婦癌
婦癌
婦癌
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Taipei Veterans General Hospital<br />
Practice Guideline for GYN Cancer<br />
1<br />
2012 台北榮總<strong>婦癌</strong>診療指引<br />
初版 2007 年 10 月 17 日<br />
修正版 ( 七 ) 2012 年 04 月 25 日
1.前言<br />
2. Cervical Cancer<br />
目錄<br />
(1) Stage -------------------------------------------------------- 4<br />
(2) Treatment Strategy -------------------------------------- 5<br />
(3) Chemotherapeutic Regimens -------------------------- 9<br />
3. Endometrial Cancer<br />
2<br />
2012 台北榮總<strong>婦癌</strong>診療指引<br />
(1) Stage (uterine carcinoma & sarcoma) --------------- 14<br />
(2) Treatment Strategy -------------------------------------- 17<br />
(3) Chemotherapeutic Regimens -------------------------- 21<br />
4. Epithelial Ovarian Cancer<br />
(1) Stage (ovary, PPSC , and tube cancer) ---------------- 25<br />
(2) Treatment Strategy -------------------------------------- 27<br />
(3) Chemotherapeutic Regimens -------------------------- 28<br />
5. Borderline Ovarian Cancer<br />
(1) Treatment Strategy -------------------------------------- 35<br />
6. 化療的毒性--------------------------------------------------- 37<br />
7. 參考資料-------------------------------------------------------42
前言<br />
3<br />
2012 台北榮總<strong>婦癌</strong>診療指引<br />
95 年癌症委員會與本院癌症治療專家共同參與討論制定癌症治療準<br />
則,於 95 年 5 月制定本院子宮頸癌治療準則,<strong>婦癌</strong>多專科醫療團隊以國家<br />
衛生研究院<strong>婦癌</strong>診療指引及 NCCN GUIDELINE 治療準則為基準,於 96 年<br />
10 月始召開本院第一次子宮頸癌團隊會議,腫瘤個案管理師並於 96 年 10<br />
月針對新診斷子宮頸癌個案開始收案,新診斷個案定義:含 class 1~3 病人,<br />
class 1 (本院診斷,於本院接受全部或部分首次治療療程,含拒絕治療決定<br />
不治療)、class 2 (外院診斷,於本院接受全部或部分首次治療療程,含拒絕<br />
治療決定不治療)、class 3 (外院診斷,於外院接受全部首次治療療程),為<br />
服務更多<strong>婦癌</strong>病患,於 98 年 1 月開始進行子宮內膜癌個案收案 (不含惡性<br />
肉瘤,99 年開始 MMMT 併入子宮內膜癌收案),99 年 1 月開始,針對卵巢<br />
癌個案收案(只收上皮性卵巢癌,於 100 年 1 月開始進行非上皮性卵巢癌收<br />
案) ,101 年 1 月開始將腹膜癌及輸卵管癌列入卵巢癌診療指引,團隊成員<br />
經多次會議修訂本院<strong>婦癌</strong>診療共識,並至少每年修訂診療指引一次,據以<br />
公告週知以供查閱。<br />
本共識與上一版差異<br />
1. 將三癌 (子宮頸癌、子宮體癌、卵巢癌) 分開版本彙整為一個版本 (<strong>婦癌</strong>)<br />
2. 加入子宮頸癌、子宮內膜癌、肉瘤 (未列入收案)、卵巢癌及輸卵管癌<br />
FIGO 及 TNM 期別參考 (2010 年第 7 版:The MX designation has been<br />
eliminated from the AJCC/UJCC TNM system)。<br />
3. 新增子宮體癌病理分化程度等級及第一型、第二型子宮體癌說明表格。<br />
4. 新增顏明賢主任編著之化療的毒性<br />
返回目錄
Cervical Cancer<br />
4<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮頸癌<br />
Staging cervical cancer (FIGO stage, 2009 and TNM AJCC 7th ed, 2010)<br />
Primary tumor (T)<br />
TNM FIGO Definition<br />
T1 I Cervical carcinoma confined to uterus (extension to corpus should be disregarded)<br />
T1a IA<br />
T1a1 IA1<br />
T1a2 IA2<br />
Invasive carcinoma diagnosed only by microscopy. Stromal invasion with a maximum<br />
depth of 5.0 mm measured from the base of the epithelium and a horizontal spread of<br />
7.0 mm or less. Vascular space involvement, venous or lymphatic, does not affect<br />
classification.<br />
Measured stromal invasion 3.0 mm or less in depth and 7.0 mm or less in horizontal<br />
spread<br />
Measured stromal invasion more than 3.0 mm and not more than 5.0 mm in depth with<br />
a horizontal spread 7.0 mm or less<br />
T1b IB Clinically visible lesion confined to the cervix or microscopic lesion greater than T1a/IA2<br />
T1b1 IB1 Clinically visible lesion 4.0 cm or less in greatest dimension<br />
T1b2 IB2 Clinically visible lesion more than 4.0 cm in greatest dimension<br />
T2 II<br />
Cervical carcinoma invades beyond uterus but not to pelvic wall or to lower third of<br />
vagina<br />
T2a IIA Tumor without parametrial invasion or involvement of the lower one-third of the vagina<br />
T2a1 IIA1<br />
T2a2 IIA2<br />
Clinically visible lesion 4.0 cm or less in greatest dimension with involvement of less than<br />
the upper two-thirds of the vagina<br />
Clinically visible lesion more than 4.0 cm in greatest dimension with involvement of less<br />
than the upper two-thirds of the vagina<br />
T2b IIB Tumor with parametrial invasion<br />
T3 III<br />
Tumor extends to pelvic wall and/or involves lower third of vagina, and/or causes<br />
hydronephrosis or nonfunctioning kidney<br />
T3a IIIA Tumor involves lower third of vagina, no extension to pelvic wall<br />
T3b IIIB Tumor extends to pelvic wall and/or causes hydronephrosis or nonfunctioning kidney<br />
T4 IVA<br />
Regional lymph nodes (N)<br />
Tumor invades mucosa of bladder or rectum, and/or extends beyond true pelvis (bullous<br />
edema is not sufficient to classify a tumor as T4)<br />
TNM FIGO Definition<br />
NX<br />
N0<br />
Regional lymph nodes cannot be assessed<br />
No regional lymph node metastasis<br />
N1 IIIB Regional lymph node metastasis<br />
Distant metastasis (M)<br />
TNM FIGO Definition<br />
M0<br />
M1 IVB<br />
No distant metastasis<br />
Distant metastasis (including peritoneal spread, involvement of supraclavicular,<br />
mediastinal, or paraaortic lymph nodes, lung, liver, or bone)<br />
*Note: All macroscopically visible lesion-even with superficial invasion are T1b/IB<br />
返回目錄
術前準備<br />
- Blood analysis<br />
- Pathology proved<br />
- Tumor marker<br />
子宮頸癌治療指引<br />
- CT scan / MRI / PET-CT (小心健保剔退) if clinically indicated<br />
- Cystoscopy / Colonoscopy if clinically indicated<br />
FIGO Early Stage (IA to IIA, selective IIB)<br />
Stage Treatment Plan<br />
IA1<br />
IA2<br />
IB1<br />
IIA1<br />
IB2<br />
IIA2<br />
Selective IIB<br />
50 y/o, adenocarcinoma, and poorly differentiated.<br />
● Treatment guideline for other cell types (adenosquamous、neuroendocrine、adenosarcoma、clear<br />
cell、MMMT、sarcoma ) will be discussed and planned after evaluation by the gynecology<br />
oncology committee.<br />
● Ovarian transposition during RH if adjuvant radiotherapy considered (No oophorectomy).<br />
●Laparotomy or Laparoscopic surgery is acceptable (stage IA1、IA2、IB1、IIA1,但 Radical<br />
trachelectomy 狀況除外) .<br />
返回目錄
手術後的輔助治療 (FIGO 早期)<br />
6<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮頸癌<br />
LN Parametrium Bulky size Management<br />
(-)<br />
(-)<br />
(-)<br />
(+)<br />
(+) (-) or (+)<br />
(+) (-) or (+) (-) or (+)<br />
LVSI (-)<br />
DSI (-)<br />
LVSI (+)<br />
and / or<br />
DSI (+)<br />
LVSI (+)<br />
and / or<br />
DSI (+)<br />
LVSI (+)<br />
and / or<br />
DSI (+)<br />
LVSI (+)<br />
and / or<br />
DSI (+)<br />
If vaginal cut end (+) additional radiotherapy required<br />
Prognostic Risk Factors:<br />
High Risk:<br />
- LN (+) / Parametrial margin (+) / Vaginal cut end margin (+)<br />
Intermediate Risk:<br />
- Bulky tumor size ( ≥ 4 cm ) / LVSI (+) / DSI (+)<br />
Others<br />
- Age / Diploidy / Differentiation / Histological type<br />
Adenocarcinoma type<br />
- Adjuvant systemic treatment may be considered in the stage IB<br />
- IB2 with intermediate risk<br />
CCRT for primary treatment followed by systematic chemotherapy<br />
Observation<br />
Radiotherapy (C-1)<br />
or Observation<br />
Radiotherapy (C-1)<br />
or Obsertvation<br />
or CCRT (see below)<br />
CCRT (see below)<br />
or Radiotherapy<br />
CCRT (see below) ± vaginal<br />
brachytherapy (C-1)<br />
or Chemotherapy (see below)<br />
Or Radiotherapy<br />
返回目錄
FIGO 早期不能手術及晚期患者<br />
Step 1<br />
Lymph Node Assessment<br />
- Image study (CT scan, MRI or PET) ± FNA<br />
