CH. 19: Abnormal Red Reflex
CH. 19: Abnormal Red Reflex
CH. 19: Abnormal Red Reflex
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
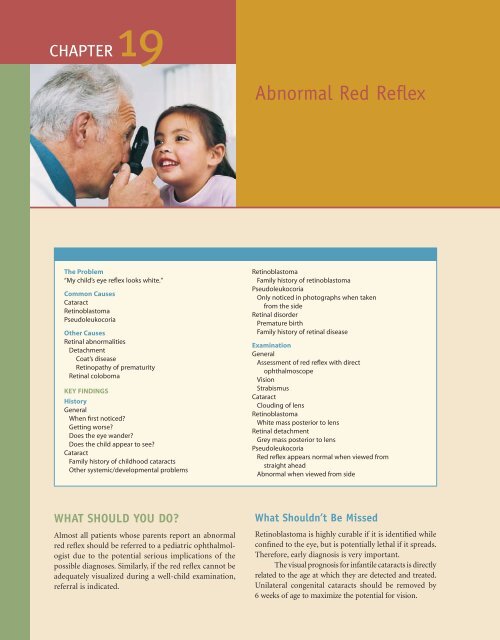
<strong>CH</strong>APTER <strong>19</strong><br />
The Problem<br />
“My child’s eye refl ex looks white.”<br />
Common Causes<br />
Cataract<br />
Retinoblastoma<br />
Pseudoleukocoria<br />
Other Causes<br />
Retinal abnormalities<br />
Detachment<br />
Coat’s disease<br />
Retinopathy of prematurity<br />
Retinal coloboma<br />
KEY FINDINGS<br />
History<br />
General<br />
When fi rst noticed?<br />
Getting worse?<br />
Does the eye wander?<br />
Does the child appear to see?<br />
Cataract<br />
Family history of childhood cataracts<br />
Other systemic/developmental problems<br />
WHAT SHOULD YOU DO?<br />
Almost all patients whose parents report an abnormal<br />
red refl ex should be referred to a pediatric ophthalmologist<br />
due to the potential serious implications of the<br />
possible diagnoses. Similarly, if the red refl ex cannot be<br />
adequately visualized during a well-child examination,<br />
referral is indicated.<br />
<strong>Abnormal</strong> <strong>Red</strong> Refl ex<br />
Retinoblastoma<br />
Family history of retinoblastoma<br />
Pseudoleukocoria<br />
Only noticed in photographs when taken<br />
from the side<br />
Retinal disorder<br />
Premature birth<br />
Family history of retinal disease<br />
Examination<br />
General<br />
Assessment of red refl ex with direct<br />
ophthalmoscope<br />
Vision<br />
Strabismus<br />
Cataract<br />
Clouding of lens<br />
Retinoblastoma<br />
White mass posterior to lens<br />
Retinal detachment<br />
Grey mass posterior to lens<br />
Pseudoleukocoria<br />
<strong>Red</strong> refl ex appears normal when viewed from<br />
straight ahead<br />
<strong>Abnormal</strong> when viewed from side<br />
What Shouldn’t Be Missed<br />
Retinoblastoma is highly curable if it is identifi ed while<br />
confi ned to the eye, but is potentially lethal if it spreads.<br />
Therefore, early diagnosis is very important.<br />
The visual prognosis for infantile cataracts is directly<br />
related to the age at which they are detected and treated.<br />
Unilateral congenital cataracts should be removed by<br />
6 weeks of age to maximize the potential for vision.
