Gram-negative facultative anaerobe rods (Enterobacteriaceae)
Gram-negative facultative anaerobe rods (Enterobacteriaceae)
Gram-negative facultative anaerobe rods (Enterobacteriaceae)
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
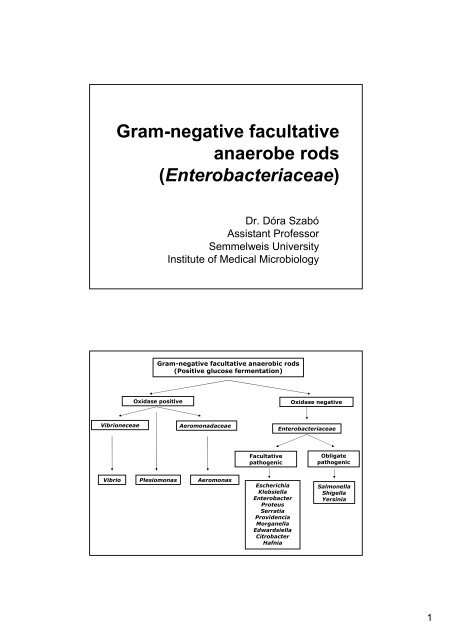
<strong>Gram</strong>-<strong>negative</strong> <strong>facultative</strong><br />
<strong>anaerobe</strong> <strong>rods</strong><br />
(<strong>Enterobacteriaceae</strong>)<br />
Dr. Dóra Szabó<br />
Assistant Professor<br />
Semmelweis University<br />
Institute of Medical Microbiology<br />
<strong>Gram</strong>-<strong>negative</strong> <strong>facultative</strong> anaerobic <strong>rods</strong><br />
(Positive glucose fermentation)<br />
Oxidase positive Oxidase <strong>negative</strong><br />
Vibrioneceae Aeromonadaceae<br />
Vibrio Plesiomonas<br />
Aeromonas<br />
Facultative<br />
pathogenic<br />
Escherichia<br />
Klebsiella<br />
Enterobacter<br />
Proteus<br />
Serratia<br />
Providencia<br />
Morganella<br />
Edwardsiella<br />
Citrobacter<br />
Hafnia<br />
<strong>Enterobacteriaceae</strong><br />
Obligate<br />
pathogenic<br />
Salmonella<br />
Shigella<br />
Yersinia<br />
1
Salmonellae<br />
The genus Salmonella was named after<br />
Daniel Elmer Salmon, an American veterinary<br />
pathologist.<br />
While Theobald Smith was the actual<br />
discoverer of the bacteria that causes hog<br />
cholera (Salmonella enterica var.<br />
Choleraesius)<br />
Salmon was the administrator of the USDA<br />
research program and thus the organism was<br />
named after him.<br />
2
Salmonella classification<br />
Classification has been changing in the last few years. Based on<br />
genetic backgound, there two species<br />
S. enteritica, and 7 subspecies: 1, 2 ,3a ,3b ,4 ,5, and 6.<br />
S. bongori<br />
- S. enteritica subgroup 1has only medical importance<br />
- The other subspecies and S. bongori are the parasites of<br />
vertabrae<br />
- 1500 serotypes belong to S. enteritica subgroup 1<br />
- Only cc 12 responsible for most of the human infections<br />
- Earlier these serotypes had their own name: for example: S.<br />
enteritidis, S. typhimurium, S. typhi<br />
Phase variation of Salmonella<br />
3
Biochemistry and serology<br />
Clinically Salmonella isolates are often still reported out as serogroups or<br />
serotypes based on the Kauffman-White scheme of classification.Based<br />
on O and H (flagella) antigens.<br />
O antigens<br />
O antigens are vary variable<br />
Mozaik stucture<br />
Epitop combination, special antigens of the isolate<br />
The H (flagella) antigens<br />
H antigens has a mozaik structure as well<br />
occur in two phases; 1 and 2 and only 1 phase is expressed at a given<br />
time<br />
Polyvalent antisera is used followed by group specific antisera (A, B, C1, C2,<br />
D, and E)<br />
Salmonella typhi also has a Vi antigen which is a capsular antigen.<br />
For serotyping<br />
To determinate the O antigen<br />
To deteminate H (flagella) antigen<br />
To detect the presence or absence Vi antigen<br />
Salmonella<br />
Biochemistry<br />
TSI K/A + gas and H 2 S: S. typhi produces only a<br />
small amount of H 2 S and no gas , and S. paratyphi A<br />
produces no H 2 S<br />
Urea –<br />
Motility +<br />
Citrate +/-<br />
Indole -<br />
4
Salmonella virulence factors<br />
Type III secretion systems and effector molecules – 2<br />
different systems may be found:<br />
One type is involved in promoting entry into intestinal<br />
epithelial cells<br />
The other type is involved in the ability of Salmonella to<br />
survive inside macrophages<br />
Outer membrane proteins - involved in the ability of<br />
Salmonella to survive inside macrophages<br />
Flagella – help bacteria to move through intestinal<br />
mucous<br />
Enterotoxin - may be involved in gastroenteritis<br />
Iron capturing ability<br />
Endotoxin – may play a role in intracellular survival<br />
Capsule (for S. typhi and some strains of S. paratyphi)<br />
Adhesions – both fimbrial and non-fimbrial<br />
Host specificity<br />
Wide host specificity<br />
normal flora in the GI of animal<br />
in human can cause gastroenteritis; zoonosis<br />
S. enteritidits S. typhimurium<br />
