FSTMK Annual Meeting 2011 - Foreningen af Specialtandlæger i ...
FSTMK Annual Meeting 2011 - Foreningen af Specialtandlæger i ...
FSTMK Annual Meeting 2011 - Foreningen af Specialtandlæger i ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Final announcement<br />
The Danish Association of Oral & Maxillofacial Surgeons<br />
(<strong>Foreningen</strong> <strong>af</strong> <strong>Specialtandlæger</strong> i Tand- Mund- og Kæbekirurgi)<br />
<strong>Annual</strong> <strong>Meeting</strong> Friday 4.11 – 5.11 <strong>2011</strong>, EC-hours = 9<br />
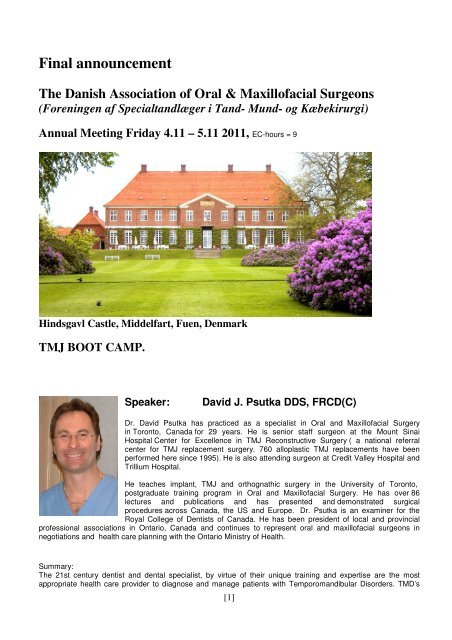
Hindsgavl Castle, Middelfart, Fuen, Denmark<br />
TMJ BOOT CAMP.<br />
Speaker: David J. Psutka DDS, FRCD(C)<br />
Dr. David Psutka has practiced as a specialist in Oral and Maxillofacial Surgery<br />
in Toronto, Canada for 29 years. He is senior st<strong>af</strong>f surgeon at the Mount Sinai<br />
Hospital Center for Excellence in TMJ Reconstructive Surgery ( a national referral<br />
center for TMJ replacement surgery. 760 alloplastic TMJ replacements have been<br />
performed here since 1995). He is also attending surgeon at Credit Valley Hospital and<br />
Trillium Hospital.<br />
He teaches implant, TMJ and orthognathic surgery in the University of Toronto,<br />
postgraduate training program in Oral and Maxillofacial Surgery. He has over 86<br />
lectures and publications and has presented and demonstrated surgical<br />
procedures across Canada, the US and Europe. Dr. Psutka is an examiner for the<br />
Royal College of Dentists of Canada. He has been president of local and provincial<br />
professional associations in Ontario, Canada and continues to represent oral and maxillofacial surgeons in<br />
negotiations and health care planning with the Ontario Ministry of Health.<br />
Summary:<br />
The 21st century dentist and dental specialist, by virtue of their unique training and expertise are the most<br />
appropriate health care provider to diagnose and manage patients with Temporomandibular Disorders. TMD’s<br />
[1]
are ubiquitous, <strong>af</strong>fecting 5 % of the population and causing millions of dollars in lost productivity and health care<br />
expense. Every dental practitioner will encounter these patients frequently. Many TMD's are managed<br />
successfully non-surgically. TMJ surgery has a definite role to play in TMD treatment algorithms and is currently<br />
a very underutilized modality. This lecture will blend current dentofacial orthopedic and rheumatological concepts<br />
necessary to a modern approach to understanding, diagnosing and treating TMD. In this presentation, Dr. David<br />
J. Psutka will talk about:<br />
Anatomy , growth and development<br />
Physiology and Patho-physiology<br />
Classification and Diagnosis of TMDs<br />
An approach to management of TMDs.<br />
A detailed overview of the current practice of TMJ Surgery.<br />
Program:<br />
Friday Nov. 04., <strong>2011</strong><br />
8.00- 8.30 Register<br />
8.30- 9.00 Breakfast<br />
9.00- 9.10 Welcome – Troels B. Folkmar<br />
9.10-11.00 Lecture: From embryology to total joint reconstruction<br />
11.00-11.45 Coffee break and exhibition<br />
11.45-12.30 Lecture: cont<br />
12.30-13.30 Lunch<br />
13.30-14.15 Lecture: cont<br />
14.15-14.45 Coffee break and exhibition<br />
14.45-15.50 Lecture: cont<br />
15.50-16.20 Discussion<br />
16.20-17.30 Topic related oral abstracts ( 10 min presentations)<br />
• Thomas Klit Pedersen – Aarhus University Hospital<br />
• Janek Dalsgaard Jensen – Aalborg Hospital<br />
• Kristian Andersen – Aarhus University Hospital<br />
• Lena Nørgaard – Odense University Hospital<br />
• Nils Worsae - Rigshospitalet<br />
• Esben Aagaard – Odense University Hospital<br />
• Esben Aagaard – Odense University Hospital<br />
19.00 Wellcome drink<br />
19.30 Dinner<br />
[2]
Saturday Nov. 5 <strong>2011</strong><br />
