CHAPTER 13 SKIN - NHS Devon
CHAPTER 13 SKIN - NHS Devon
CHAPTER 13 SKIN - NHS Devon
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
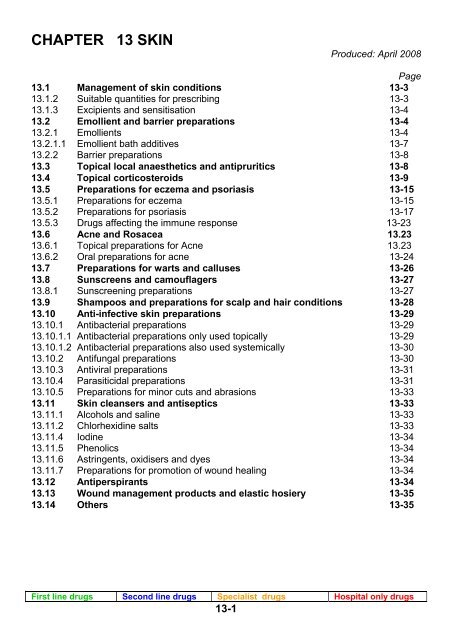
<strong>CHAPTER</strong> <strong>13</strong> <strong>SKIN</strong><br />
Produced: April 2008<br />
Page<br />
<strong>13</strong>.1 Management of skin conditions <strong>13</strong>-3<br />
<strong>13</strong>.1.2 Suitable quantities for prescribing <strong>13</strong>-3<br />
<strong>13</strong>.1.3 Excipients and sensitisation <strong>13</strong>-4<br />
<strong>13</strong>.2 Emollient and barrier preparations <strong>13</strong>-4<br />
<strong>13</strong>.2.1 Emollients <strong>13</strong>-4<br />
<strong>13</strong>.2.1.1 Emollient bath additives <strong>13</strong>-7<br />
<strong>13</strong>.2.2 Barrier preparations <strong>13</strong>-8<br />
<strong>13</strong>.3 Topical local anaesthetics and antipruritics <strong>13</strong>-8<br />
<strong>13</strong>.4 Topical corticosteroids <strong>13</strong>-9<br />
<strong>13</strong>.5 Preparations for eczema and psoriasis <strong>13</strong>-15<br />
<strong>13</strong>.5.1 Preparations for eczema <strong>13</strong>-15<br />
<strong>13</strong>.5.2 Preparations for psoriasis <strong>13</strong>-17<br />
<strong>13</strong>.5.3 Drugs affecting the immune response <strong>13</strong>-23<br />
<strong>13</strong>.6 Acne and Rosacea <strong>13</strong>.23<br />
<strong>13</strong>.6.1 Topical preparations for Acne <strong>13</strong>.23<br />
<strong>13</strong>.6.2 Oral preparations for acne <strong>13</strong>-24<br />
<strong>13</strong>.7 Preparations for warts and calluses <strong>13</strong>-26<br />
<strong>13</strong>.8 Sunscreens and camouflagers <strong>13</strong>-27<br />
<strong>13</strong>.8.1 Sunscreening preparations <strong>13</strong>-27<br />
<strong>13</strong>.9 Shampoos and preparations for scalp and hair conditions <strong>13</strong>-28<br />
<strong>13</strong>.10 Anti-infective skin preparations <strong>13</strong>-29<br />
<strong>13</strong>.10.1 Antibacterial preparations <strong>13</strong>-29<br />
<strong>13</strong>.10.1.1 Antibacterial preparations only used topically <strong>13</strong>-29<br />
<strong>13</strong>.10.1.2 Antibacterial preparations also used systemically <strong>13</strong>-30<br />
<strong>13</strong>.10.2 Antifungal preparations <strong>13</strong>-30<br />
<strong>13</strong>.10.3 Antiviral preparations <strong>13</strong>-31<br />
<strong>13</strong>.10.4 Parasiticidal preparations <strong>13</strong>-31<br />
<strong>13</strong>.10.5 Preparations for minor cuts and abrasions <strong>13</strong>-33<br />
<strong>13</strong>.11 Skin cleansers and antiseptics <strong>13</strong>-33<br />
<strong>13</strong>.11.1 Alcohols and saline <strong>13</strong>-33<br />
<strong>13</strong>.11.2 Chlorhexidine salts <strong>13</strong>-33<br />
<strong>13</strong>.11.4 Iodine <strong>13</strong>-34<br />
<strong>13</strong>.11.5 Phenolics <strong>13</strong>-34<br />
<strong>13</strong>.11.6 Astringents, oxidisers and dyes <strong>13</strong>-34<br />
<strong>13</strong>.11.7 Preparations for promotion of wound healing <strong>13</strong>-34<br />
<strong>13</strong>.12 Antiperspirants <strong>13</strong>-34<br />
<strong>13</strong>.<strong>13</strong> Wound management products and elastic hosiery <strong>13</strong>-35<br />
<strong>13</strong>.14 Others <strong>13</strong>-35<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-1
Appendices<br />
Appendix 1 – The Dermatology Referral Process <strong>13</strong> - 36<br />
Appendix 2 – Excipients that may cause sensitisation <strong>13</strong> - 37<br />
Appendix 3 – Urticaria Care Pathway <strong>13</strong> - 38<br />
Appendix 4 – NICE referral Advice for Atopic Eczema in Children, December<br />
2001 <strong>13</strong> - 39<br />
– NICE referral Advice for Psoriasis, December 2001<br />
Appendix 5 – Care Pathway for Atopic Eczema <strong>13</strong> - 41<br />
Appendix 6 – Detailed Instructions on the Use of Topical Tacrolimus <strong>13</strong> - 42<br />
and Pimecrolimus<br />
Appendix 7 – Psoriasis Care Pathway <strong>13</strong> - 44<br />
Appendix 8 – Acne Care Pathway <strong>13</strong> - 45<br />
Appendix 9 – Sun Damaged Skin Pathway <strong>13</strong> - 46<br />
Appendix 10 –NPSA Alert No 4: Fire Hazard with Paraffin Based Skin Products<br />
on Dressings and Clothing <strong>13</strong> - 47<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-2
<strong>13</strong>.1 Management of skin conditions<br />
Correct diagnosis of skin conditions is essential to effective treatment. The local<br />
dermatologists have recommended the following websites which give useful information for<br />
GPs and their patients to assist diagnosis and treatment.<br />
♦ British Association of Dermatologists: www.bad.org.uk<br />
♦ New Zealand Dermatological Society: www.dermnetnz.org<br />
♦ Clinical Knowledge Summaries (PRODIGY guidance): www.cks.library.nhs.uk<br />
♦ National Library for Health: www.library.nhs.uk<br />
The Dermatology department has also produced a number of care pathways as<br />
appendices to the chapter on the topics listed below.<br />
♦ The Dermatology Referral Process Appendix 1<br />
♦ Urticaria Appendix 3<br />
♦ Atopic Eczema Appendix 5<br />
♦ Psoriasis Appendix 7<br />
♦ Acne Appendix 8<br />
♦ Sun Damaged Skin Lesions Appendix 9<br />
IMPORTANT NOTE:<br />
♦ It is extremely important to consider patient acceptability of a skin product to maximise<br />
compliance. A wide range of products is available and patient acceptance of individual<br />
preparations is variable.<br />
♦ The aim of this formulary is to provide guidance on initial choice and sequence of<br />
treatments and to include sufficient agents to cover the vast majority of patient needs.<br />
♦ We recognise that in specific circumstances, dermatologists may need to use a nonformulary<br />
product. In such cases, the GP will be given sufficient information to<br />
continue prescribing where appropriate.<br />
<strong>13</strong>.1.2 Suitable quantities for prescribing<br />
The table below shows suitable quantities of dermatological preparations to be prescribed<br />
for specific areas of the body based on twice daily application for 1 week.<br />
This does not apply to corticosteroid preparations - See section <strong>13</strong>.4 for suitable<br />
quantities for corticosteroid preparations.<br />
Ointments and Creams Lotions<br />
Face 15 – 30g 100ml<br />
Both hands 25 – 50g 200ml<br />
Scalp 50 – 100g 200ml<br />
Both arms or both legs 100 – 200g 200ml<br />
Trunk 400g 500ml<br />
Groins and genitalia 15-25g 100ml<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-3
<strong>13</strong>.1.3 Excipients and sensitisation<br />
CSM Advice: In 2003 the CSM advised that medicinal products containing arachis oil<br />
should not be used in patients known to be peanut allergic because of a slight risk of the<br />
presence of some peanut protein in pharmaceutical grade arachis oil. They also advised<br />
that patients allergic to soya should also avoid products containing arachis oil because of a<br />
risk of cross-sensitivity.<br />
A table of excipients in topical preparations that may rarely be associated with sensitisation<br />
is provided in Appendix 2. Throughout this formulary, the presence of these possible<br />
sensitisers in products is indicated to aid product selection.<br />
If a patient is not responding to treatment and getting worse, consider the effect of<br />
sensitisers in topical preparations and refer for patch testing.<br />
Extemporaneous (‘specials’) preparation<br />
• A product should only be extemporaneously prepared when there is no product with a<br />
marketing authorisation available.<br />
• A pharmacy or specials manufacturer may do this, depending on the formulation.<br />
Where a specials manufacturer prepares the product, additional charges will be<br />
incurred.<br />
• Typically a special will cost in excess of £100 regardless of quantity and will have a<br />
shelf life of less than 28 days.<br />
Only prescribe commercially available products, unless otherwise advised by a<br />
dermatologist.<br />
<strong>13</strong>.2 Emollient and barrier preparations<br />
<strong>13</strong>.2.1 Emollients<br />
General information:<br />
• Emollients are essential in the management of dry skin conditions, but are underused<br />
in general practice. They reduce water loss from the epidermis resulting in softer,<br />
suppler skin. Used regularly, emollients may reduce flare-ups of eczema and the need<br />
for topical corticosteroids.<br />
• Greasy preparations (ointments) are preferable to creams in most circumstances<br />
because:<br />
♦ They contain fewer skin sensitisers.<br />
♦ They are more moisturising (i.e. water retaining).<br />
♦ They facilitate better penetration of active ingredients.<br />
• Patients should use the cheapest effective emollient that they are prepared to use<br />
regularly and is cosmetically acceptable.<br />
• Emollients should be smoothed on in the direction of hair growth. They should not be<br />
rubbed in.<br />
• Urea, salicylic acid and lactic acid are added to some products and may help hydrate<br />
thickened, keratinised skin.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-4
First Choice Emollients<br />
Note: All paraffin based and other greasy moisturisers are flammable. Patients supplied<br />
with an emollient, particularly those containing paraffin should be counselled that these<br />
products on dressings, clothing or skin are easily ignited on exposure to naked flame or<br />
cigarettes. Please see Appendix 10 – NPSA Alert 4.<br />
Greasy<br />
3<br />
Less<br />
greasy<br />
Preparation Comments<br />
50:50 Liquid and<br />
White Soft Paraffin<br />
Ointment<br />
2 Diprobase® Cream<br />
(contains cetostearyl alcohol,<br />
chlorocresol)<br />
1<br />
Aqueous Cream BP<br />
(contains cetostearyl alcohol)<br />
• Greasy but messy.<br />
• Good for dry skin eczema or<br />
acutely inflamed eczema or<br />
psoriasis.<br />
• Useful as a soap substitute and<br />
moisturiser.<br />
• Useful soap substitute.<br />
• Not moisturising enough for<br />
childhood or active eczema.<br />
• May irritate infant skins.<br />
Second Choice Emollients<br />
Preparation Comments<br />
Greasy<br />
3<br />
2<br />
1<br />
Less<br />
greasy<br />
Emulsifying Ointment<br />
(contains cetostearyl alcohol)<br />
Hydrous Ointment BP<br />
(oily cream)<br />
(contains lanolin)<br />
• Good for hands and feet.<br />
• Good soap substitute.<br />
• Can be stiff and difficult to apply if<br />
cold; therefore warm in a jug of<br />
warm water.<br />
• Useful general moisturiser.<br />
Doublebase ® gel • Quickly dries on the skin so<br />
convenient for frequent use during<br />
the day.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-5
Alternatives<br />