7<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮頸癌<br />
- Surgical staging (laparotomy, extrafascial, or laparoscopic lymph node sampling)<br />
Step 2<br />
Lymph Node (-)<br />
- CCRT (platinum-based chemotherapy) ± Para-aortic boost (Point A ≧ 85Gy)<br />
Lymph Node(+)<br />
Step 3<br />
- CCRT (platinum-based chemotherapy) + Para-aortic boost (Point A ≧ 85Gy)<br />
Consolidation chemotherapy, if necessary<br />
- 5 year survival rate<br />
- Stage IIB-IVA: 20-60%<br />
- Stage IVB: < 20 %<br />
返回目錄
單純子宮切除後意外發現<br />
Stroma<br />
Invasion<br />
Depth < 3 mm<br />
Stroma<br />
Invasion<br />
Depth < 3 mm<br />
with LVSI (+)<br />
or<br />
Depth ≧ 3mm<br />
Surgical<br />
Margin<br />
(-)<br />
(+)<br />
* Re-operate includes the following:<br />
8<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮頸癌<br />
LVSI Management<br />
(-) Observation<br />
(+) See below<br />
LN status<br />
(Image<br />
study)<br />
(-)<br />
(+)<br />
(-)<br />
(+)<br />
Management<br />
Re-operation*<br />
or<br />
brachytherapy ±<br />
Pelvic R/T<br />
LND + CCRT<br />
or<br />
Re-operation*<br />
or<br />
CCRT (see below)<br />
Radiotherapy<br />
or<br />
CCRT (see below)<br />
or<br />
Re-operation*<br />
LND + CCRT<br />
or<br />
Re-operation*<br />
or<br />
CCRT (see below)<br />
- Radical parametrectomy + Upper vaginectomy + PLND ± PALNS<br />
- Image study consistent with the following:<br />
- No parametrial invasion<br />
- No pelvic side-wall invasion<br />
- No rectal or bladder invasion<br />
Adjuvant<br />
Therapy<br />
According to<br />
pathological<br />
risk factors<br />
(see above)<br />
返回目錄
化療處方建議<br />
子宮頸癌化療處方適應症-<br />
- Adjuvant chemotherapy for postoperative lymph node metastasis<br />
- Neoadjuvant chemotherapy for bulky tumor<br />
- Followed by surgery<br />
- Followed by radiotherapy<br />
- Concurrent chemoradiotherapy<br />
- Early bulky tumor followed by surgery<br />
9<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮頸癌<br />
- Postoperative with parametrial involvement and lymph node metastasis<br />
- Local advanced cancer<br />
- Consolidation chemotherapy after concurrent chemoradiotherapy for advanced cancer<br />
- Palliative chemotherapy for distant, recurrent, or metastatic cancer<br />
- If distant metastasis or recurrence Systemic Chemotherapy ± Palliative Radiotherapy<br />
Neoadjuvant Chemotherapy: (新輔助化療)<br />
1. Cisplatin Only (q w x 3 cycle)<br />
Cisplatin 40 mg/m 2 (at least > 25 mg/m 2 ) IVD 1hr<br />
- RH performed on 3 rd day after completing chemotherapy<br />
2. Palcitaxel + Cisplatin Regimen (q 10 d x 3 cycle)<br />
Palcitaxel 60 mg/m 2 IVD 1.5 hrs<br />
Cisplatin 60 mg/m 2 IVD 1 hr<br />
- RH performed within 3 weeks after completing chemotherapy<br />
CCRT regimen: (同步化學放射治療)<br />
1. Cisplatin Only (q w)<br />
Cisplatin 40 mg/m 2 IVD 1 hr<br />
2. POB Regimen (q 3 w)<br />
Cisplatin 50 mg/m 2 1 hr<br />
Vincristine 1 mg/m 2 IVD 15-30 mins<br />
Bleomycin 15 mg (D1~3) IVD 15 mins(累積劑量不可>150mg )<br />
Consolidation Chemotherapy Regimen: (鞏固化療)<br />
1. I+P regimen (q 3 w x 6 cycle)<br />
(1) Ifosfamide (24 hrs) + Cisplatin<br />
Ifosfamide 5 gm/m 2 IVD 24 hrs<br />
Cisplatin 50 mg/m 2 IVD 1 hr<br />
返回目錄
(2) Ifosfamide (3 days) +Cisplatin<br />
Ifosfamide 1 gm/m 2 IVD 24 hrs<br />
Cisplatin 50 mg/m 2 IVD 1 hr<br />
2. Paclitaxel + Cisplatin Regimen (q 3 w x 6 cycle)<br />
Paclitaxel 135 mg/m 2 IVD 3 hrs<br />
Cisplatin 50 mg/m 2 IVD 1 hr<br />
3. Topotecan (D1~3) + Platinum Regimen (q 3 w x 6 cycle)<br />
Topotecan 0.75 mg/m 2 (D1~D3) IVD 30 mins<br />
10<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮頸癌<br />
Cisplatin 50 mg/m 2 (D1) or Carboplatin AUC5 (D3) if Ccr
Cisplatin 50 mg/m 2<br />
7. Irinotecan + Cisplatin Regimen(x 6 cycle)<br />
Irinotecan 60mg/m 2 (D1 / D8 / D15)<br />
Cisplatin 60 mg/m 2 (D1) IVD 1 hr<br />
Common used Regimen for Non-squamous Cell Carcinoma<br />
1. Paclitaxel + Cisplatin Regimen (q 3 w)<br />
Paclitaxel 175 mg/m 2 IVD 3 hrs<br />
Cisplatin 75 mg/m 2 IVD 1 hr<br />
2. Paclitaxel Only (q3w)<br />
Paclitaxel 175 mg/m 2 IVD 3 hrs<br />
11<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮頸癌<br />
Paclitaxel 135 mg/m 2 IVD 3 hrs (if prior radiotherapy)<br />
- Dose escalation to 200 mg/m 2 or de-escalation to 110 mg/m 2 depending on toxicity<br />
3. Etoposide Only (every 28 days)<br />
- Oral Etoposide 50 mg/m 2 /day for 21 days<br />
- Oral Etoposide 40 mg/m 2 /day (if prior radiotherapy) for 21 days<br />
- Dose escalation to 60mg/m 2 /day depending on toxicity<br />
4. VIP Regimem (for neuroendocrine cell type) (q 3~4 w x 6 courses)<br />
- Etoposide 100mg/m 2 IVD 1 hr (D1~3)<br />
- Ifosfamide 1500 mg/m 2 IVD 1 hr (D1~3)<br />
- Cisplatin 50 mg/m 2 IVD 2 hr (D1)<br />
備註:Cisplatin 為子宮頸癌治療化學治療首選藥物,若 (CCr < 60),Carboplatin 可做<br />
為替代藥物取代 (<strong>婦癌</strong>個案注射 Cisplatin 若因 CCR ≤ 60,weekly Cisplatin 40<br />
mg/m 2 ,可改為 Carboplatin AUC 2;若非 weekly 用法,如 Cisplatin Q 3 W 使用,則<br />
為 75 mg/m 2 改為 Carboplatin AUC 5。)<br />
疾病持續/復發治療策略<br />
考慮因素:<br />
- Site of recurrence or metastases<br />
Pelvic Extra-pelvic<br />
- Central - Intra-abdominal organs<br />
- Side wall - Distant lymph nodes<br />
- Combined - Distant disseminated metastases<br />
- Prior therapy<br />
- Surgery Radiotherapy<br />
- Radiotherapy Surgery<br />
返回目錄
- Possible routes or mechanisms of spread<br />
- Status of patient's performance<br />
- Palliative or Curative treatment<br />
Cervical Cancer with Central Recurrence (中央復發)<br />
Prior Surgery<br />
- Surgical intervention if no contraindication<br />
- Radiotherapy if surgical intervention not possible<br />
Prior Radiotherapy<br />
- Surgical intervention if no contraindication<br />
- Radiotherapy indicated if recurrence outside of previously treated field<br />
- Palliative radiotherapy<br />
- Palliative chemotherapy (see above)<br />
Surgical Intervention<br />
- If previous surgery is only total abdominal hysterectomy<br />
- Radical parametrectomy + PLND + PALNS<br />
- If previous surgery is radical hysterectomy + PLND + PALNS<br />
- Exenteration can be considered (Total / Anterior / Posterior)<br />
12<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮頸癌<br />
- Exenterative surgery should NOT be used as a palliative treatment, except in the<br />
presence of malignant fistulas in the pelvis.<br />
- Final intraoperative assessment:<br />
- The final decision to proceed with exenteration will not be made until the<br />
abdomen has been opened and assessment of the pelvic side-wall and posterior<br />
abdominal wall has been made, utilizing frozen section where necessary.<br />
- Contraindication of exenterative surgery<br />
Absolute Contraindication Relative Contraindication<br />
- Metastases to extrapelvic LN - Obesity<br />
- Metastases to abdominal viscera<br />
- Metastases to lung or bones - Triad *<br />
* TRIAD:<br />
- Pelvic side-wall spread:<br />
direct extension or nodal metastases<br />
1. Unilateral uropathy, non-functional kidney, or ureteric obstruction<br />
2. Unilateral leg edema<br />
3. Sciatic leg pain<br />
返回目錄
13<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮頸癌<br />
Cervical Cancer with Pelvic Side Wall Recurrence (側壁復發)<br />
Prior Surgery<br />
- Radiotherapy recommended<br />