9.00-10.30 Residents hour – presentations mainly in Danish<br />
• Jens Hartlev – Aarhus University Hospital<br />
• Anja Carlsen – Aalborg Hospital<br />
• Kristian Thesbjerg – Aalborg Hospital<br />
• Tue Lindbjerg Blæhr – Aalborg Hospital<br />
• Lone Fuks - Rigshospitalet<br />
• Kristian Rude – Odense Universitetshospital<br />
• Anders Torp Jensen - Rigshospitalet<br />
• Pouya Yazdi - Rigshospitalet<br />
10.45-12.30 General Assembley (only for members)<br />
12.30 Lunch<br />
13.30 End of <strong>Annual</strong> <strong>Meeting</strong><br />
[3]
Abstracts:<br />
Friday Nov. 04., <strong>2011</strong><br />
16.20-17.30 Topic related oral abstracts ( 10 min presentations)<br />
Thomas Klit Pedersen, chief orthodontist, PhD<br />
Department of Maxillofacial Surgery, Aarhus University Hospital, Department of Orthodontics,<br />
Aarhus University, Denmark<br />
Abstract<br />
Inflammatory conditions of the temporomandibular joint.<br />
Idiopathic condylar resorption, condylysis, progressive condylar osteolysis, condylar atrophy are all<br />
terms used when a condition of changed morphology is seen of the mandibular condylar process. The<br />
terminology does not give any explanation concerning the etiology and the processes leading to<br />
condylar deformation. Furthermore, the course of progression and, maybe most important, the state of<br />
stability of the joint are not documented to a sufficient level assuring a constant result of the<br />
reconstructive treatment necessary to retrieve adequate, asymptomatic function and esthetics.<br />
Pathologic changes of the components of the temporomandibular joint causes mandibular positional<br />
alterations in adults and growth disturbances in the juvenile. Uncertainness exists concerning etiology,<br />
diagnosis, prognostic assessment, treatment and defining stability of the joint. The present lecture<br />
discusses possible etiology from an inflammatory point of view, possible treatment modalities and joint<br />
stability. A method for determining the state of pathology in the joint are described in order to support<br />
diagnosis and treatment.<br />
Jannek Dalsgaard Jensen, Consultant Oral and Maxillofacial Surgeon<br />
[4]
Dept. of Maxillofacial Surgery, Aalborg Hospital, Denmark<br />
Abstract:<br />
Modified condylotomi<br />
The modified condylotomi is an ekstra-articular surgical procedure used to manage patients with<br />
temporomandibular joint dysfunction. I will go through the procedure and tell you about the patients we<br />
have been treated in Aalborg.<br />
Kristian Andersen - PhD student<br />
Department of Maxillofacial Surgery, Aarhus University Hospital, Denmark<br />
Abstract<br />
Long-term follow-up on total reconstruction of the temporomandibular joint - functional,<br />
psychosocial and radiological assessments in a case-series study.<br />
Andersen K, Dahl M, Nørholt SE, Futarmal S, Svensson P.<br />
Department of Oral and Maxillofacial Surgery, Aarhus University Hospital and Department of<br />
Clinical Oral Physiology, Institute of Odontology, Aarhus University.<br />
This case-series included seven subjects who had total joint reconstruction with Biomet® Total<br />
Temporomandibular Joint (TMJ) Replacement System at Department of Oral and Maxillofacial<br />
Surgery, Aarhus University Hospital. The follow-up examination included a functional, psychosocial<br />
and radiological examination. The functional assessment was conducted according to the Research<br />
Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD). The radiological assessment<br />
involved a cone beam computed tomography (CBCT) (NewTom, USA). Oral health impact on quality<br />
of life was assessed by the Danish version of the Oral Health Impact Profile questionnaire (OHIP).<br />
Results: The prostheses were placed in average six years before the follow-up examination (range 4-9<br />