Notes:<br />
Patients may experience stinging or irritation of the skin when using emollients. If further<br />
options are required, consider the following preparations:<br />
Greasy<br />
3<br />
2<br />
Less<br />
greasy<br />
1<br />
Preparation Comments<br />
Epaderm ® Ointment<br />
(contains cetostearyl alcohol)<br />
E45 ® Cream<br />
(contains cetyl alcohol, cetostearyl<br />
alcohol, hydroxybenzoates<br />
(parabens), lanolin)<br />
Aveeno ® Lotion<br />
ACBS<br />
(contains benzyl alcohol, cetyl<br />
alcohol, isopropyl palmitate)<br />
Dermol ® 500 lotion<br />
(contains cetostearyl alcohol)<br />
• Good soap substitute.<br />
• Easier to apply when warm and<br />
soft.<br />
• Can feel ‘sticky’ to apply.<br />
• Soothing and cooling.<br />
• Based on oatmeal.<br />
• Also available OTC.<br />
• Contains antimicrobial agent-<br />
useful for weeping, mildly infected<br />
eczema.<br />
• Use alternative moisturiser when<br />
infection has cleared.<br />
Dermamist ® spray • Expensive.<br />
• A pressurised aerosol.<br />
• Occasionally useful for elderly<br />
patients or children with delicate<br />
skin.<br />
• Flammable.<br />
Neutrogena ®<br />
Dermatological<br />
Cream<br />
• Sometimes useful for hand<br />
eczema.<br />
• Encourage patients to buy over<br />
the counter.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-6
Emollient Preparations Containing Urea<br />
Urea, added to some products, may help hydrate thickened, keratinised skin.<br />
Preparation Comments<br />
Aquadrate ® Cream<br />
Balneum ® Plus Cream<br />
(contains benzyl alcohol, polysorbates)<br />
<strong>13</strong>.2.1.1 Emollient bath additives<br />
Contains 10 % urea.<br />
• For dry scaling and itching skin.<br />
• May help hands and feet<br />
• Apply generously and smooth into area<br />
as required.<br />
Contains 5 % urea and soya oil.<br />
• Has antipruritic properties.<br />
• Useful in elderly patients as bath oils<br />
often unsuitable.<br />
• Apply generously twice a day.<br />
Notes:<br />
1. Soap substitutes, aqueous cream or emulsifying ointment are safer than bath oils as<br />
they are less likely to make the bath slippery compared with bath oils.<br />
2. Soap substitutes are necessary in inflammatory skin disease.<br />
3. A bath mat may help reduce the risk of slipping where bath oils are used.<br />
Preparation Comments<br />
Hydromol Emollient ® Bath<br />
additive<br />
Oilatum ® Emollient bath<br />
additive<br />
(contains isopropyl palmitate, fragrance)<br />
Oilatum ® Shower<br />
emollient gel (contains fragrance)<br />
• Less expensive per ml than Oilatum ® .<br />
• Adults add 1-3 capfuls to the bath;<br />
infants: ½-2 capfuls<br />
• Adults add 1-3 capfuls to the bath;<br />
infants: ½-2 capfuls<br />
• Expensive but can be applied directly to<br />
skin as a moisturiser.<br />
• Gel formulation less likely to cause<br />
slipping compared with oils.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-7
Antimicrobial / emollient combination products<br />
Notes:<br />
1. Routine prophylactic use of antiseptic / emollient combinations is not recommended.<br />
2. A short course of a suitable oral antibiotic may be appropriate in patients with physical<br />
signs of infection and proven on skin swab.<br />
3. In recurrent staphylococcal infection please do a nasal swab.<br />
4. If not responding to the above preparations, the addition of an antimicrobial may be<br />
warranted.<br />
Preparation Comments<br />
Oilatum ® Plus<br />
bath additive<br />
(contains wool fat, isopropyl palmitate)<br />
Dermol ® 500 lotion<br />
(contains cetostearyl alcohol)<br />
• Contains benzalkonium chloride 6%,<br />
triclosan 2% and liquid paraffin 52.5%.<br />
• May sting.<br />
• Add 1-2 capfuls to the bath (infant over<br />
6 months 1ml added to the bath)<br />
• Contains benzalkonium chloride and<br />
chlorhexidine.<br />
• Apply to skin or use as a soap<br />
substitute.<br />
<strong>13</strong>.2.2 Barrier preparations<br />
Preparation Comments<br />
Zinc and castor oil<br />
ointment BP<br />
Zinc oxide 7.5%, castor oil 50%<br />
(contains beeswax, cetostearyl alcohol,<br />
peanut oil)<br />
Conotrane ® Cream<br />
(contains cetostearyl alcohol, fragrance)<br />
• For nappy and urinary rash<br />
• For nappy and urinary rash and<br />
pressure sores<br />
Metanium ® Ointment • For nappy rash and related disorders<br />
<strong>13</strong>.3 Topical local anaesthetics and antipruritics<br />
Notes on treatment of pruritus:<br />
1. An emollient may be of value in pruritus associated with dry skin.<br />
2. Antihistamines can prove valuable in treating generalised itching. (see Chapter 3)<br />
3. We cannot recommend the use of doxepin cream, which is sometimes used for pruritis<br />
ani. It is very expensive and current evidence shows that it is little more effective than<br />
vehicle cream alone.<br />
4. Calamine preparations are often ineffective and have little proven benefit. If necessary<br />
it is best to buy calamine in aqueous cream OTC.<br />
A DETAILED CARE PATHWAY FOR URTICARIA IS PROVIDED - SEE APPENDIX 3<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-8
Preparation Comments<br />
Eurax ® (Crotamiton)<br />
Cream<br />
(contains beeswax, fragrance,<br />
hydroxybenzoates (parabens), stearyl<br />
alcohol)<br />
Eurax ® (Crotamiton)<br />
Lotion<br />
(contains cetyl alcohol, fragrance, propylene<br />
glycol, sorbic acid, stearyl alcohol)<br />
• Contains antipruritic agent crotamiton.<br />
• More soothing than cream<br />
• Contains antipruritic agent crotamiton.<br />
• Dries skin, so not suitable for eczema.<br />
<strong>13</strong>.4 Topical corticosteroids<br />
Many patients are reluctant to use topical corticosteroids because of the fear of local and<br />
systemic effects. Patients should be reassured that side-effects are rarely seen when mild<br />
or moderately potent steroids are used in short or intermittent courses.<br />
Emollients can reduce the need to use topical steroids in atopic eczema and psoriasis.<br />
All patients with dry skin conditions should be using an effective emollient regimen. Soaps<br />
and detergents should be avoided by using substitutes such as aqueous cream. (See<br />
section <strong>13</strong>.2.1.1)<br />
When topical steroids are prescribed for eczema, the following should be explained:<br />
The incurable and chronic nature of the disease<br />
That we aim to manage the disease<br />
The different potencies of each steroid preparation<br />
The area(s) of the body where each product should be used<br />
How much to apply<br />
How long to apply them for and when to restart<br />
How often to apply them in relation to other treatments<br />
As with all topical preparations, topical corticosteroids should be smoothed<br />
onto the skin in the direction of hair growth. Do not rub in.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-9
AGE<br />
ONE Adult<br />
finger tip unit<br />
(FTU) *<br />
Face &<br />
Neck<br />
Number of Finger Tip Units (FTUs)<br />
Arm &<br />
Hand<br />
Leg &<br />
Foot<br />
Trunk<br />
(front)<br />
Trunk<br />
(back incl.<br />
buttocks)<br />
Adult 2 ½ 4 8 7 7<br />
Children:<br />
3-6 months 1 1 1 ½ 1 1 ½<br />
1-2 years 1 ½ 1 ½ 2 2 3<br />
3-5 years 1 ½ 2 3 3 3 ½<br />
6-10 years 2 2 ½ 4 ½ 3 ½ 5<br />
* One adult finger tip unit (FTU) is the amount of ointment or cream expressed from a tube<br />
with a standard 5mm diameter nozzle, applied from the distal crease to the tip of the index<br />
finger. If preferred the patient can be counselled to use a ruler to measure the amount i.e.<br />
2cm (or 1inch) = 1 FTU.<br />
How much to prescribe?<br />
The table below shows suitable quantities of dermatological preparations to be prescribed<br />
for specific areas of the body based on twice daily application for 1 week. It is important<br />
to prescribe sufficient quantities to last 1-2 weeks.<br />
Ointments and creams<br />
Face and neck 15 – 30 g<br />
Both hands 15 - 30 g<br />
Scalp 15 - 30 g<br />
Both arms 30 - 60 g<br />
Both legs 100 g<br />
Trunk 100 g<br />
Groins and genitalia 15 - 30 g<br />
“To be spread thinly” is a cautionary warning which can be misleading and worry some<br />
patients. It is therefore vital to counsel patients on the correct application by<br />
fingertip units and ensure adequate coverage of affected areas.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-10
NICE TAG81: Frequency of application of topical corticosteroids for atopic eczema,<br />
August 2004<br />
It is recommended that<br />
• Topical corticosteroids for atopic eczema should be prescribed for application only once<br />
or twice daily.<br />
• Where more than one alternative topical corticosteroid is considered clinically<br />
appropriate within a potency class, the drug with the lowest acquisition cost should be<br />
prescribed, taking into account pack size and frequency of application.”<br />
Choice of Preparation<br />
• CAUTION MUST BE USED WHEN SELECTING CORTICOSTEROIDS FOR<br />
DIFFERENT PARTS OF THE BODY.<br />
♦ Use lower potency corticosteroids for the face and other sensitive areas.<br />
♦ Use the least potent steroid to control symptoms.<br />
• Ointments are preferable to creams in most circumstances because:<br />
♦ They contain fewer skin sensitisers.<br />
♦ They are more moisturising (i.e. water retaining).<br />
♦ They facilitate better penetration of steroid.<br />
• Creams can be useful for:<br />
♦ Application to the face.<br />
♦ Moist or weeping lesions.<br />
♦ Daytime use with an ointment at night.<br />
Topical Corticosteroid Use<br />
1. Flare-ups can be treated initially with a potent steroid and then stepped down to a lower<br />
potency or an emollient.<br />
2. Topical steroids should normally be used for short periods (3-7 days) to treat<br />
exacerbations.<br />
3. Topical steroids should not be used regularly for more than 4 weeks without review.<br />
4. Review patients requiring steroid maintenance therapy at least every 3 months.<br />
5. Long-term use of potent and very potent steroids should be supervised by a<br />
dermatologist / nurse specialist.<br />
6. Topical steroids should not be used routinely on infected skin, unless the infection is<br />
being treated. A short course of a suitable oral antibiotic may be indicated.<br />
7. Remind patients to dispose of unwanted or out of date medicines as reuse of a<br />
microbially contaminated steroid product could be harmful.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-11
Topical Corticosteroid preparations<br />
Preparation Comments<br />
Mild Potency<br />
Moderate Potency<br />
Potent<br />
Very Potent<br />
Hydrocortisone:<br />
Efcortelan ®<br />
(excipients may differ depending on<br />
brand see BNF)<br />
Ointment: 0.5%, 1%, 2.5%<br />
Cream: 0.5%, 1%,2.5%<br />
Betamethasone<br />
