Changes in Surgical Procedures for Acromioclavicular Joint ... - Healio
Changes in Surgical Procedures for Acromioclavicular Joint ... - Healio
Changes in Surgical Procedures for Acromioclavicular Joint ... - Healio
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
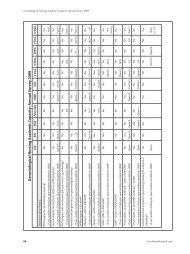
n Feature Article<br />
<strong>Changes</strong> <strong>in</strong> <strong>Surgical</strong> <strong>Procedures</strong> <strong>for</strong><br />
<strong>Acromioclavicular</strong> Jo<strong>in</strong>t Dislocation<br />
Over the Past 30 Years<br />
Katsumi Takase, MD, PhD; Kengo Yamamoto, MD, PhD<br />
abstract<br />
Full article available onl<strong>in</strong>e at <strong>Healio</strong>.com/Orthopedics. Search: 20130920-20<br />
Generally, surgical treatment is recommended <strong>for</strong> Rockwood type 5 traumatic acromioclavicular<br />
jo<strong>in</strong>t dislocations. S<strong>in</strong>ce 1980, the authors have per<strong>for</strong>med the modified<br />
Dewar procedure, the modified Cadenat procedure, and anatomical reconstruction of<br />
the coracoclavicular ligaments <strong>for</strong> this <strong>in</strong>jury. The goal of this study was to determ<strong>in</strong>e<br />
the ideal surgical procedure <strong>for</strong> acromioclavicular jo<strong>in</strong>t dislocations by compar<strong>in</strong>g<br />
these 3 procedures.<br />
A<br />
The modified Dewar procedure was per<strong>for</strong>med on 55 patients (Dewar group), the<br />
modified Cadenat procedure was per<strong>for</strong>med on 73 patients (Cadenat group), and<br />
anatomical reconstruction of the coracoclavicular ligaments was per<strong>for</strong>med on 11<br />
patients (reconstruction group). Accord<strong>in</strong>g to the UCLA scor<strong>in</strong>g system, therapeutic<br />
results averaged 27.3 po<strong>in</strong>ts <strong>in</strong> the Dewar group, 28.2 <strong>in</strong> the Cadenat group, and 28.4<br />
<strong>in</strong> the reconstruction group. The <strong>in</strong>cidence of residual subluxation or dislocation <strong>in</strong><br />
the acromioclavicular jo<strong>in</strong>t was evaluated at f<strong>in</strong>al radiographic follow-up. Subluxation<br />
occurred <strong>in</strong> 21 patients <strong>in</strong> the Dewar group, 18 <strong>in</strong> the Cadenat group, and 3 <strong>in</strong> the<br />
reconstruction group. Dislocation occurred <strong>in</strong> 3 patients <strong>in</strong> the Dewar group. Osteoarthritic<br />
changes <strong>in</strong> the acromioclavicular jo<strong>in</strong>t occurred <strong>in</strong> 20 patients <strong>in</strong> the Dewar<br />
group, 9 <strong>in</strong> the Cadenat group, and 1 <strong>in</strong> the reconstruction group.<br />
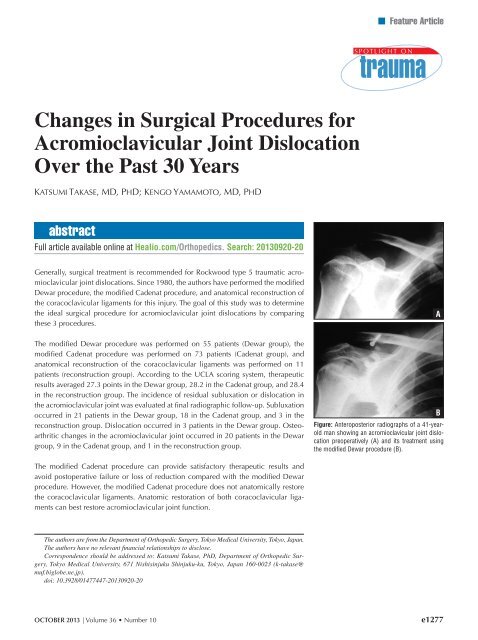
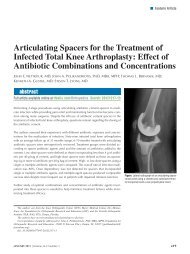
Figure: Anteroposterior radiographs of a 41-yearold<br />
man show<strong>in</strong>g an acromioclavicular jo<strong>in</strong>t dislocation<br />
preoperatively (A) and its treatment us<strong>in</strong>g<br />
the modified Dewar procedure (B).<br />
B<br />
The modified Cadenat procedure can provide satisfactory therapeutic results and<br />
avoid postoperative failure or loss of reduction compared with the modified Dewar<br />
procedure. However, the modified Cadenat procedure does not anatomically restore<br />
the coracoclavicular ligaments. Anatomic restoration of both coracoclavicular ligaments<br />
can best restore acromioclavicular jo<strong>in</strong>t function.<br />
The authors are from the Department of Orthopedic Surgery, Tokyo Medical University, Tokyo, Japan.<br />
The authors have no relevant f<strong>in</strong>ancial relationships to disclose.<br />
Correspondence should be addressed to: Katsumi Takase, PhD, Department of Orthopedic Surgery,<br />
Tokyo Medical University, 671 Nishis<strong>in</strong>juku Sh<strong>in</strong>juku-ku, Tokyo, Japan 160-0023 (k-takase@<br />
muf.biglobe.ne.jp).<br />
doi: 10.3928/01477447-20130920-20<br />
OCTOBER 2013 | Volume 36 • Number 10<br />
e1277
n Feature Article<br />
Various treatment methods, both<br />
conservative and surgical, have<br />
been used <strong>for</strong> traumatic acromioclavicular<br />
jo<strong>in</strong>t dislocations. Generally,<br />
surgical treatment is recommended <strong>for</strong><br />
Rockwood type 4, 5, and 6 dislocations. 1<br />
However, surgical and conservative treatments<br />
