HEAD & NECK SURGERY - Stanford University School of Medicine
HEAD & NECK SURGERY - Stanford University School of Medicine
HEAD & NECK SURGERY - Stanford University School of Medicine
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
S T ANFORD U NIVERSITY D EPARTMENT OF O TOLARYNGOLOGY– <strong>HEAD</strong> & N ECK S URGERY<br />
R ESEARCH P ROGRAMS<br />
THE EVALUATION, MANAGE-<br />
MENT, AND PREVENTION<br />
OF CISPLATIN OTOTOXICITY IN<br />
PEDIATRIC PATIENTS.<br />
Kay Chang, MD<br />
Cisplatin is a commonly administered<br />
chemotherapeutic agent in multiple<br />
pediatric neoplasms. The ototoxicity <strong>of</strong><br />
this agent is well-documented, though<br />
poorly characterized. Reports <strong>of</strong> ototoxicity<br />
rates in children vary from 1% to 82%.<br />
This disparity is due to extreme variability<br />
between institutions in the audiologic<br />
assessment <strong>of</strong> sick pediatric patients, as<br />
well as the lack <strong>of</strong> a well established and<br />
clinically validated classification for<br />
degrees <strong>of</strong> ototoxicity. The Common Terminology<br />
Criteria for Adverse Events<br />
(CTCAE v3.0) widely used by oncologists,<br />
fails to classify ototoxicity in a clinically<br />
consistent, or relevant manner.<br />
Due to a lack <strong>of</strong> a robust grading system<br />
for ototoxicity, it is difficult to design ototoxicity<br />
studies in patients that can be<br />
easily compared to other studies. I have<br />
developed a more clinically useful grading<br />
system for pediatric ototoxicity and<br />
have validated it to a large 5-year cohort<br />
<strong>of</strong> children treated by the Lucile Packard<br />
Children’s Hospital (LPCH) at <strong>Stanford</strong><br />
Pediatric Oncology department. By examining<br />
details such as dose delivery schedule<br />
and co-administered drugs, a number<br />
<strong>of</strong> interesting revelations regarding optimal<br />
methods <strong>of</strong> reducing ototoxicity in<br />
children have been discovered, and will<br />
be presented at the next ASCO meeting.<br />
As an active member <strong>of</strong> the Children’s<br />
Oncology Group (COG), a national organization<br />
involved in improving the oncologic<br />
care <strong>of</strong> children, I have been intimately<br />
involved in the ototoxicity<br />
assessment <strong>of</strong> multiple large multi-institutional<br />
studies administered by COG<br />
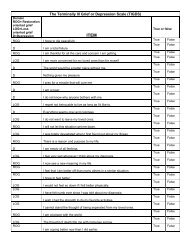
12<br />
20<br />
15<br />
10<br />
5<br />
0<br />
dB<br />
-5<br />
-10<br />
-15<br />
-20<br />
-25<br />
Post-Treatment DPOAEs<br />
2000 2378 2828 3364 4000 4757 5657 6727 8000 9514 11314 13454 16000<br />
Hz<br />
(including the Intergroup Hepatoblastoma<br />
Study P9645 and the ARAR0331<br />
Nasopharyngeal Carcinoma Study). This<br />
grading system has been a valuable tool<br />
and has helped to improve methodologies<br />
for accurately assessing and characterizing<br />
ototoxic effects. This is particularly<br />
important since children seem to be<br />
much more susceptible to ototoxicity<br />
than adults. Furthermore, while the effects<br />
<strong>of</strong> ototoxicity may be quite limited in<br />
adults who have mastered speech and<br />
language, in pre-lingual young children,<br />
ototoxicity may result in severe speech<br />
delay and the inability to ever assume a<br />
normal role in society. So while the children<br />
may be cured <strong>of</strong> their cancer, they<br />
really never fully recover from their treatment<br />
to live normal unhindered lives.<br />
While accurately monitoring cisplatin<br />
ototoxicity may provide some insights<br />
into improved dosing strategies for<br />
reducing adverse effects in children, a<br />
