br />
A continuing nursing education activity sponsored by<br />
HealthStream. Grant funds provided by <strong>Cook</strong> <strong>Medical</strong>.<br />
20 www.cookmedical.com<br />
UPCOMING EVENTS<br />
ACG Regional Post Graduate Kansas City, MO Aug. 28-29<br />
Mayo Clinic - ERCP A-Z Rochester, MN Sept. 17-18<br />
ASGE - Excellence in GI Endoscopy Nursing Oak Brook, IL Sept. 25<br />
Asian Pacific Digestive Week (APDW) 2009 Taipei, Taiwan Sept. 28-Oct. 1<br />
Int. Course on Therapeutic Endoscopy (Marcon) Toronto, Canada Sept. 30-Oct. 3<br />
CSGNA (Canadian Society Of<br />
Gastroenterological Nurses)<br />
Toronto, Canada Oct.1- 3<br />
Gastroenterology & Hepatology (UCI) Las Vegas, NV Oct. 2-4<br />
Boston Live Endoscopy Boston, MA Oct. 8-9<br />
JDDW Kyoto, Japan Oct. 14-17<br />
AGW Brisbane, Australia Oct. 22-26<br />
ACG (American College of Gastroenterology) San Diego, CA Oct. 25-28<br />
Interventional GI Endoscopy Techniques Strasbourg, France Oct. 26-28<br />
MUSC - ERCP for Physicians Charleston, SC Oct. 29-30<br />
AASLD (Liver Meeting) Boston, MA Oct. 30 - Nov. 3<br />
Harvard Live EUS 09 Boston, MA Nov. 6-8<br />
UEGW & WCOG Congress London, UK Nov. 21-25<br />
ASGE - ERCP Boot Camp for the GI Team Oak Brook, IL Dec. 4-5<br />
MUSC - EUS for Physicians Charleston, SC Dec. 4-5<br />
24th International Workshop<br />
on Therapeutic Endoscopy<br />
Hong Kong Dec. 8 - 10<br />
MUSC - EUS for Nurses Charleston, SC Dec. 10-11<br />
NYSGE New York, NY Dec. 16-19<br />
An official publication of <strong>Cook</strong> <strong>Medical</strong>.<br />
4900 Bethania Station Road, Winston-Salem, NC 27105<br />
If you would like to submit material for The Channel, please email us at<br />
thechannel@cookmedical.com. We welcome your comments and suggestions.<br />
18804/0709