valerate:<br />
Betnovate RD ® 0.025%<br />
ointment or cream (cream contains:<br />
cetostearyl alcohol, chlorocresol)<br />
Clobetasone butyrate:<br />
Eumovate ® 0.05% ointment or<br />
cream (cream contains: beeswax<br />
substitute, cetostearyl alcohol,<br />
chlorocresol<br />
Betamethasone<br />
valerate Betnovate ®<br />
Ointment or cream: 0.1% (excipients<br />
for cream vary depending on brand,<br />
see BNF)<br />
Mometasone furoate<br />
Elocon ® 0.1% ointment or cream<br />
(cream contains: stearyl alcohol)<br />
Clobetasol propionate<br />
Dermovate ® 0.05% ointment<br />
or cream (cream contains: beeswax<br />
(or beeswax substitute), cetostearyl<br />
alcohol, chlorocresol, propylene<br />
glycol)<br />
• Please prescribe as Efcortelan ® it<br />
is much cheaper.<br />
• 1% ointment and cream is sold OTC<br />
for treatment (max 1 week) of<br />
allergic contact dermatitis, irritant<br />
dermatitis, insect bite reactions and<br />
mild to moderate eczema. It can’t be<br />
sold for use on eyes/face, anogenital<br />
region, broken or infected skin.<br />
• Cream is sold OTC for short-term<br />
treatment and control of patches of<br />
eczema and dermatitis (not<br />
seborrhoeic dermatitis) for adults<br />
and children over 12 years.<br />
• Of similar potency to Betnovate<br />
RD ®<br />
• Some patients are intolerant to the<br />
ointment as it sometimes stings.<br />
• Do not use unless<br />
a potent steroid is<br />
not sufficient<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-12
Corticosteroid Preparations for the Scalp<br />
Preparation Comments<br />
Potent<br />
Very Potent<br />
Betamethasone<br />
valerate<br />
Betnovate ® Scalp<br />
Application: 0.1% (watermiscible<br />
base)<br />
Betacap ® Scalp<br />
Application: 0.1% (watermiscible<br />
base contains coconut oil)<br />
Fluocinolone<br />
acetonide<br />
Synalar ® 0.025% gel<br />
Use on scalp (gel contains parabens<br />
and propylene glycol)<br />
Dermovate ® Scalp<br />
Application: 0.05%, in a<br />
thickened alcoholic basis<br />
• Contains no alcohol – less likely<br />
to irritate scalp.<br />
• Some patients find this more<br />
acceptable than Betnovate ®<br />
application which may sting.<br />
• Penetrates better to the scalp<br />
than Betnovate ® .<br />
• Gel for scalp can be easier to<br />
control and is less likely to dribble<br />
onto face.<br />
• Has an alcoholic base. It is very<br />
useful for some patients with<br />
psoriasis.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-<strong>13</strong>
Antimicrobial / steroid combination products<br />
• Topical steroid preparations that include an antibacterial or antifungal may<br />
occasionally have a place where there is associated bacterial or fungal infection.<br />
• Antibacterials that are used for other purposes should not be used for “possibly”<br />
infected skin – i.e. SODIUM FUSIDATE AS FUCIDIN, FUCIDIN HC OR FUCIBET.<br />
• The use of Betnovate-C ® or Daktacort ® is preferable.<br />
Mild Potency<br />
Moderate<br />
Potency<br />
Potent<br />
Preparation Comments<br />
Vioform-<br />
Hydrocortisone ®<br />
Hydrocortisone 1%, clioquinol 3%;<br />
ointment or cream<br />
Daktacort ®<br />
Hydrocortisone 1%, miconazole<br />
nitrate 2% Ointment / Cream<br />
(contains: butylated hydroxyanisole,<br />
disodium edetate)<br />
Trimovate ®<br />
Clobetasone butyrate 0.05%,<br />
oxytetracycline 3%, nystatin<br />
100,000 units/g; cream (contains:<br />
cetostearyl alcohol, chlorocresol,<br />
sodium metabisulphite)<br />
Betnovate-C ®<br />
Betamethasone 0.1%, clioquinol<br />
3%; ointment or cream (cream<br />
contains: cetostearyl alcohol,<br />
chlorocresol)<br />
Note: Stains clothing<br />
• Useful for seborrheic dermatitis.<br />
• Has both antifungal and<br />
antibacterial properties<br />
• 15g cream can be sold over the<br />
counter for short-term treatment<br />
of athlete’s foot and candidal<br />
intertrigo.<br />
Note: Stains clothing<br />
Note: stains clothing<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-14
<strong>13</strong>.5 Preparations for eczema and psoriasis<br />
<strong>13</strong>.5.1 Preparations for eczema<br />
NICE Referral Advice for Atopic Eczema in Children, 2001 is provided<br />
- See Appendix 4<br />
A DETAILED CARE PATHWAY FOR ECZEMA IS PROVIDED - APPENDIX 5<br />
Treatment of eczema<br />
The main treatments for eczema are broadly outlined below<br />
1. Emollients and soap substitutes (See Section <strong>13</strong>.2.1 for more info):<br />
• Emollients should be the mainstay of eczema treatment.<br />
• Must be used frequently, at least twice daily, on all areas of the skin even where<br />
there is no visible sign of eczema. They should be used every 2 hours when the<br />
condition is florid.<br />
2. Topical steroids (See Section <strong>13</strong>.4 for more info):<br />
• Useful for reducing inflammation and itching.<br />
• Choice of steroid prescribed should depend upon patient age, site affected,<br />
severity of the eczema and whether or not infection is present.<br />
3. Drugs affecting the immune system: Please see below for NICE guidance on<br />
tacrolimus/pimecrolimus.<br />
4. Antihistamine treatment:<br />
• Sedating antihistamines can be useful for itching at night, but are not advisable in<br />
the day time.<br />
5. Treatment of infection:<br />
• Infection of broken skin is common making the patient feel unwell and limiting<br />
movement.<br />
• Staph. aureus infection is the commonest cause of acute flare up of atopic eczema<br />
and should be treated accordingly, e.g. flucloxacillin.<br />
6. Other treatments:<br />
• Dry tubular bandages applied over topical treatments or wet/paste bandages<br />
applied to severe eczema can help soothe discomfort. These methods should be<br />
demonstrated to the patient/carer by a health professional trained to do this.<br />
• This will increase absorption of the topical steroids, therefore use only mild and<br />
moderate potency steroids for this purpose.<br />
• Ichthammol is a specialist (amber) drug and should only be used in ENT.<br />
Please refer to Chapter 12.<br />
• There is no evidence to support the use of gamolenic acid in eczema.<br />
Prescribers are recommended not to prescribe unlicensed gamolenic acid or<br />
evening primrose oil.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-15
Eczema Treatment:<br />
Drugs affecting the immune response (from BNF section <strong>13</strong>.5.3)<br />
Preparation Comments<br />
Azathioprine<br />
Tablets (25mg and 50mg tablets)<br />
Ciclosporin<br />
Capsules (25mg, 50mg and 100mg tablets)<br />
Can only be prescribed by<br />
GPs<br />
under Shared Care agreement-<br />
See Chapter 20.<br />
Used for severe refractory eczema<br />
(unlicensed indication)<br />
Can only be prescribed by<br />
GPs<br />
under Shared Care agreement-<br />
See Chapter 20.<br />
Can be used for severe atopic eczema<br />
unresponsive to conventional treatments<br />
Alitretinoin ♦ Capsules 10mg, 30mg<br />
NICE Guidance (TAG 177) Alitretinoin for the treatment of severe chronic hand<br />
eczema (August 2009)<br />
Alitretinoin is recommended as a possible treatment for people with severe chronic hand<br />
eczema if:<br />
• their eczema has not improved with treatments called potent topical corticosteroids<br />
and:<br />
• standard assessments show their eczema is severe and is affecting their quality of life.<br />
See http://guidance.nice.org.uk/TA177 for full guidance.<br />
Topical Immunomodulators<br />
Tacrolimus<br />
Ointment 0.1%<br />
Ointment 0.03%<br />
Pimecrolimus<br />
Cream 1%<br />
Preparation Comments<br />
Guideline For use only in accordance with<br />
NICE guideline below. For detailed usage<br />
instructions see Appendix 4<br />
Guideline For use only in accordance with<br />
NICE guideline below.<br />
Summarised NICE TA082 (August 2004) guidelines: Tacrolimus and Pimecrolimus<br />
for Atopic Eczema<br />
• Topical tacrolimus and pimecrolimus are not recommended for the treatment of mild<br />
atopic eczema or as first-line treatments for atopic eczema of any severity.<br />
• These preparations are only recommended by NICE under the circumstances detailed<br />
in the table below provided the skin is free from infection AND WHEN:<br />
(a) Eczema is resistant to adequate use of topical corticosteroids at maximum<br />
strength and potency appropriate for patient’s age and area being treated AND<br />
(b) There is a serious risk of important adverse effects from further topical<br />
corticosteroid use, particularly irreversible skin atrophy.<br />
The table below summarises the NICE recommendations for each product.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-16
Product Strength NICE<br />
Recommended<br />
age group<br />
Tacrolimus<br />
Ointment<br />
Tacrolimus<br />
Ointment<br />
Pimecrolimus<br />
Cream<br />
NICE<br />
Recommended<br />
0.1% Adults ≥ 16yrs Any area of the<br />
body including<br />
face, neck and<br />
flexures.<br />
0.03% Adults and<br />
Children ≥<br />
2yrs<br />
1% * Children aged 2-<br />
16yrs ONLY<br />
Any area of the<br />
body including<br />
face, neck and<br />
flexures.<br />
Face and neck<br />
ONLY for<br />
patients<br />
intolerant to<br />
tacrolimus<br />
Severity of<br />
Eczema<br />
licensed for<br />
Moderate to<br />
severe<br />
Moderate to<br />
severe<br />
Moderate ONLY<br />
* Weak evidence for efficacy of pimecrolimus 1% compared with tacrolimus 0.1% in<br />
adults.<br />
Because the effect of long term use of immunomodulators is unclear NICE recommends<br />
that topical tacrolimus and pimecrolimus is ONLY initiated by physicians (including GPs)<br />
with a special interest and experience in dermatology, and only after careful discussion with<br />
the patient of the potential risks and benefits of all appropriate second-line treatment<br />
options. Advice is available from the dermatology department (01803 654837).<br />
DETAILED COUNSELLING POINTS AND USAGE INSTRUCTIONS FOR TOPICAL<br />
TACROLIMUS AND PIMECROLIMUS ARE PROVIDED IN APPENDIX 6<br />
<strong>13</strong>.5.2 Preparations for psoriasis<br />
NICE Referral Advice for Psoriasis, December 2001 is Provided – See Appendix 4<br />
DETAILED CARE PATHWAY FOR PSORIASIS IS PROVIDED - APPENDIX 7<br />
Treatment of Psoriasis<br />
Treatment is usually effective; the skin becomes less scaly and may even look completely<br />
normal. Topical treatment may include the following:<br />
1. Emollients – used as frequently as needed<br />
2. Vitamin D derivatives – more expensive than other topical treatments, but equally or<br />
slightly more effective than the alternatives (other than for guttate psoriasis when<br />
vitamin D derivatives are generally less effective).<br />
3. Tar preparations – can help, but many find them “messy” and can stain clothing<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-17