<strong>for</strong> type 3 dislocations are controversial<br />
and have not been standardized.<br />
Many surgical procedures have been considered<br />
and reported <strong>in</strong> the literature, with<br />
no consensus at present. 2,3<br />
S<strong>in</strong>ce 1980, the current authors have<br />
per<strong>for</strong>med the modified Dewar procedure<br />
<strong>for</strong> the reduction of the dislocated acromioclavicular<br />
jo<strong>in</strong>t us<strong>in</strong>g the dynamic muscle<br />
strength of the conjo<strong>in</strong>ed tendon. 4 However,<br />
this procedure has various problems,<br />
<strong>in</strong>clud<strong>in</strong>g damage by surgical <strong>in</strong>vasion and<br />
long-term immobilization. In consideration<br />
of these problems, s<strong>in</strong>ce 1995 the authors<br />
have per<strong>for</strong>med the modified Cadenat<br />
procedure, which reconstructs the coracoclavicular<br />
ligaments us<strong>in</strong>g the coracoacromial<br />
ligaments. 5 However, anatomic restoration<br />
of the coracoclavicular ligaments<br />
can best restore acromioclavicular jo<strong>in</strong>t<br />
function. Based on the anatomical data <strong>for</strong><br />
the structures of the trapezoid and conoid<br />
ligaments, 6 these procedures do not aim to<br />
anatomically reconstruct the coracoclavicular<br />
ligaments. There<strong>for</strong>e, the authors<br />
have attempted to correctly reconstruct the<br />
anatomy of the coracoclavicular ligaments<br />
(trapezoid and conoid ligaments) us<strong>in</strong>g the<br />
ipsilateral palmaris longus tendon and an<br />
EndoButton (Smith & Nephew Endoscopy,<br />
Andover, Massachusetts) as the reconstruct<strong>in</strong>g<br />
ligament and fixation material,<br />
respectively. 7<br />
The goal of this study was to discover<br />
the ideal surgical procedure <strong>for</strong> acromioclavicular<br />
jo<strong>in</strong>t dislocations by compar<strong>in</strong>g the<br />
modified Dewar procedure, the modified<br />
Cadenat procedure, and anatomical reconstruction<br />
of the coracoclavicular ligaments.<br />
Materials and Methods<br />
Accord<strong>in</strong>g to Rockwood’s classification,<br />
on pla<strong>in</strong> radiographs all patients<br />
were evaluated as hav<strong>in</strong>g type 5 traumatic<br />
acromioclavicular jo<strong>in</strong>t dislocations.<br />
Modified Dewar Procedure<br />
The modified Dewar procedure was<br />
per<strong>for</strong>med <strong>in</strong> 55 patients (Dewar group)<br />
between 1980 and 1994. The group comprised<br />
51 (92.7%) men and 4 (7.3%)<br />
women with a mean age of 34.5 years<br />
(range, 16-66 years) at surgery. The right<br />
side was affected <strong>in</strong> 29 (52.7%) patients<br />
and the left side <strong>in</strong> 26 (47.3%) patients.<br />
The mechanism of <strong>in</strong>jury was a traffic<br />
accident <strong>in</strong> 25 (45.5%) patients, a sports<br />
accident <strong>in</strong> 19 (34.5%), and other causes<br />
<strong>in</strong> 11 (20%) patients. Mean follow-up was<br />
50 months (range, 33-106 months).<br />
Dur<strong>in</strong>g the procedure, the coracoid<br />
process was directly confirmed through<br />
the deltopectoral approach. Then, approximately<br />
1.5 cm of the tip of the<br />
coracoid process was osteomized and<br />
detached, along with the coracobrachialis<br />
muscle and short head of the biceps<br />
brachialis muscle. The dislocated<br />
acromioclavicular jo<strong>in</strong>t was fixed us<strong>in</strong>g<br />
2 K-wires, preserv<strong>in</strong>g the <strong>in</strong>traarticular<br />
disk as much as possible, and the<br />
torn capsule and acromioclavicular ligaments<br />
were sequentially repaired. F<strong>in</strong>ally,<br />
the detached coracoid process was fixed<br />
with these muscles to the anterior side of<br />
the clavicle approximately 3 cm from the<br />
distal edge of the clavicle us<strong>in</strong>g a screw<br />
with a spike washer (Figure 1) .<br />
Postoperative treatment consisted of<br />
immobilization with a Velpeau bandage<br />
<strong>for</strong> 5 weeks. Beg<strong>in</strong>n<strong>in</strong>g at postoperative<br />
week 6, <strong>for</strong>ward elevation by passive<br />
movement <strong>in</strong> the sup<strong>in</strong>e position and pendulum<br />
exercises were prescribed. The K-<br />
