Seizures and Epilepsy
Seizures and Epilepsy
Seizures and Epilepsy
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
CHAPTER 3<br />
DEFINITIONS AND EPIDEMIOLOGY<br />
A general simplified definition of a seizure is a sudden<br />
temporary change in brain function caused by an<br />
abnormal rhythmic electrical discharge. <strong>Epilepsy</strong> is,<br />
simply put, a state of recurrent seizure activity. The<br />
mechanism whereby a seizure turns into epilepsy, a<br />
process known as epileptogenesis, is controversial.<br />
<strong>Seizures</strong> are common in humans, with an incidence<br />
of approximately 80/100,000 per year <strong>and</strong> an<br />
overall risk of epilepsy of 1% to 3%. 1 Status epilepticus<br />
is a less common form of severe prolonged seizure activity<br />
with a high morbidity <strong>and</strong> mortality.<br />
PATHOGENESIS<br />
<strong>Seizures</strong> arise secondary to a number of etiologies. Idiopathic<br />
seizures, or “cryptogenic” seizures, are fairly common.<br />
Contrary to what many patients <strong>and</strong> families<br />
might think, the inability to find a cause for the seizure<br />
is not necessary “bad.” In fact, this may portend a somewhat<br />
better prognosis for long-term seizure control.<br />
Febrile seizures are common in children <strong>and</strong> are covered<br />
in detail in Chapter 4.<br />
Trauma contributes to the risk of seizures in two<br />
fairly distinct fashions. Early posttraumatic seizures are<br />
typically associated with intracranial hemorrhage, focal<br />
neurological deficits, posttraumatic amnesia exceeding<br />
24 hours, <strong>and</strong> linear skull fractures. Late posttraumatic<br />
seizures are also associated with intracranial hemorrhage<br />
<strong>and</strong> posttraumatic amnesia exceeding 24 hours,<br />
but are usually seen in patients with depressed skull<br />
fractures <strong>and</strong> with the injury after age 16 years. 2–4<br />
A number of congenital malformations increase<br />
the risk for epilepsy. Disorders associated with migrational<br />
<strong>Seizures</strong> <strong>and</strong> <strong>Epilepsy</strong><br />
Paul R. Carney <strong>and</strong> James D. Geyer<br />
disorders <strong>and</strong> structural anomalies often increase the<br />
risk of subsequent seizures. The genetic diseases listed in<br />
Table 3-1 also increase the risk of epilepsy whether or not<br />
they are associated with structural malformations. 5–7<br />
Infections are also common causes of seizure<br />
activity in the pediatric population. Meningitis <strong>and</strong><br />
encephalitis can result in seizures either related to the<br />
fever or to the direct effects of the infection. These are<br />
covered in detail in the chapters on infectious disease.<br />
Bacterial infections can result in meningitis, encephalitis,<br />
<strong>and</strong> abscess formation. Herpes simplex virus (HSV) is a<br />
well known cause of seizures <strong>and</strong> can be catastrophic. 8<br />
Other viral infections including cytomegalovirus (CMV)<br />
infection <strong>and</strong> various viral encephalitides can result in<br />
seizures. Fungal infections <strong>and</strong> toxoplasmosis also raise<br />
the risk of developing seizures.<br />
A wide array of toxic <strong>and</strong> metabolic disorders can<br />
result in seizures. These derangements can cause<br />
seizures to occur de novo but can also worsen a preexisting<br />
epilepsy. The common metabolic <strong>and</strong> toxic<br />
causes of seizures are listed in Table 3-2.<br />
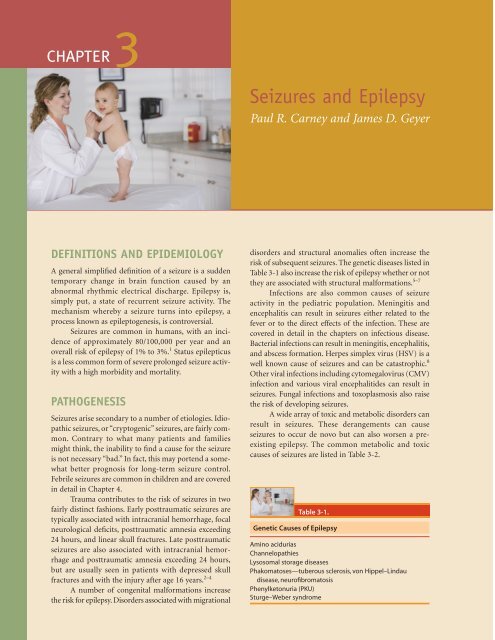
Table 3-1.<br />
Genetic Causes of <strong>Epilepsy</strong><br />
Amino acidurias<br />
Channelopathies<br />
Lysosomal storage diseases<br />
Phakomatoses—tuberous sclerosis, von Hippel–Lindau<br />
disease, neurofibromatosis<br />
Phenylketonuria (PKU)<br />
Sturge–Weber syndrome
Table 3-2.<br />
Toxic/Metabolic Causes of <strong>Seizures</strong><br />
Drug Intoxication<br />
Amphetamines<br />
Cocaine<br />
Lidocaine<br />
Theophylline<br />
Tricyclic antidepressants<br />
Drug withdrawal<br />
Antiepileptic drugs (AEDs)<br />
Barbiturates<br />
Benzodiazepines<br />
Ethanol<br />
Electrolyte—hypo/hypernatremia, hypo/hyperglycemia,<br />
hypocalcemia, hypomagnesemia<br />
Heavy metals—lead, mercury<br />
Hyperosmolarity<br />
Hypoxia<br />
Liver failure<br />
Porphyria<br />
Pyridoxine deficiency<br />
Thyroid storm<br />
Uremia (usually following 3 days of anuria)<br />
Cerebral ischemia is a common cause of seizures<br />
in the neonate <strong>and</strong> in the older adult but is relatively<br />
uncommon in the older pediatric population.<br />
<strong>Seizures</strong> usually occur in the more slowly growing<br />
tumors. Tumors located in the supratentorial region<br />
cause seizures more frequently than do cerebellar or<br />
brainstem tumors.<br />
CLINICAL PRESENTATION<br />
<strong>Epilepsy</strong> is divided into several categories with significant<br />
differences in the characteristics of the electrical discharges<br />
as well as the clinical manifestations. Localizationrelated<br />
epilepsy or partial epilepsy has a primary focus<br />
from which the electrical discharges arise. Complex partial<br />
seizures occur with alteration of awareness while<br />
simple partial seizures have no alteration of awareness.<br />
Jacksonian motor seizures, Rol<strong>and</strong>ic epilepsy, temporal<br />
lobe epilepsy, <strong>and</strong> frontal lobe epilepsy are all examples<br />
of partial epilepsy.<br />
The Revised International Classification of Epilepsies,<br />
Epileptic Syndromes <strong>and</strong> Related Seizure Disorders<br />
divides the localization-related epilepsies as follows: 10<br />
Idiopathic localization-related epilepsy<br />
Symptomatic or secondary localization-related<br />
epilepsy<br />
Cryptogenic localization-related epilepsy<br />
Generalized seizures are the other major seizure<br />
type. In this category of epilepsy, the seizure affects the<br />
entire cortex electrically. Several subtypes of generalized<br />