Adapted to animal<br />
Serious infection in animal<br />
focal infection in human (mainly kids)<br />
S. cholerasuis<br />
Adapted to human<br />
only in human<br />
S. typhi, S. paratyphi A, B, and C<br />
5
Clinical Significance<br />
Gastroenteritis.<br />
the Salmonella multiply and their presence induces a strong<br />
inflammatory response which causes most of the symptoms seen in<br />
gastroenteritis (mild to moderate fever with diarrhea and abdominal<br />
cramps).<br />
The inflammatory response prevents the spread beyond the GI tract<br />
and eventually kills the bacteria.<br />
Enteric fevers<br />
In enteric fevers (typhoid and paratyphoid) the Salmonella<br />
disseminate before they multiply to high enough levels to stimulate a<br />
strong inflammatory response so the initial symptoms are only a lowgrade<br />
fever and constipation.<br />
GASTROENTERITIS<br />
6
Salmonella-gastroenteritis<br />
Clinical picture<br />
18-48 hours incubation<br />
GASTROENTERITIS, but can be:<br />
dizziness<br />
vomiting<br />
Abdominal pain<br />
The symptoms can be similar to dysentery<br />
The symptoms moderate in a few days<br />
spontan recovery in a week<br />
INVASIVE INFECTION<br />
Sepsis<br />
Meningitis<br />
in very young, or very old, as well as immunocompromised patients<br />
7
Salmonella-gastroenteritis<br />
Epidemiology<br />
The most common cause of foodpoisoning<br />
More than 15 000 know cases per year in Hungary<br />
1-10% of the real cases<br />
Increasing incidence<br />
ZOONOSIS!!<br />
Reservoirs:<br />
Chicken –and duck eggs<br />
Chicken and swine<br />
Insufficient heat treatment is necessary<br />
Salmonella-gastroenteritis<br />
Pathogenesis I.<br />
Mechanism<br />
Bacteria adhere to the epithelial cells<br />
Membrane ruffles will be evolved<br />
The cell incorpotare the bacteria<br />
The role of enterotoxins are not<br />
confirmed<br />
Increased secration because of the<br />
local inflammation<br />
The strains habouring a big plasmid<br />
The size is specific for serotype<br />
Coding serumresistance and survival<br />
in phagocytes<br />
Role in gastroenteritis is not confimed<br />
Role in invasive infections<br />
8
Salmonella-gastroenteritis<br />
Pathogenesis II.<br />
Transient bacteraemia can occur<br />
Permanent bacteraemia:<br />
Very old patient<br />
Very young patient<br />
Immunsuppressed and AIDS patient<br />
Focal infections can occur<br />
lung<br />
brain<br />
In atherosclerotic plaque of aorta<br />
prothesis<br />
Salmonella-gastroenteritis<br />
Pathogenesis III.<br />
Asymptomatic carriers<br />
After recovery carrier status<br />
That patient can be a source of infection later<br />
9
Special characteristics of S.<br />
cholerasuis<br />
The general properties are similar to the<br />
other Salmonella species<br />
S. cholerasuis is tend to cause septic clinical<br />
picture<br />
Microbiological diagnosis<br />
Clinical specimen:<br />
faeces : positive from first week, and may remain + for several weeks<br />
blood for blood-culture: just in 2-4 % (+)<br />
CSF, and food leftover<br />
Direct smear has no value in the diagnosis.<br />
Culture:<br />
Samples are inoculated onto brilliant green and/or bismuth sulphite<br />
selective media.<br />
10
Brillant-green culture media<br />
brillant green – for selection<br />
lactose, dextrose, sacharose<br />
Andrade indicator<br />
(acidic pH → -<br />
Salmonella lactose neg.– no colour<br />
- E. coli lactose+ - red)<br />
Bismuth-sulphite<br />
brillant green – for selection<br />
bismuth salt + sodium sulphite<br />
→ Salmonella H2S production<br />
⇒ Bismuth sulphide (black)<br />
Microbiological diagnosis<br />
n Biochemical identification: (refer to<br />
flow charts) Lactose (-), dextrose<br />
fermentation w/o gas formation, H2S (+)<br />
n Serological identification:<br />
Slide agglutination with specific<br />
antibodies<br />
11
Epidemiological investigations<br />
For strain with similar biochemical and<br />
serological pattern!<br />
Phag typing<br />
Molecular methods<br />
PCR-s (arbritary primed (AP)-PCR, ERIC-PCR)<br />
Pulse-field gel-electrophoresis PFGE<br />
rRNS sequencing<br />
Phage typing<br />
n phage typing of a strain of<br />
