Antibiotic Therapy For Todays Ocular Infections 2011 - Michigan ...
Antibiotic Therapy For Todays Ocular Infections 2011 - Michigan ...
Antibiotic Therapy For Todays Ocular Infections 2011 - Michigan ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
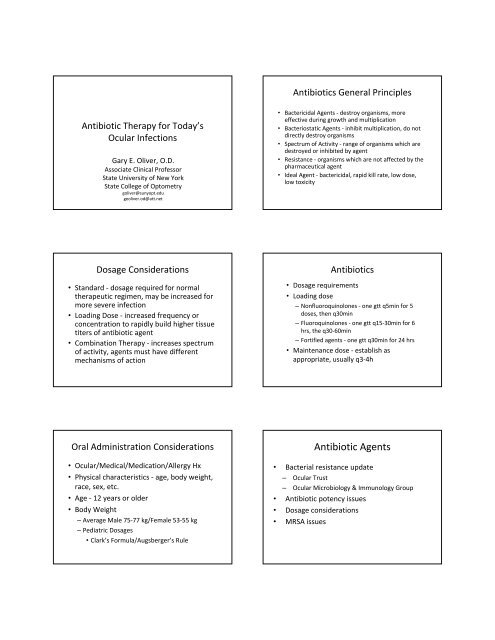
<strong>Antibiotic</strong> <strong>Therapy</strong> for Today’s<br />
<strong>Ocular</strong> <strong>Infections</strong><br />
Gary E. Oliver, O.D.<br />
Associate Clinical Professor<br />
State University of New York<br />
State College of Optometry<br />
goliver@sunyopt.edu<br />
geoliver.od@att.net<br />
Dosage Considerations<br />
• Standard ‐ dosage required for normal<br />
therapeutic regimen, may be increased for<br />
more severe infection<br />
• Loading Dose ‐ increased frequency or<br />
concentration to rapidly build higher tissue<br />
titers of antibiotic agent<br />
• Combination <strong>Therapy</strong> ‐ increases spectrum<br />
of activity, agents must have different<br />
mechanisms of action<br />
Oral Administration Considerations<br />
• <strong>Ocular</strong>/Medical/Medication/Allergy Hx<br />
• Physical characteristics ‐ age, body weight,<br />
race, sex, etc.<br />
• Age ‐ 12 years or older<br />
• Body Weight<br />
– Average Male 75‐77 kg/Female 53‐55 kg<br />
– Pediatric Dosages<br />
• Clark’s <strong>For</strong>mula/Augsberger’s Rule<br />
<strong>Antibiotic</strong>s General Principles<br />
• Bactericidal Agents ‐ destroy organisms, more<br />
effective during growth and multiplication<br />
• Bacteriostatic Agents ‐ inhibit multiplication, do not<br />
directly destroy organisms<br />
• Spectrum of Activity ‐ range of organisms which are<br />
destroyed or inhibited by agent<br />
• Resistance ‐ organisms which are not affected by the<br />
pharmaceutical agent<br />
• Ideal Agent ‐ bactericidal, rapid kill rate, low dose,<br />
low toxicity<br />
<strong>Antibiotic</strong>s<br />
• Dosage requirements<br />
• Loading dose<br />
– Nonfluoroquinolones ‐ one gtt q5min for 5<br />
doses, then q30min<br />
– Fluoroquinolones ‐ one gtt q15‐30min for 6<br />
hrs, the q30‐60min<br />
– <strong>For</strong>tified agents ‐ one gtt q30min for 24 hrs<br />
• Maintenance dose ‐ establish as<br />
appropriate, usually q3‐4h<br />
<strong>Antibiotic</strong> Agents<br />
• Bacterial resistance update<br />
– <strong>Ocular</strong> Trust<br />
– <strong>Ocular</strong> Microbiology & Immunology Group<br />
• <strong>Antibiotic</strong> potency issues<br />
• Dosage considerations<br />
• MRSA issues
Bacterial Resistance<br />
• Specific mechanisms<br />
– Development of altered receptors or enzymes that<br />
interact with the drug (production of altered penicillin<br />
binding proteins)<br />
– Decrease in concentration of drug that reaches the<br />
receptors by altered rates of entry or removal of drug<br />
(aminoglycosides may have decreased ribosomal binding<br />
due to decreased diffusion through cell wall)<br />
Methicillin Resistant Staphylococcus<br />
aureus (MRSA)<br />
• HA‐MRSA – health care associated MRSA<br />
– Older adults<br />
– Patients with weakened immune systems<br />
– Hospital, nursing home, dialysis patients<br />
• CA‐MRSA – community associated MRSA<br />
– Affects otherwise healthy patients of any age<br />
– Serious skin and soft tissue infections<br />
– Pneumonia<br />
Methicillin Resistant Staphylococcus<br />
