PCR for detection of bacteria in orthopedic samples - Journal of ...
PCR for detection of bacteria in orthopedic samples - Journal of ...
PCR for detection of bacteria in orthopedic samples - Journal of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
JCM Accepts, published onl<strong>in</strong>e ahead <strong>of</strong> pr<strong>in</strong>t on 2 May 2012<br />
J. Cl<strong>in</strong>. Microbiol. doi:10.1128/JCM.00362-12<br />
Copyright © 2012, American Society <strong>for</strong> Microbiology. All Rights Reserved.<br />
1<br />
2<br />
3<br />
4<br />
5<br />
6<br />
7<br />
8<br />
9<br />
10<br />
11<br />
12<br />
13<br />
14<br />
15<br />
16<br />
17<br />
18<br />
19<br />
Runn<strong>in</strong>g title: <strong>PCR</strong> <strong>for</strong> <strong>detection</strong> <strong>of</strong> <strong>bacteria</strong> <strong>in</strong> <strong>orthopedic</strong> <strong>samples</strong> (revised manuscript)<br />
Improvement <strong>of</strong> <strong>detection</strong> <strong>of</strong> <strong>bacteria</strong>l pathogens <strong>in</strong> normally sterile body sites with a<br />
focus on <strong>orthopedic</strong> <strong>samples</strong> by use <strong>of</strong> a commercial 16S rRNA broad-range <strong>PCR</strong> and<br />
sequence analysis<br />
K. Grif # , I. Heller # , W. M. Prod<strong>in</strong>ger * , K. Lechleitner, C. Lass-Flörl, D. Orth<br />
Division <strong>of</strong> Hygiene and Medical Microbiology, Innsbruck Medical University, Innsbruck,<br />
Austria<br />
Revised manuscript<br />
*<br />
Correspond<strong>in</strong>g author. Mail<strong>in</strong>g address: Division <strong>of</strong> Hygiene and Medical Microbiology,<br />
Innsbruck Medical University, Schoepfstrasse 41, 6020 Innsbruck, Austria. Phone: 43 512<br />
900370703. Fax: 43 512 900373700. E-mail: wolfgang.prod<strong>in</strong>ger@i-med.ac.at<br />
# These authors contributed equally to this study.<br />
1
20<br />
21<br />
22<br />
23<br />
24<br />
25<br />
26<br />
27<br />
28<br />
29<br />
30<br />
31<br />
32<br />
33<br />
34<br />
ABSTRACT<br />
A new commercially available universal 16S and 18S rRNA gene <strong>PCR</strong> test, which is followed<br />
by sequence analysis <strong>of</strong> amplicons (SepsiTest), was evaluated <strong>for</strong> rapid identification <strong>of</strong><br />
pathogens <strong>in</strong> the diagnosis <strong>of</strong> bone and jo<strong>in</strong>t <strong>in</strong>fections. Eighty three <strong>orthopedic</strong> <strong>samples</strong> and<br />
21 specimens from other normally sterile body sites collected from 84 patients were analysed<br />
<strong>in</strong> parallel by culture and <strong>PCR</strong> <strong>for</strong> <strong>detection</strong> <strong>of</strong> <strong>bacteria</strong> and fungi. Compared to culture, the<br />
diagnostic sensitivity and specificity <strong>of</strong> <strong>PCR</strong> were 88.5% and 83.5%, respectively. The<br />
<strong>detection</strong> rate <strong>of</strong> <strong>PCR</strong> (34.6%) was higher than that <strong>of</strong> <strong>bacteria</strong>l culture (25.0%) as a<br />
consequence <strong>of</strong> the presence <strong>of</strong> fastidious and non-cultivable species <strong>in</strong> <strong>samples</strong> and antibiotic<br />
treatment <strong>of</strong> patients. Thirteen culture negative <strong>in</strong>fections were identified by <strong>PCR</strong> and <strong>PCR</strong><br />
was able to detect culture-proven polymicrobial <strong>in</strong>fections. On the other hand, three <strong>samples</strong><br />
were culture positive, but <strong>PCR</strong> negative. SepsiTest demonstrated to be a valuable<br />
supplemental tool <strong>in</strong> the rapid <strong>detection</strong> <strong>of</strong> <strong>bacteria</strong>, especially <strong>for</strong> fastidious and non-<br />
cultivable organisms, allow<strong>in</strong>g earlier pathogen-adapted therapy <strong>in</strong> patients with bone and<br />
jo<strong>in</strong>t <strong>in</strong>fections.<br />
2
35<br />
36<br />
37<br />
38<br />
39<br />
40<br />
41<br />
42<br />
43<br />
44<br />
45<br />
46<br />
47<br />
48<br />
49<br />
50<br />
51<br />
52<br />
53<br />
54<br />
55<br />
56<br />
57<br />
58<br />
INTRODUCTION<br />
Rapid <strong>detection</strong> <strong>of</strong> pathogens <strong>in</strong> cl<strong>in</strong>ical <strong>samples</strong> is an important issue <strong>for</strong> a better<br />
patient outcome. In the last decade, molecular-based methods <strong>for</strong> the identification <strong>of</strong> blood<br />
stream pathogens became more important due to their rapidity, sensitivity, and<br />
reproducibility. These methods are an attractive alternative, when conventional<br />
bacteriological techniques fail to identify microorganisms, particularly slow-grow<strong>in</strong>g,<br />
fastidious, or non-cultivable organisms. Interfer<strong>in</strong>g factors such as antimicrobial therapy may<br />
cause false-negative culture results even <strong>in</strong> cases <strong>of</strong> <strong>in</strong>fections due to easy-to-culture<br />
pathogens such as staphylococci and streptococci (6,16).<br />
Molecular techniques <strong>in</strong>clude pathogen-specific, multiplex and broad-range assays.<br />
The cl<strong>in</strong>ical usefulness <strong>of</strong> pathogen specific techniques is limited by the large number <strong>of</strong><br />
pathogens potentially <strong>in</strong>volved <strong>in</strong> different k<strong>in</strong>ds <strong>of</strong> <strong>in</strong>fections. Multiplex real-time <strong>PCR</strong><br />
