Two-Lung and One-Lung Ventilation in Patients - Anesthesia ...
Two-Lung and One-Lung Ventilation in Patients - Anesthesia ...
Two-Lung and One-Lung Ventilation in Patients - Anesthesia ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
ANESTH ANALG CARDIOVASCULAR ANESTHESIA BARDOCZKY ET AL. 39<br />
2000;90:35–41 POSITION AND Fio 2 DURING OLV<br />
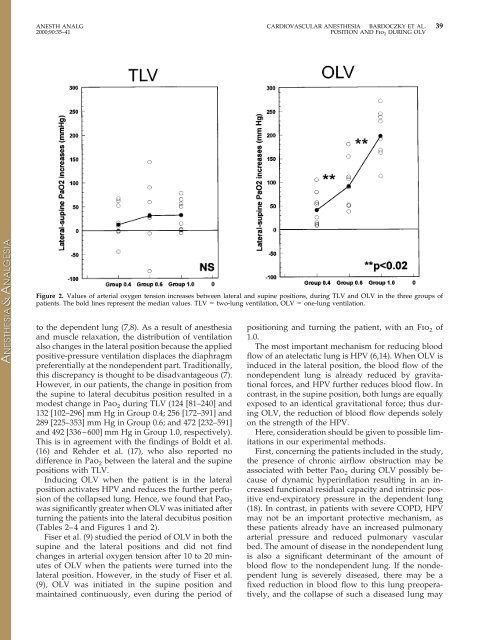
Figure 2. Values of arterial oxygen tension <strong>in</strong>creases between lateral <strong>and</strong> sup<strong>in</strong>e positions, dur<strong>in</strong>g TLV <strong>and</strong> OLV <strong>in</strong> the three groups of<br />
patients. The bold l<strong>in</strong>es represent the median values. TLV two-lung ventilation, OLV one-lung ventilation.<br />
to the dependent lung (7,8). As a result of anesthesia<br />
<strong>and</strong> muscle relaxation, the distribution of ventilation<br />
also changes <strong>in</strong> the lateral position because the applied<br />
positive-pressure ventilation displaces the diaphragm<br />
preferentially at the nondependent part. Traditionally,<br />
this discrepancy is thought to be disadvantageous (7).<br />
However, <strong>in</strong> our patients, the change <strong>in</strong> position from<br />
the sup<strong>in</strong>e to lateral decubitus position resulted <strong>in</strong> a<br />
modest change <strong>in</strong> Pao 2 dur<strong>in</strong>g TLV (124 [81–240] <strong>and</strong><br />
132 [102–296] mm Hg <strong>in</strong> Group 0.4; 256 [172–391] <strong>and</strong><br />
289 [225–353] mm Hg <strong>in</strong> Group 0.6; <strong>and</strong> 472 [232–591]<br />
<strong>and</strong> 492 [336–600] mm Hg <strong>in</strong> Group 1.0, respectively).<br />
This is <strong>in</strong> agreement with the f<strong>in</strong>d<strong>in</strong>gs of Boldt et al.<br />
(16) <strong>and</strong> Rehder et al. (17), who also reported no<br />
difference <strong>in</strong> Pao 2 between the lateral <strong>and</strong> the sup<strong>in</strong>e<br />
positions with TLV.<br />
Induc<strong>in</strong>g OLV when the patient is <strong>in</strong> the lateral<br />
position activates HPV <strong>and</strong> reduces the further perfusion<br />
of the collapsed lung. Hence, we found that Pao 2<br />
was significantly greater when OLV was <strong>in</strong>itiated after<br />
turn<strong>in</strong>g the patients <strong>in</strong>to the lateral decubitus position<br />
(Tables 2–4 <strong>and</strong> Figures 1 <strong>and</strong> 2).<br />
Fiser et al. (9) studied the period of OLV <strong>in</strong> both the<br />
sup<strong>in</strong>e <strong>and</strong> the lateral positions <strong>and</strong> did not f<strong>in</strong>d<br />
changes <strong>in</strong> arterial oxygen tension after 10 to 20 m<strong>in</strong>utes<br />
of OLV when the patients were turned <strong>in</strong>to the<br />
lateral position. However, <strong>in</strong> the study of Fiser et al.<br />
(9), OLV was <strong>in</strong>itiated <strong>in</strong> the sup<strong>in</strong>e position <strong>and</strong><br />
ma<strong>in</strong>ta<strong>in</strong>ed cont<strong>in</strong>uously, even dur<strong>in</strong>g the period of<br />
position<strong>in</strong>g <strong>and</strong> turn<strong>in</strong>g the patient, with an Fio 2 of<br />
1.0.<br />
The most important mechanism for reduc<strong>in</strong>g blood<br />
flow of an atelectatic lung is HPV (6,14). When OLV is<br />
<strong>in</strong>duced <strong>in</strong> the lateral position, the blood flow of the<br />
nondependent lung is already reduced by gravitational<br />
forces, <strong>and</strong> HPV further reduces blood flow. In<br />
contrast, <strong>in</strong> the sup<strong>in</strong>e position, both lungs are equally<br />
exposed to an identical gravitational force; thus dur<strong>in</strong>g<br />
OLV, the reduction of blood flow depends solely<br />
on the strength of the HPV.<br />
Here, consideration should be given to possible limitations<br />
<strong>in</strong> our experimental methods.<br />
First, concern<strong>in</strong>g the patients <strong>in</strong>cluded <strong>in</strong> the study,<br />
the presence of chronic airflow obstruction may be<br />
associated with better Pao 2 dur<strong>in</strong>g OLV possibly because<br />
of dynamic hyper<strong>in</strong>flation result<strong>in</strong>g <strong>in</strong> an <strong>in</strong>creased<br />
functional residual capacity <strong>and</strong> <strong>in</strong>tr<strong>in</strong>sic positive<br />
end-expiratory pressure <strong>in</strong> the dependent lung<br />
(18). In contrast, <strong>in</strong> patients with severe COPD, HPV<br />
may not be an important protective mechanism, as<br />
these patients already have an <strong>in</strong>creased pulmonary<br />
arterial pressure <strong>and</strong> reduced pulmonary vascular<br />
bed. The amount of disease <strong>in</strong> the nondependent lung<br />
is also a significant determ<strong>in</strong>ant of the amount of<br />
blood flow to the nondependent lung. If the nondependent<br />
lung is severely diseased, there may be a<br />
fixed reduction <strong>in</strong> blood flow to this lung preoperatively,<br />
<strong>and</strong> the collapse of such a diseased lung may