Allergic bronchopulmonary aspergillosis - CHEST Publications ...
Allergic bronchopulmonary aspergillosis - CHEST Publications ...
Allergic bronchopulmonary aspergillosis - CHEST Publications ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
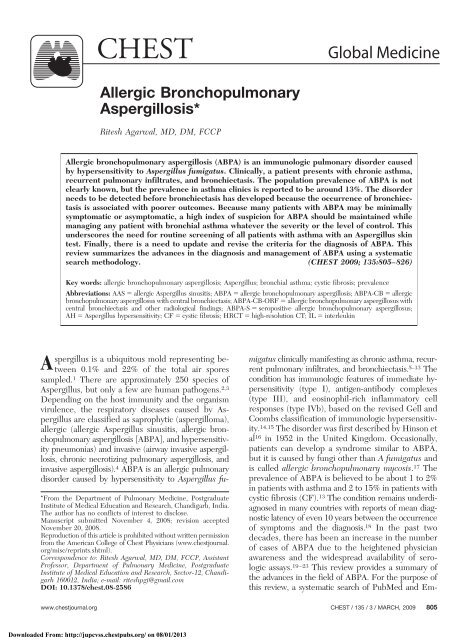
<strong>CHEST</strong> Global Medicine<br />
<strong>Allergic</strong> Bronchopulmonary<br />
Aspergillosis*<br />
Ritesh Agarwal, MD, DM, FCCP<br />
<strong>Allergic</strong> <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> (ABPA) is an immunologic pulmonary disorder caused<br />
by hypersensitivity to Aspergillus fumigatus. Clinically, a patient presents with chronic asthma,<br />
recurrent pulmonary infiltrates, and bronchiectasis. The population prevalence of ABPA is not<br />
clearly known, but the prevalence in asthma clinics is reported to be around 13%. The disorder<br />
needs to be detected before bronchiectasis has developed because the occurrence of bronchiectasis<br />
is associated with poorer outcomes. Because many patients with ABPA may be minimally<br />
symptomatic or asymptomatic, a high index of suspicion for ABPA should be maintained while<br />
managing any patient with bronchial asthma whatever the severity or the level of control. This<br />
underscores the need for routine screening of all patients with asthma with an Aspergillus skin<br />
test. Finally, there is a need to update and revise the criteria for the diagnosis of ABPA. This<br />
review summarizes the advances in the diagnosis and management of ABPA using a systematic<br />
search methodology. (<strong>CHEST</strong> 2009; 135:805–826)<br />
Key words: allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>; Aspergillus; bronchial asthma; cystic fibrosis; prevalence<br />
Abbreviations: AAS allergic Aspergillus sinusitis; ABPA allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>; ABPA-CB allergic<br />
<strong>bronchopulmonary</strong> aspergillosus with central bronchiectasis; ABPA-CB-ORF allergic <strong>bronchopulmonary</strong> aspergillosus with<br />
central bronchiectasis and other radiological findings; ABPA-S seropositive allergic <strong>bronchopulmonary</strong> aspergillosus;<br />
AH Aspergillus hypersensitivity; CF cystic fibrosis; HRCT high-resolution CT; IL interleukin<br />
Aspergillus is a ubiquitous mold representing between<br />
0.1% and 22% of the total air spores<br />
sampled. 1 There are approximately 250 species of<br />
Aspergillus, but only a few are human pathogens. 2,3<br />
Depending on the host immunity and the organism<br />
virulence, the respiratory diseases caused by Aspergillus<br />
are classified as saprophytic (aspergilloma),<br />
allergic (allergic Aspergillus sinusitis, allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> [ABPA], and hypersensitivity<br />
pneumonias) and invasive (airway invasive <strong>aspergillosis</strong>,<br />
chronic necrotizing pulmonary <strong>aspergillosis</strong>, and<br />
invasive <strong>aspergillosis</strong>). 4 ABPA is an allergic pulmonary<br />
disorder caused by hypersensitivity to Aspergillus fu-<br />
*From the Department of Pulmonary Medicine, Postgraduate<br />
Institute of Medical Education and Research, Chandigarh, India.<br />
The author has no conflicts of interest to disclose.<br />
Manuscript submitted November 4, 2008; revision accepted<br />
November 20, 2008.<br />
Reproduction of this article is prohibited without written permission<br />
from the American College of Chest Physicians (www.chestjournal.<br />
org/misc/reprints.shtml).<br />
Correspondence to: Ritesh Agarwal, MD, DM, FCCP, Assistant<br />
Professor, Department of Pulmonary Medicine, Postgraduate<br />
Institute of Medical Education and Research, Sector-12, Chandigarh<br />
160012, India; e-mail: riteshpgi@gmail.com<br />
DOI: 10.1378/chest.08-2586<br />
migatus clinically manifesting as chronic asthma, recurrent<br />
pulmonary infiltrates, and bronchiectasis. 5–13 The<br />
condition has immunologic features of immediate hypersensitivity<br />
(type I), antigen-antibody complexes<br />
(type III), and eosinophil-rich inflammatory cell<br />
responses (type IVb), based on the revised Gell and<br />
Coombs classification of immunologic hypersensitivity.<br />
14,15 The disorder was first described by Hinson et<br />
al 16 in 1952 in the United Kingdom. Occasionally,<br />
patients can develop a syndrome similar to ABPA,<br />
but it is caused by fungi other than A fumigatus and<br />
is called allergic <strong>bronchopulmonary</strong> mycosis. 17 The<br />
prevalence of ABPA is believed to be about 1 to 2%<br />
in patients with asthma and 2 to 15% in patients with<br />
cystic fibrosis (CF). 13 The condition remains underdiagnosed<br />
in many countries with reports of mean diagnostic<br />
latency of even 10 years between the occurrence<br />
of symptoms and the diagnosis. 18 In the past two<br />
decades, there has been an increase in the number<br />
of cases of ABPA due to the heightened physician<br />
awareness and the widespread availability of serologic<br />
assays. 19–23 This review provides a summary of<br />
the advances in the field of ABPA. For the purpose of<br />
this review, a systematic search of PubMed and Em-<br />
www.chestjournal.org <strong>CHEST</strong> / 135 /3/MARCH, 2009 805<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
Table 1—Studies Describing the Prevalence of AH and/or ABPA in Patients with Bronchial Asthma Over the Last<br />
Two Decades*<br />
Study/Year Type of Study<br />
Type of Skin<br />
Test Type of Antigen<br />
Attapattu 31 /1991 Prospective Intradermal Commercial (Bencard<br />
Allergie; Munich,<br />
Germany)<br />
Eaton et al 33 /2000<br />
Kumar and Gaur<br />
Prospective Prick Commercial (Hollister-<br />
Stier Laboratories)<br />
34 /<br />
2000<br />
Base was performed for relevant studies published from<br />
1952 to 2008. A total of 250 articles were reviewed for the<br />
purpose of this article.<br />
Epidemiology of ABPA<br />
Aspergillus hypersensitivity (AH) is defined by the<br />
presence of an immediate-type cutaneous hypersensitivity<br />
to A fumigatus antigens, and it is the first step<br />
in the development of ABPA. 24 Only a minority of<br />
patients with AH develop the complete clinical<br />
picture of ABPA. 25 The population prevalence of<br />
ABPA in asthma, generally referred to as 1 to<br />
2%, 5,13,26,27 is based on the inference of only three<br />
studies (one peer-reviewed and two non–peer-reviewed<br />
studies). 28,29 In the only peer-reviewed<br />
study, 28 14 patients with allergic <strong>bronchopulmonary</strong><br />
mycosis were identified from a total of 1,390 new<br />
referrals in a catchment area population of half a<br />
million, estimating a period prevalence of just above<br />
1%. The other two non–peer-reviewed questionnaire-based<br />
studies suggested a maximum prevalence<br />
of ABPA of 1% in the United States. 29 In a<br />
recent metaanalysis, 30 we demonstrated a prevalence<br />
of AH and ABPA in asthma of 28% and 12.9%,<br />
respectively. The limitation noted in this review was<br />
that all the studies were performed in specialized<br />
clinics and may not be representative of the general<br />
population. Thus the exact population prevalence of<br />
ABPA remains speculative but is likely to be fairly<br />
Criteria Used for<br />
Diagnosis of ABPA<br />
Major (A/R/T/E/P)<br />
Minor (C)<br />
Prevalence of AH<br />
in Asthma (n/N)<br />
Prevalence of ABPA<br />
in Asthma (n/N)<br />
58/134 8/134<br />
Major (A/R/T/E/P/<br />
I/C/S)<br />
47/255 9/35<br />
Prospective Intradermal Locally prepared Major (A/R/T/E/P/<br />
I/C/S)<br />
Minor (C/S/B)<br />
47/200 32/200<br />
Al-Mobeireek et al 20 / Prospective Prick Commercial (Soluprick;<br />
12/53<br />
2001<br />
ALK Laboratories;<br />
Wallingford, CT)<br />
Maurya et al 35 /2005 Prospective Intradermal Locally prepared Major (A/R/T/E/P/<br />
I/C/S)<br />
Minor (C/S)<br />
30/105 8/105<br />
Agarwal et al 23 /2007 Prospective Intradermal Commercial (Hollister- Major (A/R/T/E/P/ 291/755 155/755<br />
Stier Laboratories) I/C/S)<br />
Minor (S/B)<br />
Prasad et al 36 /2008 Prospective Intradermal Not available Major (A/R/T/E/P/<br />
I/C/S)<br />
Minor (C/S/B)<br />
74/244 18/244<br />
* Criteria for ABPA: Major (A asthma, R radiologic opacities, T immediate positive skin test, E eosinophilia, P precipitins to A<br />
fumigatus, I IgE elevated, C central bronchiectasis, S specific IgG/IgE to A fumigatus); Minor (C sputum cultures of A fumigatus,<br />
S type III skin test positivity, B brownish black mucus plugs).<br />
high in patients attending asthma clinics. Table 1<br />
summarizes the prevalence of ABPA in patients with<br />
asthma reported in various studies 20,23,31–36 over the<br />
last two decades. The prevalence of ABPA in patients<br />
admitted with acute severe asthma is even<br />
higher. In a recent study of 57 patients with acute<br />
severe asthma admitted in the respiratory ICUs, we<br />
demonstrated the prevalence of AH and ABPA to be<br />
around 51% and 39%, respectively. 37 The occurrence<br />
of AH and ABPA was significantly higher in patients<br />
with acute asthma compared to the outpatient bronchial<br />
asthma (around 39% and 21%, respectively). 23<br />
Pathogenesis of ABPA<br />
The susceptibility of asthmatic patients to develop<br />
ABPA is not fully understood (Fig 1). Some authors<br />
have reported that exposure to large concentrations<br />
of spores of A fumigatus may cause ABPA. 16,38–41<br />
Environmental factors are not considered the main<br />
pathogenetic factors because not all asthmatics develop<br />
ABPA despite being exposed to the same<br />
environment. In a genetically predisposed individual42–54<br />
(Table 2), inhaled conidia of A fumigatus<br />
persist and germinate into hyphae with release of<br />
antigens that compromise the mucociliary clearance,<br />
stimulate and breach the airway epithelial barrier,<br />
and activate the innate immunity of the lung. 55–58<br />
This leads to inflammatory cell influx and a resultant<br />
early- and late-phase inflammatory reaction. 59,60 The<br />
806 Global Medicine<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
Figure 1. A line diagram depicting the pathogenesis of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Th T-helper.<br />
antigens are also processed presented to T-cells with<br />
activation of Th2 CD4 T-cell responses. 42,61–63 The Th2<br />
cytokines (interleukin [IL]-4, IL-5, and IL-13) lead to total<br />
and A fumigatus-specific IgE synthesis, mast cell degranulation,<br />
and promotion of a strong eosinophilic response.<br />
This causes the characteristic pathology of ABPA.<br />
Pathology of ABPA<br />
The pathology of ABPA varies from patient to<br />
patient, and in different areas of the lung in the same<br />
patient (Fig 2). 64,65 Histologic examination reveals<br />
the presence of mucus, fibrin, Curschmann spirals,<br />
Charcot-Leyden crystals, and inflammatory cells.<br />
Scanty hyphae can often be demonstrated in the<br />
bronchiectatic cavities. The bronchial wall in ABPA<br />
is usually infiltrated by inflammatory cells, primarily<br />
the eosinophils. 65 The peribronchial parenchyma<br />
shows an inflammatory response with conspicuous<br />
eosinophilia. Occasionally, fungal growth in the lung<br />
parenchyma can occur in some patients with ABPA. 66<br />
Patients can also demonstrate a pattern similar to that<br />
of bronchiolitis obliterans with organizing pneumonia.<br />
67 Bronchocentric granulomatosis, the presence of<br />
noncaseating granulomas containing eosinophils and<br />
www.chestjournal.org <strong>CHEST</strong> / 135 /3/MARCH, 2009 807<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
Table 2—Genetic Factors Involved in the Pathogenesis<br />
of ABPA*<br />
HLA associations: presence of HLA DR-2 and absence of<br />
HLA-DQ2 sequences 42,44,45<br />
IL-10 promoter polymorphisms 49<br />
Polymorphism at position 1,082 produces higher levels of IL-10<br />
if 1082G allele is present and lower levels of IL-10 if the<br />
1082A allele is present<br />
In patients with CF there is a relationship between the 1082GG<br />
genotype with both Aspergillus colonization and ABPA<br />
Surfactant protein A gene polymorphisms 48,53<br />
A significantly higher frequency of the AGA allele (A1660G) of<br />
SP-A2 found in patients with ABPA vs control subjects.<br />
Coexistence of A1660G polymorphism with SP-A2 G1649C<br />
(Ala91Pro) found with 10-fold higher odds in patients with<br />
ABPA. Patients with ABPA with GCT and AGG alleles<br />
showed significantly higher levels of total IgE and percentage<br />
eosinophilia vs patients with ABPA with CCT and AGA<br />
alleles 48<br />
The T allele at T1492C and G allele at G1649C of SP-A2<br />
observed at higher frequencies in ABPA patients than in<br />
controls. Also there is a higher frequency of the TT genotype<br />
at position1492 of SP-A2 than controls 53<br />
There were no polymorphisms found in SP-A1 gene 53<br />
CFTR gene mutation: 43,46,47 increased frequency of CFTR<br />
mutations in patients with ABPA vs skin-prick test positive or<br />
negative patients with bronchial asthma<br />
IL-15 polymorphisms: 52 higher frequency of IL-15 13689*A<br />
allele and A/A genotype<br />
TNF- polymorphisms: 52 lower frequency of the TNF- 308 * A/A<br />
genotype<br />
Mannose-binding lectins: 53 the intronic single nucleotide<br />
polymorphism G1011A of mannose-binding lection seen with<br />
