Two-Lung and One-Lung Ventilation in Patients - Anesthesia ...
Two-Lung and One-Lung Ventilation in Patients - Anesthesia ...
Two-Lung and One-Lung Ventilation in Patients - Anesthesia ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
ANESTH ANALG CARDIOVASCULAR ANESTHESIA BARDOCZKY ET AL. 37<br />
2000;90:35–41 POSITION AND Fio 2 DURING OLV<br />
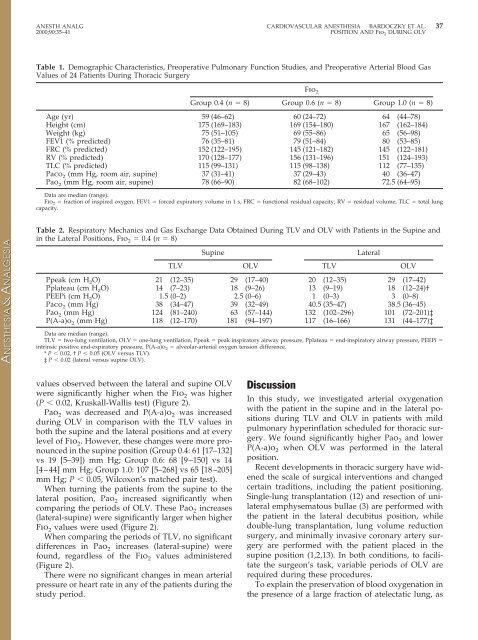
Table 1. Demographic Characteristics, Preoperative Pulmonary Function Studies, <strong>and</strong> Preoperative Arterial Blood Gas<br />
Values of 24 <strong>Patients</strong> Dur<strong>in</strong>g Thoracic Surgery<br />
values observed between the lateral <strong>and</strong> sup<strong>in</strong>e OLV<br />
were significantly higher when the Fio 2 was higher<br />
(P 0.02, Kruskall-Wallis test) (Figure 2).<br />
Pao 2 was decreased <strong>and</strong> P(A-a)o 2 was <strong>in</strong>creased<br />
dur<strong>in</strong>g OLV <strong>in</strong> comparison with the TLV values <strong>in</strong><br />
both the sup<strong>in</strong>e <strong>and</strong> the lateral positions <strong>and</strong> at every<br />
level of Fio 2. However, these changes were more pronounced<br />
<strong>in</strong> the sup<strong>in</strong>e position (Group 0.4: 61 [17–132]<br />
vs 19 [5–39]) mm Hg; Group 0.6: 68 [9–150] vs 14<br />
[4–44] mm Hg; Group 1.0: 107 [5–268] vs 65 [18–205]<br />
mm Hg; P 0.05, Wilcoxon’s matched pair test).<br />
When turn<strong>in</strong>g the patients from the sup<strong>in</strong>e to the<br />
lateral position, Pao 2 <strong>in</strong>creased significantly when<br />
compar<strong>in</strong>g the periods of OLV. These Pao 2 <strong>in</strong>creases<br />
(lateral-sup<strong>in</strong>e) were significantly larger when higher<br />
Fio 2 values were used (Figure 2).<br />
When compar<strong>in</strong>g the periods of TLV, no significant<br />
differences <strong>in</strong> Pao 2 <strong>in</strong>creases (lateral-sup<strong>in</strong>e) were<br />
found, regardless of the Fio 2 values adm<strong>in</strong>istered<br />
(Figure 2).<br />
There were no significant changes <strong>in</strong> mean arterial<br />
pressure or heart rate <strong>in</strong> any of the patients dur<strong>in</strong>g the<br />
study period.<br />
Discussion<br />
Fio 2<br />
Group 0.4 (n 8) Group 0.6 (n 8) Group 1.0 (n 8)<br />
Age (yr) 59 (46–62) 60 (24–72) 64 (44–78)<br />
Height (cm) 175 (169–183) 169 (154–180) 167 (162–184)<br />
Weight (kg) 75 (51–105) 69 (55–86) 65 (56–98)<br />
FEV1 (% predicted) 76 (35–81) 79 (51–84) 80 (53–85)<br />
FRC (% predicted) 152 (122–195) 145 (121–182) 145 (122–181)<br />
RV (% predicted) 170 (128–177) 156 (131–196) 151 (124–193)<br />
TLC (% predicted) 115 (99–131) 115 (98–138) 112 (77–135)<br />
Paco 2 (mm Hg, room air, sup<strong>in</strong>e) 37 (31–41) 37 (29–43) 40 (36–47)<br />
Pao 2 (mm Hg, room air, sup<strong>in</strong>e) 78 (66–90) 82 (68–102) 72.5 (64–95)<br />
Data are median (range).<br />