years). The range of mandibular movement was low in all directions. According to the RDC-TMD<br />
algorithm four subjects had myofacial pain. Two patients had a high chronic pain disability and three<br />
patients had a low disability. Patients with TMD disability had a high impact of oral health on quality of<br />
life for the sub-domains functional limitation, physical pain and physical disability. Heterotopic bone<br />
formation on the medial aspect of the reconstruction was observed in 8 out of 12 TMJ-reconstructions.<br />
Conclusion: This case-series study showed a 100 per cent survival rate of Biomet® Total<br />
Temporomandibular Joint (TMJ) Replacement System <strong>af</strong>ter six years of observation. A high occurrence<br />
of heterotopic bone formation on the medial aspect of the prostheses was observed. Furthermore, some<br />
patients had a chronic pain disability, low range of mandibular movement and impact of oral health on<br />
quality of life. Further studies are needed.<br />
[5]
Lena Nørgaard,<br />
Dept. of Maxillofacial Surgery, Odense University Hospital, Denmark<br />
Abstract<br />
Synovial chondromatosis in the temporomandibular joint<br />
Introduction: Synovial chondromatosis in the temporomandibular joint is a rare, benigne condition.<br />
The clinical findings include formation of metaplastic cartilage in the synovium of the joint.<br />
Subsequently, This hyperplastic formation results in numerous attached osteocartilagenous bodies.<br />
Furthermore, cartilagenous bodies are seen in the synovium. The etiology is unknown and diagnosis is<br />
often delayed due to the non specific symptoms.<br />
Materials and methods: We present a case of a 28 year old woman. The patient presented with a<br />
history of persisting, temporomandibular joint pain and crepitus in both joints and a self reported<br />
sensation of dual bite. Previous treatments included arthroscopy in the left joint, without specific<br />
findings and no effect on the patients symptoms. Furthermore, we present a review of the literature<br />
based on a systematic search in the National Library of Medicine´s PubMed. Search criteria included<br />
Synovial chondromatosis, temporomandibular joint .<br />
RESULTS: Following a new bilateral arthroscopy, the patient presents without symptoms and clinical<br />
and histologic findings revealed the diagnosis Synovial chondromatosis. 31 articles from 1952 to <strong>2011</strong><br />
confirmed, that this disease is a rare benigne condition with low recurrence. No authors have described<br />
transformation into malignant disease in the temporomandibular joint.<br />
CONCLUSION:Proper treatment and histologic verification of the clinical findings in cases with<br />
synovial chondromatosis are pertinent. The literature suggests removal of cartilage bodies or synovium<br />
and cartilage bodies, with open joint surgery or arthroscopy<br />
Nils Worsaae, DDS, Consultant Oral and Maxillofacial Surgeon<br />
Dept. of Maxillofacial Surgery, Rigshospitalet, University of Copenhagen, Denmark<br />
Abstract<br />
[6]
Interpositional arthroplasty of patients with TMJ-arthrosis. Short term results.<br />
A prospective study of 25 patients surgically treated forTMJ-arthrosis with interpositional arthroplasty<br />
using homologeous costal cartilage gr<strong>af</strong>ts (Tutoplast®) from 2007-2010.<br />
Results: Interincisal opening increased from median 31 mm (17-42) to 40 mm (37-44) and VAS pain<br />
score (0-10) was reduced from median 8 (6-9) to 2 (0-5.5) during the first year of follow-up.<br />
Complication with fragmentation of the interpositional material happened in one patient who was later<br />
reoperated. No other complications occurred<br />
From 2010 to <strong>2011</strong> ten additional patients have been operated with similar good results, except for two<br />
problematic cases.<br />
Conclusions: If the results of this moderate surgical approach are more long-standing it may be an<br />
