Program of Excellence.pdf - Yale School of Medicine
Program of Excellence.pdf - Yale School of Medicine
Program of Excellence.pdf - Yale School of Medicine
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Program</strong> <strong>of</strong> <strong>Excellence</strong><br />
SBRT team is hard at work saving more lives<br />
[This article appeared online in the June 2012<br />
Dialogue.]<br />
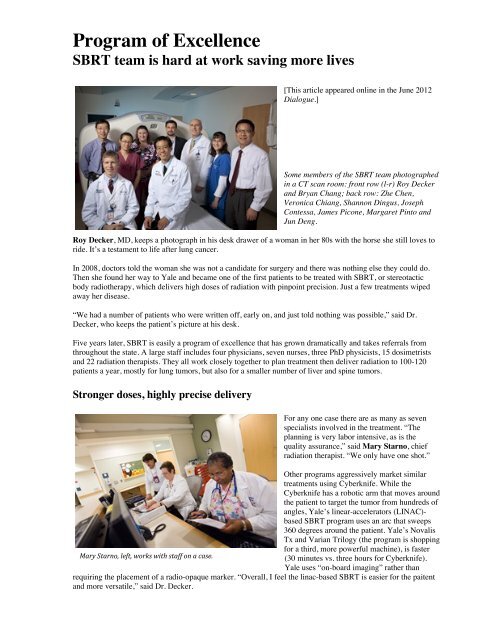
Some members <strong>of</strong> the SBRT team photographed<br />
in a CT scan room: front row (l-r) Roy Decker<br />
and Bryan Chang; back row: Zhe Chen,<br />
Veronica Chiang, Shannon Dingus, Joseph<br />
Contessa, James Picone, Margaret Pinto and<br />
Jun Deng.<br />
Roy Decker, MD, keeps a photograph in his desk drawer <strong>of</strong> a woman in her 80s with the horse she still loves to<br />
ride. It’s a testament to life after lung cancer.<br />
In 2008, doctors told the woman she was not a candidate for surgery and there was nothing else they could do.<br />
Then she found her way to <strong>Yale</strong> and became one <strong>of</strong> the first patients to be treated with SBRT, or stereotactic<br />
body radiotherapy, which delivers high doses <strong>of</strong> radiation with pinpoint precision. Just a few treatments wiped<br />
away her disease.<br />
“We had a number <strong>of</strong> patients who were written <strong>of</strong>f, early on, and just told nothing was possible,” said Dr.<br />
Decker, who keeps the patient’s picture at his desk.<br />
Five years later, SBRT is easily a program <strong>of</strong> excellence that has grown dramatically and takes referrals from<br />
throughout the state. A large staff includes four physicians, seven nurses, three PhD physicists, 15 dosimetrists<br />
and 22 radiation therapists. They all work closely together to plan treatment then deliver radiation to 100-120<br />
patients a year, mostly for lung tumors, but also for a smaller number <strong>of</strong> liver and spine tumors.<br />
Stronger doses, highly precise delivery<br />
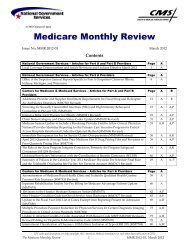
For any one case there are as many as seven<br />
specialists involved in the treatment. “The<br />
planning is very labor intensive, as is the<br />
quality assurance,” said Mary Starno, chief<br />
radiation therapist. “We only have one shot.”<br />
Other programs aggressively market similar<br />
treatments using Cyberknife. While the<br />
Cyberknife has a robotic arm that moves around<br />
the patient to target the tumor from hundreds <strong>of</strong><br />
angles, <strong>Yale</strong>’s linear-accelerators (LINAC)based<br />
SBRT program uses an arc that sweeps<br />
360 degrees around the patient. <strong>Yale</strong>’s Novalis<br />
Tx and Varian Trilogy (the program is shopping<br />
for a third, more powerful machine), is faster<br />
Mary Starno, left, works with staff on a case.<br />
(30 minutes vs. three hours for Cyberknife).<br />
<strong>Yale</strong> uses “on-board imaging” rather than<br />
requiring the placement <strong>of</strong> a radio-opaque marker. “Overall, I feel the linac-based SBRT is easier for the paitent<br />
and more versatile,” said Dr. Decker.