seizures have also been identified, including absence<br />
epilepsy with 3-Hz spike <strong>and</strong> wave activity, generalized<br />
tonic-clonic seizures, juvenile myoclonic epilepsy, <strong>and</strong><br />
progressive myoclonic epilepsy.<br />
The Revised International Classification of<br />
Epilepsies, Epileptic Syndromes <strong>and</strong> Related Seizure<br />
Disorders divides the generalized epilepsies as follows 10 :<br />
Primary generalized epilepsy<br />
Symptomatic generalized epilepsy<br />
Cryptogenic epilepsy<br />
A number of seizures <strong>and</strong> epilepsies may be very<br />
difficult to categorize. The Revised International Classification<br />
of Epilepsies, Epileptic Syndromes <strong>and</strong> Related<br />
Seizure Disorders groups these disorders in the “undetermined”<br />
category. These seizures may be divided as<br />
follows10 :<br />
Both focal <strong>and</strong> generalized<br />
Situation-related epilepsy<br />
Febrile convulsions<br />
Isolated seizure<br />
Isolated status epilepticus<br />
Toxic/metabolic<br />
In each of these cases, the electroencephalographic<br />
(EEG) findings may be different. The EEG<br />
serves as a vitally important tool in the correct diagnosis<br />
of the various epilepsy subtypes <strong>and</strong> syndromes.<br />
DIAGNOSIS<br />
Seizure Types<br />
CHAPTER 3 <strong>Seizures</strong> <strong>and</strong> <strong>Epilepsy</strong> ■ 31<br />
Generalized tonic-clonic seizures<br />
Generalized tonic-clonic seizures typically have no preceding<br />
aura but may have a prodrome of apathy or irritability.<br />
During the tonic phase, the jaw snaps shut followed<br />
by 10 to 15 seconds or longer of tonic spasms,<br />
apnea, <strong>and</strong> cyanosis. The clonic phase usually consists of<br />
1 to 2 minutes of rhythmic generalized muscle contractions<br />
<strong>and</strong> increased blood pressure. The postictal phase<br />
lasts for minutes to hours, with confusion, somnolence,<br />
<strong>and</strong> possibly agitation.<br />
The ictal EEG usually consists of generalized spike<br />
<strong>and</strong> wave or polyspike activity. The interictal EEG is<br />
highly variable with a normal background in some<br />
patients <strong>and</strong> slowing present in others.<br />
Generalized seizures are rare in newborns. Generalized<br />
seizures occur most frequently in children secondary<br />
to fevers <strong>and</strong> metabolic derangements.
32 ■ Section 2: Common Pediatric Neurologic Problems<br />
Absence seizures<br />
Absence seizures typically have no preceding aura or<br />
prodrome. An absence seizure usually lasts for only several<br />
seconds to minutes. There is a sudden interruption<br />
of consciousness, staring, 3-Hz blinking, <strong>and</strong> less frequently<br />
automatisms. There is no postictal confusion. 11<br />
The ictal EEG usually consists of 3-Hz generalized<br />
spike <strong>and</strong> wave activity with some slowing of the discharge<br />
frequency during the seizure. The interictal EEG<br />
usually has a normal background. Atypical absence<br />
seizures have generalized spike <strong>and</strong> wave activity but<br />
usually have a frequency less than 3 Hz. 12<br />
Absence seizures typically start between ages 4<br />
<strong>and</strong> 10 years <strong>and</strong> resolve by age 20 years. Atypical<br />
absence epilepsy usually occurs in children who are neurologically<br />
or developmentally abnormal. 13<br />
Febrile seizures<br />
Febrile seizures occur with a prodromal fever. A simple<br />
febrile seizure occurs as a brief generalized tonic clonic<br />
seizure occurring after the onset of fever. A complicated<br />
febrile seizure has prolonged seizure activity or focal<br />
seizure activity. Febrile seizures are covered in detail in<br />
Chapter 4.<br />
Juvenile myoclonic epilepsy<br />
The seizures associated with juvenile myoclonic epilepsy<br />
typically have no preceding aura but may have a prodrome<br />
of morning myoclonus. The seizures may consist<br />
of generalized tonic-clonic activity; however, absence<br />
seizures may also occur. The postictal phase is variable<br />
depending on the seizure type. 11<br />
The ictal EEG usually consists of generalized polyspike<br />
<strong>and</strong> slow wave activity. The interictal EEG is typically<br />
unremarkable. 12<br />
The age of onset of juvenile myoclonic epilepsy is<br />
typically 10 to 20 years. Patients are usually developmentally<br />
<strong>and</strong> neurologically normal. 13<br />
Progressive myoclonic epilepsy<br />
The family of disorders known as the progressive<br />
myoclonic epilepsies (Table 3-3) consists of a number of<br />
loosely related disorders. These epilepsy subtypes are quite<br />
rare <strong>and</strong> have complex presentations <strong>and</strong> diagnostic findings.<br />
Most of these disorders have a genetic basis, though<br />
sporadic cases have occurred in some cases (Table 3-4). The<br />
EEG associated with these disorders is variable. The background<br />
is often slow. The seizures are typically generalized. 11<br />
Infantile spasms<br />
West syndrome typically begins between 3 months <strong>and</strong><br />
3 years of age. 14–16 The seizures associated with West<br />
syndrome consist of a jack-knifing movement <strong>and</strong><br />
myoclonus. The EEG consists of a hypsarrhythmia pattern<br />
with bursts of asynchronous slow waves; spikes <strong>and</strong><br />
Table 3-3.<br />
Progressive Myoclonic Epilepsies<br />
Dentorubral-pallidoluysian atrophy<br />
Juvenile neuroaxonal atrophy<br />
Lafora disease<br />
Late infantile <strong>and</strong> juvenile GM2 gangliosidosis<br />
Myoclonic epilepsy <strong>and</strong> ragged red fibers (MERRF)<br />
Neuronal ceroid lipofuscinosis (NCL) (also known as Batten<br />
disease)<br />
Noninfantile Gaucher disease<br />
Sialidosis<br />
Unverricht–Lundborg disease (Baltic myoclonus)<br />
sharp waves alternate with a suppressed EEG. 17 The clinical<br />
features of West syndrome include infantile spasms<br />