4. Topical steroids – can be very useful for limited psoriasis, flexural psoriasis or<br />
extremely unstable erythrodermic psoriasis. The weaker steroids often do not work<br />
very well on thick patches, but may work better on the face or in the skin folds.<br />
5. Salicylic acid – can be used on heavily scaled plaques, but irritation may occur<br />
6. Dithranol – can cause severe skin irritation and should only be prescribed by those<br />
experienced in its use. It should only be used for short contact periods of 30-60<br />
minutes.<br />
7. Drugs affecting the immune system: Reserved for patients with severe psoriasis<br />
unresponsive to conventional therapies.<br />
8. For additional scalp preparations see section <strong>13</strong>.9<br />
Topical Preparations for Treating Psoriasis:<br />
N.B. Avoid irritant preparations (tar, dithranol, vitamin D derivatives) in flexure psoriasis. A<br />
mild steroid, with or without an antiseptic, is more appropriate.<br />
Vitamin D and Analogues<br />
Preparation Comments<br />
Calcipotriol<br />
Dovonex ® cream 50micrograms/g;<br />
120g (contains: cetostearyl alcohol,<br />
disodium edetate)<br />
Calcipotriol<br />
Oint 50micrograms/g; (contains: cetostearyl<br />
alcohol, disodium edetate)<br />
Dovonex ® Scalp solution<br />
50micrograms / ml; 60ml, 120ml (contains:<br />
propylene glycol)<br />
Calcitriol Silkis ®<br />
Ointment 3mcg/g 100g<br />
• Apply once or twice daily maximum<br />
100g/week, children12-16 yrs max<br />
75g/wk, children 6-12 years 50g/wk.<br />
• Dovonex ® oint discontinued- Generic<br />
ointment only available as 120g tube.<br />
• Apply twice weekly- less when cream<br />
also being used.<br />
• When preparations used together<br />
ensure total weekly dose calcipotriol<br />
is ≤ 5mg<br />
• Well tolerated.<br />
• Can be used on face and flexures<br />
where steroid use is not ideal.<br />
• Not recommended in children<br />
• Apply twice daily<br />
• Treat maximum 35% body surface area<br />
/day<br />
• Use max 30g/day<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-18
Vitamin D Analogue/Steroid Combinations<br />
Preparation Comments<br />
Dovobet ® Ointment: calcipotriol 50<br />
micrograms/g and betamethasone 500<br />
micrograms/g; 60g<br />
• For stable plaque psoriasis<br />
• Apply once daily to max 30% body<br />
surface area for max 4 weeks.<br />
• Alternate with plain calcipotriol.<br />
• Daily max = 15g, weekly max = 100g<br />
• Not recommended in children under<br />
18 yrs<br />
Coal Tar Preparations<br />
Preparation Comments<br />
Exorex ® Lotion: contains:<br />
hydroxybenzoates (parabens), polysorbate<br />
80)<br />
• Prepared coal tar 1%<br />
• Apply to skin or scalp 2-3 times/day<br />
• Dilute with a few drops of water before<br />
applying to children or elderly patients.<br />
Coal Tar Preparations with Corticosteroids<br />
Preparation Comments<br />
Alphosyl HC ® Cream Coal Tar<br />
Extract 5%, Hydrocortisone 0.5%, Allantoin<br />
2%<br />
• For psoriasis in patients over 5 years old<br />
• Apply once or twice daily<br />
• Can be particularly useful for children<br />
• Well tolerated<br />
Dithranol Preparations<br />
Preparation Comments<br />
Dithranol<br />
Micanol ®: 1% or 3% Dithranol Cream<br />
Dithranol in Lassar’s<br />
Paste, BP: usual strengths 0.1-5% of<br />
dithranol<br />
• Apply 1% to skin / scalp for up to 30<br />
minutes. At end of contact time use<br />
plenty of lukewarm (NOT HOT) water to<br />
rinse off. DO NOT USE SOAP<br />
• If necessary increase to 3% under<br />
medical supervision.<br />
• Stains skin and clothing<br />
• Lassar’s Paste – zinc oxide 24%,<br />
salicylic acid 2%, starch 24%, white soft<br />
paraffin 50%<br />
• Stains skin and clothing<br />
• Start at low strength, gradually increase<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-19
Psoralen<br />
Preparation Comments<br />
puvasoralen 8 emulsion<br />
Emulsion 0.15% 50ml<br />
• Used in combination with exposure to<br />
long wave UVA radiation.<br />
• Enhances the effect of irradiation<br />
Oral Preparations for Treating Psoriasis:<br />
For severe resistant psoriasis, oral treatments may be used. These must be initiated and<br />
supervised by a consultant.<br />
Psoralen<br />
Preparation Comments<br />
8-methoxypsoralen<br />
Tablets 10mg<br />
Retinoids<br />
Acitretin<br />
Capsules, 10mg, 25mg<br />
(Neotigason ® )<br />
– hospital pharmacy only<br />
• Used in combination with exposure to<br />
long wave UVA radiation.<br />
• Enhances the effect of irradiation<br />
• Solution used for bath PUVA.<br />
Preparation Comments<br />
• Teratogenic Risk: Female patients<br />
must avoid pregnancy for at least 1<br />
month before, during and for 2 years<br />
after treatment.<br />
• Avoid concomitant use of<br />
methotrexate or tetracyclines or high<br />
doses of vitamin A.<br />
• Avoid concomitant use of<br />
keratiolytics<br />
Psoriasis Treatment: Drugs affecting the immune response<br />
(from BNF section <strong>13</strong>.5.3)<br />
Preparation Comments<br />
Azathioprine<br />
Tablets (25mg and 50mg tablets)<br />
Ciclosporin<br />
Neoral ®<br />
Capsules (25mg,50mg and 100mg<br />
capsules)<br />
Can only be prescribed by<br />
GPs<br />
under Shared Care agreement-<br />
See Chapter 20.<br />
Used for severe refractory psoriasis<br />
(unlicensed indication)<br />
Can only be prescribed by<br />
GPs<br />
under Shared Care<br />
agreement-<br />
See Chapter 20.<br />
Always prescribe as Neoral ® as other<br />
brands are not bioequivalvent.<br />
Used for severe psoriasis unresponsive to<br />
conventional treatments.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-20
Hydroxycarbamide<br />
500mg Capsules<br />
Previously known as hydroxyurea<br />
Methotrexate<br />
2.5mg Tablets<br />
Ustekinumab<br />
90 mg/ml, 0.5-mL (45-mg) vial<br />
Cytokine inhibitors (from BNF section 10.1.3):<br />
Used for severe psoriasis uncontrolled by<br />
other treatments (unlicensed indication)<br />
(Refer to chapter 8 for more information on<br />
prescribing of hydroxycarbamide)<br />
Can only be prescribed by<br />
GPs under Shared Care<br />
agreement- See Chapter 20.<br />
Used for severe psoriasis uncontrolled by<br />
other treatments.<br />
Treatment of moderate to severe plaque<br />
psoriasis in adults who failed to respond to,<br />
or who have a contraindication to, or are<br />
intolerant to other systemic therapies<br />
including ciclosporin, methotrexate and<br />
PUVA<br />
Included as per NICE guideline TAG 180<br />
See below.<br />
Preparation Comments<br />
Etanercept s/c Injection<br />
Infliximab i.v. infusion<br />
Adalimumab s/c<br />
• First choice.<br />
• For systemically unwell patients where<br />
a rapid response is required only.<br />
• Subcutaneous Injection 40mg<br />
Inhibitors of T-Cell Activation:<br />
Preparation Comments<br />
Efalizumab s/c injection<br />
• For patients unresponsive to<br />
etanercept.<br />
N.B. These drugs should only be prescribed for psoriasis by consultant dermatologists and<br />
administered by staff experienced in their use.<br />
Summarised NICE Guidance: Etanercept and efalizumab for the treatment of adults<br />
with psoriasis (TAG 103, July 2006)<br />
1.1 Etanercept, within its licensed indications, administered at a dose not exceeding 25<br />
mg twice weekly is recommended for the treatment of adults with plaque psoriasis only<br />
when the following criteria are met.<br />
The disease is severe as defined by a total Psoriasis Area Severity Index (PASI)<br />
of 10 or more and a Dermatology Life Quality Index (DLQI) of more than 10.<br />
The psoriasis has failed to respond to standard systemic therapies including<br />
ciclosporin, methotrexate and PUVA (psoralen and long-wave ultraviolet<br />
radiation); or the person is intolerant to, or has a contraindication to these<br />
treatments.<br />
1.2 Etanercept treatment should be discontinued in patients whose psoriasis has not<br />
responded adequately at 12 weeks. Further treatment cycles are not recommended in<br />
these patients. An adequate response is defined as either:<br />
a 75% reduction in the PASI score from when treatment started (PASI 75) or<br />
a 50% reduction in the PASI score (PASI 50) and a five-point reduction in DLQI<br />
from when treatment started.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-21
1.3 Efalizumab, within its licensed indications, is recommended for treatment of adults with<br />
plaque psoriasis under the circumstances detailed in section 1.1 only if their psoriasis<br />
has failed to respond to etanercept or they are shown to be intolerant of, or have<br />
contraindications to, treatment with etanercept.<br />
1.4 Further treatment with efalizumab is not recommended in patients unless their<br />
psoriasis has responded adequately at 12 weeks as defined in section 1.2.<br />
1.5 Use of etanercept and efalizumab for psoriasis should be initiated and supervised by a<br />
dermatologist experienced in the diagnosis and treatment of psoriasis. If a person has<br />
psoriasis and psoriatic arthritis their treatment should be managed by collaboration<br />
between a rheumatologist and a dermatologist.<br />
Summarised NICE Guidance: Infliximab for the treatment of adults with psoriasis<br />
(TAG <strong>13</strong>4, January 2008)<br />
1.1 Infliximab, within its licensed indications, is recommended as a treatment option for<br />
adults with plaque psoriasis only when the following criteria are met.<br />
♦ The disease is very severe as defined by a total Psoriasis Area Severity Index<br />
(PASI) of 20 or more and a Dermatology Life Quality Index (DLQI) of more than<br />
18.<br />
♦ The psoriasis has failed to respond to standard systemic therapies such as<br />
ciclosporin, methotrexate or PUVA (psoralen and long-wave ultraviolet radiation),<br />
or the person is intolerant to or has a contraindication to these treatments.<br />
1.2 Infliximab treatment should only be continued beyond 10 weeks in people whose<br />
psoriasis has shown an adequate response to treatment within 10 weeks. An<br />
adequate response is defined as either:<br />
♦ a 75% reduction in the PASI score from when treatment started (PASI 75) or<br />
♦ a 50% reduction in the PASI score (PASI 50) and a five-point reduction in the<br />
DLQI from when treatment started.<br />
1.3 When using the DLQI healthcare professionals should take care to ensure that<br />
they take account of a patient’s disabilities (such as physical impairments) or<br />
linguistic or other communication difficulties, in reaching conclusions on the<br />
severity of plaque psoriasis. In such cases healthcare professionals should<br />
ensure that their use of the DLQI continues to be a sufficiently accurate<br />
