Klinefelter Syndrome in Adolescence - The Journal of Clinical ...
Klinefelter Syndrome in Adolescence - The Journal of Clinical ...
Klinefelter Syndrome in Adolescence - The Journal of Clinical ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Wikström et al. Testicular Degeneration <strong>in</strong> Adolescent KS Boys J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab, May 2004, 89(5):2263–2270 2269<br />
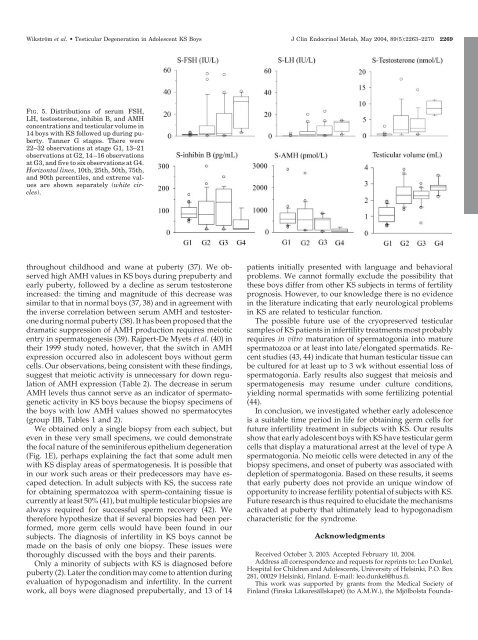
FIG. 5. Distributions <strong>of</strong> serum FSH,<br />
LH, testosterone, <strong>in</strong>hib<strong>in</strong> B, and AMH<br />
concentrations and testicular volume <strong>in</strong><br />
14 boys with KS followed up dur<strong>in</strong>g puberty.<br />
Tanner G stages. <strong>The</strong>re were<br />
22–32 observations at stage G1, 13–21<br />
observations at G2, 14–16 observations<br />
at G3, and five to six observations at G4.<br />
Horizontal l<strong>in</strong>es, 10th, 25th, 50th, 75th,<br />
and 90th percentiles, and extreme values<br />
are shown separately (white circles).<br />
throughout childhood and wane at puberty (37). We observed<br />
high AMH values <strong>in</strong> KS boys dur<strong>in</strong>g prepuberty and<br />
early puberty, followed by a decl<strong>in</strong>e as serum testosterone<br />
<strong>in</strong>creased: the tim<strong>in</strong>g and magnitude <strong>of</strong> this decrease was<br />
similar to that <strong>in</strong> normal boys (37, 38) and <strong>in</strong> agreement with<br />
the <strong>in</strong>verse correlation between serum AMH and testosterone<br />
dur<strong>in</strong>g normal puberty (38). It has been proposed that the<br />
dramatic suppression <strong>of</strong> AMH production requires meiotic<br />
entry <strong>in</strong> spermatogenesis (39). Rajpert-De Myets et al. (40) <strong>in</strong><br />
their 1999 study noted, however, that the switch <strong>in</strong> AMH<br />
expression occurred also <strong>in</strong> adolescent boys without germ<br />
cells. Our observations, be<strong>in</strong>g consistent with these f<strong>in</strong>d<strong>in</strong>gs,<br />
suggest that meiotic activity is unnecessary for down regulation<br />
<strong>of</strong> AMH expression (Table 2). <strong>The</strong> decrease <strong>in</strong> serum<br />
AMH levels thus cannot serve as an <strong>in</strong>dicator <strong>of</strong> spermatogenetic<br />
activity <strong>in</strong> KS boys because the biopsy specimens <strong>of</strong><br />
the boys with low AMH values showed no spermatocytes<br />
(group IIB, Tables 1 and 2).<br />
We obta<strong>in</strong>ed only a s<strong>in</strong>gle biopsy from each subject, but<br />
even <strong>in</strong> these very small specimens, we could demonstrate<br />
the focal nature <strong>of</strong> the sem<strong>in</strong>iferous epithelium degeneration<br />
(Fig. 1E), perhaps expla<strong>in</strong><strong>in</strong>g the fact that some adult men<br />
with KS display areas <strong>of</strong> spermatogenesis. It is possible that<br />
<strong>in</strong> our work such areas or their predecessors may have escaped<br />
detection. In adult subjects with KS, the success rate<br />
for obta<strong>in</strong><strong>in</strong>g spermatozoa with sperm-conta<strong>in</strong><strong>in</strong>g tissue is<br />
currently at least 50% (41), but multiple testicular biopsies are<br />
always required for successful sperm recovery (42). We<br />
therefore hypothesize that if several biopsies had been performed,<br />
more germ cells would have been found <strong>in</strong> our<br />