<strong>and</strong> mental retardation, which varies according to the<br />
etiology of the spasms.<br />
Aicardi syndrome is an X-linked disorder present<br />
from birth that is associated with infantile spasms. The<br />
seizures are described as infantile spasms, but alternating<br />
hemiconvulsions may also be seen. The clinical features<br />
of Aicardi syndrome include coloboma, chorioretinal<br />
lacunae, agenesis of the corpus callosum,<br />
vertebral anomalies, <strong>and</strong> seizures. 18<br />
Lennox–Gastaut syndrome<br />
Lennox–Gastaut syndrome typically begins between 1<br />
<strong>and</strong> 10 years of age. There are multiple seizure types,<br />
associated with variable degrees of mental retardation.<br />
The EEG reveals a slow spike wave complex with<br />
a frequency of 1 to 2.5 Hz, multifocal spikes, <strong>and</strong> generalized<br />
paroxysmal fast activity (GPFA). 19<br />
Partial seizures: localization-related epilepsy<br />
Jacksonian motor seizures are simple partial seizures<br />
with no alteration of consciousness. These seizures<br />
begin with tonic contractions of the face, fingers, or feet<br />
<strong>and</strong> transform into clonic movements that march to<br />
other muscle groups on the ipsilateral hemibody. There<br />
is no alteration in consciousness, but postictal aphasia<br />
may occur if the primary epileptogenic zone involves<br />
the dominant hemisphere. Simple partial seizures may<br />
involve autonomic (Table 3-5), sensory, motor, or psychic<br />
functions.<br />
Complex partial seizures<br />
Benign Rol<strong>and</strong>ic epilepsy. Benign Rol<strong>and</strong>ic epilepsy<br />
usually begins between ages 5 <strong>and</strong> 10 years <strong>and</strong> is transmitted<br />
in an autosomal dominant pattern with variable<br />
penetrance. It is fairly common, with an incidence of
Table 3-4.<br />
Distinguishing Characteristics of the Progressive<br />
Myoclonic Epilepsies<br />
Clinical Features<br />
Chorea<br />
Dentorubral-pallidoluysian atrophy<br />
Juvenile neuroaxonal dystrophy<br />
Juvenile Gaucher disease<br />
Deafness<br />
Biotin-responsive encephalopathy<br />
MERRF<br />
Sialidosis type II<br />
Focal Occipital Spikes<br />
MERRF<br />
Unverricht–Lundborg disease<br />
Little or No Dementia<br />
Biotin-responsive encephalopathy<br />
Noninfantile Gaucher disease<br />
Myoclonus—nal failure<br />
Sialidosis type I<br />
Unverricht–Lundborg disease<br />
Severe Dementia<br />
GM2 gangliosidosis<br />
Juvenile neuroaxonal dystrophy<br />
Lafora disease<br />
Late infantile NCL<br />
Severe Myoclonus<br />
Lafora’s disease<br />
MERRF<br />
Sialidosis<br />
Genetics<br />
Autosomal Dominant<br />
Dentatorubral-pallidoluysian atrophy<br />
Kuf disease<br />
Geography<br />
Canada<br />
Myoclonus—renal failure<br />
Finl<strong>and</strong><br />
Santavori disease<br />
Unverricht–Lundborg disease<br />
Japan<br />
Dentatorubral pallidoluysian atrophy<br />
Sialidosis type II<br />
Sweden<br />
Gaucher disease<br />
Maternal Inheritance<br />
MERRF<br />
21/100,000 children. 20 The clinical features include a single<br />
nocturnal seizure with clonic movement of the mouth<br />
<strong>and</strong> gurgling. Secondary generalization is common.<br />
Alteration in consciousness, aura, <strong>and</strong> postictal confusion<br />
21, 22<br />
are rare. The seizures resolve by age 16 years.<br />
CHAPTER 3 <strong>Seizures</strong> <strong>and</strong> <strong>Epilepsy</strong> ■ 33<br />
Table 3-5.<br />
Possible Autonomic Seizure Clinical Features<br />
Abdominal sensations<br />
Apnea<br />
Arrhythmia<br />
Chest pain<br />
Cyanosis<br />
Erythema<br />
Flushing<br />
Genital sensations<br />
Hyperventilation<br />
Incontinence<br />
Miosis<br />
Perspiration<br />
Vomiting<br />
The interictal EEG consists of central <strong>and</strong> midtemporal<br />
high-amplitude spike <strong>and</strong> wave with a characteristic<br />
dipole. The ictal EEG usually consists of a focal<br />
central or mid-temporal ictal onset, with the possibility<br />
of secondary generalization. 23,24<br />
Temporal lobe epilepsy. Temporal lobe epilepsy<br />
accounts for approximately 70% of partial seizures.<br />
Many patients have a prior history of febrile seizures<br />
or head trauma. A prodrome consisting of lethargy is<br />
common. Auras are also common but not universal<br />
<strong>and</strong> include an array of findings such as déjà vu. The<br />
ictal findings or semiology include oral or motor<br />
automatisms, alteration of consciousness, head <strong>and</strong><br />
eye deviation, contralateral twitching or tonic–clonic<br />
movements, <strong>and</strong> posturing. Right temporal lobe<br />
seizures are often hypermobile. Left temporal lobe<br />
seizures often result in behavior arrest. Versive head<br />
movements are relatively common, <strong>and</strong> 90% of<br />
patients with versive head movements had a primary<br />
epileptogenic zone in the contralateral hemisphere.<br />
Ipsiversive movements are less common but occur<br />
most commonly in patients with temporal foci. The<br />
postictal phase consists of minutes to hours of confusion<br />
<strong>and</strong> somnolence. 24–30<br />
Frontal lobe epilepsy. Frontal lobe epilepsy accounts<br />
for approximately 20% of partial seizures. A prodrome<br />
is rare. Auras are unusual. The seizures typically consist<br />
of combinations of behavior alteration <strong>and</strong> automatisms<br />
of very brief duration. Frontal seizures often have<br />
atypical presentations <strong>and</strong> vary widely depending on<br />
the region of the frontal lobe from which the seizures<br />
arise (Table 3-6). Postictal confusion is rare. 31–36
34 ■ Section 2: Common Pediatric Neurologic Problems<br />
Table 3-6.<br />
Frequency of Aura Types by Location<br />
Temporal Frontal Occipital<br />
Aura Type (%) (%) (%)<br />
Auditory 10 0 0<br />
Cephalic 5 15 5<br />
Epigastric 50 15 5<br />
General 10 15 5<br />
Gustatory 10 0 10<br />
None 15 40 5<br />
Olfactory 10 0 10<br />
Psychical 15 5 15<br />
Somatosensory 5 15 0<br />