alternative to more aggressive surgery in patients with severe TMJ arthrosis, although there are some<br />
limitations.<br />
Esben Aagaard, Consultant Oral and Maxillofacial Surgeon<br />
Dept. of Maxillofacial Surgery, Odense University Hospital, Denmark<br />
Abstract 1<br />
Combining Alloplastic TMJ Reconstruction with Orthognathic Movements via Digital<br />
Preoperative Planning and Custom Prostheses<br />
Aagaard E.*, Thygesen T.H.*, Flannery N.M.P.**, Weimer K.A.**, Christensen A.M.**<br />
*Dept. of Oral & Maxillofacial Surgery, Odense University Hospital, Denmark<br />
**Medical Modeling Inc., Golden, Colorado USA<br />
Purpose: Virtual surgical planning with CAD/CAM templates have been shown to facilitate<br />
orthognathic surgery as a viable alternative to traditional planning methods. Alloplastic reconstruction<br />
of the temporomandibular joint (TMJ) is performed with either off-the-shelf or custom components<br />
designed using traditional, non-digital methods. Over the last few years digital design of custom TMJ<br />
prostheses (Biomet MicroFixation) has proven to be accurate and effective. Concomitant reconstruction<br />
of the TMJ with orthognathic movements can now be directed from a completely digital plan involving<br />
CAD/CAM joint prostheses and CAD/CAM intermediate and/or final occlusal splints.<br />
Methods & Materials: Preoperative CT scans (0.75mm - 1.25mm slice spacing, .3mm-.45mm pixel<br />
size) were taken of patients requiring both orthognathic surgery and alloplastic replacement of the TMJ.<br />
The medical images were imported into the virtual surgical planning software and three-dimensional<br />
virtual models were created. The orthognathic surgery was digitally planned in a meeting between the<br />
surgeon and an engineer at the modeling company. Simulated post-operative digital models were then<br />
utilized to design customized total TMJ prostheses in a completely digital fashion. Custom implant<br />
components, anatomical model(s), surgical guide(s), orthognathic splint(s) and other template(s) were<br />
[7]
then designed and fabricated from the finalized virtual surgical plan and sent to the surgeon for use in<br />
the surgery.<br />
Results: Post operative evaluations of the surgical procedure, how the custom instruments facilitated<br />
the procedure, and how well the total joint prostheses fit will be discussed for a series of patients who<br />
underwent this procedure.<br />
Conclusion: A completely digital plan can be put together to simulate orthognathic movements and<br />
total TMJ replacement with its outputs being produced by CAD/CAM technology. Precision of implants<br />
and movements is predicatable and should be considered for cases needing combined TMJ replacement<br />
and orthognathic procedures.<br />
Abstract 2<br />
A prospective, Single Center Study on Patient Outcomes Following Temporomandibular Joint<br />
Replacement Using a Custom Made Biomet TMJ Prosthesis.<br />
1. Esben Aagaard, DDS, Chief Surgeon, 2. Torben H. Thygesen, DDS, PhD, Chief Surgeon,<br />
Department of Oral and Maxillofacial Surgery, Odense University Hospital, Soender Boulevard 29,<br />
5000 Odense C, Denmark, Europe<br />
Introduction: Traditionally, the treatment of temporomandibular disorders were based on diagnostic<br />
assessments, patient information, splint therapy, arthroscopies, arthrocentesis and finally, open joint<br />
surgeries. Earlier results of alloplastic TMJ surgery revealed inconsistent outcomes. In recent years,<br />
promising results with total joint reconstruction using new prosthesis types are published.<br />
Aim: This prospective, consecutive cohort clinical study aimed to describe a wide range of pre- and<br />
postoperative clinical variables following uni- or bilateral total, alloplastic TMJ reconstruction using a<br />