Fio 2 fraction of <strong>in</strong>spired oxygen, FEV1 forced expiratory volume <strong>in</strong> 1 s, FRC functional residual capacity, RV residual volume, TLC total lung<br />
capacity.<br />
Table 2. Respiratory Mechanics <strong>and</strong> Gas Exchange Data Obta<strong>in</strong>ed Dur<strong>in</strong>g TLV <strong>and</strong> OLV with <strong>Patients</strong> <strong>in</strong> the Sup<strong>in</strong>e <strong>and</strong><br />
<strong>in</strong> the Lateral Positions, Fio 2 0.4 (n 8)<br />
Sup<strong>in</strong>e Lateral<br />
TLV OLV TLV OLV<br />
Ppeak (cm H 2O) 21 (12–35) 29 (17–40) 20 (12–35) 29 (17–42)<br />
Pplateau (cm H 2O) 14 (7–23) 18 (9–26) 13 (9–19) 18 (12–24)†<br />
PEEPi (cm H 2O) 1.5 (0–2) 2.5 (0–6) 1 (0–3) 3 (0–8)<br />
Paco 2 (mm Hg) 38 (34–47) 39 (32–49) 40.5 (35–47) 38.5 (36–45)<br />
Pao 2 (mm Hg) 124 (81–240) 63 (57–144) 132 (102–296) 101 (72–201)‡<br />
P(A-a)o 2 (mm Hg) 118 (12–170) 181 (94–197) 117 (16–166) 131 (44–177)‡<br />
Data are median (range).<br />
TLV two-lung ventilation, OLV one-lung ventilation, Ppeak peak <strong>in</strong>spiratory airway pressure, Pplateau end-<strong>in</strong>spiratory airway pressure, PEEPi <br />
<strong>in</strong>tr<strong>in</strong>sic positive end-expiratory pressure, P(A-a)o 2 alveolar-arterial oxygen tension difference.<br />
* P 0.02, † P 0.05 (OLV versus TLV).<br />
‡ P 0.02 (lateral versus sup<strong>in</strong>e OLV).<br />
In this study, we <strong>in</strong>vestigated arterial oxygenation<br />
with the patient <strong>in</strong> the sup<strong>in</strong>e <strong>and</strong> <strong>in</strong> the lateral positions<br />
dur<strong>in</strong>g TLV <strong>and</strong> OLV <strong>in</strong> patients with mild<br />
pulmonary hyper<strong>in</strong>flation scheduled for thoracic surgery.<br />
We found significantly higher Pao 2 <strong>and</strong> lower<br />
P(A-a)o 2 when OLV was performed <strong>in</strong> the lateral<br />
position.<br />
Recent developments <strong>in</strong> thoracic surgery have widened<br />
the scale of surgical <strong>in</strong>terventions <strong>and</strong> changed<br />
certa<strong>in</strong> traditions, <strong>in</strong>clud<strong>in</strong>g the patient position<strong>in</strong>g.<br />
S<strong>in</strong>gle-lung transplantation (12) <strong>and</strong> resection of unilateral<br />
emphysematous bullae (3) are performed with<br />
the patient <strong>in</strong> the lateral decubitus position, while<br />
double-lung transplantation, lung volume reduction<br />
surgery, <strong>and</strong> m<strong>in</strong>imally <strong>in</strong>vasive coronary artery surgery<br />
are performed with the patient placed <strong>in</strong> the<br />
sup<strong>in</strong>e position (1,2,13). In both conditions, to facilitate<br />
the surgeon’s task, variable periods of OLV are<br />
required dur<strong>in</strong>g these procedures.<br />
To expla<strong>in</strong> the preservation of blood oxygenation <strong>in</strong><br />
the presence of a large fraction of atelectatic lung, as