Prior Radiotherapy<br />
- Surgical intervention if no contraindication<br />
- LEER procedure: laterally extended endopelvic resection<br />
- CORT procedure: combined operative and radio-therapeutic treatment for close or<br />
positive margins<br />
- Indication:<br />
- Histological confirmed, unifocal pelvic side-wall recurrence<br />
- Free from tumor dissemination<br />
- Tumor limited to a maximal diameter of < 5 cm<br />
- Medical condition compatible with major surgery.<br />
- Willingness to accept urinary or fecal diversion<br />
- Radiotherapy ± chemotherapy indicated if recurrence outside of previously treated field<br />
- Palliative radiotherapy<br />
- Palliative chemotherapy (see above)<br />
Cervical Cancer with Central and Pelvic Side Wall Recurrence<br />
(中央及側壁復發)<br />
Prior Surgery<br />
- Radiotherapy recommended<br />
Prior Radiotherapy<br />
- Radiotherapy indicated if recurrence outside of previously treated field<br />
- Palliative radiotherapy<br />
- Palliative chemotherapy (see above)<br />
Only Distant LN Metastasis (including para-aortic LN)<br />
(只有遠處淋巴結轉移(包括腹主動脈旁淋巴結))<br />
- Radiotherapy recommended<br />
- Chemotherapy recommended (see above)<br />
- CCRT recommended (see above)<br />
Intra-abdominal Organ Metastasis (腹內臟器轉移)<br />
- Chemotherapy recommended (see above)<br />
- Palliative surgery only for intestinal obstruction<br />
Dissemination(遠處轉移)<br />
- Multiple sites or unresectable → Chemotherapy recommended (see above)<br />
- Resectable →Surgery → R/T ± chemotherapy<br />
→ Chemotherapy ± R/T<br />
返回目錄
Uterine Cancer<br />
14<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮內膜癌<br />
Staging uterine carcinoma (FIGO stage, 2009 and TNM AJCC 7th ed,2010)<br />
Primary tumor (T) (surgical-pathologic findings)<br />
TNM<br />
categories<br />
TX<br />
T0<br />
Tis*<br />
FIGO<br />
stages<br />
Definition<br />
Primary tumor cannot be assessed<br />
No evidence of primary tumor<br />
Carcinoma in situ (preinvasive carcinoma)<br />
T1 I Tumor confined to corpus uteri<br />
T1a IA<br />
Tumor limited to endometrium or invades less than one-half of the<br />
myometrium<br />
T1b IB Tumor invades one-half or more of the myometrium<br />
T2 II<br />
T3a IIIA<br />
T3b IIIB<br />
T4 IVA<br />
Regional lymph nodes (N)<br />
TNM<br />
categories<br />
NX<br />
N0<br />
FIGO<br />
stages<br />
Tumor invades stromal connective tissue of the cervix but does not<br />
extend beyond uterus<br />
Tumor involves serosa and/or adnexa (direct extension or<br />
metastasis)<br />
Vaginal involvement (direct extension or metastasis) or parametrial<br />
involvement<br />
Tumor invades bladder mucosa and/or bowel mucosa (bullous<br />
edema is not sufficient to classify a tumor as T4)<br />
Definition<br />
Regional lymph nodes cannot be assessed<br />
No regional lymph node metastasis<br />
N1 IIIC1 Regional lymph node metastasis to pelvic lymph nodes<br />
N2 IIIC2<br />
Distant metastasis (M)<br />
TNM<br />
categories<br />
M0<br />
FIGO<br />
stages<br />
M1 IVB<br />
Regional lymph node metastasis to para-aortic lymph nodes, with<br />
or without positive pelvic lymph nodes<br />
No distant metastasis<br />
Definition<br />
Distant metastasis (includes metastasis to inguinal lymph nodes<br />
intraperitoneal disease, or lung, liver, or bone. It excludes<br />
metastasis to para-aortic lymph nodes, vagina, pelvic serosa, or<br />
adnexa.)<br />
*Note: endocervical glandular involvement only should be considered as Stage I and no<br />
longer as Stage II<br />
返回目錄
15<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮內膜癌<br />
Staging uterine sarcoma (TNM and FIGO Study)參考用,個管未列入收案<br />
Primary tumor (T)*<br />
TNM FIGO Definition<br />
Leiomyosarcoma and endometrial stromal<br />
sarcoma<br />
Adenosarcoma<br />
T1 I Tumor limited to the uterus Tumor limited to the uterus<br />
T1a IA<br />
Tumor 5 cm or less in greatest<br />
dimension<br />
T1b IB Tumor more than 5 cm<br />
T1c IC X<br />
Tumor limited to the<br />
endometrium / endocervix<br />
Tumor invades to less than<br />
half of the myometrium<br />
Tumor invades more than<br />
half of the myometrium<br />
T2 II Tumor extends beyond the uterus, within the pelvis<br />
T2a IIA Tumor involves adnexa<br />
T2b IIB Tumor involves other pelvic tissues<br />
T3 III Tumor infiltrates abdominal tissues<br />
T3a IIIA One site<br />
T3b IIIB More than one site<br />
T4 IVA Tumor invades bladder or rectum<br />
Regional lymph nodes (N)<br />
TNM<br />
categories<br />
FIGO<br />
stages<br />
Definition<br />
Leiomyosarcoma, endometrial stromal sarcoma and Adenosarcoma<br />
NX<br />
N0<br />
Regional lymph nodes cannot be assessed<br />
No regional lymph node metastasis<br />
N1 IIIC Regional lymph node metastasis<br />
Distant metastasis (M)<br />
TNM<br />
categories<br />
FIGO<br />
stages<br />
Definition<br />
Leiomyosarcoma, endometrial stromal sarcoma and Adenosarcoma<br />
M0 No distant metastasis<br />
M1 IVB<br />
Distant metastasis (excluding adnexa, pelvic and abdominal<br />
tissues)<br />
Carcinosarcomas should be staged as carcinomas of the endometrium<br />
返回目錄
子宮癌等級:病理分化程度<br />
16<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮內膜癌<br />
Cases of carcinoma of the corpus should be grouped with regard to the degree<br />
of differentiation of the adenocarcinoma as follows:<br />
G1 5 percent or less of a non-squamous or non-morular solid growth pattern<br />
G2<br />
6 percent to 50 percent of a non-squamous or non-morular solid growth<br />
pattern<br />
G3 More than 50 percent of a non-squamous or non-morular solid growth pattern<br />
Endometrial carcinoma, types 1 vs. type 2<br />
Histology endometrioid carcinoma<br />
typical patient<br />
Estrogen<br />
receptor<br />
MIB1<br />
proliferation<br />
index<br />
Molecular<br />
genetic<br />
changes<br />
perimenopausal or<br />
Type 1 Type 2<br />
early postmenopausal women<br />
background of endometrial<br />
hyperplasia<br />
serous carcinoma,<br />
clear cell carcinoma<br />
elderly women<br />
low-grade high-grade<br />
atrophic endometrium<br />
estrogen-dependent not estrogen-dependent<br />
may show a focal or diffuse<br />
papillary pattern<br />
usually positive;<br />
high-grade cases may be<br />
negative<br />
a glandular variant shows little or<br />
no papillary formation but has<br />
high-grade cytology<br />
negative<br />
low high<br />
PTEN or<br />
KRAS gene mutation;<br />
microsatellite instability<br />
P53 or<br />
HER2 or<br />
E-cadherin mutation<br />
返回目錄
術前準備<br />
- Blood analysis<br />
- Tumor marker<br />
- Ultrasound / Doppler / CT / MRI<br />
- Pathology proved<br />
主要治療<br />
- Staging surgery (分期手術)<br />
- Stage I<br />
子宮內膜癌治療指引<br />
17<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮內膜癌<br />
Peritoneal cytology + Hysterectomy (Level 1) + BSO ± (BPLND + PALNS)<br />
- Stage II<br />
Peritoneal cytology + Hysterectomy (Level 1 or 2) / Radical Hysterectomy<br />
(Level 3) + BSO + BPLND + PALND<br />
- Stage III/IV or type II histology (as ovarian cancer staging surgery)<br />
Peritoneal cytology + Hysterectomy (Level 1) + BSO + BPLND + PALNS +<br />
omentectomy + debulking surgery<br />
- Type II histology: papillary serous, clear cell or carcinosarcoma<br />