Visual 10 5 50<br />
Vertiginous 10 2 0<br />
Occipital lobe epilepsy. Occipital lobe epilepsy is rare,<br />
accounting for less than 10% of partial seizures. Prodromes<br />
are rare with occipital lobe seizures <strong>and</strong> auras<br />
are unusual. As with the frontal lobe seizures, the seizure<br />
characteristics are dependent on the area of the occipital<br />
lobe involved. When the striate cortex is involved,<br />
there are typically elemental visual hallucinations.<br />
Involvement of the lateral occipital lobe results in<br />
twinkling, pulsing lights. <strong>Seizures</strong> arising from the<br />
temporo-occipital are usually associated with formed<br />
visual hallucinations. 37-39<br />
Parietal lobe epilepsy. Parietal lobe seizures are also<br />
relatively uncommon. The may be seen as simple partial<br />
seizures but they will often propagate. The initial features<br />
can include contralateral paresthesias, contralateral<br />
pain, idiomotor apraxia, <strong>and</strong> limb movement sensations.<br />
As the seizure progresses <strong>and</strong> propagates, asymmetric<br />
tonic posturing <strong>and</strong> automatisms may develop. 40-42<br />
L<strong>and</strong>au–Kleffner syndrome. L<strong>and</strong>au–Kleffner syndrome<br />
is a rare, invariably progressive, idiopathic acquired aphasia<br />
related to a focal epileptic disturbance in the area of the<br />
brain responsible for verbal processing. 43 The syndrome<br />
begins between ages 3 <strong>and</strong> 10 in a child with normally<br />
acquired language abilities. The child then develops a<br />
verbal auditory agnosia <strong>and</strong> infrequent nocturnal partial<br />
or secondarily generalized seizures. The syndrome has a<br />
pathognomonic EEG pattern consisting of high-voltage<br />
multifocal spikes, predominating in the temporal lobes. 44<br />
Treatment is usually with valproic acid <strong>and</strong> benzodiazepines.<br />
45 Sometimes corticosteroids <strong>and</strong> IV Ig or even<br />
surgery with subpial transection 46 are used in refractory<br />
cases. The outcome for overall language <strong>and</strong> cognitive<br />
function depends in part on how early the syndrome is<br />
recognized <strong>and</strong> treated, but over 2/3 of children are left<br />
with significant language or behavioral deficits. 47<br />
Rasmussen encephalitis. Rasmussen encephalitis is a<br />
syndrome of diffuse lymphocytic infiltration of the brain<br />
associated with partial seizures <strong>and</strong> progressive neurological<br />
deterioration with hemiparesis. This disorder typically<br />
affects children 1 to 14 years old. The syndrome is associated<br />
with perivascular cuffing on pathologic sections, <strong>and</strong><br />
antibodies to the glutamate subunit GluR3 are commonly<br />
identified. The disorder is usually unilateral. Rasmussen<br />
encephalitis is very difficult to treat <strong>and</strong> frequently<br />
requires surgical management with hemispherectomy.<br />
EVALUATION<br />
As with many facets of neurology, the history is the<br />
most important diagnostic tool <strong>and</strong> should include<br />
information on each of the items in Table 3-7. The<br />
history should be obtained from family <strong>and</strong> eyewitnesses,<br />
if possible. Many patients are unable to provide<br />
accurate descriptions of the seizure <strong>and</strong> the postictal<br />
period.<br />
MRI of the head with temporal lobe protocol (thin<br />
coronal slices through hippocampi) is the preferred imaging<br />
modality for most patients. The MRI sequences are<br />
much more sensitive to the causes of epilepsy than is CT<br />
imaging. CT can, however, be of help in the emergency<br />
department setting. EEG is a vital component of the evaluation<br />
to categorize the seizure type <strong>and</strong> assist with planning<br />
of the treatment strategy. The need for laboratory<br />
testing is highly variable depending on the history. Initial<br />
evaluation with fluid balance profile (FBP), Ca++,<br />
Aura Types<br />
Table 3-7.<br />
Psychical Auras Illusion Hallucination<br />
Memory Déjà vu, jamais Flashbacks<br />
vu, strangeness<br />
Sound Advancing, receding, Voices, music<br />
louder, softer, clearer<br />
Self-image Depersonalization, Autoscopy<br />
remoteness<br />
Time St<strong>and</strong>-still, rushing,<br />
slowing<br />
Vision Macropsia, micropsia, Objects, faces,<br />
near, far, blurred scenes
Mg++, <strong>and</strong> liver function tests (LFTs) is important for<br />
both the search for a potential cause of the seizures <strong>and</strong><br />
for medication selection. Urine drug screening should be<br />
obtained for patients with new-onset seizures.<br />
TREATMENT<br />
Physicians <strong>and</strong> families often agonize over the decision<br />
about whether to initiate therapy after a single seizure.<br />
In the absence of a structural cause for the seizures or a<br />
typical syndrome of epilepsy, most patients do not<br />
require long-term treatment with an antiepileptic medication.<br />
The patient selection criteria for treatment after<br />
a single seizure are listed in Table 3-8. 48,49<br />
Stopping the antiepileptic medication can also<br />
be a challenge. The prognostic factors used for making<br />
the decision regarding discontinuation are listed in<br />
CHAPTER 3 <strong>Seizures</strong> <strong>and</strong> <strong>Epilepsy</strong> ■ 35<br />
Table 3-9.<br />
Components of a Seizure History<br />
Aura<br />
Birth <strong>and</strong> developmental history<br />
CNS infections<br />
Exacerbating factors (sleep, emotion, stress, menstrual cycle,<br />
substance abuse)<br />
Family history of epilepsy<br />
Head trauma<br />
Postictal state<br />
Seizure description by an eyewitness<br />
Table 3-9. 49 The selection of a particular antiepileptic medication<br />
for a given subtype of epilepsy has long been the<br />
subject of controversy. When selecting a given drug,<br />
the concomitant medical disorders such as headache,<br />
