Novel Posterior Splinting Technique to Avoid Heel Ulcers - Healio
Novel Posterior Splinting Technique to Avoid Heel Ulcers - Healio
Novel Posterior Splinting Technique to Avoid Heel Ulcers - Healio
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Novel</strong> <strong>Posterior</strong> <strong>Splinting</strong> <strong>Technique</strong> <strong>to</strong><br />
<strong>Avoid</strong> <strong>Heel</strong> <strong>Ulcers</strong><br />
Raymond Y. Hsu, MD; Craig R. Lareau, MD; Chris<strong>to</strong>pher T. Born, MD<br />
n tips & techniques<br />
Section Edi<strong>to</strong>r: Steven F. Harwin, MD<br />
foot and<br />
SPOTLIGHT ON<br />
ankle<br />
Abstract: <strong>Heel</strong> ulcers are a costly and preventable complication<br />
of lower-extremity immobilization, but they still occur<br />
with some regularity. A technique using a short leg posterior<br />
splint that suspends the heel away from the splint is described.<br />
This modification completely removes pressure the heel <strong>to</strong><br />
prevent decubitus ulcer formation. This technique is simple,<br />
inexpensive, and effective.<br />
The short leg posterior<br />
splint is commonly used<br />
by orthopedic surgeons <strong>to</strong> immobilize<br />
the foot and ankle<br />
after injury. It can be applied<br />
in multiple settings, including<br />
the outpatient clinic and<br />
emergency department. It is<br />
typically reserved for ankle<br />
sprains and nonoperative foot<br />
and ankle fractures. It is also<br />
useful for operative fractures,<br />
either for temporary preoperative<br />
immobilization or for<br />
pos<strong>to</strong>perative protection of<br />
fracture fixation and soft tissue<br />
management. A short leg<br />
posterior splint does not carry<br />
the risks of compartment syndrome<br />
or malleolar pressure<br />
ulcers associated with more<br />
restrictive immobilizations,<br />
such as circumferential casting<br />
or AO splinting with side gussets.<br />
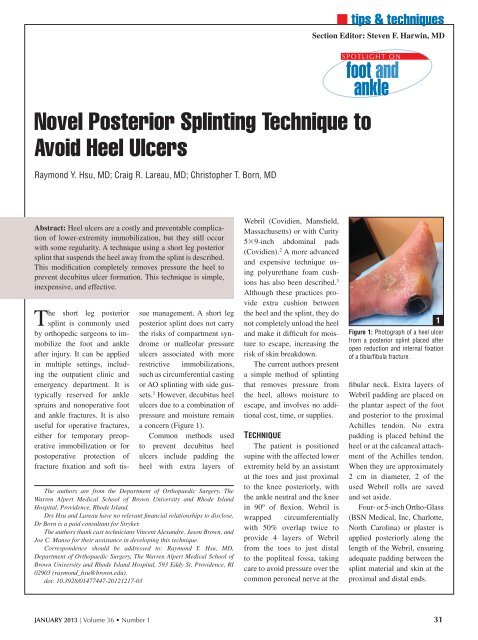
1 However, decubitus heel<br />
ulcers due <strong>to</strong> a combination of<br />
pressure and moisture remain<br />
a concern (Figure 1).<br />
Common methods used<br />
<strong>to</strong> prevent decubitus heel<br />
ulcers include padding the<br />
heel with extra layers of<br />
The authors are from the Department of Orthopaedic Surgery, The<br />
Warren Alpert Medical School of Brown University and Rhode Island<br />
Hospital, Providence, Rhode Island.<br />
Drs Hsu and Lareau have no relevant financial relationships <strong>to</strong> disclose.<br />
Dr Born is a paid consultant for Stryker.<br />
The authors thank cast technicians Vincent Alexandre, Jason Brown, and<br />
Joe C. Manso for their assistance in developing this technique.<br />
Correspondence should be addressed <strong>to</strong>: Raymond Y. Hsu, MD,<br />
Department of Orthopaedic Surgery, The Warren Alpert Medical School of<br />
Brown University and Rhode Island Hospital, 593 Eddy St, Providence, RI<br />
02903 (raymond_hsu@brown.edu).<br />
doi: 10.3928/01477447-20121217-03<br />
Webril (Covidien, Mansfield,<br />
Massachusetts) or with Curity<br />
539-inch abdominal pads<br />
(Covidien). 2 A more advanced<br />
and expensive technique using<br />
polyurethane foam cushions<br />
has also been described. 3<br />
Although these practices provide<br />
extra cushion between<br />
the heel and the splint, they do<br />
not completely unload the heel<br />
and make it difficult for moisture<br />
<strong>to</strong> escape, increasing the<br />