- Ovarian preservation: dependent on patient age, condition, and willingness<br />
- Inoperable condition (不能手術情況)<br />
- Radiotherapy<br />
返回目錄
輔助治療(According to FIGO stage 2009)<br />
Stage I (post complete surgical staging)<br />
Stage 1A<br />
MI + (-)<br />
Stage 1A<br />
MI + (+)<br />
Stage 1B<br />
Adverse<br />
risk<br />
factors<br />
(-)<br />
(+)<br />
18<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮內膜癌<br />
G1 G2 G3<br />
Observation Observation<br />
(-) Observation Observation<br />
(+)<br />
Vaginal<br />
brachytherapy<br />
(-) Observation<br />
(+)<br />
Vaginal<br />
brachytherapy<br />
or<br />
Pelvic RT ± Vaginal<br />
brachytherapy*<br />
Vaginal<br />
brachytherapy<br />
or<br />
Pelvic RT ± Vaginal<br />
brachytherapy*<br />
Observation<br />
or<br />
Vaginal<br />
brachytherapy<br />
Vaginal<br />
brachytherapy<br />
or<br />
Pelvic RT ± Vaginal<br />
brachytherapy*<br />
± Chemotherapy*<br />
Observation<br />
or<br />
Vaginal<br />
brachytherapy<br />
or<br />
Pelvic RT ± Vaginal<br />
brachytherapy*<br />
Observation<br />
or<br />
Vaginal<br />
brachytherapy<br />
or<br />
Pelvic RT ± Vaginal<br />
brachytherapy*<br />
± Chemotherapy*<br />
Pelvic RT ± Vaginal<br />
brachytherapy*<br />
± Chemotherapy*<br />
Type II histology: Stage IA, MI (-): Observation or Chemotherapy or vaginal brachytherapy<br />
MI + : myometrial invasion<br />
Stage IA, MI (+), IB: Chemotherapy ± tumor-directed RT or Whole<br />
Adverse risk factors include the following:<br />
- > 60 y/o<br />
- positive lymphovascular invasion<br />
- tumor size ≧ 2cm<br />
- lower uterine involvement<br />
* 仍未定論<br />
abdominopelvic RT<br />
± Vaginal brachytherapy*<br />
返回目錄
Stage II (post complete surgical staging)<br />
MI < 50%<br />
MI > 50%<br />
Type II histology:<br />
19<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮內膜癌<br />
G1 G2 G3<br />
Observation<br />
or<br />
Vaginal brachytherapy<br />
Pelvic radiotherapy<br />
± Vaginal brachytherapy<br />
± Chemotherapy*<br />
Observation<br />
or<br />
Vaginal brachytherapy<br />
or<br />
Pelvic radiotherapy<br />
± Vaginal brachytherapy<br />
Pelvic radiotherapy<br />
± Vaginal brachytherapy<br />
± Chemotherapy*<br />
Stage II: Chemotherapy ± tumor-directed RT or Whole abdominopelvic RT<br />
± vaginal brachytherapy*<br />
MI: myometrial invasion<br />
If stage II patient received radical hysterectomy, they can be treated as stage I<br />
Adjuvant pelvic radiotherapy (RT): 40 ~ 50 Gy to CTV<br />
Pelvic radiotherapy<br />
± Vaginal brachytherapy<br />
± Chemotherapy*<br />
Pelvic radiotherapy<br />
+ Vaginal brachytherapy<br />
± Chemotherapy*<br />
- Upper vaginal tumor bed as vaginal cut end + parametrium + pelvic lymph nodes.<br />
* 仍未定論<br />
返回目錄
Stage III/ IV (post complete surgical staging)<br />
Stage III A<br />
20<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮內膜癌<br />
G1 G2 G3<br />
Tumor-directed radiotherapy ± chemotherapy<br />
or<br />
Pelvic radiotherapy ± Vaginal brachytherapy*<br />
or<br />
Whole abdominopelvic RT ± vaginal brachytherapy*<br />
or<br />
Chemotherapy ± radiotherapy**<br />
Stage IIIB Tumor-directed radiotherapy ± chemotherapy<br />
Stage IIIC1<br />
Stage IIIC2<br />
Stage IVA/B<br />
Type II histology<br />
Debulked and without<br />
gross residual disease<br />
or microscopic<br />
abdominal disease<br />
Chemotherapy ± Tumor-directed radiotherapy<br />
*Chemotherapy ± Tumor-directed radiotherapy<br />
Stage III/IV (adequately debulked): Chemotherapy ± tumor-directed RT or<br />
Stage III/IV (inadequately debulked): Chemotherapy<br />
* 仍未定論<br />
** 尚有爭議<br />
Whole abdominopelvic RT ± vaginal brachytherapy*<br />
返回目錄
化療處方建議<br />
Single agent Regimen(單一藥劑處方)<br />
21<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮內膜癌<br />
Dose Schedule IVD Cycle<br />
Cisplatin 50 mg/m 2 Q 3 W 1 hr 6<br />
Carboplatin AUC 5 以上 Q 4 W 1 hr 6<br />
Doxorubicin 60 mg/m 2 Q 3 W 20 mins ~1 hr 6<br />
Ifosphamide 1500 mg/m 2 (3-5 days) Q 3 W 1~2 hrs 6<br />
Paclitaxel 175 mg/m 2 Q 3 W 3 hrs 6<br />
Combination Regimen (組合藥劑處方)<br />
Dose Schedule IVD Cycle<br />
Doxorubicin + Cisplatin 60 / 50 mg/m 2 Q 3 W 1 hr /1 hr 8<br />
Paclitaxel + Cisplatin 175 (3 hrs) / 50 mg/m 2 Q 3W 3 hrs /1 hr 6<br />
Paclitaxel + Carboplatin 175 (3 hrs) / AUC 5~7.5 Q 3 W 3 hrs /1 hr 6<br />
CAP<br />
Cyclophosphamide +<br />
Doxorubicin + Cisplatin<br />
TAP<br />
Paclitaxel + Doxorubicin<br />
+ Cisplatin+ GCSF<br />
600 / 45 / 50 mg/m 2 Q 4W<br />
160 / 45 / 50 mg/m 2 Q 3 W<br />
>30mins/<br />
1~2 hrs/1 hr<br />
3 hrs /<br />
>30mins/1 hr<br />
6<br />
7<br />
返回目錄
不完整分期手術後意外發現<br />
Histologic<br />
findings<br />
Stage IA G1, 2<br />
without risk<br />
factors<br />
Stage IA G1, 2<br />
with adverse risk<br />
factors<br />
Stage IB<br />
Stage II All G3<br />
22<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮內膜癌<br />
Image studies Management<br />
(-)<br />
Observation<br />
Observation<br />
or<br />
Vaginal brachytherapy<br />
or<br />
Pelvic radiotherapy<br />
(+) Complete surgical staging<br />
(-)<br />
Adverse risk factors include the following:<br />
- > 60 y/o<br />
- positive lymphovascular invasion<br />
- tumor size ≧ 2cm<br />
- lower uterine involvement<br />
* 仍未定論<br />
Pelvic radiotherapy<br />
+ Vaginal brachytherapy<br />
± Radiotherapy to PALN<br />
± Chemotherapy*<br />
(+) Complete surgical staging<br />
返回目錄
復發或復發性疾病<br />
Relapse or<br />
recurrence<br />
Vaginal<br />
recurrence<br />
Isolated<br />
metastasis<br />
Disseminated<br />
metastases<br />
Resectable<br />
lesion<br />
Unresectable<br />
lesion<br />
Asymptomatic<br />
or<br />
Grade 1<br />
Symptomatic<br />
or<br />
Grade 2.3<br />
or<br />
Large lesion<br />
23<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮內膜癌<br />
Salvage therapy<br />
Resection or Radiotherapy<br />
Surgery<br />
or<br />
± Radiotherapy<br />
Hormone treatment<br />
or<br />
Chemotherapy<br />
Hormone treatment<br />
or<br />
Chemotherapy<br />
or<br />
Clinical trials<br />
Chemotherapy or/± Tumor-directed radiotherapy<br />
or<br />
Chemotherapy ± palliative tumor directed radiotherapy<br />
or<br />
Clinical trials<br />
返回目錄
Conservative Treatment (Early Stage)早期保守治療<br />
Patient criteria<br />
- Type 1, Grade 1 tumor<br />
- No cervical or myometrial invasion (MRI)<br />
- Absence of suspicious of pelvic or para-aortic LN<br />
- Absence of synchronous ovarian tumor<br />
- No contraindication for medical treatment<br />
- Fertility preservation<br />
- Compliant and strict follow-up<br />
Medical treatment (high-dose progestin)<br />
- Medroxyprogesterone acetate: 200-600mg/day for 6 months<br />
- Megestrol acetate: 80-160mg/day<br />
Follow-up<br />
D&C every 3 months<br />
(maximum up to 6<br />
months)<br />
24<br />
2012 台北榮總<strong>婦癌</strong>診療指引-子宮內膜癌<br />
Biopsy (-) Biopsy (+)<br />
Encourage pregnancy<br />
or<br />
Intermittent biopsy<br />
Surgical intervention<br />
返回目錄
Epithelial Ovarian Cancer<br />
25<br />
2012 台北榮總<strong>婦癌</strong>診療指引-卵巢癌<br />
Staging ovarian and primary peritoneal carcinoma (FIGO stage, 2009 and TNM AJCC 7th ed, 2010)<br />
Primary tumor (T)*<br />
TNM FIGO Definition<br />
T1 I Tumor limited to ovaries (one or both)<br />