increased frequency in patients with ABPA<br />
IL-4 receptor polymorphisms: 51 single nucleotide polymorphism of<br />
the extracellular IL-4R ile75val observed in 80% of ABPA<br />
patients<br />
IL-13 polymorphisms: 50 the arg110gln polymorphism found with<br />
increased frequency in ABPA and the combination of IL-4R<br />
ile75val/IL-13 arg110gln polymorphism found with an even<br />
higher frequency<br />
Toll-like receptor gene polymorphisms: 54 susceptibility to ABPA<br />
was associated with allele C on T1237C (TLR9)<br />
*HLA human leukocyte antigen; TNF tumor necrosis factor;<br />
CFTR CF transmembrane conductance regulator.<br />
multinucleated giant cells centered on the airway, are<br />
also seen. 68,69 Rarely, invasive <strong>aspergillosis</strong> complicating<br />
the course of ABPA has also been described. 70–74<br />
Clinical Features<br />
There is no gender predilection and majority of the<br />
cases present in the third to fourth decade. A family<br />
history of ABPA may be elicited occasionally. 75 Table 3<br />
summarizes the clinical features of ABPA encountered<br />
in three large series from our institute. 19,21,23<br />
Most present with low-grade fever, wheezing, bronchial<br />
hyperreactivity, hemoptysis, or productive<br />
cough. Expectoration of brownish black mucus plugs<br />
is seen in 31 to 69% of patients. 21,23,34 The symptoms<br />
of hemoptysis, expectoration of brownish black mucus<br />
plugs, and history of pulmonary opacities in an<br />
asthmatic patient suggests ABPA. Patients can occasionally<br />
be asymptomatic, and the disorder is<br />
diagnosed on routine screening of asthmatic patients.<br />
22,23,33 Physical examination can be normal or<br />
may reveal polyphonic wheeze. Clubbing is rare,<br />
seen in only 16% of patients. On auscultation, coarse<br />
crackles can be heard in 15% of patients. 23 Physical<br />
examination can also detect complications such as<br />
pulmonary hypertension and/or respiratory failure. 76<br />
During exacerbations of ABPA, localized findings of<br />
consolidation and atelectasis can occur that needs to<br />
be differentiated from other conditions.<br />
Laboratory Findings<br />
Aspergillus Skin Test: The Aspergillus skin test is<br />
performed using an A fumigatus antigen, either<br />
commercial (eg, Aspergillin; Hollister-Stier Laboratories;<br />
Spokane, WA) or locally prepared. The test is<br />
read every 15 min for 1 h, and then after 6 to 8 h.<br />
The reactions are classified as type I if a wheal and<br />
erythema developed within 1 min, reaches a maximum<br />
after 10 to 20 min, and resolves within 1 to 2 h.<br />
A type III reaction is read after 6 h, and any amount<br />
of subcutaneous edema is considered a positive<br />
result. An immediate cutaneous hypersensitivity to A<br />
fumigatus antigens is a characteristic finding of<br />
ABPA and represents the presence A fumigatusspecific<br />
IgE antibodies, whereas a type III skin<br />
reaction probably represents the immune complex<br />
hypersensitivity reaction, although its exact significance<br />
remains unclear. The test can be performed<br />
using either a skin-prick test or intradermal injection<br />
with the latter being more sensitive. 30,77,78 A skinprick<br />
test should be performed for Aspergillus skin<br />
testing, and if the results are negative should be<br />
confirmed by an intradermal test. 30 There is no<br />
difference on the outcome of the test and the type of<br />
antigen (locally prepared or commercial) used for<br />
performance of the test. 30<br />
Total Serum IgE Levels: The total IgE level is the<br />
most useful test for diagnosis and follow-up of ABPA. A<br />
normal serum IgE level excludes ABPA as the cause of<br />
the patient’s current symptoms. The only situation<br />
where IgE levels can be normal in active ABPA is when<br />
the patient is already on glucocorticoid therapy for any<br />
reason and investigation for IgE levels has been conducted.<br />
After treatment with glucocorticoids, the serum<br />
IgE levels decline, and a 35 to 50% decrease is<br />
taken as a criteria for remission. 79 The serum IgE<br />
determination is also used for follow-up, and a doubling<br />
of the patient’s baseline IgE levels indicates relapse of<br />
ABPA. 80,81<br />
808 Global Medicine<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
Figure 2. Histopathologic findings in a patient with allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Top left, A:<br />
photomicrograph showing bronchial lumen containing allergic mucin (hematoxylin-eosin, original 100). Top<br />
right, B: high-magnification photomicrograph of allergic mucin having variegated appearance, necrotic eosinophils,<br />
Charcot-Leyden crystals (thin arrow), and an occasional septate fungal hyphae indicated by a thick arrow<br />
(hematoxylin-eosin, original 200). Bottom left, C: photomicrograph showing eosinophilic pneumonia. There is<br />
filling of the alveolar spaces by eosinophils admixed with variable number of macrophages (hematoxylin-eosin,<br />
original 200). Bottom right, D: photomicrograph showing bronchocentric granulomatosis. There is partial<br />
replacement of bronchial epithelium by palisading histiocytes (hematoxylin-eosin, original 100).<br />
Serum IgE and IgG Antibodies Specific to A<br />
fumigatus: An elevated level of A fumigatus-specific<br />
antibodies measured by fluorescent enzyme immunoassay<br />
is considered the hallmark of ABPA. 22 A<br />
cutoff value of IgG/IgE more than twice the pooled<br />
serum samples from patients with AH can greatly<br />
help in the differentiation of ABPA from other<br />
conditions. 82<br />
Table 3—Clinical Features Encountered in Three Large Case Series of ABPA Published From the Author’s<br />
Institute*<br />
Clinical Features Behera et al 19 /1994 Chakrabarti et al 21 /2002 Agarwal et al 23 /2007<br />
Patients, No. 35 89 155<br />
Male/female gender, No. 14/21 53/35 79/76<br />
Mean age, yr 34.3 36.4 33.4<br />
Mean duration of asthma, yr 11.1 12.1 8.9<br />
History of asthma 94% 90% 100%<br />
Expectoration of sputum plugs Not available 69% 46.5%<br />
Mean eosinophil count, per L 1,264<br />
AEC 500/L, % 12/28 (43%) 100% 76.1%<br />
Fleeting shadows 77% 74% 40%<br />
History of intake of antituberculous drugs<br />
Skin test against Aspergillus<br />
34% 29% 44.5%<br />
Type I 51% 85% 100%<br />
Type III 25.7% 16.9% 83.2%<br />
Mean IgE levels Not done Not done 6,434<br />
Elevated IgE levels, % 100%<br />
Aspergillus-specific IgE/IgG Not done Not done 100%<br />
Serum precipitins against Aspergillus 77% 71.9% 86.5%<br />
Central bronchiectasis<br />
*AEC absolute blood eosinophil count.<br />
71% 69% 76.1%<br />
www.chestjournal.org <strong>CHEST</strong> / 135 /3/MARCH, 2009 809<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
Radiologic Investigations: A wide spectrum of<br />
radiographic appearances can occur in ABPA (Table<br />
4). The chest radiographic findings of ABPA include<br />
transient or fixed pulmonary opacities (Fig 3), tramline<br />
shadows, finger-in-glove opacities, and toothpaste<br />
shadows. 83–87 Findings noted on high-resolution<br />
CT (HRCT) include central bronchiectasis, mucoid<br />
impaction, mosaic attenuation, presence of centrilobular<br />
nodules, and tree-in-bud opacities (Fig<br />
4). 88,89 High-attenuation mucoid impaction (mucus<br />
visually denser than the paraspinal muscle) is a<br />
pathognomonic finding encountered in patients with<br />
ABPA. 23,90–95 Central bronchiectasis with peripheral<br />
tapering of bronchi on HRCT is believed to be a sine<br />
qua non for the diagnosis of ABPA. Bronchiectasis<br />
may not be present in all patients with ABPA, may be<br />
present in patients with CF without ABPA, and<br />
almost 40% of the bronchiectatic segments can also<br />
Table 4—Radiologic Findings Encountered in Patients<br />
With ABPA<br />
1. Chest radiographic findings<br />
Transient changes<br />
Common<br />
Patchy areas of consolidation<br />
Radiologic infiltrates: toothpaste and gloved finger shadows<br />
due to mucoid impaction in dilated bronchi<br />
Collapse: lobar or segmental<br />
Uncommon<br />
Bronchial wall thickening: tramline shadows<br />
Air-fluid levels from dilated central bronchi filled with fluid<br />
Perihilar infiltrates simulating adenopathy<br />
Massive consolidation: unilateral or bilateral<br />
Small nodules<br />
Pleural effusions<br />
Permanent changes<br />
Common<br />
Parallel-line shadows representing bronchial widening<br />
Ring-shadows 1–2 cm in diameter representing dilated<br />
bronchi en face<br />
Pulmonary fibrosis: fibrotic scarred upper lobes with<br />
cavitation<br />
Uncommon<br />
Pleural thickening<br />
Mycetoma formation<br />
Linear scars<br />
2. HRCT findings<br />
Common<br />
Central bronchiectasis<br />
Mucus plugging with bronchoceles<br />
Consolidation<br />
Centrilobular nodules with tree-in-bud opacities<br />
Bronchial wall thickening<br />
Areas of atelectasis<br />
Mosaic perfusion with air trapping on expiration<br />
Uncommon<br />
High-attenuation mucus (finding most helpful in differential<br />
diagnosis)<br />
Pleural involvement<br />
Randomly scattered nodular opacities<br />
have associated peripheral bronchiectasis. 22,96 Minimal<br />
bronchiectasis can also be seen in asthma, 97,98<br />
but the findings of bronchiectasis affecting three or<br />
more lobes, centrilobular nodules, and mucoid impaction<br />
are highly suggestive of ABPA. 99 The uncommon<br />
radiologic manifestations of ABPA include<br />
miliary nodular opacities, 100 perihilar opacities<br />
simulating hilar lymphadenopathy, 84,101,102 pleural<br />
effusions, 103–105 and pulmonary masses. 106–111<br />
Serum Precipitins Against A fumigatus: The precipitating<br />
IgG antibodies are elicited from crude<br />
extracts of A fumigatus and can be demonstrated<br />
using the double gel diffusion technique. 112,113 They<br />
can also be present in other pulmonary disorders and<br />
thus represent supportive not diagnostic evidence for<br />
ABPA. 112–114<br />
Peripheral Eosinophilia: A blood absolute eosinophil<br />
count 1,000 cells/L is also a major criterion<br />
for the diagnosis of ABPA. However, 53% of patients<br />
in our series 22 had an absolute eosinophil count<br />
1,000 cells/L, and thus a low eosinophil count<br />
does not exclude the diagnosis of ABPA.<br />
Sputum Cultures for A fumigatus: Culture of A<br />
fumigatus in the sputum is supportive but not diagnostic<br />
of ABPA. The fungus can also be grown in<br />
patients with other pulmonary diseases due to the<br />
ubiquitous nature of the fungi. We rarely perform<br />
sputum cultures for the diagnosis of ABPA.<br />
Pulmonary Function Tests: These tests help categorize<br />
the severity of the lung disease but have no<br />
diagnostic value in ABPA and need not constitute<br />
the basis for screening. 22 The usual finding is an<br />
obstructive defect of varying severity. 115–117<br />
Role of Specific Aspergillus Antigens: Patients with<br />
ABPA are evaluated with crude extracts from Aspergillus,<br />
which lack reproducibility and consistency,<br />
and they frequently cross-react with other antigens.<br />
118 The advances in molecular techniques have<br />
enabled detection and cloning of specific Aspergillus<br />
antigens. The recombinant allergens Asp f1, Asp f2,<br />
Asp f3, Asp f4, and Asp f6 have been evaluated for<br />
their diagnostic performance in serologic studies in<br />
asthmatic patients 119–122 and in patients with<br />
CF 121,123–125 Preliminary data suggest a promising<br />
role of these antigens in the diagnosis of ABPA.<br />
Further studies are required before they can be<br />
implemented in routine clinical practice.<br />
Diagnosis and Diagnostic Criteria<br />
The Rosenberg-Patterson criteria6,9 are most often<br />
used for the diagnosis (Table 5). There are also a set<br />
810 Global Medicine<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
Figure 3. Chest radiograph showing transient pulmonary opacities in the right lower lobe (left) ina<br />
patient with allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> that have spontaneously disappeared (right).<br />
of minimal diagnostic criteria for ABPA (Table<br />
5). 32,33 These criteria continue to be challenged and<br />
modified because there is lack of evidence on the<br />
number of criteria that should be present to make<br />
the diagnosis. The differentiation of patients with<br />
ABPA from patients with AH can also be problematic.<br />
Serum precipitins to A fumigatus is present in<br />
69 to 90% of patients with ABPA 23,112,116,126,127 but<br />
also in 9% of asthmatics. 112 Central bronchiectasis<br />
can be seen in patients with asthma without<br />
ABPA. 97–99 There are no cutoffs for total IgE levels<br />
with many using 1,000 IU/mL, 8,9,22,23,82,128–130 and<br />
others using 1,000 ng/mL (equivalent to 417 IU/<br />
mL). 5,27,33,34 The total IgE levels may also be elevated<br />
in patients with AH without ABPA. As the<br />
understanding of ABPA has evolved, it is clear that<br />
patients with AH may present with less than the full<br />
complement of diagnostic criteria. 131 Thus, a cutoff<br />
value of 1,000 ng/mL IgE will probably lead to an<br />
overdiagnosis of ABPA. 131 The use of A fumigatus-<br />
Figure 4. HRCT images of different patients with allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Top right:<br />