wires were removed 6 weeks postoperatively<br />
(Figure 2).<br />
Modified Cadenat Procedure<br />
Between 1995 and 2009, the modified<br />
Cadenat procedure was per<strong>for</strong>med <strong>in</strong><br />
73 patients with acromioclavicular jo<strong>in</strong>t<br />
dislocations (Cadenat group). The group<br />
comprised 66 (90.4%) men and 7 (9.6%)<br />
Figure 1: Schema of the modified Dewar procedure<br />
illustrat<strong>in</strong>g the tip of the coracoid process<br />
fixed by a screw (A) and the conjo<strong>in</strong>ed tendon <strong>in</strong>clud<strong>in</strong>g<br />
the coracobrachialis and short head of the<br />
biceps brachii (B).<br />
women with a mean age of 35.4 years at<br />
surgery (range, 16-63 years). The right<br />
side was affected <strong>in</strong> 41 (56.2%) patients<br />
and the left side <strong>in</strong> 32 (43.8%) patients.<br />
The mechanism of <strong>in</strong>jury was traffic accident<br />
<strong>in</strong> 30 (41.1%) patients, sports accident<br />
<strong>in</strong> 18 (24.7%), work accident <strong>in</strong> 8<br />
(11%), and other causes <strong>in</strong> 17 (23.3%).<br />
Time from <strong>in</strong>jury to surgery was less than<br />
2 weeks <strong>in</strong> 65 (89%) patients (acute cases),<br />
1<br />
2A<br />
2B<br />
Figure 2: Anteroposterior radiographs of a 41-yearold<br />
man show<strong>in</strong>g an acromioclavicular jo<strong>in</strong>t dislocation<br />
preoperatively (A) and its treatment us<strong>in</strong>g<br />
the modified Dewar procedure (B).<br />
e1278<br />
ORTHOPEDICS | <strong>Healio</strong>.com/Orthopedics
<strong>Acromioclavicular</strong> Jo<strong>in</strong>t Dislocation | Takase & Yamamoto<br />
between 2 weeks and 1 month <strong>in</strong> 5 (6.8%)<br />
patients (subacute cases), and more than 1<br />
month <strong>in</strong> 3 (4.1%) patients (chronic cases).<br />
Fifty-three (72.6%) of these patients<br />
had participated <strong>in</strong> sports activities be<strong>for</strong>e<br />
<strong>in</strong>jury, and 48 (65.8%) patients, <strong>in</strong>clud<strong>in</strong>g<br />
32 contact sports players, engaged <strong>in</strong><br />
high-level sports activities. Mean followup<br />
was 30 months (range, 14-75 months).<br />
Dur<strong>in</strong>g the procedure, the coracoid<br />
process was directly confirmed through<br />
the deltopectoral approach. Initially, the<br />
coracoacromial ligaments at the acromial<br />
<strong>in</strong>sertion site and a small bone tip were<br />
detached (Figure 3). The dislocated acromioclavicular<br />
jo<strong>in</strong>t was fixed us<strong>in</strong>g a hook<br />
plate, preserv<strong>in</strong>g the <strong>in</strong>tra-articular disk<br />
as much as possible, and the torn capsule<br />
and acromioclavicular ligaments were sequentially<br />
repaired. F<strong>in</strong>ally, the detached<br />
coracoacromial ligament with the bone tip<br />
was fixed to the anterior side of the clavicle<br />
us<strong>in</strong>g a screw with a spike washer <strong>in</strong> a<br />
position that allowed sufficient tension to<br />
be obta<strong>in</strong>ed (Figure 4).<br />
Postoperative treatment consisted of<br />
immobilization with a Désault bandage<br />
<strong>for</strong> 2 weeks. Beg<strong>in</strong>n<strong>in</strong>g at postoperative<br />
week 4, <strong>for</strong>ward elevation by passive<br />
movement <strong>in</strong> the sup<strong>in</strong>e position and pendulum<br />
exercises were prescribed (Figure<br />
5). The Wolter clavicular plate was removed<br />
4 months postoperatively.<br />
Figure 3: Schema of the modified Cadenat procedure<br />
show<strong>in</strong>g the acromial <strong>in</strong>sertion area of the<br />
coracoacromial ligament (diagonal l<strong>in</strong>e), the coracoacromial<br />
ligament (A), and the lateral (B) and<br />
medial (C) edges of the coracoacromial ligament.<br />
5A<br />
3<br />
Figure 4: Schema of the modified Cadenat procedure<br />
show<strong>in</strong>g the detached coracoacromial ligament<br />
with the bone tip fixed to the anterior side of<br />
the clavicle us<strong>in</strong>g a screw with a spike washer <strong>in</strong> a<br />
position that allowed sufficient tension to be obta<strong>in</strong>ed.<br />
Abbreviations: A, coracoacromial ligament;<br />
B, lateral edge of the coracoacromial ligament; C,<br />
medial edge of the coracoacromial ligament.<br />