T1a IA<br />
T1b IB<br />
T1c IC<br />
Tumor limited to one ovary; capsule intact, no tumor on ovarian surface. No<br />
malignant cells in ascites or peritoneal washings.<br />
Tumor limited to both ovaries; capsules intact, no tumor on ovarian<br />
surface. No malignant cells in ascites or peritoneal washings.<br />
Tumor limited to one or both ovaries with any of the following:<br />
capsule ruptured, tumor on ovarian surface, malignant cells in ascites or<br />
peritoneal washings<br />
T2 II Tumor involves one or both ovaries with pelvic extension<br />
T2a IIA<br />
T2b IIB<br />
T2c IIC<br />
T3 III<br />
Extension and/or implants on uterus and/or tube(s).<br />
No malignant cells in ascites or peritoneal washings.<br />
Extension to and/or implants on other pelvic tissues.<br />
No malignant cells in ascites or peritoneal washings.<br />
Pelvic extension and/or implants (T2a or T2b) with malignant cells in<br />
ascites or peritoneal washings<br />
Tumor involves one or both ovaries with microscopically confirmed<br />
peritoneal metastasis outside the pelvis<br />
T3a IIIA Microscopic peritoneal metastasis beyond pelvis (no macroscopic tumor)<br />
T3b IIIB<br />
T3c IIIC<br />
Regional lymph nodes (N)<br />
Macroscopic peritoneal metastasis beyond pelvis 2 cm or less in greatest<br />
dimension<br />
Peritoneal metastasis beyond pelvis more than 2 cm in greatest dimension<br />
and/or regional lymph node metastasis<br />
TNM FIGO Definition<br />
NX<br />
N0<br />
Regional lymph nodes cannot be assessed<br />
No regional lymph node metastasis<br />
N1 IIIC Regional lymph node metastasis<br />
Distant metastasis (M)<br />
TNM FIGO Definition<br />
M0<br />
No distant metastasis<br />
M1 IV Distant metastasis (excludes peritoneal metastasis)<br />
Note: liver capsule metastasis is T3/Stage III;<br />
liver parenchymal metastasis,M1/ Stage IV.<br />
Pleural effusion must have positive cytology for M1/ Stage IV.<br />
返回目錄
26<br />
2012 台北榮總<strong>婦癌</strong>診療指引-卵巢癌<br />
Staging fallopian tube cancer (FIGO stage, 2009 and TNM AJCC 7th ed, 2010)<br />
Primary tumor (T)*<br />
TNM FIGO Definition<br />
Tis• Carcinoma in situ (limited to tubal mucosa)<br />
T1 I Tumor limited to the fallopian tube(s)<br />
T1a IA<br />
T1b IB<br />
T1c IC<br />
Tumor limited to one tube, without penetrating the serosal surface;<br />
no ascites<br />
Tumor limited to both tubes, without penetrating the serosal surface;<br />
no ascites<br />
Tumor limited to one or both tubes with extension onto or through the<br />
tubal serosa, or with malignant cells in ascites or peritoneal washings<br />
T2 II Tumor involves one or both fallopian tubes with pelvic extension<br />
T2a IIA Extension and/or metastasis to the uterus and/or ovaries<br />
T2b IIB Extension to other pelvic structures<br />
T2c IIC Pelvic extension with malignant cells in ascites or peritoneal washings<br />
T3 III<br />
Tumor involves one or both fallopian tubes, with peritoneal implants<br />
outside the pelvis<br />
T3a IIIA Microscopic peritoneal metastasis outside the pelvis<br />
T3b IIIB<br />
T3c IIIC<br />
Macroscopic peritoneal metastasis outside the pelvis 2 cm or less in<br />
greatest dimension<br />
Peritoneal metastasis outside the pelvis and more than 2 cm in<br />
diameter<br />
Regional lymph nodes (N)<br />
TNM FIGO Definition<br />
NX<br />
N0<br />
Regional lymph nodes cannot be assessed<br />
No regional lymph node metastasis<br />
N1 IIIC Regional lymph node metastasis<br />
Distant metastasis (M)<br />
TNM FIGO Definition<br />
M0<br />
No distant metastasis<br />
M1 IV Distant metastasis (excludes metastasis within the peritoneal cavity)<br />
Note: liver capsule metastasis is T3/Stage III;<br />
liver parenchymal metastasis,M1/ Stage IV.<br />
Pleural effusion must have positive cytology for M1/ Stage IV.<br />
返回目錄
卵巢癌治療指引<br />
27<br />
2012 台北榮總<strong>婦癌</strong>診療指引-卵巢癌<br />
(Include fallopian tube cancer and primary peritoneal cancer from 2012.01.01)<br />
I Primary Treatment<br />
- Standard treatment<br />
- Initial surgical cytoreduction followed by chemotherapy<br />
- Alternative treatment<br />
- Neodjuvant chemotherapy + interval cytoreductive surgery + adjuvant<br />
chemotherapy<br />
II Salvage Therapy<br />
- 2 nd look surgical reassessment<br />
- Extent of disease surgical reassessment<br />
- Secondary cytoreductive surgery<br />
- Intraperitoneal chemotherapy<br />
- Radiotherapy for local control<br />
III Palliative Therapy<br />
- Palliative chemotherapy<br />
- Palliative surgery<br />
- Hospice care<br />
術前準備<br />
* Stage IVb with malignant pleural effusion consider pleurodesis<br />
- Ultrasound and / or abdominal CT<br />
- Chest imaging<br />
- CBC/DC<br />
- Chemistry profile with liver and renal function tests<br />
- Institutional pathology review (if diagnosis by previous surgery or tissue biopsy)<br />
- CA-125 or other tumor markers as clinically indicated<br />
- Upper / Lower GI endoscopy if clinically indicated<br />
- Breast image survey if clinically indicated<br />
建議之減積手術<br />
- Debulking surgery<br />
- Complete staging surgery + dissection of all removable tumor<br />
- Complete staging surgery<br />
- Peritoneal cytology + Hysterectomy + BSO + BPLND + PALNS +<br />
返回目錄
28<br />
2012 台北榮總<strong>婦癌</strong>診療指引-卵巢癌<br />
Appendectomy + Infracolic omentectomy + Subdiaphragm smear + Liver surface<br />
smear<br />
- Conservative staging surgery<br />
- Peritoneal cytology + Unilateral salpingo-oophorectomy + BPLND + PALNS +<br />
Appendectomy + Infracolic omentectomy + Subdiaphragm smear + Liver surface<br />
smear<br />
* Only for Early stage (Ia & Ib) and Grade I, II<br />
* 且強烈要求保留生育能力的患者<br />
化療處方建議<br />
epithelial ovarian cancer (including tubal cancer, peritoneal cancer、MMMT) for adjuvant<br />
chemotherapy:<br />
(一) Primary Chemotherapy/Primary adjuvant therapy regimens for stage II-IV<br />
(Paclitaxel 的健保局給付規定: 只給付在 Advanced stage 如:stage III or IV、recurrent disease)<br />
1. Paclitaxel + Carboplatin or Cisplatin (stage III, IV) (q 3 w × 6 cycles)<br />
Paclitaxel (175 mg/m 2 ) IVD 3 hrs<br />
Carboplatin (AUC 5 ~7.5) or Cisplatin (75 mg/m 2 ) IVD 1 hr<br />
2. Paclitaxel + Carboplatin or Cisplatin (q 3 w × 6 cycles)<br />
+ Maintenance Paclitaxel 自費 (for clinical complete responders Individualized q m x 12 courses)<br />
Paclitaxel (175 mg/m 2 ) IVD 3 hrs on D1<br />
Carboplatin (AUC 5 ~7.5) or Cisplatin 75 mg/m 2 IVD 1 hr on D1<br />
Paclitaxel (135 mg/m 2 ) IVD 3 hrs<br />
3. Paclitaxel + Carboplatin (q 3 w × 6 cycles)<br />
+ Maintenance Bevacizumab 自費 (cycles 2~22, q 3 w, 共 21 次)<br />
Paclitaxel (175 mg/m 2 ) IVD 3 hrs on D1<br />
Carboplatin (AUC 6) IVD 1hr on D1<br />
Bevacizumab 15mg/kg<br />
4. Paclitaxel + Carboplatin (q 3 w × 6 cycles)<br />
+ Maintenance Bevacizumab 自費 (cycles 1 or 2~18, q 3 week,共 17~18 次)<br />
Paclitaxel (175 mg/m 2 ) IVD 3 hrs on D1<br />
Carboplatin (AUC 5~ 6) IVD 1 hr on D1<br />
Bevacizumab 7.5 mg/kg<br />
返回目錄
5. Paclitaxel weekly + Carboplatin (q 3 w)<br />
Paclitaxel (80 mg/m 2 ) IVD 1 hr on D1, D8, D15<br />
Carboplatin (AUC 5~ 6) IVD 1~2 hrs on D1<br />
6. Cyclophosphamide + Cisplatin (stage I, II) (q 3 w × 6 courses)<br />