bilateral central bronchiectasis with centrilobular nodules and tree-in-bud opacities in the left lung. Top<br />
left: bilateral central bronchiectasis with many mucus-filled bronchi. Bottom, left and right: images from<br />
the same patient show high-attenuation mucoid impaction. Bottom right: the mucoid impaction in the<br />
right lung is visually denser than the paraspinal skeletal muscle.<br />
www.chestjournal.org <strong>CHEST</strong> / 135 /3/MARCH, 2009 811<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
Table 5—Criteria Used for the Diagnosis of ABPA<br />
Rosenberg-Patterson criteria 6,9<br />
Major criteria (mnemonic ARTEPICS)<br />
A Asthma<br />
R Roentgenographic fleeting pulmonary opacities<br />
T Skin test positive for Aspergillus (type I reaction,<br />
immediate cutaneous hyperreactivity)<br />
E Eosinophilia<br />
P Precipitating antibodies (IgG) in serum<br />
I IgE in serum elevated ( 1,000 IU/mL)<br />
C Central bronchiectasis<br />
S Serums A fumigatus-specific IgG and IgE (more than<br />
twice the value of pooled serum samples from patients with<br />
asthma who have Aspergillus hypersensitivity)<br />
Minor criteria<br />
Presence of Aspergillus in sputum<br />
Expectoration of brownish black mucus plugs<br />
Delayed skin reaction to Aspergillus antigen (type III<br />
reaction)<br />
The presence of six of eight major criteria makes the diagnosis<br />
almost certain; the disease is further classified as ABPA-S or<br />
ABPA-CB on the absence or presence of central<br />
bronchiectasis, respectively<br />
Minimal diagnostic criteria for ABPA 32<br />
Minimal ABPA-CB<br />
Asthma<br />
Immediate cutaneous hyperreactivity to Aspergillus antigens<br />
Central bronchiectasis<br />
Elevated IgE<br />
Raised A fumigatus-specific IgG and IgE<br />
Minimal ABPA-S<br />
Asthma<br />
Immediate cutaneous hyperreactivity to Aspergillus antigens<br />
Transient pulmonary infiltrates on chest radiograph<br />
Elevated IgE<br />
Raised A fumigatus-specific IgG and IgE<br />
specific IgE and IgG levels can help in confirming<br />
the diagnosis of ABPA because values of IgG/IgE<br />
more than twice the pooled serum samples from<br />
patients with asthma are raised only in ABPA. 113,132<br />
We currently use a cutoff value of 1,000 IU/mL for<br />
the diagnosis of ABPA. 22,23 While investigating a<br />
patient with asthma, we first perform an Aspergillus<br />
skin test. Once it is positive, the total serum IgE<br />
levels are done. 131 If the value is 1,000 IU/mL, we<br />
perform the other tests (Fig 5). If the value is<br />
between 500 and 1,000 IU/mL, the next step is analysis<br />
of A fumigatus-specific IgE and IgG antibodies. If the<br />
levels are raised, the patient is followed up every 6 weeks<br />
with total IgE levels. If the absolute value rises 1,000<br />
IU/mL or there is a rising trend with clinical deterioration,<br />
the treatment is started. If the value is between 500 and<br />
1,000 IU/mL and IgE and IgG specific to A fumigatus are<br />
not raised, the patient is followed up with a yearly total<br />
IgE levels (Fig 5).<br />
Natural History<br />
The natural history of ABPA is not well characterized.<br />
9,128,133–136 An early diagnosis and initiation of<br />
systemic corticosteroids are essential to prevent irreversible<br />
damage. 137 The natural course of ABPA can<br />
be best understood if we recognize the two important<br />
classification schemes (Tables 6 and 7) of ABPA:<br />
(1) classification of ABPA into five stages as described<br />
by Patterson et al 8 , and (2) classification of<br />
ABPA into ABPA-S (seropositive ABPA) and ABPA-CB<br />
(ABPA with central bronchiectasis) described by<br />
Greenberger et al. 12<br />
Staging of ABPA: ABPA has been classified into<br />
five stages, but a patient does not necessarily<br />
progress from one stage to the other sequentially<br />
(Table 6). Patients in stage I or III (depending on<br />
whether or not the disorder has been previously<br />
diagnosed) are generally symptomatic with radiographic<br />
infiltrates, raised IgE levels, and elevated A<br />
fumigatus-specific IgG/IgE. 23 With glucocorticoid<br />
therapy, there is clearing of radiographic opacities<br />
with a 35 to 50% decline in IgE levels by 6 weeks<br />
that defines remission or stage II. The aim of<br />
glucocorticoid therapy is not normalization of total<br />
IgE levels because the immunologic process goes in<br />
remission with just 35 to 50% decline in IgE levels,<br />
and in many patients the IgE levels do not come to<br />
down to normal values. The test needs to be often<br />
repeated during therapy to determine the lowest<br />
level for an individual patient that serves as the<br />
baseline for that particular patient. Treatment is<br />
continued for 6 to 9 months, and if there are no<br />
exacerbations over the next 3 months after stopping<br />
therapy, we label it as “complete remission.” Patients<br />
in complete remission are followed up by serial IgE<br />
levels every 6 months for the first year and then<br />
annually. Even in patients with complete remission,<br />
the IgE levels decline to normal in only a minority of<br />
patients, 128,133 and the aim of glucocorticoid therapy<br />
is not achievement of normal IgE levels. 79 A complete<br />
remission does not imply a permanent remission<br />
because exacerbations can occur several years<br />
after remission. 135 Almost 25 to 50% of the patients<br />
have relapse/exacerbation of the disease, defined by<br />
doubling of the baseline IgE levels (stage III). 8,9,22<br />
Patients in stage IV require oral glucocorticoids for<br />
control of asthma (glucocorticoid-dependent asthma)<br />
or ABPA (glucocorticoid-dependent ABPA). 10,22 Patients<br />
in stage V are those with widespread bronchiectasis<br />
and varying degrees of pulmonary dysfunction.<br />
We define patients in stage V if they have<br />
hypercapnic respiratory failure (Pao 2 60 mm Hg<br />
and Paco 2 45 mm Hg) and/or cor pulmonale.<br />
Even in stage V ABPA, the disease can be clinically<br />
as well as immunologically active requiring longterm<br />
glucocorticoid therapy. 136,138<br />
812 Global Medicine<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
Figure 5. Algorithm followed in the diagnostic workup for allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in the author’s chest clinic.<br />
Radiologic Classification of ABPA: ABPA is classified<br />
as ABPA-S or ABPA-CB, respectively, depending<br />
on the absence or presence of bronchiectasis<br />
or as ABPA-S (mild), ABPA-CB (moderate),<br />
and ABPA-CB-ORF (other radiologic findings)<br />
(Table 7). Patients with ABPA-S probably represent<br />
the earliest stage of the disorder. It is believed<br />
that patients with ABPA-S have a milder<br />
www.chestjournal.org <strong>CHEST</strong> / 135 /3/MARCH, 2009 813<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
clinical course and less severe immunologic findings<br />
when compared to ABPA-CB based on the<br />
inference of three studies (total of 124 patients).<br />
12,139,140 In the largest of these three studies<br />
(76 patients), only the A fumigatus-specific IgG<br />
levels were higher in patients with ABPA-CB<br />
compared to ABPA-S. Other immunologic parameters<br />
were not significantly different between the<br />
two groups. 12 In our study of 126 patients, the<br />
clinical, spirometric, and immunologic findings<br />
were not significantly different when classifying<br />
ABPA into ABPA-S and ABPA-CB or as ABPA-S,<br />
ABPA-CB, and ABPA-CB-ORF. 22<br />
However, the course of patients with ABPA-S is<br />
likely to be less severe when compared to those with<br />
ABPA-CB. In a multivariate analysis of 155 patients<br />
with ABPA, we demonstrated that the severity of<br />
bronchiectasis and presence of hyperattenuating<br />
mucoid impaction on HRCT-predicted relapses of<br />
ABPA and the severity of bronchiectasis was an<br />
independent predictor of failure to achieve longterm<br />
remission. 23 Thus it may not be important to<br />
stage the severity of ABPA based on the presence<br />
or absence of CB, but it remains prudent to<br />
diagnose and treat ABPA early to prevent the<br />
development of bronchiectasis because it in-<br />
Table 6—Stages of ABPA 8,22<br />
Stage Description Clinical Picture Radiologic Findings Immunologic Features<br />
I Acute phase Usually symptomatic,<br />
fever, weight loss,<br />
wheeze<br />
Normal or presence of<br />
radiologic opacities<br />
II Remission Asymptomatic Generally normal or significant<br />
resolution of radiologic<br />
opacities from the acute<br />
phase<br />
III Exacerbation Symptomatic as in acute Transient or fixed pulmonary<br />
phase<br />
opacities<br />
IV Glucocorticoid-dependent Symptomatic Transient or fixed pulmonary<br />
ABPA<br />
opacities<br />
V End-stage (fibrotic)<br />
ABPA<br />
Symptomatic, findings of<br />
fixed airway<br />
obstruction, severe<br />
pulmonary<br />
dysfunction, type II<br />
respiratory failure, cor<br />
pulmonale<br />
Evidence of bronchiectasis,<br />
pulmonary fibrosis,<br />
pulmonary hypertension<br />
IgE 1,000 IU/mL, raised<br />
specific IgG/IgE and<br />
precipitins to A fumigatus<br />
Usually 35–50% decline in IgE<br />
levels by 6 wk to 3 mo; we<br />
give additional label of<br />
“complete remission” if the<br />
patient did not have any<br />
additional ABPA exacerbations<br />
over the next 3 mo after<br />
stopping steroid therapy<br />
Doubling of IgE levels from<br />
baseline<br />
Two groups can be identified:<br />
one in whom IgE levels do not<br />
rise but require steroids for<br />
asthma control (glucocorticoiddependent<br />
asthma); the other<br />
in whom steroids are required<br />
to continually suppress the<br />
disease activity (glucocorticoiddependent<br />
ABPA)<br />
Serum IgE levels and specific<br />
immunoglobulins do not<br />
become normal in most<br />
patients, and even these<br />
patients can have frequent<br />
exacerbations<br />
creases the probability of a smoother course of this<br />
relapsing-remitting disorder.<br />
Management<br />
The management of ABPA includes two important<br />
aspects: institution of glucocorticoids to control the<br />
immunologic activity and close monitoring for detection<br />
of relapses. Another possible target is the use of<br />
antifungal agents to attenuate the fungal burden<br />
secondary to the fungal colonization in the airways.<br />
Systemic Glucocorticoid Therapy: Oral corticosteroids<br />
are the treatment of choice for ABPA. They not<br />
only suppress the immune hyperfunction but are also<br />
antiinflammatory. There are no data to guide the<br />
dose and duration of glucocorticoids, and different<br />
regimens of glucocorticoids have been used (Table<br />
8). The use of lower doses of glucocorticoids was<br />
associated with frequent relapses or corticosteroid<br />
dependence (45%). 9 We use a higher dosage of<br />
glucocorticoids for a longer duration and observed<br />
higher remission rates and a lower prevalence of<br />
glucocorticoid-dependent ABPA (13.5%). 22 This<br />
raises the possibility of a higher dose and prolonged<br />
duration of corticosteroid therapy being associated<br />
814 Global Medicine<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
Table 7—Radiologic Classification of ABPA*<br />
Classification Features<br />
Greenberger et al12 classification<br />
ABPA-S All the diagnostic features of ABPA<br />
but no evidence of central<br />
bronchiectasis on HRCT.<br />
Patients with ABPA-S may be<br />
classified as Patterson stages I to<br />
IV. These patients may have<br />
recurrent exacerbations and may<br />
also be classified as stage III<br />
(ABPA-CB) All findings of ABPA including CB<br />
on HRCT. Patients with ABPA-<br />
CB may belong to any of the<br />
Patterson stages<br />
Kumar140 classification<br />
ABPA-S ABPA without CB<br />
ABPA-CB ABPA with CB<br />
ABPA-CB-ORF ABPA with CB other radiologic<br />
features such as pulmonary<br />
fibrosis, bleb, bullae,<br />
pneumothorax, parenchymal<br />
scarring, emphysematous change,<br />
multiple cyst, fibrocavitary<br />
lesions, aspergilloma, groundglass<br />
appearance, collapse,<br />
mediastinal lymph node, pleural<br />
effusion, and pleural thickening<br />
*Both the classification schemes believe that patients without CB and<br />
ORF have serologically milder disease, but it has been shown that<br />
there is no difference in clinical, spirometric, and serological<br />
severity between patients with and without bronchiectasis (see text<br />
for details).<br />
with better outcomes. However, there are no direct<br />
comparisons between the two regimens, and the<br />
selection is a matter of personal preference. The<br />
clinical effectiveness of steroid therapy is reflected<br />
by marked decreases in the patient’s total serum IgE<br />
levels (there seems to be no correlation between<br />
serum levels of A fumigatus-specific IgE levels and<br />
disease activity 141 ) along with symptom and radiographic<br />
improvements. The goal of therapy is not to<br />
attempt normalization of IgE levels but to decrease<br />
the IgE levels by 35 to 50%, which leads to clinical<br />
and radiographic improvement. One should also<br />
establish a stable serum level of total IgE to serve as<br />
a guide to future detection of relapse.<br />
Inhaled Corticosteroids: Although small case studies<br />
suggest some benefit of inhaled corticosteroids in<br />