Pulmonary and liver patients typically receive 3-5 treatments—traditional radiation would require 30 or 40—<br />
following detailed treatment design, integrating technologies such as PET-CT scanning, 4-dimensional<br />
simulation(4-D Sim), and comfortable stabilization to minimize body motion during radiotherapy delivery.<br />
Specialists explore a variety <strong>of</strong> uses<br />
Veronica Chiang, MD<br />
!<br />
James Yu, MD !<br />
ica Chiang, MD<br />
James Yu, MD<br />
Lung cancer patients are the majority <strong>of</strong> the caseload and have the most successful<br />
outcomes, with a success rate <strong>of</strong> 80 to 90 percent. They include patients with small<br />
early stage lung cancers and carefully selected patients who have metastatic tumors.<br />
“We have a lot more experience than many other centers in treating situations that<br />
are considered high risk-tumors that are closer to the central airways,” Dr. Decker<br />
said.<br />
Veronica Chiang, MD, a neurosurgeon, and James Yu, MD, a therapeutic<br />
radiologist, together are treating the program’s fastest growing group: patients with<br />
spinal tumors. Because spine metastases are treated in a single dose up against the<br />
spinal cord, they consider targeting a spinal tumor to require even more precision<br />
than a lung tumor, and therefore have been selecting patients very conservatively.<br />
Treatment <strong>of</strong> spine metastases is currently delivered using the Novalis Tx machine.<br />
There is still lot to learn about non-palliative indications for SBRT treatment for<br />
spinal tumors, because as with all radiation treatments, the rate <strong>of</strong> local cure long<br />
term is unknown,” Dr. Chiang said. “For those who come with pain as a symptom <strong>of</strong><br />
their spine metastases, however, SBRT results in faster pain relief—and more<br />
patients get longer lasting relief—than with standard spine radiation.”<br />
Meanwhile, therapeutic radiologist Bryan Chang, MD is using the technique to treat<br />
an average <strong>of</strong> two patients a month for liver tumors, including primary liver tumors<br />
and cancer that has metastasized from other parts <strong>of</strong> the body. Since many patients<br />
travel long distances to receive the treatment, Dr. Chang carefully reviews patients’<br />
scans to determine whether they are suitable candidates before a consultation is<br />
performed. “We look at scans for all patients we see in consultation, but for patients<br />
who are referred from far away, I carefully review the scans in advance to make sure<br />
they are good candidates before accepting the consult,” he said.<br />
“Cancer that has metastasized is generally thought <strong>of</strong> as being incurable,” he said.<br />
“But we know that in certain selected cases, we can treat one or two tumors in the<br />
liver with radiation, and the patient will survive a long time or even potentially be<br />
cured. That is a fairly radical shift in thinking. In terms <strong>of</strong> treating metastatic disease,<br />
there clearly is potential for SBRT as chemotherapy continues to improve, making<br />
local control <strong>of</strong> sites like the liver more important to patient survival.”<br />
An intensive, high-tech team<br />
Another critical element is teamwork, said Starno. “The whole thing is a team effort<br />
and we couldn’t do it without each other. Everybody on the team is important.”<br />
Discussions among team members have resulted in more compassionate patient care.<br />
For example, at first they didn’t schedule appointments until the planning was<br />
completed, but waiting for a call proved to be stressful for the patient. Now new<br />
patients come in for a consultation and imaging, and leave with an appointment,<br />
typically scheduled for a week later.<br />
Bryan Chang, MD<br />
Staff that works directly with patients receive consistently high Press Ganey scores.<br />
“We’re very familiar, obviously, with trying to break the ice and make patients<br />
comfortable,” said radiation therapist Shannon Dingus. Patients also appreciate the simplicity <strong>of</strong> the treatment<br />
itself, she added. “In short periods <strong>of</strong> time, doctors and researchers have come up with things that are amazing.<br />
They’re really thinking about the patient as a person.”