measure. The same approach should apply in the context of a decision about<br />
whether to continue the use of the drug.<br />
NICE TAG 146: Adalimumab for the treatment of psoriasis<br />
(July 2008)<br />
Adalimumab is recommended as a possible treatment for adults with plaque psoriasis only<br />
if:<br />
♦ their condition is severe and<br />
♦ their condition has not improved with other treatments such as ciclosporin,<br />
methotrexate and PUVA (psoralen and long-wave ultraviolet radiation), or they have<br />
had side effects with these in the past or there is a medical reason why they should<br />
not be given these treatments.<br />
NICE guidance (TAG 180) Ustekinumab for the treatment of adults with moderate to<br />
severe psoriasis (September 2009)<br />
Ustekinumab is recommended as a possible treatment for people with plaque psoriasis if:<br />
♦ standard assessments show that their psoriasis is severe and is affecting their quality<br />
of life and<br />
♦ their psoriasis has not improved with other treatments such as ciclosporin,<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-22
methotrexate or PUVA (psoralen and long-wave ultraviolet radiation), or they have had<br />
side effects with these treatments in the past or there is a medical reason why they<br />
should not be given them.<br />
<strong>13</strong>.5.3 Drugs affecting the immune response<br />
The drugs relevant to this BNF section have been placed under the skin conditions for<br />
which they are used.<br />
<strong>13</strong>.6 Acne and rosacea<br />
NICE Referral Advice for Acne, December 2001 is provided – Appendix 4<br />
A DETAILED CARE PATHWAY FOR ACNE IS PROVIDED - SEE APPENDIX 8<br />
<strong>13</strong>.6.1 Topical preparations for acne<br />
Notes:<br />
1. Mild acne can generally be treated with topical agents alone.<br />
2. Moderate to severe acne requires the use of both systemic and topical agents.<br />
3. Benzoyl peroxide or topical retinoids are first choice agents for mild comedonal acne.<br />
4. Benzoyl peroxide is the agent of choice for mild inflammatory acne.<br />
Topical benzoyl peroxide and azelaic acid<br />
Preparation Comments<br />
Benzoyl peroxide<br />
PanOxyl ®<br />
Aquagel: 2.5%, 5%, 10% (contains:<br />
propylene glycol)<br />
Cream: 5% (contains: isopropyl palmitate,<br />
propylene glycol)<br />
Gel: 5%, 10% (contains: fragrance)<br />
Wash: 10% (contains: imidurea)<br />
Azelaic acid<br />
Skinoren ® cream, 20% (contains:<br />
proplyene glycol<br />
Topical antibiotics for acne<br />
DO NOT use topical and systemic antibiotics at the same time.<br />
• Effective in mild to moderate acne.<br />
• Comedones and inflamed lesions<br />
respond well.<br />
• Start with a low strength increase<br />
gradually.<br />
• May bleach clothing and bed covers.<br />
• If no response after 2 months then<br />
consider a topical antibiotic.<br />
• A possible alternative to benzoyl<br />
peroxide where skin irritation is a<br />
problem.<br />
• If no response after 2 months then<br />
consider using a topical antibiotic.<br />
Preparation Comments<br />
Zineryt ®<br />
Erythromycin 40mg/ml<br />
Topical solution, powder for reconstitution<br />
Clindamycin 1%<br />
Topical solution (alcoholic basis)<br />
(contains: propylene glycol) Lotion<br />
(aqueous basis) (contains: cetostearyl<br />
alcohol, hydroxybenzoates (parabens))<br />
• Lasts 5 weeks once reconstituted.<br />
For most cases 30ml should be prescribed.<br />
Only prescribe 90ml if treatment area is<br />
very large.<br />
• Lotion is less drying.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-23
Topical retinoids and related preparations for acne<br />
• Redness and skin peeling may occur for several days, but usually settles with time.<br />
• Acne may worsen for the first few weeks.<br />
• Several months treatment may be needed- use until no new lesions appear.<br />
• Advise to avoid ultraviolet lamps and minimise exposure to sunlight.<br />
• Advise to allow peeling (e.g. from benzoyl peroxide) to subside before using a topical<br />
retinoid.<br />
• Avoid concomitant use of abrasive cleaners or astringent cosmetics.<br />
• Topical retinoids must not be used in pregnancy.<br />
• WOMEN OF CHILDBEARING AGE MUST USE ADEQUATE CONTRACEPTION<br />
WHILE USING A RETINOID.<br />
• DO NOT USE ON SEVERE ACNE COVERING LARGE AREAS.<br />
Tretinoin<br />
Retin-A ®<br />
Cream, 0.025%<br />
Gel, 0.01%, 0.025%<br />
Preparation Comments<br />
Isotretinoin<br />
Isotrex ®<br />
Gel, 0.05% (contains: butylated<br />
hydroxytoluene)<br />
• Licensed for acne vulgaris.<br />
• Apply thinly once or twice a day.<br />
• Cream better for dry or fair skin.<br />
• Cream contains: butylated<br />
hydroxytoluene, sorbic acid, stearyl<br />
alcohol<br />
• Gel contains: butylated hydroxytoluene<br />
• Licensed for mild to moderate acne.<br />
• Can sometimes be better tolerated than<br />
Retin-A ® .<br />
• Apply thinly once or twice a day.<br />
Other topical preparations for acne<br />
Notes:<br />
1. The BNF states that these products are considered less suitable for prescribing.<br />
2. Salicylic acid is available for sale to the public for the treatment of mild acne.<br />
3. Preparations containing sulphur and abrasive agents are not considered beneficial for<br />
acne.<br />
<strong>13</strong>.6.2 Oral preparations for acne<br />
Oral antibiotics for acne<br />
Notes:<br />
1. An adequate dose of an oral antibiotic should be given for at least 3 months before<br />
deciding a patient has failed to respond.<br />
2. Treatment should not be used for longer than necessary (usually between 6 and 12<br />
months).<br />
3. If acne returns, reuse the same drug if the previous response was satisfactory with<br />
that agent.<br />
DO NOT use topical and systemic antibiotics at the same time.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-24
Oxytetracycline<br />
Tablets<br />
Lymecycline<br />
Capsules<br />
Erythromycin<br />
Tablets<br />
Trimethoprim<br />
Tablets<br />
Minocycline<br />
Tablets<br />
Preparation Comments<br />
• 500mg twice a day<br />
• 408mg daily<br />
• 500mg twice a day<br />
• Reserved for situations where other<br />
antibiotics are unsuitable.<br />
• Proprionibacterial resistance to this<br />
drug is quite common.<br />
• 300mg BD<br />
• For consultant initiation.<br />
• Sometimes useful for resistant acne<br />
• 3 rd Line Treatment.<br />
• If given for > 6months monitor for<br />
hepatotoxicity, unusual skin pigmentation<br />
and SLE. Discontinue if these develop.<br />
Hormone Treatment for acne<br />
Preparation Comments<br />
Co-cyprindiol<br />
tablets<br />
• Cheaper to prescribe generically<br />
rather than as Dianette ® .<br />
• Licensed for women with severe acne<br />
unresponsive to oral antibiotics, or<br />
moderately severe hirsutism. .<br />
• If prescribed as a contraceptive as well<br />
as for acne, mark the prescription “♀”<br />
otherwise a prescription charge must be<br />
paid by the patient<br />
It is vital that patients taking co-cyprindiol are regularly reviewed to ensure that it is still<br />
appropriate for the patient.<br />
CSM Advice<br />
1. Co-cyprindiol is not licensed solely for contraceptive purposes .<br />
2. Withdraw co-cyprindiol 3 to 4 cycles after the treated condition has resolved.<br />
3. VTE incidence in co-cyprindiol users is higher than that in women who use low-dose<br />
oestrogens combined oral contraceptives.<br />
4. Co-cyprindiol is contra-indicated in women with a personal or close family history of<br />
confirmed, idiopathic VTE and in those with known current venous thrombotic or<br />
embolic disorders.<br />
5. Women who have severe acne or hirsutism may have an inherently increased<br />
cardiovascular risk.<br />
N.B. Always counsel patients when prescribing co-cyprindiol, as with other oral<br />
contraceptives. Please refer to Chapter 7.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-25
Oral Retinoids for acne<br />
Preparation Comments<br />
Isotretinoin<br />
Capsules 5mg, 20mg<br />
• Should only be prescribed by, or under<br />
the supervision of a consultant<br />
dermatologist.<br />
• Usually given for a minimum of 16<br />
weeks; repeat courses are not normally<br />
required.<br />
• Do not take vitamin preparations<br />
containing more than 4000-5000 i.u. of<br />
vitamin A.<br />
• Teratogenic Risk: Female patients must<br />
avoid pregnancy for at least 1 month<br />
before, during and for 2 months after<br />
treatment.<br />
• Side effects: severe dryness of skin and<br />
mucous membranes, nosebleeds and<br />
joint pains.<br />
<strong>13</strong>.7 Preparations for warts and calluses<br />
Preparation Comments<br />
Salicylic acid Salactol ®<br />
Paint; 16.7% salicylic acid, 16.7% lactic acid<br />
Podophyllum<br />
Podophyllin Paint,<br />
Compound, BP<br />
Podophyllotoxin<br />
Warticon ® 0.15% Cream 5g<br />
Podophyllotoxin<br />
Warticon ® 0.5% Solution 3ml<br />
• For treatment of viral warts and verrucae<br />
on hands and feet.<br />
• Many products are available for<br />
purchase OTC.<br />
• For external genital warts<br />
• Applied weekly at genitourinary clinic (or<br />
at GP surgery by a trained nurse).<br />
• For self treatment of external genital<br />
warts in females.<br />
• Apply twice daily for 3 days followed by a<br />
4 day break. Repeat for maximum 4<br />
treatments.<br />
• For self treatment of external genital<br />
warts in females.<br />
• Apply twice daily for 3 days followed by a<br />
4 day break. Repeat for maximum 4<br />
treatments.<br />
Cryotherapy is not appropriate for viral warts on the hands and feet. There is evidence for<br />
a lack of efficacy in hand warts, it is painful, can cause significant scarring and may<br />
exacerbate the warts. Surgical treatment is also inappropriate for these lesions.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-26
<strong>13</strong>.8 Sunscreens and camouflagers<br />
<strong>13</strong>.8.1 Sunscreening preparations<br />
Can only be prescribed for the following indications (endorsed ACBS) for:<br />
• Skin protection against ultraviolet radiation in abnormal cutaneous photosensitivity<br />
resulting from genetic disorders;<br />
• Photodermatoses, including vitiligo and those resulting from radiotherapy;<br />
• Chronic or recurrent herpes simplex labialis.<br />
Preparation Comments<br />
E45 Sun Block SPF30+ ®<br />
ACBS lotion<br />
Sunsense ® Sunblock<br />
ACBS<br />
• Tends to leave a white sheen on the<br />
skin.<br />
SPF 30+ (contains<br />
hydroxybenzoates (parabens),<br />
isopropyl palmitate)<br />
• Doesn’t leave a white sheen on the skin.<br />
Preparations to treat photodamage<br />
A DETAILED CARE PATHWAY FOR SUN DAMAGED <strong>SKIN</strong> LESIONS IS PROVIDED -<br />
APPENDIX 9<br />
Preparation Comments<br />
Fluorouracil (Efudix ® )<br />