Salmonella is done in<br />
epidemiological studies<br />
n the surface of the plate is<br />
inoculated with a broth<br />
culture<br />
n a number of phages are<br />
spotted on the plate<br />
n after incubation the phage<br />
type is determined by the<br />
pattern of lyses<br />
12
Pulde field gel electrophoresis (PFGE)<br />
Therapy<br />
The vast majority of enterocolitis cases do not require<br />
an antibiotic treatment.<br />
After antibiotic treatment carrier status occurs more<br />
frequently.<br />
Antimicrobial treatment of Salmonella infection of<br />
neonates, as well as invasive salmonella infections is<br />
important.<br />
ampicillin<br />
sulfomethoxazole + trimethoprim<br />
fluoroquinolons<br />
3rd generation cephalosporins<br />
susceptibility tests are important<br />
13
1984 Rajneeshee bioterror attack<br />
1984 Rajneeshee bioterror attack<br />
The 1984 Rajneeshee bioterror attack was the food poisoning<br />
ímore than 750 individuals in The Dalles, Oregon, United States<br />
through the contamination of salad bars at ten local restaurants with<br />
salmonella.<br />
A leading group of followers of Osho, then known as Bhagwan<br />
Shree Rajneesh, had hoped to incapacitate the voting population of<br />
the city so that their own candidates would win the 1984 Wasco<br />
County elections.<br />
The incident was the first bioterrorism attack in the United States,<br />
and the single largest bioterrorist attack in United States history.<br />
The attack is one of only two confirmed terrorist uses of biological<br />
weapons to harm humans.<br />
14
Seven hundred and fifty one people<br />
contracted salmonellosis as a result of the<br />
attack, of whom 45 were hospitalized.<br />
There were no fatalities.<br />
Although an initial investigation by the<br />
Oregon Public Health Division and the<br />
Centers for Disease Control did not rule out<br />
deliberate contamination, the actual source of<br />
the contamination was only discovered a year<br />
later.<br />
Enteric fever<br />
15
Salmonella typhi, S. paratyphi A, B, C<br />
gripsdb.dimdi.de<br />
Human pathogen<br />
Antigen<br />
O<br />
H<br />
Vi Ag<br />
Salmonella typhi, S. paratyphi A, B, C<br />
Figure 1. Salmonella typhi, the agent<br />
of typhoid. <strong>Gram</strong> stain. (CDC)<br />
www.textbookofbacteriology.net<br />
Figure 2. Flagellar stain of a Salmonella<br />
Typhi. Like E. coli, Salmonella are motile<br />
by means of peritrichous flagella. A close<br />
relative that causes enteric infections is<br />
the bacterium Shigella. Shigella is not<br />
motile, and therefore it can be<br />
differentiated from Salmonella on the bais<br />
of a motility test or a flagellar stain. (CDC)<br />
16
Thyphoid fever<br />
caused by S. typhi<br />
a S. paratyphi A, B and C cause the<br />
paratyphus<br />
Milder disease<br />
The source is always human!!<br />
Pathogenesis<br />
First period is the PRIMER BACTERAEMIA<br />
After oral infection the incubation period is two<br />
weeks<br />
Bacteria get through mucosa via the M cells of Peyer<br />
plaques<br />
Infect the local macrophages<br />
S. typhi has no serotype-specific plasmid<br />
Chromosomal genes for survival in<br />
macrophages<br />
Macrophages deliver the bacteria to the mesentarial<br />
lymph nodes<br />
Through the ductus thoracicus and blood stream the<br />
bacteria get to spleen, liver, kidney, lung<br />
The CFU is low<br />
The patient is asymptomatic or subfebrile<br />
SECUNDER BACTERAEMIA<br />
Bacteria multiply in RES<br />
Mainly in Kupffer-cells<br />
Getting out the bactera there is a bacteraemia with<br />
high CFU<br />
Perforation of the terminal ileum and proximal colon<br />
Through bile back to the intestine multiplication in the Payer’s<br />
patches ulceration → bleeding → perforation<br />
Permanent carrier stage<br />
From bile<br />
17
Salmonella<br />
The bacteria move via the lymphatics and bloodstream to the<br />
liver and spleen where phagocytosis and multiplication occurs.<br />
The bacteria re-enter the bloodstream to disseminate throughout<br />
the body to all organs causing fever, headaches, myalgia, and<br />
GI problems.<br />