aureus (MRSA)<br />
• CA‐MRSA<br />
– Young age<br />
– Participation in contact sports<br />
– Sharing towels or athletic equipment<br />
– Weakened immune system<br />
– Crowded or unsanitary conditions<br />
– Association with health care workers<br />
• HA‐MRSA<br />
– Current or recent hospitalization<br />
– Live in long term care facility<br />
– Use of invasive devices<br />
– Recent antibiotic use<br />
Bacterial Resistance<br />
• Enhanced destruction or inactivation of drug (B‐<br />
lactamases which catalyze the hydrolysis of<br />
penicillins)<br />
• Synthesis of resistant metabolic pathways<br />
(trimethoprim resistance in Streptococcus due to<br />
production of thymidine nucleotides by alternative<br />
pathway)<br />
• Failure to metabolize the drug (anaerobic bacteria<br />
may not metabolize drug metronidazole to active<br />
metabolites)<br />
Methicillin Resistant Staphylococcus<br />
aureus (MRSA)<br />
• Risk factors<br />
– <strong>Antibiotic</strong> resistance<br />
– Unnecessary antibiotic use<br />
– <strong>Antibiotic</strong>s in food, water<br />
– Bacterial mutation<br />
Methicillin Resistant Staphylococcus<br />
aureus (MRSA)<br />
• <strong>Ocular</strong> infection<br />
– Suspect MRSA in unresponsive bacterial infections<br />
– Consider possibility of MRSA in higher risk patients<br />
• Initial treatment options in known MRSA infections<br />
– Conjunctivitis ‐ Trimethoprim‐Polymyxin B, Besifloxacin or<br />
Tobramycin<br />
– Bacterial Keratitis – Fluoroquinolone combined with<br />
Trimethoprim‐Polymyxin B. Cosnider Besifloxacin.<br />
Vancomycin for nonresponsive infection or hospital<br />
acquired infection.
<strong>Antibiotic</strong> Agents<br />
• Topical Agents<br />
– 0.5% moxifloxacin (Vigamox, Moxeza)<br />
– 0.3%, 0.5% gatifloxacin (Zymar, Zymaxid)<br />
– 0.6% besifloxacin (Besivance)<br />
– 0.5%, 1.5% levofloxacin (Quixin, Iquix)<br />
– 0.3% ciprofloxacin (Ciloxan)<br />
– 0.3% ofloxacin (Ocuflox)<br />
Topical Fluoroquinolones<br />
– Besifloxacin (Besivance) – chlorofluoroquinolone<br />
agent, vehicle permits increased contact time<br />
– 0.5% Moxifloxacin (Moxeza) – vehicle permits<br />
increased contact time, less frequent dosing<br />
– 0.5% Gatifloxacin (Zymaxid) –higher<br />
concentration than Zymar<br />
Topical <strong>Antibiotic</strong>s<br />
• Clinical Insights<br />
– Most efficacious agents for Staph. aureus –<br />
trimethoprim, besifloxacin, tobramycin<br />
– Also are the preferred agents for MRSA<br />
– Aminoglycosides more toxic to cornea than most<br />
other agents<br />
– Least corneal toxicity –trimethoprim,<br />
moxifloxacin, bacitracin/polymyxin B and<br />
erythromycin<br />
Topical Fluoroquinolones<br />
• Clinical Insights<br />
– Concentration dependent activity<br />
– Broad spectrum efficacy<br />
– Possibly less efficacious against Staph. aureus<br />
than other Gram+ organisms<br />
– Preferred agents for corneal infection<br />
<strong>Antibiotic</strong> Agents<br />
• Topical Agents<br />
– 0.3% tobramycin (Tobrex)<br />
– 0.3% gentamicin (Genoptic)<br />
– 1% azithromycin (AzaSite)<br />
– Trimethoprim/polymyxin B (Polytrim)<br />
– Bacitracin/polymyxin B (Polysporin)<br />
– Neomycin/polysporin B/gramicidin (Neosporin)<br />
– 0.5% erythromycin (Ilotycin)<br />
– 10% sulfacetamide (Bleph‐10)<br />
Topical <strong>Antibiotic</strong>s<br />