assays, on the other hand, facilitate the rapid identification <strong>of</strong> pathogens and are a promis<strong>in</strong>g<br />
approach <strong>for</strong> rout<strong>in</strong>e use. Several studies have shown the value <strong>of</strong> this diagnostic tool <strong>for</strong><br />
rapid <strong>detection</strong> <strong>of</strong> blood stream pathogens, particularly <strong>in</strong> pre-treated patients (4,5,25). Also<br />
<strong>for</strong> cl<strong>in</strong>ical specimens other than blood, these assays show a great potential <strong>for</strong> diagnos<strong>in</strong>g<br />
<strong>bacteria</strong>l <strong>in</strong>fections (21). An obvious limitation is the <strong>in</strong>ability to detect microorganisms that<br />
are not <strong>in</strong>cluded <strong>in</strong> the targeted spectrum <strong>of</strong> the multiplex <strong>PCR</strong>.<br />
The <strong>PCR</strong> <strong>of</strong> conserved regions <strong>of</strong> microbial genomes, <strong>in</strong> particular the 16S rRNA <strong>of</strong><br />
<strong>bacteria</strong> and the 18S rRNA <strong>of</strong> fungi, respectively, is a broad-range approach when comb<strong>in</strong>ed<br />
with sequence analysis. This method potentially allows the direct <strong>detection</strong> <strong>of</strong> any cultivable<br />
or non-cultivable <strong>bacteria</strong>l or fungal pathogen. Specific applications <strong>of</strong> broad-range 16S and<br />
18S rRNA <strong>PCR</strong> <strong>in</strong> cl<strong>in</strong>ical diagnosis <strong>in</strong>clude sepsis, endocarditis, men<strong>in</strong>gitis and other central<br />
nervous system <strong>in</strong>fections and bone and jo<strong>in</strong>t <strong>in</strong>fections (16,22).<br />
3
59<br />
60<br />
61<br />
62<br />
63<br />
The SepsiTest (Molzym, Bremen, Germany), a commercial assay based on this<br />
technique, has been evaluated <strong>for</strong> different k<strong>in</strong>ds <strong>of</strong> cl<strong>in</strong>ical <strong>samples</strong> like whole blood and<br />
heart valves (14,23). The aim <strong>of</strong> this study was to evaluate SepsiTest <strong>for</strong> <strong>samples</strong> from other<br />
normally sterile body sites with a focus on <strong>orthopedic</strong> <strong>samples</strong> such as synovial fluid (SF) and<br />
jo<strong>in</strong>t tissues (JT).<br />
4
64<br />
65<br />
66<br />
67<br />
68<br />
69<br />
70<br />
71<br />
72<br />
73<br />
74<br />
75<br />
76<br />
77<br />
78<br />
79<br />
80<br />
81<br />
82<br />
83<br />
84<br />
85<br />
86<br />
87<br />
MATERIALS AND METHODS<br />
Study population. One hundred and four cl<strong>in</strong>ical <strong>samples</strong> from 59 patients <strong>of</strong> the<br />
University Hospital Innsbruck (n=78), from 14 patients <strong>of</strong> four smaller district hospitals<br />
(n=15) and from 11 patients <strong>of</strong> general practitioners <strong>in</strong> Tyrol (n=11) were collected<br />
prospectively at the Division <strong>of</strong> Hygiene and Medical Microbiology, Innsbruck Medical<br />
University, between September 2010 and February 2011. The majority <strong>of</strong> <strong>samples</strong> were SF<br />
(n=47) and JT (n=36). Additionally 21 non-<strong>orthopedic</strong> <strong>samples</strong>, i. e. cerebrosp<strong>in</strong>al fluid (CSF)<br />
(n=8), heart valves (HV) (n=6), peritoneal fluid (n=3), lymph node tissue (n=1), lung tissue<br />
(n=1) and tissue <strong>samples</strong> ga<strong>in</strong>ed at post mortem exam<strong>in</strong>ation (bra<strong>in</strong> and liver, n=1 each) were<br />
<strong>in</strong>vestigated. Samples were aseptically divided <strong>in</strong>to two fractions <strong>for</strong> SepsiTest assay and <strong>for</strong><br />
culture, respectively. Various microbiological <strong>samples</strong> from other body sites were also<br />
collected <strong>for</strong> test<strong>in</strong>g when cl<strong>in</strong>ically <strong>in</strong>dicated. Cl<strong>in</strong>ical data and the antimicrobial therapy<br />
adm<strong>in</strong>istered were recorded on the day <strong>of</strong> sampl<strong>in</strong>g.<br />
The study was approved by the ethic committee <strong>of</strong> the Innsbruck Medical University (Nr.<br />
290/4.7)<br />
DNA isolation. All <strong>samples</strong> were prepared <strong>for</strong> molecular analysis with<strong>in</strong> 48 h after<br />
tak<strong>in</strong>g the specimens from the patients. DNA was extracted with UMD Universal assay kit<br />
accord<strong>in</strong>g to the protocol supplied by the manufacturer (Molzym, Bremen, Germany) and<br />
eluates were stored at -20°C. To avoid contam<strong>in</strong>ation <strong>of</strong> the DNA <strong>samples</strong>, DNA isolation<br />
was prepared <strong>in</strong> a lam<strong>in</strong>ar flow cab<strong>in</strong>et decontam<strong>in</strong>ated daily by UV radiation, and strictly<br />
separated from <strong>PCR</strong> process<strong>in</strong>g.<br />
<strong>PCR</strong> and sequence analysis. The broad-spectrum rRNA real-time <strong>PCR</strong> assay was<br />
per<strong>for</strong>med <strong>in</strong> a Light Cycler 2.0 Instrument (Roche Diagnostics, Vienna, Austria) accord<strong>in</strong>g to<br />
the manufacturer’s <strong>in</strong>structions (SepsiTest, Molzym, Bremen, Germany). The procedure<br />
5
88<br />
89<br />
90<br />
91<br />
92<br />
93<br />
94<br />
