HCMC_P_049062 - Hennepin County Medical Center
HCMC_P_049062 - Hennepin County Medical Center
HCMC_P_049062 - Hennepin County Medical Center
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Case Reports<br />
5<br />
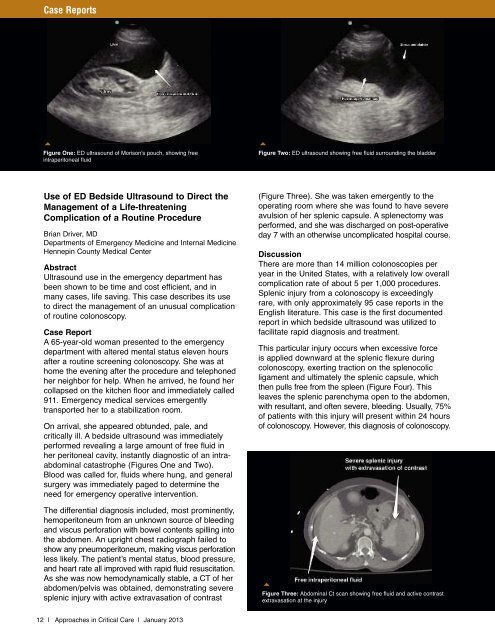
Figure One: ED ultrasound of Morison's pouch, showing free<br />
intraperitoneal fluid<br />
5<br />
Figure Two: ED ultrasound showing free fluid surrounding the bladder<br />
Use of ED Bedside Ultrasound to Direct the<br />
Management of a Life-threatening<br />
Complication of a Routine Procedure<br />
Brian Driver, MD<br />
Departments of Emergency Medicine and Internal Medicine<br />
<strong>Hennepin</strong> <strong>County</strong> <strong>Medical</strong> <strong>Center</strong><br />
Abstract<br />
Ultrasound use in the emergency department has<br />
been shown to be time and cost efficient, and in<br />
many cases, life saving. This case describes its use<br />
to direct the management of an unusual complication<br />
of routine colonoscopy.<br />
Case Report<br />
A 65-year-old woman presented to the emergency<br />
department with altered mental status eleven hours<br />
after a routine screening colonoscopy. She was at<br />
home the evening after the procedure and telephoned<br />
her neighbor for help. When he arrived, he found her<br />
collapsed on the kitchen floor and immediately called<br />
911. Emergency medical services emergently<br />
transported her to a stabilization room.<br />
On arrival, she appeared obtunded, pale, and<br />
critically ill. A bedside ultrasound was immediately<br />
performed revealing a large amount of free fluid in<br />
her peritoneal cavity, instantly diagnostic of an intraabdominal<br />
catastrophe (Figures One and Two).<br />
Blood was called for, fluids where hung, and general<br />
surgery was immediately paged to determine the<br />
need for emergency operative intervention.<br />
The differential diagnosis included, most prominently,<br />
hemoperitoneum from an unknown source of bleeding<br />
and viscus perforation with bowel contents spilling into<br />
the abdomen. An upright chest radiograph failed to<br />
show any pneumoperitoneum, making viscus perforation<br />
less likely. The patient’s mental status, blood pressure,<br />
and heart rate all improved with rapid fluid resuscitation.<br />
As she was now hemodynamically stable, a CT of her<br />
abdomen/pelvis was obtained, demonstrating severe<br />
splenic injury with active extravasation of contrast<br />
(Figure Three). She was taken emergently to the<br />
operating room where she was found to have severe<br />
avulsion of her splenic capsule. A splenectomy was<br />
performed, and she was discharged on post-operative<br />
day 7 with an otherwise uncomplicated hospital course.<br />
Discussion<br />
There are more than 14 million colonoscopies per<br />
year in the United States, with a relatively low overall<br />
complication rate of about 5 per 1,000 procedures.<br />
Splenic injury from a colonoscopy is exceedingly<br />
rare, with only approximately 95 case reports in the<br />
English literature. This case is the first documented<br />
report in which bedside ultrasound was utilized to<br />
facilitate rapid diagnosis and treatment.<br />
This particular injury occurs when excessive force<br />
is applied downward at the splenic flexure during<br />
colonoscopy, exerting traction on the splenocolic<br />
ligament and ultimately the splenic capsule, which<br />
then pulls free from the spleen (Figure Four). This<br />
leaves the splenic parenchyma open to the abdomen,<br />
with resultant, and often severe, bleeding. Usually, 75%<br />
of patients with this injury will present within 24 hours<br />
of colonoscopy. However, this diagnosis of colonoscopy.<br />
5<br />
Figure Three: Abdominal Ct scan showing free fluid and active contrast<br />
extravasation at the injury<br />
12 | Approaches in Critical Care | January 2013