bone marrow dysfunction, <strong>and</strong> liver insufficiency<br />
should be considered. Guidelines for the selection of<br />
antiepileptic drugs, the pharmacology of the common<br />
Table 3-8.<br />
Characteristics of Frontal Lobe <strong>Seizures</strong> by Region of Onset<br />
Anteromedial Frontal<br />
Contralateral eye <strong>and</strong> head version<br />
Frequent generalization<br />
Somatosensory aura<br />
Tonic posture<br />
Cingular<br />
Amnesia<br />
Facial expressions of fear <strong>and</strong> anger<br />
“Psychotic” appearance<br />
Dorsolateral frontal<br />
Simple partial<br />
Tonic eye <strong>and</strong> head contraversion<br />
Frontopolar<br />
Loss of tone<br />
Rapid generalization<br />
Opercular/Insular<br />
Complex seizures include gagging, swallowing, chewing,<br />
amnesia, genital manipulation<br />
<strong>Seizures</strong> include gustatory sensation, salivation, gagging<br />
Orbitofrontal<br />
Blinking or staring<br />
Complex automatisms<br />
Supplementary Motor Area<br />
Contralateral tonic posture<br />
Simple motor seizure<br />
Somatosensory aura<br />
Tonic eye <strong>and</strong> head contraversion<br />
Vocalizes<br />
antiepileptic drugs, <strong>and</strong> potential interactions are<br />
reviewed in Tables 3-10 to 3-13. 50-53<br />
Surgery for epilepsy is an important but often<br />
underutilized treatment option. The surgical option<br />
provides an opportunity for some patients to become<br />
seizure free. However, this is a complex discussion <strong>and</strong><br />
beyond the scope of this book.<br />
Table 3-10.<br />
Patient Selection Criteria for Treatment After a Single<br />
Seizure<br />
Probably<br />
AVM<br />
Brain tumor<br />
CNS infection<br />
Immediate family history of epilepsy<br />
Probably Not<br />
Acute febrile illness<br />
Drug withdrawal or intoxication<br />
Electrolye imbalance<br />
EtOH withdrawal<br />
Hyper/hypoglycemia<br />
Immediate posttraumatic seizure<br />
Severe sleep deprivation–related seizure
36 ■ Section 2: Common Pediatric Neurologic Problems<br />
Table 3-11.<br />
Prognostic Factors for Stopping AEDs<br />
Favorable Unfavorable<br />
Primary generalized epilepsy Partial epilepsy<br />
Idiopathic epilepsy Identifiable lesions<br />
Childhood onset Adult onset<br />
Easy to control Difficult to control<br />
Normal neurological examination Abnormal neurologic<br />
examination<br />
Normal intelligence Mental retardation<br />
More than 2–3 years seizure-free Less than 3 years seizurefree<br />
Normal EEG Epileptiform EEG<br />
From Geyer J, Keating J, Potts D, Carney P, eds. Neurology for the Boards. 3rd ed.<br />
Philadelphia: Lippincott Williams & Wilkins; 2006.<br />
Non-epileptic Events<br />
Non-epileptic events are unusual in the pediatric population,<br />
especially in the younger child. Several categories<br />
of non-epileptic events (thrashing, staring, etc.) have<br />
different natural histories <strong>and</strong> variable prognosis. Etiologies<br />
include conversion disorder, malingering, <strong>and</strong><br />
medical conditions, especially cardiac disorders. Symptoms<br />
suggesting non-epileptic events include closed<br />
eyes, resisted eyelid opening, non-physiologic progression,<br />
pelvic thrusting, lack of cyanosis, lack of tongue<br />
biting, variable semiology, crying, <strong>and</strong> rapid reorientation<br />
following the event. 54-56<br />
Neonatal <strong>Seizures</strong><br />
Neonatal seizures are poorly classified, under-recognized,<br />
especially in sick neonates, <strong>and</strong> often difficult to treat.<br />
Table 3-12.<br />
Antiepileptic Drug Selection a<br />
Neonatal seizures are often the presenting clinical<br />
manifestation of underlying neurological conditions<br />
such as hypoxic-ischemic encephalopathy, stroke,<br />
intraventricular or intraparenchymal hemorrhages,<br />
meningitis, sepsis, or metabolic disorders. Of these,<br />
hypoxic ischemic encephalopathy is the most common<br />
etiology, accounting for 50% to 60% of patients with<br />
neonatal seizures. 57<br />
The neonatal brain is particularly vulnerable to<br />
seizure activity as a result of an imbalance of excitatory<br />
to inhibitory circuitry. The imbalance favors excitation,<br />
<strong>and</strong> does so to facilitate important developmental<br />
processes that occur during the neonatal period (synaptogenesis,<br />
apoptosis, progressive integration of circuitry,<br />
synaptic pruning). The imbalance occurs anatomically<br />
<strong>and</strong> physiologically by an overexpression of NMDA<br />
receptor in the hippocampus <strong>and</strong> neocortical regions of<br />
the neonatal brain, a delay in the maturation of the<br />
inhibitory system, <strong>and</strong> neurons in such regions as the<br />
hippocampus are excited rather than inhibited by the<br />
neurotransmitter GABA (normally the primary<br />
inhibitory neurotransmitter in the brain).<br />
Clinical presentation<br />
Subtle. Subtle seizures are more common in premature<br />
infants. As the name suggests, the seizures may be<br />
difficult to identify with only tonic horizontal eye movements,<br />
sustained eye opening, chewing, or apnea. In<br />
some cases there may be “boxing” movements. These<br />
seizures may have limited EEG changes correlating with<br />
the seizure activity. 58-61<br />
Clonic. Clonic seizures typically present as rhythmic,<br />
slow movements. The movements have a frequency of<br />
1 to 3 Hz. Focal clonic seizures involve one side of the<br />
body, <strong>and</strong> the infant is not clearly unconscious.<br />
Seizure Type VPA LTG TPM LVT ETX ACTH GBP CBZ PHT PHB<br />
Infantile spasms 1 2<br />
Absence 2 2 1<br />
Tonic-clonic 1 2 2 2 3 2 4, 1 bb<br />
Myoclonic 1 2<br />
Atypical absence 1 2<br />
Simple partial 3 2 2 2 1 2 1 bb<br />
Complex partial 2 2 2 2 2 1 2 1 bb<br />
aNumbers refer to order of preference for use in specific seizure types.<br />
bb<br />
Infants.<br />
From Geyer J, Keating J, Potts D, Carney P, eds. Neurology for the Boards. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2006.