95<br />
96<br />
97<br />
98<br />
99<br />
100<br />
101<br />
102<br />
103<br />
104<br />
105<br />
106<br />
107<br />
108<br />
109<br />
110<br />
111<br />
112<br />
described elsewhere <strong>in</strong> detail (23) <strong>in</strong>cludes real-time <strong>PCR</strong> analysis us<strong>in</strong>g primers target<strong>in</strong>g<br />
conserved regions <strong>of</strong> the 16S and 18S rRNA-genes <strong>of</strong> <strong>bacteria</strong> and fungi, respectively.<br />
Sequenc<strong>in</strong>g <strong>of</strong> 16S rRNA amplicons employs two primers encompass<strong>in</strong>g Gram-negative and<br />
Gram-positive <strong>bacteria</strong>, respectively, and a separate primer <strong>for</strong> 18S rRNA amplicons.<br />
Amplicons from positive <strong>PCR</strong> reactions were purified with ExoSap-it (Affymetrix,<br />
Cleveland, USA) and sequenced us<strong>in</strong>g sequenc<strong>in</strong>g primers supplied <strong>in</strong> the SepsiTest kit.<br />
Sequence analysis <strong>of</strong> all amplicons was accomplished with the 3500 Genetic Analyzer<br />
(Applied Biosystems, Darmstadt, Germany). Pathogens were identified by us<strong>in</strong>g the<br />
SepsiTest-BLAST tool database (http://www.sepsitest-blast.net) and the onl<strong>in</strong>e search<br />
BLAST tool (2). Analysis <strong>of</strong> mixed sequences was per<strong>for</strong>med us<strong>in</strong>g the web based RipSeq<br />
s<strong>of</strong>tware (13). Genus and species identification was presumed <strong>in</strong> cl<strong>in</strong>ical <strong>samples</strong> with<br />
sequence identities <strong>of</strong> > 97 % and > 99 %, respectively, to reference sequences <strong>of</strong> stra<strong>in</strong>s <strong>in</strong><br />
the database.<br />
Interpretation criteria <strong>for</strong> discrepant results. A microorganism detected by <strong>PCR</strong><br />
only was def<strong>in</strong>ed as a “true pathogen”, if (i) this pathogen was cultured from further<br />
specimens collected from the same <strong>in</strong>fectious site dur<strong>in</strong>g the same <strong>in</strong>fectious episode and/or<br />
(ii) the species was specific <strong>for</strong> the patient’s type <strong>of</strong> <strong>in</strong>fection. “Possible pathogen” was<br />
assigned, if the respective pathogen detected by only one method has been reported as a<br />
causative agent <strong>in</strong> the literature. “Indeterm<strong>in</strong>ate” was assigned to positive <strong>PCR</strong> results<br />
meet<strong>in</strong>g neither the “true” nor the “possible” pathogen def<strong>in</strong>ition. A pathogen identified only<br />
by culture was regarded as “true” as culture was def<strong>in</strong>ed as the golden standard <strong>for</strong> this study<br />
Culture. The specimens were immediately cultured on 5% sheep blood Columbia agar<br />
(Heipha, Eppelheim, Germany), Chocolate agar (Heipha, Eppelheim, Germany) and<br />
Schaedler´s agar (Oxoid, Bas<strong>in</strong>gstoke, UK) and <strong>in</strong>cubated at 37°C <strong>in</strong> parallel <strong>in</strong> aerobic and<br />
anaerobic atmosphere <strong>for</strong> 48 h. Additionally, specimens were <strong>in</strong>oculated <strong>in</strong>to bra<strong>in</strong> heart<br />
6
113<br />
114<br />
115<br />
116<br />
117<br />
118<br />
119<br />
120<br />
121<br />
122<br />
123<br />
124<br />
125<br />
126<br />
<strong>in</strong>fusion broth (Mast Group, Merseyside, UK) and thioglycollate broth (Becton Dick<strong>in</strong>son,<br />
Heidelberg, Germany), and <strong>in</strong>cubated at 37°C <strong>for</strong> 7 days. Isolated colonies were identified<br />
with standard microbiological procedures. In brief, isolates were first evaluated based on plate<br />
morphologies after overnight growth. Colonies consistent with staphylococci were confirmed<br />
with rapid catalase, Staphylococcus aureus was dist<strong>in</strong>guished from coagulase negative<br />
staphylococci (CoNS) with the Slidex Staph Plus latex agglut<strong>in</strong>ation test (bioMérieux, Marcy<br />
l´Etoile, France) and coagulase test<strong>in</strong>g. CoNS were identified to group level and not further<br />
differentiated. Beta-hemolytic streptococci were grouped with the Phadebact latex<br />
agglut<strong>in</strong>ation test (Bactus AB, Hudd<strong>in</strong>ge, Sweden). Other streptococci, Gram-negative and<br />
anaerobic <strong>bacteria</strong> were identified with different commercial identification systems,<br />
pr<strong>in</strong>cipally the API and Vitek2 systems (bioMérieux).<br />
Statistical analysis. Calculation <strong>of</strong> significance <strong>for</strong> comparison <strong>of</strong> SepsiTest and<br />
culture <strong>for</strong> <strong>detection</strong> <strong>of</strong> pathogens was per<strong>for</strong>med by us<strong>in</strong>g the McNemar’s test. A P value <strong>of</strong><br />
127<br />
128<br />
129<br />
130<br />
131<br />
132<br />
133<br />
134<br />
135<br />
136<br />
137<br />
138<br />
139<br />
140<br />
141<br />
142<br />
143<br />
144<br />
145<br />
146<br />
147<br />
148<br />
149<br />
150<br />
151<br />
RESULTS<br />
Of the 104 <strong>samples</strong>, 26 <strong>samples</strong> from 18 patients were culture positive. <strong>PCR</strong> yielded<br />
positive results <strong>in</strong> 36 <strong>samples</strong> from 25 patients. Among 47 synovial fluid specimens, 3 (6.4%)<br />
were positive with culture and 9 (19.1%) were positive with <strong>PCR</strong>. Fifteen (41.7%) culture<br />
