The Anesthetic Management of Triplet Cesarean Delivery: A ...
The Anesthetic Management of Triplet Cesarean Delivery: A ...
The Anesthetic Management of Triplet Cesarean Delivery: A ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
994 OBSTETRIC ANESTHESIA MARINO ET AL. ANESTH ANALG<br />
ANESTHESIA FOR TRIPLETS 2001;93:991–5<br />
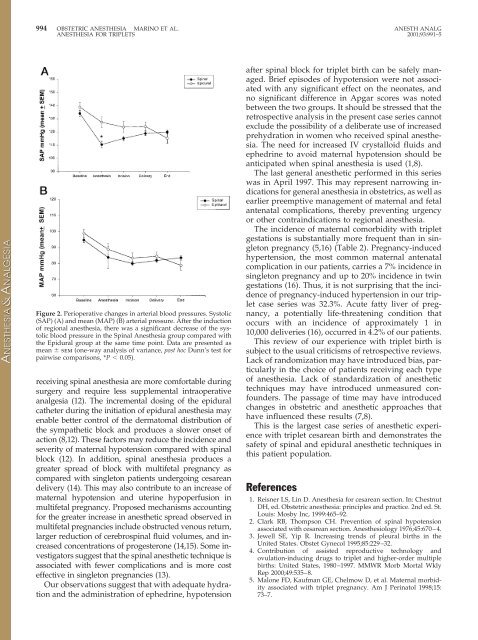
Figure 2. Perioperative changes in arterial blood pressures. Systolic<br />
(SAP) (A) and mean (MAP) (B) arterial pressure. After the induction<br />
<strong>of</strong> regional anesthesia, there was a significant decrease <strong>of</strong> the systolic<br />
blood pressure in the Spinal Anesthesia group compared with<br />
the Epidural group at the same time point. Data are presented as<br />
mean sem (one-way analysis <strong>of</strong> variance, post hoc Dunn’s test for<br />
pairwise comparisons, *P 0.05).<br />
receiving spinal anesthesia are more comfortable during<br />
surgery and require less supplemental intraoperative<br />
analgesia (12). <strong>The</strong> incremental dosing <strong>of</strong> the epidural<br />
catheter during the initiation <strong>of</strong> epidural anesthesia may<br />
enable better control <strong>of</strong> the dermatomal distribution <strong>of</strong><br />
the sympathetic block and produces a slower onset <strong>of</strong><br />
action (8,12). <strong>The</strong>se factors may reduce the incidence and<br />
severity <strong>of</strong> maternal hypotension compared with spinal<br />
block (12). In addition, spinal anesthesia produces a<br />
greater spread <strong>of</strong> block with multifetal pregnancy as<br />
compared with singleton patients undergoing cesarean<br />
delivery (14). This may also contribute to an increase <strong>of</strong><br />
maternal hypotension and uterine hypoperfusion in<br />
multifetal pregnancy. Proposed mechanisms accounting<br />
for the greater increase in anesthetic spread observed in<br />
multifetal pregnancies include obstructed venous return,<br />
larger reduction <strong>of</strong> cerebrospinal fluid volumes, and increased<br />
concentrations <strong>of</strong> progesterone (14,15). Some investigators<br />
suggest that the spinal anesthetic technique is<br />
associated with fewer complications and is more cost<br />
effective in singleton pregnancies (13).<br />
Our observations suggest that with adequate hydration<br />
and the administration <strong>of</strong> ephedrine, hypotension<br />
after spinal block for triplet birth can be safely managed.<br />
Brief episodes <strong>of</strong> hypotension were not associated<br />
with any significant effect on the neonates, and<br />
no significant difference in Apgar scores was noted<br />
between the two groups. It should be stressed that the<br />
retrospective analysis in the present case series cannot<br />
exclude the possibility <strong>of</strong> a deliberate use <strong>of</strong> increased<br />
prehydration in women who received spinal anesthesia.<br />
<strong>The</strong> need for increased IV crystalloid fluids and<br />
ephedrine to avoid maternal hypotension should be<br />
anticipated when spinal anesthesia is used (1,8).<br />
<strong>The</strong> last general anesthetic performed in this series<br />
was in April 1997. This may represent narrowing indications<br />
for general anesthesia in obstetrics, as well as<br />
earlier preemptive management <strong>of</strong> maternal and fetal<br />
antenatal complications, thereby preventing urgency<br />
or other contraindications to regional anesthesia.<br />
<strong>The</strong> incidence <strong>of</strong> maternal comorbidity with triplet<br />
gestations is substantially more frequent than in singleton<br />
pregnancy (5,16) (Table 2). Pregnancy-induced<br />
hypertension, the most common maternal antenatal<br />
complication in our patients, carries a 7% incidence in<br />
singleton pregnancy and up to 20% incidence in twin<br />
gestations (16). Thus, it is not surprising that the incidence<br />
<strong>of</strong> pregnancy-induced hypertension in our triplet<br />
case series was 32.3%. Acute fatty liver <strong>of</strong> pregnancy,<br />
a potentially life-threatening condition that<br />
occurs with an incidence <strong>of</strong> approximately 1 in<br />
10,000 deliveries (16), occurred in 4.2% <strong>of</strong> our patients.<br />
This review <strong>of</strong> our experience with triplet birth is<br />
subject to the usual criticisms <strong>of</strong> retrospective reviews.<br />
Lack <strong>of</strong> randomization may have introduced bias, particularly<br />
in the choice <strong>of</strong> patients receiving each type<br />
<strong>of</strong> anesthesia. Lack <strong>of</strong> standardization <strong>of</strong> anesthetic<br />
techniques may have introduced unmeasured confounders.<br />
<strong>The</strong> passage <strong>of</strong> time may have introduced<br />
changes in obstetric and anesthetic approaches that<br />
have influenced these results (7,8).<br />
This is the largest case series <strong>of</strong> anesthetic experience<br />
with triplet cesarean birth and demonstrates the<br />
safety <strong>of</strong> spinal and epidural anesthetic techniques in<br />
this patient population.<br />
References<br />
1. Reisner LS, Lin D. Anesthesia for cesarean section. In: Chestnut<br />
DH, ed. Obstetric anesthesia: principles and practice. 2nd ed. St.<br />
Louis: Mosby Inc, 1999:465–92.<br />
2. Clark RB, Thompson CH. Prevention <strong>of</strong> spinal hypotension<br />
associated with cesarean section. Anesthesiology 1976;45:670–4.<br />
3. Jewell SE, Yip R. Increasing trends <strong>of</strong> pleural births in the<br />
United States. Obstet Gynecol 1995;85:229–32.<br />
4. Contribution <strong>of</strong> assisted reproductive technology and<br />
ovulation-inducing drugs to triplet and higher-order multiple<br />
births: United States, 1980–1997. MMWR Morb Mortal Wkly<br />
Rep 2000;49:535–8.<br />
5. Malone FD, Kaufman GE, Chelmow D, et al. Maternal morbidity<br />
associated with triplet pregnancy. Am J Perinatol 1998;15:<br />
73–7.