Cyclophosphamide (750 mg/m 2 ) IVD 2 hrs on D1<br />
Cisplatin (75 mg/m 2 ) IVD 1 hr on D1<br />
7. Cyclophosphamide + Carboplatin (q 3 w × 6courses)<br />
Cyclophosphamide (750 mg/m 2 ) IVD 2hrs on D1<br />
Carboplatin (AUC 5~7.5) IVD 1hr on D1<br />
8. Paclitaxel over 24 hrs+ Cisplatin<br />
Paclitaxel (135 mg/m 2 ) IVD 24 hrs on D1<br />
Cisplatin (75 mg/m 2 )<br />
(二) Acceptable Recurrence Therapies<br />
1. Combination if platinum sensitive<br />
(1) Paclitaxel + Carboplatin (q 3 w × 6 cycles)<br />
Paclitaxel (175 mg/m 2 ) IVD 3 hrs on D1<br />
Carboplatin (AUC 5 ~7.5) IVD 1 hr on D1<br />
(2) Weekly paclitaxel /Carboplatin (6 cycles)<br />
Paclitaxel (80 mg/m 2 ) IVD 1 hr on D1<br />
Carboplatin (AUC 1.5) IVD 1 hr on D1<br />
(3) Docetaxel /Carboplatin<br />
Docetaxel (60 mg/m 2 ) IVD 1 hr<br />
Carboplatin (AUC 5 ~7.5) IVD 1 hr<br />
(4) Gemcitabine / Carboplatin (q 3 w × 6 cycles)<br />
Gemcitabine (1000 mg/m 2 ) IVD 30 mins on D1, D8<br />
29<br />
2012 台北榮總<strong>婦癌</strong>診療指引-卵巢癌<br />
Carboplatin (AUC 4) IVD 1 hr on D1 (或 Cisplatin 30mg/m 2 IVD 1 hr on D1, D8)<br />
(5) Liposomal doxorubicin/ Carboplatin(q 4 w × 6 cycles)<br />
Pegylated Liposomal Doxorubicin (40 mg/m 2 ) IVD 90 mins on D1<br />
Carboplatin (AUC 5) IVD 1 hr on D1 (Cisplatin 建議可用 30-50 mg/m 2 )<br />
2. Single-agent if platinum sensitive<br />
(1) Carboplatin<br />
Carboplatin (AUC 5 ~7.5)<br />
(2) Cisplatin<br />
Cisplatin (50~75 mg/m 2 )<br />
返回目錄
3. Single-agent non-platinum based if platinum resistant<br />
(1) Docetaxel (q 3 w)<br />
Docetaxel 100 mg/m 2 IVD 1 hr<br />
(2) Melphalan, oral (q 4~6 w)<br />
Melphalan 0.2 mg/kg/day × 5 days<br />
(3) Gemcitabine weekly<br />
Gemcitabine 800 mg/m 2 IVD 1 hr<br />
(4) Liposomal doxorubicin (q 4 w × 6 cycles)<br />
Liposomal Doxorubicin (40~50 mg/m 2 ) IVD 90 mins on D1<br />
(5) Paclitaxel, weekly (6 cycles)<br />
Paclitaxel (60~80 mg/m 2 ) IVD 1 hr on D1<br />
(6) Paclitaxel<br />
Paclitaxel 135 mg/m 2 IVD 3 hrs<br />
(7) Topotecan<br />
Topotecan (q 1 w on D1, D8, D15,休一周-q 28 day× 6 cycles)<br />
Topotecan (4mg/m 2 ) IVD 90 mins on D1<br />
Topotecan (q 21 day × 6 cycles)<br />
Topotecan (1.25 mg/m 2 /day) IVD 30 mins on D1~D5<br />
(三) Intraperitoneal Chemotherapy<br />
(1) Paclitaxel + Cisplatin<br />
Paclitaxel (175 mg/m 2 ) IVD 3 hrs on D1<br />
Cisplatin (100 mg/m 2 ) IP 1 hr on D1<br />
(2) Paclitaxel + Cisplatin + Paclitaxel<br />
Paclitaxel (135 mg/m 2 ) IVD 24 hrs D1<br />
Cisplatin (100 mg/m 2 ) IP 1 hr on D1<br />
Paclitaxel (60 mg/m 2 ) IP 1 hr on D8<br />
(四) Chemotherapy for non-epithelial ovarian cancer<br />
1. Germ cell tumor of the ovary<br />
(1) PE (q 3~4 w × 6 cycles)<br />
Etoposide (100 mg/m 2 ) IVD 1 hr on D1~D3<br />
Cisplatin (100 mg/m 2 ) IVD 1 hr on D1<br />
30<br />
2012 台北榮總<strong>婦癌</strong>診療指引-卵巢癌<br />
返回目錄
(2) PVB (q 3~4 w × 4~6 cycles) for immature teratoma<br />
Etoposide (100 mg/m 2 ) IVD 1 hr on D1~D3 (或 D1~D5)<br />
Cisplatin (100 mg/m 2 ) IVD 1 hr on D1 (或 20 mg/m 2 D1~D5)<br />
Bleomycin (25 mg) IVD 30 mins on D2 (或 300 mg/m 2 D2、9、16)<br />
2. Sex cord-stromal tumor of the ovary, advanced or recurrent:<br />
(1) PVB (q 3~4 w × 6 cycles)<br />
Etoposide (100 mg/m 2 ) IVD 1 hr on D1~D3<br />
Cisplatin (100 mg/m 2 ) IVD 1 hr on D1<br />
Bleomycin (25 mg) IVD 30 mins on D2<br />
(2) Paclitaxel+ Cisplatin or Carboplatin (stage III, IV)<br />
Paclitaxel (175 mg/m 2 ) IVD 3 hrs on D1<br />
Cisplatin (75 mg/m 2 ) or Carboplatin (AUC 5) IVD 1 hr on D1<br />
妊娠滋養層細胞腫瘤疾病抗癌藥物治療處方:<br />
(Chemotherapy Regimen for Gestational Trophoblastic Disease)<br />
1. MTX-single agent (low-risk GTT)<br />
Methotrexate (MTX) (1 mg/Kg) IM on D1, 3, 5, 7<br />
Folinic acid (0.1 mg/ Kg) IM on D2, 4, 6, 8<br />
2. MTX + Actinomycin-D (low-risk GTT)<br />
Methotrexate (MTX) (1 mg/Kg) IM on D1, 3, 5, 7<br />
Folinic acid (0.1 mg/ Kg) IM on D2, 4, 6, 8<br />
Actinomycin-D (1.25 mg/m 2 ) IVD 15 mins on D1 (q 2 w × 4 cycles)<br />
31<br />
2012 台北榮總<strong>婦癌</strong>診療指引-卵巢癌<br />
3. EMA/CO (medium- & high-risk GTT) (q 2 w × 4~5 cycles) (medium-risk), (q 2 weeks ×<br />
6~7 cycles) (high-risk) after undetectable hCG level<br />
Actinomycin-D (0.5 mg/m 2 ) IVD 15 mins on D1<br />
Etoposide (VP-16) (100 mg/m 2 ) IVD 1 hr on D1<br />
Methotrexate (MTX) (100 mg/m 2 IVD < 5 mins and then 200 mg/m 2 IVD 12 hr) on D1<br />
Actinomycin-D (0.5 mg/m 2 ) IVD 15 mins on D2<br />
Etoposide (VP-16) (100 mg/m 2 ) IVD 1 hr on D2<br />
Folinic acid 15mg PO q12h × 4 doses; beginning 24 hrs after start of MTX on D2<br />
Vincristine (Oncovin) (1 mg/m 2 ) IVD 10 mins on D8<br />
Cyclophosphamide (endoxan) (600 mg/m 2 ) IVD 10 mins on D8<br />
** Carboplatin 的健保局使用規定 : 限 Ccr < 60 cc/min<br />
返回目錄
完整或保守的分期手術後治療策略<br />
Stage Management<br />
Stage IA or IB<br />
Stage Ic<br />
Stage II, III, IV<br />
32<br />
2012 台北榮總<strong>婦癌</strong>診療指引-卵巢癌<br />
Grade 1 Observation and follow-up.<br />
Grade 2<br />
Grade 3<br />
* Treat clear cell type pathology as grade III<br />
Observation<br />
or<br />
Intravenous chemotherapy for 3-6 cycles and<br />
then close follow-up<br />
Intravenous chemotherapy for 6 cycles<br />
and then close follow-up.<br />
Intravenous chemotherapy for 6 cycles<br />
and then close follow-up.<br />
Intravenous Paclitaxel/Carboplatin for a total of 6-8 cycles<br />
or<br />
Intraperitoneal chemotherapy [Optimally debulked (< 1 cm)]<br />
返回目錄
不完整分期手術後意外發現<br />
Reassessment with appropriate evaluation:<br />
Suspicion Management<br />
Stage IA or IB<br />
Grade 1<br />
Stage IA or IB<br />
Grade 2 or 3<br />
Stage IC<br />
Stage II, III, IV<br />
Residual Tumor<br />
(-)<br />
Residual Tumor<br />
(+)<br />
Resectable<br />
residual tumor<br />
Unresectable<br />
residual tumor<br />
33<br />
2012 台北榮總<strong>婦癌</strong>診療指引-卵巢癌<br />
Surgical staging procedure<br />
Chemotherapy for 6 cycles<br />
or<br />
Surgical staging procedure<br />
Surgical staging procedure<br />
Debulking surgery<br />
Chemotherapy for a total of 6-8 cycles.<br />
or<br />
Neoadjuvant chemotherapy for 3 cycles<br />
followed by surgical staging procedure<br />
and postoperative chemotherapy<br />
* Arrange treatment plan as recommended by guideline after complete staging surgery and<br />
determining final disease stage (see above)<br />
返回目錄
追蹤<br />
- 門診追蹤<br />
第一年每 2 個月 1 次<br />
第二年每 3 個月 1 次<br />
此後每 6 個月追蹤 1 次<br />
- 追蹤建議<br />
34<br />
2012 台北榮總<strong>婦癌</strong>診療指引-卵巢癌<br />
若 CA-125 或其他腫瘤指數一開始即高於正常值,建議每次追蹤依個人狀況若有臨床<br />
需求可行抽血(CBC 或其他功能)、身體檢查如骨盆腔檢查,依臨床徵象需要可行影像<br />
檢查如:Chest / Abdominal / Pelvic CT, MRI, PET-CT, PET or Chest x-ray。<br />
臨床完全緩解<br />
- Observe<br />
- Maintenance chemotherapy with paclitaxel 135-175mg/m2 every 4 weeks for 12 cycles<br />
- Clinical trial<br />
持續性或復發疾病<br />
評估疾病的程度和進展<br />
- Clinical symptoms and signs<br />
- Imaging studies<br />
- Chest / Abdominal / Pelvic CT, MRI or PET as clinically indicated.<br />
- Tumor marker level<br />
停止化療後完全緩解,但 6 個月疑似復發情形。<br />
Consider secondary cytoreductive surgery / PET scan followed by chemotherapy (可同<br />
first line C/T regimen;或 platinum-based + 非 paclitaxel 類 agent;或<br />
non-platinum-based agent)<br />
Consider secondary cytoreductive surgery followed by clinical trial<br />
停止化療後完全緩解,但 >12 個月內復發<br />
Consider secondary cytoreductive surgery followed by platinum-based combination<br />