Table 3-13.<br />
CHAPTER 3 <strong>Seizures</strong> <strong>and</strong> <strong>Epilepsy</strong> ■ 37<br />
Drug–Drug Interactions: Effects on Serum Concentration of Adding a Second Antiepileptic Drug to First<br />
Antiepileptic Drug<br />
Original Drug Added Drug<br />
Effects of Added Drug on Serum<br />
Concentration of Original Drug<br />
Carbamazepine Clonazepam No change<br />
Phenobarbital Decrease<br />
Phenytoin Decrease<br />
Primidone Decrease<br />
Clonazepam Phenobarbital Decrease<br />
Phenytoin Decrease<br />
Valproate No change<br />
Ethosuximide Carbamazepine Decrease<br />
Methylphenobarbital Increase<br />
Phenobarbital No change<br />
Phenytoin No change<br />
Primidone No change<br />
Valproate Increase or no change<br />
Phenobarbital Carbamazepine No change<br />
Clonazepam Data conflicting<br />
Methsuximide Increase<br />
Phenytoin Increase<br />
Valproate Increase<br />
Phenytoin Carbamazepine Increase or decrease<br />
Clonazepam Data conflicting<br />
Ethosuximide No change<br />
Methsuximide Increase<br />
Phenobarbital Decrease, increase, or no change<br />
Primidone No change<br />
Valproate Decrease<br />
Primidone Carbamazepine Increased concentration of derived phenobarbital<br />
Clonazepam No change<br />
Ethosuximide No change<br />
Phenytoin Increased concentration of derived phenobarbital<br />
Valproate Increase<br />
Valproate Carbamazepine Decrease, increase, or no change<br />
Clonazepam No change<br />
Ethosuximide No change<br />
Phenobarbital Decrease<br />
Phenytoin Decrease<br />
Primidone Decrease<br />
From Geyer J, Keating J, Potts D, Carney P, eds. Neurology for the Boards. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2006.<br />
Multifocal clonic seizures involve several body parts,<br />
often in a migrating pattern. Generalized clonic seizures<br />
are rarely observed in newborn because of the incomplete<br />
myelination of the brain. 58–61<br />
Tonic. Focal tonic seizures result in sustained posturing<br />
of a limb, the trunk, or the neck. These seizures are<br />
usually accompanied by EEG changes. Generalized<br />
tonic seizures exhibit tonic extension of all limbs<br />
(mimicking decorticate posturing) or tonic flexion of<br />
upper limbs <strong>and</strong> tonic extension of lower limbs (mimicking<br />
decerebrate posturing). There are no EEG<br />
changes in 85% of cases. 58–61<br />
Myoclonic. Focal myoclonic seizures usually involve<br />
flexor muscles of an upper extremity. Often, there are no<br />
EEG changes. Conversely, generalized myoclonic<br />
seizures exhibit bilateral jerks of both upper <strong>and</strong> lower<br />
limbs, <strong>and</strong> may resemble infantile spasms. These generalized<br />
seizures are more likely to have EEG changes. 58–61
38 ■ Section 2: Common Pediatric Neurologic Problems<br />
Syndromes<br />
Benign familial neonatal seizures<br />
Benign familial neonatal seizures occur as a genetic<br />
disorder with an autosomal dominant inheritance pattern<br />
associated with chromosome 20q. The seizures<br />
typically start on day of life 2 or 3. The neonate may<br />
have as many as 10 to 20 seizures per day. The syndrome<br />
is usually self-limited <strong>and</strong> benign, but approximately<br />
10% of cases progress to an antiepileptic<br />
drug-requiring seizure disorder. Neurological development<br />
is normal. 58–61<br />
Fifth-day fits<br />
Fifth-day fits usually begin on day of life 4 to 6. The<br />
seizures are typically multifocal clonic seizures <strong>and</strong> are<br />
frequently associated with apnea. The seizures usually<br />
last for less than 24 hours. Fifth-day fits progress to status<br />
epilepticus in 80% of cases. 58–61<br />
Benign neonatal sleep myoclonus<br />
Benign neonatal sleep myoclonus begins during the first<br />
week of life. The seizures are usually bilateral myoclonic<br />
jerks that last for several minutes <strong>and</strong> occur only during<br />
NREM sleep. The EEG is normal or slow. The seizures<br />
worsen with the administration of benzodiazepines. The<br />
seizures usually resolve within 2 months <strong>and</strong> neurological<br />
outcome is normal. 58–61<br />
Benign myoclonus of early infancy<br />
Benign myoclonus of early infancy has an onset at age 3<br />
to 9 months but it can be much earlier. The seizures<br />
resemble infantile spasms but the EEG is normal. The<br />
seizures usually occur while the patient is awake. The<br />
seizures disorder may continue for 1 to 2 years but neurological<br />
outcome is normal. 58–61<br />
Treatment<br />
The clinician should first search for underlying etiologies<br />
producing the seizures <strong>and</strong> treat (hypoglycemia,<br />
hypocalcemia, sepsis). If the clinician cannot find a<br />
readily identifiable <strong>and</strong> treatable etiology, the frontline<br />
agent of choice for treating seizures is phenobarbital<br />
(see Table 3-14 for dosing suggestions). 62 Phenobarbital<br />
as a single agent will stop seizure activity in 42% of<br />
patients. When the seizure does not respond to a single<br />
agent, phenytoin is added with an increase in efficacy to<br />
65%. Currently, fosphenytoin, the salt ester of phenytoin,<br />
is preferred in the neonate because it is an aqueous<br />
solution that is soluble in glucose-containing solutions,<br />
can be administered more quickly than phenytoin, <strong>and</strong><br />
will not cause “purple glove syndrome.” 62 Purple glove<br />