Rose spots (erythematous, muculopapular lesions) are seen on<br />
the abdomen. Osteomyelitis, cystitis, and gall bladder infections<br />
may occur.<br />
Symptoms of paratyphoid fevers (due to S. paratyphi A, B, or C)<br />
are similar to but less severe than those that occur with typhoid<br />
fever (due to S. typhi)<br />
Clinical signs<br />
headache<br />
fever<br />
Very high in a few days<br />
The sense is typhosus<br />
relative bradycardia<br />
hepatosplenomegalia<br />
Gastroenteritis is NOT characteristic<br />
Roseolas on the chest and abdomen<br />
Blood is characteristic<br />
leukopenia<br />
aneosinophilia<br />
lymphocytosis<br />
18
Typhoid fever (a: petechia, Peyer plaque(b) and necrosis<br />
of the ileum (c), d: perforation of the Peyer-plaque<br />
Typhus abdominalis<br />
Τψπηυσ Τψπηυσ αβδοµιναλισ<br />
gripsdb.dimdi.de<br />
19
Rose spots on abdomen of a patient with typhoid fever<br />
due to the bacterium Salmonella typhi. www.wrongdiagnosis.com<br />
Rose spots on the chest of a patient with typhoid fever<br />
due to the bacterium Salmonella typhi. www.wrongdiagnosis.com<br />
20
Fig. 4.37 Typhoid fever. Numerous ulcers of the small intestine<br />
overlying hyperplastic lymphoid follicles (Peyer’s patches). By courtesy<br />
of Dr. J. Newman.<br />
Fig. 4.39 Typhoid fever. Mononuclear cells and red blood cells in the<br />
stool. Trichrome stain. By courtesy of Dr. H.L. DuPont.<br />
21
Microbiological diagnosis<br />
Clinical specimen:<br />
faeces: positive from the second or third weeks<br />
urine : positive from the second week<br />
bile, bone marrow aspirate<br />
blood for blood-culture : often positive in the first week<br />
Direct smear has no value in the diagnosis.<br />
Culture:<br />
Samples are inoculated onto brilliant green and/or bismuth sulphite<br />
selective media.<br />
Biochemical identification: (refer to flow charts) Lactose<br />
(-), dextrose fermentation w/o gas formation, H2S (+)<br />
Serological identification:<br />
Slide agglutination with specific antibodies to show<br />
presence of S. typhi cells in the culture.<br />
22
Blood serology:<br />
=> Gruber-Widal reaction (Widal`s type tube agglutination): (Ag =<br />
'H' as well as 'O' antigens of the laboratory strain of S. typhi) to<br />
show presence and establish titre of specific antibodies in the<br />
patients` sera.<br />
Treatment<br />
Antibiotics according to susceptibility tests: S. typhi strains are usually susceptible<br />
to<br />
ampicillin,<br />
sulfomethoxazole + trimethoprim,<br />
3rd generation cephalosporins.<br />
Prevention<br />
Specific sanitary measures and control of chronic carriers.<br />
Active immunisation with acetone killed bacterial suspension administered<br />
parenterally is available for high-risk individuals.<br />
An orally administered vaccine of a live avirulent mutant of S. typhi also provides<br />
significant protection.<br />
“Carriers”<br />
3 % of survivors of typhoid become permanent carriers, harboring the organisms<br />
in the gallbladder, biliary tract or urinary tract.<br />
23
Geographical distribution of<br />
the typhoid fever<br />
24
E. coli intestinal infections<br />
Gastroenteritis – there are several<br />
distinct types of E. coli that are<br />
involved in different types of<br />
gastroenteritis:<br />
enterotoxigenic E. coli (ETEC),<br />
enteroinvasive E. coli (EIEC),<br />
enteropathogenic E. coli (EPEC) ,<br />
enteroaggregative E. coli (EAEC),<br />
and<br />
enterohemorrhagic E. coli (EHEC).<br />
ETEC – enterotoxigenic E. coli<br />
Pathogenesis<br />
The organism attaches to the intestinal mucosa<br />
(mainly in small intestine) via colonization factors<br />
(CFA) and then liberates enterotoxin.<br />
Specific to human small intestine<br />
like CFA I, II, III<br />
Structure: :<br />
fimbria<br />
fibrilla<br />
afimbria adhezin<br />
Good antigens, the antibody<br />
Imhibit the adhesion<br />
Good for detection<br />
Enterotoxins – produced by enterotoxigenic strains of<br />
E. coli (ETEC). Causes a movement of water and ions<br />
from the tissues to the bowel resulting in watery<br />
diarrhea. There are two types of enterotoxin:<br />
LT – is heat labile and binds to specific Gm 1<br />