5% Cream<br />
Solaraze ® Gel<br />
Diclofenac sodium 3% in sodium<br />
hyaluronate basis. (contains: benzyl alcohol)<br />
• See care pathway - Appendix 9<br />
• First choice for actinic keratosis because<br />
of stronger evidence base and likely to be<br />
cost effective.<br />
• Apply thinly to affected area once or twice<br />
daily. Cover with occlusive dressing in<br />
malignant conditions.<br />
• Max area of skin to be treated at one time<br />
is 500cm 2<br />
• Usual duration of initial therapy = 3-4<br />
weeks.<br />
• Produces a more marked inflammatory<br />
reaction than with diclofenac but lesions<br />
resolve more quickly.<br />
• See care pathway - Appendix 9<br />
• For actinic keratosis.<br />
• For use where fluorouracil is<br />
contraindicated, poorly tolerated or large<br />
areas need treatment. Can be particularly<br />
useful for superficial lesions but evidence<br />
not as robust as for fluorouracil.<br />
• Apply thinly twice daily for 60-90 days.<br />
Max 8g daily.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-27
Preparations to treat Basal Cell Carinoma and Bowens Disease<br />
Preparation Comments<br />
Imiquimod<br />
Aldara ®<br />
5 % Cream<br />
• For superficial BCC when surgery or<br />
cryotherapy is contra-indicated.<br />
• Apply to the lesion and 1cm beyond it for<br />
5 days each week for a total of 6 weeks.<br />
Response should be assessed after a<br />
further 12 weeks.<br />
• Leave on BCC for 8 hours then wash off<br />
with mild soap and water.<br />
• Also used for Bowens Disease.<br />
<strong>13</strong>.9 Shampoos and preparations for scalp and hair conditions<br />
Preparation Comments<br />
Polytar Plus ®<br />
Liquid (contains: fragrance, imidurea,<br />
polysorbate 80, peanut oil)<br />
Capasal ®<br />
Shampoo; coal tar 1%, coconut oil 1%,<br />
salicylic acid 0.5%<br />
Ceanel ® Concentrate<br />
Shampoo; cetrimide 10%, undecenoic acid<br />
1%, phenylethyl alcohol 7.5%<br />
Ketoconazole<br />
Shampoo; 2% (contains: imidurea)<br />
Cocois ®<br />
Scalp ointment; coal tar solution 12%,<br />
salicylic acid 2%, precipitated sulphur 4% in<br />
a coconut emollient basis (contains:<br />
cetostearyl alcohol)<br />
• For scalp disorders including psoriasis,<br />
seborrhoea, eczema, pruritis and<br />
dandruff.<br />
• Use once or twice weekly<br />
• For scaly scalp disorders including<br />
psoriasis, seborrheic dermatitis, dandruff<br />
and cradle cap.<br />
• Use daily as necessary.<br />
• For scalp psoriasis, seborrheic<br />
dermatitis and dandruff.<br />
• Apply three times in the first week then<br />
twice weekly.<br />
• Useful for seborrheic dermatitis.<br />
• Available for sale OTC to the public for<br />
seborrheic dermatitis of the scalp and<br />
dandruff<br />
• Used to treat pityriasis versicolor – if<br />
extensive or resistant may need oral<br />
antifungal (See Chapter 5)<br />
• Used for scalp psoriasis<br />
• Rub in, leave for 2 hours then comb out<br />
to remove loose scales, then shampoo<br />
out with Capasal® shampoo<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-28
<strong>13</strong>.10 Anti-infective skin preparations<br />
<strong>13</strong>.10.1 Antibacterial preparations<br />
<strong>13</strong>.10.1.1 Antibacterial preparations only used topically<br />
SMAC Report: Topical antimicrobial agents and disinfectants (1998, The Path of<br />
Least resistance p64 – p65)<br />
The use of topical antimicrobial agents has long been discouraged, on the grounds that<br />
it carries a particular risk of selecting resistance. However, some topical antibacterial use is<br />
strongly defensible, for example:<br />
• the use of sulphonamides with silver nitrate (silver sulphadiazine) to prevent and<br />
treat infections in extensive burns<br />
• The use of mupirocin to eliminate colonisation and superficial infections caused by<br />
MRSA. Nevertheless, mupirocin can be abused, e.g. by being given as blanket<br />
treatment or prophylaxis.<br />
Preparation Comment<br />
Silver Sulphadiazine<br />
Flamazine ®<br />
Cream, 1% 20g, 50g, 250g, 500g<br />
Mupirocin<br />
Bactroban ®<br />
Ointment or cream, 2%<br />
and nasal cream<br />
Chlorhexidine 0.1% with<br />
Neomycin 0.5%<br />
Naseptin ®<br />
Nasal cream,<br />
(contains: arachis oil and cetostearyl<br />
alchohol)<br />
• Prescribe for single patient use only.<br />
• Use only for burns.<br />
• Prevents Gram negative sepsis in<br />
extensive burns patients<br />
• Caution with hepatic/ renal impairment.<br />
• Apply daily and cover area with dressing.<br />
• Discard tube (20g/50g) 7 days after<br />
opening.<br />
Discard jars (250g/500g) 24hrs after<br />
opening.<br />
• Useful in treating MRSA<br />
• Only use if organism is mupirocin<br />
sensitive and recommended by<br />
Infection Control or Microbiology to<br />
avoid resistance developing.<br />
• Ointment used for skin infections.<br />
• Cream is used for secondarily<br />
infected traumatic lesions.<br />
• Use for no longer than 10 days.<br />
Bactroban ® nasal ointment is of value when<br />
the carriage of Staphlococcus aureus in the<br />
nose or ears has to be cleared. See<br />
chapter 12.2.3.<br />
• Naseptin® is of value when the carriage<br />
of Staphlococcus aureus in the nose has<br />
to be cleared. See chapter 12.2.3.<br />
• SDHCFT infection control policy<br />
states that this should ONLY be used<br />
on advice from microbiology.<br />
• Use four times a day for 5 days then reswab<br />
3 days after completing treatment.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-29
<strong>13</strong>.10.1.2 Antibacterial preparations also used systemically<br />
Preparation Comment<br />
Fusidic acid<br />
Ointment, 2% (contains: cetyl alcohol,<br />
wool fat)<br />
Cream, 2% (contains: butylated<br />
hydroxyanisole, cetyl alcohol)<br />
Metronidazole<br />
Rozex ®<br />
cream or gel, 0.75% (cream contains:<br />
benzyl alcohol, isopropyl palmitate gel<br />
contains: disodium edetate,<br />
hydroxybenzoates (parabens), propylene<br />
glycol)<br />
Metronidazole<br />
Metrotop ® gel 0.8%<br />
Only use for PROVEN staphylococcal<br />
skin infection.<br />
• Licensed for acne rosacea<br />
• Licensed for malodorous tumours and<br />
skin ulcers.<br />
<strong>13</strong>.10.2 Antifungal preparations<br />
Yeast infections<br />
Notes:<br />
1. Obtain a positive culture before prescribing a topical antifungal. Hair, nail<br />
clippings or scalp scrapings can be used to determine the presence of fungal infection.<br />
There is no urgency in diagnosing fungal infections.<br />
2. Oncomycosis should only be treated orally if there is a positive culture. If positive<br />
for microscopy but negative for culture, TAKE A FURTHER SPECIMEN. Please see<br />
Chapter 5.<br />
Preparation Comment<br />
Clotrimazole Cream 1%<br />
Canesten ® spray, 1% in isopropyl<br />
alcohol (contains: propylene glycol<br />
Miconazole nitrate<br />
Daktarin ®<br />
Cream 2% (contains: butylated<br />
hydroxyanisole)<br />
• Spray included for treatment of pityriasis<br />
versicolor.<br />
• Spray also for chronic paronychia, which<br />
is associated with a secondary infection<br />
of Candida albicans.<br />
• Apply twice a day continuing for 10<br />
days after lesions have healed<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-30
Dermatophyte infections<br />
Preparation Comment<br />
Ketoconazole (Nizoral ® )<br />
SLS<br />
Cream 2% (contains: cetyl alcohol,<br />
polysorbates, propylene glycol, stearyl<br />
alcohol)<br />
Terbinafine<br />
Cream 1% (contains: benzyl alcohol, cetyl<br />
alcohol, polysorbate 60, stearyl alcohol)<br />
• Can only prescribe for seborrhoeic<br />
dermatitis or pityriasis versicolor. FP10<br />
prescriptions - must be endorsed “SLS”.<br />
• For tinea corporis. Fungal infection of<br />
the scalp, hands and feet often require<br />
systemic treatment.<br />
<strong>13</strong>.10.3 Antiviral preparations<br />
Preparation Comment<br />
Aciclovir<br />
Cream 5% 2g, 10 g<br />
(excipients may differ depending on generic<br />
or proprietary preparation)<br />
<strong>13</strong>.10.4 Parasiticidal preparations<br />
Suitable quantities of parasiticidal preparations<br />
• Licensed for initial and recurrent labial<br />
and genital herpes simplex infection.<br />
• Must begin using early during ‘tingling<br />
phase’ and a supply kept to hand for<br />
repeat breakouts.<br />
• Once a lesion appears, aciclovir is little<br />
more effective than a base cream.<br />
• Systemic treatment is needed for buccal<br />
or vaginal infections. See Chapter 5<br />
Skin creams Lotions Cream rinses<br />
Scalp (head lice) - 50-100ml 50-100ml<br />
Body (scabies) 30-60g 100ml -<br />
Body (crab lice) 30-60g 100ml -<br />
These amounts are usually suitable for an adult for single application.<br />
Scabies (Sarcoptes scabiei)<br />
• Once diagnosed, close household contacts (bed partners and children) also require<br />
treatment. It requires about 5 minutes skin to skin contact to acquire the infection.<br />
• Patients are contagious from a few days after acquiring the infection when no sign of the<br />
infection may be present.<br />
• Itching, particularly at night, is the main symptom of scabies. This is usually delayed for<br />
1-2 months after exposure except when the patient has been exposed before, in which<br />
case itching can start after 1 week.<br />
• Itching still occurs after treatment and this does not always imply treatment failure.<br />
Scabies Treatment: permethrin (Lyclear® Dermal Cream); malathion (Derbac M®)<br />
• Apply treatment before going to bed and leave on overnight.<br />
• Reapply to hands if they are washed and at least 4-6 times a day on the day of<br />
treatment.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-31
• In adults - apply treatment to cover the body from below the jaw line down and including<br />
the soles of feet and genitalia.<br />
• In elderly and young patients - apply from the head to toe.<br />
• Treat all household members at the same time.<br />
• Second application less than one week apart advised.<br />
N.B. Crusted or Norwegian scabies, affecting mainly immunosuppressed patients<br />
and nursing / residential home patients are more difficult to treat and require more<br />
applications of treatment. Seek advice from the Consultant in Communicable<br />
Diseases - mass treatment of staff and residents will be needed in a care home<br />
setting.<br />
Head lice (Pediculus capitis)<br />
• Lice eggs hatch within 7-10 days. The empty egg cases (nits) move further along the<br />
hair shaft as the hair grows out.<br />
• Lice take about 6-14 days to fully mature, then they are capable of reproduction.<br />
Head Lice Treatment: malathion (Quellada M ® ); permethrin (Lyclear ® Crème Rinse);<br />
phenothrin (Full Marks ® liquid)<br />