syndrome is necrosis or injury of the soft tissue that can<br />
occur with intravenous infusion of the highly alkaline<br />
phenytoin. The drug of choice for neonates in status is<br />
lorazepam. This agent has several properties that make<br />
it ideal—a long half-life <strong>and</strong> a small volume of distribution,<br />
which prolongs its retention at high levels in the<br />
brain.<br />
REFERENCES<br />
Table 3-14.<br />
Neonatal AED Dosing Suggestions<br />
Phenobarbital—20 mg/kg load over 10 to 15 min.<br />
If necessary add more phenobarbital in 5-mg/kg boluses<br />
Fosphenytoin—20 mg/kg at 1 mg/kg/min<br />
Ativan—0.1 mg/kg<br />
From Rennie J, Boylan G. Treatment of neonatal seizures. Arch Dis Child Fetal<br />
Neonatal 2007;92:F148–F150.<br />
1. Hauser WA, Beghi E. First seizure definitions <strong>and</strong> worldwide<br />
incidence <strong>and</strong> mortality. Epilepsia. 2008; 49(suppl 1):<br />
8-12.<br />
2. Teasell R, Bayona N, Lippert C, Villamere J, Hellings C.<br />
Post-traumatic seizure disorder following acquired brain<br />
injury. Brain Inj. 2007;21:201-214.<br />
3. Statler KD. Pediatric posttraumatic seizures: epidemiology,<br />
putative mechanisms of epileptogenesis <strong>and</strong> promising<br />
investigational progress. Dev Neurosci. 2006;28:<br />
354-363.<br />
4. Agrawal A, Timothy J, P<strong>and</strong>it L, Manju M. Post-traumatic<br />
epilepsy: an overview. Clin Neurol Neurosurg. 2006;<br />
108:433-439.<br />
5. Weber YG, Lerche H. Genetic mechanisms in idiopathic<br />
epilepsies. Dev Med Child Neurol. 2008;50:648-654.<br />
6. Leventer RJ, Guerrini R, Dobyns WB. Malformations of<br />
cortical development <strong>and</strong> epilepsy. Dialogues Clin Neurosci.<br />
2008;10:47-62.<br />
7. Steinlein OK. Genetics <strong>and</strong> epilepsy. Dialogues Clin Neurosci.<br />
2008;10:29-38.<br />
8. Griffith JF, Ch’ien LT. Herpes simplex virus encephalitis.<br />
Diagnostic <strong>and</strong> treatment considerations. Med Clin North<br />
Am. 1983;67:991-1008.<br />
9. Geyer J, Keating J, Potts D, Carney P, eds. Neurology for the<br />
Boards. 3rd ed. Philadelphia: Lippincott Williams &<br />
Wilkins;2006.<br />
10. Riviello JJ. Classification of seizures <strong>and</strong> epilepsy. Curr<br />
Neurol Neurosci Rep. 2003;3:325-331.<br />
11. Durón RM, Medina MT, Martínez-Juárez IE, et al.<br />
<strong>Seizures</strong> of idiopathic generalized epilepsies. Epilepsia.<br />
2005;46:34-47.<br />
12. Gardiner M. Genetics of idiopathic generalized epilepsies.<br />
Epilepsia. 2005;46(suppl 9):15-20.<br />
13. Jallon P, Latour P. Epidemiology of idiopathic generalized<br />
epilepsies. Epilepsia. 2005;46(suppl 9):10-14.
14. West WJ. On a peculiar form of infantile convulsions.<br />
Lancet. 1841;1:724-725.<br />
15. Wong M, Trevanthan E. Infantile spasms Pediatr Neurol.<br />
2001;24:89-98.<br />
16. Riikonen R. The latest on infantile spasms. Curr Opin<br />
Neurol. 2005;18:91-95.<br />
17. Hrachovy RA, Frost JD Jr. Infantile epileptic encephalopathy<br />
with hypsarrhythmia (infantile spasms/West syndrome).<br />
J Clin Neurophysiol. 2003;20:408-425.<br />
18. Aicardi J. Aicardi syndrome. Brain Dev. 2005;27:164-171.<br />
19. Mark<strong>and</strong> ON. Lennox–Gastaut syndrome (childhood<br />
epileptic encephalopathy). J Clin Neurophysiol. 2003;20:<br />
426-441.<br />
20. Neubauer BA, Hahn A, Stephani U, Doose H. Clinical<br />
spectrum <strong>and</strong> genetics of Rol<strong>and</strong>ic epilepsy. Adv Neurol.<br />
2002;89:475-479.<br />
21. Camfield P, Camfield C. Epileptic syndromes in childhood:<br />
clinical features, outcomes, <strong>and</strong> treatment. Epilepsia.<br />
2002;43(suppl 3):27-32.<br />
22. Saint-Martin AD, Carcangiu R, Arzimanoglou A, et al.<br />
Semiology of typical <strong>and</strong> atypical Rol<strong>and</strong>ic epilepsy: a<br />
video-EEG analysis. Epileptic Disord. 2001;3:173-182.<br />
23. Kellaway P. The electroencephalographic features of<br />
benign centrotemporal (rol<strong>and</strong>ic) epilepsy of childhood.<br />
Epilepsia. 2000;41:1053-1056.<br />
24. Rodriguez AJ, Buechler RD, Lahr BD, So EL. Temporal<br />
lobe seizure semiology during wakefulness <strong>and</strong> sleep.<br />
<strong>Epilepsy</strong> Res. 2007;74:211-214.<br />
25. Maillard L, Vignal JP, Gavaret M, et al. Semiologic <strong>and</strong><br />
electrophysiologic correlations in temporal lobe seizure<br />
subtypes. Epilepsia. 2004;45:1590-1599.<br />
26. Hoffmann JM, Elger CE, Kleefuss-Lie AA. Lateralizing<br />
value of behavioral arrest in patients with temporal lobe<br />
epilepsy. <strong>Epilepsy</strong> Behav. 2008;13(4):634-636.<br />
27. Marks WJ Jr, Laxer KD. Semiology of temporal lobe<br />
seizures: value in lateralizing the seizure focus. Epilepsia.<br />
1998;39:721-726.<br />
28. Geyer JD, Payne TA, Faught E, Drury I. Postictal noserubbing<br />
in the diagnosis, lateralization, <strong>and</strong> localization of<br />
seizures. Neurology. 1999;52:743-745.<br />
29. French JA, Williamson PD, Thadani VM, et al. Characteristics<br />
of mesial temporal lobe epilepsy. I. Results of history<br />
<strong>and</strong> physical examination. Ann Neurol. 1983;34:<br />
374-380.<br />
30. Geyer JD, Bilir E, Faught RE, et al. Significance of<br />
interictal temporal lobe delta activity for localization<br />
of the primary epileptogenic region. Neurology.1999;<br />
52:202-205.<br />
31. O’Brien TJ, Mosewich RK, Britton JW, Cascino GD, So EL.<br />