the management of ABPA, 142–145 a double-blind multicenter<br />
placebo-controlled trial in 32 patients suggested<br />
no superiority over placebo. 146 We use inhaled<br />
corticosteroids only for the control of asthma once the<br />
oral prednisolone dose is reduced to 10 mg/day.<br />
Oral Itraconazole: Ketoconazole has been tried in<br />
the past 147 and has been replaced by the less toxic<br />
Table 8—Treatment Protocols for the Management of<br />
ABPA<br />
Oral glucocorticoids<br />
Regime 1 5<br />
Prednisolone, 0.5 mg/kg/d, for 1–2 wk, then on alternate days<br />
for 6–8 wk. Then taper by 5–10 mg every 2 wk and<br />
discontinue<br />
Repeat the total serum IgE concentration and chest<br />
radiograph in 6 to 8 wk<br />
Regime 2 22,113<br />
Prednisolone, 0.75 mg/kg, for 6 wk, 0.5 mg/kg for 6 wk, then<br />
tapered by 5 mg every 6 wk to continue for a total duration<br />
of at least 6 to 12 mo. The total IgE levels are repeated<br />
every 6 to 8 wk for 1 yr to determine the baseline IgE<br />
concentrations<br />
Follow-up and monitoring<br />
The patients are followed up with a medical history and<br />
physical examination, chest radiograph, and measurement of<br />
total IgE levels every 6 wk to demonstrate decline in IgE<br />
levels and clearing of the chest radiograph<br />
A 35% decline in IgE level signifies satisfactory response to<br />
therapy. Doubling of the baseline IgE value can signify a<br />
silent ABPA exacerbation<br />
If the patient cannot be tapered off prednisolone, the disease<br />
has evolved into stage IV. Management should be<br />
attempted with alternate-day prednisone with the least<br />
possible dose<br />
Monitor for adverse effects (eg, hypertension, secondary<br />
diabetes)<br />
Prophylaxis for osteoporosis: oral calcium and bisphosphonates<br />
Oral itraconazole<br />
Dose: 200 mg bid for 16 wk then once a day for 16 wk<br />
Indication: First relapse of ABPA or glucocorticoid-dependent<br />
ABPA<br />
Follow-up and monitoring<br />
Monitor for adverse effects (eg, nausea, vomiting, diarrhea,<br />
and elevated liver enzymes)<br />
Monitor for drug–drug interactions<br />
Monitor clinical response based on clinical course,<br />
radiography, and total IgE levels<br />
agent, itraconazole. 130,141,148–160 Only two randomized<br />
controlled studies (84 patients) have evaluated<br />
the role of itraconazole in ABPA. 130,156 Pooled analysis<br />
showed that itraconazole could significantly decrease<br />
the IgE levels by 25% when compared to<br />
placebo but did not cause significant improvement in<br />
lung function. 161 A major limitation was that neither<br />
of the studies reported long-term outcomes in<br />
ABPA. Thus longer term trials are required before a<br />
firm recommendation can be made for the use of<br />
itraconazole in ABPA. We currently use itraconazole<br />
only after the first relapse of ABPA despite glucocorticoid<br />
therapy or in patients with glucocorticoiddependent<br />
ABPA (Table 8). In the limited numbers<br />
of patients in whom we have used the drug, there<br />
was no observable advantage. 22 Itraconazole not only<br />
has numerous adverse effects, 162 but it also inhibits<br />
the metabolism of methylprednisolone (but not<br />
prednisolone) with resultant increased frequency of<br />
www.chestjournal.org <strong>CHEST</strong> / 135 /3/MARCH, 2009 815<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
Table 9—Studies Describing Prevalence of AH and/or ABPA in Patients With CF<br />
Study Year Nature of Study Patients, No. AH in CF ABPA* in CF Diagnosis of AH†<br />
Mearns et al 184<br />
1967 Prospective 86 28/86 Skin test<br />
Allan et al 185<br />
1975 Prospective 30 11/30 Skin test<br />
Silverman et al 186<br />
1978 Prospective 48 17 Skin test<br />
Nelson et al 187<br />
1979 Prospective 46 18/46 5/46 Skin test<br />
Laufer et al 177<br />
1984 Prospective 100 53/100 10/100 Skin test<br />
Feanny et al 188<br />
1988 Prospective 117 18/117 12/117 Skin test<br />
Schonheyder et al 189<br />
1988 Prospective 200 10/200<br />
Zeaske et al 190<br />
1988 Prospective 75 44/75 10/75 Skin test<br />
Knutsen et al 176<br />
1990 Prospective 73 18/73 9/73 Skin test<br />
Nicolai et al 179<br />
1990 Prospective 148 58/148 Serology<br />
Simmonds et al 191<br />
1990 Prospective 137 8/137<br />
Hutcheson et al 192<br />
1991 Prospective 79 24/79 Skin test<br />
el-Dahr et al 193<br />
1994 Prospective 147 30/147 22/147 Serology<br />
Marchant et al 194<br />
1994 Retrospective 160 16/160 Skin test<br />
Mroueh and Spock 178<br />
1994 Retrospective 236 38/87 15/236 Skin test<br />
Becker et al 181<br />
1996 Prospective 53 15/51 1/53 Skin test<br />
Hutcheson et al 195<br />
1996 Prospective 118 47/112 6/118 Skin test<br />
Geller et al 182<br />
1999 Prospective 14,210 281/14,210<br />
Nepomuceno et al 153<br />
1999 Retrospective 172 16/172<br />
Cimon et al 196<br />
2000 Prospective 128 5/128<br />
Mastella et al 174<br />
2000 Prospective 12,447 967/12,447<br />
Taccetti et al 197<br />
2000 Prospective 3,089 191/3,089<br />
Ritz et al 180<br />
2005 Prospective 160 20/160 11/160 Serology<br />
Skov et al 183<br />
2005 Retrospective 277 13/277<br />
Almeida et al 198<br />
2006 Prospective 32 11/32 2/32 Skin test<br />
Kraemer et al 173<br />
2006 Prospective 122 16/122<br />
Chotirmall et al 199<br />
2008 Prospective 50 6/50<br />
Rapaka and Kolls 200<br />
2008 Retrospective 440 31/440<br />
* ABPA: Studies have used different inclusion criteria for diagnosing ABPA. See text for further details.<br />
† AH: Defined as immediate cutaneous hypersensitivity to Aspergillus antigen or a positive specific IgE in serum against A fumigatus<br />
(radioallergosorbent test class 2) and/or increased specific IgE in serum against rAsp f1 9.6 EU/mL, with normal values for rAsp f4 ( 8.4<br />
EU/mL) and rAsp f6 ( 7.2 EU/mL)<br />
steroid side effects including adrenal insufficiency. 163<br />
Adrenal suppression has also been reported with the<br />
concomitant use of itraconazole and inhaled budesonide.<br />
164,165<br />
Other Therapies: There is a single patient case<br />
report of ABPA treated with inhaled amphotericin<br />
and budesonide. 166 Similarly, there is another case<br />
record on the use of omalizumab for the management<br />
of ABPA. 167 One author has also used pulse<br />
doses of IV methylprednisolone for the treatment of<br />
severe ABPA. 168 Recently, voriconazole has also<br />
been tried in the treatment of ABPA. 169–171<br />
Differential Diagnosis and Complications<br />
The disorder needs to be differentiated from the<br />
following conditions: Aspergillus hypersensitive<br />
bronchial asthma, pulmonary tuberculosis in endemic<br />
areas, community-acquired pneumonia (especially<br />
acute presentations), and other inflammatory<br />
pulmonary disorders such as eosinophilic pneumonia,<br />
bronchocentric granulomatosis, and Churg-<br />
Strauss syndrome. The complications of ABPA in-<br />
clude recurrent asthma exacerbations and, if<br />
untreated, the development of bronchiectasis with<br />
subsequent pulmonary hypertension and respiratory<br />
failure. In fact, this is the reason why routine screening<br />
is recommended in bronchial asthma to prevent<br />
the complications just described.<br />
ABPA in Special Situations<br />
ABPA Complicating CF: The association of ABPA<br />
and CF was first reported in 1965. 172 The occurrence<br />
of ABPA in CF is associated with deterioration<br />
of lung function, higher rates of microbial colonization,<br />
pneumothorax, massive hemoptysis, and poorer<br />
nutritional status. 153,173,174 A key element in the<br />
immunopathogenesis may be exposure to high levels<br />
of Aspergillus allergens due to abnormal mucus<br />
properties. 175 The recognition of ABPA in CF can be<br />
difficult because ABPA shares many clinical characteristics<br />
with poorly controlled CF lung disease.<br />
Presence of wheezing, pulmonary infiltrates, bronchiectasis,<br />
and mucus plugging are common manifestations<br />
of CF-related pulmonary disease without<br />
ABPA. The prevalence of AH in patients with CF<br />
816 Global Medicine<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
has been reported between 29% and 53%, 176–180 and<br />
the prevalence of ABPA as 1 to 15%. Atopy seems to<br />
be an important risk factor for ABPA in CF, with<br />
ABPA observed in 22% of atopic patients but only<br />
2% of nonatopic patients. 153,181–183<br />
To determine the prevalence of AH/ABPA in CF,<br />
a systematic search was performed. The search<br />
yielded 28 studies (16 studies [1,391 patients] describing<br />
the prevalence of AH in CF and 23<br />
studies [32,589 patients] describing the prevalence<br />
of ABPA in CF) that have described the prevalence<br />
of AH and/or ABPA in patients with CF<br />
(Table 9). 153,173,174,176–200 A proportion metaanalysis of<br />
these studies suggested the prevalence of AH in CF<br />
of 34% (95% confidence interval, 27 to 41) and the<br />
prevalence of ABPA of 7.8% (95% confidence interval,<br />
5.8 to 10) using a random effects model [Figs 6<br />
and 7]. There was no uniformity in the diagnostic<br />
criteria between different studies with varying criteria<br />
used for diagnosis of AH and ABPA. This fact has<br />
also been previously reported in a questionnairebased<br />
study, which revealed a considerable variability<br />
in the criteria used for the diagnosis of ABPA in<br />
CF. 201 Therefore, prospective reporting of cases with<br />
uniform criteria would be the only way to reliably<br />
identify the true prevalence of ABPA in CF.<br />
Although a high proportion of CF patients develop<br />
sensitization to A fumigatus, many demonstrate a<br />
spontaneous decline in many immunologic parameters,<br />
including IgE levels. 192 The diagnosis of ABPA<br />
Figure 6. Proportion metaanalysis showing the prevalence of Aspergillus hypersensitivity in patients with cystic fibrosis (random effects<br />
model).<br />
www.chestjournal.org <strong>CHEST</strong> / 135 /3/MARCH, 2009 817<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
Figure 7. Proportion metaanalysis showing the prevalence of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in patients with CF (random<br />
effects model).<br />
in CF should not be based solely on serology and<br />
skin test results, and prolonged testing might be<br />
required to make a definite diagnosis (Table 10). The<br />
treatment of ABPA in CF is not very different from<br />
that of ABPA in bronchial asthma, except minimal<br />
data are available to formulate conclusive treatment<br />
recommendations for ABPA in CF. The treatment<br />
issues are further complicated because pulmonary<br />
exacerbations in a patient with ABPA and CF could<br />
be related to ABPA or pulmonary infection, and<br />
818 Global Medicine<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
Table 10—Consensus Conference Proposed Diagnostic<br />
and Screening Criteria for ABPA in CF 202<br />
Classic diagnostic criteria<br />
1. Acute or subacute clinical deterioration (cough, wheeze, and<br />
other pulmonary symptoms) not explained by another etiology<br />
2. Serum total IgE levels 1,000 IU/mL<br />
3. Immediate cutaneous reactivity to Aspergillus or presence of<br />
serum IgE antibody to A fumigatus<br />
4. Precipitating antibodies to A fumigatus or serum IgG antibody<br />
to A fumigatus<br />
5. New or recent abnormalities on chest radiograph or chest CT<br />
scan that have not cleared with antibiotics and standard<br />
physiotherapy<br />
Minimal diagnostic criteria<br />
1. Acute or subacute clinical deterioration (cough, wheeze, and<br />
other pulmonary symptoms) not explained by another etiology<br />
2. Total serum IgE levels 500 IU/mL. If total IgE level is 200–<br />
500 IU/mL, repeat testing in 1–3 mo is recommended<br />
3. Immediate cutaneous reactivity to Aspergillus or presence of<br />
serum IgE antibody to A fumigatus<br />
4. One of the following: (1) precipitins to A fumigatus or<br />
demonstration of IgG antibody to A fumigatus; or (2) new or<br />
recent abnormalities on chest radiography (on chest radiography<br />
or chest CT scan that have not cleared with antibiotics and<br />
standard physiotherapy)<br />
Screening for ABPA in CF<br />
1. Maintain a high level of suspicion for ABPA in patients with CF<br />
2. Determine the total serum IgE levels annually. If the total<br />
serum IgE levels is 500 IU/mL, perform A fumigatus skin test<br />
or use an IgE antibody to A fumigatus. If results are positive,<br />
consider diagnosis on the basis of minimal criteria<br />
3. If the total serum IgE levels is 200–500 IU/mL, repeat the<br />
measurement if there is increased suspicion for ABPA and perform<br />
further diagnostic tests (immediate skin test reactivity to A<br />
fumigatus, IgE antibody to A fumigatus, A fumigatus precipitins, or<br />
serum IgG antibody to A fumigatus, and chest radiography)<br />
hence continuous assessment may be required over<br />
months with repeat performance of all the serologic<br />
investigations for ABPA before a decision to treat an<br />
individual case is made. 202<br />
ABPA Without Bronchial Asthma: ABPA may<br />
occasionally develop in an individual without preexisting<br />
asthma. We have performed a systematic<br />
MEDLINE search for the occurrence of ABPA<br />
without bronchial asthma. 100 In total they included<br />
36 cases reported across the globe; two cases demonstrated<br />