gangliosides on the epithelial cells of the small<br />
intestine where it ADP-ribosylates Gs which stimulates<br />
adenylate cyclase to increase production of cAMP.<br />
Increased cAMP alters the activity of sodium and<br />
chloride transporters producing an ion imbalance that<br />
results in fluid transport into the bowel.<br />
ST – is heat stable, affects the cGMP system.<br />
25
E. coli gastroenteritis<br />
ETEC – enterotoxigenic E. coli<br />
Clinical picture<br />
In developing countries the most common cause of<br />
diarrhea of young kids, less than two years<br />
is a common cause of traveler’s diarrhea<br />
The diarrhea is severe, cholera-like<br />
The disease is characterized by a watery diarrhea,<br />
nausea, abdominal cramps and low-grade fever for<br />
1-5 days.<br />
Transmission is via contaminated food or water.<br />
No specific histology<br />
E. coli gastroenteritis<br />
ETEC – enterotoxigenic E. coli<br />
Diagnostic<br />
Serotyping is not good for diagnostis, lots of<br />
serotype<br />
In vivo animal study<br />
LT in rabbit<br />
ST in newborn mice<br />
Not routine<br />
LT-sensitive cell culture<br />
ELISA for LT and ST<br />
Molecular biology methods for toxins or CFA :<br />
hybridization or PCR<br />
26
Enteropathogenic E. coli (EPEC)<br />
The diarrhea with large amounts of mucous<br />
without blood or pus occurs along with<br />
vomiting, malaise and low grade fever.<br />
Age-specific: just under 1 year old<br />
Adults can be infected with high dose<br />
In developing countries<br />
20 % of diarrheae in hospitalized infants<br />
In fifties, sixties outbreaks is developed countries<br />
Only sporadic<br />
EPEC – enteropathogenic E. coli<br />
Bundle forming pili are involved in<br />
attachment to the intestinal<br />
mucosa.<br />
This leads to changes in signal<br />
transduction in the cells,<br />
effacement of the microvilli, and<br />
to intimate attachment via a nonfimbrial<br />
adhesion called intimin.<br />
The exact mode of pathogenesis<br />
is unclear, the<br />
secretion/absorbtion ratio<br />
changes<br />
27
Enteroinvasive E. coli (EIEC)<br />
The organism attaches to the intestinal mucosa via pili and outer membrane proteins<br />
are involved in direct penetration, invasion of the intestinal cells, mainly in the colon,<br />
and destruction of the intestinal mucosa.<br />
There is lateral movement of the organism from one cell to adjacent cells.<br />
Symptoms include fever,severe abdominal cramps, malaise, and diarrhea followed<br />
by scanty stools containing blood, mucous, and pus.<br />
Virulence genes similar to Shigella<br />
220 kb size virulence plasmid similar to Shigella’s<br />
Biochemistry is similar biokémiai reakciók is hasonlítanak a Shigellákéhoz<br />
O antigens crossreaction<br />
Lactose <strong>negative</strong>, lysin <strong>negative</strong>, non-motile<br />
Infective dosis is higher than Shigella’s<br />
Outbreaks were reported<br />
Enteroinvasive E. coli (EIEC)<br />
Diagnostic<br />
15 serotypes<br />
Virulence tests<br />
Serény-test (Shigella)<br />
HeLa-sejt invasion test<br />
ELISA for virulence specific antigens<br />
Molecular biology tests for virulence plasmids<br />
28
Enterohaemorrhagiás E. coli (EHEC)<br />
Epidemiology<br />
In 1982 first case<br />
Most common reason of bloody diarhheae in<br />
developed countries<br />
Calves’s diarrheae or asymptomatic in<br />
animals<br />
Low infective dose, contact persons are<br />
source of infections<br />
Enterohaemorrhagic E. coli (EHEC)<br />
Clinical picture<br />
In mild cases gastroenteritis<br />
Severe colitis<br />
Bloody diarrheae<br />
NOT CHARACTERISTIC:<br />
fever<br />
Mucopurulent secretion<br />
10%<br />
children hemolitic uraemic syndrom (HUS)<br />
Adults with kidney problems<br />
thrombotics trombocytopenic purpura (TTP)<br />
29
Enterohaemorrhagiás E. coli (EHEC)<br />
Pathogenesis<br />
The organism attaches via pili to the intestinal<br />
mucosa and liberates the shiga-like toxin Adhesion<br />
molecule similar to EPEC BFP<br />
AE mechanisms of EPEC<br />
Citotoxins as virulence factors coding by temperated<br />
phages<br />
lizogen konversion<br />
Toxic effect on Vero-cells<br />