Figure 5: Anteroposterior radiographs of a 29-year-old man show<strong>in</strong>g an acromioclavicular jo<strong>in</strong>t dislocation<br />
preoperatively (A) and treatment with the modified Cadenat procedure (B).<br />
4<br />
5B<br />
Anatomical Reconstruction of the<br />
Coracoclavicular Ligaments<br />
S<strong>in</strong>ce 2008, the authors have reconstructed<br />
the anatomical structure of the<br />
coracoclavicular ligaments (trapezoid and<br />
conoid ligaments) with an artificial ligament<br />
and the ipsilateral palmaris longus<br />
tendon used as substitute ligaments, respectively<br />
(reconstruction group). Eleven<br />
patients with acromioclavicular jo<strong>in</strong>t dislocations<br />
underwent this procedure. The<br />
group comprised 11 men with a mean<br />
age of 38.6 years at surgery (range, 19-<br />
67 years). The right side was affected <strong>in</strong><br />
7 (63.6%) patients and the left side <strong>in</strong> 4<br />
(36.4%) patients. The mechanism of <strong>in</strong>jury<br />
was traffic accident <strong>in</strong> 2 (18.2%) patients,<br />
sports accident <strong>in</strong> 4 (36.4%), and<br />
a fall <strong>in</strong> 5 (45.5%). Mean time from <strong>in</strong>jury<br />
to surgery was 16.3 days (range, 9-30<br />
days). Mean follow-up was 17 months<br />
(range, 12-43 months).<br />
The double-bundle procedure reconstruct<strong>in</strong>g<br />
both the trapezoid and conoid<br />
ligaments was per<strong>for</strong>med. Initially, a 16-<br />
cm or longer length of the palmaris longus<br />
tendon was excised from the ipsilateral<br />
side as the substitute <strong>for</strong> the conoid ligament<br />
(Figure 6A). An artificial ligament<br />
(Dacron; Smith & Nephew Endoscopy)<br />
was used <strong>for</strong> reconstruct<strong>in</strong>g the trapezoid<br />
ligament (Figure 6B). An EndoButton<br />
was used <strong>for</strong> fixation of the tendon or artificial<br />
ligament on the coracoid process<br />
side, and a screw with a spike washer was<br />
used on the clavicle side. The excised palmaris<br />
longus tendon was fashioned <strong>in</strong>to a<br />
quadruple-stranded graft with a m<strong>in</strong>imal<br />
length of 4 cm <strong>for</strong> reconstruct<strong>in</strong>g the conoid<br />
ligament. Dur<strong>in</strong>g these preparations,<br />
the EndoButton was placed at the loop<br />
end of the conoid graft and the artificial<br />
ligament at the other end of the conoid<br />
graft. The conoid ligament reconstruction<br />
was per<strong>for</strong>med under arthroscopy. To<br />
acquire firm fixation and prevent s<strong>in</strong>k<strong>in</strong>g<br />
OCTOBER 2013 | Volume 36 • Number 10<br />
e1279
n Feature Article<br />
and pendulum exercises were prescribed.<br />
All immobilization was discont<strong>in</strong>ued at 2<br />
weeks postoperatively (Figure 8).<br />
6A<br />
6B<br />
Figure 6: Graft preparation <strong>for</strong> the conoid (A) and<br />
trapezoid (B) ligaments show<strong>in</strong>g the EndoButton<br />
(Smith & Nephew Endoscopy, Andover, Massachusetts)<br />
cont<strong>in</strong>uous loop (C), quadruple-stranded<br />
palmaris longus tendon (D), artificial ligament (E),<br />
and EndoButton (F).<br />
Figure 7: Schema of anatomical reconstruction of<br />
the coracoclavicular ligaments show<strong>in</strong>g the trapezoid<br />
ligament (1) fixed to the medial edge of the<br />
coracoid process (A1) and the conoid ligament (2)<br />
fixed to the undersurface of the basement of the<br />
coracoid process (A2).<br />
7<br />
Therapeutic Results and Statistical Analysis<br />
Therapeutic results were evaluated<br />
based on the UCLA scor<strong>in</strong>g system (30<br />
po<strong>in</strong>ts), 8 which consists of pa<strong>in</strong>, function,<br />
range of motion, and strength, exclud<strong>in</strong>g<br />
the patient’s satisfaction. Also, radiographic<br />
f<strong>in</strong>d<strong>in</strong>gs were evaluated, <strong>in</strong>clud<strong>in</strong>g<br />
the occurrence of osteoarthritic changes<br />
and the complete reduction or lack thereof<br />
<strong>in</strong> the acromioclavicular jo<strong>in</strong>t.<br />
Statistical analysis evaluated the differences<br />
among the 3 groups. A P level<br />
less than .05 us<strong>in</strong>g the Mann-Whitney U<br />
test was considered significant.<br />
8A<br />
