HCMC_P_049062 - Hennepin County Medical Center
HCMC_P_049062 - Hennepin County Medical Center
HCMC_P_049062 - Hennepin County Medical Center
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Case Reports<br />
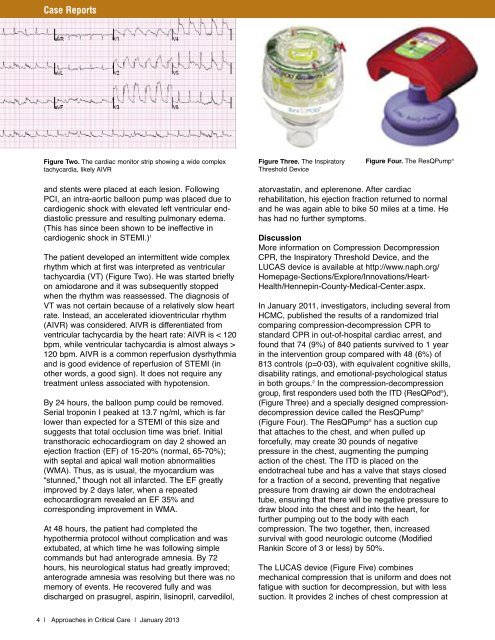
Figure Two. The cardiac monitor strip showing a wide complex<br />
tachycardia, likely AIVR<br />
Figure Three. The Inspiratory<br />
Threshold Device<br />
Figure Four. The ResQPump ®<br />
and stents were placed at each lesion. Following<br />
PCI, an intra-aortic balloon pump was placed due to<br />
cardiogenic shock with elevated left ventricular enddiastolic<br />
pressure and resulting pulmonary edema.<br />
(This has since been shown to be ineffective in<br />
cardiogenic shock in STEMI.) 1<br />
The patient developed an intermittent wide complex<br />
rhythm which at first was interpreted as ventricular<br />
tachycardia (VT) (Figure Two). He was started briefly<br />
on amiodarone and it was subsequently stopped<br />
when the rhythm was reassessed. The diagnosis of<br />
VT was not certain because of a relatively slow heart<br />
rate. Instead, an accelerated idioventricular rhythm<br />
(AIVR) was considered. AIVR is differentiated from<br />
ventricular tachycardia by the heart rate: AIVR is < 120<br />
bpm, while ventricular tachycardia is almost always ><br />
120 bpm. AIVR is a common reperfusion dysrhythmia<br />
and is good evidence of reperfusion of STEMI (in<br />
other words, a good sign). It does not require any<br />
treatment unless associated with hypotension.<br />
By 24 hours, the balloon pump could be removed.<br />
Serial troponin I peaked at 13.7 ng/ml, which is far<br />
lower than expected for a STEMI of this size and<br />
suggests that total occlusion time was brief. Initial<br />
transthoracic echocardiogram on day 2 showed an<br />
ejection fraction (EF) of 15-20% (normal, 65-70%);<br />
with septal and apical wall motion abnormalities<br />
(WMA). Thus, as is usual, the myocardium was<br />
“stunned,” though not all infarcted. The EF greatly<br />
improved by 2 days later, when a repeated<br />
echocardiogram revealed an EF 35% and<br />
corresponding improvement in WMA.<br />
At 48 hours, the patient had completed the<br />
hypothermia protocol without complication and was<br />
extubated, at which time he was following simple<br />
commands but had anterograde amnesia. By 72<br />
hours, his neurological status had greatly improved;<br />
anterograde amnesia was resolving but there was no<br />
memory of events. He recovered fully and was<br />
discharged on prasugrel, aspirin, lisinopril, carvedilol,<br />
atorvastatin, and eplerenone. After cardiac<br />
rehabilitation, his ejection fraction returned to normal<br />
and he was again able to bike 50 miles at a time. He<br />
has had no further symptoms.<br />
Discussion<br />
More information on Compression Decompression<br />
CPR, the Inspiratory Threshold Device, and the<br />
LUCAS device is available at http://www.naph.org/<br />
Homepage-Sections/Explore/Innovations/Heart-<br />
Health/<strong>Hennepin</strong>-<strong>County</strong>-<strong>Medical</strong>-<strong>Center</strong>.aspx.<br />
In January 2011, investigators, including several from<br />
<strong>HCMC</strong>, published the results of a randomized trial<br />
comparing compression-decompression CPR to<br />
standard CPR in out-of-hospital cardiac arrest, and<br />
found that 74 (9%) of 840 patients survived to 1 year<br />
in the intervention group compared with 48 (6%) of<br />
813 controls (p=0·03), with equivalent cognitive skills,<br />
disability ratings, and emotional-psychological status<br />
in both groups. 2 In the compression-decompression<br />
group, first responders used both the ITD (ResQPod ® ),<br />
(Figure Three) and a specially designed compressiondecompression<br />
device called the ResQPump ®<br />
(Figure Four). The ResQPump ® has a suction cup<br />
that attaches to the chest, and when pulled up<br />
forcefully, may create 30 pounds of negative<br />
pressure in the chest, augmenting the pumping<br />
action of the chest. The ITD is placed on the<br />
endotracheal tube and has a valve that stays closed<br />
for a fraction of a second, preventing that negative<br />
pressure from drawing air down the endotracheal<br />
tube, ensuring that there will be negative pressure to<br />
draw blood into the chest and into the heart, for<br />
further pumping out to the body with each<br />
compression. The two together, then, increased<br />
survival with good neurologic outcome (Modified<br />
Rankin Score of 3 or less) by 50%.<br />
The LUCAS device (Figure Five) combines<br />
mechanical compression that is uniform and does not<br />
fatigue with suction for decompression, but with less<br />
suction. It provides 2 inches of chest compression at<br />
4 | Approaches in Critical Care | January 2013