Photogrammetry of the optic disc in glaucoma and ocular ...
Photogrammetry of the optic disc in glaucoma and ocular ...
Photogrammetry of the optic disc in glaucoma and ocular ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Volume 18<br />
Nutnlxr 12 Stereophotogrammetry <strong>of</strong> <strong>optic</strong> <strong>disc</strong> 1255<br />
<strong>disc</strong> photographs were manually processed by a<br />
photogrammetric eng<strong>in</strong>eer accord<strong>in</strong>g to st<strong>and</strong>ard<br />
techniques. 21 The photogrammetry data were<br />
converted to digital form <strong>and</strong> analyzed by computer<br />
to determ<strong>in</strong>e depth, area, volume, <strong>and</strong><br />
o<strong>the</strong>r pert<strong>in</strong>ent geometric measurements <strong>of</strong> <strong>the</strong><br />
<strong>optic</strong> cup.<br />
Visual field test<strong>in</strong>g. A comb<strong>in</strong>ation <strong>of</strong> extensive<br />
static <strong>and</strong> k<strong>in</strong>etic perimetry was used to evaluate<br />
visual fields. K<strong>in</strong>etic perimetry (with ei<strong>the</strong>r <strong>the</strong><br />
Goldmann or Tub<strong>in</strong>gen perimeters) consisted <strong>of</strong> at<br />
least 2 isopters beyond 30° radius, 3 isopters<br />
with<strong>in</strong> 30° radius, <strong>and</strong> numerous spot checks between<br />
isopters with<strong>in</strong> <strong>the</strong> central 40° radius, as<br />
previously described by Portney <strong>and</strong> Krohn. 22<br />
Static perimetry (with <strong>the</strong> Tub<strong>in</strong>gen perimeter)<br />
consisted <strong>of</strong> threshold determ<strong>in</strong>ations along <strong>the</strong><br />
45°, 135°, 225°, <strong>and</strong> 315° meridians <strong>in</strong> 1° <strong>in</strong>tervals<br />
out to 20° radius <strong>and</strong> 2° <strong>in</strong>tervals between 20° <strong>and</strong><br />
30° radius. Additional static perimetry was performed<br />
along both radial (meridian) <strong>and</strong> circular<br />
paths which <strong>in</strong>tersected <strong>the</strong> length <strong>and</strong> width <strong>of</strong><br />
visual field defects plotted by k<strong>in</strong>etic perimetry.<br />
Approximately two thirds <strong>of</strong> <strong>the</strong> eyes were evaluated<br />
with this procedure, which required about 1<br />
hr per eye. The rema<strong>in</strong><strong>in</strong>g one third <strong>of</strong> <strong>the</strong> eyes<br />
were tested accord<strong>in</strong>g to <strong>the</strong> method described<br />
below.<br />
In view <strong>of</strong> recent f<strong>in</strong>d<strong>in</strong>gs 22 which show that<br />
static perimetry is more sensitive <strong>and</strong> reliable than<br />
k<strong>in</strong>etic perimetry for detection <strong>of</strong> early <strong>glaucoma</strong>tous<br />
visual field defects, 42 eyes were tested with<br />
<strong>the</strong> revised procedure illustrated <strong>in</strong> Fig. 1 (shown<br />
for a right eye). This visual field exam<strong>in</strong>ation consisted<br />
<strong>of</strong> at least 2 isopters beyond 30° radius (k<strong>in</strong>etic<br />
test<strong>in</strong>g) <strong>and</strong> static perimetry along four<br />
meridians (45°, 135°, 225°, 315°) <strong>in</strong> 2° <strong>in</strong>tervals <strong>and</strong><br />
six <strong>in</strong>termediate meridians <strong>in</strong> 2.5° <strong>in</strong>tervals across<br />
<strong>the</strong> central 30° radius <strong>of</strong> <strong>the</strong> visual field. Additional<br />
circular <strong>and</strong> radial (meridian) static perimetry was<br />
performed when it was necessary to fur<strong>the</strong>r def<strong>in</strong>e<br />