• Clinical Insights<br />
– Preferred agents for pediatric infection<br />
• Trimethoprim/polymyxin B<br />
• Moxifloxacin<br />
• Azithromycin<br />
• Tobramycin<br />
• Erythromycin
<strong>Antibiotic</strong>/Steroid Combinations<br />
• Steroid first, antibiotic second<br />
• Should have indication for steroid treatment<br />
• Dosage dependent on steroid requirements<br />
– Tobramycin/dexamethosone<br />
– Tobramycin/loteprednol<br />
– Sulfacetamide/prednisolone phosphate<br />
– Sulfacetamide/prednisolone acetate<br />
– Gentamicin/prednisolone acetate<br />
Oral <strong>Antibiotic</strong>s<br />
• Penicillins ‐ Gram positive organisms, need efficacy<br />
against penicillinase producing Staphylococcus<br />
aureus, administer 1‐1.5 g/day in split doses<br />
– Amoxicillin/clavulanate potassium (Augmentin)<br />
– Dicloxacillin<br />
– Amoxicillin<br />
Fluoroquinolones<br />
• Broad spectrum antibacterial activity with<br />
greater potency than most other agents<br />
• Efficacy against both G+ & G‐ organisms<br />
• However, resistant strains are developing<br />
particularly to the earlier generation drugs<br />
Oral <strong>Antibiotic</strong> Agents<br />
• Oral Medications<br />
– Penicillins<br />
• Amoxicillin/clavulanic acid<br />
• Dicloxacillin<br />
• Amoxicillin<br />
– Cephalosporins<br />
• Cephalexin<br />
• Cefaclor<br />
• Cefadroxil<br />
– Fluoroquinolones<br />
• Levofloxacin<br />
• Moxifloxacin<br />
• Ciprofloxacin<br />
Oral <strong>Antibiotic</strong>s<br />
• Cephalosporins ‐ may have broader spectrum of<br />
activity, need efficacy against penicillinase producing<br />
Staphylococcus aureus, administer 1‐1.5 g/day in<br />
split doses<br />
– Cefadroxil (Duricef)<br />
– Cephalexin (Keflex, KefTab)<br />
– Cefaclor (Ceclor)<br />
– Cefazolin (Ancef) –topical only as fortified agent<br />
– Ceftazidime (Ceptaz, <strong>For</strong>taz) –topical only as fortified<br />
agent<br />
– Ceftriaxone (Rocephin) – injectable, IV only<br />
Oral <strong>Antibiotic</strong>s<br />
• Fluoroquinolones ‐ broad spectrum G+ & G‐ activity<br />
– Levofloxacin (Levaquin) typical dosage 500‐750<br />
mg qd x 7 days<br />
– Moxifloxacin (Avelox) typical dosage 400mg qd x 7<br />
days<br />
– Ciprofloxacin (Cipro) typical dosage 250‐500 mg<br />
bid x 7days
Fluoroquinolones<br />
• Fluoroquinolone agents usually not preferred over<br />
penicillins, cephalosporins or macrolides for routine<br />
cases.<br />
• However, may be needed if other agents have been<br />
ineffective or patient has risk factors, such as blood<br />
borne viral disease or being immunocompromised<br />
• Fluoroquinolone agents not usually preferred for<br />
pediatric infection due to risk of adverse reactions.<br />
• Not good choice for children ‐ cartilage damage, bone<br />
development issues, increased risk of tendon rupture<br />
(Achilles), can elevate theophylline levels<br />
Oral <strong>Antibiotic</strong>s<br />
• Macrolides ‐ both G+ & G‐ activity with<br />
efficacy against Chlamydia trachomatis<br />
– Azithromycin (Zithromax) 500 mg first day,<br />
followed by 250 mg x 4 days<br />
• <strong>For</strong> Chlamydia trachomatis ‐ Initially 1,000 mg single<br />
dose<br />
• If not effective, give full course of drug or switch to<br />
doxycycline<br />
– Erythromycin EES 400 mg qid<br />
• Achieve equivalent of erythromycin 500 mg base<br />