bronchodilator reversibility, 203 and one<br />
showed airway hyperresponsiveness to methacholine<br />
challenge. 204 Most of the cases demonstrated hypersensitivity<br />
to A fumigatus, but three cases<br />
showed hypersensitivity to Helminthosporium, 203<br />
and one case each to Aspergillus niger. 205,206 Because<br />
of the absence of bronchial asthma, these<br />
cases are often mistaken initially for other pulmonary<br />
disorders like bronchogenic carcinoma 206–208<br />
or pulmonary tuberculosis. 100<br />
ABPA Complicating Other Conditions: Occasionally<br />
ABPA has been reported to complicate other<br />
lung diseases like idiopathic bronchiectasis, 209<br />
post-tubercular bronchiectasis, 210 bronchiectasis<br />
secondary to Kartagener syndrome, 211 COPD, 212<br />
and in patients with chronic granulomatous disease<br />
and hyper IgE syndrome. 213 However, these<br />
are case reports or small case studies, and larger<br />
observations are required to definitely establish an<br />
association.<br />
Coexistence of ABPA and Aspergilloma: The serologic<br />
findings of ABPA have also been reported in<br />
patients with aspergilloma 214–224 and chronic necrotizing<br />
pulmonary <strong>aspergillosis</strong>. 225 This ABPA-like<br />
syndrome probably represents a true hypersensitivity<br />
reaction consequent to the colonization of Aspergillus<br />
in long-standing pulmonary cavities and the<br />
continuous release of Aspergillus antigens that leads<br />
to immunologic activation. 214,215 Most patients show<br />
a brisk response to glucocorticoids. 214–217,224<br />
<strong>Allergic</strong> Bronchopulmonary Mycosis: <strong>Allergic</strong><br />
<strong>bronchopulmonary</strong> mycosis is the occurrence of an<br />
ABPA-like syndrome due to non-A fumigatus fungal<br />
organisms. A variety of fungal agents (Table 11) have<br />
been reported to cause this syndrome, but the frequency<br />
is far less when compared to ABPA. 218,226–240<br />
ABPA and <strong>Allergic</strong> Aspergillus Sinusitis: <strong>Allergic</strong><br />
Aspergillus sinusitis (AAS) is a clinical entity in which<br />
mucoid impaction akin to that of ABPA occurs in the<br />
paranasal sinuses. 241 The pathogenesis is also similar<br />
to ABPA and represents an allergic hypersensitivity<br />
response to the presence of fungi within the sinus<br />
cavity. 242 The patient is often asymptomatic or can<br />
manifest with symptoms of nasal obstruction, rhinor-<br />
Table 11—Fungi Implicated in the Causation of<br />
<strong>Allergic</strong> Bronchopulmonary Mycosis<br />
Fungi Study/Year<br />
A niger Sharma et al 218 /1985<br />
Helminthosporium spp Dolan et al 226 /1970<br />
Penicillium spp Sahn and Lakshminarayan 227 /1973<br />
Aspergillus ochraceus Novey and Wells 228 /1978<br />
Stemphylium spp Benatar et al 229 /1980<br />
Aspergillus terreus Laham et al 230 /1981<br />
Drechslera spp McAleer et al 231 /1981<br />
Torulopsis spp Patterson et al 232 /1982<br />
Mucor-like spp Patterson et al 232 /1982<br />
Candida spp Akiyama et al 234 /1984<br />
Pseudallescheria spp Lake et al 235 /1990<br />
Bipolaris spp Lake et al 236 /1991<br />
Curvularia spp Lake et al 236 /1991<br />
Schizophyllum spp Kamei et al 237 /1994<br />
Fusarium spp Backman et al 238 /1995<br />
Cladosporium spp Moreno-Ancillo et al 239 /1996<br />
Saccharomyces spp Ogawa et al 240 /2004<br />
www.chestjournal.org <strong>CHEST</strong> / 135 /3/MARCH, 2009 819<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
hea, headache, and epistaxis. Occasionally, the<br />
allergic fungal sinusitis may extend into adjacent<br />
spaces such as the orbit and manifest as proptosis.<br />
243 Although in many patients with ABPA,<br />
sinusitis can often be radiologically demonstrated,<br />
it may not be possible to confirm the diagnosis of<br />
AAS because many patients decline to undergo the<br />
diagnostic procedures required to establish the<br />
diagnosis. We currently label the patients with<br />
ABPA as having concomitant AAS if there is<br />
combination of hyperattenuating mucus and/or<br />
bony erosion on a paranasal CT scan. Treatment is<br />
initiated for ABPA with patients receiving additional<br />
intranasal glucocorticoids. If the symptoms<br />
persist or are troublesome, surgical management<br />
may be required for the management of AAS.<br />
Conclusions<br />
A high index of suspicion for ABPA should be<br />
maintained while managing any patient with bronchial<br />
asthma whatever the severity or the level of<br />
control. Host immunologic responses are central to<br />
the pathogenesis, and they are the primary determinants<br />
of the clinical, biologic, pathologic, and radiologic<br />
features of this disorder. ABPA may precede<br />
the clinical recognition of the disorder for many<br />
years or even decades, and it is often misdiagnosed as<br />
a variety of pulmonary diseases. Because a patient<br />
with ABPA can be minimally symptomatic or asymptomatic,<br />
all patients with bronchial asthma should be<br />
routinely screened with an Aspergillus skin test. In<br />
patients with Aspergillus hypersensitivity, further<br />
immunologic studies are warranted to diagnose<br />
ABPA before the development of bronchiectasis<br />
because bronchiectasis is a poor prognostic marker<br />
in the natural history of this disease.<br />
ACKNOWLEDGMENT: The author wishes to thank Dr. Amanjit<br />
Bal, Assistant Professor, Department of Histopathology,<br />
PGIMER, Chandigarh for providing the histopathology photographs.<br />
References<br />
1 Bardana EJ Jr. The clinical spectrum of <strong>aspergillosis</strong>—part<br />
1: epidemiology, pathogenicity, infection in animals and<br />
immunology of Aspergillus. Crit Rev Clin Lab Sci 1981;<br />
13:21–83<br />
2 Geiser DM, Klich MA, Frisvad JC, et al. The current status<br />
of species recognition and identification in Aspergillus. Stud<br />
Mycol 2007; 59:1–10<br />
3 Walsh TJ, Anaissie EJ, Denning DW, et al. Treatment of<br />
<strong>aspergillosis</strong>: clinical practice guidelines of the infectious<br />
diseases society of America. Clin Infect Dis 2008; 46:327–<br />
360<br />
4 Soubani AO, Chandrasekar PH. The clinical spectrum of<br />
pulmonary <strong>aspergillosis</strong>. Chest 2002; 121:1988–1999<br />
5 Greenberger PA. <strong>Allergic</strong> <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
J Allergy Clin Immunol 2002; 110:685–692<br />
6 Rosenberg M, Patterson R, Mintzer R, et al. Clinical and<br />
immunologic criteria for the diagnosis of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Ann Intern Med 1977; 86:405–414<br />
7 Greenberger PA, Patterson R, Ghory A, et al. Late sequelae<br />
of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. J Allergy Clin<br />
Immunol 1980; 66:327–335<br />
8 Patterson R, Greenberger PA, Radin RC, et al. <strong>Allergic</strong><br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong>: staging as an aid to management.<br />
Ann Intern Med 1982; 96:286–291<br />
9 Patterson R, Greenberger PA, Halwig JM, et al. <strong>Allergic</strong><br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong>: natural history and classification<br />
of early disease by serologic and roentgenographic<br />
studies. Arch Intern Med 1986; 146:916–918<br />
10 Patterson R, Greenberger PA, Lee TM, et al. Prolonged<br />
evaluation of patients with corticosteroid-dependent asthma<br />
stage of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. J Allergy<br />
Clin Immunol 1987; 80:663–668<br />
11 Greenberger PA, Patterson R. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> and the evaluation of the patient with asthma.<br />
J Allergy Clin Immunol 1988; 81:646–650<br />
12 Greenberger PA, Miller TP, Roberts M, et al. <strong>Allergic</strong><br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in patients with and without<br />
evidence of bronchiectasis. Ann Allergy 1993; 70:333–338<br />
13 Greenberger PA. Clinical aspects of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Front Biosci 2003; 8:S119–S127<br />
14 Rajan TV. The Gell-Coombs classification of hypersensitivity<br />
reactions: a re-interpretation. Trends Immunol 2003; 24:376–<br />
379<br />
15 Geha RS, Sampson HA, Askenase PW, et al. Allergy and<br />
hypersensitivity. In: Janeway CA, Travers P, Walport M, et al.<br />
eds. Immunobiology. New York, NY: Garland, 2001; 517–556<br />
16 Hinson KFW, Moon AJ, Plummer NS. Broncho-pulmonary<br />
<strong>aspergillosis</strong>; a review and a report of eight new cases.<br />
Thorax 1952; 7:317–333<br />
17 Muscat I, Oxborrow S, Siddorn J. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
mycosis. Lancet 1988; 1:1341<br />
18 Kirsten D, Nowak D, Rabe KF, et al. [Diagnosis of <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> is often made too late]. Med Klin<br />
(Munich) 1993; 88:353–356<br />
19 Behera D, Guleria R, Jindal SK, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>: a retrospective study of 35 cases.<br />
Indian J Chest Dis Allied Sci 1994; 36:173–179<br />
20 Al-Mobeireek AF, El-Rab M, Al-Hedaithy SS, et al. <strong>Allergic</strong><br />
<strong>bronchopulmonary</strong> mycosis in patients with asthma: period<br />
prevalence at a university hospital in Saudi Arabia. Respir<br />
Med 2001; 95:341–347<br />
21 Chakrabarti A, Sethi S, Raman DS, et al. Eight-year study of<br />
allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in an Indian teaching<br />
hospital. Mycoses 2002; 45:295–299<br />
22 Agarwal R, Gupta D, Aggarwal AN, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>: lessons from 126 patients attending<br />
a chest clinic in North India. Chest 2006; 130:442–448<br />
23 Agarwal R, Gupta D, Aggarwal AN, et al. Clinical significance<br />
of hyperattenuating mucoid impaction in allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong>: an analysis of 155 patients.<br />
Chest 2007; 132:1183–1190<br />
24 Agarwal R, Chakrabarti A. Epidemiology of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. In: Pasqualotto A, ed. Aspergillosis:<br />
from diagnosis to prevention. New York, NY:<br />
Springer, 2009 (in press)<br />
25 Bateman ED. A new look at the natural history of Aspergillus<br />
hypersensitivity in asthmatics. Respir Med 1994; 88:325–<br />
327<br />
26 Malde B, Greenberger PA. <strong>Allergic</strong> <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
Allergy Asthma Proc 2004; 25:S38–S39<br />
820 Global Medicine<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
27 Tillie-Leblond I, Tonnel AB. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Allergy 2005; 60:1004–1013<br />
28 Donnelly SC, McLaughlin H, Bredin CP. Period prevalence<br />
of allergic <strong>bronchopulmonary</strong> mycosis in a regional hospital<br />
outpatient population in Ireland 1985–88. Ir J Med Sci<br />
1991; 160:288–290<br />
29 Novey HS. Epidemiology of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Immunol Allergy Clin North Am 1998; 18:641–<br />
653<br />
30 Agarwal R, Aggarwal AN, Gupta D, et al. Prevalence of<br />
Aspergillus hypersensitivity and allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> in patients with bronchial asthma: a systematic<br />
review and meta-analysis. Int J Tuberc Lung Dis 2009 (in<br />
press)<br />
31 Attapattu MC. <strong>Allergic</strong> <strong>bronchopulmonary</strong> <strong>aspergillosis</strong><br />
among asthmatics. Ceylon Med J 1991; 36:45–51<br />
32 Schwartz HJ, Greenberger PA. The prevalence of allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in patients with asthma,<br />
determined by serologic and radiologic criteria in patients at<br />
risk. J Lab Clin Med 1991; 117:138–142<br />
33 Eaton T, Garrett J, Milne D, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> in the asthma clinic: a prospective evaluation<br />
of CT in the diagnostic algorithm. Chest 2000; 118:<br />
66–72<br />
34 Kumar R, Gaur SN. Prevalence of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> in patients with bronchial asthma. Asian<br />
Pac J Allergy Immunol 2000; 18:181–185<br />
35 Maurya V, Gugnani HC, Sarma PU, et al. Sensitization to<br />
Aspergillus antigens and occurrence of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> in patients with asthma. Chest 2005;<br />
127:1252–1259<br />
36 Prasad R, Garg R, Sanjay, et al. A study on prevalence of<br />
allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in patients of bronchial<br />
asthma. Internet J Pulmonary Med 2008; 9<br />
37 Agarwal R, Nath A, Aggarwal AN, et al. Aspergillus hypersensitivity<br />
and allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in<br />
patients with acute severe asthma in a respiratory ICU in<br />
North India. Mycoses 2009 (in press)<br />
38 Henderson AH. <strong>Allergic</strong> <strong>aspergillosis</strong>: review of 32 cases.<br />
Thorax 1968; 23:513–523<br />
39 Kramer MN, Kurup VP, Fink JN. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> from a contaminated dump site. Am Rev<br />
Respir Dis 1989; 140:1086–1088<br />
40 Kagen SL, Kurup VP, Sohnle PG, et al. Marijuana smoking<br />
and fungal sensitization. J Allergy Clin Immunol 1983;<br />
71:389–393<br />
41 Allmers H, Huber H, Baur X. Two year follow-up of a<br />
garbage collector with allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong><br />
(ABPA). Am J Ind Med 2000; 37:438–442<br />
42 Chauhan B, Knutsen A, Hutcheson PS, et al. T cell subsets,<br />
epitope mapping, and HLA-restriction in patients with<br />
allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. J Clin Invest 1996;<br />
97:2324–2331<br />
43 Miller PW, Hamosh A, Macek M Jr, et al. Cystic fibrosis<br />
transmembrane conductance regulator (CFTR) gene mutations<br />
in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Am J Hum<br />
Genet 1996; 59:45–51<br />
44 Aron Y, Bienvenu T, Hubert D, et al. HLA-DR polymorphism<br />
in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. J Allergy<br />
Clin Immunol 1999; 104:891–892<br />
45 Chauhan B, Santiago L, Hutcheson PS, et al. Evidence for<br />
the involvement of two different MHC class II regions in<br />
susceptibility or protection in allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. J Allergy Clin Immunol 2000; 106:723–729<br />
46 Marchand E, Verellen-Dumoulin C, Mairesse M, et al. Frequency<br />
of cystic fibrosis transmembrane conductance regulator<br />
gene mutations and 5T allele in patients with allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Chest 2001; 119:762–767<br />
47 Eaton TE, Weiner Miller P, Garrett JE, et al. Cystic fibrosis<br />
transmembrane conductance regulator gene mutations: do<br />
they play a role in the aetiology of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>? Clin Exp Allergy 2002; 32:756–761<br />
48 Saxena S, Madan T, Shah A, et al. Association of polymorphisms<br />
in the collagen region of SP-A2 with increased levels<br />
of total IgE antibodies and eosinophilia in patients with<br />
allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. J Allergy Clin Immunol<br />
2003; 111:1001–1007<br />
49 Brouard J, Knauer N, Boelle PY, et al. Influence of interleukin-10<br />
on Aspergillus fumigatus infection in patients with<br />
cystic fibrosis. J Infect Dis 2005; 191:1988–1991<br />
50 Knutsen AP. Genetic and respiratory tract risk factors for<br />
<strong>aspergillosis</strong>: ABPA and asthma with fungal sensitization.<br />
Med Mycol 2006; 44(suppl 1):61–70<br />
51 Knutsen AP, Kariuki B, Consolino JD, et al. IL-4 alpha chain<br />
receptor (IL-4R) polymorphisms in allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Clin Mol Allergy 2006; 4:3<br />
52 Sambatakou H, Pravica V, Hutchinson IV, et al. Cytokine<br />
profiling of pulmonary <strong>aspergillosis</strong>. Int J Immunogenet<br />
2006; 33:297–302<br />
53 Vaid M, Kaur S, Sambatakou H, et al. Distinct alleles of<br />
mannose-binding lectin (MBL) and surfactant proteins A<br />
(SP-A) in patients with chronic cavitary pulmonary <strong>aspergillosis</strong><br />
and allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Clin<br />
Chem Lab Med 2007; 45:183–186<br />
54 Carvalho A, Pasqualotto AC, Pitzurra L, et al. Polymorphisms<br />
in toll-like receptor genes and susceptibility to<br />
pulmonary <strong>aspergillosis</strong>. J Infect Dis 2008; 197:618–621<br />
55 Tomee JF, Wierenga AT, Hiemstra PS, et al. Proteases from<br />
Aspergillus fumigatus induce release of proinflammatory<br />
cytokines and cell detachment in airway epithelial cell lines.<br />
J Infect Dis 1997; 176:300–303<br />
56 Tomee JF, Kauffman HF, Klimp AH, et al. Immunologic<br />
significance of a collagen-derived culture filtrate containing<br />
proteolytic activity in Aspergillus-related diseases. J Allergy<br />
Clin Immunol 1994; 93:768–778<br />
57 Hogaboam CM, Blease K, Schuh JM. Cytokines and chemokines<br />
in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> (ABPA)<br />
and experimental Aspergillus-induced allergic airway or<br />
asthmatic disease. Front Biosci 2003; 8:e147–e156<br />
58 Kauffman HF. Immunopathogenesis of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> and airway remodeling. Front Biosci<br />
2003; 8:e190–e196<br />
59 Kauffman HK, Tomee JFC. Inflammatory cells and airway<br />
defense against Aspergillus fumigatus. Immunol Allergy Clin<br />
North Am 1998; 18:619–640<br />
60 Kauffman HF, Tomee JF, van de Riet MA, et al. Proteasedependent<br />
activation of epithelial cells by fungal allergens<br />
leads to morphologic changes and cytokine production.<br />
J Allergy Clin Immunol 2000; 105:1185–1193<br />
61 Chauhan B, Santiago L, Kirschmann DA, et al. The<br />
association of HLA-DR alleles and T cell activation with<br />
allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. J Immunol 1997;<br />
159:4072–4076<br />
62 Schuyler M. The Th1/Th2 paradigm in allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. J Lab Clin Med 1998; 131:194–196<br />
63 Knutsen AP, Bellone C, Kauffman H. Immunopathogenesis<br />
of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in cystic fibrosis.<br />
J Cyst Fibros 2002; 1:76–89<br />
64 Slavin RG, Bedrossian CW, Hutcheson PS, et al. A<br />
pathologic study of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
J Allergy Clin Immunol 1988; 81:718–725<br />
65 Chan-Yeung M, Chase WH, Trapp W, et al. <strong>Allergic</strong> bron-<br />
www.chestjournal.org <strong>CHEST</strong> / 135 /3/MARCH, 2009 821<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
chopulmonary <strong>aspergillosis</strong>. Clinical and pathologic study of<br />
three cases. Chest 1971; 59:33–39<br />
66 Riley DJ, Mackenzie JW, Uhlman WE, et al. <strong>Allergic</strong><br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong>: evidence of limited tissue<br />
invasion. Am Rev Respir Dis 1975; 111:232–236<br />
67 Case records of the Massachusetts General Hospital.<br />
Weekly clinicopathological exercises. Case 24–2001. A 46year-old<br />
woman with chronic sinusitis, pulmonary nodules,<br />
and hemoptysis. N Engl J Med 2001; 345:443–449<br />
68 Hanson G, Flor N, Wells I, et al. Bronchocentric granulomatosis:<br />
a complication of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
J Allergy Clin Immunol 1977; 59:83–90<br />
69 Kradin RL, Mark EJ. The pathology of pulmonary disorders<br />
due to Aspergillus spp. Arch Pathol Lab Med 2008; 132:<br />
606–614<br />
70 Starke ID, Keal EE. Cerebral aspergilloma in a patient with<br />
allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Br J Dis Chest<br />
1980; 74:301–305<br />
71 Bodey GP, Glann AS. Central nervous system <strong>aspergillosis</strong><br />
following steroidal therapy for allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Chest 1993; 103:299–301<br />
72 Chung Y, Kraut JR, Stone AM, et al. Disseminated <strong>aspergillosis</strong><br />
in a patient with cystic fibrosis and allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Pediatr Pulmonol 1994; 17:131–134<br />
73 Tsimikas S, Hollingsworth HM, Nash G. Aspergillus brain<br />
abscess complicating allergic Aspergillus sinusitis. J Allergy<br />
Clin Immunol 1994; 94:264–267<br />
74 Ganassini A, Cazzadori A. Invasive pulmonary <strong>aspergillosis</strong><br />
complicating allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Respir<br />
Med 1995; 89:143–145<br />
75 Shah A, Kala J, Sahay S, et al. Frequency of familial occurrence<br />
in 164 patients with allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
Ann Allergy Asthma Immunol 2008; 101:363–369<br />
76 Agarwal R, Singh N, Gupta D. Pulmonary hypertension as a<br />
presenting manifestation of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
Indian J Chest Dis Allied Sci 2009; 51:37–40<br />
77 Ownby DR. Diagnostic tests in allergy. In: Lieberman P,<br />
Anderson JA, eds. <strong>Allergic</strong> diseases: diagnosis and treatment.<br />
Totowa, NJ: Humana Press, 2007; 27–38<br />
78 Malo JL, Paquin R. Incidence of immediate sensitivity to<br />
Aspergillus fumigatus in a North American asthmatic population.<br />
Clin Allergy 1979; 9:377–384<br />
79 Ricketti AJ, Greenberger PA, Patterson R. Serum IgE as an<br />
important aid in management of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. J Allergy Clin Immunol 1984; 74:68–71<br />
80 Imbeau SA, Nichols D, Flaherty D, et al. Relationships<br />
between prednisone therapy, disease activity, and the total<br />
serum IgE level in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
J Allergy Clin Immunol 1978; 62:91–95<br />
81 Leser C, Kauffman HF, Virchow C Sr, et al. Specific serum<br />
immunopatterns in clinical phases of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. J Allergy Clin Immunol 1992; 90:589–599<br />
82 Wang JL, Patterson R, Rosenberg M, et al. Serum IgE and<br />
IgG antibody activity against Aspergillus fumigatus as a<br />
diagnostic aid in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
Am Rev Respir Dis 1978; 117:917–927<br />
83 McCarthy DS, Simon G, Hargreave FE. The radiological<br />
appearances in allergic broncho-pulmonary <strong>aspergillosis</strong>.<br />
Clin Radiol 1970; 21:366–375<br />
84 Mintzer RA, Rogers LF, Kruglik GD, et al. The spectrum of<br />
radiologic findings in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
Radiology 1978; 127:301–307<br />
85 Shah A, Panchal N, Agarwal AK. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>: the spectrum of roentgenologic appearances.<br />
Indian J Radiol Imaging 1999; 9:107–112<br />
86 Shah A. <strong>Allergic</strong> <strong>bronchopulmonary</strong> and sinus aspergillo-<br />
sis: the roentgenologic spectrum. Front Biosci 2003; 8:<br />
e138–e146<br />
87 Phelan MS, Kerr IH. <strong>Allergic</strong> broncho-pulmonary <strong>aspergillosis</strong>:<br />
the radiological appearance during long-term followup.<br />
Clin Radiol 1984; 35:385–392<br />
88 Lynch DA. Imaging of asthma and allergic <strong>bronchopulmonary</strong><br />
mycosis. Radiol Clin North Am 1998; 36:129–142<br />
89 Panchal N, Bhagat R, Pant C, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>: the spectrum of computed tomography<br />
appearances. Respir Med 1997; 91:213–219<br />
90 Goyal R, White CS, Templeton PA, et al. High attenuation<br />
mucous plugs in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>:<br />
CT appearance. J Comput Assist Tomogr 1992; 16:649–650<br />
91 Logan PM, Muller NL. High-attenuation mucous plugging<br />
in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Can Assoc Radiol<br />
J 1996; 47:374–377<br />
92 Karunaratne N, Baraket M, Lim S, et al. Case quiz: thoracic<br />
CT illustrating hyperdense bronchial mucous plugging; allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Australas Radiol<br />
2003; 47:336–338<br />
93 Molinari M, Ruiu A, Biondi M, et al. Hyperdense mucoid<br />
impaction in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>: CT<br />
appearance. Monaldi Arch Chest Dis 2004; 61:62–64<br />
94 Agarwal R, Aggarwal AN, Gupta D. High-attenuation mucus<br />
in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>: another cause of<br />
diffuse high-attenuation pulmonary abnormality. AJR Am J<br />
Roentgenol 2006; 186:904<br />
95 Morozov A, Applegate KE, Brown S, et al. High-attenuation<br />
mucus plugs on MDCT in a child with cystic fibrosis:<br />
potential cause and differential diagnosis. Pediatr Radiol<br />
2007; 37:592–595<br />
96 Scadding JG. The bronchi in allergic <strong>aspergillosis</strong>. Scand J<br />
Respir Dis 1967; 48:372–377<br />
97 Neeld DA, Goodman LR, Gurney JW, et al. Computerized<br />
tomography in the evaluation of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Am Rev Respir Dis 1990; 142:1200–<br />
1205<br />
98 Angus RM, Davies ML, Cowan MD, et al. Computed<br />
tomographic scanning of the lung in patients with allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong> and in asthmatic patients<br />
with a positive skin test to Aspergillus fumigatus. Thorax<br />
1994; 49:586–589<br />
99 Ward S, Heyneman L, Lee MJ, et al. Accuracy of CT in the<br />
diagnosis of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in asthmatic<br />
patients. AJR Am J Roentgenol 1999; 173:937–942<br />
100 Agarwal R, Aggarwal AN, Gupta D, et al. A rare cause of<br />
miliary nodules: allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
BJR 2009 (in press)<br />
101 Agarwal R, Reddy C, Gupta D. An unusual cause of hilar<br />
lymphadenopathy. Lung India 2006; 23:90–92<br />
102 Shah A, Kala J, Sahay S. <strong>Allergic</strong> <strong>bronchopulmonary</strong> <strong>aspergillosis</strong><br />
with hilar adenopathy in a 42-month-old boy.<br />
Pediatr Pulmonol 2007; 42:747–748<br />
103 Murphy D, Lane DJ. Pleural effusion in allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>: two case reports. Br J Dis Chest<br />
1981; 75:91–95<br />
104 O’Connor TM, O’Donnell A, Hurley M, et al. <strong>Allergic</strong><br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong>: a rare cause of pleural<br />
effusion. Respirology 2001; 6:361–363<br />
105 Ogasawara T, Iesato K, Okabe H, et al. A case of pleural<br />
effusion associated with allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong><br />
during a relapse of the disease. Nihon Kokyuki Gakkai<br />
Zasshi 2003; 41:905–910<br />
106 Cote CG, Cicchelli R, Hassoun PM. Hemoptysis and a lung<br />
mass in a 51-year-old patient with asthma. Chest 1998;<br />
114:1465–1468<br />
107 Ko WK, Choi SW, Park JM, et al. A case of allergic<br />
822 Global Medicine<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
onchopulmonary <strong>aspergillosis</strong> shown as bilateral pulmonary<br />
masses. Tuberc Respir Dis 1999; 46:260–265<br />
108 Otero Gonzalez I, Montero Martinez C, Blanco Aparicio M,<br />
et al. Pseudotumoral allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
Arch Bronconeumol 2000; 36:351–353<br />
109 Sanchez-Alarcos JM, Martinez-Cruz R, Ortega L, et al.<br />