FIGURE <strong>19</strong>–1 ■ <strong>Abnormal</strong> red refl ex, right eye, secondary to infantile<br />
cataract.<br />
COMMON CAUSES<br />
1. Cataracts. Cataracts in infants are most commonly<br />
identifi ed by an abnormal red refl ex<br />
(Figure <strong>19</strong>–1). Due to the high risk of amblyopia<br />
in unilateral cataracts, prompt referral to a<br />
pediatric ophthalmologist is indicated. Bilateral<br />
cataracts may occur in association with several<br />
syndromes or diseases, and these children<br />
require evaluation for these systemic disorders<br />
(see Chapter 30).<br />
2. Retinoblastoma. Retinoblastoma is rare, but it<br />
is the most common primary intraocular<br />
tumor in children. It most frequently presents<br />
due to an abnormal red refl ex (Figure <strong>19</strong>–2A<br />
and B). It is one of the few life- threatening<br />
disorders encountered in pediatric ophthalmology.<br />
Intraocular retinoblastoma is very<br />
treatable, but the mortality for metastatic<br />
disease is high. Identification of tumors<br />
before systemic spread is critical. Most children<br />
with large unilateral tumors will require<br />
enucleation (surgical removal of the eye),<br />
but the eye and vision may sometimes be<br />
preserved if the tumors are identifi ed when<br />
they are small.<br />
3. Pseudoleukocoria. The optic nerve head at the<br />
back of the eye is white. If a light is shined<br />
into the eye from an oblique angle temporally,<br />
the refl ection from the optic nerve head may<br />
fi ll the pupillary opening, producing pseudoleukocoria<br />
(Figure <strong>19</strong>–3). This usually requires<br />
evaluation by a pediatric ophthalmologist to<br />
verify.<br />
4. Retinal disorders. Retinal disorders that cause<br />
detachments are rare in children. They most<br />
commonly occur in infants with retinopathy of<br />
prematurity and may also occur following<br />
A<br />
B<br />
<strong>CH</strong>APTER <strong>19</strong> <strong>Abnormal</strong> <strong>Red</strong> Refl ex ■ 115<br />
FIGURE <strong>19</strong>–2 ■ Retinoblastoma, left eye. (A) <strong>Abnormal</strong> red refl ex.<br />
(B) Magnifi ed view shows vascularized elevated white retinal mass.<br />
The lens is clear.<br />
FIGURE <strong>19</strong>–3 ■ Pseudoleukocoria, left eye. The light refl ex in the<br />
left eye appears white due to a refl ection from the optic nerve head<br />
(which is white). Note that the photograph is taken from the<br />
patient’s left side.
116 ■ Section 2: Symptoms<br />
Table <strong>19</strong>–1.<br />
Causes of Retinal Detachment in Children<br />
■ Retinopathy of prematurity<br />
■ Systemic diseases<br />
Incontinentia pigmenti<br />
Familial exudative vitreoretinopathy<br />
■ Trauma<br />
■ Toxocara<br />
■ Coat’s disease<br />
A<br />
B<br />
trauma or due to rare familial disorders<br />
(Table <strong>19</strong>–1). Large retinal colobomas may also<br />
produce leukocoria (Figure <strong>19</strong>–4A and B).<br />
Toxocara infections may cause both retinal<br />
detachments and cataracts. They usually present<br />
as inflammatory white masses in the<br />
peripheral retina (Figure <strong>19</strong>–5).<br />
FIGURE <strong>19</strong>–4 ■ Retinal coloboma. (A) Leukocoria secondary to<br />
refl ection from abnormal retina. Note the small iris coloboma (arrow).<br />
(B) Fundus examination shows large inferior retinal coloboma.<br />
FIGURE <strong>19</strong>–5 ■ Toxocara infection of the retina. These usually present<br />
as infl ammatory white masses in the peripheral retina. Note the<br />
traction bands extending from the surface of the lesion (arrow).<br />
APPROA<strong>CH</strong> TO THE PATIENT<br />
An abnormal red refl ex is often the fi rst abnormality<br />
noted in patients with potentially life- and vision-<br />
threatening disorders. Many of these occur in infants<br />
and young children, who are unable to vocalize complaints.<br />
It is important to realize that in young children,<br />
even if one eye has extremely poor vision, as long as the<br />
other eye sees normally, the child will function well visually.<br />
Therefore, the absence of any complaints about the<br />
child’s vision in no way rules out the possibility of unilateral<br />
eye problems. Because of this, examination of<br />
the red refl ex should be part of every routine wellchild<br />
check.<br />
History<br />
Parents may come in to the pediatrician having noted<br />
an abnormal red refl ex, or it may be noted during a<br />
routine examination. In either setting, one should ask<br />
how well the child appears to see. If the family has<br />
noticed an abnormal red refl ex, the age when it was fi rst<br />
noted should be determined. If only one eye is affected,<br />
the child will usually appear to see normally. If a child<br />
has a bilateral disorder, abnormal visual behavior will<br />
often be the fi rst symptom noted by parents. If a child<br />
has decreased vision in one eye for any reason, strabismus<br />
often develops. This may be either esotropia or<br />
exotropia, and is often intermittent.<br />
Questions about the child’s general health may<br />
raise the suspicion of syndromes that may be associated<br />
with cataracts. Premature birth may lead to retinopathy<br />
of prematurity, which may cause retinal detachments.<br />
Retinoblastoma, cataracts, and many retinal disorders<br />
may be inherited, and therefore obtaining a family history<br />
is important.