Macrolides<br />
• Erythromycin may also be contraindicated if<br />
patient taking any of the following drugs.<br />
– Anticoagulant agents<br />
– Digoxin<br />
– Statin agents<br />
– Dilantin<br />
– Theophylline<br />
Oral <strong>Antibiotic</strong> Agents<br />
• Oral Medications<br />
– Macrolides<br />
• Azithromycin<br />
• Erythromycin<br />
– Tetracyclines<br />
• Doxycycline<br />
• Tetracycline<br />
• Minocycline<br />
– Folic acid inhibitor<br />
• Trimethoprim/Sulfamethoxazole<br />
Macrolides<br />
• Erythromycin is the antibiotic agent with the<br />
highest risk of interacting with other oral<br />
medications. If not certain, check PDR,<br />
PubMed, MedlinePlus, etc. prior to<br />
prescribing.<br />
• Example ‐ Fexofenadine taken concurrently<br />
with erythromycin may lead to a toxic<br />
reaction in susceptible patients.<br />
Oral <strong>Antibiotic</strong>s<br />
• Tetracyclines ‐ anti‐inflammatory effects,<br />
collagenase inhibitor, metalloproteinase‐9<br />
inhibitor<br />
– Tetracycline 250 mg qid<br />
– Doxycycline (Vibramycin) 50‐100 mg bid<br />
– Minocycline (Cleeravue‐M) 50‐100 mg bid
Tetracyclines<br />
• Three groups of drugs ranging from short to long<br />
acting<br />
• Most useful drugs:<br />
– Tetracycline ‐ short acting<br />
– Doxycycline ‐ long acting<br />
– Minocycline ‐ long acting<br />
• Some tetracyclines are incompletely absorbed in<br />
fasting state<br />
• Doxycycline and minocycline absorbed more<br />
completely, more tolerant of dairy products<br />
Tetracyclines<br />
• Tetracyclines (including doxycycline, minocycline)<br />
not effective against many common bacteria due to<br />
bacterial resistance issues. In eye care, drugs mainly<br />
utilized for their apparent anti‐inflammatory effects<br />
and treatment of Chlamydia trachomatis.<br />
• When treating acne rosacea (inflammation),<br />
important to taper tetracycline agent over several<br />
months.<br />
Trimethoprim & Pyrimethamine<br />
• Trimethoprim efficacious for most Gram positive and<br />
negative organisms, not effective against<br />
Pseudomonas aeruginosa<br />
• Trimethoprim well absorbed from the GI tract<br />
• Pyrimethamine initially used to treat malaria<br />
• Both drugs used for treatment of toxoplasmosis in<br />
combination with sulfonamides<br />
• Sulfamethoxazole and Trimethoprim (Bactrim DS)<br />
typical dosage for bacterial infection 800 mg of<br />
sulfamethoxazole and 160 mg of trimethoprim q12h,<br />
duration dependent on clinical entity<br />
Tetracyclines<br />
• Some antibiotic agents can interfere with oral birth<br />
control agents, particularly tetracycline.<br />
• Actual breast cancer risk with tetracycline or<br />
doxycycline still uncertain. Keep up with literature<br />
in this area.<br />
• Optic disc edema and pseudotumor cerebrei have<br />
been reported as adverse events with tetracycline<br />
agents but are not common. However, monitor and<br />
be suspicious of patients reporting headaches while<br />
being treated with these agents.<br />
Oral <strong>Antibiotic</strong>s<br />
Sulfonamide/Trimethoprim Combinations<br />
• Sulfamethoxazole and Trimethoprim<br />
(Bactrim, Bactrim DS)<br />
• Typical dosage for bacterial infection is double<br />
strength formulation 800 mg of<br />
sulfamethoxazole and 160 mg of<br />
trimethoprim q12h<br />
• Duration dependent on clinical entity