risk of skin breakdown.<br />
The current authors present<br />
a simple method of splinting<br />
that removes pressure from<br />
the heel, allows moisture <strong>to</strong><br />
escape, and involves no additional<br />
cost, time, or supplies.<br />
<strong>Technique</strong><br />
The patient is positioned<br />
supine with the affected lower<br />
extremity held by an assistant<br />
at the <strong>to</strong>es and just proximal<br />
<strong>to</strong> the knee posteriorly, with<br />
the ankle neutral and the knee<br />
in 90º of flexion. Webril is<br />
wrapped circumferentially<br />
with 50% overlap twice <strong>to</strong><br />
provide 4 layers of Webril<br />
from the <strong>to</strong>es <strong>to</strong> just distal<br />
<strong>to</strong> the popliteal fossa, taking<br />
care <strong>to</strong> avoid pressure over the<br />
common peroneal nerve at the<br />
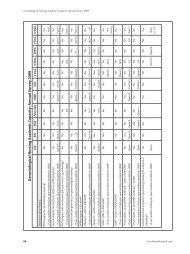
Figure 1: Pho<strong>to</strong>graph of a heel ulcer<br />
from a posterior splint placed after<br />
open reduction and internal fixation<br />
of a tibia/fibula fracture.<br />
fibular neck. Extra layers of<br />
Webril padding are placed on<br />
the plantar aspect of the foot<br />
and posterior <strong>to</strong> the proximal<br />
Achilles tendon. No extra<br />
padding is placed behind the<br />
heel or at the calcaneal attachment<br />
of the Achilles tendon.<br />
When they are approximately<br />
2 cm in diameter, 2 of the<br />
used Webril rolls are saved<br />
and set aside.<br />
Four- or 5-inch Ortho-Glass<br />
(BSN Medical, Inc, Charlotte,<br />
North Carolina) or plaster is<br />
applied posteriorly along the<br />
length of the Webril, ensuring<br />
adequate padding between the<br />
splint material and skin at the<br />
proximal and distal ends.<br />
1<br />
JANUARY 2013 | Volume 36 • Number 1 31
n tips & techniques<br />
2A<br />
2C<br />
Figure 2: Pho<strong>to</strong>graphs showing 2 small rolls of Webril (Covidien, Mansfield, Massachusetts) placed posterior <strong>to</strong> the<br />
heel between the Webril padding and splint material (A). After an elastic bandage is applied and the splint hardens (B),<br />
the ACE wrap is windowed <strong>to</strong> allow the 2 small rolls of Webril <strong>to</strong> be removed (C). The ACE wrap is readjusted back <strong>to</strong><br />
its original position (D).<br />
2B<br />
2D<br />
when immobilized and would<br />
benefit from this modification.<br />
4 This splinting technique<br />
is particularly helpful when<br />
heels are at an increased risk<br />
of skin breakdown from moisture.<br />
This includes patients<br />
with pitting edema, serous<br />
drainage from incisions, or<br />
calcaneal traction pin sites.<br />
Although useful for all patients,<br />
this splint is most valuable<br />
in patients at increased risk<br />
of heel complications secondary<br />
<strong>to</strong> diabetes mellitus, neurologic<br />
disorders, noncompliance,<br />
and draining wounds. In<br />
the authors’ experience with<br />
this splinting modification over<br />
the past year, no heel ulcers<br />
have developed.<br />
When using plaster, extra<br />
caution must be used with<br />
water temperature, padding,<br />
splint thickness, and inadvertent<br />
placement of the extremity<br />
on<strong>to</strong> insulating material (eg,<br />
plastic-covered hospital pillow)<br />
that may cause a partial- or fullthickness<br />
skin burn. To create a<br />
space <strong>to</strong> unload the heel, the 2<br />