positive and 13 (37.1%) <strong>PCR</strong> positive results were detected with<strong>in</strong> 36 jo<strong>in</strong>t tissues. Twenty-<br />
one non-<strong>orthopedic</strong> specimens showed 38.1% positive culture f<strong>in</strong>d<strong>in</strong>gs and 66.7% <strong>PCR</strong><br />
positive signals. The <strong>detection</strong> rate <strong>of</strong> <strong>PCR</strong> (34.6%) was higher than that <strong>of</strong> culture (25.0%) (p<br />
= 0.02). Compared to culture, the diagnostic sensitivity and specificity <strong>of</strong> the <strong>PCR</strong> were<br />
88.5% and 83.5%, respectively. Only <strong>bacteria</strong>l species, no fungal organisms were detected.<br />
Eleven different <strong>bacteria</strong>l species were found by culture and 16 species by <strong>PCR</strong>. Sequence<br />
analysis was successful with species identification <strong>in</strong> 34 cases, <strong>in</strong> one case at the genus level<br />
only (clostridial bacterium). In one case <strong>PCR</strong> could not differentiate between Shigella sonnei<br />
and Escherichia fergusonii. All <strong>PCR</strong> controls run with each series <strong>of</strong> experiments (<strong>in</strong>ternal,<br />
positive and negative <strong>PCR</strong> controls) yielded the expected results.<br />
Congruence <strong>of</strong> culture and <strong>PCR</strong> results. Seventy n<strong>in</strong>e <strong>samples</strong> yielded congruent<br />
results regard<strong>in</strong>g culture and <strong>PCR</strong>. Fourteen <strong>samples</strong> from 12 patients showed identical<br />
positive results. The follow<strong>in</strong>g organisms were detected: Staphylococcus aureus (n=7),<br />
CoNS/Staphylococcus epidermidis (n=4), Streptococcus pneumoniae (n=2), and Neisseria<br />
men<strong>in</strong>gitidis (n=1). Sixty five specimens from 57 patients showed negative results by both<br />
methods. Thus, the concordance <strong>of</strong> <strong>PCR</strong> and culture <strong>for</strong> both identical positive and negative<br />
<strong>samples</strong> was (14+65/104), i.e., 76.0%.<br />
<strong>PCR</strong> positive, culture negative results. In 13 specimens from 11 patients a positive<br />
<strong>PCR</strong> result <strong>in</strong> culture negative <strong>samples</strong> was found (Table 1). These <strong>samples</strong> were distributed<br />
among six SF, one JT, three HV, one peritoneal fluid and two specimens from bra<strong>in</strong> and liver<br />
tissue. <strong>PCR</strong> sequences <strong>of</strong> 11 different <strong>bacteria</strong>l species were found. In two patients the <strong>PCR</strong><br />
8
152<br />
153<br />
154<br />
155<br />
156<br />
157<br />
158<br />
159<br />
160<br />
161<br />
162<br />
163<br />
164<br />
165<br />
166<br />
167<br />
168<br />
169<br />
170<br />
171<br />
172<br />
173<br />
174<br />
175<br />
f<strong>in</strong>d<strong>in</strong>gs were supported by the <strong>detection</strong> <strong>of</strong> the same pathogen <strong>in</strong> other specimens from the<br />
same <strong>in</strong>fectious site. Four <strong>of</strong> these 11 patients had received adequate antibiotic therapy at the<br />
time <strong>of</strong> sampl<strong>in</strong>g, <strong>in</strong>clud<strong>in</strong>g all three patients <strong>in</strong> whom a “true” pathogen was detected by <strong>PCR</strong><br />
only. Of the rema<strong>in</strong><strong>in</strong>g seven patients, five had been untreated. In two no <strong>in</strong><strong>for</strong>mation about<br />
antibiotic pre-treatment was available.<br />
<strong>PCR</strong> negative, culture positive results. Three <strong>orthopedic</strong> <strong>samples</strong> were positive by<br />
culture, but negative by <strong>PCR</strong> (Table 1). Two <strong>of</strong> them conta<strong>in</strong>ed CoNS and one Streptococcus<br />
mitis. In one case the culture f<strong>in</strong>d<strong>in</strong>g was supported by culture results yield<strong>in</strong>g the same<br />
pathogen (CoNS) <strong>in</strong> other specimens from the same <strong>in</strong>fectious site.<br />
Discordances <strong>in</strong> species identification. In 9 <strong>samples</strong> from 4 patients, culture and <strong>PCR</strong><br />
identified different organisms: one <strong>of</strong> these <strong>samples</strong> was matched at the genus level<br />
(Streptococcus mitis vs. Streptococcus milleri). The other <strong>samples</strong> with discordant species<br />
identification were l<strong>in</strong>ked to polymicrobial <strong>in</strong>fections (Table 1). An <strong>in</strong>fection was presumed<br />
as polymicrobial, if two or more microorganisms were detected by <strong>PCR</strong> or by culture or <strong>in</strong><br />
other <strong>samples</strong> collected from the same <strong>in</strong>fectious site dur<strong>in</strong>g the same <strong>in</strong>fectious episode.<br />
With<strong>in</strong> 5 tissue <strong>samples</strong> from patient ID #89 (a case with prosthetic jo<strong>in</strong>t <strong>in</strong>fection)<br />
polymicrobial <strong>in</strong>fection with Enterococcus faecalis and CoNS (Staphylococcus epidermidis)<br />
was found by <strong>PCR</strong> <strong>in</strong> 2 <strong>samples</strong> and <strong>in</strong> 1 sample by culture. Each method missed one <strong>of</strong> the<br />
pathogens: <strong>PCR</strong> failed to detect Enterococcus faecalis <strong>in</strong> 3 <strong>samples</strong>, whereas culture missed<br />
