The Anesthetic Management of Triplet Cesarean Delivery: A ...
The Anesthetic Management of Triplet Cesarean Delivery: A ...
The Anesthetic Management of Triplet Cesarean Delivery: A ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
ANESTH ANALG OBSTETRIC ANESTHESIA MARINO ET AL. 993<br />
2001;93:991–5 ANESTHESIA FOR TRIPLETS<br />
Table 1. Indications for <strong>Cesarean</strong> <strong>Delivery</strong><br />
Indication Spinal (n 71) Epidural (n 20) General (n 5)<br />
Preterm labor 33 (47.8) 11 (55) 0<br />
Premature rupture <strong>of</strong> membranes 8 (11.3) 3 (15) 0<br />
Preeclampsia 13 (18.3) 4 (20) 0<br />
Preeclampsia with coagulopathy 0 0 2 (40)<br />
Acute fatty liver 3 (4.2) 0 1 (20)<br />
Term gestation a<br />
7 (9.9) 2 (10) 0<br />
Nonreassuring fetal HR tracing 6 (8.5) 0 2 (40)<br />
Data are presented as n (%).<br />
HR heart rate.<br />
a Patients delivered at 37 wk gestation.<br />
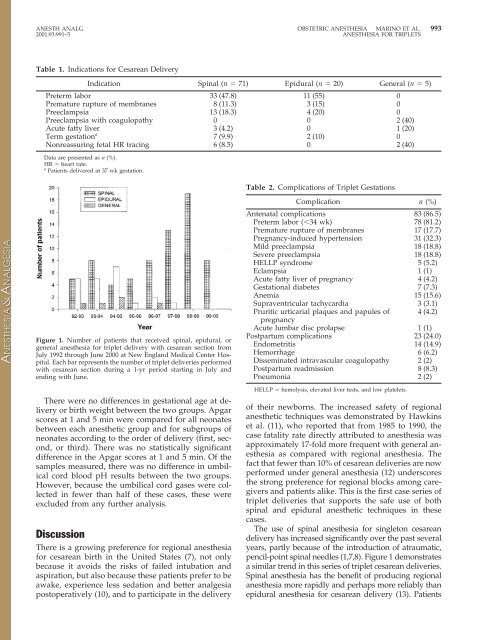
Figure 1. Number <strong>of</strong> patients that received spinal, epidural, or<br />
general anesthesia for triplet delivery with cesarean section from<br />
July 1992 through June 2000 at New England Medical Center Hospital.<br />
Each bar represents the number <strong>of</strong> triplet deliveries performed<br />
with cesarean section during a 1-yr period starting in July and<br />
ending with June.<br />
<strong>The</strong>re were no differences in gestational age at delivery<br />
or birth weight between the two groups. Apgar<br />
scores at 1 and 5 min were compared for all neonates<br />
between each anesthetic group and for subgroups <strong>of</strong><br />
neonates according to the order <strong>of</strong> delivery (first, second,<br />
or third). <strong>The</strong>re was no statistically significant<br />
difference in the Apgar scores at 1 and 5 min. Of the<br />
samples measured, there was no difference in umbilical<br />
cord blood pH results between the two groups.<br />
However, because the umbilical cord gases were collected<br />
in fewer than half <strong>of</strong> these cases, these were<br />
excluded from any further analysis.<br />
Discussion<br />
<strong>The</strong>re is a growing preference for regional anesthesia<br />
for cesarean birth in the United States (7), not only<br />
because it avoids the risks <strong>of</strong> failed intubation and<br />
aspiration, but also because these patients prefer to be<br />
awake, experience less sedation and better analgesia<br />
postoperatively (10), and to participate in the delivery<br />
Table 2. Complications <strong>of</strong> <strong>Triplet</strong> Gestations<br />
Complication n (%)<br />
Antenatal complications 83 (86.5)<br />
Preterm labor (34 wk) 78 (81.2)<br />
Premature rupture <strong>of</strong> membranes 17 (17.7)<br />
Pregnancy-induced hypertension 31 (32.3)<br />
Mild preeclampsia 18 (18.8)<br />
Severe preeclampsia 18 (18.8)<br />
HELLP syndrome 5 (5.2)<br />
Eclampsia 1 (1)<br />
Acute fatty liver <strong>of</strong> pregnancy 4 (4.2)<br />
Gestational diabetes 7 (7.3)<br />
Anemia 15 (15.6)<br />
Supraventricular tachycardia 3 (3.1)<br />
Pruritic urticarial plaques and papules <strong>of</strong><br />
pregnancy<br />
4 (4.2)<br />
Acute lumbar disc prolapse 1 (1)<br />
Postpartum complications 23 (24.0)<br />
Endometritis 14 (14.9)<br />
Hemorrhage 6 (6.2)<br />
Disseminated intravascular coagulopathy 2 (2)<br />
Postpartum readmission 8 (8.3)<br />
Pneumonia 2 (2)<br />
HELLP hemolysis, elevated liver tests, and low platelets.<br />
<strong>of</strong> their newborns. <strong>The</strong> increased safety <strong>of</strong> regional<br />
anesthetic techniques was demonstrated by Hawkins<br />
et al. (11), who reported that from 1985 to 1990, the<br />
case fatality rate directly attributed to anesthesia was<br />
approximately 17-fold more frequent with general anesthesia<br />
as compared with regional anesthesia. <strong>The</strong><br />
fact that fewer than 10% <strong>of</strong> cesarean deliveries are now<br />
performed under general anesthesia (12) underscores<br />
the strong preference for regional blocks among caregivers<br />
and patients alike. This is the first case series <strong>of</strong><br />
triplet deliveries that supports the safe use <strong>of</strong> both<br />
spinal and epidural anesthetic techniques in these<br />
cases.<br />
<strong>The</strong> use <strong>of</strong> spinal anesthesia for singleton cesarean<br />
delivery has increased significantly over the past several<br />
years, partly because <strong>of</strong> the introduction <strong>of</strong> atraumatic,<br />
pencil-point spinal needles (1,7,8). Figure 1 demonstrates<br />
a similar trend in this series <strong>of</strong> triplet cesarean deliveries.<br />
Spinal anesthesia has the benefit <strong>of</strong> producing regional<br />
anesthesia more rapidly and perhaps more reliably than<br />
epidural anesthesia for cesarean delivery (13). Patients