Two toxin, one of them is similar to Shiga toxin<br />
Shiga-like toxinoks (SLT)<br />
Enterohaemorrhagiás E. coli (EHEC)<br />
Shiga-like toxinok<br />
Two types: SLT-I AND -II<br />
AB-toxinS<br />
B subunit responsible for adhesion to capillarendothel<br />
A subunit by inhibiting EF-1 blokks the protein<br />
synthesis<br />
Capillar damage<br />
Bloody stool<br />
hemolysis, anaemia<br />
Kidney failure, uraemia<br />
Central nervus system signs<br />
30
E. coli gastroenteritis<br />
enterohemorrhagic E. coli (EHEC).<br />
This is most often caused by serotypes O157:H7.<br />
This strain of E. coli can be differentiated from other strains of E. coli by<br />
the fact that it does not ferment sorbitol in 48 hours (other strains do).<br />
A sorbitol-Mac (SMAC) plate (contains sorbitol instead of lactose) is used<br />
to selectively isolate this organism.<br />
One must confirm that the isolate is E. coli O1547:H7 using serological<br />
testing and confirm production of the shiga-like toxin before reporting out<br />
results.<br />
E. coli gastroenteritis<br />
enteroaggregative E. coli (EAEC),<br />
EAEC – Mucous associated autoagglutinins cause aggregation<br />
of the bacteria at the cell surface and result in the formation of a<br />
mucous biofilm.<br />
Enteroaggregative ST-like toxin – produced by<br />
enteroaggregative strains of E. coli (EAEC) – causes watery<br />
diarrhea.<br />
The organisms attach via pili and liberate a cytotoxin distinct<br />
from, but similar to the ST and LT enterotoxins liberated by<br />
ETEC.<br />
Symptoms include watery diarrhea, vomiting, dehydration and<br />
occasional abdominal pain.<br />
31
E.coli<br />
Antimicrobic therapy- E. coli is usually susceptible<br />
to a variety of chemotherapeutic agents,<br />
Though drug resistant strains are increasingly<br />
prevalent.<br />
It is essential to do susceptibility testing.<br />
Summary of E.coli strains that cause gastroenteritis.<br />
32
Shigella genus<br />
Contains four species that differ antigenically and, to a lesser<br />
extent, biochemically.<br />
Serogroup A: S. dysenteriae (12 serotypes)<br />
Serogroup B: S. flexneri (6 serotypes)<br />
Serogroup C: S. boydii (23 serotypes)<br />
Serogroup D: S. sonnei (1 serotype)<br />
OBLIGATE HUMAN PATHOGEN<br />
33
Shigella species<br />
Antigenic structure<br />
Differentiation into groups (A, B, C, and D) is based on<br />
O antigen serotyping; K antigens may interfere with<br />
serotyping, but are heat labile.<br />
O antigen is similar to E. coli, so it is important to ID as<br />
Shigella before doing serotyping.<br />
Virulence factors<br />
Shiga toxin – is produced by S. dysenteriae and in<br />
smaller amounts by S. flexneri and S. sonnei.<br />
Acts to inhibit protein synthesis by inactivating the<br />
60S ribosomal subunit by cleaving a glycosidic<br />
bond in one of the rRNA constituents.<br />
This plays a role in the ulceration of the intestinal<br />
mucosa.<br />
Shigella species<br />
Outer membrane and secreted proteins<br />
These proteins are expressed at body<br />
temperature and upon contact with M cells<br />
in the intestinal mucosa they induce<br />
phagocytosis of the bacteria into vacuoles.<br />
Shigella destroy the vacuoles to escape<br />
into the cytoplasm.<br />
From there they spread laterally<br />
(Polymerization of actin filaments propels<br />
them through the cytoplasm.) to epithelial<br />
cells where they multiply but do not usually<br />
disseminate beyond the epithelium.<br />
34
Shigella biochemistry and<br />
serology<br />
relative inactive<br />
Lactose-<strong>negative</strong><br />
Aexcept S. sonnei<br />
Slowly in some days<br />
Non-motile<br />
Lost of serotypes in S. dysenteriae, S. flexneri and S. boydii species<br />
Based on O antigen<br />
Public health importance<br />
Important S. dysenteriae I-es típusa<br />
Toxin production (Shiga-toxin)<br />
Ressistant to antibiotics and can ause outbreaks<br />
S. sonnei has onyl one O antigen: phase I<br />
Encoded by virulence plasmid<br />
With no virulence plasmid, no O antigens<br />
Roughy colonies<br />
Phase II<br />
Shigella<br />
Clinical significance<br />
Causes shigellosis or bacillary dysentery.<br />
