Correction of Residual Hyperopia After Cataract Surgery ... - Iogen
Correction of Residual Hyperopia After Cataract Surgery ... - Iogen
Correction of Residual Hyperopia After Cataract Surgery ... - Iogen
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
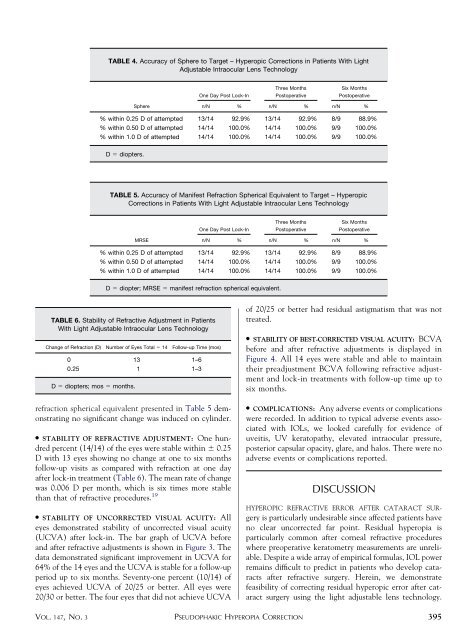
TABLE 4. Accuracy <strong>of</strong> Sphere to Target – Hyperopic <strong>Correction</strong>s in Patients With Light<br />
Adjustable Intraocular Lens Technology<br />
Sphere<br />
One Day Post Lock-In<br />
refraction spherical equivalent presented in Table 5 demonstrating<br />
no significant change was induced on cylinder.<br />
● STABILITY OF REFRACTIVE ADJUSTMENT: One hundred<br />
percent (14/14) <strong>of</strong> the eyes were stable within 0.25<br />
D with 13 eyes showing no change at one to six months<br />
follow-up visits as compared with refraction at one day<br />
after lock-in treatment (Table 6). The mean rate <strong>of</strong> change<br />
was 0.006 D per month, which is six times more stable<br />
than that <strong>of</strong> refractive procedures. 19<br />
● STABILITY OF UNCORRECTED VISUAL ACUITY: All<br />
eyes demonstrated stability <strong>of</strong> uncorrected visual acuity<br />
(UCVA) after lock-in. The bar graph <strong>of</strong> UCVA before<br />
and after refractive adjustments is shown in Figure 3. The<br />
data demonstrated significant improvement in UCVA for<br />
64% <strong>of</strong> the 14 eyes and the UCVA is stable for a follow-up<br />
period up to six months. Seventy-one percent (10/14) <strong>of</strong><br />
eyes achieved UCVA <strong>of</strong> 20/25 or better. All eyes were<br />
20/30 or better. The four eyes that did not achieve UCVA<br />
Three Months<br />
Postoperative<br />
Six Months<br />
Postoperative<br />
n/N % n/N % n/N %<br />
% within 0.25 D <strong>of</strong> attempted 13/14 92.9% 13/14 92.9% 8/9 88.9%<br />
% within 0.50 D <strong>of</strong> attempted 14/14 100.0% 14/14 100.0% 9/9 100.0%<br />
% within 1.0 D <strong>of</strong> attempted 14/14 100.0% 14/14 100.0% 9/9 100.0%<br />
D diopters.<br />
TABLE 5. Accuracy <strong>of</strong> Manifest Refraction Spherical Equivalent to Target – Hyperopic<br />
<strong>Correction</strong>s in Patients With Light Adjustable Intraocular Lens Technology<br />
MRSE<br />
One Day Post Lock-In<br />
Three Months<br />
Postoperative<br />
Six Months<br />
Postoperative<br />
n/N % n/N % n/N %<br />
% within 0.25 D <strong>of</strong> attempted 13/14 92.9% 13/14 92.9% 8/9 88.9%<br />
% within 0.50 D <strong>of</strong> attempted 14/14 100.0% 14/14 100.0% 9/9 100.0%<br />
% within 1.0 D <strong>of</strong> attempted 14/14 100.0% 14/14 100.0% 9/9 100.0%<br />
D diopter; MRSE manifest refraction spherical equivalent.<br />
TABLE 6. Stability <strong>of</strong> Refractive Adjustment in Patients<br />
With Light Adjustable Intraocular Lens Technology<br />
Change <strong>of</strong> Refraction (D) Number <strong>of</strong> Eyes Total 14 Follow-up Time (mos)<br />
0 13 1–6<br />
0.25 1 1–3<br />
D diopters; mos months.<br />
<strong>of</strong> 20/25 or better had residual astigmatism that was not<br />
treated.<br />
● STABILITY OF BEST-CORRECTED VISUAL ACUITY: BCVA<br />
before and after refractive adjustments is displayed in<br />
Figure 4. All 14 eyes were stable and able to maintain<br />
their preadjustment BCVA following refractive adjustment<br />
and lock-in treatments with follow-up time up to<br />
six months.<br />
● COMPLICATIONS: Any adverse events or complications<br />
were recorded. In addition to typical adverse events associated<br />
with IOLs, we looked carefully for evidence <strong>of</strong><br />
uveitis, UV keratopathy, elevated intraocular pressure,<br />
posterior capsular opacity, glare, and halos. There were no<br />
adverse events or complications reported.<br />
DISCUSSION<br />
HYPEROPIC REFRACTIVE ERROR AFTER CATARACT SURgery<br />
is particularly undesirable since affected patients have<br />
no clear uncorrected far point. <strong>Residual</strong> hyperopia is<br />
particularly common after corneal refractive procedures<br />
where preoperative keratometry measurements are unreliable.<br />
Despite a wide array <strong>of</strong> empirical formulas, IOL power<br />
remains difficult to predict in patients who develop cataracts<br />
after refractive surgery. Herein, we demonstrate<br />
feasibility <strong>of</strong> correcting residual hyperopic error after cataract<br />
surgery using the light adjustable lens technology.<br />
VOL. 147, NO. 3 PSEUDOPHAKIC HYPEROPIA CORRECTION<br />
395