FIGURE <strong>19</strong>–6 ■ <strong>Red</strong> refl ex examination. This is most easily performed<br />
by using the direct ophthalmoscope from 2 to 3 feet away<br />
from the patient in a dim room. The examiner focuses on the child’s<br />
face with the ophthalmoscope, and the red refl ex can be compared<br />
between the two eyes.<br />
Examination<br />
The child’s vision and examination of the anterior segment<br />
should be performed in the normal manner. To<br />
best evaluate the red reflex, use the direct ophthalmoscope<br />
from 2 to 3 feet away from the patient in a dim room.<br />
Focus the ophthalmoscope on the patient’s face. The red<br />
reflex can then be assessed and compared between the two<br />
eyes (Figure <strong>19</strong>–6). The symmetry of the corneal light<br />
reflexes can also be noted at this time to screen for strabismus.<br />
Pseudoleukocoria, retinoblastoma, and retinal<br />
colobomas usually cause a very white refl ex, whereas<br />
retinal detachments are typically gray. The appearance<br />
of cataracts is highly variable. If a parent reports an<br />
abnormal red refl ex, but it is not noted when shining<br />
the light into the patient’s eyes from straight ahead, you<br />
should assess the red refl ex as you move the direct ophthalmoscope<br />
from side to side. Tumors of the nasal<br />
retina, for instance, may not be noted until the light is<br />
shined into the eye from a lateral position (Figure<br />
<strong>19</strong>–7A–D). This may be diffi cult to differentiate from<br />
pseudoleukocoria, which is also only noted when viewed<br />
from a lateral position.<br />
PLAN<br />
If a parent reports an abnormal red refl ex or if you note<br />
this on examination, the child should be referred<br />
promptly to a pediatric ophthalmologist. This is particularly<br />
important for retinoblastoma, which may be<br />
lethal if it spreads beyond the eye. If an abnormal red<br />
refl ex is found on a newborn screening, the patient<br />
should also be referred promptly. In a newborn, a cataract<br />
is the most likely etiology for leukocoria. If an infant<br />
has a unilateral cataract, surgical removal should be performed<br />
in the fi rst 6 weeks of life to maximize the visual<br />
potential.<br />
A<br />
B<br />
C<br />
D<br />
<strong>CH</strong>APTER <strong>19</strong> <strong>Abnormal</strong> <strong>Red</strong> Refl ex ■ 117<br />
FIGURE <strong>19</strong>–7 ■ Leukocoria due to nasal retinoblastoma, left eye.<br />
(A) <strong>Red</strong> refl ex appears normal when viewed from straight ahead.<br />
(B) Crescent-shaped abnormality (arrow) begins to appear when light<br />
is moved to left. (C) <strong>Red</strong> refl ex absent as light moved further to left.<br />
(D) Fundus examination reveals a large tumor fi lling the nasal retina.<br />
The optic nerve is marked by an arrow.
118 ■ Section 2: Symptoms<br />
Only in photos taken<br />
from oblique angle or<br />
on examination of red<br />
reflex from patient's side<br />
Probable optic nerve<br />
head reflection<br />
Rarely retinoblastoma<br />
Refer to ophthalmology<br />
to verify<br />
Cornea<br />
abnormality<br />
Iris/pupil<br />
not visible<br />
Refer to<br />
ophthalmology<br />
FIGURE <strong>19</strong>–8 ■ Causes of an abnormal red refl ex.<br />
WHAT SHOULDN’T BE MISSED<br />
<strong>Abnormal</strong> red reflex<br />
Lens opacity<br />
Cataract<br />
Refer to<br />
ophthalmology<br />
Cataracts and retinoblastoma both often present with leukocoria.<br />
These are among the most treatable potentially<br />
vision- and life-threatening disorders in pediatric ophthalmology,<br />
and early referral is critical (Figure <strong>19</strong>–8).<br />
Retinoblastoma<br />
Refer to<br />
ophthalmology<br />
When to Refer<br />
Mass<br />
Retina<br />
Retinal<br />
detachment<br />
Refer to<br />
ophthalmology<br />
■ Any child with an abnormal red refl ex should be<br />
referred to a pediatric ophthalmologist<br />
No mass<br />
Affected eye<br />
often smaller<br />
Retinal<br />
coloboma<br />
Refer to<br />
ophthalmology