patient matched implant (TAR). (Biomet Microfixation´s Patient Matched Temporomandibular Joint<br />
(TMJ) Implant).<br />
Material and methods: A total of 81 alloplastic TMJ reconstructions were performed in 63 consecutive<br />
patients between November 2007 and August 2010. Five men and fifty-eight females (41 ± 16 years),<br />
participated in up to nine sessions: one before alloplastic reconstruction and 1 week, 1, 3, 6 12, 18, 24<br />
and 36 months <strong>af</strong>ter alloplastic TMJ reconstruction in either one or both sides (47 unilateral and 17<br />
bilateral). All patients were classified by the Wilkes Classification (n=5 Class III; n=19 Class IV; n=47<br />
Class V). Ten patients could not be staged by Wilkes classification (fracture, ankylosis, revisions and<br />
benign neoplasms). At each session VAS scores on jaw pain intensity were scored, as well as clinical<br />
evaluation of maximum incisal opening (MIO). In addition, frequency of adverse events such as<br />
hematoma, infection, swelling trismus, and joint revision were recorded.<br />
Results: The most common diagnoses were degenerated/resorbed joints (85.2%) and osteoarthritis<br />
(79.0%). The most common previous surgical treatment was arthroscopic lavage (81.5%). The mean<br />
follow up was 14.1 months (range: 3 months - 3 years). The results showed significant improvement<br />
relative to baseline (p
pain and unspecific swelling and one implant was removed due to severe infection and pain. The<br />
remaining adverse events resolved through proper treatment with antibiotics.<br />
Conclusions: The present study indicates, that TAR is a relevant treatment option, even in patients with<br />
a broad range of temporomandibular disorders. Our results showed, that the mean patients gained<br />
almost normal range of mouth opening and gained a significant reduction of pain following surgery.<br />
Although our results seem promising, it should be emphasized, that TAR is associated with some side<br />
effects and, thus, should only be used when less invasive procedures fail and a comprehensive<br />
presurgical work up is performed. Ongoing prospective studies with longer term follow-up are needed<br />
to consolidate possible significant treatment outcomes.<br />
[9]
Saturday Nov. 5 <strong>2011</strong><br />
9.00-10.00 Residents hour<br />
Jens Hartlev, resident<br />
Department of Maxillofacial Surgery, Aarhus University Hospital, NBG, Denmark<br />
Abstract<br />
Delvis rekonstruktion <strong>af</strong> zygomamaksil-komplekset med computer- designet alloplastisk<br />
implantat<br />
Baggrund: Kraniedefekter kan rekonstrueres med computerdesignede alloplastiske implantater.<br />
Polyetheretherketones (PEEK) patient specifikt implantat (PSI) til rekonstruktion <strong>af</strong> atrofi <strong>af</strong> zygomamaksilregionen<br />
er et nyt behandlingsalternativ, der ikke tidligere er beskrevet i litteraturen.<br />
Patienttilfælde 1: En 18-årig mand henvises fra Øjen<strong>af</strong>delingen, Aarhus Sygehus til Tand-, Mund- og<br />
Kæbekirurgisk Afdeling med henblik på rekonstruktion <strong>af</strong> atrofi omkring højre zygoma-maksilregion<br />
efter stråleterapi i tidlig barndom pga. retinoblastom. Ved en mindre kirurgisk operation korrigeres det<br />
atrofiske område vha. et PEEK PSI.<br />
Patienttilfælde 2: En 30-årig mand henvises fra Skadestuen, Aarhus Sygehus til Tand-, Mund- og<br />
Kæbekirurgisk Afdeling, med henblik på sekundær korrektion <strong>af</strong> ansigtsasymmetri omkring venstre<br />
zygoma-maksilregion efter traume. Ved en mindre kirurgisk operation korrigeres det asymmetriske<br />
område vha. et PEEK PSI.<br />
Konklusion: Rekonstruktion <strong>af</strong> ansigtsdeformiteter med et computerdesignet PEEK-PSI må i disse<br />
patienttilfælde betegnes som en succesfuld behandling i både funktionel, kosmetisk og psykologisk<br />