Staphylococcus epidermidis <strong>in</strong> 4 <strong>samples</strong>. Several other specimens from the same <strong>in</strong>fectious<br />
site (jo<strong>in</strong>t tissue knee) showed growth <strong>of</strong> both organisms.<br />
One <strong>of</strong> two <strong>samples</strong> <strong>of</strong> hip tissue from patient ID #99 (case with septic arthritis) yielded<br />
Streptococcus dysgalactiae by <strong>PCR</strong>, but CoNS by culture, though both <strong>of</strong> them were found <strong>in</strong><br />
other specimens dur<strong>in</strong>g the same <strong>in</strong>fectious episode.<br />
9
176<br />
177<br />
178<br />
179<br />
180<br />
Both patients (ID #89 and #99) were under adequate antibiotic therapy at time <strong>of</strong> sampl<strong>in</strong>g.<br />
One <strong>of</strong> two peritoneal fluid <strong>samples</strong> <strong>of</strong> patient ID #81 yielded Escherichia coli, Streptococcus<br />
pyogenes and Bacteroides fragilis by culture, whereas <strong>PCR</strong> missed E. coli, but identified the<br />
other two pathogens. In the second sample only one <strong>of</strong> three species was detected by each<br />
method: Bacteroides fragilis by culture and Streptococcus pyogenes by <strong>PCR</strong> (Table 1).<br />
10
181<br />
182<br />
183<br />
184<br />
185<br />
186<br />
187<br />
188<br />
189<br />
190<br />
191<br />
192<br />
193<br />
194<br />
195<br />
196<br />
197<br />
198<br />
199<br />
200<br />
201<br />
202<br />
203<br />
204<br />
DISCUSSION<br />
In this study, we analysed 83 <strong>orthopedic</strong> <strong>samples</strong> and 21 specimens from other<br />
normally sterile body sites with SepsiTest, a new commercial <strong>PCR</strong> test. The concordance <strong>of</strong><br />
positive and negative <strong>PCR</strong> and culture results was 76.0%. The sensitivity <strong>of</strong> <strong>PCR</strong> compared to<br />
culture was 88.5%, which is <strong>in</strong> keep<strong>in</strong>g with the data from other studies that applied SepsiTest<br />
to analyse cl<strong>in</strong>ical <strong>samples</strong>: Well<strong>in</strong>ghausen and co-authors compared SepsiTest to blood<br />
culture <strong>for</strong> the diagnosis <strong>of</strong> blood stream <strong>in</strong>fections and found a sensitivity <strong>of</strong> 87% among 342<br />
blood <strong>samples</strong> (23). Kühn et al. evaluated SepsiTest <strong>for</strong> patients with <strong>in</strong>fectious endocarditis:<br />
thirty four HV were <strong>in</strong>vestigated, the sensitivity compared to culture was 85% (14).<br />
Regard<strong>in</strong>g <strong>PCR</strong> positive, but culture negative results, we used predef<strong>in</strong>ed criteria to<br />
categorize the detected pathogen as a “true” or “possible” cause. Of thirteen pathogens<br />
detected by <strong>PCR</strong> only, five were considered as “true” and seven as “possible” (one <strong>PCR</strong> result<br />
was “<strong>in</strong>determ<strong>in</strong>ate”). “True” was assigned to three <strong>samples</strong> from two patients (IDs #7 and<br />
#99; Table 1) upon further, corroborat<strong>in</strong>g culture results and to two <strong>samples</strong> from patient ID<br />
#84 due to <strong>PCR</strong>-<strong>detection</strong> <strong>of</strong> a diagnosis-specific pathogen, i. e., Neisseria men<strong>in</strong>gitidis <strong>in</strong><br />
autopsy <strong>samples</strong> <strong>of</strong> a case <strong>of</strong> men<strong>in</strong>gitis. All three patients had received adequate antibiotic<br />
therapy which may expla<strong>in</strong> the negative culture results.<br />
For the seven cases with “possible pathogens”, case reports underl<strong>in</strong>e the plausibility<br />
<strong>of</strong> the <strong>PCR</strong> result, i. e., Pseudomonas aerug<strong>in</strong>osa from a HV sample <strong>in</strong> endocarditis (1,7,17),<br />
Ureaplasma urealyticum <strong>in</strong> a female patient with peritonitis and adnexitis (3,24), and<br />
Staphylococcus epidermidis from SF <strong>in</strong> an arthritis patient (9). The four further <strong>orthopedic</strong><br />
<strong>samples</strong> yielded anaerobic, fastidious or non-cultivable organisms (i. e., a clostridial<br />
bacterium, F<strong>in</strong>egoldia magna, Granulicatella adiacens and Tropheryma whipplei) each <strong>of</strong><br />
which is a documented possible agent <strong>of</strong> arthritis (8,10-12,15,18-20).<br />
11
205<br />
206<br />
207<br />
208<br />
209<br />
210<br />
211<br />
212<br />
213<br />
214<br />
215<br />
216<br />
217<br />
218<br />
219<br />
220<br />
221<br />
222<br />
223<br />
224<br />
225<br />
226<br />
227<br />
228<br />
229<br />
In the “<strong>in</strong>determ<strong>in</strong>ate” case, <strong>PCR</strong> could not differentiate between Shigella sonnei and<br />
Escherichia fergusonii and no cultural or cl<strong>in</strong>ical data supported the <strong>PCR</strong> result.<br />
In three <strong>samples</strong> (2.9%) with <strong>PCR</strong> negative, but culture positive results, <strong>PCR</strong> was<br />
considered as false negative. False negative <strong>PCR</strong> results have also been observed <strong>in</strong> the other<br />
studies evaluat<strong>in</strong>g SepsiTest: seven <strong>samples</strong> (2.0%) among 342 blood culture specimens (23)<br />
and two <strong>of</strong> 34 (5.9%) tested HV <strong>samples</strong> (14). An explanation <strong>for</strong> the negative <strong>PCR</strong> results<br />
