Kidney Transplant Ureteroneocystostomy Techniques and ...
Kidney Transplant Ureteroneocystostomy Techniques and ...
Kidney Transplant Ureteroneocystostomy Techniques and ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
KIDNEY TRANSPLANT LITERATURE REVIEW 1415<br />
wall so that the ureteral end is ancored to the inner bladder<br />
wall (Figure 3). The tunneling procedure is performed in a<br />
similar manner to LG by imbricating the seromuscular layer<br />
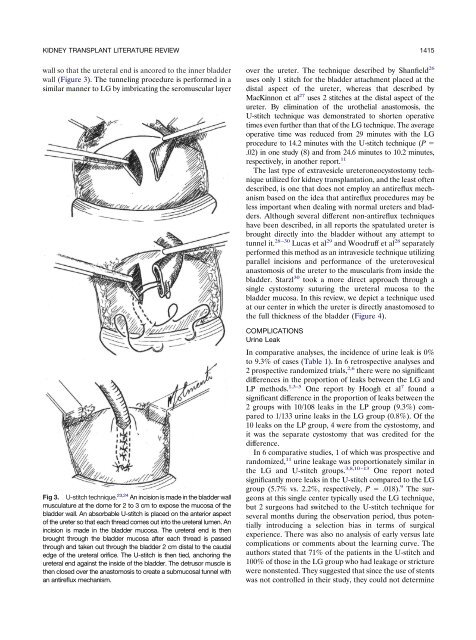
Fig 3. U-stitch technique. 23,24 An incision is made in the bladder wall<br />
musculature at the dome for 2 to 3 cm to expose the mucosa of the<br />
bladder wall. An absorbable U-stitch is placed on the anterior aspect<br />
of the ureter so that each thread comes out into the ureteral lumen. An<br />
incision is made in the bladder mucosa. The ureteral end is then<br />
brought through the bladder mucosa after each thread is passed<br />
through <strong>and</strong> taken out through the bladder 2 cm distal to the caudal<br />
edge of the ureteral orifice. The U-stitch is then tied, anchoring the<br />
ureteral end against the inside of the bladder. The detrusor muscle is<br />
then closed over the anastomosis to create a submucosal tunnel with<br />
an antireflux mechanism.<br />
over the ureter. The technique described by Shanfield 26<br />
uses only 1 stitch for the bladder attachment placed at the<br />
distal aspect of the ureter, whereas that described by<br />
MacKinnon et al 27 uses 2 stitches at the distal aspect of the<br />
ureter. By elimination of the urothelial anastomosis, the<br />
U-stitch technique was demonstrated to shorten operative<br />
times even further than that of the LG technique. The average<br />
operative time was reduced from 29 minutes with the LG<br />
procedure to 14.2 minutes with the U-stitch technique (P <br />
.02) in one study (8) <strong>and</strong> from 24.6 minutes to 10.2 minutes,<br />
respectively, in another report. 11<br />
The last type of extravesicle ureteroneocystostomy technique<br />
utilized for kidney transplantation, <strong>and</strong> the least often<br />
described, is one that does not employ an antireflux mechanism<br />
based on the idea that antireflux procedures may be<br />
less important when dealing with normal ureters <strong>and</strong> bladders.<br />
Although several different non-antireflux techniques<br />
have been described, in all reports the spatulated ureter is<br />
brought directly into the bladder without any attempt to<br />
tunnel it. 28–30 Lucas et al 29 <strong>and</strong> Woodruff et al 28 separately<br />
performed this method as an intravesicle technique utilizing<br />
parallel incisions <strong>and</strong> performance of the ureterovesical<br />
anastomosis of the ureter to the muscularis from inside the<br />
bladder. Starzl 30 took a more direct approach through a<br />
single cystostomy suturing the ureteral mucosa to the<br />
bladder mucosa. In this review, we depict a technique used<br />
at our center in which the ureter is directly anastomosed to<br />
the full thickness of the bladder (Figure 4).<br />
COMPLICATIONS<br />
Urine Leak<br />
In comparative analyses, the incidence of urine leak is 0%<br />
to 9.3% of cases (Table 1). In 6 retrospective analyses <strong>and</strong><br />
2 prospective r<strong>and</strong>omized trials, 2,6 there were no significant<br />
differences in the proportion of leaks between the LG <strong>and</strong><br />
LP methods. 1,3–5 One report by Hoogh et al 7 found a<br />
significant difference in the proportion of leaks between the<br />
2 groups with 10/108 leaks in the LP group (9.3%) compared<br />
to 1/133 urine leaks in the LG group (0.8%). Of the<br />
10 leaks on the LP group, 4 were from the cystostomy, <strong>and</strong><br />
it was the separate cystostomy that was credited for the<br />
difference.<br />
In 6 comparative studies, 1 of which was prospective <strong>and</strong><br />
r<strong>and</strong>omized, 11 urine leakage was proportionately similar in<br />
the LG <strong>and</strong> U-stitch groups. 3,8,10–13 One report noted<br />
significantly more leaks in the U-stitch compared to the LG<br />
group (5.7% vs. 2.2%, respectively, P .018). 9 The surgeons<br />
at this single center typically used the LG technique,<br />
but 2 surgeons had switched to the U-stitch technique for<br />
several months during the observation period, thus potentially<br />
introducing a selection bias in terms of surgical<br />
experience. There was also no analysis of early versus late<br />
complications or comments about the learning curve. The<br />
authors stated that 71% of the patients in the U-stitch <strong>and</strong><br />
100% of those in the LG group who had leakage or stricture<br />
were nonstented. They suggested that since the use of stents<br />
was not controlled in their study, they could not determine