more exciting approach is actual prevention<br />
<strong>of</strong> ototoxicity by administering various<br />
“otoprotective” agents. In the course<br />
<strong>of</strong> investigating the protective effect <strong>of</strong><br />
the anti-oxidant N-acetylcysteine in the<br />
guinea pig cochlea, my laboratory discovered<br />
a novel otoprotective effect<br />
induced by the transtympanic administration<br />
<strong>of</strong> lactate to the middle ear. In<br />
this experiment, guinea pigs treated with<br />
cisplatin that were administered either<br />
lactated Ringer’s solution or N-acetylcysteine<br />
had significantly improved cochlear<br />
function, as measured by DPOAE, compared<br />
to the normal saline and negative<br />
control groups (see figure). Currently,<br />
with the collaboration the LPCH Pediatric<br />
Oncology department, standardized protocols<br />
utilizing my grading scale are<br />
being developed to investigate these as<br />
well as other otoprotective agents, including<br />
EPO and several gene therapy<br />
agents. Our goal is with these<br />
efforts is to eliminate this most<br />
devastating late-effect <strong>of</strong> chemotherapy<br />
in young children.<br />
Legend<br />
IR<br />
N-AC<br />
NS<br />
Control<br />
Mean post-treatment DPOAE data. Stimulus<br />
parameters were L2 = 55 dB and F2 ranging<br />
from 2 to 16 kHz. Error bars represent one<br />
SEM, and are plotted for the Control and LR<br />
groups; however they were comparable<br />
across all 4 groups (average SEM across frequencies<br />
measured 2.88, 3.27, 2.93, and 2.78<br />
for the 4 groups). The light dotted line at the<br />
bottom <strong>of</strong> the graph represents the average<br />
noise floor during emission recording.<br />
CLINICAL RESEARCH IN SLEEP<br />
<strong>SURGERY</strong><br />
Richard L. Goode, MD, Jose E. Barrera, MD,<br />
Nelson Powell, MD, Robert Riley, MD<br />
The Division <strong>of</strong> sleep surgery aims to<br />
develop improved diagnostic methods<br />
in evaluating site <strong>of</strong> obstruction in sleep<br />
apnea patients. We are taking two<br />
approaches to improve our understanding<br />
<strong>of</strong> the anatomic reasons for collapse<br />
<strong>of</strong> the upper airway in obstructive sleep<br />
apnea. A protocol which is being coordinated<br />
with Dr. Gerald Popelka will utilize<br />
cine real-time MRI scanning <strong>of</strong> the upper<br />
airway in patients with sleep disordered<br />
breathing and normal volunteers, and<br />
correlate these findings with the endoscopic<br />
evaluation <strong>of</strong> patients before and<br />
after surgery. Electroencephalogram,<br />
actigraphy, and pulse oximetry data in<br />
combination with MRI images will be<br />
collected from patients with upper airway<br />
resistance syndrome, obstructive<br />
sleep apnea, and normal controls. We expect<br />
to be able to significantly improve<br />
our understanding <strong>of</strong> the anatomic reasons<br />
for a given patient’s obstructive<br />
symptoms, and thus improve clinical<br />
staging and surgical decision-making.<br />
Real time MRI scan<br />
Our second project aims to evaluate<br />
functional obstruction during sleep as a<br />
measure <strong>of</strong> pressure manometry. The use<br />
<strong>of</strong> a multi-site pressure probe tube that<br />
is worn during sleep will be utilized to<br />
determine the site <strong>of</strong> obstruction based<br />
on pressure changes across five transducers<br />
within the probe tube precisely<br />
located in the upper airway. We hope to<br />
characterize what causes multi-site<br />
obstruction and to what degree patients<br />
with with obstructive sleep apnea are<br />
affected.