could be the process<strong>in</strong>g <strong>for</strong> the <strong>samples</strong>: they are split <strong>in</strong>to two parts, thus the lesser sample<br />
volume used <strong>for</strong> <strong>PCR</strong> analysis could result <strong>in</strong> a pathogen DNA amount be<strong>in</strong>g below the<br />
<strong>detection</strong> limit (23). In addition, the sensitivity <strong>of</strong> 1 cfu per specimen (as <strong>for</strong> well culturable<br />
pathogens) is hardly reached by <strong>PCR</strong>.<br />
It has been claimed that <strong>PCR</strong> assays cannot be used to identify each pathogen <strong>in</strong> cases<br />
<strong>of</strong> mixed <strong>in</strong>fection (26). Nevertheless, our data demonstrate the simultaneous <strong>detection</strong> <strong>of</strong> two<br />
species by <strong>PCR</strong> <strong>in</strong> two <strong>of</strong> the three culture-proven cases <strong>of</strong> polymicrobial <strong>in</strong>fection (Table 1).<br />
Although the comb<strong>in</strong>ations <strong>of</strong> all test results per patient give clear pictures, this is not the case<br />
on the level <strong>of</strong> the s<strong>in</strong>gle specimen, however, as only 3 <strong>of</strong> 7 <strong>PCR</strong>s and 2 <strong>of</strong> 7 cultures,<br />
respectively, yielded both pathogens. There<strong>for</strong>e, our study supports the notion that a<br />
comb<strong>in</strong>ation <strong>of</strong> methods is optimal <strong>for</strong> the <strong>detection</strong> <strong>of</strong> mixed <strong>in</strong>fections. Kühn and co-<br />
workers found three cases <strong>of</strong> polymicrobial <strong>in</strong>fection among 34 HV <strong>samples</strong> by SepsiTest<br />
only (14). In 11 <strong>of</strong> 342 blood <strong>samples</strong>, polymicrobial <strong>in</strong>fection was detected by <strong>PCR</strong> only, but<br />
was missed by <strong>PCR</strong> <strong>in</strong> four cases (23).<br />
In conclusion, SepsiTest appears as a valuable tool <strong>for</strong> diagnos<strong>in</strong>g bone and jo<strong>in</strong>t<br />
<strong>in</strong>fections <strong>in</strong> particular. In our op<strong>in</strong>ion the major advantage is its ability to detect and identify<br />
virtually any cultivable or non-cultivable <strong>bacteria</strong>l species and non-viable <strong>bacteria</strong> from<br />
patients treated with antibiotics. Nevertheless, SepsiTest should always be used <strong>in</strong><br />
comb<strong>in</strong>ation with culture, as this <strong>in</strong>creases sensitivity especially <strong>in</strong> cases <strong>of</strong> polymicrobial<br />
12
230<br />
231<br />
232<br />
<strong>in</strong>fections and culture is <strong>in</strong>dispensable <strong>for</strong> antimicrobial susceptibility test<strong>in</strong>g. Further studies<br />
are needed to evaluate the cost effectiveness <strong>of</strong> SepsiTest and, on the long run, the impact <strong>of</strong><br />
this assay on the cl<strong>in</strong>ical outcome <strong>of</strong> patients.<br />
13
233<br />
234<br />
235<br />
236<br />
237<br />
238<br />
239<br />
240<br />
241<br />
242<br />
243<br />
244<br />
245<br />
246<br />
247<br />
248<br />
249<br />
250<br />
251<br />
252<br />
253<br />
254<br />
255<br />
REFERENCES<br />
1. Aggarwal, A., N. Ritter, L. Reddy, D. L<strong>in</strong>gutla, F. Nasar, N. El-Daher, and D.<br />
Hsi. 2011. Recurrent Pseudomonas aortic root abscess complicat<strong>in</strong>g mitral valve<br />
endocarditis. Heart Lung. <strong>in</strong> press, http://dx.doi.org/10.1016/j.hrtlng.2011.01.008,<br />
[Epub ahead <strong>of</strong> pr<strong>in</strong>t).<br />
2. Altschul, S. F., W. Gish, W. Miller, E. W. Myers, and D. J. Lipman. 1990. Basic<br />
local alignment search tool. J.Mol.Biol. 215:403-410.<br />
3. Bailey, E. A., L. R. Solomon, N. Berry, J. S. Cheesbrough, J. E. Moore, X. Jiru,<br />
D. R. Ware<strong>in</strong>g, T. Harrison, and D. Pitcher. 2002. Ureaplasma urealyticum CAPD<br />
peritonitis follow<strong>in</strong>g <strong>in</strong>sertion <strong>of</strong> an <strong>in</strong>trauter<strong>in</strong>e device: diagnosis by eu<strong>bacteria</strong>l<br />
polymerase cha<strong>in</strong> reaction. Perit.Dial.Int. 22:422-424.<br />
4. Bloos, F., F. H<strong>in</strong>der, K. Becker, S. Sachse, D. A. Mekontso, E. Straube, V.<br />
Cattoir, C. Brun-Buisson, K. Re<strong>in</strong>hart, G. Peters, and M. Bauer. 2010. A<br />
multicenter trial to compare blood culture with polymerase cha<strong>in</strong> reaction <strong>in</strong> severe<br />
human sepsis. Intensive Care Med. 36:241-247.<br />
5. Bravo, D., J. Blanquer, M. Tormo, G. Aguilar, R. Borras, C. Solano, M. A. Clari,<br />
E. Costa, B. Munoz-Cobo, M. Argueso, J. R. P<strong>in</strong>eda, and D. Navarro. 2011.<br />
Diagnostic accuracy and potential cl<strong>in</strong>ical value <strong>of</strong> the LightCycler SeptiFast assay <strong>in</strong><br />
the management <strong>of</strong> bloodstream <strong>in</strong>fections occurr<strong>in</strong>g <strong>in</strong> neutropenic and critically ill<br />
patients. Int.J.Infect.Dis. 15:326-331.<br />
6. Breitkopf, C., D. Hammel, H. H. Scheld, G. Peters, and K. Becker. 2005. Impact<br />
<strong>of</strong> a molecular approach to improve the microbiological diagnosis <strong>of</strong> <strong>in</strong>fective heart<br />
valve endocarditis. Circulation. 111:1415-1421.<br />
14
256<br />
257<br />
258<br />