Transmission is via the fecal-oral route.<br />
The infective dose required to cause infection is very low (10-<br />
200 organisms).<br />
There is an incubation of 1-7 days followed by fever, cramping,<br />
abdominal pain, and watery diarrhea (due to the toxin)for 1-3<br />
days.<br />
This may be followed by frequent, scant stools with blood,<br />
mucous, and pus (due to invasion of intestinal mucosa).<br />
It is rare for the organism to disseminate.<br />
The severity of the disease depends upon the species one is<br />
infected with.<br />
S. dysenteria is the most pathogenic followed by S. flexneri, S.<br />
sonnei and S. boydii.<br />
35
Fig. 4.34 Shigellosis.<br />
Sigmoidiscopic view of colonic<br />
mucosa in a fatal case of<br />
infection with S. dysenteriae<br />
type 1 showing extensive<br />
pseudomembranous colitis. By<br />
courtesy of Dr. R.H. Gilman<br />
and Dr. F. Koster.<br />
Fig. 4.33 Shigellosis.<br />
Sigmoidiscopic view of colonic<br />
mucosa in a mild case of infection<br />
due to S. flexneri. Note the thin<br />
whitish exsudate, which is made up<br />
of fibrin and polymorphonuclear<br />
leucocytes. By courtesy of Dr. R.H.<br />
Gilman.<br />
36
Shigella boydii<br />
Blood agar<br />
Microbiological diagnosis<br />
Clinical specimen: faeces, food<br />
leftover<br />
Direct smear has no diagnostic<br />
value<br />
Culture:<br />
Eosine-methylenblue agar<br />
small, round-shaped, colourless<br />
colonies (lactose -)<br />
Desoxycholate-citrate agar ⇒<br />
containing desoxycholic acid,<br />
sodium citrate, lead acetate,<br />
ferrous ammonium sulfate,<br />
lactose, and neutral red<br />
indicator<br />
Shigellae: small, round-shaped,<br />
colourless colonies (lactose -,<br />
H2S-).<br />
www.biologie.de<br />
38
Appearance of Colonies on Salmonella-Shigella Agar<br />
D: Proteus mirabilis<br />
Shigella Shigella<br />
Shigella<br />
Selective –<br />
differentiating<br />
media<br />
www.textbookofbacteriology.net<br />
A. Klebsiella pneumoniae<br />
B. Escherichia coli<br />
Klebsiella pneumoniae &<br />
Escherichia coli are positive<br />
for acid production from<br />
fermentation of the<br />
carbohydrate(s) present.<br />
C: Salmonella sp.<br />
Both Salmonella<br />
sp. & Proteus<br />
mirabilis product<br />
hydrogen sulfide.<br />
The Pseudomonas colonies are nearly colorless.<br />
www.rci.rutgers.edu<br />
E: Pseudomona aeruginosa<br />
39
Fig. 4.18 Positive Serény test. Keratoconjunctivitis in the rabbit<br />
produced by the instillation of shigella microorganism. By courtesy of<br />
Dr. H.L. DuPont.<br />
Shigella<br />
Antimicrobial therapy<br />
Sulfonamides are commonly used as are<br />
streptomycin, tetracycline, ampicillin, and<br />
chloramphenicol.<br />
Resistant strains are becoming increasingly common,<br />
so sensitivity testing is required.<br />
40
Yersinia<br />
Three species are important pathogens in human<br />
Yersinia pestis – causes plague<br />
Yersinia enterocolitica – enteropathogenic<br />
Yersinia pseudotuberculosis – enteropathogenic<br />
41
Yersinia pestis<br />
nonenteric<br />
tiny, gram-<strong>negative</strong> rod, unusual bipolar<br />
staining & capsules<br />
virulence factors – capsular & envelope<br />
proteins protect against phagocytosis & foster<br />
intracellular growth<br />
coagulase, endotoxin, murine toxin<br />
Yersinia pestis bipolar staining<br />
42
Yersinia pestis Wayson’s stain<br />
Yersinia species<br />
TSI K/A no gas<br />
LIA K/A<br />
Urea –<br />
Guinea pig or mouse pathogenicity studies:<br />
LD 50
Y. pestis<br />
Y. pestis – clinical significance<br />
In man plague occurs in two forms; bubonic and pneumonic<br />
Bubonic plague – transmitted by fleas from an infected rodent (is<br />
endemic in our local mountains).<br />
The bacteria travel in the blood to the nearest lymph node where<br />
they are engulfed by fixed macrophages.<br />
A high fever develops and the lymph nodes in the groin and armpit<br />
become enlarged (buboes) as the bacteria proliferate and stimulate<br />
an inflammatory response.<br />
The bacteria growing in the lymph node leak into the bloodstream.<br />
Lysis of the bacteria releases LPS, causing septic shock.<br />