Treatment should only be considered when live lice are observed on the scalp.<br />
Treatment options:<br />
1) Wet combing every 3 days for 2 weeks<br />
2) Insecticide – 2 applications used 7 days apart to prevent lice re-emerging from any<br />
eggs that survive the first application. (Alternatively, wet combing can be used to check<br />
for immature lice before re-application at 3-5 and 10-12 days.)<br />
To overcome the development of resistance, if a course of treatment fails to cure, a<br />
different insecticide should be used for the next course.<br />
The value of head lice repellents and alternative remedies, which are on sale to the public,<br />
is uncertain and, therefore, NOT recommended.<br />
Crab lice (Pthirus pubis)<br />
Treatment: malathion (Quellada M ®) ; permethrin (Lyclear ® Dermal Cream)<br />
Crab lice (or pubic lice) can exist in eyelashes, beard hair, axillary hair and the hair on the<br />
trunk and limbs, as well as pubic hair.<br />
Preparation<br />
Malathion Quellada M ® liquid, 0.5% in an aqueous basis (contains:<br />
cetostearyl alcohol, fragrance, hydroxybenzoates (parabens)<br />
Derbac M ® liquid, 0.5% in an aqueous basis (contains: cetostearyl alcohol,<br />
fragrance, hydroxybenzoates (parabens)<br />
Permethrin<br />
Lyclear ®<br />
Crème Rinse, 1% in isopropyl alcohol base (contains: cetyl alcohol)<br />
Dermal Cream, 5% (contains: butylated hydroxytoluene, wool fat derivative)<br />
Phenothrin<br />
Full Marks ® liquid, 0.5% in aqueous basis (contains: cetostearyl alcohol, fragrance,<br />
hydroxybenzoates (parabens)<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-32
Notes:<br />
1. Benzyl benzoate is not considered suitable for prescribing. It is an irritant and is less<br />
effective than malathion and permethrin in treating scabies.<br />
2. Experimental data in animals suggests that carbaryl could be a potential human<br />
carcinogen and is not included.<br />
3. Alcoholic lotions are not recommended for head lice in severe eczema, asthma or in<br />
small children, or for scabies or crab lice<br />
<strong>13</strong>.10.5 Preparations for minor cuts and abrasions<br />
Preparation Comment<br />
Flexible collodion<br />
• May be used to seal partially healed<br />
minor cuts and wounds.<br />
• Can cause a lot of irritation.<br />
Surgical tissue adhesive<br />
Note: The range of surgical tissue adhesives required to cover the increasing spectrum of<br />
uses is considered beyond the scope of this formulary.<br />
<strong>13</strong>.11 Skin cleansers and antiseptics<br />
See chapter 5 (appendix 3) for details of MRSA screening, decolonisation and<br />
treatment protocols.<br />
<strong>13</strong>.11.1 Alcohols and saline<br />
Preparation Comment<br />
Industrial methylated spirit<br />
Surgical spirit<br />
Sodium chloride 0.9%<br />
Normasol ®<br />
Irriclens ®<br />
• Drinking water can be used to irrigate the<br />
majority of wounds such as a chronic leg<br />
ulcer where a sterile product is not<br />
indicated.<br />
<strong>13</strong>.11.2 Chlorhexidine salts<br />
Preparation Comment<br />
Hydrex ®<br />
Surgical Scrub, chlorhexidine gluconate 4%<br />
in an alcoholic solution<br />
• Used for pre-op hand and skin<br />
preparation and for general hand<br />
disinfection.<br />
• Chlorhexidine use not recommended in<br />
the community.<br />
CX powder ® • For use as a dusting powder to,<br />
perineum, groin and axillae as per MRSA<br />
decolonisation policy.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-33
<strong>13</strong>.11.4 Iodine<br />
Preparation Comment<br />
Videne ®<br />
Antiseptic solution (Videne ® has replaced<br />
Betadine ® aqueous solution which has been<br />
discontinued)<br />
• Chlorinated solutions are considered less<br />
suitable for prescribing<br />
• Avoid regular use on patients with thyroid<br />
disease or those receiving lithium<br />
therapy.<br />
• It may also interfere with thyroid function<br />
tests.<br />
<strong>13</strong>.11.5 Phenolics<br />
Preparation Comment<br />
Triclosan<br />
Aquasept ® (contains: chlorocresol,<br />
edetic acid (EDTA), propylene glycol,<br />
fragrance)<br />
• At the time of writing this formulary<br />
Aquasept® was not available in the<br />
community and so cannot be prescribed<br />
on a FP10 prescription. Please refer any<br />
requests to the Hospital pharmacy<br />
Department.<br />
<strong>13</strong>.11.6 Astringents, oxidisers and dyes<br />
Preparation Comment<br />
Potassium permanganate<br />
Permitabs ®<br />
• Use a dilution of 1:10,000.<br />
• Soaks useful for pompholyx eczema and<br />
weeping leg ulcers.<br />
<strong>13</strong>.11.7 Preparations for promotion of wound healing<br />
Appropriate wound management requires the underlying cause to be treated rather than to<br />
use preparations to promote wound healing. Therefore, none of these agents have been<br />
included. See Chapter 17 – Wound management.<br />
<strong>13</strong>.12 Antiperspirants<br />
Preparation Comment<br />
Aluminium salts<br />
Anhydrol Forte ®<br />
Driclor ®<br />
ZeaSORB ® dusting powder (contains:<br />
fragrance)<br />
Botulinum Clostridium<br />
Type A<br />
Botox ®<br />
• Aluminium chloride is a potent<br />
antiperspirant for severe hyperhidrosis.<br />
• Irritation reduced if applied to completely<br />
dry skin. i.e. apply with a hairdryer<br />
directed at the axillae or palms.<br />
• Included for severe hyperhidrosis of the<br />
axillae which does not respond to topical<br />
treatment with antiperspirants or<br />
antihidrotics.<br />
Note: Propantheline bromide is included in chapter 1.2 for use in accordance only with the<br />
local Map of Medicine pathway on dermatological treatments for local hyperhidrosis.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-34
<strong>13</strong>.<strong>13</strong> Wound management products and elastic hosiery<br />
Please refer to Chapter 17 Wound Management<br />
<strong>13</strong>.14 Others<br />
Pure Lanolin<br />
(Lansinoh ® )<br />
10g, 56g ointment<br />
Preparation Comment<br />
• used by midwives to treat sore and<br />
cracked nipples.<br />
Lansinoh® may be obtained from several of the pharmacy wholesalers or direct from:<br />
Lansinoh Laboratories,<br />
First Floor,<br />
Alexandra House,<br />
Well Lane,<br />
Chapel Allerton,<br />
Leeds<br />
LS7 4PQ<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-35
Appendix 1: The Dermatology Referral Process<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-36
Appendix 2<br />
Excipients that may cause sensitisation<br />
The following excipients in topical preparations may rarely be associated with sensitisation.<br />
Throughout this formulary, the presence of these excipients in products is indicated to aid<br />
product selection.<br />
Beeswax Benzyl alcohol Butylated hydroxyanisole<br />
Butylated hydroxytoluene Cetostearyl alcohol<br />
(including cetyl and stearyl<br />
alcohol)<br />
Edetic acid (EDTA)<br />
Hydroxybenzoates<br />
(parabens)<br />
N-(3-Chloroallyl)<br />
hexaminium chloride<br />
(quaternium 15)<br />
Chlorocresol<br />
Ethylenediamine Fragrances<br />
Imidurea Isopropyl palmitate<br />
Polysorbates Propylene glycol<br />
Sodium metabisulphite Sorbic acid Wool fat and related<br />
substances incl. lanolin 1<br />
1.<br />
Purified versions of wool fat have reduced the problem<br />
It is difficult to ‘rank’ these agents in order of their potential to cause sensitisation<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-37
Appendix 3: Urticaria Care Pathway<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-38
Appendix 4<br />
NICE Referral Advice for Atopic Eczema in Children, December 2001<br />
Most children with atopic eczema can be managed in primary care. Referral to a specialist<br />
service, which may be prompted by features such as sleep disturbance and school<br />
absenteeism, is advised if:<br />
**** infection with disseminated herpes simplex (eczema herpeticum) is suspected<br />
*** the disease is severe and has not responded to appropriate therapy in primary<br />
care<br />
*** the rash becomes infected with bacteria (manifest as weeping, crusting, or<br />
development of pustules), and treatment with an oral antibiotic plus a topical<br />
corticosteroid has failed<br />
** the rash is giving rise to severe social or psychological problems<br />
** treatment requires the use of excessive amounts of potent topical corticosteroids<br />
* management in primary care has not controlled the rash satisfactorily. Utimately,<br />
failure to improve is probably best based upon subjective assessment by the<br />
child or parent<br />
* the patient or family might benefit from additional advice on application of<br />
treatments (e.g. bandaging techniques)<br />
* contact dermatitis is suspected and confirmation requires patch testing (this is<br />
rarely needed)<br />
* the child has uncontrolled eczema and dietary factors are suspected (refer<br />
directly to dietician)<br />
Key to referral timings: Arrangements should be made so that the patient:<br />
**** is seen immediately 1<br />
*** is seen urgently 2<br />
** is seen soon 2<br />
* has a routine appointment 2<br />
∆ is seen within an appropriate time depending on his or her clinical circumstances<br />
(discretionary)<br />
1. Within a day.<br />
2. Health authorities, trusts and primary care organisations should work to local<br />
definitions of maximum waiting times in each of these categories. The multidisciplinary<br />
advisory groups considered a maximum waiting time of 2 weeks to be appropriate for<br />
the urgent category.<br />
The adoption of this system should take place in the context of local strategies for<br />
achieving outpatient waiting times and inpatient waiting list targets.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-39
Appendix 4 (continued)<br />
NICE Referral Advice for Psoriasis, December 2001<br />
Most patients with psoriasis can be managed in primary care. Referral to specialist<br />
services, which may be prompted by features such as sleep disturbance, social exclusion,<br />
reduced quality of life or reduced self-esteem, is advised if:<br />
**** the patient has generalised pustular or erythrodermic psoriasis<br />
*** the patient’s psoriasis is acutely unstable<br />
*** the patient has widespread guttate psoriasis (so that he/she can benefit from<br />
early phototherapy)<br />
** the condition is causing severe social or psychological problems<br />
** the rash is sufficiently extensive to make self-management impractical<br />
** the rash is in a sensitive area (such as face, hands, feet, genitalia) and the<br />
symptoms particularly troublesome<br />
** the rash is leading to time off work or school which is interfering with employment<br />
or education<br />