ABPA mimicking bronchogenic cancer. Allergy 2001; 56:<br />
80–81<br />
110 Coop C, England RW, Quinn JM. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> masquerading as invasive pulmonary <strong>aspergillosis</strong>.<br />
Allergy Asthma Proc 2004; 25:263–266<br />
111 Agarwal R, Srinivas R, Aggarwal AN, et al. Pulmonary<br />
masses in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>: mechanistic<br />
explanations. Respir Care 2008; 53:1744–1748<br />
112 Longbottom JL, Pepys J. Pulmonary <strong>aspergillosis</strong>: diagnostic<br />
and immunological significance of antigens and<br />
C-substance in Aspergillus fumigatus. J Pathol Bacteriol<br />
1964; 88:141–151<br />
113 Vlahakis NE, Aksamit TR. Diagnosis and treatment of<br />
allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Mayo Clin Proc<br />
2001; 76:930–938<br />
114 Greenberger PA. <strong>Allergic</strong> <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
J Allergy Clin Immunol 1984; 74:645–653<br />
115 Malo JL, Hawkins R, Pepys J. Studies in chronic allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong>: 1. Clinical and physiological<br />
findings. Thorax 1977; 32:254–261<br />
116 McCarthy DS, Pepys J. <strong>Allergic</strong> broncho-pulmonary <strong>aspergillosis</strong>.<br />
Clinical immunology: 1. Clinical features. Clin<br />
Allergy 1971; 1:261–286<br />
117 Nichols D, Dopico GA, Braun S, et al. Acute and chronic<br />
pulmonary function changes in allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Am J Med 1979; 67:631–637<br />
118 Kurup VP. Aspergillus antigens: which are important? Med<br />
Mycol 2005; 43(suppl):S189–S196<br />
119 Kurup VP, Banerjee B, Hemmann S, et al. Selected recombinant<br />
Aspergillus fumigatus allergens bind specifically to<br />
IgE in ABPA. Clin Exp Allergy 2000; 30:988–993<br />
120 Crameri R, Hemmann S, Ismail C, et al. Disease-specific<br />
recombinant allergens for the diagnosis of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Int Immunol 1998; 10:1211–1216<br />
121 Crameri R. Recombinant Aspergillus fumigatus allergens:<br />
from the nucleotide sequences to clinical applications. Int<br />
Arch Allergy Immunol 1998; 115:99–114<br />
122 Crameri R, Lidholm J, Gronlund H, et al. Automated specific<br />
IgE assay with recombinant allergens: evaluation of the recombinant<br />
Aspergillus fumigatus allergen I in the Pharmacia Cap<br />
System. Clin Exp Allergy 1996; 26:1411–1419<br />
123 Nikolaizik WH, Moser M, Crameri R, et al. Identification of<br />
allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in cystic fibrosis<br />
patients by recombinant Aspergillus fumigatus I/a-specific<br />
serology. Am J Respir Crit Care Med 1995; 152:634–639<br />
124 Hemmann S, Nikolaizik WH, Schoni MH, et al. Differential<br />
IgE recognition of recombinant Aspergillus fumigatus allergens<br />
by cystic fibrosis patients with allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> or Aspergillus allergy. Eur J Immunol<br />
1998; 28:1155–1160<br />
125 Nikolaizik WH, Weichel M, Blaser K, et al. Intracutaneous<br />
tests with recombinant allergens in cystic fibrosis patients<br />
with allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> and Aspergillus<br />
allergy. Am J Respir Crit Care Med 2002; 165:916–921<br />
126 Campbell MJ, Clayton YM. Bronchopulmonary <strong>aspergillosis</strong>.<br />
A correlation of the clinical and laboratory findings in<br />
272 patients investigated for <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
Am Rev Respir Dis 1964; 89:186–196<br />
127 McCarthy DS, Pepys J. <strong>Allergic</strong> broncho-pulmonary <strong>aspergillosis</strong>:<br />
clinical immunology; 2. Skin, nasal and bronchial<br />
tests. Clin Allergy 1971; 1:415–432<br />
128 Wang JL, Patterson R, Roberts M, et al. The management of<br />
allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Am Rev Respir Dis<br />
1979; 120:87–92<br />
129 Denning DW, O’Driscoll BR, Hogaboam CM, et al. The<br />
link between fungi and severe asthma: a summary of the<br />
evidence. Eur Respir J 2006; 27:615–626<br />
130 Wark PA, Hensley MJ, Saltos N, et al. Anti-inflammatory<br />
effect of itraconazole in stable allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>: a randomized controlled trial. J Allergy Clin<br />
Immunol 2003; 111:952–957<br />
131 Agarwal R, Chakrabarti A. Clinical features and natural<br />
history of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. In: Pasqualotto<br />
A, ed. Aspergillosis: from diagnosis to prevention.<br />
New York, NY: Springer, 2009 (in press)<br />
132 Greenberger PA, Patterson R. Application of enzyme-linked<br />
immunosorbent assay (ELISA) in diagnosis of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. J Lab Clin Med 1982; 99:288–293<br />
133 Rosenberg M, Patterson R, Roberts M, et al. The assessment<br />
of immunologic and clinical changes occurring during<br />
corticosteroid therapy for allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
Am J Med 1978; 64:599–606<br />
134 Ricketti AJ, Greenberger PA, Patterson R. Varying presentations<br />
of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Int Arch<br />
Allergy Appl Immunol 1984; 73:283–285<br />
135 Halwig JM, Greenberger PA, Levine M, et al. Recurrence of<br />
allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> after seven years of<br />
remission. J Allergy Clin Immunol 1984; 74:738–740<br />
136 Lee TM, Greenberger PA, Patterson R, et al. Stage V<br />
(fibrotic) allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>: a review<br />
of 17 cases followed from diagnosis. Arch Intern Med 1987;<br />
147:319–323<br />
137 Patterson R. <strong>Allergic</strong> <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> and<br />
hypersensitivity reactions to fungi. In: Fishman AP, Elias JA,<br />
Fishman JA, et al, eds. Fishman’s pulmonary diseases and<br />
disorders. New York, NY: McGraw-Hill, 1998; 777–782<br />
138 Baur X, Weiss W, Jarosch B, et al. Immunoprint pattern in<br />
patients with allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in<br />
different stages. J Allergy Clin Immunol 1989; 83:839–844<br />
139 Kumar R, Chopra D. Evaluation of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> in patients with and without central bronchiectasis.<br />
J Asthma 2002; 39:473–477<br />
140 Kumar R. Mild, moderate, and severe forms of allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong>: a clinical and serologic<br />
evaluation. Chest 2003; 124:890–892<br />
141 Denning DW, Van Wye JE, Lewiston NJ, et al. Adjunctive<br />
therapy of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> with<br />
itraconazole. Chest 1991; 100:813–819<br />
142 Heinig JH, Weeke ER, Groth S, et al. High-dose local<br />
steroid treatment in <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>: a pilot<br />
study. Allergy 1988; 43:24–31<br />
143 Balter MS, Rebuck AS. Treatment of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> with inhaled corticosteroids. Respir<br />
Med 1992; 86:441–442<br />
144 Imbeault B, Cormier Y. Usefulness of inhaled high-dose<br />
corticosteroids in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
Chest 1993; 103:1614–1617<br />
145 Seaton A, Seaton RA, Wightman AJ. Management of allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong> without maintenance oral<br />
corticosteroids: a fifteen-year follow-up. QJM 1994; 87:529–<br />
537<br />
146 Inhaled beclomethasone dipropionate in allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>: report to the Research Committee<br />
of the British Thoracic Association. Br J Dis Chest 1979;<br />
73:349–356<br />
147 Shale DJ, Faux JA, Lane DJ. Trial of ketoconazole in<br />
non-invasive pulmonary <strong>aspergillosis</strong>. Thorax 1987;<br />
42:26–31<br />
www.chestjournal.org <strong>CHEST</strong> / 135 /3/MARCH, 2009 823<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
148 De Beule K, De Doncker P, Cauwenbergh G, et al. The<br />
treatment of <strong>aspergillosis</strong> and aspergilloma with itraconazole,<br />
clinical results of an open international study (1982–<br />
1987). Mycoses 1988; 31:476–485<br />
149 Mannes GP, van der Heide S, van Aalderen WM, et al.<br />
Itraconazole and allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in<br />
twin brothers with cystic fibrosis. Lancet 1993; 341:492<br />
150 Pacheco A, Martin JA, Cuevas M. Serologic response to<br />
itraconazole in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
Chest 1993; 103:980–981<br />
151 Germaud P, Tuchais E. <strong>Allergic</strong> <strong>bronchopulmonary</strong> <strong>aspergillosis</strong><br />
treated with itraconazole. Chest 1995; 107:883<br />
152 Nikaido Y, Nagata N, Yamamoto T, et al. A case of allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong> successfully treated with<br />
itraconazole. Respir Med 1998; 92:118–119<br />
153 Nepomuceno IB, Esrig S, Moss RB. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> in cystic fibrosis: role of atopy and<br />
response to itraconazole. Chest 1999; 115:364–370<br />
154 Salez F, Brichet A, Desurmont S, et al. Effects of itraconazole<br />
therapy in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
Chest 1999; 116:1665–1668<br />
155 Suzuki M, Sugiyama Y, Kitamura S. A case of allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong> refractory to the corticosteroid<br />
therapy and successfully treated by itraconazole. Japanese<br />
J Chest Dis 1999; 58:770–775<br />
156 Stevens DA, Schwartz HJ, Lee JY, et al. A randomized trial<br />
of itraconazole in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
N Engl J Med 2000; 342:756–762<br />
157 Skov M, Hoiby N, Koch C. Itraconazole treatment of<br />
allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in patients with<br />
cystic fibrosis. Allergy 2002; 57:723–728<br />
158 Kumar R, Singh P, Arora R, et al. Effect of itraconazole<br />
therapy in allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Saudi<br />
Med J 2003; 24:546–547<br />
159 Morimoto T, Ohnishi H, Fujiyama R, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> successfully treated with itraconazole<br />
and fluticasone. Japanese J Chest Dis 2003; 62:55–60<br />
160 Ferrari M, Bodini I, Lo Cascio V. Rhabdomyolysis after the<br />
administration of itraconazole to an asthmatic patient with<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Respiration 2004; 71:289–291<br />
161 Wark PA, Gibson PG, Wilson AJ. Azoles for allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> associated with asthma. Cochrane<br />
Database Syst Rev (database online). Issue 3, 2004<br />
162 Tucker RM, Haq Y, Denning DW, et al. Adverse events<br />
associated with itraconazole in 189 patients on chronic<br />
therapy. J Antimicrob Chemother 1990; 26:561–566<br />
163 Lebrun-Vignes B, Archer VC, Diquet B, et al. Effect of<br />
itraconazole on the pharmacokinetics of prednisolone and<br />
methylprednisolone and cortisol secretion in healthy subjects.<br />
Br J Clin Pharmacol 2001; 51:443–450<br />
164 Main KM, Skov M, Sillesen IB, et al. Cushing’s syndrome<br />
due to pharmacological interaction in a cystic fibrosis patient.<br />
Acta Paediatr 2002; 91:1008–1011<br />
165 Skov M, Main KM, Sillesen IB, et al. Iatrogenic adrenal<br />
insufficiency as a side-effect of combined treatment of<br />
itraconazole and budesonide. Eur Respir J 2002; 20:127–133<br />
166 Laoudi Y, Paolini JB, Grimfed A, et al. Nebulised corticosteroid<br />
and amphotericin B: an alternative treatment for<br />
ABPA? Eur Respir J 2008; 31:908–909<br />
167 van der Ent CK, Hoekstra H, Rijkers GT. Successful<br />
treatment of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> with<br />
recombinant anti-IgE antibody. Thorax 2007; 62:276–277<br />
168 Thomson JM, Wesley A, Byrnes CA, et al. Pulse intravenous<br />
methylprednisolone for resistant allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> in cystic fibrosis. Pediatr Pulmonol 2006; 41:<br />
164–170<br />
169 Mulliez P, Croxo C, Roy-Saint Georges F, et al. <strong>Allergic</strong><br />
broncho-pulmonary <strong>aspergillosis</strong> treated with voriconazole.<br />
Rev Mal Respir 2006; 23:93–94<br />
170 Bandres Gimeno R, Munoz Martinez MJ. Prolonged therapeutic<br />
response to voriconazole in a case of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Arch Bronconeumol 2007; 43:<br />
49–51<br />
171 Erwin GE, Fitzgerald JE. Case report: allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> and allergic fungal sinusitis successfully<br />
treated with voriconazole. J Asthma 2007; 44:891–895<br />
172 Mearns M, Young W, Batten J. Transient pulmonary infiltrations<br />
in cystic fibrosis due to allergic <strong>aspergillosis</strong>. Thorax<br />
1965; 20:385–392<br />
173 Kraemer R, Delosea N, Ballinari P, et al. Effect of allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong> on lung function in children<br />
with cystic fibrosis. Am J Respir Crit Care Med 2006;<br />
174:1211–1220<br />
174 Mastella G, Rainisio M, Harms HK, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> in cystic fibrosis: a European epidemiological<br />
study; Epidemiologic Registry of Cystic Fibrosis.<br />
Eur Respir J 2000; 16:464–471<br />
175 de Almeida MB, Bussamra MH, Rodrigues JC. <strong>Allergic</strong><br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in paediatric cystic fibrosis<br />
patients. Paediatr Respir Rev 2006; 7:67–72<br />
176 Knutsen AP, Hutcheson PS, Mueller KR, et al. Serum<br />