Subcutaneous hemorrhages , probably due to LPS causing DIC gave<br />
the disease the name, the black death, in the middle ages.<br />
The untreated mortality rate is quite high.<br />
Y. pestis<br />
44
Pathology of plague<br />
3-50 bacilli<br />
bubonic – bacillus multiplies in flea bite, enters lymph,<br />
causes necrosis & swelling called a bubo in groin or<br />
axilla<br />
septicemic – progression to massive bacterial growth;<br />
virulence factors cause intravascular coagulation<br />
subcutaneous hemorrhage & purpura – black plague<br />
pneumonic – infection localized to lungs, highly<br />
contagious; fatal without treatment<br />
treatment: streptomycin, tetracycline or<br />
chloramphenicol<br />
Killed or attenuated vaccine<br />
Buboes<br />
45
Y. enterocolitica growth on CIN<br />
Yersinia species<br />
Yersinia enterocolitica and Y. pseudotuberculosis – clinical significance<br />
Both are acquired by ingestion of contaminated food or water.<br />
Reservoirs : rodents, domestic animals<br />
Y. enterocolitica is a common cause of human disease, whereas, Y.<br />
pseudotuberculosis is mainly a disease of other animals.<br />
Both cause a disease involving fever and abdominal pain. Y.<br />
enterocolitica also causes a bloody diarrhea.<br />
After ingestion, the bacteria invade the intestinal epithelium by invasion of<br />
M cells.<br />
They are transcytosed through the M cells and released at the basal<br />
surface.<br />
Once through the intestional epithelium, the bacteria penetrate into the<br />
underlying lymphoid tissue, where they multiply both inside and<br />
outside host cells.<br />
46
Yersinia species<br />
Multiplication of the bacteria produces an inflammatory<br />
response that is responsible for the extreme pain<br />
associated with the infections (resembles acute<br />
appendicitis)<br />
Fever is due to the activity of the LPS endotoxin.<br />
Sometimes they drain into adjacent mesenteric lymph<br />
nodes, causing mesenteric lymphadenitis.<br />
Immuncomplex formation reactive arthritis, spondylosis<br />
ankylopetica, erythema nodosum may occur in some<br />
people following Y. enterocolitica infection.<br />
It is thought to be due to cross reacting T cells or<br />
antibodies that attack the joints.<br />
- Rare septic case: pneumonia, meningitis<br />
Yersinia Yersinia Yersinia Yersinia enterocolitica<br />
enterocolitica<br />
enterocolitica<br />
enterocolitica<br />
Morphology <strong>Gram</strong>-<strong>negative</strong>,<br />
Bipolar <strong>rods</strong><br />
www.wadsworth.org<br />
47
Laboratory diagnosis<br />
Sample to be taken: faeces, blood for blood culture,<br />
materials obtained at surgical exploration.<br />
Direct smear: not contributory to the diagnosis.<br />
Culture:<br />
On blood agar at 28 C, aerobically, for 24 hours → colonies<br />
are tiny, round shaped, greyish.<br />
"cold enrichment" (faeces is incubated in buffered, pH 7.6,<br />
saline at 4 oC, for 2 weeks) then inoculated onto<br />
MacConkey agar, or eosine-metyleneblue medium →<br />
colonies are tiny, round shaped and colourless.<br />
Yersinia Yersinia Yersinia Yersinia enterocolitica<br />
enterocolitica<br />
enterocolitica<br />
enterocolitica<br />
www.szu.cz<br />
Véres agar<br />
Blood agar<br />
Blutagar<br />
www.ktl.fi<br />
Y. enterocolitica<br />
O:5,27 CIN-ag<br />
48
Y. enterocolitica<br />
Biochemical identification:<br />
lactose (-), but ONPG (+), urease (+), oxidase (-)<br />
Serological identification:<br />
Slide agglutination to identify cultures with specific<br />
antibodies (test serum) based on the 'O' -antigen.<br />
Blood serology:<br />
Tube agglutination (ag = formalin inactivated bacteria) to<br />
show specific antibodies in patients’ serum.<br />
de.wikipedia.org<br />
49
•Treatment<br />
In mild diarrhea disease is self-limited, the<br />
benefit of antibiotic therapy is unknown.<br />
In severe cases (sepsis, meningitis), antibiotic<br />
treatment should be started as soon as possible with<br />
3rd generation cephalosporins in combination with<br />
aminoglycosides or with fluoroquinolones.<br />
Prevention<br />
No specific preventive measures are available.<br />
50