Figure 8: Anteroposterior radiographs of a 23-year-old man show<strong>in</strong>g an acromioclavicular jo<strong>in</strong>t dislocation<br />
preoperatively (A) and treatment with anatomical reconstruction of the coracoclavicular ligaments<br />
show<strong>in</strong>g the bone tunnels <strong>for</strong> the conoid (boxed C) and trapezoid (boxed D) ligaments (B).<br />
of the EndoButton, the soft tissue under<br />
the surface of the coracoid process was<br />
cleaned to expose the cortex through the<br />
anterior portal.<br />
To create a bone tunnel <strong>for</strong> reconstruct<strong>in</strong>g<br />
the conoid ligament, a 2-mm<br />
diameter K-wire was <strong>in</strong>serted from the<br />
conoid tubercle of the clavicle to the base<br />
of the coracoid process under arthroscopy.<br />
Then, a 4-mm bone tunnel was created<br />
<strong>for</strong> the conoid graft us<strong>in</strong>g a cannulated<br />
drill bit with a diameter matched with the<br />
graft diameter by overdrill<strong>in</strong>g along that<br />
wire from the clavicle. Similarly, another<br />
2-mm diameter K-wire was <strong>in</strong>serted from<br />
the 1.5-cm medial portion from the lateral<br />
8B<br />
end of the clavicle to the medial side of<br />
the body of the coracoid process <strong>for</strong> reconstruct<strong>in</strong>g<br />
the trapezoid ligament. F<strong>in</strong>ally,<br />
each graft was <strong>in</strong>troduced through<br />
the anterior portal to the clavicle tunnel<br />
and fixed on the undersurface of the<br />
coracoid process by the EndoButton, respectively<br />
(Figure 7). Then, the clavicle<br />
side of each graft was fixed together by a<br />
screw with a spike washer. No temporary<br />
fixation of the acromioclavicular jo<strong>in</strong>t was<br />
per<strong>for</strong>med.<br />
Postoperative treatment consisted of<br />
immobilization with a Désault bandage <strong>for</strong><br />
approximately 1 week. Beg<strong>in</strong>n<strong>in</strong>g at postoperative<br />
week 2, only a sl<strong>in</strong>g was used,<br />
Results<br />
Accord<strong>in</strong>g to the UCLA scor<strong>in</strong>g system,<br />
mean therapeutic result was 27.3<br />
po<strong>in</strong>ts (range, 18-30 po<strong>in</strong>ts) <strong>in</strong> the Dewar<br />
group, 28.2 po<strong>in</strong>ts (range, 24-30 po<strong>in</strong>ts) <strong>in</strong><br />
the Cadenat group, and 28.4 po<strong>in</strong>ts (range,<br />
24-30 po<strong>in</strong>ts) <strong>in</strong> the reconstruction group.<br />
When the results were exam<strong>in</strong>ed, no significant<br />
difference among these groups<br />
was observed. However, regard<strong>in</strong>g postoperative<br />
range of motion, 59 (80.8%) of<br />
73 patients <strong>in</strong> the Cadenat group recovered<br />
more than 160° <strong>for</strong>ward elevation<br />
and 160° abduction at 3 months postoperatively,<br />
but 21 (38.1%) of 55 patients <strong>in</strong><br />
the Dewar group required approximately<br />
1 year to ga<strong>in</strong> their pre<strong>in</strong>jury range of motion.<br />
The rema<strong>in</strong><strong>in</strong>g patients did not rega<strong>in</strong><br />
their pre<strong>in</strong>jury range of motion.<br />
The <strong>in</strong>cidence of residual subluxation<br />
or dislocation <strong>in</strong> the acromioclavicular<br />
jo<strong>in</strong>t was evaluated at f<strong>in</strong>al radiographic<br />
follow-up. In the Dewar group, subluxation<br />
that represented less than 5 mm of<br />
superior translation of the clavicle occurred<br />
<strong>in</strong> 14 (25.5%) patients, subluxation<br />
that represented 5 to 10 mm of superior<br />
translation of the clavicle occurred <strong>in</strong> 7<br />
(12.7%) patients, and complete dislocation<br />
occurred <strong>in</strong> 3 (5.5%) patients. In the<br />
Cadenat group, subluxation that repre-<br />
e1280<br />
ORTHOPEDICS | <strong>Healio</strong>.com/Orthopedics
<strong>Acromioclavicular</strong> Jo<strong>in</strong>t Dislocation | Takase & Yamamoto<br />
sented less than 5 mm of superior translation<br />
of the clavicle occurred <strong>in</strong> 18 (24.7%)<br />
patients, and subluxation that represented<br />
more than 5 mm of superior translation of<br />
the clavicle or redislocation occurred <strong>in</strong> 0<br />
patients. In the reconstruction group, subluxation<br />