Helping the program grow<br />
Dr. Decker examines a new patient.<br />
Dr. Decker, who developed the SBRT<br />
<strong>Program</strong> in 2007 after completing his radiation<br />
oncology residency at <strong>Yale</strong>-New Haven<br />
Hospital (YNHH), gives partial credit for its<br />
success to time spent upfront educating<br />
referring physicians, and speaking at CME<br />
dinners and tumor boards, among other things.<br />
He is also grateful to <strong>Yale</strong>-New Haven<br />
Hospital, which invested in the program, and<br />
Frank Detterbeck, MD, chief <strong>of</strong> thoracic<br />
surgery; Lynn Tanoue, MD, medical director<br />
<strong>of</strong> the <strong>Yale</strong> Cancer Center Thoracic Oncology<br />
<strong>Program</strong>; and Lynn Wilson, MD, clinical<br />
director <strong>of</strong> therapeutic radiology. “Without<br />
their support we were not going to go<br />
anywhere,” he said.<br />
The program’s latest stride is the pending<br />
finalization <strong>of</strong> a radiosurgery fellowship that will include training in central nervous system radiosurgery (brain<br />
and spine), lung and body SBRT. While the fellowship is an exciting milestone, Dr. Decker said it’s important to<br />
remember that the SBRT <strong>Program</strong> is still evolving.<br />
There are questions to be answered about such matters as patients’ tolerance for high doses, SBRT’s<br />
effectiveness for patients with advanced disease, and the increasing number <strong>of</strong> patients choosing SBRT as an<br />
alternative to surgery, not just as a last resort. “What is the best way to work it into these treatment plans?” Dr.<br />
Decker asked. “We don’t know. For a lot <strong>of</strong> patients, the precise role <strong>of</strong> SBRT still hasn’t been clearly defined.<br />
It’s still part <strong>of</strong> our research.”<br />
SBRT team members<br />
Radiation Oncologists:<br />
• Roy H. Decker, MD, PhD<br />
• Veronica Chiang, MD<br />
• Bryan Chang, MD<br />
• Joseph Contessa, MD PhD<br />
• Suzanne B. Evans, MD, PhD<br />
• Bruce A. McGibbon, MD<br />
• James B. Yu, MD<br />
Certified technologists:<br />
• Helen Civitello, RTT<br />
• Laura Cretella, RTT<br />
• Nancy Deforest, RTT<br />
• Shannon Dingus, RTT<br />
• Daniel Longo, RTT<br />
• Anna McKinzie, RTT<br />
• Heather Montz, RTT<br />
• Charlene Peschel, RTT<br />
• Violet Ratchford, RTT<br />
• Christa Ryszczyk, RTT<br />
• Arhonti Simmons, RTT<br />
• Iris Torres, RTT<br />
• Kathryn Waldron, RTT<br />
Radiological physicists and dosimetrists:<br />
• David Carlson, PhD<br />
• Jun Deng, PhD<br />
• Fanqing Guo, PhD<br />
• Wu Liu, PhD<br />
• Arthur Gifty, BS<br />
• Destinee Fortunato, AS<br />
• Monica Kaur, BS<br />
• John Kim, BA<br />
• James Kimmett, BS<br />
• Huan Liu, MS<br />
• James Picone, BA<br />
• Martha Picone, BS<br />
• Richard Stanton, AS<br />
• Di Wu, BS<br />
• Jing Ye, BS<br />
Clinic staff:<br />
• Margaret Pinto, RN<br />
• Laura Lucarelli, RN<br />
• Carol Kennedy, RN<br />
• Kay Oddie, RN<br />
• Nancy Andaluz, PCA<br />
Additional staff:<br />
• Ann McKeon, data manager<br />
• Jeannie Kluytenaar, RN, research nurse