immunoglobulins E and G anti-Aspergillus fumigatus antibody<br />
in patients with cystic fibrosis who have allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. J Lab Clin Med 1990;<br />
116:724–727<br />
177 Laufer P, Fink JN, Bruns WT, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> in cystic fibrosis. J Allergy Clin Immunol<br />
1984; 73:44–48<br />
178 Mroueh S, Spock A. <strong>Allergic</strong> <strong>bronchopulmonary</strong> <strong>aspergillosis</strong><br />
in patients with cystic fibrosis. Chest 1994; 105:32–36<br />
179 Nicolai T, Arleth S, Spaeth A, et al. Correlation of IgE<br />
antibody titer to Aspergillus fumigatus with decreased lung<br />
function in cystic fibrosis. Pediatr Pulmonol 1990; 8:12–15<br />
180 Ritz N, Ammann RA, Casaulta Aebischer C, et al. Risk<br />
factors for allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> and sensitization<br />
to Aspergillus fumigatus in patients with cystic<br />
fibrosis. Eur J Pediatr 2005; 164:577–582<br />
181 Becker JW, Burke W, McDonald G, et al. Prevalence of<br />
allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> and atopy in adult<br />
patients with cystic fibrosis. Chest 1996; 109:1536–1540<br />
182 Geller DE, Kaplowitz H, Light MJ, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> in cystic fibrosis: reported prevalence,<br />
regional distribution, and patient characteristics; Scientific<br />
Advisory Group, Investigators, and Coordinators of<br />
the Epidemiologic Study of Cystic Fibrosis. Chest 1999;<br />
116:639–646<br />
183 Skov M, McKay K, Koch C, et al. Prevalence of allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in cystic fibrosis in an area<br />
with a high frequency of atopy. Respir Med 2005; 99:887–<br />
893<br />
184 Mearns M, Longbottom J, Batten J. Precipitating antibodies<br />
to Aspergillus fumigatus in cystic fibrosis. Lancet 1967;<br />
1:538–539<br />
185 Allan JD, Moss AD, Wallwork JC, et al. Immediate hypersensitivity<br />
in patients with cystic fibrosis. Clin Allergy 1975;<br />
5:255–261<br />
186 Silverman M, Hobbs FD, Gordon IR, et al. Cystic fibrosis,<br />
atopy, and airways lability. Arch Dis Child 1978; 53:873–877<br />
187 Nelson LA, Callerame ML, Schwartz RH. Aspergillosis and<br />
atopy in cystic fibrosis. Am Rev Respir Dis 1979; 120:863–873<br />
188 Feanny S, Forsyth S, Corey M, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> in cystic fibrosis: a secretory immune response<br />
to a colonizing organism. Ann Allergy 1988; 60:64–68<br />
189 Schonheyder H, Jensen T, Hoiby N, et al. Clinical and<br />
824 Global Medicine<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
serological survey of pulmonary <strong>aspergillosis</strong> in patients with<br />
cystic fibrosis. Int Arch Allergy Appl Immunol 1988; 85:472–<br />
477<br />
190 Zeaske R, Bruns WT, Fink JN, et al. Immune responses to<br />
Aspergillus in cystic fibrosis. J Allergy Clin Immunol 1988;<br />
82:73–77<br />
191 Simmonds EJ, Littlewood JM, Evans EG. Cystic fibrosis and<br />
allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>. Arch Dis Child<br />
1990; 65:507–511<br />
192 Hutcheson PS, Rejent AJ, Slavin RG. Variability in parameters<br />
of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in patients with<br />
cystic fibrosis. J Allergy Clin Immunol 1991; 88:390–394<br />
193 el-Dahr JM, Fink R, Selden R, et al. Development of<br />
immune responses to Aspergillus at an early age in children<br />
with cystic fibrosis. Am J Respir Crit Care Med 1994;<br />
150:1513–1518<br />
194 Marchant JL, Warner JO, Bush A. Rise in total IgE as an<br />
indicator of allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in cystic<br />
fibrosis. Thorax 1994; 49:1002–1005<br />
195 Hutcheson PS, Knutsen AP, Rejent AJ, et al. A 12-year<br />
longitudinal study of Aspergillus sensitivity in patients with<br />
cystic fibrosis. Chest 1996; 110:363–366<br />
196 Cimon B, Carrere J, Chazalette JP, et al. Bronchopulmonary<br />
mycoses in cystic fibrosis: results of a five-year longitudinal<br />
study. J Mycol Med 2000; 10:128–135<br />
197 Taccetti G, Procopio E, Marianelli L, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> in Italian cystic fibrosis patients:<br />
prevalence and percentage of positive tests in the employed<br />
diagnostic criteria. Eur J Epidemiol 2000; 16:837–842<br />
198 Almeida MB, Bussamra MH, Rodrigues JC. ABPA diagnosis<br />
in cystic fibrosis patients: the clinical utility of IgE specific to<br />
recombinant Aspergillus fumigatus allergens. J Pediatr (Rio J)<br />
2006; 82:215–220<br />
199 Chotirmall SH, Branagan P, Gunaratnam C, et al. Aspergillus/allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in an Irish cystic<br />
fibrosis population: a diagnostically challenging entity. Respir<br />
Care 2008; 53:1035–1041<br />
200 Rapaka RR, Kolls JK. Pathogenesis of allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> in cystic fibrosis: current understanding<br />
and future directions. Med Mycol 2008; 1–7<br />
201 Cunningham S, Madge SL, Dinwiddie R. Survey of criteria<br />
used to diagnose allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in<br />
cystic fibrosis. Arch Dis Child 2001; 84:89<br />
202 Stevens DA, Moss RB, Kurup VP, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> in cystic fibrosis: state of the art;<br />
Cystic Fibrosis Foundation Consensus Conference. Clin<br />
Infect Dis 2003; 37(suppl):S225–S264<br />
203 Glancy JJ, Elder JL, McAleer R. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
fungal disease without clinical asthma. Thorax 1981; 36:345–<br />
349<br />
204 Yoshida N, Suguro H, Kohara F, et al. A case of allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong> with no history of bronchial<br />
asthma. Nihon Kyobu Shikkan Gakkai Zasshi 1992; 30:2123–<br />
2127<br />
205 Hoshino H, Tagaki S, Kon H, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> due to Aspergillus niger without bronchial<br />
asthma. Respiration 1999; 66:369–372<br />
206 Shah A, Maurya V, Panjabi C, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> without clinical asthma caused by Aspergillus<br />
niger. Allergy 2004; 59:236–237<br />
207 Berkin KE, Vernon DR, Kerr JW. Lung collapse caused by<br />
allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong> in non-asthmatic<br />
patients. BMJ (Clin Res Ed) 1982; 285:552–553<br />
208 Bondue B, Remmelink M, Gevenois PA, et al. A pulmonary<br />
cavitated mass complicating long-standing allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Respir Med Extra 2005; 1:39–42<br />
209 Bahous J, Malo JL, Paquin R, et al. <strong>Allergic</strong> bronchopulmo-<br />
nary <strong>aspergillosis</strong> and sensitization to Aspergillus fumigatus<br />
in chronic bronchiectasis in adults. Clin Allergy 1985;<br />
15:571–579<br />
210 Agarwal R, Singh N, Aggarwal AN. An unusual association<br />
between Mycobacterium tuberculosis and Aspergillus fumigatus.<br />
Monaldi Arch Chest Dis 2008; 69:32–34<br />
211 Sharma B, Sharma M, Bondi E. Kartagener’s syndrome<br />
associated with allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong>.<br />
MedGenMed 2005; 7:25<br />
212 Agarwal R, Srinivas R, Jindal SK. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> complicating chronic obstructive pulmonary<br />
disease. Mycoses 2008; 51:83–85<br />
213 Eppinger TM, Greenberger PA, White DA, et al. Sensitization<br />
to Aspergillus species in the congenital neutrophil<br />
disorders chronic granulomatous disease and hyper-IgE<br />
syndrome. J Allergy Clin Immunol 1999; 104:1265–1272<br />
214 Safirstein BH. Aspergilloma consequent to allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Am Rev Respir Dis 1973; 108:940–943<br />
215 Ein ME, Wallace RJ Jr, Williams TW Jr. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>-like syndrome consequent to aspergilloma.<br />
Am Rev Respir Dis 1979; 119:811–820<br />
216 Israel RH, Poe RH, Bomba PA, et al. The rapid development<br />
of an aspergilloma secondary to allergic <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong>. Am J Med Sci 1980; 280:41–44<br />
217 Rosenberg IL, Greenberger PA. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> and aspergilloma: long-term follow-up without<br />
enlargement of a large multiloculated cavity. Chest 1984;<br />
85:123–125<br />
218 Sharma TN, Gupta PR, Mehrotra AK, et al. Aspergilloma<br />
with ABPA due to Aspergillus niger. J Assoc Physicians India<br />
1985; 33:748<br />
219 Shah A, Khan ZU, Chaturvedi S, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> with coexistent aspergilloma: a longterm<br />
followup. J Asthma 1989; 26:109–115<br />
220 Bhagat R, Shah A, Jaggi OP, et al. Concomitant allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong> and allergic Aspergillus sinusitis<br />
with an operated aspergilloma. J Allergy Clin Immunol<br />
1993; 91:1094–1096<br />
221 Shah A, Bhagat R, Pant K, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
<strong>aspergillosis</strong> with aspergilloma: exacerbation after prolonged<br />
remission. Indian J Tuberc 1993; 40:39–41<br />
222 Jaques D, Bonzon M, Polla BS. Serological evidence of<br />
Aspergillus type I hypersensitivity in a subgroup of pulmonary<br />
aspergilloma patients. Int Arch Allergy Immunol 1995;<br />
106:263–270<br />
223 Sharma P, Agarwal AK, Shah A. Formation of an aspergilloma<br />
in a patient with allergic <strong>bronchopulmonary</strong> <strong>aspergillosis</strong><br />
on corticosteroid therapy. Indian J Chest Dis Allied Sci<br />
1998; 40:269–273<br />
224 Shah A, Panjabi C. Contemporaneous occurrence of allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong>, allergic Aspergillus sinusitis,<br />
and aspergilloma. Ann Allergy Asthma Immunol 2006;<br />
96:874–878<br />
225 Denning DW, Riniotis K, Dobrashian R, et al. Chronic<br />
cavitary and fibrosing pulmonary and pleural <strong>aspergillosis</strong>:<br />
case series, proposed nomenclature change, and review.<br />
Clin Infect Dis 2003; 37(suppl):S265–S280<br />
226 Dolan CT, Weed LA, Dines DE. Bronchopulmonary helminthosporiosis.<br />
Am J Clin Pathol 1970; 53:235–242<br />
227 Sahn SA, Lakshminarayan S. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
penicilliosis. Chest 1973; 63:286–288<br />
228 Novey HS, Wells ID. <strong>Allergic</strong> <strong>bronchopulmonary</strong> <strong>aspergillosis</strong><br />
caused by Aspergillus ochraceus. Am J Clin Pathol<br />
1978; 70:840–843<br />
229 Benatar SR, Allan B, Hewitson RP, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
stemphyliosis. Thorax 1980; 35:515–518<br />
230 Laham MN, Allen RC, Greene JC. <strong>Allergic</strong> bronchopulmo-<br />
www.chestjournal.org <strong>CHEST</strong> / 135 /3/MARCH, 2009 825<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013
nary <strong>aspergillosis</strong> (ABPA) caused by Aspergillus terreus:<br />
specific lymphocyte sensitization and antigen-directed serum<br />
opsonic activity. Ann Allergy 1981; 46:74–80<br />
231 McAleer R, Kroenert DB, Elder JL, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
disease caused by Curvularia lunata and Drechslera<br />
hawaiiensis. Thorax 1981; 36:338–344<br />
232 Patterson R, Samuels BS, Phair JJ, et al. Bronchopulmonary<br />
torulopsosis. Int Arch Allergy Appl Immunol 1982; 69:30–33<br />
233 Kino T, Yamada Y, Honda K, et al. Diagnosis and treatment<br />
of a case of allergic <strong>bronchopulmonary</strong> mycosis caused by<br />
Mucor-like fungus. Nihon Kyobu Shikkan Gakkai Zasshi<br />
1983; 21:896–903<br />
234 Akiyama K, Mathison DA, Riker JB, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
candidiasis. Chest 1984; 85:699–701<br />
235 Lake FR, Tribe AE, McAleer R, et al. Mixed allergic<br />
<strong>bronchopulmonary</strong> fungal disease due to Pseudallescheria<br />
boydii and Aspergillus. Thorax 1990; 45:489–491<br />
236 Lake FR, Froudist JH, McAleer R, et al. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
fungal disease caused by Bipolaris and Curvularia.<br />
Aust NZJMed1991; 21:871–874<br />
237 Kamei K, Unno H, Nagao K, et al. <strong>Allergic</strong> bronchopulmo-<br />
nary mycosis caused by the basidiomycetous fungus Schizophyllum<br />
commune. Clin Infect Dis 1994; 18:305–309<br />
238 Backman KS, Roberts M, Patterson R. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
mycosis caused by Fusarium vasinfectum. Am J<br />
Respir Crit Care Med 1995; 152:1379–1381<br />
239 Moreno-Ancillo A, Diaz-Pena JM, Ferrer A, et al. <strong>Allergic</strong><br />
<strong>bronchopulmonary</strong> cladosporiosis in a child. J Allergy Clin<br />
Immunol 1996; 97:714–715<br />
240 Ogawa H, Fujimura M, Tofuku Y. <strong>Allergic</strong> <strong>bronchopulmonary</strong><br />
fungal disease caused by Saccharomyces cerevisiae. J<br />
Asthma 2004; 41:223–228<br />
241 Shah A, Panchal N, Agarwal AK. Concomitant allergic<br />
<strong>bronchopulmonary</strong> <strong>aspergillosis</strong> and allergic Aspergillus sinusitis:<br />
a review of an uncommon association. Clin Exp<br />
Allergy 2001; 31:1896–1905<br />
242 Saravanan K, Panda NK, Chakrabarti A, et al. <strong>Allergic</strong><br />
fungal rhinosinusitis: an attempt to resolve the diagnostic<br />
dilemma. Arch Otolaryngol Head Neck Surg 2006; 132:<br />
173–178<br />
243 Shah TS, Sundaram P, Rege JD, et al. Proptosis in an<br />
asthmatic patient. Postgrad Med J 2003; 79:710<br />
826 Global Medicine<br />
Downloaded From: http://jupcvss.chestpubs.org/ on 08/01/2013