that represented less than 5 mm<br />
of superior translation of the clavicle occurred<br />
<strong>in</strong> 3 (27.3%) patients, and subluxation<br />
that represented more than 5 mm of<br />
superior translation of the clavicle or redislocation<br />
occurred <strong>in</strong> 0 patients.<br />
Osteoarthritic changes occurred <strong>in</strong> the<br />
acromioclavicular jo<strong>in</strong>t <strong>in</strong> 20 (36.4%) patients<br />
<strong>in</strong> the Dewar group, 9 (12.3%) patients<br />
<strong>in</strong> the Cadenat group, and 1 (9.1%)<br />
patient <strong>in</strong> the reconstruction group.<br />
Discussion<br />
<strong>Acromioclavicular</strong> jo<strong>in</strong>t separations<br />
are frequently treated <strong>in</strong> cl<strong>in</strong>ical practice.<br />
The degree or direction of translation of<br />
the clavicle aga<strong>in</strong>st the acromion depends<br />
on the <strong>in</strong>jury states of the acromioclavicular<br />
and coracoclavicular ligaments<br />
and detachment of deltoid or trapezius<br />
muscle from the clavicle. Rockwood et<br />
al 1 and Tossy et al 9 classified the degree<br />
or direction of displacement <strong>in</strong> acromioclavicular<br />
jo<strong>in</strong>t separations <strong>in</strong>to 6 and<br />
3 types, respectively. Generally, Rockwood<br />
type 5 dislocations are considered<br />
a good <strong>in</strong>dication <strong>for</strong> surgical treatment.<br />
Many surgical treatments exist <strong>for</strong> acromioclavicular<br />
jo<strong>in</strong>t dislocation, <strong>in</strong>clud<strong>in</strong>g<br />
repair of the acromioclavicular ligament<br />
(Phemister procedure 10 or Neviaser procedure<br />
11 ), fixation between the clavicle<br />
and the coracoid process (Bosworth procedure<br />
12 ), reconstruction of the coracoclavicular<br />
ligament us<strong>in</strong>g the coracoacromial<br />
ligament (Weaver-Dunn procedure 13 and<br />
Cadenat procedure 5 ), and dynamic stabilization<br />
of the coracoclavicular jo<strong>in</strong>t by<br />
the transferred conjo<strong>in</strong>ed tendon (Dewar<br />
procedure 4 ).<br />
Between 1980 and 2008, the current<br />
authors per<strong>for</strong>med 2 different surgical<br />
procedures (modified Dewar procedure<br />
and modified Cadenat procedure), which<br />
were not anatomical reconstruction of<br />
the coracoclavicular ligament, <strong>in</strong> patients<br />
with Rockwood type 5 acromioclavicular<br />
jo<strong>in</strong>t dislocations. The modified Dewar<br />
procedure has some disadvantages, <strong>in</strong>clud<strong>in</strong>g<br />
a long period required <strong>for</strong> range<br />
of motion recovery, a high frequency of<br />
residual subluxation or dislocation, and<br />
postoperative osteoarthritic changes on<br />
the acromioclavicular jo<strong>in</strong>t. In particular,<br />
the latter 2 disadvantages were considered<br />
to result from the dynamic stabilization<br />
of the acromioclavicular jo<strong>in</strong>t by the conjo<strong>in</strong>ed<br />
tendons. Skjeldal et al 14 reported<br />
that nonoperative treatment gave equal or<br />
better long-term functional results compared<br />
with the modified Dewar procedure<br />
<strong>in</strong> acute acromioclavicular dislocations,<br />
and they did not recommend the procedure<br />
<strong>in</strong> acute cases.<br />
Consider<strong>in</strong>g these disadvantages, the<br />
current authors began per<strong>for</strong>m<strong>in</strong>g the<br />
modified Cadenat procedure on patients<br />
with acromioclavicular jo<strong>in</strong>t dislocations<br />
<strong>in</strong> 1995. Patients undergo<strong>in</strong>g the modified<br />
Cadenat procedure needed a mean<br />
of 3.4 months to return to their occupation<br />
and a mean of 3.1 months to return<br />
to pre<strong>in</strong>jury-level sports activities. However,<br />
the modified Cadenat procedure also<br />
has some disadvantages. The mechanism<br />
of stabilization <strong>for</strong> the acromioclavicular<br />
jo<strong>in</strong>t is established by the coracoacromial<br />
ligament transferred from the acromion<br />
to the clavicle. This transferred coracoacromial<br />
ligament does not anatomically<br />
reconstruct the trapezoid and conoid ligaments<br />
that compose the coracoclavicular<br />
ligament. The conoid ligament attaches<br />