chemotherapy (同 first line C/T regimen)<br />
Consider secondary cytoreductive surgery followed by clinical trial<br />
無臨床復發,但 CA-125 上升<br />
Delay treatment until clinical relapse<br />
Immediate treatment as recurrent disease<br />
返回目錄
I Primary Treatment<br />
- Standard treatment<br />
II Chemotherapy<br />
- Surgical cytoreduction<br />
- No recommendations / Individualized<br />
III Salvage Therapy<br />
- 2 nd look surgical reassessment<br />
- Extent of disease surgical reassessment<br />
- Secondary cytoreductive surgery<br />
- Whole abdominal radiation (WAR)<br />
IV Palliative Therapy<br />
- Palliative chemotherapy<br />
- Palliative surgery<br />
- Hospice care<br />
術前準備<br />
- Ultrasound and /or abdominal CT<br />
- Chest imaging<br />
- CBC/DC<br />
低惡性度卵巢癌診療指引<br />
- Chemistry profile with liver and renal function tests<br />
35<br />
2012 台北榮總<strong>婦癌</strong>診療指引-低惡性度卵巢癌<br />
- Institutional pathology review (if diagnosis by previous surgery or tissue biopsy)<br />
- CA-125 or other tumor markers as clinically indicated<br />
- Upper/Lower GI endoscopy if clinically indicated<br />
建議之減積手術<br />
- Debulking surgery<br />
- Complete staging surgery + dissection of all removable tumor<br />
- Complete staging surgery<br />
- Peritoneal cytology + Hysterectomy +BSO+ BPLND + PALNS + Appendectomy +<br />
Infracolic omentectomy + Subdiaphragm smear + Liver surface smear<br />
返回目錄
- Conservative staging surgery<br />
36<br />
2012 台北榮總<strong>婦癌</strong>診療指引-低惡性度卵巢癌<br />
- Peritoneal cytology + Unilateral salpingo-oophorectomy + BPLND + PALNS +<br />
Appendectomy + Infracolic omentectomy + Subdiaphragm smear + Liver surface<br />
smear<br />
* Only for Early stage (Ia & Ib)<br />
* 且強烈要求保留生育能力的患者<br />
Stage I-IV<br />
- After completion of surgical staging, regular out-patient follow up is suggested<br />
- Chemotherapy is not recommended<br />
Recurrent Disease<br />
- Consider secondary cytoreductive surgery then arrange regular follow up.<br />
返回目錄
37<br />
2012 台北榮總<strong>婦癌</strong>診療指引-化療的毒性<br />
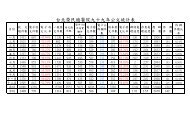
化療的毒性 (引用自中華民國<strong>婦癌</strong>醫學雜誌 – 顏明賢主任編著)<br />
化療藥物是醫師治病中最具毒性的處方,不管劑量、療程、給藥方式,都是相當<br />
重要。嚴重時,即使正確使用藥物、劑量、與適當的療程,仍有 1-3%的病人,因其<br />
藥物毒性或併發症造成病人死亡,不可不慎!<br />
返回目錄
38<br />
2012 台北榮總<strong>婦癌</strong>診療指引-化療的毒性<br />
返回目錄
39<br />
2012 台北榮總<strong>婦癌</strong>診療指引-化療的毒性<br />
返回目錄
40<br />
2012 台北榮總<strong>婦癌</strong>診療指引-化療的毒性<br />
返回目錄
41<br />
2012 台北榮總<strong>婦癌</strong>診療指引-化療的毒性<br />
返回目錄
42<br />
2012 台北榮總<strong>婦癌</strong>診療指引-參考資料<br />
參考資料<br />
1. <strong>婦癌</strong>研究委員會(2011.06)‧<strong>婦癌</strong>臨床診療指引‧苗栗:國家衛生研究院。<br />
2. NCCN Clinical Practice Guidelines in OncologyTM Cancer Cancer (version 1. 2012 ).2012 National<br />
Comprehensive Cancer Network,Inc.<br />
3. NCCN Clinical Practice Guidelines in OncologyTM Uterine Neoplasms (version 3. 2012 ).2012 National<br />
Comprehensive Cancer Network,Inc.<br />
4. NCCN Clinical Practice Guidelines in OncologyTM Ovarian Cancer (version 3. 2012 ).2012 National<br />
Comprehensive Cancer Network,Inc<br />
5. GLOBOCAN 2000: Cancer Incidence, Mortality and Prevalence Worldwide. World Health Organization.<br />
2004.<br />
6. Cervical Cancer, in National Comprehensive Cancer Network ( NCCN) Clinical Practice Guidelines in<br />
Oncology, v.1. 2006. http://www.nccn.org.<br />
7. Benedet JL, Bender H, Jones H, III, et al. FIGO staging classifications and clinical practice guidelines in<br />
the management of gynecologic cancers. FIGO Committee on Gynecologic Oncology. International<br />
Journal of Gynecology & Obstetrics 2000; 70:209-262<br />
8. Cervical Cancer (PDQR): Treatment, Health Professional Version. National Cancer Institute. 2003.<br />
9. Resbeut M, Fondrinier E, Fervers B, et al. Standards, Options and Recommendations for the management<br />
of invasive cervical cancer patients ( non metastatic). Bulletin du Cancer 2003;90:333-346<br />
10. Resbeut M, Fondrinier E, Fervers B, et al. Carcinoma of the cervix. Br. J. Cancer 2001;84 Suppl 2:24-30.<br />
11. Landoni F, Maneo A, Colombo A, et al. Randomised study of radical surgery versus radiotherapy for<br />
stage Ib-II2 cervical cancer. Lancet 1997; 350:535-540.<br />
12. Chang TC, Lai CH, Hong JH, et al. Randomized trial of neoadjuvant cisplatin vincrinstine, bleomycin,<br />
and radical hysterectomy versus radiation therapy for bulky stage IB and IIa cervical cancer. J. Clin.<br />
Oncol. 2000. Apr; 18(8): 1740-1747.<br />
13. Neoadjuvant chemotherapy for locally advanced cervical cancer: a systemic review and meta-analysis of<br />
individual patient data from 21 randomised trials. European Journal of Cancer 2003; 39:2470-2486.<br />
14. Whitney CW, Sause W, Bundy BN, et al. Randomized comparison of fluorouracil plus cisplatin versus<br />
hydroxyurea as an adjunct to radiation therapy in stage IIb- IVa carcinoma of the cervix with negative<br />
para-aortic lymph nodes: a Gynecologic Oncology Group and Southwest Oncology Group study. J. Clin.<br />
Oncol. 1999; 17: 1339-1348.<br />
15. Keys HM, Bundy Bn, Stehman FB, et al. Cisplatin, radiation, and adjuvant hysterectomy compared with<br />
radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. N. Engl. J. Med. 1999; 340:<br />
1154-1161.<br />
16. Morris M, Eifel PJ, Lu J, et al. Pelvic radiation with concurrent chemotherapy compared with pelvic and<br />
para-aortic radiation for high risk cervical cancer, N. Engl. J. Med, 1999; 340: 1137-1143.<br />
17. Rose PG, Bundy Bn, Watkins EB, et al. Concurrent cisplatin-based radiotherapy and chemotherapy for<br />
locally advanced cervical cancer. N. Engl. J. Med. 1999; 340:1144-1153<br />
18. Green JA, Kirwan JM, Tierney JF, et al. Survival and recurrence after concomitant chemotherapy and<br />
radiotherapy for cancer of the uterine cervix: a ystematic review and meta-analysis. Lancet 2001; 358:
781-786.<br />
43<br />
2012 台北榮總<strong>婦癌</strong>診療指引-參考資料<br />
19. Neoadjuvant chemotherapy for locally advanced cervical cancer: a systemic review and meta-analysis of<br />
individual patient data from 21 randomized trials. European Journal of Cancer 2003; 39: 2470-2486.<br />
20. Lai CH, Juang KG, Hong JH, et al. Randomized trial of surgical staging( extraperitoneal or laparoscopic)<br />
versus clinical staging in locally advanced cervical cancer. Gynecol. Oncol. 2003;89: 160-167.<br />
21. Haie C, Pejovic MH, Gerbaulet A, et al. Is prophylactic para-aortic irradiation worthwhile in the treatment<br />
of advanced cervical carcinoma? Results of a controlled clinical trial of the EORTC radiotherapy group.<br />
Radiother. Oncol. 1988;11:101-112.<br />
22. Rotman M, Pajak TF, Choi K, et al. Prophylactic extended-field irradiation of para-aortic lymph nodes in<br />
stages IIb and bulky Ib and IIa cervical carcinomas. Ten-year treatment results of RTOG 79-20, JAMA<br />
1995; 274: 387-393.<br />
23. Peters WA, Lui PY, Barrett RJ, et al. Concurrent chemotherapy and pelvic radiation therapy compared<br />
with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage<br />
cancer of the cervix. J. Clin. Oncol. 2000; Apr; 18(8): 1606-1613.<br />
24. Sedlis A, Bundy BN, Rotman MZ, et al. A randomized trial of pelvic radiation therapy versus no further<br />
therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic<br />
lymphadenectomy: A Gynecologic Oncology Group Study. Gynecol. Oncol. 1999;73: 177-183.<br />
25. Bloss JD, Blessing JA, Behrens BC. et al. Randomized trial of cisplatin and ifosfamide with or without<br />
bleomycin in squamous cell carcinoma of cervix: A Gynecologic Oncology Group Study. J. Clin. Oncol.<br />
2002; 20(7): 1832-1837.<br />
26. Moore DH, Blessing JA, McQuellon RP, et al. Phase III study of cisplatin with or without paclitaxel in<br />
stage IVB, recurrent, or persistent squamous cell carcinoma of the cervix: A Gynecologic Oncology<br />
Group Study. J. Clin. Oncol. 2004; 22(15): 3113-3119.<br />
27. Long III HJ, Bundy BN, Grendys Jr EC, et al. Randomized phase III trial of cisplatin with or without<br />
topotecan in carcinoma of the uterine cervix. A Gynecologic Oncology Group Study. J. Clin. Oncol.<br />
2005;23(21): 4626-4633.<br />
28. Eifel PJ, Burke TW, Morris M, Smith TL. Adenocarcinoma as an independent riskfactor for disease<br />
recurrence in patients with stage 1B cervical carcinoma. GynecolOncol 1995;59:38–44.<br />
29. Sedlis A, Bundy BN, RotmanMZ, Lentz SS,Muderspach LI, Zaino RJ.A randomized trial of pelvic radiation<br />
therapy versus no further therapy in selected patients with stage1b carcinoma of the cervix after radical<br />
hysterectomy and pelvic lymphadenectomy:a Gynecologic Oncology Group study. Gynecol Oncol<br />
1999;73:177–83.<br />
30. del Campo JM, Prat A, Gil-Moreno A, Perez J, Parera M. Update on noveltherapeutic agents for cervical<br />
cancer. Gynecol Oncol 2008;110:S72–6.<br />
31. Monk BJ, Wang J, Im S, Stock RJ, Peters WA, Liu PY, et al. Rethinking the use ofradiation and<br />
chemotherapy after radical hysterectomy: a clinical–pathologicanalysis of a Gynecologic Oncology<br />
Group/Southwest Oncology Group/RadiationTherapy Oncology Group trial. Gynecol Oncol 2005;96:721–8.<br />
32. Kurtz JE, Hardy-Bessard AC, Deslandres M, Lavau-Denis S, Largillier R, Roemer-Becuwe C, et al.<br />
Cetuximab, topotecan and cisplatin for the treatment of advancedcervical cancer: a phase II GINECO trial.
Gynecol Oncol 2009;113:16–20.<br />
44<br />
2012 台北榮總<strong>婦癌</strong>診療指引-參考資料<br />
33. Gien LT, Beauchemin MC, Thomas G. Adenocarcinoma: Aunique cervicqal cancer. Gynecol Oncol<br />
2010 ;116 :140-6.<br />
34. Takeshima N, Hirai Y, Tanaka N, et al. Pelvic lymph node metastasis in endometrial cancer with no<br />
myometrial invasion. Obstet Gynecol. 1996 Aug;88(2):280-282.<br />
35. Cirisano FD Jr, Robboy SJ, Dodge RK, et al. The outcome of stage I-II clinically and surgically staged<br />
papillaryserous and clear cell endometrial cancers when compared with endometrial carcinoma. Gynecol<br />
Oncol. 2000 Apr;77(1):55-65.<br />
36. Gehrig PA, Groben PA, Fowler WC Jr, et al. Noninvasive papillary serous carcinoma of the endometrium.<br />
Obstet Gynecol. 2001 Jan;97(1):153-157.<br />
37. Straughn JM Jr, Huh WK, Kelly FJ,et al. Conservative management of stage I endometrial carcinoma after<br />
surgical staging. Gynecol Oncol 2002; 84:194-200.<br />
38. Ayhan A, Taskiran C, Celik C, et al. Is there a survival benefit to adjuvant radiotherapy in high-risk surgical<br />
stage I endometrial cancer? Gynecol Oncol 2002;86:259-63.<br />
39. Lewin S, Herzog T, Barrena Medel N, et al: Comparative performance of the new versus old FIGO staging<br />
system for endometrial cancer. Gynecol Oncol 2010;116:S6-7,.<br />
40. Hahn HS, Yoon SG, Hong JS, et al. Conservative treatment with progestin and pregnancy outcomes in<br />
endometrial cancer. Int J Gynecol Cancer. 2009 Aug;19(6):1068-73.<br />
41. Tangjitgamol S, Manusirivithaya S, Hanprasertpong J. Fertility-sparing in endometrial cancer. Gynecol<br />
Obstet Invest. 2009;67(4):250-68.<br />
42. Gurgan T, Bozdag G, Demirol A, Ayhan A. Preserving fertility before assisted reproduction in women with<br />
endometrial carcinoma: case report and literature review. Reprod Biomed Online. 2007 Nov;15(5):561-5.<br />
43. Levgur M. Estrogen and combined hormone therapy for women after genital malignancies: a review. J<br />
Reprod Med. 2004 Oct;49(10):837-48.<br />
44. FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. Int<br />
J Gynecol Obstet 2000; 70:209-262.<br />
45. Standards, Options and Recommendations. Clinical practice guidelines for cancer care from the French<br />
National Federation of Cancer (FNCLCC). Ovarian cancer. Bri J Cancer 2001; 84(Suppl 2):18-23.<br />
46. Ozols RF, Rubin SC, Thomas G, et al. Epithelial ovarian cancer, in Hoskins WJ, Perez CA, Young RC (eds):<br />
Principles and Practice of Gynecologic Oncology, 2nd ed, chap 32, pp 939-941. Philadelphia, Lippincott<br />
Williams & Wilkins, 1997.<br />
47. Omura GA, Brady MF, Homesley HD, et al. Long-term follow-up and prognostic factor analysis in<br />
advanced ovarian carcinoma: the Gynecologic Oncology Group experience. J Clin Oncol 1991;<br />
9:1138-1150.<br />
48. van Houwelingen JC, ten Bokkel Huinink WW, van der Burg ME, et al. Predictability of the survival of<br />
patients with advanced ovarian cancer. J Clin Oncol 1989; 7:769-773.<br />
49. Thigpen T, Brady MF, Omura GA, et al. Age as a prognostic factor in ovarian carcinoma. The Gynecologic<br />
Oncology Group experience. Cancer 1993; 71(2 Suppl): 606-614.<br />
50. Bristow RE, Karlan BY. Ovulation induction, infertility, and ovarian cancer risk. Fertil Steril 1996;
66:499-507.<br />
45<br />
2012 台北榮總<strong>婦癌</strong>診療指引-參考資料<br />
51. Rossing MA, Daling JR, Weiss NS, et al. Ovarian tumors in a cohort of infertile women. N Engl J Med<br />
1994; 331:771-776.<br />
52. Lynch HT, Watson P, Lynch JF, et al. Hereditary ovarian cancer. Heterogeneity in age at onset. Cancer<br />
1993; 71(2 Suppl): 573-581.<br />
53. Statement of the American Society of Clinical Oncology: genetic testing for cancer susceptibility, Adopted<br />
on February 20, 1996. J Clin Oncol 1996; 14:1730-1736.<br />
54. Frank TS, Deffenbaugh AM, Reid JE, et al. Clinical characteristics of individuals with germline mutations<br />
in BRCA1 and BRCA2: analysis of 10,000 individuals. J Clin Oncol 2002; 20:1480-1490.<br />
55. Narod SA, Risch H, Moslehi R, et al. Oral contraceptives and the risk of hereditary ovarian cancer.<br />
Hereditary Ovarian Cancer Clinical Study Group. N Engl J Med 1998; 339:424-428.<br />
56. Rebbeck TR, Lynch HT, Neuhausen SL, et al. The Prevention and Observation of Surgical End Points Study<br />
Group. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med 2002;<br />
346:1616-1622.<br />
57. Kauff ND, Satagopan JM, Robson ME, et al. Risk-reducing salpingo-oophorectomy in women with a<br />
BRCA1 or BRCA2 mutation. N Engl J Med 2002; 346:1609-1615.<br />
58. Haber D. Prophylactic oophorectomy to reduce the risk of ovarian and breast cancer in carriers of BRCA<br />
mutations. N Engl J Med 2002; 346:1660-1662.<br />
59. Shepherd JH. Revised FIGO staging for gynaecological cancer. Br J Obstet Gynaecol 1989; 96:889-892.<br />
60. McGuire WP, Hoskins WJ, Brady MF, et al. Cyclophosphamide and cisplatin compared with paclitaxel and<br />
cisplatin in patients with stage III and stage IV ovarian cancer. N Engl J Med 1996; 334:1-6.