259<br />
260<br />
261<br />
262<br />
263<br />
264<br />
265<br />
266<br />
267<br />
268<br />
269<br />
270<br />
271<br />
272<br />
273<br />
274<br />
275<br />
276<br />
277<br />
278<br />
7. Dawson, N. L., L. M. Brumble, B. S. Pritt, J. D. Yao, J. D. Echols, and S. Alvarez.<br />
2011. Left-sided Pseudomonas aerug<strong>in</strong>osa endocarditis <strong>in</strong> patients without <strong>in</strong>jection<br />
drug use. Medic<strong>in</strong>e (Baltimore). 90:250-255.<br />
8. Fenollar, F., P. Y. Levy, and D. Raoult. 2008. Usefulness <strong>of</strong> broad-range <strong>PCR</strong> <strong>for</strong><br />
the diagnosis <strong>of</strong> osteoarticular <strong>in</strong>fections. Curr.Op<strong>in</strong>.Rheumatol. 20:463-470.<br />
9. Fenollar, F., V. Roux, A. Ste<strong>in</strong>, M. Drancourt, and D. Raoult. 2006. Analysis <strong>of</strong><br />
525 <strong>samples</strong> to determ<strong>in</strong>e the usefulness <strong>of</strong> <strong>PCR</strong> amplification and sequenc<strong>in</strong>g <strong>of</strong> the<br />
16S rRNA gene <strong>for</strong> diagnosis <strong>of</strong> bone and jo<strong>in</strong>t <strong>in</strong>fections. J.Cl<strong>in</strong>.Microbiol. 44:1018-<br />
1028.<br />
10. Fukuda, R., M. Oki, A. Ueda, H. Yanagi, M. Komatsu, M. Itoh, A. Oka, M.<br />
Nish<strong>in</strong>a, H. Ozawa, and A. Takagi. 2010. Vertebral osteomyelitis associated with<br />
Granulicatella adiacens. Tokai J.Exp.Cl<strong>in</strong>.Med. 35:126-129.<br />
11. Hepburn, M. J., S. L. Fraser, T. A. Rennie, C. M. S<strong>in</strong>gleton, and B. Delgado, Jr.<br />
2003. Septic arthritis caused by Granulicatella adiacens: diagnosis by <strong>in</strong>oculation <strong>of</strong><br />
synovial fluid <strong>in</strong>to blood culture bottles. Rheumatol.Int. 23:255-257.<br />
12. Koligi, K., D. Mertz, D. Benz, T. Vogt, G. V. Bloemberg, L. W<strong>in</strong>ter, A. Tyndall,<br />
M. Battegay, and U. A. Walker. 2011. Of bugs and jo<strong>in</strong>ts. Oligoarthritis caused by<br />
Tropheryma whipplei. Internist (Berl). 52:884-888.<br />
13. Kommedal, O., B. Karlsen, and O. Saebo. 2008. Analysis <strong>of</strong> mixed sequenc<strong>in</strong>g<br />
chromatograms and its application <strong>in</strong> direct 16S rRNA gene sequenc<strong>in</strong>g <strong>of</strong><br />
polymicrobial <strong>samples</strong>. J.Cl<strong>in</strong>.Microbiol. 46:3766-3771.<br />
14. Kuhn, C., C. Disque, H. Muhl, P. Orszag, M. Stiesch, and A. Haverich. 2011.<br />
Evaluation <strong>of</strong> commercial universal rRNA gene <strong>PCR</strong> plus sequenc<strong>in</strong>g tests <strong>for</strong><br />
15
279<br />
280<br />
281<br />
282<br />
283<br />
284<br />
285<br />
286<br />
287<br />
288<br />
289<br />
290<br />
291<br />
292<br />
293<br />
294<br />
295<br />
296<br />
297<br />
298<br />
299<br />
300<br />
identification <strong>of</strong> <strong>bacteria</strong> and fungi associated with <strong>in</strong>fectious endocarditis.<br />
J.Cl<strong>in</strong>.Microbiol. 49:2919-2923.<br />
15. Lange, U. and J. Teichmann. 2003. Whipple arthritis: diagnosis by molecular<br />
analysis <strong>of</strong> synovial fluid--current status <strong>of</strong> diagnosis and therapy. Rheumatology.<br />
42:473-480.<br />
16. Manc<strong>in</strong>i, N., S. Carletti, N. Ghidoli, P. Cichero, R. Burioni, and M. Clementi.<br />
2010. The era <strong>of</strong> molecular and other non-culture-based methods <strong>in</strong> diagnosis <strong>of</strong><br />
sepsis. Cl<strong>in</strong>.Microbiol.Rev. 23:235-251.<br />
17. Nasim, A., S. Baqi, and S. F. Akhtar. 2011. Pseudomonas aerug<strong>in</strong>osa endocarditis <strong>in</strong><br />
renal transplant recipients. Transpl.Infect.Dis. doi:10.1111/j.1399-3062.2011.00667.x.,<br />
[Epub ahead <strong>of</strong> pr<strong>in</strong>t].<br />
18. Prassler, R., T. Kempmann, and P. Vierl<strong>in</strong>g. 2008. Whipple's disease with<br />
segmental lesions <strong>in</strong> the proximal small <strong>in</strong>test<strong>in</strong>e. Dtsch.Med.Wochenschr. 133:460-<br />
463.<br />
19. Puechal, X., F. Fenollar, and D. Raoult. 2007. Cultivation <strong>of</strong> Tropheryma whipplei<br />
from the synovial fluid <strong>in</strong> Whipple's arthritis. Arthritis Rheum. 56:1713-1718.<br />
20. Riede, U., P. Graber, and P. E. Ochsner. 2004. Granulicatella (Abiotrophia)<br />
adiacens <strong>in</strong>fection associated with a total knee arthroplasty. Scand.J.Infect.Dis.<br />
36:761-764.<br />
21. Sancho-Tello, S., D. Bravo, R. Borras, E. Costa, B. Munoz-Cobo, and D. Navarro.<br />
2011. Per<strong>for</strong>mance <strong>of</strong> the LightCycler SeptiFast test Mgrade <strong>in</strong> detect<strong>in</strong>g microbial<br />
pathogens <strong>in</strong> purulent fluids. J.Cl<strong>in</strong>.Microbiol. 49:2988-2991.<br />
16
301<br />
302<br />
303<br />
304<br />
305<br />
306<br />
307<br />
308<br />
309<br />
310<br />
311<br />
312<br />
313<br />
314<br />
315<br />
316<br />
317<br />
318<br />
319<br />
320<br />
22. Sontakke, S., M. B. Cadenas, R. G. Maggi, P. P. D<strong>in</strong>iz, and E. B. Breitschwerdt.<br />
2009. Use <strong>of</strong> broad range16S rDNA <strong>PCR</strong> <strong>in</strong> cl<strong>in</strong>ical microbiology.<br />
J.Microbiol.Methods. 76:217-225.<br />
23. Well<strong>in</strong>ghausen, N., A. J. Kochem, C. Disque, H. Muhl, S. Gebert, J. W<strong>in</strong>ter, J.<br />
Matten, and S. G. Sakka. 2009. Diagnosis <strong>of</strong> bacteremia <strong>in</strong> whole-blood <strong>samples</strong> by<br />