anatomically to the conoid tubercle,<br />
which is located at the posterior edge of<br />
the clavicle, and the clavicle can make an<br />
axial rotation dur<strong>in</strong>g <strong>for</strong>ward elevation of<br />
the shoulder jo<strong>in</strong>t. However, <strong>in</strong> the modified<br />
Cadenat procedure, it is possible that<br />
this axial rotation of the clavicle is restricted<br />
because the transferred coracoacromial<br />
ligament is fixed to the anterior<br />
edge of the clavicle. For this reason, even<br />
if the dislocated acromioclavicular jo<strong>in</strong>t is<br />
reduced <strong>in</strong> a normal position, it is possible<br />
that osteoarthritic changes can occur to<br />
the acromioclavicular jo<strong>in</strong>t. The Weaver-<br />
Dunn procedure, <strong>in</strong> which the transferred<br />
coracoacromial ligament is <strong>in</strong>serted <strong>in</strong>to<br />
the distal edge of the resected clavicle, is<br />
close to anatomical reconstruction of the<br />
trapezoid ligament. However, this procedure<br />
does not aim to reconstruct the anatomical<br />
acromioclavicular jo<strong>in</strong>t due to the<br />
distal clavicle resection.<br />
To reconstruct the coracoclavicular<br />
ligaments, Yoo et al 15 used the semitend<strong>in</strong>osus<br />
tendon, Sloan et al 16 used the lateral<br />
half slip of the conjo<strong>in</strong>ed tendon, Lädermann<br />
et al 17 and Marchie et al 18 used suture<br />
threads, and Wei et al 19 and Salzmann<br />
et al 20 used an artificial ligament. However,<br />
of these procedures, only the method<br />
us<strong>in</strong>g an artificial ligament achieved reconstruction<br />
of the anatomical coracoclavicular<br />
ligaments. In addition, us<strong>in</strong>g an<br />
artificial ligament <strong>for</strong> the procedure may<br />
make it impossible to acquire the same<br />
function as the congenital ligaments.<br />
The current authors per<strong>for</strong>med a double-bundle<br />
procedure with an artificial ligament<br />
and the palmaris longus tendon <strong>for</strong><br />
anatomical reconstruction of the trapezoid<br />
and conoid ligaments, respectively. On<br />
consider<strong>in</strong>g its location, features, and operative<br />
demerits, the authors believe that<br />
the palmaris longus tendon is a suitable<br />
substitute <strong>for</strong> the ligament. However, this<br />
tendon is th<strong>in</strong> and short <strong>for</strong> reconstruct<strong>in</strong>g<br />
the trapezoid and conoid ligaments.<br />
There<strong>for</strong>e, the authors used the palmaris<br />
longus tendon to reconstruct the conoid<br />
ligament, which is ma<strong>in</strong>ly responsible <strong>for</strong><br />
stabilization of the superior translation of<br />
the clavicle.<br />
This procedure aimed to anatomically<br />
reproduce the distribution and attachment<br />
sites of the trapezoid and conoid<br />
ligaments. Although the excision of the<br />
palmaris longus tendon is a disadvantage,<br />
anatomical reduction of the acromioclavicular<br />
jo<strong>in</strong>t was accomplished <strong>in</strong> 8<br />
(72.7%) of 11 patients. Also, it is possible<br />
to per<strong>for</strong>m this surgical technique under<br />
OCTOBER 2013 | Volume 36 • Number 10<br />
e1281
n Feature Article<br />
arthroscopy. Dur<strong>in</strong>g the follow-up period,<br />
no osseous erosion on the clavicle and<br />
no displacement of the EndoButton were<br />
noted. However, fracture of the coracoid<br />
process or the clavicle is possible <strong>in</strong>traoperatively.<br />
There<strong>for</strong>e, the tunnel creation <strong>in</strong><br />
the coracoid process or the clavicle should<br />
be carefully per<strong>for</strong>med.<br />
Conclusion<br />
The modified Cadenat procedure can<br />
provide satisfactory therapeutic results<br />
and avoid postoperative failure or loss of<br />
reduction of acromioclavicular jo<strong>in</strong>t separations<br />
compared with the modified Dewar<br />
procedure. However, the modified Cadenat<br />
procedure does not anatomically<br />
restore the coracoclavicular ligaments.<br />
Anatomic reconstruction of both coracoclavicular<br />
ligaments can best restore acromioclavicular<br />
jo<strong>in</strong>t function.<br />
References<br />
1. Rockwood CA Jr, Williams GR, Young<br />
