Large Intestine (Colon) - Axon
Large Intestine (Colon) - Axon
Large Intestine (Colon) - Axon
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
n Gastrointestinal Tract<br />
The proximal colon to the splenic flexure derives its<br />
blood supply from the superior mesenteric artery through<br />
the ileocolic, right colic, and middle colic branches. The<br />
remainder of the colon is supplied by the left colic and<br />
sigmoid branches of the inferior mesenteric artery. The inferior<br />
mesenteric artery and iliac vessels provide blood to the<br />
rectum. Veins accompany the arteries and share their names.<br />
The large bowel venous drainage enters the portal circulation<br />
except for the distal rectum, which drains into the<br />
systemic circulation through the middle and inferior rectal<br />
veins. In portal hypertension, this area can serve as a portalsystemic<br />
shunt and can be a site of varices. The lymph node<br />
drainage is divided into those lymph nodes close to the<br />
bowel wall (e.g., pericolic, perirectal) and those that follow<br />
the blood vessels (e.g., mesenteric).<br />
The vagus nerves supply stimulatory nervous activity to<br />
the ascending colon and proximal transverse colon. The<br />
remainder of the large bowel is supplied by pelvic postganglionic<br />
parasympathetic nerves. The inhibitory nervous<br />
activity is derived from the superior and inferior mesenteric<br />
plexuses.<br />
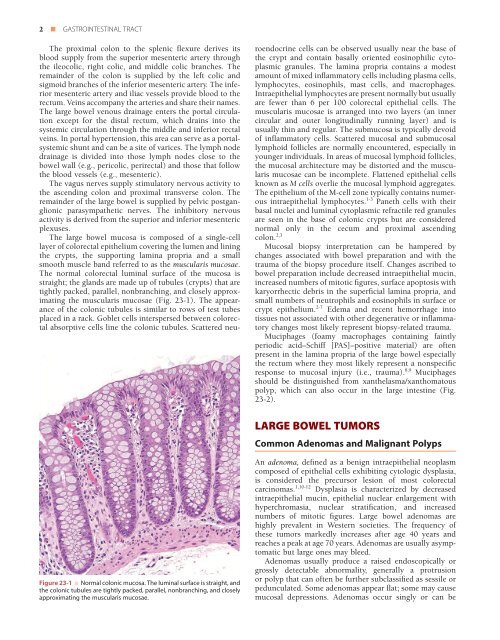
The large bowel mucosa is composed of a single-cell<br />
layer of colorectal epithelium covering the lumen and lining<br />
the crypts, the supporting lamina propria and a small<br />
smooth muscle band referred to as the muscularis mucosae.<br />
The normal colorectal luminal surface of the mucosa is<br />
straight; the glands are made up of tubules (crypts) that are<br />
tightly packed, parallel, nonbranching, and closely approximating<br />
the muscularis mucosae (Fig. 23-1). The appearance<br />
of the colonic tubules is similar to rows of test tubes<br />
placed in a rack. Goblet cells interspersed between colorectal<br />
absorptive cells line the colonic tubules. Scattered neuroendocrine<br />
cells can be observed usually near the base of<br />
the crypt and contain basally oriented eosinophilic cytoplasmic<br />
granules. The lamina propria contains a modest<br />
amount of mixed inflammatory cells including plasma cells,<br />
lymphocytes, eosinophils, mast cells, and macrophages.<br />
Intraepithelial lymphocytes are present normally but usually<br />
are fewer than 6 per 100 colorectal epithelial cells. The<br />
muscularis mucosae is arranged into two layers (an inner<br />
circular and outer longitudinally running layer) and is<br />
usually thin and regular. The submucosa is typically devoid<br />
of inflammatory cells. Scattered mucosal and submucosal<br />
lymphoid follicles are normally encountered, especially in<br />
younger individuals. In areas of mucosal lymphoid follicles,<br />
the mucosal architecture may be distorted and the muscularis<br />
mucosae can be incomplete. Flattened epithelial cells<br />
known as M cells overlie the mucosal lymphoid aggregates.<br />
The epithelium of the M-cell zone typically contains numerous<br />
intraepithelial lymphocytes. 1-3 Paneth cells with their<br />
basal nuclei and luminal cytoplasmic refractile red granules<br />
are seen in the base of colonic crypts but are considered<br />
normal only in the cecum and proximal ascending<br />
colon. 2,3<br />
Mucosal biopsy interpretation can be hampered by<br />
changes associated with bowel preparation and with the<br />
trauma of the biopsy procedure itself. Changes ascribed to<br />
bowel preparation include decreased intraepithelial mucin,<br />
increased numbers of mitotic figures, surface apoptosis with<br />
karyorrhectic debris in the superficial lamina propria, and<br />
small numbers of neutrophils and eosinophils in surface or<br />
crypt epithelium. 2-7 Edema and recent hemorrhage into<br />
tissues not associated with other degenerative or inflammatory<br />
changes most likely represent biopsy-related trauma.<br />
Muciphages (foamy macrophages containing faintly<br />
periodic acid–Schiff [PAS]–positive material) are often<br />
present in the lamina propria of the large bowel especially<br />
the rectum where they most likely represent a nonspecific<br />
response to mucosal injury (i.e., trauma). 8,9 Muciphages<br />
should be distinguished from xanthelasma/xanthomatous<br />
polyp, which can also occur in the large intestine (Fig.<br />
23-2).<br />
LARGE BOWEL TUMORS<br />
Common Adenomas and Malignant Polyps<br />
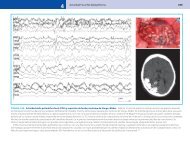
Figure 23-1 ■ Normal colonic mucosa. The luminal surface is straight, and<br />
the colonic tubules are tightly packed, parallel, nonbranching, and closely<br />
approximating the muscularis mucosae.<br />
An adenoma, defined as a benign intraepithelial neoplasm<br />
composed of epithelial cells exhibiting cytologic dysplasia,<br />
is considered the precursor lesion of most colorectal<br />
carcinomas. 1,10-12 Dysplasia is characterized by decreased<br />
intraepithelial mucin, epithelial nuclear enlargement with<br />
hyperchromasia, nuclear stratification, and increased<br />
numbers of mitotic figures. <strong>Large</strong> bowel adenomas are<br />
highly prevalent in Western societies. The frequency of<br />
these tumors markedly increases after age 40 years and<br />
reaches a peak at age 70 years. Adenomas are usually asymptomatic<br />
but large ones may bleed.<br />
Adenomas usually produce a raised endoscopically or<br />
grossly detectable abnormality, generally a protrusion<br />
or polyp that can often be further subclassified as sessile or<br />
pedunculated. Some adenomas appear flat; some may cause<br />
mucosal depressions. Adenomas occur singly or can be