subjects. <strong>The</strong> diagnosis <strong>of</strong> <strong>in</strong>fertility <strong>in</strong> KS boys cannot be<br />
made on the basis <strong>of</strong> only one biopsy. <strong>The</strong>se issues were<br />
thoroughly discussed with the boys and their parents.<br />
Only a m<strong>in</strong>ority <strong>of</strong> subjects with KS is diagnosed before<br />
puberty (2). Later the condition may come to attention dur<strong>in</strong>g<br />
evaluation <strong>of</strong> hypogonadism and <strong>in</strong>fertility. In the current<br />
work, all boys were diagnosed prepubertally, and 13 <strong>of</strong> 14<br />
patients <strong>in</strong>itially presented with language and behavioral<br />
problems. We cannot formally exclude the possibility that<br />
these boys differ from other KS subjects <strong>in</strong> terms <strong>of</strong> fertility<br />
prognosis. However, to our knowledge there is no evidence<br />
<strong>in</strong> the literature <strong>in</strong>dicat<strong>in</strong>g that early neurological problems<br />
<strong>in</strong> KS are related to testicular function.<br />
<strong>The</strong> possible future use <strong>of</strong> the cryopreserved testicular<br />
samples <strong>of</strong> KS patients <strong>in</strong> <strong>in</strong>fertility treatments most probably<br />
requires <strong>in</strong> vitro maturation <strong>of</strong> spermatogonia <strong>in</strong>to mature<br />
spermatozoa or at least <strong>in</strong>to late/elongated spermatids. Recent<br />
studies (43, 44) <strong>in</strong>dicate that human testicular tissue can<br />
be cultured for at least up to 3 wk without essential loss <strong>of</strong><br />
spermatogonia. Early results also suggest that meiosis and<br />
spermatogenesis may resume under culture conditions,<br />
yield<strong>in</strong>g normal spermatids with some fertiliz<strong>in</strong>g potential<br />
(44).<br />
In conclusion, we <strong>in</strong>vestigated whether early adolescence<br />
is a suitable time period <strong>in</strong> life for obta<strong>in</strong><strong>in</strong>g germ cells for<br />
future <strong>in</strong>fertility treatment <strong>in</strong> subjects with KS. Our results<br />
show that early adolescent boys with KS have testicular germ<br />
cells that display a maturational arrest at the level <strong>of</strong> type A<br />
spermatogonia. No meiotic cells were detected <strong>in</strong> any <strong>of</strong> the<br />
biopsy specimens, and onset <strong>of</strong> puberty was associated with<br />
depletion <strong>of</strong> spermatogonia. Based on these results, it seems<br />
that early puberty does not provide an unique w<strong>in</strong>dow <strong>of</strong><br />
opportunity to <strong>in</strong>crease fertility potential <strong>of</strong> subjects with KS.<br />
Future research is thus required to elucidate the mechanisms<br />
activated at puberty that ultimately lead to hypogonadism<br />
characteristic for the syndrome.<br />
Acknowledgments<br />
Received October 3, 2003. Accepted February 10, 2004.<br />
Address all correspondence and requests for repr<strong>in</strong>ts to: Leo Dunkel,<br />
Hospital for Children and Adolescents, University <strong>of</strong> Hels<strong>in</strong>ki, P.O. Box<br />
281, 00029 Hels<strong>in</strong>ki, F<strong>in</strong>land. E-mail: leo.dunkel@hus.fi.<br />
This work was supported by grants from the Medical Society <strong>of</strong><br />
F<strong>in</strong>land (F<strong>in</strong>ska Läkaresällskapet) (to A.M.W.), the Mjölbolsta Founda-