CD. Injuries to the acromioclavicular jo<strong>in</strong>t.<br />
In: Rockwood CA Jr, Green DP, Bucholz<br />
RW, Heckman JD, eds. Fractures <strong>in</strong> Adults.<br />
vol 2, 4th ed. Philadelphia, PA: Lipp<strong>in</strong>cott-<br />
Raven; 1996:1341-1414.<br />
2. Calvo E, López-Franco M, Arribas IM.<br />
Cl<strong>in</strong>ical and radiologic outcomes of surgical<br />
and conservative treatment of type acromioclavicular<br />
jo<strong>in</strong>t <strong>in</strong>jury. J Shoulder Elbow<br />
Surg. 2006; 15(3):300-305.<br />
3. Gstettner C, Tauber M, Hitzl W, Resch H.<br />
Rockwood type acromioclavicular dislocation:<br />
surgical versus conservative treatment.<br />
J Shoulder Elbow Surg. 2008; 17(2):220-<br />
225.<br />
4. Dewar FP, Barr<strong>in</strong>gton TW. The treatment<br />
of chronic acromio-clavicular dislocation. J<br />
Bone Jo<strong>in</strong>t Surg Br. 1965; 47(1):32-35.<br />
5. Cadenat FM. The treatment of dislocations<br />
and fractures of the outer end of the clavicle.<br />
Int Cl<strong>in</strong>. 1917; 1:145-169.<br />
6. Takase K. The coracoclavicular ligaments:<br />
an anatomic study. Surg Radiol Anat. 2010;<br />
32(7):683-688.<br />
7. Takase K, Kumakura T, Kono R, Sh<strong>in</strong>mura<br />
K. <strong>Surgical</strong> techniques and therapeutic results<br />
of anatomical reconstruction coracoclavicular<br />
ligaments <strong>for</strong> acromioclavicular<br />
jo<strong>in</strong>t dislocations. Eur J Orthop Surg Traumatol.<br />
2012; 22(7):555-560.<br />
8. Ellman H, Hanker G, Bayer M. Repair of<br />
the rotator cuff. J Bone Jo<strong>in</strong>t Surg Am. 1986;<br />
68(8):1136-1144.<br />
9. Tossy JD, Mead NC, Sigmond HM. <strong>Acromioclavicular</strong><br />
separations: useful and practical<br />
classification <strong>for</strong> treatment. Cl<strong>in</strong> Orthop<br />
Relat Res. 1963; (28):111-119.<br />
10. Phemister DB. The treatment of dislocation<br />
of the acromioclavicular jo<strong>in</strong>t by open reduction<br />
and threaded-wire fixation. J Bone<br />
Jo<strong>in</strong>t Surg Am. 1942; 24(1):166-168.<br />
11. Neviaser JS. <strong>Acromioclavicular</strong> dislocation<br />
treated by transference of the coracoacromial<br />
ligament. AMA Arch Surg. 1952;<br />
64(3):292-297.<br />
12. Bosworth BM. <strong>Acromioclavicular</strong> dislocation:<br />
end-results of screw suspension treatment.<br />
Ann Surg. 1948; 127(1):98-111.<br />
13. Weaver JK, Dunn HK. Treatment of acromioclavicular<br />
<strong>in</strong>juries, especially complete<br />
acromioclavicular separation. J Bone Jo<strong>in</strong>t<br />
Surg Am. 1972; 54(6):1187-1194.<br />
14. Skjeldal S, Lundblad R, Dullerud R. Coracoid<br />
process transfer <strong>for</strong> acromioclavicular dislocation.<br />
Acta Orthop Scand. 1988; 59(2):180-182.<br />
15. Yoo JC, Ahn JH, Yoon JR, Yang JH. Cl<strong>in</strong>ical<br />
results of s<strong>in</strong>gle-tunnel coracoclavicular<br />
ligament reconstruction us<strong>in</strong>g autogenous<br />
semitend<strong>in</strong>osus tendon. Am J Sports Med.<br />
2010; 38(5):950-957.<br />
16. Sloan SM, Budoff JE, Hipp JA, Nguyen L.<br />
Coracoclavicular ligament reconstruction us<strong>in</strong>g<br />
the lateral half of the conjo<strong>in</strong>ed tendon. J<br />
Shoulder Elbow Surg. 2004; 13(2):186-190.<br />
17. Lädermann A, Grosclaude M, Lübbeke A, et<br />
al. <strong>Acromioclavicular</strong> and coracoclavicular<br />
cerclage reconstruction <strong>for</strong> acute acromioclavicular<br />
jo<strong>in</strong>t dislocations. J Shoulder Elbow<br />
Surg. 2011; 20(3):401-408.<br />
18. Marchie A, Kumar A, Catre M. A modified<br />
surgical technique <strong>for</strong> reconstruction of an<br />
acute acromioclavicular jo<strong>in</strong>t dislocation.<br />
Int J Shoulder Surg. 2009; 3(3):66-68.<br />
19. Wei HF, Chen YF, Zeng BF, et al. Triple<br />
Endobutton technique <strong>for</strong> the treatment of<br />
acute complete acromioclavicular jo<strong>in</strong>t dislocations:<br />
prelim<strong>in</strong>ary results. Int Orthop.<br />
2011; 35(4):555-559.<br />
20. Salzmann GM, Walz L, Buchmann S, Glabgly<br />
P, Venjakob A, Imhoff AB. Arthroscopically<br />
assisted 2-bundle anatomical reduction<br />
of acute acromioclavicular jo<strong>in</strong>t separations.<br />
Am J Sports Med. 2010; 38(6):1179-1187.<br />
e1282<br />
ORTHOPEDICS | <strong>Healio</strong>.com/Orthopedics