saved 2-cm rolls of Webril are<br />
inserted deep in<strong>to</strong> the splint<br />
material and superficial <strong>to</strong> the<br />
Webril posterior <strong>to</strong> the heel and<br />
the attachment of the Achilles<br />
tendon (Figure 2A).<br />
An elastic bandage is then<br />
wrapped loosely <strong>to</strong> secure<br />
the splint in standard fashion.<br />
After the splint material has<br />
hardened, the 2 small rolls of<br />
Webril are removed (Figures<br />
2B, C) and the ACE bandage<br />
is adjusted back <strong>to</strong> its original<br />
position (Figure 2D).<br />
Discussion<br />
To the authors’ knowledge,<br />
this heel suspension short leg<br />
posterior splint has not been<br />
described previously in the<br />
literature. It provides a simple<br />
and inexpensive method<br />
of preventing what can be a<br />
costly complication of lowerextremity<br />
immobilization.<br />
A recent study of 216 patients<br />
with lower-extremity<br />
casts reported a 17.6% rate<br />
of heel pressure ulcers. 4<br />
Although no studies have examined<br />
the financial costs of<br />
heel pressure ulcers from casting,<br />
a significant body of literature<br />
examines the economic<br />
and legal costs of heel ulcers<br />
in general. 5 The cost of treating<br />
a single heel pressure ulcer<br />
is estimated <strong>to</strong> be between<br />
$2000 and $30,000. 6 These<br />
estimates are for general heel<br />
pressure ulcers and do not account<br />
for the additional costs<br />
in the presence of an operative<br />
fracture, such as delays in fixation<br />
and difficulties with bone<br />
and hardware coverage.<br />
The described splinting<br />
modification removes pressure<br />
from the heel and better<br />
ventilates the most dependent<br />
aspect of the splint without<br />
sacrificing immobilization<br />
strength. Although all patients<br />
are instructed <strong>to</strong> follow heel<br />
precautions, which involves<br />
avoiding direct pressure over<br />
the heel of the splint, this<br />
splint protects the heel in patients<br />
who are unable or refuse<br />
<strong>to</strong> comply with these recommendations.<br />
Patients with signs of heel<br />
soreness at splinting have been<br />
shown <strong>to</strong> be at significantly<br />
increased risk of heel ulcers<br />
References<br />
1. Halanski M, Noonan KJ. Cast<br />
and splint immobilization:<br />
complications. J Am Acad Orthop<br />
Surg. 2008; 16(1):30-40.<br />
2. Hipps HE. Prevention of cast<br />
pressure-sores on the heel.<br />
Southwest Med. 1964; 45:19-<br />
22.<br />
3. Forni C, Loro L, Tremosini M,<br />
et al. Use of polyurethane foam<br />
inside plaster casts <strong>to</strong> prevent<br />
the onset of heel sores in the<br />
population at risk. A controlled<br />
clinical study. J Clin Nurs.<br />
2011; 20(5-6):675-680.<br />
4. Forni C, Zoli M, Loro L, et al.<br />
Cohort study of the incidence<br />
of heel pressure sores in patients<br />
with leg casts at the Rizzoli<br />
Orthopedic Hospital and<br />
of the associated risk fac<strong>to</strong>rs<br />
[in Italian]. Assist Inferm Ric.<br />
2009; 28(3):125-130.<br />
5. Lyder CH. Preventing heel<br />
pressure ulcers: economic and<br />
legal implications. Nurs Manage.<br />
2011; 42(11):16-19.<br />
6. Lyman V. Successful heel pressure<br />
ulcer prevention program<br />
in a long-term care setting. J<br />
Wound Os<strong>to</strong>my Continence<br />
Nurs. 2009; 36(6):616-621.<br />
32 ORTHOPEDICS | <strong>Healio</strong>.com/Orthopedics