use <strong>of</strong> a commercial universal 16S rRNA gene-based <strong>PCR</strong> and sequence analysis.<br />
J.Cl<strong>in</strong>.Microbiol. 47:2759-2765.<br />
24. Yager, J. E., E. S. Ford, Z. P. Boas, L. A. Haseley, B. T. Cookson, D. J. Sengupta,<br />
F. C. Fang, and G. S. Gottlieb. 2010. Ureaplasma urealyticum cont<strong>in</strong>uous<br />
ambulatory peritoneal dialysis-associated peritonitis diagnosed by 16S rRNA gene<br />
<strong>PCR</strong>. J.Cl<strong>in</strong>.Microbiol. 48:4310-4312.<br />
25. Yanagihara, K., Y. Kitagawa, M. Tomonaga, K. Tsukasaki, S. Kohno, M. Seki,<br />
H. Sugimoto, T. Shimazu, O. Tasaki, A. Matsushima, Y. Ikeda, S. Okamoto, N.<br />
Aikawa, S. Hori, H. Obara, A. Ishizaka, N. Hasegawa, J. Takeda, S. Kamihira, K.<br />
Sugahara, S. Asari, M. Murata, Y. Kobayashi, H. G<strong>in</strong>ba, Y. Sumiyama, and M.<br />
Kitajima. 2010. Evaluation <strong>of</strong> pathogen <strong>detection</strong> from cl<strong>in</strong>ical <strong>samples</strong> by real-time<br />
polymerase cha<strong>in</strong> reaction us<strong>in</strong>g a sepsis pathogen DNA <strong>detection</strong> kit. Crit Care. 14.<br />
doi:10.1186/cc9234, [Epub ahead <strong>of</strong> pr<strong>in</strong>t].<br />
26. Zimmerli, W., A. Trampuz, and P. E. Ochsner. 2004. Prosthetic-jo<strong>in</strong>t <strong>in</strong>fections.<br />
N.Engl.J.Med. 351:1645-1654.<br />
17
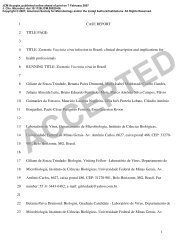
Patient<br />
ID<br />
TABLE 1. Discrepant test results <strong>for</strong> culture and <strong>PCR</strong> (25 specimens from 17 patients)<br />
Diagnosis Specimens<br />
No <strong>of</strong><br />
<strong>samples</strong><br />
Pathogen detected<br />
Culture<br />
positive<br />
<strong>PCR</strong><br />
positive<br />
Further specimens positive by culture<br />
Detection <strong>of</strong> a s<strong>in</strong>gle ”true” a 7 Endocarditis Heart valve tissue 2<br />
pathogen<br />
Streptococcus agalactiae 0 2 S. agalactiae <strong>in</strong> blood culture (d10-) b<br />
84 Men<strong>in</strong>gococcal sepsis Bra<strong>in</strong>, liver tissue 2 Neisseria men<strong>in</strong>gitidis 0 2 no<br />
13 Infected prosthetic jo<strong>in</strong>t Hip tissue 1 Streptococcus mitis 1 0 no<br />
40 Infected prosthetic jo<strong>in</strong>t Jo<strong>in</strong>t tissue knee 1 CoNS c 1 0 CoNS <strong>in</strong> tissue and swab (d0) from knee<br />
86 Infected prosthetic jo<strong>in</strong>t Jo<strong>in</strong>t tissue knee 1 CoNS 1 0 no<br />
78 Spondylodiscitis Sp<strong>in</strong>e tissue 1 Streptococcus mitis<br />
Streptococcus milleri<br />
Detection <strong>of</strong> >1 “true” a 89 Infected prosthetic jo<strong>in</strong>t Jo<strong>in</strong>t tissue knee 5<br />
pathogens<br />
Enterococcus faecalis<br />
CoNS/ Staphylococcus epidermidis d<br />
81 Fournier’s gangrene Peritoneal fluid 2 Streptococcus pyogenes<br />
Bacteroides fragilis<br />
Escherichia coli<br />
99 Septic arthritis Hip tissue 2 Streptococcus dysgalactiae<br />
CoNS<br />
0<br />
1<br />
5<br />
1<br />
1<br />
2<br />
1<br />
0<br />
1<br />
1<br />
0<br />
2<br />
5<br />
2<br />
1<br />
0<br />
2<br />
0<br />
no<br />
S. epidermidis, E. faecalis <strong>in</strong> jo<strong>in</strong>t tissue knee<br />
(d2-, d0)<br />
S. pyogenes, B. fragilis, E. coli <strong>in</strong> peritoneal<br />
fluid and tissue abdomen (d0)<br />
S. dysgalactiae <strong>in</strong> swab hip (d0), tissue hip<br />
(d1-), CoNS <strong>in</strong> jo<strong>in</strong>t tissue and swab hip (d0,<br />
d2+)<br />
Detection <strong>of</strong> a “possible” a 12 Arthritis Synovial fluid knee 1<br />
pathogen<br />
clostridial bacterium 0 1 no<br />
52 Infected prosthetic jo<strong>in</strong>t Synovial fluid knee 1 Granulicatella adiacens 0 1 S. epidermidis <strong>in</strong> synovial tissue knee (d0)<br />
27 Infected prosthetic jo<strong>in</strong>t Synovial fluid hip 1 F<strong>in</strong>egoldia magna 0 1 no<br />
50 Infected prosthetic jo<strong>in</strong>t Synovial fluid hip 1 Tropheryma whipplei 0 1 no<br />
83 Peritonitis, adnexitis Peritoneal fluid 1 Ureaplasma urealyticum 0 1 no<br />
4 Endocarditis Heart valve tissue 1 Pseudomonas aerug<strong>in</strong>osa 0 1 no<br />
41 Arthritis Synovial fluid knee 1 Staphylococcus epidermidis 0 1 no<br />
Indeterm<strong>in</strong>ate results a<br />
79 Arthritis Synovial fluid knee 1 Shigella sonnei/ Escherichia fergusonii 0 1 no<br />
a As described under Methods, a “true” pathogen is def<strong>in</strong>ed as (i) a pathogen cultured from further specimens collected from the same <strong>in</strong>fectious site dur<strong>in</strong>g the same <strong>in</strong>fectious<br />
episode and/or (ii) specific <strong>for</strong> the patient´s type <strong>of</strong> <strong>in</strong>fection. “Possible” pathogen: detected by only one method, but described as a causative agent <strong>in</strong> the literature.<br />
“Indeterm<strong>in</strong>ate” is assigned to positive <strong>PCR</strong> results meet<strong>in</strong>g neither the “true” nor the “possible” pathogen def<strong>in</strong>ition.<br />
b time po<strong>in</strong>t <strong>of</strong> pathogen <strong>detection</strong> <strong>in</strong> days: (-), pathogen <strong>detection</strong> be<strong>for</strong>e sampl<strong>in</strong>g: (+), pathogen <strong>detection</strong> after sampl<strong>in</strong>g.<br />
c coagulase negative staphylococci<br />
d differentiation: to group level by culture and to species level by <strong>PCR</strong>, respectively