henseende. Operationen er <strong>af</strong> mindre invasiv karakter med få postoperative gener.<br />
Anja Carlsen, resident<br />
Dept. of Maxillofacial Surgery, Aalborg Hospital, Denmark<br />
Abstract<br />
Donor site complications when harvesting from the mandible ramus<br />
[10]
Background: Treatment of tooth loss with osseointegrated oral implants has a high success rate.<br />
However, placement of implants is frequently comprised or impossible due to atrophy of the alveolar<br />
process. Autogenous bone is generally the preferred gr<strong>af</strong>t material for reconstruction of the alveolar<br />
process and is usually harvested from the mandibular ramus. However the use of autogenous bone<br />
gr<strong>af</strong>ts is associated with the risk of donor site morbidity and complications.<br />
Purpose: The aim of the present study was to evaluate the morbidity and complications <strong>af</strong>ter bone<br />
harvesting from the mandibular ramus.<br />
Material and methods: 374 surgical procedures performed at The Department of Oral and Maxillofacial<br />
Surgery in Aalborg from the year 2000 to 2010 were retrospectively analysed based on records and Xrays.<br />
Data from records and X-rays was conducted according to registration sheet.<br />
Results: The frequency of temporary change in sensitivity was 5,9 % (n=22). The frequency of<br />
permanent reduced sensitivity was 0,5% (n=2). Hematoma occurred in 20 cases. Infection was<br />
registered in one case.<br />
Conclusion: The results of this study showed that bone harvested from the mandibular ramus is a s<strong>af</strong>e<br />
surgical procedure with few complications.<br />
Kristian Thesbjerg, resident<br />
Dept. of Maxillofacial Surgery, Aalborg Hospital, Denmark<br />
Abstract<br />
Deviation <strong>af</strong> næseseptum ved SARME<br />
Formål: At undersøge om løsning <strong>af</strong> næseseptum i forbindelse med SARME operationer har betydning<br />
for postoperativ deviation <strong>af</strong> næseseptum.<br />
Materiale og metode: I alt 20 patienter indgik i undersøgelsen (M=9, F=11) Patienterne blev vilkårligt<br />
grupperet i to grupper. Gruppe I (n=10) med løsning <strong>af</strong> næseseptum og gruppe II (n=10) uden løsning <strong>af</strong><br />
næseseptum. På alle patienterne blev der foretaget CBCT optagelser umiddelbart før<br />
distraktionsprocessen og ved <strong>af</strong>sluttet distraktion. Opmåling blev foretaget i Dolphin Imaging 11.0.<br />
Målemetoden blev testet ved at opmåle samme 10 patienter 2 gange med en uges mellemrum.<br />
Resultater: Gruppe I: 4 patienter viste en deviation på > 1,5 mm. efter distraktion. Gruppe II 1 patient<br />
havde deviation på > 1,5mm. Metode studie viste en maximalt SD på 0,46 mm og et konfidensniveau<br />
95 % på maximalt 0,33 mm.<br />
Diskussion/konklusion: Nærværende undersøgelse viser at løsning <strong>af</strong> næseseptum er nødvendig i<br />
forbindelse med SARME. Imidlertid er den kliniske betydning for den øgede risiko for deviation <strong>af</strong><br />
næseseptum stadig uklar, men formentlig uden betydning. Der er med baggrund heri grundlag for<br />
yderligere undersøgelse, involverende en klinisk vurdering <strong>af</strong> næseseptum<br />
[11]
Lone Fuks, resident<br />
Dept. of Oral and Maxillofacial Surgery, Rigshospitalet, University of Copenhagen, Denmark<br />
Abstract<br />
SAPHO syndrom.<br />
Præsentation <strong>af</strong> et klinisk tilfælde, gennemgang <strong>af</strong> symptomer og behandlingmuligheder.<br />
Dette syndrom bliver ofte overset ved udredning <strong>af</strong> patienter med klinisk manifesteret osteomyelitis og<br />
fejldiagnostiseres derfor med diagnosen "diffus scleroserende osteomyelitis" . Fejlagtig opstartes<br />
langvarig antibiotika behandling uden den ønskede effekt.<br />
Syndromet er bl.a. kendetegnet ved udvikling <strong>af</strong> "steril knoglenekrose" samt hud- og ledgener.<br />