History <strong>and</strong> seizure semiology in distinguishing frontal<br />
lobe seizures <strong>and</strong> temporal lobe seizures. <strong>Epilepsy</strong> Res.<br />
2008;82(2-3):177-182.<br />
32. Battaglia D, Lettori D, Contaldo I, et al. Seizure semiology<br />
of lesional frontal lobe epilepsies in children. Neuropediatrics.<br />
2007;38:287-291.<br />
33. Lee JJ, Lee SK, Lee SY, et al. Frontal lobe epilepsy: clinical<br />
characteristics, surgical outcomes <strong>and</strong> diagnostic modalities.<br />
Seizure. 2008;17:514-523.<br />
34. Bonelli SB, Lurger S, Zimprich F, Stogmann E, Assem-<br />
Hilger E, Baumgartner C. Clinical seizure lateralization in<br />
frontal lobe epilepsy. Epilepsia. 2007;48:517-523.<br />
CHAPTER 3 <strong>Seizures</strong> <strong>and</strong> <strong>Epilepsy</strong> ■ 39<br />
35. Bleasel A, Kotagal P, Kankirawatana P, Rybicki L. Lateralizing<br />
value <strong>and</strong> semiology of ictal limb posturing <strong>and</strong> version<br />
in temporal lobe <strong>and</strong> extratemporal epilepsy. Epilepsia.<br />
1997;38:168-174.<br />
36. Gardella E, Rubboli G, Tassinari CA. Ictal grasping: prevalence<br />
<strong>and</strong> characteristics in seizures with different semiology.<br />
Epilepsia. 2006;47(suppl 5):59-63.<br />
37. Taylor I, Berkovic SF, Kivity S, Scheffer IE. Benign occipital<br />
epilepsies of childhood: clinical features <strong>and</strong> genetics.<br />
Brain. 2008;131:2287-2294.<br />
38. Ludwig, BI, Ajmone-Marsan C. Clincial ictal patterns in<br />
epileptic patients with occipital electroencephalographic<br />
foci. Neurology. 1975;25:463-471.<br />
39. Blume WT, Wiebe S, Tapsell LM. Occipital epilepsy: lateral<br />
versus mesial. Brain. 2005;128:1209-1225.<br />
40. Kim DW, Lee SK, Yun CH, et al. Parietal lobe epilepsy: the<br />
semiology, yield of diagnostic workup, <strong>and</strong> surgical outcome.<br />
Epilepsia. 2004;45:641-649.<br />
41. Cascino GD, Hulihan JF, Sharborough FW, Kelly PJ. Parietal<br />
lobe lesional epilepsy: electroclinical correlation <strong>and</strong><br />
operative outcome. Epilepsia. 1993;34:522-527.<br />
42. Williamson PD, Boon PA, Thadani VM, et al. Parietal lobe<br />
epilepsy: diagnostic considerations <strong>and</strong> results of surgery.<br />
Ann Neurol. 1992;31:193-201.<br />
43. Hirsh E, Valenti MP, Rudolf G, et al. L<strong>and</strong>au–Kleffner syndrome<br />
is not an eponymic badge of ignorance. <strong>Epilepsy</strong><br />
Res. 2006;70:S239-S247.<br />
44. L<strong>and</strong>au WM, Kleffner FR. Syndrome of acquired aphasia<br />
with convulsive disorder in children. Neurology. 1957;<br />
7:523-530.<br />
45. Mikati MA, Shamseddine AN. Management of L<strong>and</strong>au–<br />
Kleffner syndrome. Pediatric Drugs. 2005;7:377-389.<br />
46. Morrell F, Whisler WW, Smith MC, et al. L<strong>and</strong>au–Kleffner<br />
syndrome: treatment with subpial intracortical transaction.<br />
Brain. 1995;118:1529-1546.<br />
47. Beaumanoir A. The L<strong>and</strong>au–Kleffner syndrome. In :<br />
Roger J, Bureau M, Dravet C, et al., eds. Epileptic Syndromes<br />
in Infancy, Childhood <strong>and</strong> Adolescence. London;<br />
John Libbey;1992:231-243.<br />
48. Berg AT, Shinnar S. The risk of seizure recurrence following<br />
a first unprovoked seizure: a quantitative review. Neurology.<br />
1991;41:965-972.<br />
49. Hughes JR, Fino JJ. Focal seizures <strong>and</strong> EEG: prognostic considerations.<br />
Clin Electroencephalogr. 2003;34:174-181.<br />
50. Riikonen R. Infantile spasms: therapy <strong>and</strong> outcome. J<br />
Child Neurol. 2004;19:401-404.<br />
51. Mackay MT, Weiss SK, Adams-Webber T, et al., for the<br />
American Academy of Neurology; Child Neurology Society.<br />
Practice parameter: medical treatment of infantile<br />
spasms: report of the American Academy of Neurology<br />
<strong>and</strong> the Child Neurology Society. Neurology. 2004;<br />
62:1668-1681.<br />
52. Sato S, White BG, Penry JK, et al. Valproic acid vs ethosuximide<br />
in the treatment of absence seizures. Neurology.<br />
1982;32(2):157-163.<br />
54. Selwa LM, Geyer J, Nikakhtar N, Brown MB, Schuh LA,<br />
Drury I. Nonepileptic seizure outcome varies by type of<br />
spell <strong>and</strong> duration of illness. Epilepsia. 2000;41:1330-1334.<br />
55. Geyer JD, Payne TA, Drury I. The value of pelvic thrusting<br />
in the diagnosis of seizures <strong>and</strong> pseudoseizures. Neurology.<br />
2000;54:227-229.
40 ■ Section 2: Common Pediatric Neurologic Problems<br />
56. Duncan R, Oto M, Russell AJ, Conway P. Pseudosleep<br />
events in patients with psychogenic non-epileptic<br />
seizures: prevalence <strong>and</strong> associations. J Neurol Neurosurg<br />
Psychiatry. 2004;75:1009-1012.<br />
57. Tuxhorn I, Kotagal P. Classification. Semin Neurol.<br />
2008;28:277-288.<br />
58. Nabbout R, Dulac O. Epileptic syndromes in infancy<br />
<strong>and</strong> childhood. Curr Opin Neurol. 2008;21:161-166.<br />
59. Tich SN, d’Allest AM, Villepin AT, et al. Pathological features<br />
of neonatal EEG in preterm babies born before 30 weeks of<br />
gestational age. Neurophysiol Clin. 2007;37: 325-370.<br />
60. Silverstein FS, Jensen FE. Neonatal seizures. Ann Neurol.<br />
2007;62:112-120.<br />
61. Specchio N, Vigevano F. The spectrum of benign infantile<br />
seizures. <strong>Epilepsy</strong> Res. 2006;70(suppl 1):S156-S167.<br />
62. Rennie J, Boylan G. Treatment of neonatal seizures. Arch<br />
Dis Child Fetal Neonatal Ed. 2007;92:F148-F150.