specific portions <strong>of</strong> <strong>the</strong> visual field. All determ<strong>in</strong>ations<br />
were conducted on <strong>the</strong> Tub<strong>in</strong>gen perimeter<br />
<strong>and</strong> required approximately 45 to 50 m<strong>in</strong> per eye.<br />
This revised procedure thus provided <strong>the</strong> dual advantages<br />
<strong>of</strong> greater time efficiency <strong>and</strong> more effective<br />
detection <strong>of</strong> early <strong>glaucoma</strong>tous visual field<br />
defects.<br />
Specific criteria were established to def<strong>in</strong>e <strong>the</strong><br />
presence or absence <strong>of</strong> visual field defects, based<br />
upon extensive previous experience <strong>and</strong> exist<strong>in</strong>g<br />
guidel<strong>in</strong>es developed by o<strong>the</strong>r <strong>in</strong>vestigators. 23 ' 24<br />
Accord<strong>in</strong>g to our st<strong>and</strong>ards, areas <strong>of</strong> visual field<br />
loss had to be at least (1) 5° by 5° <strong>in</strong> size <strong>and</strong> 0.5 log<br />
unit <strong>of</strong> lum<strong>in</strong>ance (apostilbs) deep or (2) 3° by 3° <strong>in</strong><br />
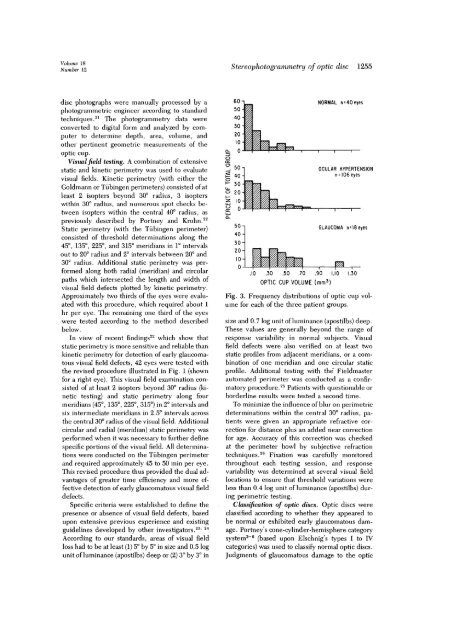
60-<br />
50-<br />
.10 .30 .50 .70 .90 1.10<br />
OPTIC CUP VOLUME (mm 3 )<br />
NORMAL n = 40 eyes<br />
OCULAR HYPERTENSION<br />
n = 106 eyes<br />
GLAUCOMA n= 18 eyes<br />
Fig. 3. Frequency distributions <strong>of</strong> <strong>optic</strong> cup volume<br />
for each <strong>of</strong> <strong>the</strong> three patient groups.<br />
size <strong>and</strong> 0.7 log unit <strong>of</strong> lum<strong>in</strong>ance (apostilbs) deep.<br />
These values are generally beyond <strong>the</strong> range <strong>of</strong><br />
response variability <strong>in</strong> normal subjects. Visual<br />
field defects were also verified on at least two<br />
static pr<strong>of</strong>iles from adjacent meridians, or a comb<strong>in</strong>ation<br />
<strong>of</strong> one meridian <strong>and</strong> one circular static<br />
pr<strong>of</strong>ile. Additional test<strong>in</strong>g with <strong>the</strong>' Fieldmaster<br />
automated perimeter was conducted as a confirmatory<br />
procedure. 25 Patients with questionable or<br />
borderl<strong>in</strong>e results were tested a second time.<br />
To m<strong>in</strong>imize <strong>the</strong> <strong>in</strong>fluence <strong>of</strong> blur on perimetric<br />
determ<strong>in</strong>ations with<strong>in</strong> <strong>the</strong> central 30° radius, patients<br />
were given an appropriate refractive correction<br />
for distance plus an added near correction<br />
for age. Accuracy <strong>of</strong> this correction was checked<br />
at <strong>the</strong> perimeter bowl by subjective refraction<br />
techniques. 26 Fixation was carefully monitored<br />
throughout each test<strong>in</strong>g session, <strong>and</strong> response<br />
variability was determ<strong>in</strong>ed at several visual field<br />
locations to ensure that threshold variations were<br />
less than 0.4 log unit <strong>of</strong> lum<strong>in</strong>ance (apostilbs) dur<strong>in</strong>g<br />
perimetric test<strong>in</strong>g.<br />
Classification <strong>of</strong> <strong>optic</strong> <strong>disc</strong>s. Optic <strong>disc</strong>s were<br />
classified accord<strong>in</strong>g to whe<strong>the</strong>r <strong>the</strong>y appeared to<br />
be normal or exhibited early <strong>glaucoma</strong>tous damage.<br />
Portney's cone-cyl<strong>in</strong>der-hemisphere category<br />
system 2 " 6 (based upon Elschnigs types I to IV<br />
categories) was used to classify normal <strong>optic</strong> <strong>disc</strong>s.<br />
Judgments <strong>of</strong> <strong>glaucoma</strong>tous damage to <strong>the</strong> <strong>optic</strong>