Tue Lindbjerg Blæhr, resident<br />
Dept. of Maxillofacial Surgery, Aalborg Hospital, Denmark<br />
Abstract<br />
Benign fibrøs histiocytom, en case<br />
Benign fibrøs histiocytom er en mesenkymal tumor, der oftest optræder i huden på ekstremiteterne. Den<br />
ses meget sjældent i knoglevæv og ekstremt sjældent i kæbeskelettet. Tumoren forekommer i alle aldre,<br />
men oftest over 60-års alderen. Tumoren præsenterer sig i knogle oftest som en som en langsomt<br />
voksende hævelse medførende ekspansion <strong>af</strong> knoglen og eventuelt patologisk fraktur. Benign fibrøs<br />
histiocytom kan vokse aggressivt med indvækst i nærliggende anatomiske regioner, og behandles med<br />
kirurgisk resektion. I nærværende kasuistik præsenteres en 73-årig kvinde med et benign fibrøs<br />
histiocytom i underkæben, og de differentialdiagnostiske overvejelser diskuteres.<br />
Kristian Rude, resident<br />
Dept. of Maxillofacial Surgery, Odense University Hospital, Denmark<br />
Abstract<br />
Recenstruction of the maxilla using the fibula gr<strong>af</strong>t, immidiat implant placement and virtual<br />
planning techniques<br />
[12]
Purpose<br />
Presentation of a case of maxillary reconstruction using the microvascularized fibula gr<strong>af</strong>t, medpore<br />
implant and immidiate dental implants. Preoperative CT scans, manufacturing of rapid prototyping<br />
surgery template. Pre- and postoperative CT scans illustrating the predictability of the surgry.<br />
Dental implants are placed using template before (transplant) of the fibula gr<strong>af</strong>t making the case unique.<br />
Key words:<br />
Fibula gr<strong>af</strong>t, maxillary reconstruction, virtual planning,dental implants<br />
Case presentation<br />
A 15 year-old female introduced to the department of plastic surgery and the department of oral and<br />
maxillofacial surgery for (seeking) reconstruction of her right maxillary.<br />
1) Diagnose venøs vaskulær<br />
2) Primær kirurgi<br />
3) Resektion<br />
4) Præoperativ: æstetisk og funktionel problematik, herunder obturator, syn tygge,<br />
tale,livskvalitet<br />
5) ”Backward planning” mandibel positio – implantat position – postition <strong>af</strong> fibula<br />
6) transplantat<br />
Visuelt materiale:<br />
Klinisk foto præ-OP ( en face, profil)<br />
Pre- and postsurgical CT Superimposer<br />
Virtual plan and postsurgical CT superimposed<br />
Anders Torp Jensen, resident<br />
Dept. of Oral and Maxillofacial Surgery, Rigshospitalet, University of Copenhagen, Denmark<br />
Abstract<br />
Diagnostik og behandling <strong>af</strong> fibrøs dysplasi<br />
Der vil blive lagt vægt på differentialdiagnostikken med det ossificerende fibrom, herunder nye<br />
muligheder for diffentialdiagnostik vha. molekylærbiologi.<br />
Behandlingsmuligheder med Bisphosphonat-præperater, samt bedre forudsigelsen <strong>af</strong> fortsat progression<br />
ved måling <strong>af</strong> alkalisk phosphatase.<br />
Pouya Yazdi, resident<br />
Dept. of Oral and Maxillofacial Surgery, Rigshospitalet, University of Copenhagen, Denmark<br />
Abstract<br />
Tromboseprofylakse i forbindelse med tand,- mund- og kæbekirurgiske indgreb.<br />
[13]
Baggrund: Venøs tromboembolisme (VTE), defineret som dyb venøs trombose (DVT), lungeemboli<br />
(LE), eller en kombination <strong>af</strong> begge, er blandt de mest hyppige komplikationer hos indlagte patienter.<br />
LE er den hyppigste årsag til mortalitet blandt indlagte patienter, som kan forebygges. Med den<br />
kontinuerlige udvidelse <strong>af</strong> både det kirurgiske felt, samt behandling <strong>af</strong> kompleks medicinske patienter<br />
indenfor tand,- mund- og kæbekirurgi, er det en nødvendighed at have fokus på risikofaktorer for VTE.<br />
Formål: At give et indblik i eksisterende litteratur på området, samt at omtale gældende retningslinjer<br />
vedrørende tromboseprofylakse.<br />
[14]