** the patient requires assessment for the management of associated arthropathy<br />
* the rash fails to respond to management in general practice. Failure is probably<br />
best based on the subjective assessment of the patient. Sometimes failure<br />
occurs when patients are unable to apply the treatment themselves<br />
Refer to Atopic Eczema table for key to referral timing<br />
NICE Referral Advice for Acne, December 2001<br />
Most patients with acne can be managed in primary care. However, referral to a specilaist<br />
service is advised if they:<br />
*** have a very severe variant such as fulminating acne with systemic symptoms<br />
(acne fulminans)<br />
** have severe acne or painful, deep nodules or cysts (nodulocystic acne) and could<br />
benefit from oral isotretinoin<br />
** have severe social or psychological problems, including a morbid fear of<br />
deformity (dysmorphophobia)<br />
* are at risk of, or are developing, scarring despite primary care therapies<br />
* have moderate acne that has failed to respond to treatment which should<br />
generally include several courses of both topical and systemic treatment over a<br />
period of at least 6 months. Failure is probably best based upon a subjective<br />
assessment by the patient<br />
* are suspected of having an underlying endocrinological cause for the acne (such<br />
as polycystic ovary syndrome) that needs assessment<br />
Refer to Atopic Eczema table for key to referral timing<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-40
Appendix 5: Care pathway for Atopic Eczema<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-41
Appendix 6<br />
Detailed Instructions on The Use of Topical Tacrolimus and<br />
Pimecrolimus.<br />
Before commencing treatment the following MUST be discussed with every patient:<br />
1. There have been rare reports of lymphoma, skin cancers and other malignancies<br />
in a small number of patients using topical tacrolimus and pimecrolimus.<br />
• A link can’t be confirmed or refuted based on evidence so far.<br />
• The EMEA concluded that the benefits still outweigh the risks.<br />
• Skin exposure to sunlight should be minimised and the use of ultraviolet (UV) light<br />
from a solarium. Appropriate sun protection methods should be used.<br />
• UVB or UVA therapy combined with psoralens (PUVA) should be avoided during<br />
treatment with tacrolimus ointment.<br />
2. The effect of treatment on the developing immune system of children, especially<br />
the young, has not been established.<br />
3. Treatment may be associated with increased risk of herpes simplex virus<br />
infection (including herpes, cold sores and eczema herpeticum [Kaposi’s varicelliform<br />
eruption)<br />
4. Stinging and burning may occur when applied<br />
5. There is a risk of vaccination failure while using these products:<br />
• Vaccination should be administered prior to commencement of treatment or<br />
during a treatment-free interval.<br />
• Allow 14 days between the last application of the product and the vaccination.<br />
• Allow 28 days for live, attenuated vaccine.<br />
6. These products MUST NOT be used in the following circumstances:<br />
• In the presence of infection.<br />
• In immunocompromised patients.<br />
• On cancerous or pre-cancerous lesions.<br />
7. Tacrolimus or pimecrolimus should be stopped in the event of poor toleration,<br />
lack of efficacy or the development of infection.<br />
Experience of dermatologists:<br />
♦ Tacrolimus has been found to be generally well tolerated.<br />
♦ In practice tacrolimus ointment has been found to be useful in severe eczema<br />
particularly for those where ciclosporin is being considered.<br />
♦ Facial eczema (including eyelid eczema) and flexural eczema previously unresponsive<br />
to topical corticosteroids appears to respond very well to tacrolimus ointment.<br />
Appendix 6 (continued)<br />
Detailed Instructions on The Use of Topical Tacrolimus and<br />
Pimecrolimus<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-42
Tacrolimus Ointment Usage instructions<br />
• Avoid using on thickened, lichenified eczema where penetration seems to be poor.<br />
• It may be used on any part of the body, including face, neck and flexure areas, except<br />
on mucous membranes.<br />
• Affected regions should be treated until clearance occurs and then treatment should<br />
be discontinued.<br />
• Generally improvement is seen within one week of starting tacrolimus. If no<br />
improvement is seen after two weeks treatment the diagnosis should be re-evaluated<br />
and alternative options considered.<br />
• Tacrolimus ointment can be used for short term and intermittent long term treatment.<br />
• Do not apply tacrolimus at the same time as other topical preparations (e.g.<br />
emollients, sun screens) which should be applied 2 hours or more afterwards.<br />
• If a patient has lymphadenopathy (enlarged lymph nodes or ‘glands’) at the start of<br />
treatment, the doctor should investigate it and keep it under review.<br />
Dosage instructions<br />
Adults (16 years of age and above)<br />
• Start with tacrolimus ointment 0.1% - apply a thin layer twice daily for up to 3 weeks.<br />
• Then reduce to tacrolimus ointment 0.03% twice daily.<br />
• Attempt to reduce the frequency of application if the condition allows.<br />
• Treatment should be continued until clearance of the lesion.<br />
Children (2 years of age and above)<br />
• Start with tacrolimus ointment 0.03% twice daily for up to 3 weeks.<br />
• Reduce frequency of application to once a day until clearance of lesion.<br />
Pimecrolimus Cream Usage instructions<br />
• Pimecrolimus should only be used in patients who cannot tolerate the side effects<br />
from tacrolimus.<br />
• Do not apply under occlusion.<br />
• It may only be used on the face and neck.<br />
• If no improvement is seen after 6 weeks, or in case of disease exacerbation,<br />
treatment should be stopped and further options considered.<br />
• It may be used for intermittent long term treatment.<br />
• Emollients may be applied immediately after using pimecrolimus.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-43
Appendix 7: Psoriasis Care Pathway<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-44
Appendix 8: Acne Care Pathway<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-45
Appendix 9: Sun Damaged Skin Pathway<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-46
Appendix 10: Fire Hazard with Paraffin Based Skin Products on<br />
Dressings and Clothing<br />
NPSA Alert 4: Fire Hazard with Paraffin Based Skin Products on Dressings and<br />
Clothing<br />
On 26/11/2007 the National Patient Safety Agency (NPSA) alerted all healthcare staff<br />
involved in the prescribing, dispensing or administration of paraffin based skin products of<br />
a potential fire hazard. Bandages, dressings and clothing in contact with paraffin based<br />
products, for example White Soft Paraffin, White Soft Paraffin plus 50% Liquid Paraffin or<br />
Emulsifying ointment are easily ignited with a naked flame or cigarette.<br />
Further information and supporting materials (poster, patient information leaflet and videos<br />
of fire hazard testing) concerning are available at: www.npsa.nhs.uk/health/alerts<br />
The NPSA has directed the <strong>NHS</strong> to undertake the following actions for all patients in all<br />
settings being dispensed, or treated with, large quantities (100g or more) of paraffin based<br />
products:<br />
• Information should be given about the potential fire risks of smoking (or being near to<br />
people who are smoking), or exposure to any open flame or other potential cause of<br />
ignition during treatment; and about regularly changing clothing or bedding impregnated<br />
with paraffin based products (preferably on a daily basis) as the paraffin soaks into the<br />
fabrics and can potentially be a fire hazard.<br />
• This information should be given on the first occasion that such treatment is prescribed,<br />
dispensed or administered by a healthcare professional and a record kept confirming<br />
that such advice has been given. A check should be made on subsequent occasions<br />
that the advice has been received previously and understood.<br />
• Fire safety information should be displayed prominently in every clinical area where<br />
patients may be treated with large quantities of paraffin based products. If, against<br />
advice, a hospitalised patient intends to leave the ward to smoke, they should be<br />
informed of the risk and advised to wear a thick outer covering that has not been<br />
contaminated with paraffin based products.<br />
• Relatives or carers should be informed if a patient does not comply with safety advice.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-47
Appendix 10 (continued)<br />
NPSA Alert 4: Fire Hazard with Paraffin Based Skin Products on Dressings and<br />
Clothing: Examples of products containing paraffin<br />
Examples of products containing paraffin<br />
Following a patient safety incident, the NPSA commissioned the Health and Safety<br />
Executive to undertake fire hazard testing with White Soft Paraffin at concentrations of<br />
over 50% on a variety of bandages, dressings and clothing. The results showed the ability<br />
to reproduce the fire hazard in a controlled environment. The following commonly<br />
prescribed products contain White Soft Paraffin (WSP) at concentrations of over 50%:<br />
Product Concentration of<br />
Product Concentration of WSP<br />
Diprobase Ointment<br />
95 %<br />
Emulsifying Ointment<br />
Liquid Paraffin 50%/White Soft Paraffin<br />
50%<br />
White Soft Paraffin<br />
Zinc And Salicylic Acid Paste BP<br />
Zinc Ointment BP<br />
50 %<br />
50%<br />
100 %<br />
50 %<br />
72.25 %<br />
Paraffin products can also be found as constituents in some commonly prescribed<br />
‘specials’ creams and ointment, for example emulsifying ointment is often used as a<br />
diluent to lower the strength of a ready prepared ointment.<br />
The evidence currently only relates to White Soft Paraffin and there is currently no<br />
evidence of a risk of fire hazard with preparations containing concentrations of WSP<br />
lower than 50%, however the NPSA has taken the view that this risk could apply to any<br />
paraffin ‘based’ product. In this respect the guidance should also apply to the following<br />
products. Dithranol Ointment (YSP), Epaderm (Emulsifying Wax, LP & YSP) and<br />
Hydromol Ointment (Emulsifying Wax, LP & YSP).<br />
LP = Liquid Paraffin; YSP = Yellow Soft Paraffin<br />
NB: These lists are not exhaustive and practitioners should make a professional<br />
judgement and risk assess whether the guidance should apply to other products.<br />
First line drugs Second line drugs Specialist drugs Hospital only drugs<br />
<strong>13</strong>-48